Abstract
This study aimed to verify whether sleep quality is a mediator of the relationship between burnout, stress and multisite pain in healthcare workers in a longitudinal study with 12 months of follow-up during the COVID-19 pandemic. Online questionnaires were used for data collection. The sociodemographic questionnaire contained personal and occupational data. The short version of the Copenhagen Psychosocial Questionnaire (COPSOQ II-Br) was used to assess burnout and stress. The Pittsburgh Sleep Quality Index (PSQI-Br) assessed sleep quality over one month. The Nordic Musculoskeletal Questionnaire (NMQ) aimed to identify the presence of multisite musculoskeletal pain in the last 12 months and the last 7 days. Mediation analysis was used to verify whether the effect of the predictor variables (burnout and stress) on the dependent variable (number of pain sites in the last 12 months and 7 days) was due to an intervening variable (sleep quality). Stress and burnout were associated with multisite pain in healthcare workers in the last 12 months and the last 7 days. Sleep quality was a significant mediator of this association in the last 12 months, indicating that some of the association between burnout, stress and multisite pain can be explained by poor sleep quality. Thus, a comprehensive approach to long-term multisite pain should consider psychosocial aspects such as burnout, stress and sleep quality.
1. Introduction
The health status of healthcare workers can affect their quality of life and the treatment offered to their patients. The COVID-19 pandemic has brought this issue to the forefront, given the high work demands and rapid changes in this sector. Physical, mental and emotional overload of healthcare workers has always existed [1]; however, events such as outbreaks and pandemics deserve attention [2].
Burnout symptoms can be an expression of emotional overload, where the response to work-related chronic stress causes damage at cognitive and emotional levels due to extreme exhaustion, stress and physical exhaustion resulting from work situations [3]. Burnout symptoms can differ within and between individuals [4] and can lead to sick leave and absence from work [5]. A systematic review of medical students in Brazil before the pandemic identified the prevalence of burnout (13%), stress (50%), poor sleep quality (52%) and excessive daytime sleepiness (46%) [6]. Another study of physicians conducted before the pandemic found that anesthesiologists affected by burnout report a loss of efficiency and less value for their achievements, but still consider that they do a good job compared with non-medical professionals [7]. Systematic reviews of healthcare workers during global infectious disease outbreaks, for example, COVID-19, SARS, H1N1, EBOLA and MERS found high incidences of burnout (28–32%), acute stress (30%), post-traumatic stress disorder (13%) and insomnia (40%) [2,6,8].
Another condition that can cause emotional and physical exhaustion is occupational stress. Theories about stress emphasize the influence of psychic factors on bodily functions [9], leading to a negative or positive response in the stressor, which may have an impact on mental or physical health due to the balance between perceived demands and individuals’ resources and skills [10]. A study in Argentina (2021) found a prevalence of stress (94%) and burnout (74%) in physicians [11]. In the USA, another study classified healthcare workers into those with high or very high daily stress (30%) and those with high or very high burnout (49%) [12]. Other studies also found high rates of burnout (57%, 49% and 44%), emotional exhaustion (36%, 29% and 92%), and depersonalization (58%, 18% and 27%) in this population [13,14,15].
Relationships between burnout, stress and musculoskeletal symptoms are present in the literature [16,17]. In healthcare workers, general stress and work-related stress were considered strong risk factors for musculoskeletal disorders [17].
More than half of nurses in a study conducted in Vietnam had musculoskeletal symptoms in the last 12 months, with a prevalence of 51% in men and 58% in women [18]. Physicians and other healthcare workers also had high incidences of musculoskeletal pain in the neck (60%), shoulders (52%) and lower back (49%) [19,20,21].
In addition to burnout being considered an important predictor of musculoskeletal pain [22], it can also interfere with sleep quality [5]. Sleep disturbances are important causative and maintaining factors for burnout [23] and sleep physiology improves following recovery from burnout [24].
Stress can also interfere with sleep quality. A study of healthcare workers conducted in India during the pandemic found that 36% of workers had poor sleep quality, while 25% had moderate burnout [25]. Poor sleep and work-related stress can interfere with patient care [26]. Nurses with high levels of stress also report lower sleep quality [27], while nurses with high levels of burnout and traumatic stress are more likely to have physical and mental health problems, with sleep disturbance being a partial mediator of these relationships [28].
Insomnia has also been associated with pain and sleep disturbances in various body parts in nurses [29,30]. Low back pain is associated with lower sleep quality [31]. Nurses who sleep for less than 7 h have more chronic discomfort in the neck and shoulders [32] and patients with chronic musculoskeletal pain report more insomnia [33].
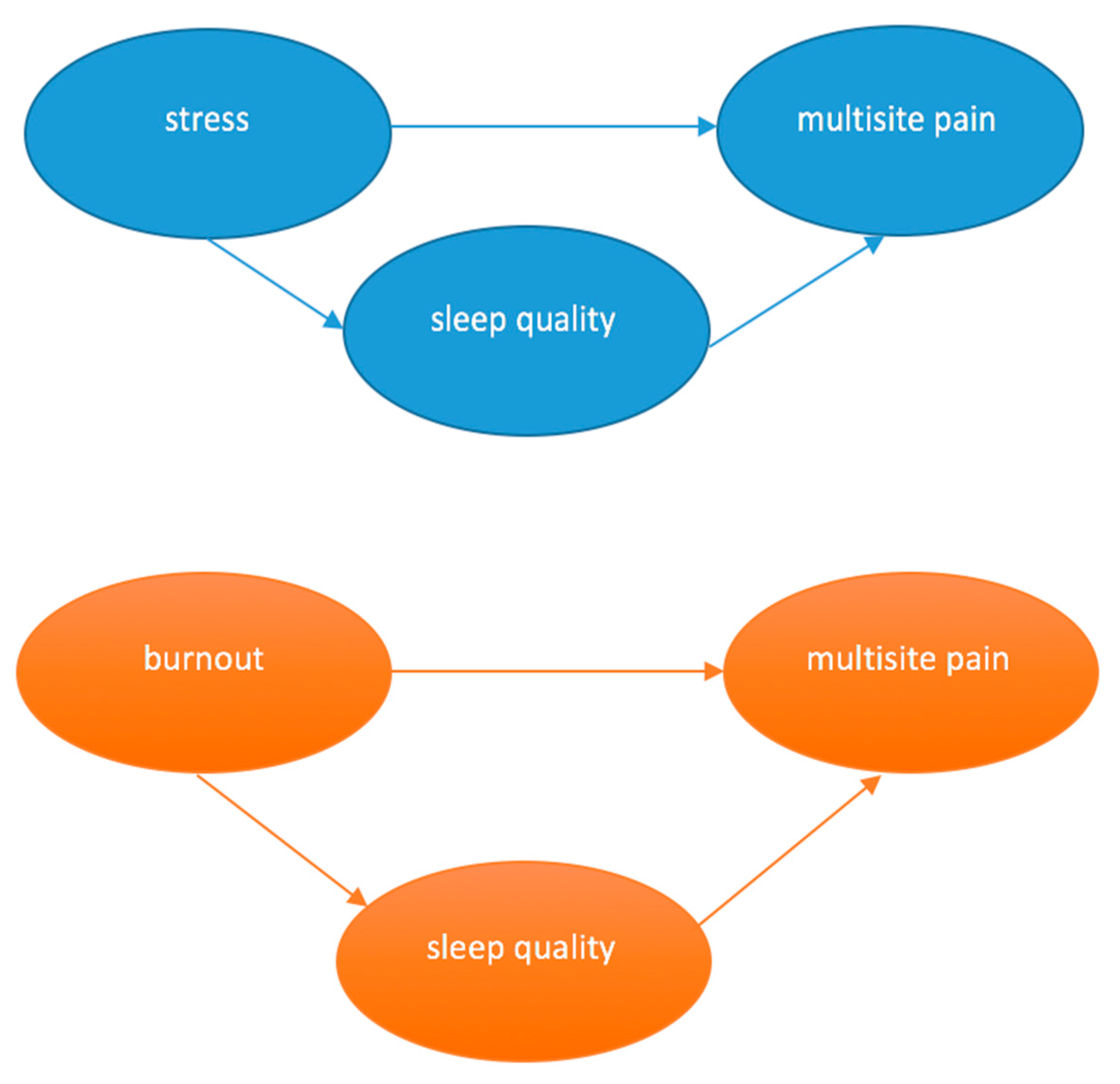
Mediation analysis can clarify the relationship between variables and outcomes, as the measurement model is important for understanding these mechanisms. The mediating variable that accounts for the relationship between a predictor and an outcome can be a qualitative or quantitative one and can fully explain the relationship (full mediation) or explain the relationship to a limited degree only (partial mediation), assuming a three-variable system (Figure 1). In this model, two existing paths can lead to the outcome (dependent) variable: the direct effect of the independent variable on the dependent variable and the effect of the mediating variable on the dependent variable, and a path that connects the independent variable to the mediating variable [34,35,36].
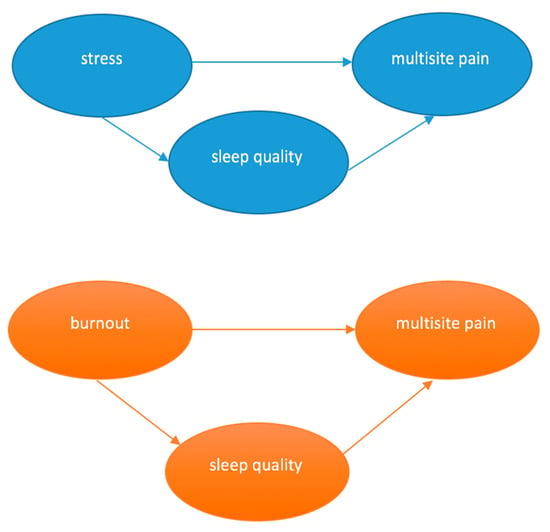
Figure 1.
Schematic representation of stress and burnout as multisite pain predictors mediated by sleep quality based on Hayes’s measurement model 4 [34].
However, the mediation relationship between psychosocial aspects and musculoskeletal pain is inconclusive [37]. Considering that we did not find similar studies in the literature, it is important to examine relationships between burnout, stress, sleep quality and multisite musculoskeletal pain in the last 12 months and the last 7 days. Therefore, the objective of this study was to verify whether sleep quality is a full or partial mediator of the relationship between burnout, stress and multisite pain in healthcare workers in a longitudinal study with a 12-month follow-up during the COVID-19 pandemic.
2. Materials and Methods
2.1. Study Design
This was a longitudinal study of healthcare workers in Brazil conducted during the COVID-19 pandemic between 19 June 2021 and 18 December 2022. The STrengthening the Reporting of OBservational Studies in Epidemiology (STROBE) statement checklist was followed [38].
2.2. Participants
We analyzed data from the HEROES (HEalth conditions of healthcaRe wOrkErS—HEROES) cohort composed of 125 healthcare workers [39]. For this study, baseline and quarterly follow-up data collected over 12 months were considered. The project was approved by the Research Ethics Committee (CAAE: 39705320.9.0000.5504).
Recruitment of participants was conducted through the Internet, using social networks and e-mails available on institutional websites. Posts about the project were placed on Instagram, Facebook and YouTube. In addition, e-mails were sent to public hospitals, Departments and Health Units for dissemination.
The inclusion criteria were: healthcare worker in the National Health System, aged between 18 and 60 years old and active in care activities. Participation was voluntary and there was no financial incentive. Students, retirees, duplicate responses and inconsistent data were excluded.
2.3. Data Collection Instruments
Online questionnaires were used for data collection. The sociodemographic questionnaire contained personal and occupational data, including age, sex, marital status, education, smoking, use of medication and working hours.
The short version of the Copenhagen Psychosocial Questionnaire (COPSOQ II-Br) was used to assess burnout and stress [40,41,42]. This questionnaire consists of 23 dimensions and 40 questions [40]. The questions are related to the last four weeks and are scored based on a Likert scale with 5 response options. The dimensions of burnout (18A + 18B) and stress (19A + 19B) are scored as follows: 0: not at all; 1: a small part of the time; 2: part of the time; 3: a large part of the time; 4: all the time. The scores range from 0 to 8. Burnout and stress were calculated by summing the answers to the individual questions for each dimension [40].
The Pittsburgh Sleep Quality Index (PSQI-Br) assesses sleep quality and disturbances over one month. It consists of 19 questions whose responses are obtained through self-reporting and 5 questions that are directed at the spouse or roommate. The final 5 questions are used only for clinical practice and do not contribute to the total index score. The 19 questions are categorized into 7 components, rated on scores from 0 (no difficulty) to 3 (severe difficulty). The PSQI components are subjective sleep quality (C1), sleep latency (C2), sleep duration (C3), habitual sleep efficiency (C4), sleep disturbances (C5), use of sleeping medication (C6) and daytime sleep dysfunction (C7). The sums of the values attributed to the 7 components range from 0 to 21 and the higher the number, the worse the sleep quality [43]. The PSQI-Br was translated and validated in the Brazilian population [44].
The Nordic Musculoskeletal Questionnaire (NMQ) aims to identify the presence of musculoskeletal symptoms in different body regions: neck, shoulders, elbows, wrists/hands, thoracic spine, lumbar spine, hip, knees and ankles/feet [45]. It assesses the presence of symptoms, the occurrence of functional disability and seeking help from a health professional 12 months and/or 7 days prior to data collection. The answers have a dichotomous characteristic (presence or absence). For this study, we used the validated NMQ Brazilian version [46] and analyzed only data on symptoms in the last 12 months and the last 7 days.
2.4. Data Analysis
Data were analyzed descriptively (frequencies, means, standard deviation and confidence intervals) using SPSS software (version 23.0). Mediation analysis was performed using the Process macro developed by Hayes [34] in the SPSS statistical program. The dependent variable (Y) was the number of regions with pain in the last 12 months and the last 7 days, ranging from 0 to 9 sites. The independent or predictive variables (X) were burnout and stress (ranging from 0 to 8 points) included in separate models (Figure 1). The mediating variable (M) was the total sleep quality score (ranging from 0 to 21 points).
Mediation analysis enables the assessment of whether the effect of a predictor variable (burnout and stress) on a dependent variable (number of regions with pain) is due to an intervening variable (sleep quality). The results of the mediation analysis are reported using the total effect (c), indirect effect (a*b) and direct effect (c’). The indirect effect (a*b) is the effect of the predictor variable X on the dependent variable Y mediated by M. The direct effect (c’) is the effect of X on Y controlled by the mediator M. The total effect is the sum of direct and indirect effects. The mediated effect, that is, the relative contribution of the mediator, was also calculated.
The assumptions of the mediation analysis were tested, namely: X must predict Y, X must predict M, M must predict Y and X should predict weaker Y after adding M [34]. Bootstrapping is a nonparametric approach to statistical inference that produces standard errors and confidence intervals (CIs) for each of the parameters. Bootstrapping was performed using 5000 resampling steps and 95% CIs for bias correction to investigate indirect effects [34].
The sample size was calculated a posteriori, based on the formula proposed by Fritz and MacKinnon [47]. The formula was applied considering a type I error of 5%, a power of 80%, and one predictor. The sample size varied based on the coefficient obtained in each part of the mediation model, varying from 7 to 78,500 participants. The relationship between sleep and pain was underpowered for all tested associations, with the minimum required number of participants being 274.
3. Results
The healthcare workers (n = 125) who participated in the study aged 38 years were female (83%), married (57%), had completed higher education (80%), used medication (66%), composed the nursing team (58%), worked in the hospital (49%) and had a weekly workload of more than 30 h (71%). The mean values for burnout and stress were high (Table 1). Comparison between groups with no pain/single-site pain and multisite pain identified differences in burnout and stress, with a higher mean in the multisite pain group.

Table 1.
Sociodemographic and personal data of the healthcare workers at baseline (n = 125).
The components of the Pittsburg Sleep Quality Index are presented in Table 2. Most workers reported good subjective sleep quality (58%), acceptable sleep latency (52%), 6 or more hours of sleep (54%), >85% sleep efficiency (62%), up to two sleep disturbances (90%), no use of sleeping medication in the last month (66%) and one daytime dysfunction (58%). Most healthcare workers were classified as poor sleepers (74%). Comparison between groups with no pain/single-site pain and multisite pain identified differences in all components of the PSQI, except sleep duration and habitual sleep efficiency, with worse indices in the multisite pain group.

Table 2.
Components of the Pittsburg Sleep Quality Index (PSQI) at baseline (n = 125).
The number of pain sites in the last 12 months and the last 7 days are presented in Table 3. Most workers reported between 4 and 6 pain sites in the last 12 months and between 0 and 2 pain sites in the last 7 days.

Table 3.
Number of pain sites in the last 12 months and the last 7 days at baseline and follow-up.
The results of the mediation analysis are presented in Table 4 and Table 5. The associations between burnout and multisite pain (c) and between burnout and sleep quality (a) were significant (p < 0.01) at all time points evaluated in the last 12 months. Sleep quality was significantly associated with multisite pain (b) at baseline only (p = 0.04). The association between burnout and pain was significant and weaker after the addition of the mediator (c’) at all the time points evaluated. The mediated effect ranged from 13.6 to 20.4%, indicating a partial mediation effect. For the last 7 days, the associations between burnout and multisite pain (c) and between burnout and sleep quality (a) were significant at all evaluated time points (p < 0.01). However, sleep quality was not significantly associated with multisite pain (b) (p > 0.05). For all time points evaluated, the association between burnout and pain (c’) was weaker after the addition of the mediator, although the mediation effect was not significant.

Table 4.
Mediation analysis between burnout and multisite pain in the last 12 months and the last 7 days, with sleep quality as the mediator.

Table 5.
Mediation analysis between stress and multisite pain in the last 12 months and the last 7 days, with sleep quality as the mediator.
The associations between stress and 12-month multisite pain (c) and between stress and sleep (a) were significant at all time points evaluated (p < 0.01). Sleep quality was significantly associated with 12-month multisite pain (b) at all assessment times, except at the 9-month follow-up (p = 0.07). The association between stress and pain (c’) was significant and weaker after the addition of the mediator at all the time points evaluated. The mediated effect ranged from 21.8 to 30.6%, indicating a partial mediation effect.
For the last 7 days, the associations between stress and multisite pain (c) and between stress and sleep (a) were significant at all time points evaluated (p < 0.01), except at 3 months. Sleep quality was not significantly associated with multisite pain (b) at all assessment times (p > 0.05). The association between stress and pain (c’) was weaker after the addition of the mediator at all the time points evaluated, and the mediation effect was significant at baseline, 6 months and 12 months (Table 5).
4. Discussion
Stress and burnout were significantly associated with multisite pain in the last 12 months and the last 7 days in healthcare workers. Burnout and stress were also significantly associated with sleep quality. Sleep quality was a significant mediator of the relationship between stress and multisite pain in the last 12 months. However, no mediation effect was observed when pain in the last 7 days was analyzed.
Healthcare workers suffer from burnout and stress, with high mean levels of burnout (5.3) and stress (4.9) recorded. Burnout and stress are considered predictors of musculoskeletal pain [22,48] and poor sleep quality [49], but the mediating effect of sleep quality in multisite pain was not clear. This finding can be explained by methodological aspects such as the small sample size used in the follow-up measurements.
A systematic meta-analysis [49] found a positive and significant correlation between high levels of burnout and poor quality of sleep in nurses. The dissatisfaction with sleep quality was also associated with burnout in shift workers [50].
Most healthcare workers were classified as bad sleepers (74%); this was similar to results obtained in Colombian healthcare workers [51]. Although healthcare workers may be more propense to sleep problems due to the nature of their work, a systematic review of Western healthcare workers showed high levels of stress, sleep disturbances, burnout and other illnesses, with more frequent and intense symptoms in women and frontline nurses working during the COVID-19 pandemic [52].
Stress at work has a negative impact on sleep quality [53]. A two-year follow-up study of healthcare workers also showed that stress levels increased and sleep quality worsened during the pandemic [54]. The systematic review by Dragioti [55] corroborates these findings, as healthcare workers affected by COVID-19 suffered from stress and sleep problems (33% and 37%).
Sleep disturbances are associated with pain [56] and sleep deficiencies predict incidences and exacerbations of chronic pain [57], where deprivation and sleep interruptions increase sensitivity and vulnerability to pain and can form a vicious cycle where they maintain and increase each other [58]. Restricting sleep to 6 h can increase pro-inflammatory cytokines [59]. Sleep deprivation is also associated with cognitive impairment [60]. A systematic review of military personnel revealed the association between insufficient sleep and musculoskeletal injuries [61].
A cohort study also showed that stress, non-restorative sleep and physical inactivity are risk factors for the development of chronic pain [62]. Using mediation analysis, Walton et al. [63] found that the association between perceived stress and pain intensity was wholly mediated by sleep interference [63]. Another study investigating the environmental factors that affect the well-being of critical care surgeons found that they were at increased risk of sleep deprivation, musculoskeletal pain and injuries and burnout [64], where sleep-associated problems seemed to precede low back pain and exhaustion in the working population [65]. Thus, it seems that stress and sleep management, as well as ergonomic interventions, post the COVID-19 pandemic are urgent in healthcare services and can help to improve musculoskeletal health.
Limitations and Strengths of the Study
This study provides information on the role of sleep quality as a mediator of the association between burnout, stress and multisite pain in health professionals; however, some limitations must be considered when interpreting the findings. Although the longitudinal nature of the study is a strength, the small sample size and the lack of a priori sample size calculation are limitations. The use of questionnaires to obtain data on burnout, stress and sleep quality can also be a limitation. Specific questionnaires are suggested to assess stress and burnout.
5. Conclusions
Burnout, stress, sleep quality and multisite musculoskeletal pain are topics relevant to healthcare workers in the COVID-19 pandemic context.
Our findings showed that sleep quality mediates the association between stress, burnout and multisite pain in Brazilian healthcare workers in the previous 12 months. Thus, this study highlights the need for a comprehensive approach, which also considers psychosocial work aspects and sleep quality, to multisite pain management.
Author Contributions
Conceptualization, L.M.S.M.d.A.V., V.A.M. and T.d.O.S.; methodology, L.M.S.M.d.A.V., V.A.M. and T.d.O.S.; validation, L.M.S.M.d.A.V., V.A.M. and T.d.O.S.; formal analysis, L.M.S.M.d.A.V. and T.d.O.S.; investigation, L.M.S.M.d.A.V., V.A.M. and T.d.O.S.; resources, V.A.M. and T.d.O.S.; data curation, T.d.O.S.; writing—original draft preparation, L.M.S.M.d.A.V., V.A.M. and T.d.O.S.; writing—review and editing, L.M.S.M.d.A.V., V.A.M. and T.d.O.S.; supervision, V.A.M. and T.d.O.S.; project administration, V.A.M. and T.d.O.S.; funding acquisition, V.A.M. and T.d.O.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES), grant number Finance Code 001, and São Paulo Research Foundation (FAPESP), grant number 2020/10098-1.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Universidade Federal de São Carlos (protocol code 39705320.9.0000.5504; date of approval 12 February 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, T.d.O.S.
Acknowledgments
Hospital Universitário da Universidade Federal de São Carlos (HU-UFSCar), Santa Casa de Misericórdia de São Carlos, Secretaria Municipal de Saúde de São Carlos.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Vittori, A.; Marinangeli, F.; Bignami, E.G.; Simonini, A.; Vergallo, A.; Fiore, G.; Petrucci, E.; Cascella, M.; Pedone, R. Analysis on burnout, job conditions, alexithymia, and other psychological symptoms in a sample of italian anesthesiologists and intensivists, assessed just before the COVID-19 pandemic: An AAROI-EMAC study. Healthcare 2022, 10, 1370. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Ripoll, M.J.; Meneses-Echavez, J.F.; Ricci-Cabello, I.; Fraile-Navarro, D.; Fiol-deRoque, M.A.; Pastor-Moreno, G.; Castro, A.; Ruiz-Pérez, I.; Zamanillo Campos, R.; Gonçalves-Bradley, D.C. Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta-analysis. J. Affect. Disord. 2020, 277, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Edú-Valsania, S.; Laguía, A.; Moriano, J.A. Burnout: A review of theory and measurement. Int. J. Environ. Res. Public Health 2022, 19, 1780. [Google Scholar] [CrossRef] [PubMed]
- Danhof-Pont, M.B.; van Veen, T.; Zitman, F.G. Biomarkers in burnout: A systematic review. J. Psychosom. Res. 2011, 70, 505–524. [Google Scholar] [CrossRef]
- Kärkkäinen, R.; Saaranen, T.; Hiltunen, S.; Ryynänen, O.P.; Räsänen, K. Systematic review: Factors associated with return to work in burnout. Occup. Med. 2017, 67, 461–468. [Google Scholar] [CrossRef]
- Pacheco, J.P.; Giacomin, H.T.; Tam, W.W.; Ribeiro, T.B.; Arab, C.; Bezerra, I.M.; Pinasco, G.C. Mental health problems among medical students in Brazil: A systematic review and meta-analysis. Braz. J. Psychiatry 2017, 39, 369–378. [Google Scholar] [CrossRef]
- Usas, H.; Weilenmann, S.; Princip, M.; Fuchs, W.J.; van Nuffel, M.; von Känel, R.; Spiller, T.R. Physician-specific symptoms of burnout compared to a non-physicians group. Int. J. Environ. Res. Public Health 2023, 20, 2693. [Google Scholar] [CrossRef]
- Busch, I.M.; Moretti, F.; Mazzi, M.; Wu, A.W.; Rimondini, M. What We Have Learned from Two Decades of Epidemics and Pandemics: A Systematic Review and Meta-Analysis of the Psychological Burden of Frontline Healthcare Workers. Psychother. Psychosom. 2021, 90, 178–190. [Google Scholar] [CrossRef]
- Dantzer, R. Stress theories and the somatization process. L’encephale 1995, 21, 3–9. [Google Scholar]
- ILO 2016. International Labour Organization 2016. Available online: https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---safework/documents/publication/wcms_466547.pdf (accessed on 19 July 2023).
- Appiani, F.J.; Cairoli, F.R.; Sarotto, L.; Yaryour, C.; Basile, M.E.; Duarte, J.M. Prevalence of stress, burnout syndrome, anxiety and depression among physicians of a teaching hospital during the COVID-19 pandemic. Arch. Argent. Pediatr. 2021, 119, 317–324. [Google Scholar] [CrossRef]
- Prasad, K.; McLoughlin, C.; Stillman, M.; Poplau, S.; Goelz, E.; Taylor, S.; Nankivil, N.; Brown, R.; Linzer, M.; Cappelucci, K.; et al. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. eClinicalMedicine 2021, 35, 100879. [Google Scholar] [CrossRef] [PubMed]
- Akova, I.; Kiliç, E.; Özdemir, M.E. Prevalence of Burnout, Depression, Anxiety, Stress, and Hopelessness Among Healthcare Workers in COVID-19 Pandemic in Turkey. Inq. J. Health Care Organ. Provis. Financ. 2022, 59, 469580221079684. [Google Scholar] [CrossRef] [PubMed]
- de Medeiros, A.I.C.; de Mesquita, R.B.; Macêdo, F.D.S.; Matos, A.G.D.C.; Pereira, E.D. Prevalence of burnout among healthcare workers in six public referral hospitals in northeastern Brazil during the COVID-19 pandemic: A cross-sectional study. Sao Paulo Med. J. 2022, 140, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Athanasiou, N.; Sakkas, N.; Patrinos, S.; Sakka, E.; Barmparessou, Z.; Tsikrika, S.; Adraktas, A.; Pataka, A.; Migdalis, I.; et al. From Recession to Depression? Prevalence and Correlates of Depression, Anxiety, Traumatic Stress and Burnout in Healthcare Workers during the COVID-19 Pandemic in Greece: A Multi-Center, Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 2390. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Yeh, C.-J.; Lee, C.-M.; Jong, G.-P. Mediation Effect of Musculoskeletal Pain on Burnout: Sex-Related Differences. Int. J. Environ. Res. Public Health 2022, 19, 12872. [Google Scholar] [CrossRef] [PubMed]
- Hämmig, O. Work- and stress-related musculoskeletal and sleep disorders among health professionals: A cross-sectional study in a hospital setting in Switzerland. BMC Musculoskelet. Disord. 2020, 21, 319. [Google Scholar] [CrossRef]
- Nguyen, T.H.; Hoang, D.L.; Hoang, T.G.; Pham, M.K.; Bodin, J.; Dewitte, J.D.; Roquelaure, Y. Prevalence and Characteristics of Multisite Musculoskeletal Symptoms among District Hospital Nurses in Haiphong, Vietnam. BioMed Res. Int. 2020, 2020, 3254605. [Google Scholar] [CrossRef]
- Epstein, S.; Sparer, E.H.; Tran, B.N.; Ruan, Q.Z.; Dennerlein, J.T.; Singhal, D.; Lee, B.T. Prevalence of Work-Related Musculoskeletal Disorders Among Surgeons and Interventionalists: A systematic review and meta-analysis. JAMA Surg. 2018, 153, e174947. [Google Scholar] [CrossRef]
- Dalager, T.; Søgaard, K.; Boyle, E.; Jensen, P.T.; Mogensen, O. Surgery Is Physically Demanding and Associated With Multisite Musculoskeletal Pain: A Cross-Sectional Study. J. Surg. Res. 2019, 240, 30–39. [Google Scholar] [CrossRef]
- dos Santos, E.C.; Andrade, R.D.; Lopes, S.G.R.; Valgas, C. Prevalence of musculoskeletal pain in nursing professionals working in orthopedic setting. Rev. Dor 2017, 18, 298–306. [Google Scholar] [CrossRef]
- Salvagioni, D.A.J.; Melanda, F.N.; Mesas, A.E.; González, A.D.; Gabani, F.L.; De Andrade, S.M. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PLoS ONE 2017, 12, e0185781. [Google Scholar] [CrossRef] [PubMed]
- Grossi, G.; Perski, A.; Osika, W.; Savic, I. Stress-related exhaustion disorder—Clinical manifestation of burnout? A review of assessment methods, sleep impairments, cognitive disturbances, and neuro-biological and physiological changes in clinical burnout. Scand. J. Psychol. 2015, 56, 626–636. [Google Scholar] [CrossRef] [PubMed]
- Ekstedt, M.; Söderström, M.; Åkerstedt, T. Sleep physiology in recovery from burnout. Biol. Psychol. 2009, 82, 267–273. [Google Scholar] [CrossRef]
- Yella, T.; Dmello, M.K. Burnout and sleep quality among community health workers during the pandemic in selected city of Andhra Pradesh. Clin. Epidemiol. Glob. Health 2022, 16, 101109. [Google Scholar] [CrossRef]
- Stimpfel, A.W.; Goldsamt, L.; Liang, E.; Costa, D.K. Work Organization Factors Associated With Nurses’ Stress, Sleep, and Performance: A Pre-pandemic Analysis. J. Nurs. Regul. 2022, 13, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Zarei, S.; Fooladvand, K. Mediating effect of sleep disturbance and rumination on work-related burnout of nurses treating patients with coronavirus disease. BMC Psychol. 2022, 10, 197. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.J.; Wehrlen, L.; Ding, Y.; Ross, A. Professional quality of life, sleep disturbance and health among nurses: A mediation analysis. Nurs. Open 2021, 9, 2771–2780. [Google Scholar] [CrossRef]
- Matre, D.; Nilsen, K.B.; Katsifaraki, M.; Waage, S.; Pallesen, S.; Bjorvatn, B. Pain complaints are associated with quick returns and insomnia among Norwegian nurses, but do not differ between shift workers and day only workers. Int. Arch. Occup. Environ. Health 2020, 93, 291–299. [Google Scholar] [CrossRef]
- Dong, H.; Zhang, Q.; Zhang, Z.; Zhu, C. Association of sleep disturbance with shift work, occupational stress, and musculoskeletal pain in Chinese public hospital emergency workers: A multicentre cross-sectional study. Chronobiol. Int. 2022, 39, 886–894. [Google Scholar] [CrossRef]
- AlHamam, N.M.; Buhalim, R.A.; AlSaeed, M.N.; AlFuraikh, B.F.; AlJughaiman, M.S. Low back pain and its correlations with poor sleep quality among health care providers. J. Taibah Univ. Med. Sci. 2021, 17, 28–37. [Google Scholar] [CrossRef]
- Chin, W.; Chen, Y.; Lin, T.; Guo, Y.L.; Shiao, J.S.C. Short sleep and chronic neck and shoulder discomfort in nurses. J. Occup. Health 2021, 63, e12236. [Google Scholar] [CrossRef] [PubMed]
- Garnæs, K.K.; Mørkved, S.; Tønne, T.; Furan, L.; Vasseljen, O.; Johannessen, H.H. Mental health among patients with chronic musculoskeletal pain and its relation to number of pain sites and pain intensity, a cross-sectional study among primary health care patients. BMC Musculoskelet. Disord. 2022, 23, 1115. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis a Regression-Based Approach, 3rd ed.; Guilford Press: London, UK, 2022. [Google Scholar]
- Liu, J.; Ulrich, C. Mediation analysis in nursing research: A methodological review. Contemp. Nurse 2016, 52, 643–656. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, R.R.N.; Cashin, A.G.; Bagg, M.K.; Gustin, S.M.; Lee, H.; McAuley, J.H. A Systematic Review of the Reporting Quality of Observational Studies That Use Mediation Analyses. Prev. Sci. 2022, 23, 1041–1052. [Google Scholar] [CrossRef]
- Koch, P.; Schablon, A.; Latza, U.; Nienhaus, A. Musculoskeletal pain and effort-reward imbalance—A systematic review. BMC Public Health 2014, 14, 37. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; Strobe Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med. 2007, 4, e297. [Google Scholar] [CrossRef]
- Sato, T.D.O.; de Faria, B.S.F.; Albuquerque, B.B.; da Silva, F.L.; Rohwedder, L.S.; de Azevedo, R.T.; Gonçalves, J.S.; Vieira, L.M.S.M.D.A.; Triches, M.I.; de Sousa, R.A.; et al. Poor Health Conditions among Brazilian Healthcare Workers: The Study Design and Baseline Characteristics of the HEROES Cohort. Healthcare 2022, 10, 2096. [Google Scholar] [CrossRef]
- Gonçalves, J.S.; Moriguchi, C.S.; Chaves, T.C.; Sato, T.D.O. Cross-cultural adaptation and psychometric properties of the short version of COPSOQ II-Brazil. Rev. Saúde Públ. 2021, 55, 69. [Google Scholar] [CrossRef]
- Kristensen, T.S.; Hannerz, H.; Høgh, A.; Borg, V. The Copenhagen Psychosocial Questionnaire—A tool for the assessment and improvement of the psychosocial work environment. Scand. J. Work Environ. Health 2005, 31, 438–449. [Google Scholar] [CrossRef]
- Pejtersen, J.H.; Søndergå, T.; Kristensen, R.D.; Borg, V.; Bjorner, J.B. The second version of the Copenhagen Psychosocial Questionnaire. Scand. J. Public Health 2010, 38, 8–24. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Bertolazi, A.N.; Fagondes, S.C.; Hoff, L.S.; Dartora, E.G.; Miozzo, I.C.D.S.; de Barba, M.E.F.; Barreto, S.S.M. Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med. 2011, 12, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- De Barros, E.N.C.; Alexandre, N.M.C. Cross-cultural adaptation of the Nordic musculoskeletal questionnaire. Int. Nurs. Rev. 2003, 50, 101–108. [Google Scholar] [CrossRef]
- Fritz, M.S.; MacKinnon, D.P. Required Sample Size to Detect the Mediated Effect. Psychol. Sci. 2007, 18, 233–239. [Google Scholar] [CrossRef]
- Crofford, L.J. Chronic Pain: Where the Body Meets the Brain. Trans. Am. Clin. Climatol. Assoc. 2015, 126, 167–183. [Google Scholar]
- Membrive-Jiménez, M.J.; Gómez-Urquiza, J.L.; Suleiman-Martos, N.; Velando-Soriano, A.; Ariza, T.; De la Fuente-Solana, E.I.; la Fuente, G.A.C.-D. Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis. Healthcare 2022, 10, 954. [Google Scholar] [CrossRef]
- Vidotti, V.; Ribeiro, R.P.; Galdino, M.J.Q.; Martins, J.T. Burnout Syndrome and shift work among the nursing staff. Rev. Latino-Am. Enferm. 2018, 26, e3022. [Google Scholar] [CrossRef] [PubMed]
- Waich, A.; Barahona-Correa, J.E.; Figueredo, M.D.C.; Rondón-Sepúlveda, M.A.; Ruiz, A.J.; Castellanos, J.C.; Hidalgo-Martínez, P. Sleep Quality, Insomnia, and Perceived Stress among Colombian Healthcare Workers during the COVID-19 Pandemic. Sleep Sci. 2023, 16, 44–50. [Google Scholar] [CrossRef]
- Danet, A.D. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review. Med. Clin. 2021, 156, 449–458. [Google Scholar] [CrossRef]
- Qin, A.; Hu, F.; Qin, W.; Dong, Y.; Li, M.; Xu, L. Educational degree differences in the association between work stress and depression among Chinese healthcare workers: Job satisfaction and sleep quality as the mediators. Front. Public Health 2023, 11, 1138380. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.; Haji, E.A.; Saif, Z.Q.; Aljeeran, N.O.; Aljawder, A.I.; Shehabdin, F.N.; Fekih-Romdhane, F.; Trabelsi, K.; BaHammam, A.S.; Vitiello, M.V. Sleep Quality Worsens While Perceived Stress Improves in Healthcare Workers over Two Years during the COVID-19 Pandemic: Results of a Longitudinal Study. Healthcare 2022, 10, 1588. [Google Scholar] [CrossRef]
- Dragioti, E.; Li, H.; Tsitsas, G.; Lee, K.H.; Choi, J.; Kim, J.; Choi, Y.J.; Tsamakis, K.; Estradé, A.; Agorastos, A.; et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 2022, 94, 1935–1949. [Google Scholar] [CrossRef] [PubMed]
- Dzierzewski, J.M.; Williams, J.M.; Roditi, D.; Marsiske, M.; McCoy, K.; McNamara, J.; Dautovich, N.; Robinson, M.E.; McCrae, C.S. Daily Variations in Objective Nighttime Sleep and Subjective Morning Pain in Older Adults with Insomnia: Evidence of Covariation over Time. J. Am. Geriatr. Soc. 2010, 58, 925–930. [Google Scholar] [CrossRef]
- Finan, P.H.; Goodin, B.R.; Smith, M.T. The Association of Sleep and Pain: An Update and a Path Forward. J. Pain 2013, 14, 1539–1552. [Google Scholar] [CrossRef]
- Lautenbacher, S.; Kundermann, B.; Krieg, J.-C. Sleep deprivation and pain perception. Sleep Med. Rev. 2006, 10, 357–369. [Google Scholar] [CrossRef] [PubMed]
- Vgontzas, A.N.; Zoumakis, E.; Bixler, E.O.; Lin, H.-M.; Follett, H.; Kales, A.; Chrousos, G.P. Adverse Effects of Modest Sleep Restriction on Sleepiness, Performance, and Inflammatory Cytokines. J. Clin. Endocrinol. Metab. 2004, 89, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Protective and damaging effects of stress mediators: Central role of the brain. Dialogues Clin. Neurosci. 2006, 8, 367–381. [Google Scholar] [CrossRef]
- Lisman, P.; Ritland, B.M.; Burke, T.M.; Sweeney, L.; A Dobrosielski, D. The Association Between Sleep and Musculoskeletal Injuries in Military Personnel: A Systematic Review. Mil. Med. 2022, 187, 1318–1329. [Google Scholar] [CrossRef]
- Lindell, M.; Grimby-Ekman, A. Stress, non-restorative sleep, and physical inactivity as risk factors for chronic pain in young adults: A cohort study. PLoS ONE 2022, 17, e0262601. [Google Scholar] [CrossRef]
- Walton, D.M.; Pourkazemi, F.; Ghodrati, M.; Elliott, J.M. A Mediational Analysis of Stress, Inflammation, Sleep, and Pain in Acute Musculoskeletal Trauma. Clin. J. Pain 2020, 36, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Hess, A.; Porter, M.; Byerly, S. Environmental Factors Impacting Wellness in the Trauma Provider. Curr. Trauma Rep. 2023, 9, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Elfering, A.; Kottwitz, M.U.; Tamcan, Ö.; Müller, U.; Mannion, A.F. Impaired sleep predicts onset of low back pain and burnout symptoms: Evidence from a three-wave study. Psychol. Health Med. 2018, 23, 1196–1210. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).