The Cost and the Value of Stroke Care in Greece: Results from the SUN4P Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Analysis Framework and Study Population
2.2. Direct Healthcare Costs
2.3. Loss of Productivity and Informal Care Cost
2.4. Quality-Adjusted Life Years
2.5. Statistical Analysis
2.6. Ethics
3. Results
3.1. Total Costs of Illness and Outcomes
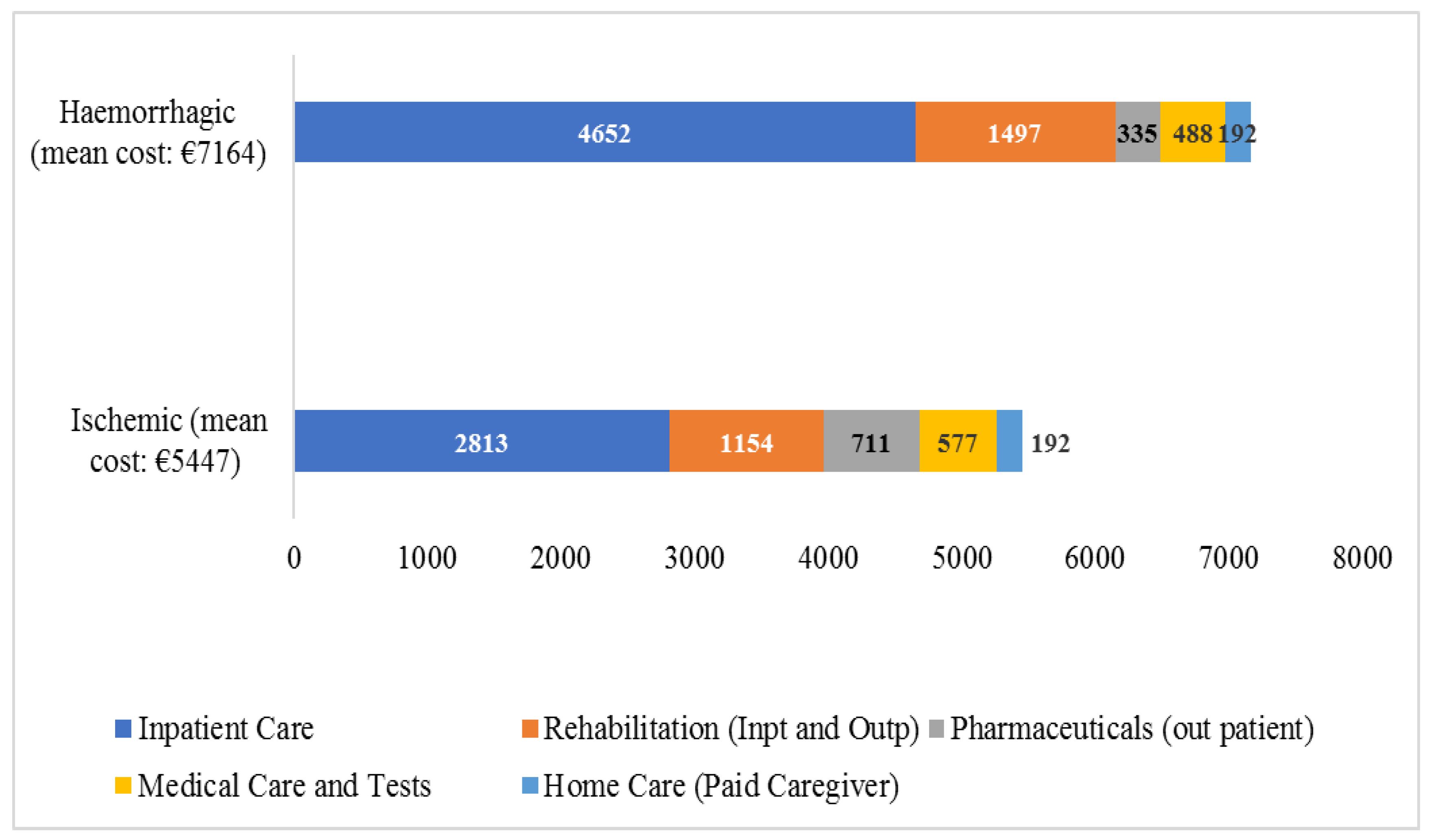
3.2. Average Direct Healthcare Cost per Type of Care and Type of Stroke
3.3. Loss of Productivity
4. Discussion
Policy Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feigin, V.L.; Brainin, M.; Norrving, B.; Martins, S.; Sacco, R.L.; Hacke, W.; Fisher, M.; Pandian, J.; Lindsay, P. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int. J. Stroke Off. J. Int. Stroke Soc. 2022, 17, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Feigin, V.L.; Nguyen, G.; Cercy, K.; Johnson, C.O.; Alam, T.; Parmar, P.G.; Abajobir, A.A.; Abate, K.H.; Abd-Allah, F.; Abejie, A.N.; et al. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N. Engl. J. Med. 2018, 379, 2429–2437. [Google Scholar] [PubMed]
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abedi, V.; et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef] [PubMed]
- Barrenho, E.; Haywood, P.; Kendir, C.; Klazinga, N.S. International comparisons of the quality and outcomes of integrated care: Findings of the OECD pilot on stroke and chronic heart failure. OECD Health Work. Pap. 2022. [Google Scholar] [CrossRef]
- Wafa, H.A.; Wolfe, C.D.A.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of Stroke in Europe: Thirty-Year Projections of Incidence, Prevalence, Deaths, and Disability-Adjusted Life Years. Stroke 2020, 51, 2418–2427. [Google Scholar] [CrossRef] [PubMed]
- Wein, T.; Mancini, J.; Rogoza, R.; Pericleous, L. New View on the Canadian Burden of Stroke: Productivity Loss in Adults Who Return to Work. Can. J. Neurol. Sci. 2021, 48, 421–424. [Google Scholar] [CrossRef] [PubMed]
- Donkor, E.S. Stroke in the 21st Century: A Snapshot of the Burden, Epidemiology, and Quality of Life. Stroke Res. Treat. 2018, 2018, 3238165. [Google Scholar]
- Luengo-Fernandez, R.; Violato, M.; Candio, P.; Leal, J. Economic burden of stroke across Europe: A population-based cost analysis. Eur. Stroke J. 2020, 5, 17–25. [Google Scholar] [CrossRef]
- Karantali, E.; Vemmos, K.; Tsampalas, E.; Xynos, K.; Karachalia, P.; Lambrou, D.; Angeloglou, S.; Kazakou, M.; Karagianni, A.; Aravantinou-Fatorou, K.; et al. Temporal trends in stroke incidence and case-fatality rates in Arcadia, Greece: A sequential, prospective, population-based study. Int. J. Stroke 2022, 17, 37–47. [Google Scholar] [CrossRef]
- Kritikou, P.; Spengos, K.; Zakopoulos, N.; Tountas, Y.; Yfantopoulos, J.; Vemmos, K. Resource utilization and costs for treatment of stroke patients in an acute stroke unit in Greece. Clin. Neurol. Neurosurg. 2016, 142, 8–14. [Google Scholar] [CrossRef]
- Gioldasis, G.; Taleli, P.; Chroni, E.; Daouli, J.; Papapetropoulos, T.; Elul, J. In hospital direct cost of acute ischemic and hemorrhagic stroke in Greece. Acta Neurol. Scand. 2008, 118, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Siskou, O.; Korompoki, E.; Ntaios, G.; Tsampalas, E.; Alexopoulou, H.; Kalliontzakis, I.; Kouridaki, A.; Tountopoulou, A.; Kouzi, I.; Vasilopoulou, S.; et al. Access of Stroke Patients’ to Optimal Healthcare Technology in Greece: Messages to Policy Makers. Stud. Health Technol. Inform. 2020, 272, 421–424. [Google Scholar] [PubMed]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluation of Health Care Programmes; Oxford University Press: Cary, NC, USA, 2015. [Google Scholar]
- Chapman, C.S.; Kern, A.; Laguecir, A.; Angelé-Halgand, N.; Angert, A.; Campenale, C.; Cinquini, L.; Doyle, G.; Garrot, T.; Hansen, A.; et al. Interantional Approaches to Clinical Costing. Healthcare Financial Management Association and Monitor and Health Management Group at Imperial College Business School. December 2013. Available online: https://www.hfma.org.uk/docs/default-source/our-networks/healthcare-costing-for-value-institute/costing/international-approaches-to-clinical-costing.pdf?sfvrsn=9ec6b4e4_0 (accessed on 5 September 2023).
- Papastefanatos, G.; Papastefanatos, S.; Korompoki, E.; Galanis, P.; Konstantakopoulou, O.; Karagkouni, I.; Gallos, P.; Ntaios, G.; Vemmos, K.; Siskou, O. Sun4Patients Web Platform: Facilitating Long-Term Monitoring of Stroke Patients. Stud. Health Technol. Inform. 2020, 272, 411–412. [Google Scholar] [PubMed]
- Broderick, J.P.; Adeoye, O.; Elm, J. Evolution of the Modified Rankin Scale and Its Use in Future Stroke Trials. Stroke 2017, 48, 2007–2012. [Google Scholar] [CrossRef] [PubMed]
- Ni, W.; Kunz, W.G.; Goyal, M.; Ng, Y.L.; Tan, K.; De Silva, D.A. Lifetime quality of life and cost consequences of delays in endovascular treatment for acute ischaemic stroke: Acost-effectiveness analysis from a Singapore healthcare perspective. BMJ Open. 2020, 10, e036517. [Google Scholar] [CrossRef] [PubMed]
- Korompoki, E.; Ntaios, G.; Tountopoulou, A.; Mavraganis, G.; Tsampalas, E.; Kalliontzakis, I.; Vassilopoulou, S.; Manios, E.; Savvopoulos, C.; Milionis, H.; et al. Quality indicators and clinical outcomes of acute stroke: Results from a prospective multicenter registry in Greece (SUN4P). Eur. J. Intern. Med. 2023; submitted. [Google Scholar]
- SAFE. The Economic Impact of Stroke. At What Cost the Economic Impact of Stroke in Europe. Available online: https://www.safestroke.eu/economic-impact-of-stroke/ (accessed on 30 May 2023).
- Andersen, K.K.; Olsen, T.S.; Dehlendorff, C.; Kammersgaard, L.P. Hemorrhagic and ischemic strokes compared: Stroke severity, mortality, and risk factors. Stroke 2009, 40, 2068–2072. [Google Scholar] [CrossRef]
- Wang, J.; Wang, J.; Qiu, S.; Zhou, C.; Zhang, H.; Li, Q.; Sun, S. Pharmaceutical care program for ischemic stroke patients: A randomized controlled trial. Int. J. Clin. Pharm. 2021, 43, 1412–1419. [Google Scholar] [CrossRef]
- Evers, S.M.; Struijs, J.N.; Ament, A.J.; Genugten, M.L.V.; Jager, J.H.; Bos, G.A.V.D. International comparison of stroke cost studies. Stroke 2004, 35, 1209–1215. [Google Scholar] [CrossRef]
- Kavga, A.; Kalemikerakis, I.; Faros, A.; Milaka, M.; Tsekoura, D.; Skoulatou, M.; Tsatsou, I.; Govina, O. The Effects of Patients’ and Caregivers’ Characteristics on the Burden of Families Caring for Stroke Survivors. Int. J. Environ. Res. Public Health 2021, 18, 7298. [Google Scholar] [CrossRef]
- Koumanakos, G. 2015 Trends and Challenges in Home Care in Greece. In Proceedings of the ErgocareBank International Conference, The best Ergonomic Practices in Age Care, Argostoli, Greece, 17–18 September 2015. [Google Scholar]
- Lamura, G.; Mnich, E.; Nolan, M.; Wojszel, B.; Krevers, B.; Mestheneos, L.; Döhner, H.; EUROFAMCARE Group. Family carers’ experiences using support services in Europe: Empirical evidence from the EUROFAMCARE study. Gerontologist 2008, 48, 752–771. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Cadilhac, D.A.; Thompson, S.; Gommans, J.; Davis, A.; Barber, P.A.; Fink, J.; Harwood, M.; Levack, W.; McNaughton, H.; et al. Comparison of stroke care costs in urban and non-urban hospitals and its association with Outcomes in New Zealand: A nationwide economic evaluation. Stroke 2023, 54, 848–856. [Google Scholar] [CrossRef] [PubMed]
- de Sousa, D.A.; von Martial, R.; Abilleira, S.; Gattringer, T.; Kobayashi, A.; Gallofré, M.; Fazekas, F.; Szikora, I.; Feigin, V.; Caso, V.; et al. Access to and delivery of acute ischemic stroke treatments: A survey of national scientific societies and stroke experts in 44 European countries. Eur. Stroke J. 2019, 4, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Lahr, M.M.; van der Zee, D.J.; Luijckx, G.J.; Buskens, E. Optimizing acute stroke care organization: A simulation study to assess the potential to increase intravenous thrombolysis rates and patient gains. BMJ Open 2020, 10, e032780. [Google Scholar] [CrossRef] [PubMed]
- Eurostat Data Base, Health Care Expenditure SHA (2011). Available online: https://ec.europa.eu/eurostat/web/main/data/database (accessed on 20 May 2023).
- Salvadori, E.; Papi, G.; Insalata, G.; Rinnoci, V.; Donnini, I.; Martini, M.; Falsini, C.; Hakiki, B.; Romoli, A.; Barbato, C.; et al. Comparison between Ischemic and Hemorrhagic Strokes in Functional Outcome at Discharge from an Intensive Rehabilitation Hospital. Diagnostics 2020, 11, 38. [Google Scholar] [CrossRef] [PubMed]
- Vemmos, K.; Boubouchairopoulou, N.; Stafylas, P.; Vitsou, E.; Giannakoulas, G.; Ntaios, G.; Milionis, H.; Hahalis, G.; Parthenakis, F.; Tsioufis, K. Estimation of the economic burden of atrial fibrillation-related stroke in Greece. Expert Rev. Pharmacoecon. Outcomes Res. 2022, 22, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Bettger, J.; Cadilhac, D. Stroke Care Costs and Cost-Effectiveness to Inform Health Policy. Stroke 2022, 53, 2078–2081. [Google Scholar] [CrossRef]
- Joo, H.; Wang, G.; George, M.G. Age-Specific Cost Effectiveness of Using Intravenous Recombinant Tissue Plasminogen Activator for Treating Acute Ischemic Stroke. Am. J. Prev. Med. 2017, 53, S205–S212. [Google Scholar] [CrossRef][Green Version]
- Pan, Y.; Chen, Q.; Zhao, X.; Liao, X.; Wang, C.; Du, W.; Liu, G.; Liu, L.; Wang, C.; Wang, Y.; et al. Cost-Effectiveness of Thrombolysis within 4.5 Hours of Acute Ischemic Stroke in China. PLoS ONE 2014, 9, e110525. [Google Scholar] [CrossRef]
- Ehlers, L.; Andersen, G.; Clausen, L.B.; Bech, M.; Kjølby, M. Cost-effectiveness of intravenous thrombolysis with alteplase within a 3-hour window after acute ischemic stroke. Stroke 2007, 38, 85–89. [Google Scholar] [CrossRef]
- Kazley, A.S.; Simpson, K.N.; Simpson, A.; Jauch, E.; Adams, R.J. Optimizing the Economic Impact of rtPA Use in a Stroke Belt State: The Case of South Carolina. Am. Health Drug Benefits 2013, 6, 155–163. [Google Scholar] [PubMed]
- Stafylas, P.; Siskou, O.; Galanis, P.; Konstantakopoulou, O.; Karagkouni, I.; Karaiskou, M.; Tountopoulou, A.; Kouzi, I.; Vasilopoulou, S.; Kalliontzakis, I.; et al. The value of thrombolysis for the management of acute ischemic stroke: A cost-effectiveness analysis based on real world data from the SUN4P study. Reg. Value Health, 2023; submitted. [Google Scholar]
- Zhai, S.; Gardiner, F.; Neeman, T.; Jones, B.; Gawarikar, Y. The Cost-Effectiveness of a Stroke Unit in Providing Enhanced Patient Outcomes in an Australian Teaching Hospital. J. Stroke Cerebrovasc. Dis. 2017, 26, 2362–2368. [Google Scholar] [CrossRef] [PubMed]
- Lund Ul Schneider, A.; Larsen, K.; Bache, K.; Robberstad, B. Cost-Effectiveness of Mobile Stroke Unit Care in Norway. Stroke 2022, 53, 3173–3181. [Google Scholar] [CrossRef] [PubMed]
- Angerova, Y.; Marsalek, P.; Chmelova, I.; Gueye, T.; Uherek, S.; Briza, J.; Bartak, M.; Rogalewicz, V. Cost and cost-effectiveness of early inpatient rehabilitation after stroke varies with initial disability: The Czech Republic perspective. Int. J. Rehabil. Res. 2020, 43, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Candio, P.; Violato, M.; Luengo-Fernandez, R.; Leal, J. Cost-effectiveness of home-based stroke rehabilitation across Europe: A modelling study. Health Policy 2022, 126, 183–189. [Google Scholar] [CrossRef]
| All Patients (NAll = 892) | Ischemic Stroke (NIsch = 755) | Hemorrhagic Stroke (NHem = 137) | p-Value | |
|---|---|---|---|---|
| Age, mean (SD) | 75.6 (13.5) | 75.6 (13.6) | 75.8 (13.2) | 0.419 |
| Age groups | 0.653 | |||
| <65 | 186 (20.9) | 159 (21.1 | 27 (19.7) | |
| 65–74 | 156 (17.5) | 136 (18.0) | 20 (14.6) | |
| 75–84 | 297 (33.3) | 246 (32.6) | 51 (37.2) | |
| 85+ | 253 (28.4) | 214 (28.3) | 39 (15.4) | |
| Gender (Men) | 447 (50.1) | 368 (48.7) | 79 (57.7) | 0.063 |
| mRS 0–1 prior to admission | 704 (78.9) | 591 (78.3) | 113 (82.5) | 0.306 |
| NIHSS scale at admission, median (interquartile range) | 7 (3–12) | 6 (3–11) | 12 (5–23) | <0.001 |
| Discharge destination in patients or relatives’ home (781 alive at discharge) | 649 (83.1) | 587 (85.4) | 62 (66.0) | 0.000 |
| History of Stroke risk factors | ||||
| Hypertension | 616 (691.1) | 522 (69.1) | 94 (68.6) | 0.920 |
| Diabetes | 230 (25.8) | 208 (27.5) | 22 (16.1) | 0.004 |
| Current smoking | 211 (23.7) | 184 (24.4) | 27 (19.7) | 0.275 |
| Hyperlipidemia | 328 (36.8) | 288 (38.1) | 40 (29.2) | 0.054 |
| Atrial Fibrillation | 265 (29.7) | 228 (30.2) | 37 (27.0) | 0.478 |
| Coronary Artery Disease | 117 (13.1) | 101 (13.4) | 16 (11.7) | 0.680 |
| Previous TIAs | 81 (9.1) | 66 (8.8) | 15 (10.9) | 0.419 |
| Classification of ischemic strokes | ||||
| Large vessel atherosclerotic | 71 (9.4) | |||
| Cardioembolic | 240 (31.8) | |||
| Lacunar | 117 (15.5) | |||
| Other | 16 (2.1) | |||
| Cryptogenic | 311 (41.2) | |||
| 1 year mortality | 220 (24.7) | 162 (21.5) | 58 (42.3) | 0.000 |
| Cost in Million Euros | Ischemic Stroke | Haemorrhagic Stroke | All Types of Stroke | % of Total Cost |
|---|---|---|---|---|
| I. Direct Healthcare Cost | 147 | 35.9 | 182.9 | 53.3 |
| Inpatient Care | 75.9 | 23.3 | 99.2 | 28.9 |
| Rehabilitation (Inpt and Outp) | 31.2 | 7.5 | 38.7 | 11.3 |
| Pharmaceuticals (Outp) | 19.2 | 1.7 | 20.9 | 6.1 |
| Medical Care and Tests | 15.6 | 2.4 | 18 | 5.2 |
| Home Care (paid caregiver) | 5.1 | 1.0 | 6.1 | 1.8 |
| II. Loss of Productivity | 102.68 | 57.54 | 160.22 | 46.7 |
| Loss of Productivity due to Morbidity (premature retirement and absenteeism from work) | 59.455 | 23.266 | 82.72 | 24.1 |
| Loss of Productivity due to Mortality | 3.486 | 24.286 | 27.772 | 8.1 |
| Informal Care costs | 39.742 | 9.985 | 49.727 | 14.5 |
| Total = I + II | 249.66 | 93.44 | 343.1 | 100 |
| QALYs | ||||
| Total QALYs | 12,555.6 | 2110.2 | 14,720 | |
| Mean QALYs (SD) | 0.4638 (0.4616) | 0.4282 (0.4138) | 0.46 (0.38) | |
| Total Cost/QALY (in euros) | 19,884 | 44,281 | 23,308 | p < 0.005 |
| All Patients (NAll = 892) | Ischemic Stroke (NIsch = 755) | Hemorrhagic Stroke (NHem = 137) | p-Value | |
|---|---|---|---|---|
| ALoS-Average Length of Stay, median (interquartile range) | 6 (4–10) | 6 (4–9) | 9 (6–15) | <0.001 |
| Treated in Specialized ASU-Acute Stroke Unit | 127 (14%) | 116 (15.4%) | 11 (8%) | 0.024 |
| rtPA Administration: Eligible /Undertook | 109 (14.4%)/35 (4.6%) | |||
| Early inpatient rehabilitation | 271 (30.4%) | 225 (29.8%) | 46 (33.6%) | >0.05 |
| Survivors’ (n = 772) admission to Rehabilitation center after discharge | 105 (13.6%) | 83 (12%) | 22 (23.4%) | <0.001 |
| mRS at discharge | <0.001 | |||
| 0–1 | 39% | 43% | 16.8% | |
| 2–3 | 24.3% | 25.2% | 19.7% | |
| 4–5 | 24.3% | 22.9% | 32.1% | |
| Dead | 12.3% | 8.9% | 31.4% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siskou, O.; Galanis, P.; Konstantakopoulou, O.; Stafylas, P.; Karagkouni, I.; Tsampalas, E.; Garefou, D.; Alexopoulou, H.; Gamvroula, A.; Lypiridou, M.; et al. The Cost and the Value of Stroke Care in Greece: Results from the SUN4P Study. Healthcare 2023, 11, 2545. https://doi.org/10.3390/healthcare11182545
Siskou O, Galanis P, Konstantakopoulou O, Stafylas P, Karagkouni I, Tsampalas E, Garefou D, Alexopoulou H, Gamvroula A, Lypiridou M, et al. The Cost and the Value of Stroke Care in Greece: Results from the SUN4P Study. Healthcare. 2023; 11(18):2545. https://doi.org/10.3390/healthcare11182545
Chicago/Turabian StyleSiskou, Olga, Petros Galanis, Olympia Konstantakopoulou, Panagiotis Stafylas, Iliana Karagkouni, Evangelos Tsampalas, Dafni Garefou, Helen Alexopoulou, Anastasia Gamvroula, Maria Lypiridou, and et al. 2023. "The Cost and the Value of Stroke Care in Greece: Results from the SUN4P Study" Healthcare 11, no. 18: 2545. https://doi.org/10.3390/healthcare11182545
APA StyleSiskou, O., Galanis, P., Konstantakopoulou, O., Stafylas, P., Karagkouni, I., Tsampalas, E., Garefou, D., Alexopoulou, H., Gamvroula, A., Lypiridou, M., Kalliontzakis, I., Fragkoulaki, A., Kouridaki, A., Tountopoulou, A., Kouzi, I., Vassilopoulou, S., Manios, E., Mavraganis, G., Vemmou, A., ... Kaitelidou, D. (2023). The Cost and the Value of Stroke Care in Greece: Results from the SUN4P Study. Healthcare, 11(18), 2545. https://doi.org/10.3390/healthcare11182545













