Health Science Students’ Perceptions of Hand Hygiene Education and Practice in a South African University: Introducing the University Hand Hygiene Improvement Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Sample Size Estimation
2.3. Data Collection: Self-Reported Questionnaire
2.4. Proposed Model for Hand Hygiene Training
2.5. Data Analysis
2.6. Ethical Consideration
3. Results
3.1. Sociodemographic Characteristics
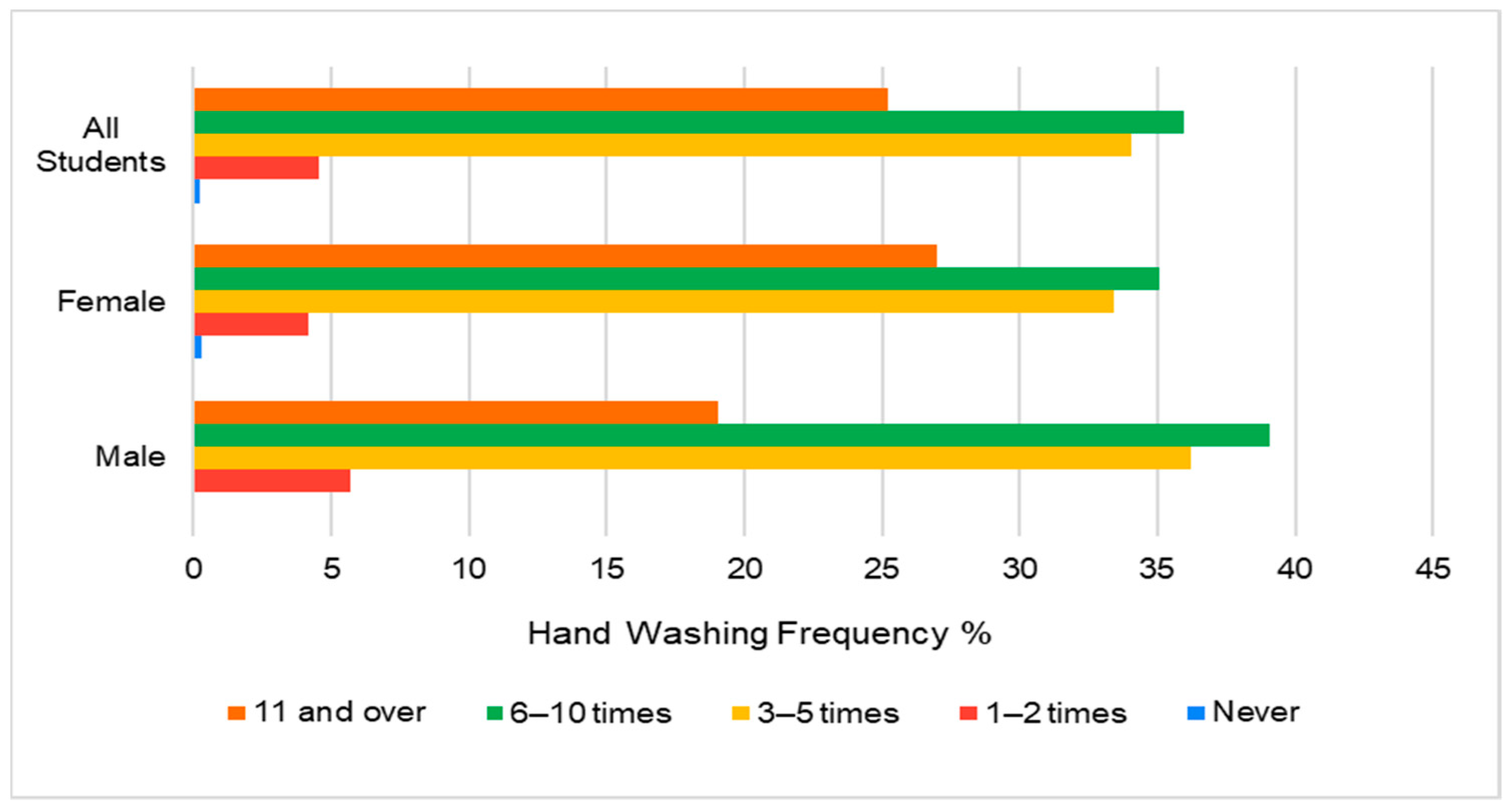
3.2. Handwashing Frequency
3.3. Hand Hygiene Knowledge, Practice, and Skills Responses
3.4. Hand Hygiene Training Model Development
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Price, L.; Melone, L.; McLarnon, N.; Bunyan, D.; Kilpatrick, C.; Flowers, P.; Reilly, J. A systematic review to evaluate the evidence base for the World Health Organization’s adopted hand hygiene technique for reducing the microbial load on the hands of healthcare workers. Am. J. Infect. Control 2018, 46, 814–823. [Google Scholar] [CrossRef] [PubMed]
- Baek, E.H.; Kim, S.E.; Kim, D.H.; Cho, O.H.; Hong, S.I.; Kim, S. The difference in hand hygiene compliance rate between unit-based observers and trained observers for World Health Organization checklist and optimal hand hygiene. Int. J. Infect. Dis. 2020, 90, 197–200. [Google Scholar] [CrossRef] [PubMed]
- Yousef, R.H.A.; Salem, M.R.; Mahmoud, A.T. Impact of implementation of a modified World Health Organization multimodal hand hygiene strategy in a university teaching hospital. Am. J. Infect. Control 2020, 48, 249–254. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care is Safer Care; World Health Organisation: Geneva, Switzerland, 2009.
- Centers for Disease Control and Prevention. Handwashing in Communities: Clean. Hands Save Lives; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2022. [Google Scholar]
- Bloomfield, S.F.; Aiello, A.E.; Cookson, B.; O’Boyle, C.; Larson, E.L. The effectiveness of hand hygiene procedures in reducing the risks of infections in home and community settings including handwashing and alcohol-based hand sanitizers. Am. J. Infect. Control 2007, 35, S27–S64. [Google Scholar] [CrossRef]
- Zimmerman, P.A.P.; Sladdin, I.; Shaban, R.Z.; Gilbert, J.; Brown, L. Factors influencing hand hygiene practice of nursing students: A descriptive, mixed-methods study. Nurse Educ. Pract. 2020, 44, 102746. [Google Scholar] [CrossRef]
- Harun, M.d.G.D.; Anwar, M.M.U.; Sumon, S.A.; Mohona, T.M.; Hassan, M.d.Z.; Rahman, A.; Abdullah, S.A.H.M.; Islam, M.S.; Oakley, L.P.; Malpiedi, P.; et al. Hand Hygiene compliance and associated factors among healthcare workers in selected tertiary care hospitals in Bangladesh. J. Hosp. Infect. 2023, 139, 220–227. [Google Scholar] [CrossRef]
- WHO Advice for the Public: Coronavirus Disease (COVID-19). World Health Organisation. 2023. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed on 30 July 2023).
- WHO. My 5 moments for hand hygiene. In Save Lives: Clean Your Hands; World Health Organisation: Geneva, Switzerland, 2015. [Google Scholar]
- Blundell, S.J.; Singh, A.; Yelverton, Y.; Barnard, T. The Impact of Hand Hygiene Intervention on the Bacterial Population on Chiropractors Hands. Master’s Dissertation, University of Johannesburg, Johannesburg, South Africa, 2018. [Google Scholar]
- Fuller, A.; Singh, A.; Yelverton, Y.; Barnard, T.G. Evaluating Chiropractic Students Hand Washing Practices Using GloGerm TM as a Surrogate for Microbial Pathogens. Master’s Dissertation, University of Johannesburg, Johannesburg, South Africa, 2019. [Google Scholar]
- Sekhukhuni, T.L.; Singh, A.; Barnard, T.; Razlog, R. The Inference of Hand Hygiene on the Spread of Disease in the University Health Training Centre. Master’s Dissertation, University of Johannesburg, Johannesburg, South Africa, 2020. [Google Scholar]
- Corre, M.H.; Delafont, V.; Legrand, A.; Berjeaud, J.M.; Verdon, J. Exploiting the richness of environmental waterborne bacterial species to find natural legionella pneumophila competitors. Front. Microbiol. 2019, 10, 3360. [Google Scholar] [CrossRef]
- Jemal, S. Knowledge and Practices of Hand Washing among Health Professionals in Dubti Referral Hospital, Dubti, Afar, Northeast Ethiopia. Adv. Prev. Med. 2018, 2018, 5290797. [Google Scholar] [CrossRef]
- Allegranzi, B.; Pittet, D. Role of hand hygiene in healthcare-associated infection prevention. J. Hosp. Infect. 2009, 73, 305–315. [Google Scholar] [CrossRef]
- Currie, K.; Melone, L.; Stewart, S.; King, C.; Holopainen, A.; Clark, A.M.; Reilly, J. Understanding the patient experience of health care–associated infection: A qualitative systematic review. Am. J. Infect. Control 2018, 46, 936–942. [Google Scholar] [CrossRef]
- Vermeil, T.; Peters, A.; Kilpatrick, C.; Pires, D.; Allegranzi, B.; Pittet, D. Hand hygiene in hospitals: Anatomy of a revolution. J. Hosp. Infect. 2019, 101, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Pittet, D.; Allegranzi, B.; Sax, H.; Dharan, S.; Pessoa-Silva, C.L.; Donaldson, L.; Boyce, J.M. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect. Dis. 2006, 6, 641–652. [Google Scholar] [CrossRef] [PubMed]
- Agbana, R.; Ogundeji, S.; Owoseni, J. A survey of hand hygiene knowledge, attitude and practices among health care workers in a tertiary hospital, Southwestern Nigeria. Arch. Community Med. Public. Health 2020, 6, 146–151. [Google Scholar] [CrossRef]
- Gilbert, G.L.; Kerridge, I. Hospital Infection Prevention and Control (IPC) and Antimicrobial Stewardship (AMS): Dual Strategies to Reduce Antibiotic Resistance (ABR) in Hospitals. Ethics Drug Resist. Collect. Responsib. Glob. Public Health 2020, 5, 89–108. [Google Scholar] [CrossRef]
- Dramowski, A.; Cotton, M.F.; Whitelaw, A. A framework for preventing healthcare-associated infection in neonates and children in South Africa. S. Afr. Med. J. 2017, 107, 192. [Google Scholar] [CrossRef]
- Maphumulo, W.T.; Bhengu, B.R. Challenges of quality improvement in the healthcare of South Africa post-apartheid: A critical review. Curationis 2019, 42, 1901. [Google Scholar] [CrossRef]
- Richter, S.M.; Barnard, T.G. Knowledge, Attitudes, and Perceptions Towards Hand Hygiene of Optometry Students Pre- and Peri-COVID-19 at a Tertiary Institution in Johannesburg, South Africa. Clin Optom 2022, 14, 195–205. [Google Scholar] [CrossRef]
- Al Kadi, A.; Salati, S.A. Hand hygiene practices among medical students. Interdiscip. Perspect. Infect. Dis. 2012, 2012, 679129. [Google Scholar] [CrossRef]
- Amissah, I.; Sali, S.; Craymah, J. A Study to Assess Hand Hygiene Knowledge and Practices among Health Care Workers in a Teaching Hospital in Ghana. Int. J. Sci. Res. 2016, 5, 301–307. [Google Scholar] [CrossRef]
- Assefa, D.; Melaku, T.; Bayisa, B.; Alemu, S. Knowledge, Attitude and Self-Reported Performance and Challenges of Hand Hygiene Using Alcohol-Based Hand Sanitizers Among Healthcare Workers during COVID-19 Pandemic at a Tertiary Hospital: A Cross-Sectional Study. Infect. Drug Resist. 2021, 14, 303–313. [Google Scholar] [CrossRef]
- Aghdassi, S.J.S.; Schröder, C.; Lemke, E.; Behnke, M.; Fliss, P.M.; Plotzki, C.; Wenk, J.; Gastmeier, P.; Kramer, T.S. A multimodal intervention to improve hand hygiene compliance in peripheral wards of a tertiary care university centre: A cluster randomised controlled trial. Antimicrob. Resist. Infect. Control 2020, 9, 113. [Google Scholar] [CrossRef] [PubMed]
- Mbroh, L.A. Assessing Knowledge, Attitude and Practices of Hand Hygiene Among University Students. Master’s Thesis, Minnesota State University, Mankato, MN, USA, 2019. [Google Scholar]
- Ergin, A.; Bostanci, M.; Önal, Ö.; Bozkurt, A.I.; Ergin, N. Evaluation of students’ social hand washing knowledge, practices, and skills in a university setting. Cent. Eur. J. Public. Health 2011, 19, 222–227. [Google Scholar] [CrossRef]
- Singh, A.; Yelverton, C.J.; Barnard, T.G. Rapid Quantification of the Total Viable Bacterial Population on Human Hands Using Flow Cytometry with SYBR® Green, I. Cytom. B Clin. Cytom. 2019, 96, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Pittet, D. Hand hygiene: From research to action. J. Infect. Prev. 2017, 18, 100–102. [Google Scholar] [CrossRef] [PubMed]
- Pittet, D.; Boyce, J.M.; Allegranzi, B. Hand Hygiene; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2017. [Google Scholar] [CrossRef]
- Gould, D.J.; Navaie, D.; Purssell, E.; Drey, N.S.; Creedon, S. Changing the paradigm: Messages for hand hygiene education and audit from cluster analysis. J. Hosp. Infect. 2018, 98, 345–351. [Google Scholar] [CrossRef]
- Saito, H.; Inoue, K.; Ditai, J.; Wanume, B.; Abeso, J.; Balyejussa, J.; Weeks, A. Alcohol-based hand rub and incidence of healthcare associated infections in a rural regional referral and teaching hospital in Uganda (‘WardGel’ study). Antimicrob. Resist. Infect. Control 2017, 6, 129. [Google Scholar] [CrossRef]
- Baye, A.M.; Ababu, A.; Bayisa, R.; Abdella, M.; Diriba, E.; Wale, M.; Selam, M.N. Alcohol-Based Handrub Utilization Practice for COVID-19 Prevention among Pharmacy Professionals in Ethiopian Public Hospitals: A Cross-Sectional Study. Drug Healthc. Patient Saf. 2021, 13, 37–46. [Google Scholar] [CrossRef]
- Maxwell, J.A. The Value of Qualitative Inquiry for Public Policy; SAGE Publications: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Creswell, J.; Creswell, J. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 5th ed.; SAGE Publications: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Price, L.; MacDonald, J.; Gozdzielewska, L.; Howe, T.; Flowers, P.; Shepherd, L.; Watt, Y.; Reilly, J. Interventions to improve healthcare workers’ hand hygiene compliance: A systematic review of systematic reviews. Infect. Control Hosp. Epidemiol. 2018, 39, 1449–1456. [Google Scholar] [CrossRef]
- Pittet, D.; Hugonnet, S.; Harbarth, S.; Mourouga, P.; Sauvan, V.; Touveneau, S.; Perneger, T.V. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet 2000, 356, 1307–1312. [Google Scholar] [CrossRef]
- Whitby, M.; Pessoa-Silva, C.L.; McLaws, M.-L.; Allegranzi, B.; Sax, H.; Larson, E.; Seto, W.H.; Donaldson, L.; Pittet, D. Behavioural considerations for hand hygiene practices: The basic building blocks. J. Hosp. Infect. 2007, 65, 1–8. [Google Scholar] [CrossRef]
- Erasmus, V.; Daha, T.J.; Brug, H.; Richardus, J.H.; Behrendt, M.D.; Vos, M.C.; van Beeck, E.F. Systematic Review of Studies on Compliance with Hand Hygiene Guidelines in Hospital Care. Infect. Control Hosp. Epidemiol. 2010, 31, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Gloria Umuhoza, A.; Bosco Kamugisha, J.; Nashwan, A.J.; Tahuna Soko, G. Assessment of knowledge and practices of hand hygiene among health workers in Rwanda. Int. J. Afr. Nurs. Sci. 2023, 19, 100585. [Google Scholar] [CrossRef]
- Yehouenou, C.L.; Abedinzadeh, A.; Houngnihin, R.; Baxerres, C.; Dossou, F.M.; Simon, A.; Dalleur, O. Understanding Hand Hygiene Behavior in a Public Hospital in Benin Using the Theoretical Domain Frameworks: The First Step for Designing Appropriate Interventions. Healthcare 2022, 10, 1924. [Google Scholar] [CrossRef]
- Kupfer, T.R.; Wyles, K.J.; Watson, F.; La Ragione, R.M.; Chambers, M.A.; Macdonald, A.S. Determinants of hand hygiene behaviour based on the Theory of Interpersonal Behaviour. J. Infect. Prev. 2019, 20, 232–237. [Google Scholar] [CrossRef]
- Hefzy, E.M.; Wegdan, A.A.; Abdel Wahed, W.Y. Hospital outpatient clinics as a potential hazard for healthcare associated infections. J. Infect. Public. Health 2016, 9, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Jeanes, A.; Coen, P.G.; Drey, N.S.; Gould, D.J. The development of hand hygiene compliance imperatives in an emergency department. Am. J. Infect. Control 2018, 46, 441–447. [Google Scholar] [CrossRef]
- Sultana, M.; Alam Mahumud, R.; Razzaque Sarker, A.; Mahmud Hossain, S. Hand hygiene knowledge and practice among university students: Evidence from private universities of Bangladesh. Risk Manag. Healthc. Policy 2016, 9, 13–20. [Google Scholar] [CrossRef]
- Lopez-Quintero, C.; Freeman, P.; Neumark, Y. Hand Washing among School Children in Bogotá, Colombia. Am. J. Public. Health 2009, 99, 94–101. [Google Scholar] [CrossRef]
- Gould, D.J.; Moralejo, D.; Drey, N.; Chudleigh, J.H.; Taljaard, M. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst. Rev. 2017, 2017, CD005186. [Google Scholar] [CrossRef]
- Allegranzi, B.; Gayet-Ageron, A.; Damani, N.; Bengaly, L.; McLaws, M.-L.; Moro, M.-L.; Memish, Z.; Urroz, O.; Richet, H.; Storr, J. Global implementation of WHO’s multimodal strategy for improvement of hand hygiene: A quasi-experimental study. Lancet Infect. Dis. 2013, 13, 843–851. [Google Scholar] [CrossRef]
- Price, L.; Gozdzielewska, L.; Matuluko, A.; Pittet, D.; Allegranzi, B.; Reilly, J. Comparing the effectiveness of hand hygiene techniques in reducing the microbial load and covering hand surfaces in healthcare workers: Updated systematic review. Am. J. Infect. Control 2022, 50, 1079–1090. [Google Scholar] [CrossRef] [PubMed]
- Ahmadipour, M.; Dehghan, M.; Ahmadinejad, M.; Jabarpour, M.; Mangolian Shahrbabaki, P.; Ebrahimi Rigi, Z. Barriers to hand hygiene compliance in intensive care units during the COVID-19 pandemic: A qualitative study. Front. Public. Health 2022, 10, 968231. [Google Scholar] [CrossRef]
- Tan, J.B.X.; de Kraker, M.E.A.; Pires, D.; Soule, H.; Pittet, D. Handrubbing with sprayed alcohol-based hand rub: An alternative method for effective hand hygiene. J. Hosp. Infect. 2020, 104, 430–434. [Google Scholar] [CrossRef] [PubMed]
- Tartari, E.; Fankhauser, C.; Masson-Roy, S.; Márquez-Villarreal, H.; Fernández Moreno, I.; Rodriguez Navas, M.L.; Sarabia, O.; Bellissimo-Rodrigues, F.; Hernández-de Mezerville, M.; Lee, Y.F.; et al. Train-the-Trainers in hand hygiene: A standardized approach to guide education in infection prevention and control. Antimicrob. Resist. Infect. Control 2019, 8, 206. [Google Scholar] [CrossRef]
- Yehouenou, C.L.; Yehouenou, C.L.; Yehouenou, C.L.; Dohou, A.M.; Dohou, A.M.; Fiogbe, A.D.; Esse, M.; Degbey, C.; Simon, A.; Dalleur, O. Hand hygiene in surgery in Benin: Opportunities and challenges. Antimicrob. Resist. Infect. Control 2020, 9, 85. [Google Scholar] [CrossRef] [PubMed]
- Nieva, V.; Sorra, J. Safety culture assessment: A tool for improving patient safety in healthcare organizations. Qual. Saf. Health Care 2003, 12, ii17–ii23. [Google Scholar] [CrossRef]
- Doronina, R.; Jones, D.; Martello, M.; Biron, A.; Lavoie-Tremblay, M. A Systematic Review on the Effectiveness of Interventions to Improve Hand Hygiene Compliance of Nurses in the Hospital Setting. J. Nurs. Scholarsh. 2017, 49, 143–152. [Google Scholar] [CrossRef]
- Sax, H.; Allegranzi, B.; Uçkay, I.; Larson, E.; Boyce, J.; Pittet, D. ‘My five moments for hand hygiene’: A user-centred design approach to understand, train, monitor and report hand hygiene. J. Hosp. Infect. 2007, 67, 9–21. [Google Scholar] [CrossRef]
- Ivers, N.; Jamtvedt, G.; Flottorp, S.; Young, J.M.; Odgaard-Jensen, J.; French, S.D.; O’Brien, M.A.; Johansen, M.; Grimshaw, J.; Oxman, A.D. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2012, 60, CD000259. [Google Scholar] [CrossRef]
- Staats, B.R.; Dai, H.; Hofmann, D.; Milkman, K.L. Motivating Process Compliance Through Individual Electronic Monitoring: An Empirical Examination of Hand Hygiene in Healthcare. Manag. Sci. 2017, 63, 1563–1585. [Google Scholar] [CrossRef]
- Kouhi, R.; Panahi, R.; Ramezankhani, A.; Amin Sobhani, M.; Khodakarim, S.; Amjadian, M. The effect of education based on health belief model on hand hygiene behavior in the staff of Tehran dentistry centers: A quasi-experimental intervention study. Health Sci. Rep. 2023, 6, e1408. [Google Scholar] [CrossRef]
- Sin, C.S.; Rochelle, T.L. Using the theory of planned behaviour to explain hand hygiene among nurses in Hong Kong during COVID-19. J. Hosp. Infect. 2022, 123, 119–125. [Google Scholar] [CrossRef] [PubMed]
- White, K.M.; Jimmieson, N.L.; Obst, P.L.; Graves, N.; Barnett, A.; Cockshaw, W.; Gee, P.; Haneman, L.; Page, K.; Campbell, M. Using a theory of planned behaviour framework to explore hand hygiene beliefs at the ‘5 critical moments’ among Australian hospital-based nurses. BMC Health Serv. Res. 2015, 15, 59. [Google Scholar] [CrossRef] [PubMed]
- Lotfinejad, N.; Peters, A.; Pittet, D. Hand hygiene and the novel coronavirus pandemic: The role of healthcare workers. J. Hosp. Infect. 2020, 105, 776–777. [Google Scholar] [CrossRef]
- Zheng, S.; Yang, Q.; Wang, X.; Zhang, X.; Zhou, Q. Capability, Opportunity, Motivation, and Hand Hygiene Behavior in Healthcare Workers: A Structural Equation Modeling. Psychol. Res. Behav. Manag. 2022, 15, 2219–2228. [Google Scholar] [CrossRef] [PubMed]







| Variables | (n = 464) Frequency (%) |
|---|---|
| Gender | |
| Female | 359 (77.4) |
| Male | 105 (22.6) |
| Age (Years) | |
| 18–20 | 130 (28.0) |
| 21–25 | 230 (49.6) |
| >25 | 104 (22.4) |
| Academic Department | |
| 1. Biomedical Science | 17 (3.7) |
| 2. Chiropractic | 89 (19.2) |
| 3. Complimentary Medicine | 83 (17.9) |
| 4. Emergency Medical Care | 26 (5.6) |
| 5. Environmental Health | 15 (3.2) |
| 6. Medical Imaging and Radiation (MIRS) | 72 (15.5) |
| 7. Nursing | 51 (11.0) |
| 8. Optometry | 29 (6.3) |
| 9. Podiatry | 43 (9.3) |
| 10. Sport and Movement Studies | 39 (8.4) |
| Year of Study | |
| 1st | 99 (21.3) |
| 2nd | 118 (25.4) |
| 3rd | 114 (24.6) |
| 4th | 81 (17.5) |
| 5th | 25 (5.4) |
| 6th | 21 (4.5) |
| 7th | 0 (0) |
| 8th | 6 (1.3) |
| Student Category | |
| Undergraduate | 353 (76.1) |
| Postgraduate | 111 (23.9) |
| Living Location | |
| Campus Residence On Site | 32 (6.9) |
| Campus Residence Off Site | 145 (31.3) |
| With Family/Partner/Spouse | 213 (45.9) |
| Commune | 43 (9.3) |
| Alone | 31 (6.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, A.; Barnard, T.G. Health Science Students’ Perceptions of Hand Hygiene Education and Practice in a South African University: Introducing the University Hand Hygiene Improvement Model. Healthcare 2023, 11, 2553. https://doi.org/10.3390/healthcare11182553
Singh A, Barnard TG. Health Science Students’ Perceptions of Hand Hygiene Education and Practice in a South African University: Introducing the University Hand Hygiene Improvement Model. Healthcare. 2023; 11(18):2553. https://doi.org/10.3390/healthcare11182553
Chicago/Turabian StyleSingh, Atheesha, and Tobias George Barnard. 2023. "Health Science Students’ Perceptions of Hand Hygiene Education and Practice in a South African University: Introducing the University Hand Hygiene Improvement Model" Healthcare 11, no. 18: 2553. https://doi.org/10.3390/healthcare11182553






