Role of Trust, Risk Perception, and Perceived Benefit in COVID-19 Vaccination Intention of the Public
Abstract
:1. Introduction
2. Literature Review and Model Development
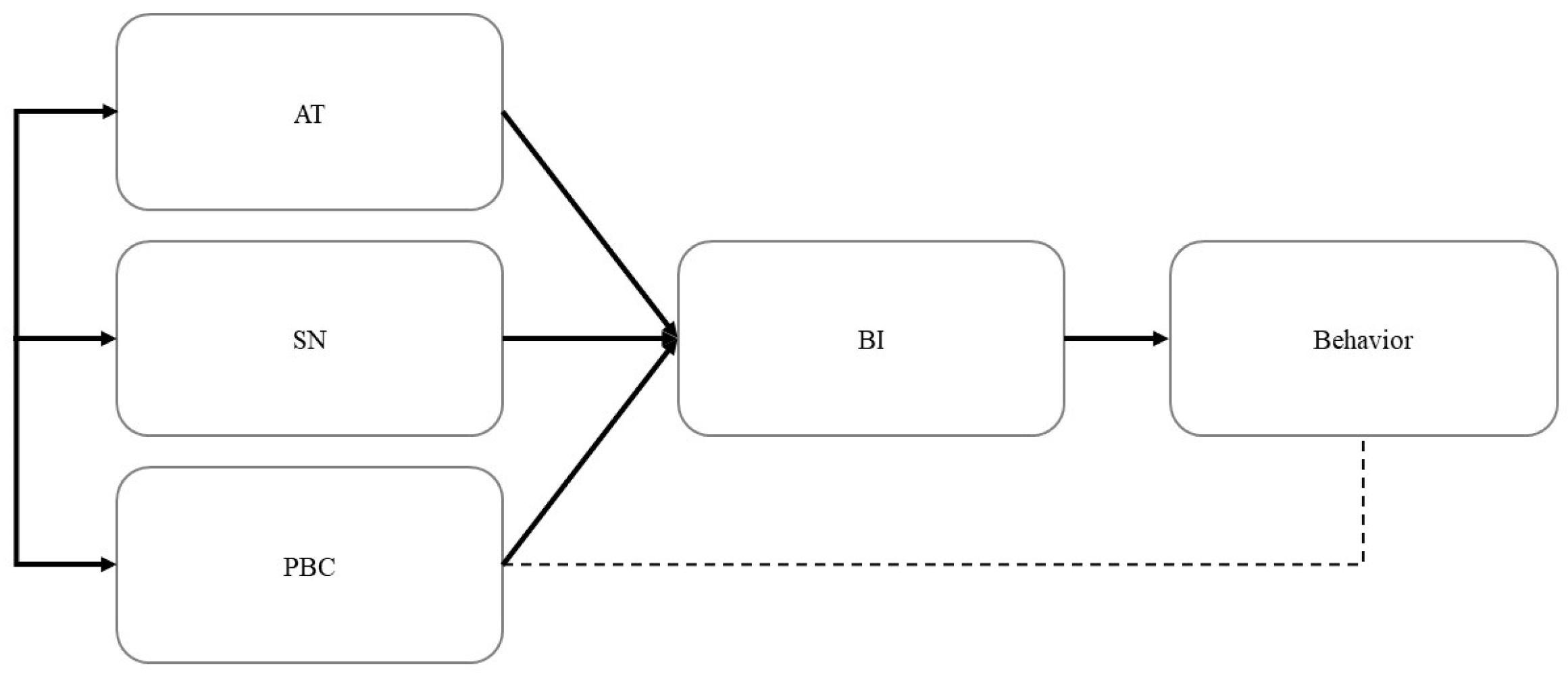
2.1. Theory of Planned Behavior (TPB)
2.2. Trust in Vaccines (TV)
2.3. Perceived Benefit (PB)
2.4. Risk Perception
2.5. Model Development
3. Methodology
3.1. Participants
3.2. Measurement
3.3. Data Analysis
4. Results
4.1. Measurement Model Assessment
4.2. Structural Model Assessment
4.3. Mediation Analysis
5. Discussion
5.1. Theoretical Implications
5.2. Practical Implications
5.3. Limitations and Directions for Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, X.; Maggioni, V.; Houser, P.; Xue, Y.; Mei, Y. The impact of weather condition and social activity on COVID-19 transmission in the United States. J. Environ. Manag. 2022, 302, 114085. [Google Scholar] [CrossRef]
- Shibeeb, S.; Khan, A. ABO blood group association and COVID-19. COVID-19 susceptibility and severity: A review. Hematol. Transfus. Cell Ther. 2022, 44, 70–75. [Google Scholar] [CrossRef]
- Hebbani, A.V.; Pulakuntla, S.; Pannuru, P.; Aramgam, S.; Badri, K.R.; Reddy, V.D. COVID-19: Comprehensive review on mutations and current vaccines. Arch. Microbiol. 2022, 204, 8. [Google Scholar] [CrossRef]
- Machingaidze, S.; Wiysonge, C.S. Understanding COVID-19 vaccine hesitancy. Nat. Med. 2021, 27, 1338–1339. [Google Scholar] [CrossRef]
- Chevalier-Cottin, E.-P.; Ashbaugh, H.; Brooke, N.; Gavazzi, G.; Santillana, M.; Burlet, N.; Tin Tin Htar, M. Communicating benefits from vaccines beyond preventing infectious diseases. Infect. Dis. Ther. 2020, 9, 467–480. [Google Scholar] [CrossRef]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Kaufman, J.; Bagot, K.L.; Tuckerman, J.; Biezen, R.; Oliver, J.; Jos, C.; Ong, D.S.; Manski-Nankervis, J.A.; Seale, H.; Sanci, L. Qualitative exploration of intentions, concerns and information needs of vaccine-hesitant adults initially prioritised to receive COVID-19 vaccines in Australia. Aust. N. Z. J. Public Health 2022, 46, 16–24. [Google Scholar] [CrossRef]
- Myers, A.; Ipsen, C.; Lissau, A. COVID-19 vaccination hesitancy among Americans with disabilities aged 18–65: An exploratory analysis. Disabil. Health J. 2022, 15, 101223. [Google Scholar] [CrossRef]
- Schilling, S.; Orr, C.J.; Delamater, A.M.; Flower, K.B.; Heerman, W.J.; Perrin, E.M.; Rothman, R.L.; Yin, H.S.; Sanders, L. COVID-19 vaccine hesitancy among low-income, racially and ethnically diverse US parents. Patient Educ. Couns. 2022, 105, 2771–2777. [Google Scholar] [CrossRef]
- Eskola, J.; Duclos, P.; Schuster, M.; MacDonald, N.E. How to deal with vaccine hesitancy? Vaccine 2015, 33, 4215–4217. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef]
- Okuhara, T.; Okada, H.; Goto, E.; Tsunezumi, A.; Kagawa, Y.; Kiuchi, T. Encouraging COVID-19 vaccination via an evolutionary theoretical approach: A randomized controlled study in Japan. Patient Educ. Couns. 2022, 105, 2248–2255. [Google Scholar] [CrossRef] [PubMed]
- Goldman, R.D.; Yan, T.D.; Seiler, M.; Cotanda, C.P.; Brown, J.C.; Klein, E.J.; Hoeffe, J.; Gelernter, R.; Hall, J.E.; Davis, A.L. Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine 2020, 38, 7668–7673. [Google Scholar] [CrossRef] [PubMed]
- Williams, L.; Gallant, A.J.; Rasmussen, S.; Brown Nicholls, L.A.; Cogan, N.; Deakin, K.; Young, D.; Flowers, P. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: Outlining evidence-based and theoretically informed future intervention content. Br. J. Health Psychol. 2020, 25, 1039–1054. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.M.; Smith, L.E.; Sim, J.; Amlot, R.; Cutts, M.; Dasch, H.; Rubin, G.J.; Sevdalis, N. COVID-19 vaccination intention in the UK: Results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum. Vaccines Immunother. 2021, 17, 1612–1621. [Google Scholar] [CrossRef]
- Loomba, S.; de Figueiredo, A.; Piatek, S.J.; de Graaf, K.; Larson, H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 2021, 5, 337–348. [Google Scholar] [CrossRef]
- Giuliani, M.; Ichino, A.; Bonomi, A.; Martoni, R.; Cammino, S.; Gorini, A. Who Is Willing to Get Vaccinated? A Study into the Psychological, Socio-Demographic, and Cultural Determinants of COVID-19 Vaccination Intentions. Vaccines 2021, 9, 810. [Google Scholar] [CrossRef]
- Drążkowski, D.; Trepanowski, R. Reactance and perceived disease severity as determinants of COVID-19 vaccination intention: An application of the theory of planned behavior. Psychol. Health Med. 2021, 9, 1–8. [Google Scholar] [CrossRef]
- Tam, C.C.; Qiao, S.; Li, X. Factors associated with decision making on COVID-19 vaccine acceptance among college students in South Carolina. Psychol. Health Med. 2022, 27, 150–161. [Google Scholar] [CrossRef]
- Nguyen, K.H.; Srivastav, A.; Razzaghi, H.; Williams, W.; Lindley, M.C.; Jorgensen, C.; Abad, N.; Singleton, J.A. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination—United States, September and December 2020. Am J Transpl. 2021, 21, 1650–1656. [Google Scholar] [CrossRef] [PubMed]
- Guillon, M.; Kergall, P. Factors associated with COVID-19 vaccination intentions and attitudes in France. Public Health 2021, 198, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Dai, M.; Xia, S. Perceived facilitators and barriers to intentions of receiving the COVID-19 vaccines among elderly Chinese adults. Vaccine 2022, 40, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Chinese parents’ intentions to vaccinate their children against SARS-CoV-2 infection and vaccine preferences. Hum. Vaccines Immunother. 2021, 12, 4806–4815. [Google Scholar] [CrossRef] [PubMed]
- Fan, C.-W.; Chen, I.-H.; Ko, N.-Y.; Yen, C.-F.; Lin, C.-Y.; Griffiths, M.D.; Pakpour, A.H. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: An online survey study. Hum. Vaccines Immunother. 2021, 17, 3413–3420. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Q.; Liu, X.; Wang, R.; Mao, Y.; Chen, H.; Li, X.; Liu, X.; Dai, J.; Gao, J.; Fu, H. Predictors of willingness to receive the COVID-19 vaccine after emergency use authorization: The role of coping appraisal. Vaccines 2021, 9, 967. [Google Scholar] [CrossRef]
- Wake, A.D. The willingness to receive COVID-19 vaccine and its associated factors:“vaccination refusal could prolong the war of this pandemic”–a systematic review. Risk Manag. Healthc. Policy 2021, 14, 2609–2623. [Google Scholar] [CrossRef]
- Ajzen, I. From intentions to actions: A theory of planned behavior. In Action-Control: From Cognition to Behavior; Kuhl, J., Beckman, J., Eds.; Springer: Heidelberg, Germany, 1985; pp. 11–39. [Google Scholar]
- Huang, X.; Dai, S.; Xu, H. Predicting tourists’ health risk preventative behaviour and travelling satisfaction in Tibet: Combining the theory of planned behaviour and health belief model. Tour. Manag. Perspect. 2020, 33, 100589. [Google Scholar] [CrossRef]
- Moeini, B.; Hazavehei, S.M.M.; Bashirian, S.; Soltanian, A.; Mousali, A.A.; Kafami, V. Effect of educational program to encourage safe sexual behaviors among addicted men refered to substance abuse treatment centers in Hamadan, Western Iran: Applying the theory of planned behavior. J. Educ. Community Health 2022, 1, 1–10. [Google Scholar] [CrossRef]
- Barati, M.; Niknami, S.; Hidarnia, A.; Allahverdipour, H. Predictors of tobacco smoking in male adolescents in Hamadan based on the theory of planned behavior. J. Educ. Community Health 2022, 1, 28–37. [Google Scholar] [CrossRef]
- Wong, T.K.M.; Man, S.S.; Chan, A.H.S. Critical factors for the use or non-use of personal protective equipment amongst construction workers. Saf. Sci. 2020, 126, 104663. [Google Scholar] [CrossRef]
- Man, S.S.; Alabdulkarim, S.; Chan, A.H.S.; Zhang, T. The acceptance of personal protective equipment among Hong Kong construction workers: An integration of technology acceptance model and theory of planned behavior with risk perception and safety climate. J. Saf. Res. 2021, 79, 329–340. [Google Scholar] [CrossRef] [PubMed]
- Moeini, B.; Taheri, M.; Roshanaei, G.; Vahidinia, A.A.; Moez, M.R. High school girl’s adherence to 5-a-day serving’s fruits and vegetables: An application theory of planned behavior. J. Educ. Community Health 2022, 1, 10–19. [Google Scholar]
- Yahaghi, R.; Ahmadizade, S.; Fotuhi, R.; Taherkhani, E.; Ranjbaran, M.; Buchali, Z.; Jafari, R.; Zamani, N.; Shahbazkhania, A.; Simiari, H. Fear of COVID-19 and perceived COVID-19 infectability supplement theory of planned behavior to explain Iranians’ intention to get COVID-19 vaccinated. Vaccines 2021, 9, 684. [Google Scholar] [CrossRef]
- Seong, B.-H.; Hong, C.-Y. Does risk awareness of COVID-19 affect visits to national parks? Analyzing the tourist decision-making process using the theory of planned behavior. Int. J. Environ. Res. Public Health 2021, 18, 5081. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Freimuth, V.S.; Jamison, A.M.; An, J.; Hancock, G.R.; Quinn, S.C. Determinants of trust in the flu vaccine for African Americans and Whites. Soc. Sci. Med. 2017, 193, 70–79. [Google Scholar] [CrossRef]
- Gilson, L. Trust and the development of health care as a social institution. Soc. Sci. Med. 2003, 56, 1453–1468. [Google Scholar] [CrossRef]
- Hall, M.A.; Dugan, E.; Zheng, B.; Mishra, A.K. Trust in physicians and medical institutions: What is it, can it be measured, and does it matter? Milbank Q. 2001, 79, 613–639. [Google Scholar] [CrossRef]
- Borah, P.; Hwang, J. Trust in doctors, positive attitudes, and vaccination behavior: The role of doctor–patient communication in H1N1 vaccination. Health Commun. 2021, 37, 1423–1431. [Google Scholar] [CrossRef]
- Matute, J.; Palau-Saumell, R.; Meyer, J.; Derqui, B.; Jiménez-Asenjo, N. Are you getting it? Integrating theories to explain intentions to get vaccinated against COVID-19 in Spain. J. Risk Res. 2021, 25, 1055–1074. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Yahaghai, R.; Alimoradi, Z.; Broström, A.; Griffiths, M.D.; Pakpour, A.H. The mediational role of trust in the healthcare system in the association between generalized trust and willingness to get COVID-19 vaccination in Iran. Hum. Vaccines Immunother. 2022, 18, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Walrave, M.; Waeterloos, C.; Ponnet, K. Adoption of a contact tracing app for containing COVID-19: A health belief model approach. JMIR Public Health Surveill. 2020, 6, e20572. [Google Scholar] [CrossRef] [PubMed]
- Ranney, M.L.; Griffeth, V.; Jha, A.K. Critical supply shortages—The need for ventilators and personal protective equipment during the COVID-19 pandemic. N. Engl. J. Med. 2020, 382, e41. [Google Scholar] [CrossRef]
- Williams, J.; Degeling, C.; McVernon, J.; Dawson, A. How should we conduct pandemic vaccination? Vaccine 2021, 39, 994–999. [Google Scholar] [CrossRef]
- Mir, H.H.; Parveen, S.; Mullick, N.H.; Nabi, S. Using structural equation modeling to predict Indian people’s attitudes and intentions towards COVID-19 vaccination. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 1017–1022. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, D.; Barbhuiya, M.R. Bottled water usage and willingness to pay among Indian tourists: Visual nudges and the theory of planned behaviour. Scand. J. Hosp. Tour. 2021, 21, 531–549. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Chao, S.-L.; Chu, Y.-W. Effects of Perceived Benefit on Vitamin D Supplementation Intention: A Theory of Planned Behaviour Perspective. Int. J. Environ. Res. Public Health 2022, 19, 1952. [Google Scholar] [CrossRef]
- Wang, D.; Jiang, S.; Liu, B.; Li, X.; Yuan, X. Research on Antecedents of Residents’ Willingness to Cooperate in Urban Regeneration Projects: Based on an Extended Theory of Planned Behavior (TPB) Model. Buildings 2022, 12, 1251. [Google Scholar] [CrossRef]
- Ong, A.K.S.; Prasetyo, Y.T.; Salazar, J.M.L.D.; Erfe, J.J.C.; Abella, A.A.; Young, M.N.; Chuenyindee, T.; Nadlifatin, R.; Redi, A.A.N.P. Investigating the acceptance of the reopening bataan nuclear power plant: Integrating protection motivation theory and extended theory of planned behavior. Nucl. Eng. Technol. 2022, 54, 1115–1125. [Google Scholar] [CrossRef]
- Man, S.S.; Chan, A.H.S.; Alabdulkarim, S. Quantification of Risk Perception: Development and Validation of the Construction Worker Risk Perception (CoWoRP) Scale. J. Saf. Res. 2019, 71, 25–39. [Google Scholar] [CrossRef]
- Commodari, E.; La Rosa, V.; Coniglio, M. Health risk perceptions in the era of the new coronavirus: Are the Italian people ready for a novel virus? A cross-sectional study on perceived personal and comparative susceptibility for infectious diseases. Public Health 2020, 187, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Qiao, S.; Tam, C.C.; Li, X. Risk exposures, risk perceptions, negative attitudes toward general vaccination, and COVID-19 vaccine acceptance among college students in South Carolina. Am. J. Health Promot. 2020, 36, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Breakwell, G.M.; Jaspal, R. Identity change, uncertainty and mistrust in relation to fear and risk of COVID-19. J. Risk Res. 2021, 24, 335–351. [Google Scholar] [CrossRef]
- Zhang, T.; Tao, D.; Qu, X.; Zhang, X.; Lin, R.; Zhang, W. The roles of initial trust and perceived risk in public’s acceptance of automated vehicles. Transp. Res. Part C Emerg. Technol. 2019, 98, 207–220. [Google Scholar] [CrossRef]
- Mutimukwe, C.; Kolkowska, E.; Grönlund, Å. Information privacy in e-service: Effect of organizational privacy assurances on individual privacy concerns, perceptions, trust and self-disclosure behavior. Gov. Inf. Q. 2020, 37, 101413. [Google Scholar] [CrossRef]
- Plohl, N.; Musil, B. Modeling compliance with COVID-19 prevention guidelines: The critical role of trust in science. Psychol. Health Med. 2021, 26, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Yu, X. The impact of perceived risk on consumers’ cross-platform buying behavior. Front. Psychol. 2020, 11, 592246. [Google Scholar] [CrossRef]
- Wang, J.; Zhao, S.; Zhang, W.; Evans, R. Why people adopt smart transportation services: An integrated model of TAM, trust and perceived risk. Transp. Plan. Technol. 2021, 44, 629–646. [Google Scholar] [CrossRef]
- Yoon, A.; Han, S.; Yoon, J.-H. What Drives People to Travel during a Pandemic: The Role of Media Information and Trust in the Government. Int. J. Hosp. Tour. Adm. 2022, 1–28. [Google Scholar] [CrossRef]
- Yue, R.P.H.; Lau, B.H.; Chan, C.L.; Ng, S.-M. Risk perception as a double-edged sword in policy compliance in COVID-19 pandemic? A two-phase evaluation from Hong Kong. J. Risk Res. 2022, 25, 1131–1145. [Google Scholar] [CrossRef]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Jiang, S.; Wu, Q. Factors influencing COVID-19 vaccination intention: The roles of vaccine knowledge, vaccine risk perception, and doctor-patient communication. Patient Educ. Couns. 2022, 105, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Wise, T.; Zbozinek, T.D.; Michelini, G.; Hagan, C.C.; Mobbs, D. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States. R. Soc. Open Sci. 2020, 7, 200742. [Google Scholar] [CrossRef] [PubMed]
- Joslyn, S.; Savelli, S.; Duarte, H.A.; Burgeno, J.; Qin, C.; Han, J.H.; Gulacsik, G. COVID-19: Risk perception, risk communication, and behavioral intentions. J. Exp. Psychol. Appl. 2021, 27, 599. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimi, O.V.; Johnson, M.S.; Ebling, S.; Amundsen, O.M.; Halsøy, Ø.; Hoffart, A.; Skjerdingstad, N.; Johnson, S.U. Risk, trust, and flawed assumptions: Vaccine hesitancy during the COVID-19 pandemic. Front. Public Health 2021, 9, 700213. [Google Scholar] [CrossRef] [PubMed]
- Siuki, H.A.; Peyman, N.; Vahedian-Shahroodi, M.; Gholian-Aval, M.; Tehrani, H. Health education intervention on HIV/AIDS prevention behaviors among health volunteers in healthcare centers: An applying the theory of planned behavior. J. Soc. Serv. Res. 2019, 45, 582–588. [Google Scholar] [CrossRef]
- Abamecha, F.; Tena, A.; Kiros, G. Psychographic predictors of intention to use cervical cancer screening services among women attending maternal and child health services in Southern Ethiopia: The theory of planned behavior (TPB) perspective. BMC Public Health 2019, 19, 434. [Google Scholar] [CrossRef]
- Caso, D.; Capasso, M.; Fabbricatore, R.; Conner, M. Understanding the psychosocial determinants of Italian parents’ intentions not to vaccinate their children: An extended theory of planned behaviour model. Psychol. Health 2021, 37, 1111–1131. [Google Scholar] [CrossRef]
- Wang, X.; Chen, D.; Xie, T.; Zhang, W. Predicting women’s intentions to screen for breast cancer based on the health belief model and the theory of planned behavior. J. Obstet. Gynaecol. Res. 2019, 45, 2440–2451. [Google Scholar] [CrossRef]
- Wolff, K. COVID-19 vaccination intentions: The theory of planned behavior, optimistic bias, and anticipated regret. Front. Psychol. 2021, 12, 648289. [Google Scholar] [CrossRef] [PubMed]
- National Health Commission of the People’s Republic of China. Press Conference of the Joint Prevention and Control Mechanism of the State Council. Available online: http://www.gov.cn/xinwen/gwylflkjz150/index.htm (accessed on 12 August 2023).
- Hong Kong Institute for Advanced Study. Institute, Centres and Laboratories. Available online: https://www.cityu.edu.hk/research/centres (accessed on 12 August 2023).
- Wang, Z.; She, R.; Chen, X.; Li, L.; Li, L.; Huang, Z.; Lau, J.T. Parental acceptability of COVID-19 vaccination for children under the age of 18 years among Chinese doctors and nurses: A cross-sectional online survey. Hum. Vaccines Immunother. 2021, 17, 3322–3332. [Google Scholar] [CrossRef] [PubMed]
- Caso, D.; Carfora, V.; Starace, C.; Conner, M. Key factors influencing Italian mothers’ intention to vaccinate sons against HPV: The influence of trust in health authorities, anticipated regret and past behaviour. Sustainability 2019, 11, 6879. [Google Scholar] [CrossRef]
- Prasetyo, Y.T.; Castillo, A.M.; Salonga, L.J.; Sia, J.A.; Seneta, J.A. Factors affecting perceived effectiveness of COVID-19 prevention measures among Filipinos during enhanced community quarantine in Luzon, Philippines: Integrating Protection Motivation Theory and extended Theory of Planned Behavior. Int. J. Infect. Dis. 2020, 99, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Degarege, A.; Krupp, K.; Fennie, K.; Srinivas, V.; Li, T.; Stephens, D.P.; Madhivanan, P.J.V. An integrative behavior theory derived model to assess factors affecting HPV vaccine acceptance using structural equation modeling. Vaccine 2019, 37, 945–955. [Google Scholar] [CrossRef]
- Wong, N.C.J.C.R. “Vaccinations are safe and effective”: Inoculating positive HPV vaccine attitudes against antivaccination attack messages. Commun. Rep. 2016, 29, 127–138. [Google Scholar] [CrossRef]
- Liao, Q.; Cowling, B.J.; Lam, W.W.T.; Fielding, R.J.P.o. Factors affecting intention to receive and self-reported receipt of 2009 pandemic (H1N1) vaccine in Hong Kong: A longitudinal study. PLoS ONE 2011, 6, e17713. [Google Scholar] [CrossRef]
- Man, S.S.; Xiong, W.; Chang, F.; Chan, A.H.S. Critical Factors Influencing Acceptance of Automated Vehicles by Hong Kong Drivers. IEEE Access 2020, 8, 109845–109856. [Google Scholar] [CrossRef]
- Quinn, S.C.; Jamison, A.M.; An, J.; Hancock, G.R.; Freimuth, V.S. Measuring vaccine hesitancy, confidence, trust and flu vaccine uptake: Results of a national survey of White and African American adults. Vaccine 2019, 37, 1168–1173. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Hamid, M.R.A.; Sami, W.; Sidek, M.H.M. Discriminant validity assessment: Use of Fornell & Larcker criterion versus HTMT criterion. J. Phys. Conf. Ser. 2017, 890, 012163. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Falk, C.F.; Biesanz, J.C. Two cross-platform programs for inferences and interval estimation about indirect effects in mediational models. SAGE Open 2016, 6, 1–13. [Google Scholar] [CrossRef]
- Man, S.S.; Chan, A.H.S.; Alabdulkarim, S.; Zhang, T. The effects of personal and organizational factors on the risk-taking behavior of Hong Kong construction workers. Saf. Sci. 2021, 163, 105155. [Google Scholar] [CrossRef]
- Li, Z.; Man, S.S.; Chan, A.H.S.; Zhu, J. Integration of Theory of Planned Behavior, Sensation Seeking, and Risk Perception to Explain the Risky Driving Behavior of Truck Drivers. Sustainability 2021, 13, 5214. [Google Scholar] [CrossRef]
- Smith, T.W.; Baron, C.E.; Caska-Wallace, C.M.; Knobloch-Fedders, L.M.; Renshaw, K.D.; Uchino, B.N. PTSD in veterans, couple behavior, and cardiovascular response during marital conflict. Emotion 2021, 21, 478–488. [Google Scholar] [CrossRef]
- Kim, D.J.; Ferrin, D.L.; Rao, H.R. A trust-based consumer decision-making model in electronic commerce: The role of trust, perceived risk, and their antecedents. Decis. Support Syst. 2008, 44, 544–564. [Google Scholar] [CrossRef]
- Gao, X.; Ding, F.; Ai, T. What Drives Elderly People in China Away from COVID-19 Information? Int. J. Environ. Res. Public Health 2022, 19, 9509. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Jung, S.-m.; Linton, N.M.; Kinoshita, R.; Hayashi, K.; Miyama, T.; Anzai, A.; Yang, Y.; Yuan, B.; Akhmetzhanov, A.R. Communicating the risk of death from novel coronavirus disease (COVID-19). J. Clin. Med. 2020, 9, 580. [Google Scholar] [CrossRef]
- Schoch-Spana, M.; Brunson, E.K.; Long, R.; Ruth, A.; Ravi, S.J.; Trotochaud, M.; Borio, L.; Brewer, J.; Buccina, J.; Connell, N. The public’s role in COVID-19 vaccination: Human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine 2021, 39, 6004–6012. [Google Scholar] [CrossRef]
- Leng, A.; Maitland, E.; Wang, S.; Nicholas, S.; Liu, R.; Wang, J. Individual preferences for COVID-19 vaccination in China. Vaccine 2021, 39, 247–254. [Google Scholar] [CrossRef]
- Guidry, J.P.; Laestadius, L.I.; Vraga, E.K.; Miller, C.A.; Perrin, P.B.; Burton, C.W.; Ryan, M.; Fuemmeler, B.F.; Carlyle, K.E. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am. J. Infect. Control 2021, 49, 137–142. [Google Scholar] [CrossRef]
- Bloom, B.R.; Nowak, G.J.; Orenstein, W. “When will we have a vaccine?”—Understanding questions and answers about COVID-19 vaccination. N. Engl. J. Med. 2020, 383, 2202–2204. [Google Scholar] [CrossRef] [PubMed]
- National Health and Wellness Commission of China. Interpretation of the Recent Work Plan for Vaccination of Key Populations against New Coronaviruses. Available online: https://www.gov.cn/zhengce/202308/content_6895993.htm (accessed on 12 August 2023).
- González-Padilla, D.A.; Tortolero-Blanco, L. Social media influence in the COVID-19 pandemic. Int. Braz. J. Urol. 2020, 46, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Centre for Health Protection. COVID-19 Vaccination Programme. Available online: https://www.chp.gov.hk/en/features/106934.html (accessed on 12 August 2023).
- Centers for Disease Control and Prevention. Use of COVID-19 Vaccines in the U.S. Available online: https://www.cdc.gov/vaccines/covid-19/clinical-considerations/interim-considerations-us.html (accessed on 12 August 2023).
- Huang, Z.; Fu, Z.; Wang, J. Review on drug regulatory science promoting COVID-19 vaccine development in China. Engineering 2022, 10, 127–132. [Google Scholar] [CrossRef]
- Taheri Soodejani, M.; Basti, M.; Tabatabaei, S.M.; Rajabkhah, K. Measles, mumps, and rubella (MMR) vaccine and COVID-19: A systematic review. Int. J. Mol. Epidemiol. Genet. 2021, 12, 35–39. [Google Scholar]
- Diwan, M.N.; Samad, S.; Mushtaq, R.; Aamir, A.; Allahuddin, Z.; Ullah, I.; Ullah Afridi, R.; Ambreen, A.; Khan, A.; Ehsan, N.; et al. Measles Induced Encephalitis: Recent Interventions to Overcome the Obstacles Encountered in the Management Amidst the COVID-19 Pandemic. Diseases 2022, 10, 104. [Google Scholar] [CrossRef] [PubMed]
- Fu, H.; Abbas, K.; Klepac, P.; van Zandvoort, K.; Tanvir, H.; Portnoy, A.; Jit, M. Effect of evidence updates on key determinants of measles vaccination impact: A DynaMICE modelling study in ten high-burden countries. BMC Med. 2021, 19, 281. [Google Scholar] [CrossRef]



| Characteristics | Frequency | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 316 | 38.7 |
| Female | 500 | 61.3 |
| Education | ||
| Grade 12 or lower | 26 | 3.2 |
| High school graduate | 207 | 25.4 |
| Bachelor’s degree | 474 | 58.1 |
| Postgraduate degree | 109 | 13.3 |
| Employment status | ||
| Student | 338 | 41.4 |
| Full-time employee | 218 | 26.7 |
| Part-time employee | 119 | 14.6 |
| Freelancer | 132 | 16.2 |
| Retired | 4 | 0.5 |
| Unemployed | 5 | 0.6 |
| Marital status | ||
| Married | 339 | 41.5 |
| Single | 428 | 52.5 |
| Divorced or widowed | 49 | 6.0 |
| Construct | Item | Content |
|---|---|---|
| PB | PB1 | I believe that receiving a COVID-19 vaccination can protect me against COVID-19. |
| PB2 | I believe that receiving a COVID-19 vaccination can help protect my family and friends against COVID-19. | |
| PB3 | I believe that receiving a COVID-19 vaccination can reduce my risk of contracting COVID-19. | |
| PBC | PBC1 | I can decide for myself whether or not to receive a COVID-19 vaccination. |
| PBC2 | I can decide on my own when to receive a COVID-19 vaccination. | |
| PBC3 | I can decide where to receive a COVID-19 vaccination. | |
| PBC4 | I can afford the price of a COVID-19 vaccination. | |
| SN | SN1 | My friends think I should receive a COVID-19 vaccination. |
| SN2 | My family thinks I should receive a COVID-19 vaccination. | |
| SN3 | The person most important to me think I should receive a COVID-19 vaccination. | |
| RPCV | RPCV1 | I am worried that a COVID-19 vaccination may cause facial palsy or other serious movement disorders such as paralysis. |
| RPCV2 | I am worried that a COVID-19 vaccination may cause infection of other serious diseases. | |
| RPCV3 | I am worried about being infected by other people in the process of getting a vaccination. | |
| RPCV4 | I am worried that the mutation of COVID-19 will make the vaccines ineffective. | |
| RPC | RPC1 | I think that COVID-19 is a serious disease. |
| RPC2 | I think that COVID-19 can lead to death. | |
| RPC3 | I think that COVID-19 can affect mental health. | |
| RPC4 | I think the COVID-19 pandemic will continue indefinitely. | |
| RPC5 | I think I am very vulnerable to COVID-19. | |
| RPC6 | I think COVID-19 mutates easily. | |
| ARCV | ARCV1 | Receiving a COVID-19 vaccination is a good idea. |
| ARCV2 | Receiving a COVID-19 vaccination is a wise idea. | |
| ARCV3 | Receiving a COVID-19 vaccination is pleasant. | |
| ARCV4 | Receiving a COVID-19 vaccination is necessary. | |
| ARCV5 | Receiving a COVID-19 vaccination is acceptable. | |
| TV | TV1 | COVID-19 vaccines are dependable. |
| TV2 | COVID-19 vaccines are reliable. | |
| TV3 | Overall, I can trust COVID-19 vaccines. | |
| CVI | CVI1 | I want to receive a COVID-19 vaccination. |
| CVI2 | I predict that I will receive a COVID-19 vaccination in the future. | |
| CVI3 | I plan to receive a COVID-19 vaccination in the future. |
| Model Fit Index | Recommended Value | Measurement Model | Structural Model |
|---|---|---|---|
| χ2/df | 5 | 3.315 | 4.831 |
| CFI | 0.95 | 0.979 | 0.964 |
| TLI | 0.95 | 0.975 | 0.959 |
| RMSEA | 0.08 | 0.053 | 0.069 |
| Construct | Item | Factor Loading | AVE | CR | Cronbach’s Alpha |
|---|---|---|---|---|---|
| PB | PB1 | 0.875 | 0.831 | 0.937 | 0.936 |
| PB2 | 0.932 | ||||
| PB3 | 0.927 | ||||
| PBC | PBC2 | 0.930 | 0.847 | 0.943 | 0.940 |
| PBC3 | 0.946 | ||||
| PBC4 | 0.884 | ||||
| SN | SN1 | 0.910 | 0.870 | 0.953 | 0.952 |
| SN2 | 0.949 | ||||
| SN3 | 0.939 | ||||
| RPCV | RPCV1 | 0.995 | 0.960 | 0.990 | 0.990 |
| RPCV2 | 0.961 | ||||
| RPCV3 | 0.995 | ||||
| RPCV4 | 0.968 | ||||
| RPC | RPC1 | 0.823 | 0.751 | 0.938 | 0.937 |
| RPC2 | 0.889 | ||||
| RPC4 | 0.928 | ||||
| RPC5 | 0.828 | ||||
| RPC6 | 0.861 | ||||
| ARCV | ATT2 | 0.885 | 0.808 | 0.926 | 0.925 |
| ATT4 | 0.874 | ||||
| ATT5 | 0.936 | ||||
| TV | TV1 | 0.935 | 0.879 | 0.956 | 0.955 |
| TV2 | 0.957 | ||||
| TV3 | 0.920 | ||||
| CVI | CVI1 | 0.961 | 0.946 | 0.981 | 0.981 |
| CVI2 | 0.984 | ||||
| CVI3 | 0.973 |
| RPC | RPCV | TV | ARCV | SN | PBC | PB | CVI | |
|---|---|---|---|---|---|---|---|---|
| RPC | 0.867 | |||||||
| RPCV | −0.130 | 0.980 | ||||||
| TV | 0.216 | −0.545 | 0.938 | |||||
| ARCV | 0.264 | −0.436 | 0.776 | 0.899 | ||||
| SN | 0.247 | −0.366 | 0.653 | 0.878 | 0.933 | |||
| PBC | 0.204 | −0.357 | 0.629 | 0.860 | 0.899 | 0.920 | ||
| PB | 0.215 | −0.381 | 0.657 | 0.860 | 0.821 | 0.867 | 0.912 | |
| CVI | 0.254 | −0.475 | 0.725 | 0.875 | 0.861 | 0.843 | 0.829 | 0.973 |
| Hypothesis | Standardized Path Coefficient | p-Value | Result |
|---|---|---|---|
| H1: ARCV → CVI | 0.349 | <0.001 | Supported |
| H2: SN → CVI | 0.379 | <0.001 | Supported |
| H3: PBC → CVI | 0.158 | <0.01 | Supported |
| H4: TV → ARCV | 0.378 | <0.001 | Supported |
| H5: TV → CVI | 0.154 | <0.001 | Supported |
| H6: PB → ARCV | 0.737 | <0.001 | Supported |
| H7: RPC → TV | 0.157 | <0.001 | Supported |
| H8: RPCV → TV | –0.527 | <0.001 | Supported |
| Independent Variable | Mediator | Dependent Variable | Standardized Indirect Effect | p-Value | Result |
|---|---|---|---|---|---|
| RPC | TV | ARCV | 0.06 | <0.001 | Significant |
| RPCV | TV | ARCV | −0.20 | <0.001 | Significant |
| RPC | TV | CVI | 0.01 | <0.001 | Significant |
| RPCV | TV | CVI | −0.05 | <0.001 | Significant |
| PB | ARCV | CVI | 0.25 | <0.001 | Significant |
| TV | ARCV | CVI | 0.13 | <0.001 | Significant |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Man, S.-S.; Wen, H.; Zhao, L.; So, B.C.-L. Role of Trust, Risk Perception, and Perceived Benefit in COVID-19 Vaccination Intention of the Public. Healthcare 2023, 11, 2589. https://doi.org/10.3390/healthcare11182589
Man S-S, Wen H, Zhao L, So BC-L. Role of Trust, Risk Perception, and Perceived Benefit in COVID-19 Vaccination Intention of the Public. Healthcare. 2023; 11(18):2589. https://doi.org/10.3390/healthcare11182589
Chicago/Turabian StyleMan, Siu-Shing, Huiying Wen, Ligao Zhao, and Billy Chun-Lung So. 2023. "Role of Trust, Risk Perception, and Perceived Benefit in COVID-19 Vaccination Intention of the Public" Healthcare 11, no. 18: 2589. https://doi.org/10.3390/healthcare11182589
APA StyleMan, S.-S., Wen, H., Zhao, L., & So, B. C.-L. (2023). Role of Trust, Risk Perception, and Perceived Benefit in COVID-19 Vaccination Intention of the Public. Healthcare, 11(18), 2589. https://doi.org/10.3390/healthcare11182589







