Long COVID Symptomatology and Associated Factors in Primary Care Patients: The EPICOVID-AP21 Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Assessments
2.4. Statistical Analysis
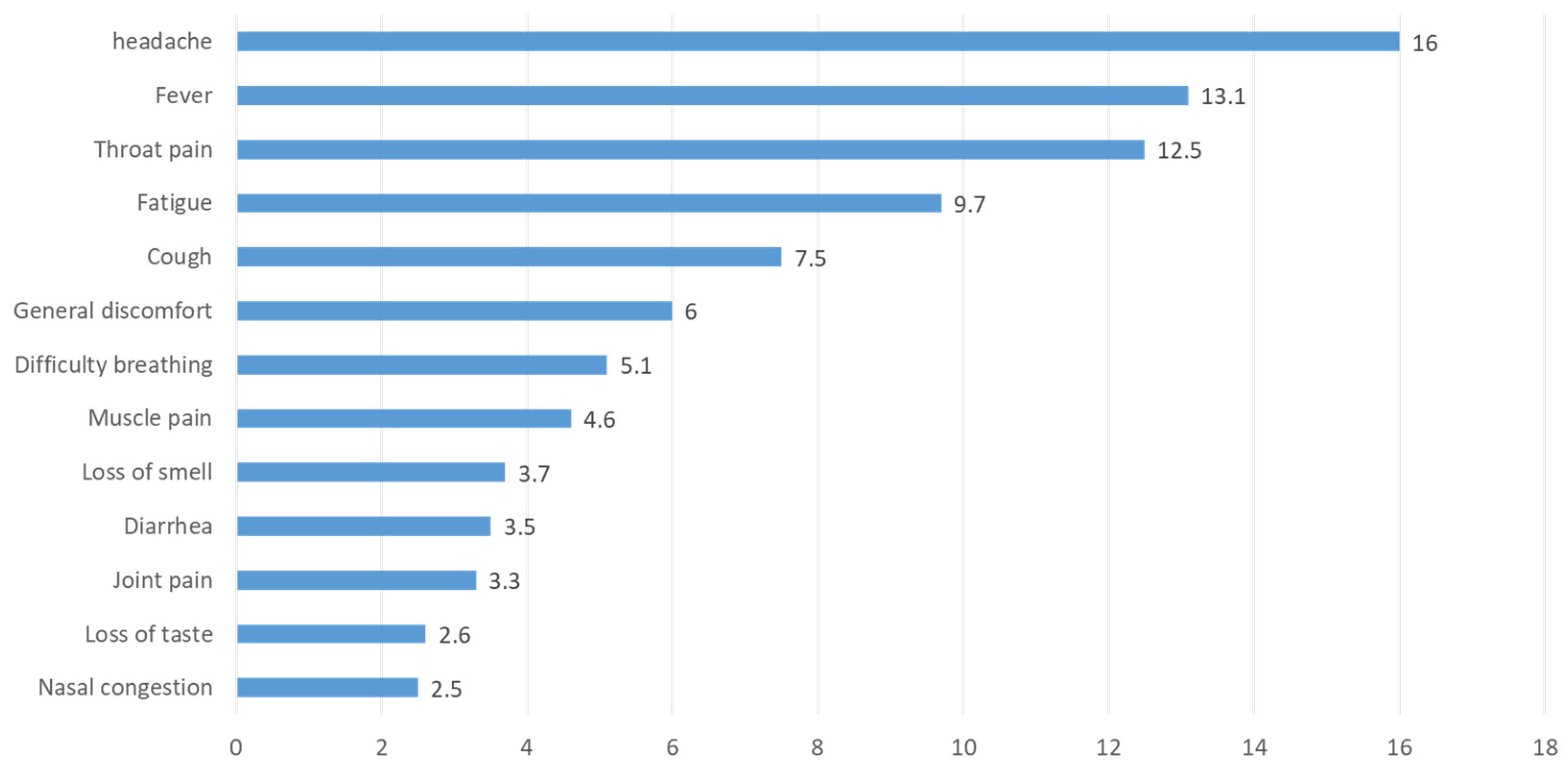
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministerio de Sanidad. Minist Sanid 2022. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/situacionActual.htm (accessed on 31 December 2021).
- Consilium. COVID-19: Respuesta de la UE en el Ámbito de la Salud Pública. Consilium Europa. 2022. Available online: https://www.consilium.europa.eu/es/policies/coronavirus/covid-19-public-health/ (accessed on 23 September 2021).
- Párraga Martínez, I.; Pérula de Torres, L.A.; González Lama, J.; Jiménez García, C.; Sánchez Montero, R.; Rider Garrido, F. Características clínico-epidemiológicas de la infección por el virus SARS-CoV-2 en médicos de familia: Un estudio de casos y controles. Aten. Primaria 2021, 53, 101956. [Google Scholar] [CrossRef]
- Pérula de Torres, L.Á.; González-Lama, J.; Jiménez García, C.; Sánchez Montero, R.; Rider Garrido, F.; Ortega López, Y.; Pajares Conde, D.; Ramírez Baena, M.; Párraga Martínez, I.; Romero-Rodríguez, E. Frequency and predictive validity of olfactory and taste dysfunction in patients with SARS-CoV-2 infection. Med. Clin. 2021, 156, 595–601. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Centros Para el Control y la Prevención de Enfermedades. Afecciones Persistentes al COVID-19 y Afecciones Posteriores al COVID-19 2022. Available online: https://espanol.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (accessed on 23 September 2021).
- Soriano, J.; Murthy, S.; Marshall, J.; Relan, P.; Diaz, J. A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- The PHOSP-COVID Collaborative Group. Clinical characteristics with inflammation profiling of long COVID and association with 1-year recovery following hospitalisation in the UK: A prospective observational study. Lancet. Respir. Med. 2022, 10, 761–775. [Google Scholar] [CrossRef]
- Guía Clínica Para la Atención al Paciente LONG COVID/COVID Persistente 2021. Available online: https://www.semg.es/index.php/consensos-guias-y-protocolos/363-guia-clinica-para-la-atencion-al-paciente-long-covid-covid-persistente (accessed on 28 September 2021).
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. eClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef] [PubMed]
- Hirschtick, J.L.; Titus, A.R.; Slocum, E.; Power, L.E.; Hirschtick, R.E.; Elliott, M.R.; McKane, P.; Fleischer, N.L. Population-Based Estimates of Post-acute Sequelae of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection (PASC) Prevalence and Characteristics. Clin. Infect. Dis. 2021, 73, 2055–2064. [Google Scholar] [CrossRef] [PubMed]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef] [PubMed]
- Bliddal, S.; Banasik, K.; Pedersen, O.B.; Nissen, J.; Cantwell, L.; Schwinn, M.; Tulstrup, M.; Westergaard, D.; Ullum, H.; Brunak, S.; et al. Acute and persistent symptoms in non-hospitalized PCR-confirmed COVID-19 patients. Sci. Rep. 2021, 11, 13153. [Google Scholar] [CrossRef]
- Chen, C.; Haupert, S.R.; Zimmermann, L.; Shi, X.; Fritsche, L.G.; Mukherjee, B. Global Prevalence of Post COVID-19 Condition or Long COVID: A Meta-Analysis and Systematic Review. J. Infect. Dis. 2022, 226, 1593–1607. [Google Scholar] [CrossRef]
- Daitch, V.; Yelin, D.; Awwad, M.; Guaraldi, G.; Milić, J.; Mussini, C.; Falcone, M.; Tiseo, G.; Carrozzi, L.; Pistelli, F.; et al. Characteristics of long COVID among older adults: A cross-sectional study. Int. J. Infect. Dis. 2022, 125, 287–293. [Google Scholar] [CrossRef]
- Fernández-De-las-peñas, C.; Martín-Guerrero, J.D.; Pellicer-Valero, Ó.J.; Navarro-Pardo, E.; Gómez-Mayordomo, V.; Cuadrado, M.L.; Arias-Navalón, J.A.; Cigarán-Méndez, M.; Hernández-Barrera, V.; Arendt-Nielsen, L. Female Sex Is a Risk Factor Associated with Long-Term Post-COVID Related-Symptoms but Not with COVID-19 Symptoms: The LONG-COVID-EXP-CM Multicenter Study. J. Clin. Med. 2022, 11, 413. [Google Scholar] [CrossRef] [PubMed]
- Yelin, D.; Margalit, I.; Nehme, M.; Bordas-Martínez, J.; Pistelli, F.; Yahav, D.; Guessous, I.; Durà-Miralles, X.; Carrozzi, L.; Shapira-Lichter, I.; et al. Patterns of Long COVID Symptoms: A Multi-Center Cross Sectional Study. J. Clin. Med. 2022, 11, 898. [Google Scholar] [CrossRef]
- Pérez-González, A.; Araújo-Ameijeiras, A.; Fernández-Villar, A.; Crespo, M.; Poveda, E.; Cabrera, J.J.; del Campo, V.; de Araujo, B.G.; Gómez, C.; Leiro, V.; et al. Long COVID in hospitalized and non-hospitalized patients in a large cohort in Northwest Spain, a prospective cohort study. Sci. Rep. 2022, 12, 3369. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.P.-V.O.J.; Navarro-Pardo, E.P.-C.D.F.L.L.; Guijarro, C.M.-G.J.D. Symptoms Experienced at the Acute Phase of SARS-CoV-2 Infection as Risk Factor of Long-term Post-COVID Symptoms: The LONG-COVID-EXP-CM Multicenter Study. Int. J. Infect. Dis. 2022, 116, 241–244. [Google Scholar] [CrossRef]
- Organización Mundial de la Salud. Enfermedad Por Coronavirus (COVID-19): Afección Posterior a la COVID-19 2021. Available online: https://www.who.int/es/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-post-covid-19-condition (accessed on 1 October 2021).
- Scientific Advisory Group. COVID-19 Scientific Advisory Group Rapid Evidence Report. Updat. Rev. Prolong. symptoms after acute COVID-19 Infect. Alberta Health Services, Physical distancing works, 2021. [Google Scholar]
- Tleyjeh, I.M.; Saddik, B.; Ramakrishnan, R.K.; AlSwaidan, N.; AlAnazi, A.; Alhazmi, D.; Aloufi, A.; AlSumait, F.; Berbari, E.F.; Halwani, R. Long term predictors of breathlessness, exercise intolerance, chronic fatigue and well-being in hospitalized patients with COVID-19: A cohort study with 4 months median follow-up. J. Infect. Public Health 2022, 15, 21–28. [Google Scholar] [CrossRef]
- Ministerio de Sanidad. Manejo en Atención Primaria y Domiciliaria del COVID-19 2020. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Manejo_primaria.pdf (accessed on 23 September 2021).
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 Long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef] [PubMed]
- Asadi-Pooya, A.A.; Akbari, A.; Emami, A.; Lotfi, M.; Rostamihosseinkhani, M.; Nemati, H.; Barzegar, Z.; Kabiri, M.; Zeraatpisheh, Z.; Farjoud-Kouhanjani, M.; et al. Risk Factors Associated with Long COVID Syndrome: A Retrospective Study. Iran. J. Med. Sci. 2021, 46, 428–436. [Google Scholar] [CrossRef]
- Salari, N.; Khodayari, Y.; Hosseinian-Far, A.; Zarei, H.; Rasoulpoor, S.; Akbari, H.; Mohammadi, M. Global prevalence of chronic fatigue syndrome among long COVID-19 patients: A systematic review and meta-analysis. Biopsychosoc. Med. 2022, 16, 21. [Google Scholar] [CrossRef] [PubMed]
- Calabria, M.; García-Sánchez, C.; Grunden, N.; Pons, C.; Arroyo, J.A.; Gómez-Anson, B.; Estévez García, M.; del, C.; Belvís, R.; Morollón, N.; et al. Post-COVID-19 fatigue: The contribution of cognitive and neuropsychiatric symptoms. J. Neurol. 2022, 269, 3990–3999. [Google Scholar] [CrossRef]
- Robbins, T.; Gonevski, M.; Clark, C.; Baitule, S.; Sharma, K.; Magar, A.; Patel, K.; Sankar, S.; Kyrou, I.; Ali, A.; et al. Hyperbaric oxygen therapy for the treatment of long COVID: Early evaluation of a highly promising intervention. Clin. Med. 2021, 21, E629–E632. [Google Scholar] [CrossRef] [PubMed]
- Tana, C.; Bentivegna, E.; Cho, S.J.; Harriott, A.M.; García-Azorín, D.; Labastida-Ramirez, A.; Ornello, R.; Raffaelli, B.; Beltrán, E.R.; Ruscheweyh, R.; et al. Long COVID headache. J. Headache Pain 2022, 23, 93. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Izquierdo, M.; Láinez-Ramos-Bossini, A.J.; de Alba, I.G.F.; Ortiz-González-Serna, R.; Serrano-Ortiz, Á.; Fernández-Martínez, N.F.; Ruiz-Montero, R.; Cervilla, J.A. Long COVID 12 months after discharge: Persistent symptoms in patients hospitalised due to COVID-19 and patients hospitalised due to other causes-a multicentre cohort study. BMC Med. 2022, 20, 92. [Google Scholar] [CrossRef]
- Sylvester, S.V.; Rusu, R.; Chan, B.; Bellows, M.; O’Keefe, C.; Nicholson, S. Sex differences in sequelae from COVID-19 infection and in long COVID syndrome: A review. Curr. Med. Res. Opin. 2022, 38, 1391–1399. [Google Scholar] [CrossRef]
- Pinzon, R.T.; Wijaya, V.O.; Al Jody, A.; Nunsio, P.N.; Buana, R.B. Persistent neurological manifestations in long COVID-19 syndrome: A systematic review and meta-analysis. J. Infect. Public Health 2022, 15, 856–869. [Google Scholar] [CrossRef] [PubMed]
- Stefanou, M.-I.; Palaiodimou, L.; Bakola, E.; Smyrnis, N.; Papadopoulou, M.; Paraskevas, G.P.; Rizos, E.; Boutati, E.; Grigoriadis, N.; Krogias, C. Neurological manifestations of long-COVID syndrome: A narrative review. Ther. Adv. Chronic Dis. 2022, 13. [Google Scholar] [CrossRef]
- Baig, A.M. Chronic long-COVID syndrome: A protracted COVID-19 illness with neurological dysfunctions. CNS Neurosci. Ther. 2021, 27, 1433–1436. [Google Scholar] [CrossRef]
- Aiyegbusi, O.L.; Hughes, S.E.; Turner, G.; Rivera, S.C.; McMullan, C.; Chandan, J.S.; Haroon, S.; Price, G.; Davies, E.H.; Nirantharakumar, K.; et al. Symptoms, complications and management of long COVID: A review. J. R. Soc. Med. 2021, 114, 428–442. [Google Scholar] [CrossRef]
- Yong, S.J. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infect. Dis. 2021, 53, 737–754. [Google Scholar] [CrossRef]
- Whitaker, M.; Elliott, J.; Chadeau-Hyam, M.; Riley, S.; Darzi, A.; Cooke, G.; Ward, H.; Elliott, P. Persistent COVID-19 symptoms in a community study of 606,434 people in England. Nat. Commun. 2022, 13, 1957. [Google Scholar] [CrossRef]
- Wu, Q.; Ailshire, J.; Crimmins, E. Long COVID and Symptom Trajectory in a Representative Sample of Americans. Res. Sq. 2022, 12, 11647. [Google Scholar] [CrossRef]
- Wang, C.; Yu, C.; Jing, H.; Wu, X.; Novakovic, V.A.; Xie, R.; Shi, J. Long COVID: The Nature of Thrombotic Sequelae Determines the Necessity of Early Anticoagulation. Front. Cell. Infect. Microbiol. 2022, 12, 861703. [Google Scholar] [CrossRef] [PubMed]
- Gao, P.; Liu, J.; Liu, M. Effect of COVID-19 Vaccines on Reducing the Risk of Long COVID in the Real World: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 12422. [Google Scholar] [CrossRef]
- Ledford, H. How vaccination affects the risk of Long Covid. Nature 2021, 599, 546–548. [Google Scholar] [CrossRef] [PubMed]
- Couzin-Frankel, J.; Vogel, G. Vaccines may cause rare, Long Covid-like symptoms. Science 2022, 375, 364–366. [Google Scholar] [CrossRef]
- Notarte, K.I.; Catahay, J.A.; Velasco, J.V.; Pastrana, A.; Ver, A.T.; Pangilinan, F.C.; Peligro, P.J.; Casimiro, M.; Guerrero, J.J.; Gellaco, M.M.L.; et al. Impact of COVID-19 vaccination on the risk of developing long-COVID and on existing long-COVID symptoms: A systematic review. eClinicalMedicine 2022, 53, 101624. [Google Scholar] [CrossRef]
- Bai, F.; Tomasoni, D.; Falcinella, C.; Barbanotti, D.; Castoldi, R.; Mulè, G.; Augello, M.; Mondatore, D.; Allegrini, M.; Cona, A.; et al. Female gender is associated with long COVID syndrome: A prospective cohort study. Clin. Microbiol. Infect. 2022, 28, 611.e9–611.e16. [Google Scholar] [CrossRef]

| Symptoms and Signs | COVID-19 n % | Long COVID n % | Disabling n % | |||
|---|---|---|---|---|---|---|
| -General and nonspecific symptoms | ||||||
| General malaise | 625 | 90.7 | 487 | 70.7 | 407 | 59.1 |
| Tiredness and fatigue | 667 | 96.8 | 616 | 89.4 | 594 | 86.2 |
| Fever | 391 | 56.7 | 119 | 17.3 | 92 | 13.4 |
| Low body temperature (hypothermia) | 237 | 34.4 | 179 | 26.0 | 59 | 8.6 |
| Chills and shivering | 409 | 59.4 | 218 | 30.9 | 79 | 13.4 |
| Sweating | 363 | 52.7 | 213 | 30.9 | 60 | 8.7 |
| Headache | 593 | 86.1 | 474 | 74.6 | 360 | 61.3 |
| Loss of appetite | 294 | 42.7 | 108 | 15.7 | 25 | 4.8 |
| Itchiness of the skin (pruritus) | 281 | 40.8 | 193 | 28.0 | 52 | 7.5 |
| Weight loss | 282 | 40.9 | 105 | 15.2 | 22 | 3.2 |
| -Body aches | ||||||
| Sore throat | 422 | 61.2 | 215 | 31.2 | 45 | 6.5 |
| Joint pain | 576 | 83.6 | 499 | 72.4 | 378 | 54.9 |
| Muscle pain | 623 | 90.4 | 528 | 76.6 | 426 | 61.8 |
| Thoracic pain | 441 | 64.0 | 312 | 45.3 | 208 | 30.2 |
| Back pain | 478 | 69.4 | 372 | 54.0 | 243 | 35.3 |
| Feeling of tightness in the chest | 486 | 70.5 | 349 | 50.7 | 245 | 35.6 |
| Stomach pain | 315 | 45.7 | 212 | 30.8 | 108 | 15.7 |
| Abdominal pain | 330 | 47.9 | 227 | 32.9 | 117 | 17.0 |
| -Respiratory | ||||||
| Cough | 453 | 65.7 | 237 | 34.4 | 89 | 12.9 |
| Sputum or phlegm (bronchial secretion) | 176 | 25.5 | 102 | 14.8 | 25 | 3.6 |
| Hemoptysis (coughing of blood) | 31 | 4.5 | 11 | 1.6 | 5 | 0.7 |
| Difficulty breathing or shortness of breath | 513 | 74.5 | 365 | 53.0 | 330 | 47.9 |
| Breathlessness, dyspnea | 558 | 81.0 | 453 | 65.7 | 378 | 54.9 |
| Nasal congestion (mucus) | 314 | 45.6 | 176 | 31.6 | 54 | 11.5 |
| Aphonia or hoarseness | 304 | 44.1 | 185 | 26.9 | 82 | 11.9 |
| -Digestive | ||||||
| Nausea | 320 | 46.4 | 190 | 27.6 | 100 | 14.5 |
| Vomiting | 122 | 17.7 | 40 | 5.8 | 33 | 4.8 |
| Diarrhea | 360 | 52.2 | 187 | 27.1 | 110 | 16.0 |
| -Neurological | ||||||
| Dizziness | 472 | 68.5 | 367 | 53.3 | 12 | 1.7 |
| Vertigo | 302 | 43.8 | 217 | 31.5 | 184 | 26.7 |
| Tremor | 267 | 38.8 | 163 | 23.7 | 87 | 12.6 |
| Paresthesia | 338 | 49.1 | 267 | 38.8 | 149 | 21.6 |
| Loss of smell | 366 | 53.1 | 141 | 20.5 | 51 | 7.4 |
| Loss of taste | 351 | 50.9 | 110 | 16.0 | 38 | 5.5 |
| Seizure | 31 | 4.5 | 21 | 3.0 | 12 | 1.7 |
| Memory loss | 533 | 77.4 | 484 | 70.2 | 399 | 57.9 |
| Mental confusion | 512 | 74.3 | 466 | 67.6 | 417 | 60.5 |
| Brain fog | 538 | 78.1 | 472 | 68.5 | 435 | 63.1 |
| Lack of concentration/attention deficit | 604 | 87.7 | 543 | 78.8 | 476 | 69.1 |
| Trouble sleeping (insomnia) | 521 | 75.6 | 431 | 62.6 | 321 | 46.6 |
| Posttraumatic stress | 280 | 40.6 | 220 | 31.9 | 167 | 24.2 |
| -Ocular | ||||||
| Conjunctivitis | 139 | 20.2 | 89 | 12.9 | 40 | 5.8 |
| Blurred vision, foreign body sensation, eye congestion | 421 | 61.6 | 332 | 48.1 | 150 | 21.8 |
| Dry eyes | 323 | 46.9 | 272 | 39.5 | 112 | 16.3 |
| -Dermatological | ||||||
| Hives or eczema on the skin | 267 | 38.8 | 169 | 24.4 | 39 | 5.7 |
| Facial erythema | 138 | 20.0 | 76 | 11.0 | 13 | 1.9 |
| Acrosyndrome | 121 | 17.6 | 72 | 11.0 | 32 | 4.6 |
| -Cardiovascular | ||||||
| Palpitation | 453 | 65.7 | 332 | 48.2 | 185 | 26.9 |
| High blood pressure | 192 | 27.9 | 145 | 21.0 | 65 | 9.4 |
| Low blood pressure | 127 | 18.4 | 94 | 13.6 | 32 | 4.6 |
| -Others | ||||||
| Swelling or inflammation in the fingers | 202 | 29.3 | 141 | 20.5 | 56 | 8.1 |
| Trouble swallowing | 193 | 28.0 | 123 | 17.9 | 52 | 7.5 |
| Tinnitus (ringing in the ears) | 326 | 47.3 | 260 | 37.7 | 103 | 14.9 |
| Hair loss | 430 | 62.4 | 252 | 36.6 | 41 | 6.0 |
| Menstrual disorder (women) | 230 | 33.4 | 150 | 21.8 | ------- ------- | |
| Erection dysfunction (men) | 49 | 7.1 | 7 | 1.0 | ||
| Affected Systems | n | % | 95% CI |
|---|---|---|---|
| Mental disorder (psychological/emotional) | 505 | 73.3 | 70.0–76.6 |
| Nervous system | 496 | 72.0 | 68.6–75.3 |
| Respiratory system | 455 | 66.0 | 62.5–69.6 |
| Digestive system | 336 | 48.8 | 45.0–52.5 |
| Endocrine system | 155 | 22.5 | 19.4–25.6 |
| Locomotor system | 390 | 56.6 | 52.9–60.3 |
| Cardiovascular system | 333 | 48.3 | 44.6–52.1 |
| Nephrourological system | 109 | 15.8 | 13.1–18.5 |
| Hematological system (coagulation) | 137 | 19.9 | 16.9–22.9 |
| Dermatological system | 210 | 30.5 | 27.0–33.9 |
| Otorhinolaryngological system | 223 | 32.4 | 28.9–35.9 |
| Eye system | 302 | 43.8 | 40.1–47.5 |
| Diseases and Chronic Medical Conditions | n | % | 95% IC |
|---|---|---|---|
| Arterial hypertension | 128 | 18.6 | 15.7–21.5 |
| Diabetes Mellitus | 31 | 4.5 | 3.0–6.0 |
| Chronic Obstructive Pulmonary Disease (COPD). | 25 | 3.6 | 2.2–5.0 |
| Bronchial asthma | 136 | 19.7 | 16.8–22.7 |
| Respiratory insufficiency | 130 | 18.9 | 15.9–21.8 |
| Hyperlipidemia | 185 | 26.9 | 23.5–30.2 |
| Overweight or obese | 235 | 34.1 | 30.6–37.6 |
| Immunosuppression (low defense level, HIV, …) | 110 | 16.0 | 13.2–18.7 |
| Autoimmune disease (ulcerative colitis…) | 89 | 12.9 | 10.4–15.4 |
| Cancer | 8 | 1.2 | 0.4–2.0 |
| Kidney failure | 24 | 3.5 | 2.1–4.9 |
| Heart failure | 39 | 5.7 | 3.9–7.4 |
| Heart disease (atrial fibrillation, heart valve disease, myocardial infarctions, angina pectoris, left ventricular hypertrophy, …) | 62 | 9.0 | 6.9–11.1 |
| Cardiovascular disease (vascular accident, stroke, artery disease, …) | 35 | 5.1 | 3.4–6.7 |
| Anxiety disorder | 312 | 45.3 | 41.6–49.0 |
| Depression | 187 | 27.1 | 23.8–30.5 |
| Mental illness (neurosis, psychosis, …) | 33 | 4.8 | 3.2–6.4 |
| Neurological disease | 174 | 25.3 | 22.0–28.5 |
| Endocrine disease (hypothyroidism, …) | 124 | 18.0 | 15.1–20.9 |
| Liver disease | 16 | 2.3 | 1.2–3.4 |
| Drugs | n | % | 95% IC |
|---|---|---|---|
| Analgesics | 410 | 59.5 | 55.8–63.2 |
| Anti-inflammatories | 321 | 56.4 | 42.9–50.3 |
| Anxiolytics | 193 | 36.7 | 24.7–31.4 |
| Antidepressants | 218 | 28.0 | 28.2–35.1 |
| Anticoagulants | 58 | 8.4 | 6.3–10.5 |
| Corticosteroids | 119 | 17.3 | 14.4–20.1 |
| Calcifediol (vitamin D) | 290 | 42.1 | 38.4–45.8 |
| Other drugs | 349 | 50.7 | 46.9–54.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romero-Rodríguez, E.; Perula-de-Torres, L.Á.; González-Lama, J.; Castro-Jiménez, R.Á.; Jiménez-García, C.; Priego-Pérez, C.; Vélez-Santamaría, R.; Simón-Vicente, L.; González-Santos, J.; González-Bernal, J.J. Long COVID Symptomatology and Associated Factors in Primary Care Patients: The EPICOVID-AP21 Study. Healthcare 2023, 11, 218. https://doi.org/10.3390/healthcare11020218
Romero-Rodríguez E, Perula-de-Torres LÁ, González-Lama J, Castro-Jiménez RÁ, Jiménez-García C, Priego-Pérez C, Vélez-Santamaría R, Simón-Vicente L, González-Santos J, González-Bernal JJ. Long COVID Symptomatology and Associated Factors in Primary Care Patients: The EPICOVID-AP21 Study. Healthcare. 2023; 11(2):218. https://doi.org/10.3390/healthcare11020218
Chicago/Turabian StyleRomero-Rodríguez, Esperanza, Luis Ángel Perula-de-Torres, Jesús González-Lama, Rafael Ángel Castro-Jiménez, Celia Jiménez-García, Carmen Priego-Pérez, Rodrigo Vélez-Santamaría, Lucía Simón-Vicente, Josefa González-Santos, and Jerónimo J. González-Bernal. 2023. "Long COVID Symptomatology and Associated Factors in Primary Care Patients: The EPICOVID-AP21 Study" Healthcare 11, no. 2: 218. https://doi.org/10.3390/healthcare11020218
APA StyleRomero-Rodríguez, E., Perula-de-Torres, L. Á., González-Lama, J., Castro-Jiménez, R. Á., Jiménez-García, C., Priego-Pérez, C., Vélez-Santamaría, R., Simón-Vicente, L., González-Santos, J., & González-Bernal, J. J. (2023). Long COVID Symptomatology and Associated Factors in Primary Care Patients: The EPICOVID-AP21 Study. Healthcare, 11(2), 218. https://doi.org/10.3390/healthcare11020218







