Healthcare Waste—A Serious Problem for Global Health
Abstract
1. Introduction
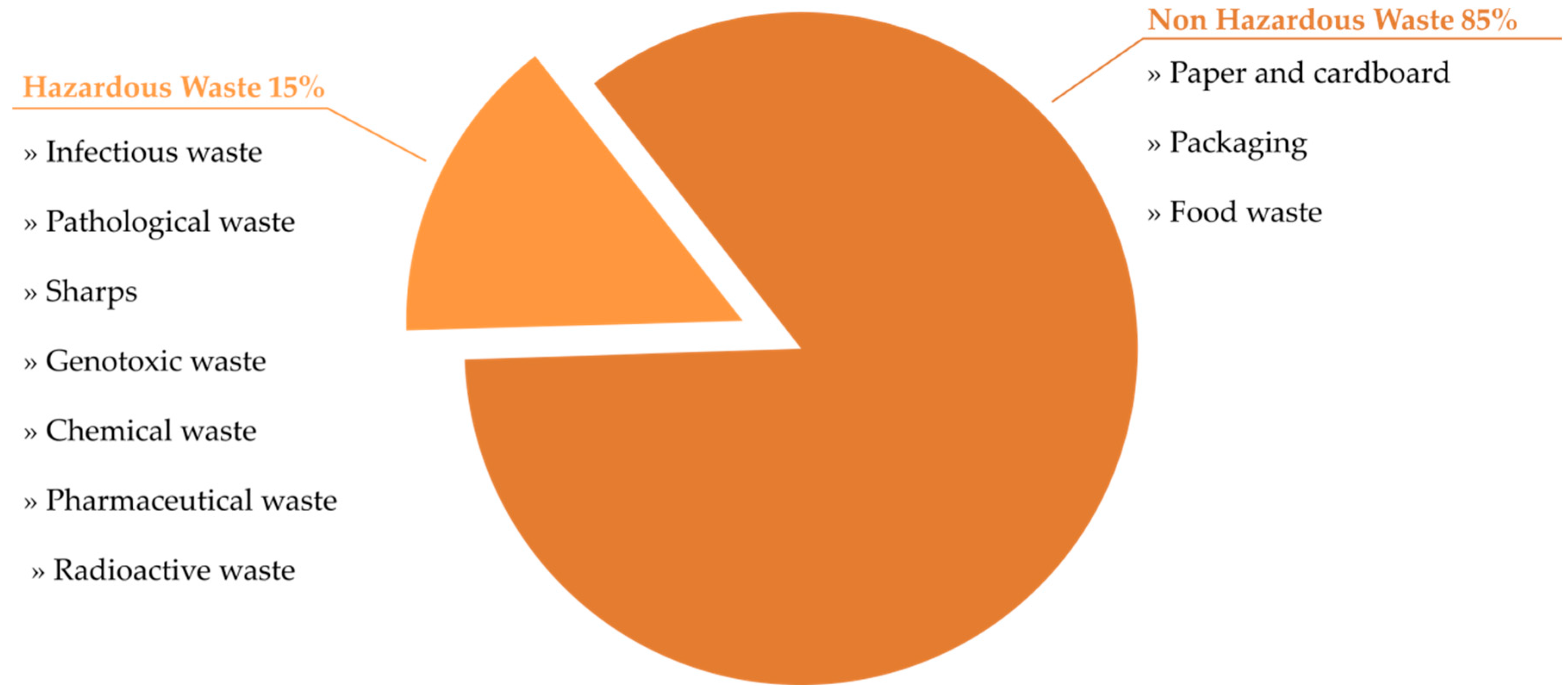
2. Categories and Sources of HCW
3. HCW Production Rate
4. HCW Production Rate during Pandemic
5. HCW Management
6. HCW Management during COVID-19 Pandemic
7. Risk Related to HCW
7.1. Infectious Waste and Sharps
7.2. Chemical and Pharmaceutical Waste
7.3. Genotoxic Waste
7.4. Radioactive Waste
8. HCW Treatment and Safety Issues
9. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Yazie, T.D.; Tebeje, M.G.; Chufa, K.A. Healthcare Waste Management Current Status and Potential Challenges in Ethiopia: A Systematic Review. BMC Res. Notes 2019, 12, 285. [Google Scholar] [CrossRef]
- Hasan, M.M.; Rahman, M.H. Assessment of Healthcare Waste Management Paradigms and Its Suitable Treatment Alternative: A Case Study. J. Environ. Public Health 2018, 2018, 6879751. [Google Scholar] [CrossRef]
- Dehghani, M.H.; Ahrami, H.D.; Nabizadeh, R.; Heidarinejad, Z.; Zarei, A. Medical Waste Generation and Management in Medical Clinics in South of Iran. MethodsX 2019, 6, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Taslimi, M.; Batta, R.; Kwon, C. Medical Waste Collection Considering Transportation and Storage Risk. Comput. Oper. Res. 2020, 120, 104966. [Google Scholar] [CrossRef]
- Chartier, Y.; World Health Organization. Safe Management of Wastes from Health-Care Activities; Nonserial Publication; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Kwikiriza, S.; Stewart, A.G.; Mutahunga, B.; Dobson, A.E.; Wilkinson, E. A Whole Systems Approach to Hospital Waste Management in Rural Uganda. Front. Public Health 2019, 7, 136. [Google Scholar] [CrossRef] [PubMed]
- Meleko, A.; Tesfaye, T.; Henok, A. Assessment of Healthcare Waste Generation Rate and Its Management System in Health Centers of Bench Maji Zone. Ethiop. J. Health Sci. 2018, 28, 125–134. [Google Scholar] [CrossRef]
- Khan, B.A.; Cheng, L.; Khan, A.A.; Ahmed, H. Healthcare Waste Management in Asian Developing Countries: A Mini Review. Waste Manag. Res. 2019, 37, 863–875. [Google Scholar] [CrossRef]
- Ciplak, N.; Kaskun, S. Healthcare Waste Management Practice in the West Black Sea Region, Turkey: A Comparative Analysis with the Developed and Developing Countries. J. Air Waste Manag. Assoc. 2015, 65, 1387–1394. [Google Scholar] [CrossRef]
- Santos, E.d.S.; Gonçalves, K.M.d.S.; Mol, M.P.G. Healthcare Waste Management in a Brazilian University Public Hospital. Waste Manag. Res. 2018, 37, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Kalogiannidou, K.; Nikolakopoulou, E.; Komilis, D. Generation and Composition of Waste from Medical Histopathology Laboratories. Waste Manag. 2018, 79, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Xin, Y. Comparison of Hospital Medical Waste Generation Rate Based on diagnosis-Related Groups. J. Clean. Prod. 2015, 100, 202–207. [Google Scholar] [CrossRef]
- Khobragade, D. Health Care Waste: Avoiding Hazards to Living and Non Living Environment by Efficient Management. Fortune J. Health Sci. 2019, 2, 14–29. [Google Scholar] [CrossRef]
- Aljabre, S.H.M. Hospital Generated Waste: A Plan for Its Proper Management. J. Fam. Community Med. 2002, 9, 61–65. [Google Scholar]
- Bokhoree, C.; Beeharry, Y.; Makoondlall-Chadee, T.; Doobah, T.; Soomary, N. Assessment of Environmental and Health Risks Associated with the Management of Medical Waste in Mauritius. APCBEE Procedia 2014, 9, 36–41. [Google Scholar] [CrossRef]
- Sepetis, A.; Zaza, P.N.; Rizos, F.; Bagos, P.G. Identifying and Predicting Healthcare Waste Management Costs for an Optimal Sustainable Management System: Evidence from the Greek Public Sector. Int. J. Environ. Res. Public Health 2022, 19, 9821. [Google Scholar] [CrossRef] [PubMed]
- Windfeld, E.S.; Brooks, M.S.-L. Medical Waste Management—A Review. J. Environ. Manag. 2015, 163, 98–108. [Google Scholar] [CrossRef]
- Singh, N.; Ogunseitan, O.A.; Tang, Y. Medical Waste: Current Challenges and Future Opportunities for Sustainable Management. Crit. Rev. Environ. Sci. Technol. 2022, 52, 2000–2022. [Google Scholar] [CrossRef]
- Minoglou, M.; Gerassimidou, S.; Komilis, D. Healthcare Waste Generation Worldwide and Its Dependence on Socio-Economic and Environmental Factors. Sustainability 2017, 9, 220. [Google Scholar] [CrossRef]
- Bdour, A.; Altrabsheh, B.; Hadadin, N.; Al-Shareif, M. Assessment of Medical Wastes Management Practice: A Case Study of the Northern Part of Jordan. Waste Manag. 2007, 27, 746–759. [Google Scholar] [CrossRef]
- Komilis, D.; Fouki, A.; Papadopoulos, D. Hazardous Medical Waste Generation Rates of Different Categories of Health-Care Facilities. Waste Manag. 2012, 32, 1434–1441. [Google Scholar] [CrossRef]
- Zamparas, M.; Kapsalis, V.C.; Kyriakopoulos, G.L.; Aravossis, K.G.; Kanteraki, A.E.; Vantarakis, A.; Kalavrouziotis, I.K. Medical Waste Management and Environmental Assessment in the Rio University Hospital, Western Greece. Sustain. Chem. Pharm. 2019, 13, 100163. [Google Scholar] [CrossRef]
- Rabeie, O.L.; Miranzadeh, M.B.; Fallah, S.H.; Dehqan, S.; Moulana, Z.; Amouei, A.; Mohammadi, A.A.; Asgharnia, H.A.; Babaie, M. Determination of Hospital Waste Composition and Management in Amol City, Iran. Health Scope 2012, 1, 127–131. [Google Scholar] [CrossRef]
- Gusca, J.; Kalnins, S.N.; Blumberga, D.; Bozhko, L.; Khabdullina, Z.; Khabdullin, A. Assessment Method of Health Care Waste Generation in Latvia and Kazakhstan. Energy Procedia 2015, 72, 175–179. [Google Scholar] [CrossRef]
- Gai, R.; Kuroiwa, C.; Xu, L.; Wang, X.; Zhang, Y.; Li, H.; Zhou, C.; He, J.; Tang, W. Hospital Medical Waste Management in Shandong Province, China. Waste Manag. Res. 2009, 27, 336–342. [Google Scholar]
- Zhang, H.-J.; Zhang, Y.-H.; Wang, Y.; Yang, Y.-H.; Zhang, J.; Wang, Y.-L.; Wang, J.-L. Investigation of Medical Waste Management in Gansu Province, China. Waste Manag. Res. 2013, 31, 655–659. [Google Scholar] [CrossRef]
- Eker, H.H.; Bilgili, M.S. Statistical Analysis of Waste Generation in Healthcare Services: A Case Study. Waste Manag. Res. 2011, 29, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Patil, G.V.; Pokhrel, K. Biomedical Solid Waste Management in an Indian Hospital: A Case Study. Waste Manag. 2005, 25, 592–599. [Google Scholar] [CrossRef]
- Da Silva, C.E.; Hoppe, A.E.; Ravanello, M.M.; Mello, N. Medical Wastes Management in the South of Brazil. Waste Manag. 2005, 25, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Diaz, L.F.; Eggerth, L.L.; Enkhtsetseg, S. Anejo de Residuos de Establecimientos de Salud en Guayaquil, Ecuador; Pan American Health Organization: Quito, Equador, 2001. [Google Scholar]
- Tesfahun, E.; Kumie, A.; Beyene, A. Developing Models for the Prediction of Hospital Healthcare Waste Generation Rate. Waste Manag. Res. 2016, 34, 75–80. [Google Scholar] [CrossRef]
- Wassie, B.; Gintamo, B.; Mekuria, Z.N.; Gizaw, Z. Healthcare Waste Management Practices and Associated Factors in Private Clinics in Addis Ababa, Ethiopia. Environ. Health Insights 2022, 16, 11786302211073383. [Google Scholar] [CrossRef]
- Shouman, E.; Al Bazedi, G.; Sorour, M.H.; Abulnour, A.G. Management of Hazardous Medical Waste Treatment in Egypt. World Appl. Sci. J. 2013, 28, 804–808. [Google Scholar]
- Saad, S.A.G. Management of Hospitals Solid Waste in Khartoum State. Environ. Monit. Assess. 2013, 185, 8567–8582. [Google Scholar] [CrossRef] [PubMed]
- Hassan, A.A.; Tudor, T.; Vaccari, M. Healthcare Waste Management: A Case Study from Sudan. Environments 2018, 5, 89. [Google Scholar] [CrossRef]
- Mbarki, A.; Kabbachi, B.; Ezaidi, A.; Benssaou, M. Medical Waste Management: A Case Study of the Souss-Massa-Draa Region, Morocco. J. Environ. Prot. 2013, 4, 36312. [Google Scholar] [CrossRef]
- Sangkham, S. Face Mask and Medical Waste Disposal During the Novel COVID-19 Pandemic in Asia. Case Stud. Chem. Environ. Eng. 2020, 2, 100052. [Google Scholar] [CrossRef]
- Peng, J.; Wu, X.; Wang, R.; Li, C.; Zhang, Q.; Wei, D. Medical Waste Management Practice During the 2019–2020 Novel Coronavirus Pandemic: Experience in a General Hospital. Am. J. Infect. Control 2020, 48, 918–921. [Google Scholar] [CrossRef]
- Singh, N.; Tang, Y.; Zhang, Z.; Zheng, C. COVID-19 Waste Management: Effective and Successful Measures in Wuhan, China. Resour. Conserv. Recycl. 2020, 163, 105071. [Google Scholar] [CrossRef]
- Rahman, M.M.; Bodrud-Doza, M.; Griffiths, M.D.; Mamun, M.A. Biomedical Waste Amid COVID-19: Perspectives from Bangladesh. Lancet. Glob. Health 2020, 8, e1262. [Google Scholar] [CrossRef]
- Ilyas, S.; Srivastava, R.R.; Kim, H. Disinfection Technology and Strategies for COVID-19 Hospital and Bio-Medical Waste Management. Sci. Total Environ. 2020, 749, 141652. [Google Scholar] [CrossRef]
- Arab, M.; Rouhollah Askari, B.; Tajvar, M.; Pourreza, A.; Omrani, G.; Mahmoudi, M. Report: The Assessment of Hospital Waste Management: A Case Study in Tehran. Waste Manag. Res. 2008, 26, 304–308. [Google Scholar] [CrossRef]
- Wafula, S.T.; Musiime, J.; Oporia, F. Health Care Waste Management among Health Workers and Associated Factors in Primary Health Care Facilities in Kampala City, Uganda: A Cross-Sectional Study. BMC Public Health 2019, 19, 203. [Google Scholar] [CrossRef]
- Sahiledengle, B. Self-Reported Healthcare Waste Segregation Practice and Its Correlate among Healthcare Workers in Hospitals of Southeast Ethiopia. BMC Health Serv. Res. 2019, 19, 591. [Google Scholar] [CrossRef]
- Tsakona, M.; Anagnostopoulou, E.; Gidarakos, E. Hospital Waste Management and Toxicity Evaluation: A Case Study. Waste Manag. 2007, 27, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Awodele, O.; Adewoye, A.A.; Oparah, A.C. Assessment of Medical Waste Management in Seven Hospitals in Lagos, Nigeria. BMC Public Health 2016, 16, 269. [Google Scholar] [CrossRef] [PubMed]
- Anozie, O.B.; Lawani, L.O.; Eze, J.N.; Mamah, E.J.; Onoh, R.C.; Ogah, E.O.; Umezurike, D.A.; Anozie, R.O. Knowledge, Attitude and Practice of Healthcare Managers to Medical Waste Management and Occupational Safety Practices: Findings from Southeast Nigeria. J. Clin. Diagn. Res. JCDR 2017, 11, IC01–IC04. [Google Scholar] [CrossRef]
- Ozder, A.; Teker, B.; Eker, H.H.; Altındis, S.; Kocaakman, M.; Karabay, O. Medical Waste Management Training for Healthcare Managers—A Necessity? J. Environ. Health Sci. Eng. 2013, 11, 20. [Google Scholar] [CrossRef]
- Parida, A.; Capoor, M.R.; Bhowmik, K.T. Knowledge, Attitude, and Practices of Bio-Medical Waste Management Rules, 2016; Bio-Medical Waste Management (Amendment) Rules, 2018; and Solid Waste Rules, 2016, among Health-Care Workers in a Tertiary Care Setup. J. Lab. Physicians 2019, 11, 292–299. [Google Scholar] [CrossRef]
- Akulume, M.; Kiwanuka, S.N. Health Care Waste Segregation Behavior among Health Workers in Uganda: An Application of the Theory of Planned Behavior. J. Environ. Public Health 2016, 2016, 8132306. [Google Scholar] [CrossRef] [PubMed]
- Datta, P.; Mohi, G.K.; Chander, J. Biomedical Waste Management in India: Critical Appraisal. J. Lab. Physicians 2018, 10, 6–14. [Google Scholar] [CrossRef]
- Pandey, A.; Ahuja, S.; Madan, M.; Asthana, A.K. Bio-Medical Waste Managment in a Tertiary Care Hospital: An Overview. J. Clin. Diagn. Res. JCDR 2016, 10, DC01–DC03. [Google Scholar] [CrossRef]
- World Health Organization. Safe Management of Wastes from Health-Care Activities: A Summary; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Singh, H.; Rehman, R.; Bumb, S. Management of Biomedical Waste: A Review. Int. J. Dent. Med. Res. 2014, 1, 14–20. [Google Scholar]
- Nghiem, L.D.; Morgan, B.; Donner, E.; Short, M.D. The COVID-19 Pandemic: Considerations for the Waste and Wastewater Services Sector. Case Stud. Chem. Environ. Eng. 2020, 1, 100006. [Google Scholar] [CrossRef]
- Mol, M.P.G.; Caldas, S. Can the Human Coronavirus Epidemic Also Spread through Solid Waste? Waste Manag. Res. 2020, 38, 485–486. [Google Scholar] [CrossRef] [PubMed]
- Sharma, H.B.; Vanapalli, K.R.; Cheela, V.R.S.; Ranjan, V.P.; Jaglan, A.K.; Dubey, B.; Goel, S.; Bhattacharya, J. Challenges, Opportunities, and Innovations for Effective Solid Waste Management During and Post COVID-19 Pandemic. Resour. Conserv. Recycl. 2020, 162, 105052. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Yu, X.; Wu, X.; Wang, J.; Yan, X.; Jiang, S.; Chen, Z. Emergency Response to the Explosive Growth of Health Care Wastes During COVID-19 Pandemic in Wuhan, China. Resour. Conserv. Recycl. 2021, 164, 105074. [Google Scholar] [CrossRef]
- Sarkodie, S.A.; Owusu, P.A. Impact of COVID-19 Pandemic on Waste Management. Environ. Dev. Sustain. 2020, 23, 7951–7960. [Google Scholar] [CrossRef]
- Meister, T.L.; Dreismeier, M.; Blanco, E.V.; Brüggemann, Y.; Heinen, N.; Kampf, G.; Todt, D.; Nguyen, H.P.; Steinmann, J.; Schmidt, W.E.; et al. Low Risk of Severe Acute Respiratory Syndrome Coronavirus 2 Transmission by Fomites: A Clinical Observational Study in Highly Infectious Coronavirus Disease 2019 Patients. J. Infect. Dis. 2022, 226, 1608–1615. [Google Scholar] [CrossRef]
- Padmanabhan, K.K.; Barik, D. Health Hazards of Medical Waste and Its Disposal. In Energy from Toxic Organic Waste for Heat and Power Generation; Elsevier: Amsterdam, The Netherlands, 2019; pp. 99–118. [Google Scholar] [CrossRef]
- Makajic-Nikolic, D.; Petrovic, N.; Belic, A.; Rokvic, M.; Radakovic, J.A.; Tubic, V. The Fault Tree Analysis of Infectious Medical Waste Management. J. Clean. Prod. 2016, 113, 365–373. [Google Scholar] [CrossRef]
- Park, H.; Lee, K.; Kim, M.; Lee, J.; Seong, S.-Y.; Ko, G. Detection and Hazard Assessment of Pathogenic Microorganisms in Medical Wastes. J. Environ. Sci. Health. Part A Toxic/Hazard. Subst. Environ. Eng. 2009, 44, 995–1003. [Google Scholar] [CrossRef]
- Blenkharn, I.; Odd, C. Sharps Injuries in Healthcare Waste Handlers. Ann. Occup. Hyg. 2008, 52, 281–286. [Google Scholar] [CrossRef]
- Udofia, E.A.; Gulis, G.; Fobil, J. Solid Medical Waste: A Cross Sectional Study of Household Disposal Practices and Reported Harm in Southern Ghana. BMC Public Health 2017, 17, 464. [Google Scholar] [CrossRef] [PubMed]
- Jahangiri, M.; Rostamabadi, A.; Hoboubi, N.; Tadayon, N.; Soleimani, A. Needle Stick Injuries and Their Related Safety Measures among Nurses in a University Hospital, Shiraz, Iran. Saf. Health Work 2016, 7, 72–77. [Google Scholar] [CrossRef]
- Gupta, D.K.; Singh, M.; Agarwal, V.K.; Sharma, S.; Mishra, S. A Study of Contaminated Sharp Injury and Associated Morbidity among Health Care Workers. Int. J. Community Med. Public Health 2020, 7, 183. [Google Scholar] [CrossRef]
- Singh, N.; Tang, Y.; Ogunseitan, O.A. Environmentally Sustainable Management of Used Personal Protective Equipment. Environ. Sci. Technol. 2020, 54, 8500–8502. [Google Scholar] [CrossRef]
- Amsalu, A.; Worku, M.; Tadesse, E.; Shimelis, T. The Exposure Rate to Hepatitis B and C Viruses among Medical Waste Handlers in Three Government Hospitals, Southern Ethiopia. Epidemiol. Health 2016, 38, e2016001. [Google Scholar] [CrossRef]
- Doddaiah, V.; Janakiram, K.; Javagal, S. Seroprevalence of Hepatitis B Virus and Hepatitis C Virus in Healthcare Workers-Aims, Bg Nagara. Am. J. Life Sci. 2013, 1, 145–149. [Google Scholar]
- Shiferaw, Y.; Abebe, T.; Mihret, A. Hepatitis B Virus Infection among Medical Aste Handlers in Addis Ababa, Ethiopia. BMC Res. Notes 2011, 4, 479. [Google Scholar] [CrossRef]
- Akpieyi, A.; Tudor, T.L.; Dutra, C. The Utilisation of Risk-Based Frameworks for Managing Healthcare Waste: A Case Study of the National Health Service in London. Saf. Sci. 2015, 72, 127–132. [Google Scholar] [CrossRef]
- Anagaw, B.; Shiferaw, Y.; Anagaw, B.; Belyhun, Y.; Erku, W.; Biadgelegn, F.; Moges, B.; Alemu, A.; Moges, F.; Mulu, A. Seroprevalence of Hepatitis B and C Viruses among Medical Waste Handlers at Gondar Town Health Institutions, Northwest Ethiopia. BMC Res. Notes 2012, 5, 55. [Google Scholar] [CrossRef]
- Alemayehu, T.; Worku, A.; Assefa, N. Medical Waste Collectors in Eastern Ethiopia Are Exposed to High Sharp Injury and Blood and Body Fluids Contamination. Prev. Inf. Cntrl. 2016, 2, 2. [Google Scholar] [CrossRef]
- He, L.; Lu, Z.; Huang, J.; Zhou, Y.; Huang, J.; Bi, Y.; Li, J. An Integrated Intervention for Increasing Clinical Nurses’ Knowledge of Hiv/Aids-Related Occupational Safety. Int. J. Environ. Res. Public Health 2016, 13, 1094. [Google Scholar] [CrossRef]
- Saadeh, R.; Khairallah, K.; Abozeid, H.; Al Rashdan, L.; Alfaqih, M.; Alkhatatbeh, O. Needle Stick and Sharp Injuries among Healthcare Workers: A Retrospective Six-Year Study. Sultan Qaboos Univ. Med. J. 2020, 20, e54–e62. [Google Scholar] [CrossRef]
- Khraisat, F.S.; Juni, M.H.; Salmiah, M.S.; Abd Rahman, A.; Hamdan-Mansour, A. Needle Stick Injuries Prevalence among Nurses in Jordanian Hospitals. Int. J. Public Health Clin. Sci. 2015, 2, 7–16. [Google Scholar]
- De Carli, G.; Abiteboul, D.; Puro, V. The Importance of Implementing Safe Sharps Practices in the Laboratory Setting in Europe. Biochem. Med. 2014, 24, 45–56. [Google Scholar] [CrossRef]
- Ghanei Gheshlagh, R.; Aslani, M.; Shabani, F.; Dalvand, S.; Parizad, N. Prevalence of Needlestick and Sharps Injuries in the Healthcare Workers of Iranian Hospitals: An Updated Meta-Analysis. Environ. Health Prev. Med. 2018, 23, 44. [Google Scholar] [CrossRef]
- Kakizaki, M.; Ikeda, N.; Ali, M.; Enkhtuya, B.; Tsolmon, M.; Shibuya, K.; Kuroiwa, C. Needlestick and Sharps Injuries among Health Care Workers at Public Tertiary Hospitals in an Urban Community in Mongolia. BMC Res. Notes 2011, 4, 184. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, C.; Sakisaka, K.; Sychareun, V.; Phensavanh, A.; Ali, M. Prevalence and Risk Factors of Needle Stick and Sharp Injury among Tertiary Hospital Workers, Vientiane, Lao Pdr. J. Occup. Health 2017, 59, 581–585. [Google Scholar] [CrossRef]
- Doggalli, D.N. Hazards and Public Health Impacts of Hospital Waste. J. Appl. Res. 2014, 4, 384. [Google Scholar] [CrossRef]
- Shaaban, H.; Alghamdi, H.; Alhamed, N.; Alziadi, A.; Mostafa, A. Environmental Contamination by Pharmaceutical Waste: Assessing Patterns of Disposing Unwanted Medications and Investigating the Factors Influencing Personal Disposal Choices. J. Pharmacol. Pharm. Res. 2018, 1, 003. [Google Scholar]
- Sasu, S.; Kümmerer, K.; Kranert, M. Assessment of Pharmaceutical Waste Management at Selected Hospitals and Homes in Ghana. Waste Manag. Res. 2011, 30, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Kümmerer, K. Pharmaceuticals in the Environment. Annu. Rev. Environ. Resour. 2010, 35, 57–75. [Google Scholar] [CrossRef]
- Sangion, A.; Gramatica, P. Hazard of Pharmaceuticals for Aquatic Environment: Prioritization by Structural Approaches and Prediction of Ecotoxicity. Environ. Int. 2016, 95, 131–143. [Google Scholar] [CrossRef]
- Chi, T.; Zhang, A.; Zhang, X.; Li, A.-D.; Zhang, H.; Zhao, Z. Characteristics of the Antibiotic Resistance Genes in the Soil of Medical Waste Disposal Sites. Sci. Total Environ. 2020, 730, 139042. [Google Scholar] [CrossRef]
- Forsberg, K.J.; Reyes, A.; Wang, B.; Selleck, E.M.; Sommer, M.O.A.; Dantas, G. The Shared Antibiotic Resistome of Soil Bacteria and Human Pathogens. Science 2012, 337, 1107. [Google Scholar] [CrossRef]
- Ghasemi, L.; Yousefzadeh, S.; Rastkari, N.; Naddafi, K.; Shariati Far, N.; Nabizadeh, R. Evaluate the Types and Amount of Genotoxic Waste in Tehran University of Medical Science’s Hospitals. J. Environ. Health Sci. Eng. 2018, 16, 171–179. [Google Scholar] [CrossRef]
- Connor, T.H.; Lawson, C.C.; Polovich, M.; McDiarmid, M.A. Reproductive Health Risks Associated with Occupational Exposures to Antineoplastic Drugs in Health Care Settings: A Review of the Evidence. J. Occup. Environ. Med. 2014, 56, 901–910. [Google Scholar] [CrossRef] [PubMed]
- Shahrasbi, A.A.; Afshar, M.; Shokraneh, F.; Monji, F.; Noroozi, M.; Ebrahimi-Khojin, M.; Madani, S.F.; Ahadi-Barzoki, M.; Rajabi, M. Risks to Health Professionals from Hazardous Drugs in Iran: A Pilot Study of Understanding of Healthcare Team to Occupational Exposure to Cytotoxics. EXCLI J. 2014, 13, 491–501. [Google Scholar]
- Capoor, M.R.; Bhowmik, K.T. Cytotoxic Drug Dispersal, Cytotoxic Safety, and Cytotoxic Waste Management: Practices and Proposed India-Specific Guidelines. Indian J. Med. Paediatr. Oncol. Off. J. Indian Soc. Med. Paediatr. Oncol. 2017, 38, 190–197. [Google Scholar] [CrossRef]
- Simegn, W.; Dagnew, B.; Dagne, H. Knowledge and Associated Factors Towards Cytotoxic Drug Handling among University of Gondar Comprehensive Specialized Hospital Health Professionals, Institutional-Based Cross-Sectional Study. Environ. Health Prev. Med. 2020, 25, 11. [Google Scholar] [CrossRef] [PubMed]
- Viegas, S.; Ladeira, C.; Costa-Veiga, A.; Perelman, J.; Gajski, G. Forgotten Public Health Impacts of Cancer—An Overview. Arch. Ind. Hyg. Toxicol. 2017, 68, 287–297. [Google Scholar] [CrossRef]
- Kovács, R.; Csenki, Z.; Bakos, K.; Urbányi, B.; Horváth, Á.; Garaj-Vrhovac, V.; Gajski, G.; Gerić, M.; Negreira, N.; López de Alda, M.; et al. Assessment of Toxicity and Genotoxicity of Low Doses of 5-Fluorouracil in Zebrafish (Danio Rerio) Two-Generation Study. Water Res. 2015, 77, 201–212. [Google Scholar] [CrossRef] [PubMed]
- Borowy, I. Medical Waste: The Dark Side of Healthcare. História Ciências Saúde-Manguinhos 2020, 27, 231–251. [Google Scholar] [CrossRef]
- Njagi, N.A.; Oloo, M.A.; Kithinji, J.; Kithinji, M.J. Health-Care Waste Incineration and Related Dangers to Public Health: Case Study of the Two Teaching and Referral Hospitals in Kenya. J. Community Health 2012, 37, 1168–1171. [Google Scholar] [CrossRef]
- de Titto, E.; Savino, A. Environmental and Health Risks Related to Waste Incineration. Waste Manag. Res. 2019, 37, 976–986. [Google Scholar] [CrossRef]
- Jang, Y.-C.; Lee, C.; Yoon, O.-S.; Kim, H. Medical Waste Management in Korea. J. Environ. Manag. 2006, 80, 107–115. [Google Scholar] [CrossRef]
- Federico, M.; Pirani, M.; Rashid, I.; Caranci, N.; Cirilli, C. Cancer Incidence in People with Residential Exposure to a Municipal Waste Incinerator: An Ecological Study in Modena (Italy), 1991–2005. Waste Manag. 2010, 30, 1362–1370. [Google Scholar] [CrossRef] [PubMed]
- Santoro, M.; Minichilli, F.; Linzalone, N.; Coi, A.; Maurello, M.T.; Sallese, D.; Bianchi, F. Adverse Reproductive Outcomes Associated with Exposure to a Municipal Solid Waste Incinerator. Ann. Dell’istituto Super. Sanita 2016, 52, 576–581. [Google Scholar]
- Domingo, J.L.; Marquès, M.; Mari, M.; Schuhmacher, M. Adverse Health Effects for Populations Living near Waste Incinerators with Special Attention to Hazardous Waste Incinerators. A Review of the Scientific Literature. Environ. Res. 2020, 187, 109631. [Google Scholar] [CrossRef]
- Saria, J.A. Levels of Heavy Metals in Bottom Ash from Medical Waste Incinerators in Dar Es Salaam. J. Multidiscip. Eng. Sci. Stud. 2016, 2, 599–605. [Google Scholar]
- Ephraim, P.I.; Ita, A.; Eusebius, I.O. Investigation of Soils Affected by Burnt Hospital Wastes in Nigeria Using Pixe. SpringerPlus 2013, 2, 208. [Google Scholar] [CrossRef]
- Dash, A.; Kumar, S.; Singh, R.K. Thermolysis of Medical Waste (Waste Syringe) to Liquid Fuel Using Semi Batch Reactor. Waste Biomass Valoriz. 2015, 6, 507–514. [Google Scholar] [CrossRef]
- Fang, S.; Jiang, L.; Li, P.; Bai, J.; Chang, C. Study on Pyrolysis Products Characteristics of Medical Waste and Fractional Condensation of the Pyrolysis Oil. Energy 2020, 195, 116969. [Google Scholar] [CrossRef]
- Ismail, Z.Z.; Talib, A.R. Recycled Medical Cotton Industry Waste as a Source of Biogas Recovery. J. Clean. Prod. 2016, 112, 4413–4418. [Google Scholar] [CrossRef]
- Olaifa, A.; Govender, R.D.; Ross, A.J. Knowledge, Attitudes and Practices of Healthcare Workers About Healthcare Waste Management at a District Hospital in Kwazulu-Natal. S. Afr. Fam. Pract. 2018, 60, 137–145. [Google Scholar] [CrossRef]
- Aung, T.S.; Luan, S.; Xu, Q. Application of Multi-Criteria-Decision Approach for the Analysis of Medical Waste Management Systems in Myanmar. J. Clean. Prod. 2019, 222, 733–745. [Google Scholar] [CrossRef]
- Woolridge, A.; Hoboy, S. Chapter 27—Medical Waste. In Waste, 2nd ed.; Letcher, T.M., Vallero, D.A., Eds.; Academic Press: Cambridge, MA, USA, 2019; pp. 517–530. [Google Scholar]
- Elnour, A.M.; Moussa, M.M.R.; El-Borgy, M.D.; Fadelella, N.E.E.; Mahmoud, A.H. Impacts of Health Education on Knowledge and Practice of Hospital Staff with Regard to Healthcare Waste Management at White Nile State Main Hospitals, Sudan. Int. J. Health Sci. 2015, 9, 315–331. [Google Scholar] [CrossRef]
- Babanyara, Y.Y.; Aliyu, A.; Gana, B.A.; Musa, M. A Review of the Knowledge, Attitude, and Practices of Healthcare Wastes Workers (Hcws) on Medical Waste in Developing Countries. In Risks and Challenges of Hazardous Waste Management: Reviews and Case Studies; Bentham Science Publishers: Karachi, Pakistan, 2020; p. 25. [Google Scholar]
| Waste Categories | Descriptions and Examples |
|---|---|
| Hazardous HCW | |
| Sharps waste | Used or unused sharps, e.g., intravenous, hypodermic or other needles, syringes with attached needles, auto-disable syringes, infusion sets, scalpels, knives, blades, pipettes, broken glass and vials |
| Infectious waste | Waste suspected of containing pathogens and presenting a risk of disease transmission, e.g., laboratory culture and microbiological stocks, waste contaminated with blood and other body fluids, waste including excreta and other materials that have been in contact with infected patients with highly infectious diseases in isolated wards |
| Pathological waste | Human and animal organs, tissues or fluids, body parts, fetuses, placentas, unused blood products, contaminated animal carcasses |
| Pharmaceutical waste | Expired pharmaceuticals, unused, contaminated vaccines and drugs, items contaminated by or containing pharmaceuticals |
| Cytotoxic waste | Waste containing substances with genotoxic properties (mutagenic, carcinogenic or teratogenic substances), e.g., cytotoxic drugs used in cancer therapy and their metabolites |
| Chemical waste | Waste containing chemicals, e.g., expired or unused disinfectants or laboratory reagents, unused, solvents, waste with high heavy metal content, such as batteries, blood pressure gauges, mercury-containing equipment and devices (e.g., old thermometers) |
| Radioactive waste | Waste containing radioactives, e.g., unused radiotherapy liquids, radioactive diagnostic material, contaminated packages, absorbent paper or glassware, urine and excreta from patients tested or treated with radionuclides, radioactive sealed sources |
| Non-hazardous or general HCW | Waste, which does not pose any particular biological, chemical, physical or radioactive hazard |
| Source | Sharp Medical Instruments | Infectious Waste | Medications, Chemicals and Potentially Toxic Waste | Non-Hazardous Waste |
|---|---|---|---|---|
| Medical department | Intravenous needles, hypodermic needles, broken ampules and vials | Bandages, dressings, gauze, gloves and masks contaminated with blood or body fluids | Broken thermometers and blood pressure gauges; split medications and disinfectants | Empty bottles, non-blood intravenous tubing, non-blood diapers and bags, packaging, flowers, paper, food scraps |
| Operating room | Needles, blades, scalpels, surgical power tools | Masks, gowns, gloves, gauze and medical equipment contaminated with blood and body fluids; organs and tissues | Anesthetic gases, disinfectant products | Package, uncontaminated medical clothing and medical personal protective equipment |
| Veterinary clinics | Needles, broken glass and vials, pipettes, Petri dishes, slides and cover slips, needles sets, blades, scalpels, syringes | Dressings, bandages, masks, gloves, sample tubes and containers contaminated with blood and body fluids; infected animal carcasses | Anesthetic gases, disinfectants, broken blood pressure gauges and thermometers, split medicaments and vaccines, dental amalgam fillings, vaccines; contaminated urine and excreta | Package, containers, paper, uncontaminated masks, gloves, hats, shoe covers and gowns, empty bottles, empty bottles, non-blood intravenous tubing, non-blood diapers and bags, paper, animal food scraps |
| Laboratory | Broken glass, vials, pipettes and slides | Blood and body fluids, microbiological cultures, sample tubes and containers contaminated with blood and body fluids; infected animal carcasses | Broken thermometers, chemicals, such as methanol, fixatives, formalin, toluene, xylene, medications, disinfectants | Package, containers, paper, uncontaminated masks, gloves, hats, shoe covers and gowns, empty bottles |
| Oncology department | Syringes and needles | Bulk chemotherapy drugs; gloves and materials contaminated with cytotoxic drugs; contaminated urine and excreta | Package, paper | |
| Pharmacy store | Expired and split medicaments and their components; gloves | Package, paper, empty containers | ||
| Vaccination proccess | Syringes and needles | Bulk and split vaccine, vials and gloves | Package, paper, empty containers | |
| Doctors’ offices | Syringes and needles, broken vials | Dressings, gauze, masks, gloves, sample tubes and containers, contaminated with blood and body fluids | Broken thermometers and blood pressure gauges; expired drugs and spent disinfectants | Package, paper, empty containers, newspapers, uncontaminated medical personal protective equipment |
| Dental clinics | Syringes and needles, broken vials | Dressings, gauze, masks, gloves, sample tubes and containers, contaminated with blood and body fluids | Dental amalgam fillings, disinfectants | Package, paper, empty containers, newspapers, uncontaminated medical personal protective equipment |
| Patients’ home | Insulin injection needles | Dressings and gauze contaminated with blood and body fluids | Broken thermometers and blood pressure gauges | Household waste |
| Continent | Countries | HCW Generation (kg/bed/day) | Reference |
|---|---|---|---|
| North America | USA | 8.4–10.7 | [16,17,18] |
| Canada | 8.2 | [16,19] | |
| Europe | Spain | 3.5–4.4 | [17,18,20] |
| Norway | 3.9 | [18,20] | |
| Greece | 0.3–3.6 | [18,21,22] | |
| France | 2.7–3.3 | [17,18,23] | |
| Asia | Kazakhstan | 5.34–5.4 | [8,18,24] |
| China | 0.6–4.03 | [18,25,26] | |
| Jordan | 2.5–6.10 | [17,18,27] | |
| India | 0.8–2.31 | [18,23,28] | |
| South America | Argentina | 2.7–3.0 | [18,23] |
| Brazil | 2.94–3.3 | [17,18,29] | |
| Ecuador | 2.09–2.1 | [18,30] | |
| Africa | Ethiopia | 1.1–1.8 | [18,31,32] |
| Egypt | 0.7–1.7 | [18,19,33] | |
| Sudan | 0.38–0.9 | [18,34,35] | |
| Morocco | 0.4–0.7 | [18,36] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Janik-Karpinska, E.; Brancaleoni, R.; Niemcewicz, M.; Wojtas, W.; Foco, M.; Podogrocki, M.; Bijak, M. Healthcare Waste—A Serious Problem for Global Health. Healthcare 2023, 11, 242. https://doi.org/10.3390/healthcare11020242
Janik-Karpinska E, Brancaleoni R, Niemcewicz M, Wojtas W, Foco M, Podogrocki M, Bijak M. Healthcare Waste—A Serious Problem for Global Health. Healthcare. 2023; 11(2):242. https://doi.org/10.3390/healthcare11020242
Chicago/Turabian StyleJanik-Karpinska, Edyta, Rachele Brancaleoni, Marcin Niemcewicz, Wiktor Wojtas, Maurizio Foco, Marcin Podogrocki, and Michal Bijak. 2023. "Healthcare Waste—A Serious Problem for Global Health" Healthcare 11, no. 2: 242. https://doi.org/10.3390/healthcare11020242
APA StyleJanik-Karpinska, E., Brancaleoni, R., Niemcewicz, M., Wojtas, W., Foco, M., Podogrocki, M., & Bijak, M. (2023). Healthcare Waste—A Serious Problem for Global Health. Healthcare, 11(2), 242. https://doi.org/10.3390/healthcare11020242






