Effect of the Active Aging-in-Place–Rehabilitation Nursing Program: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
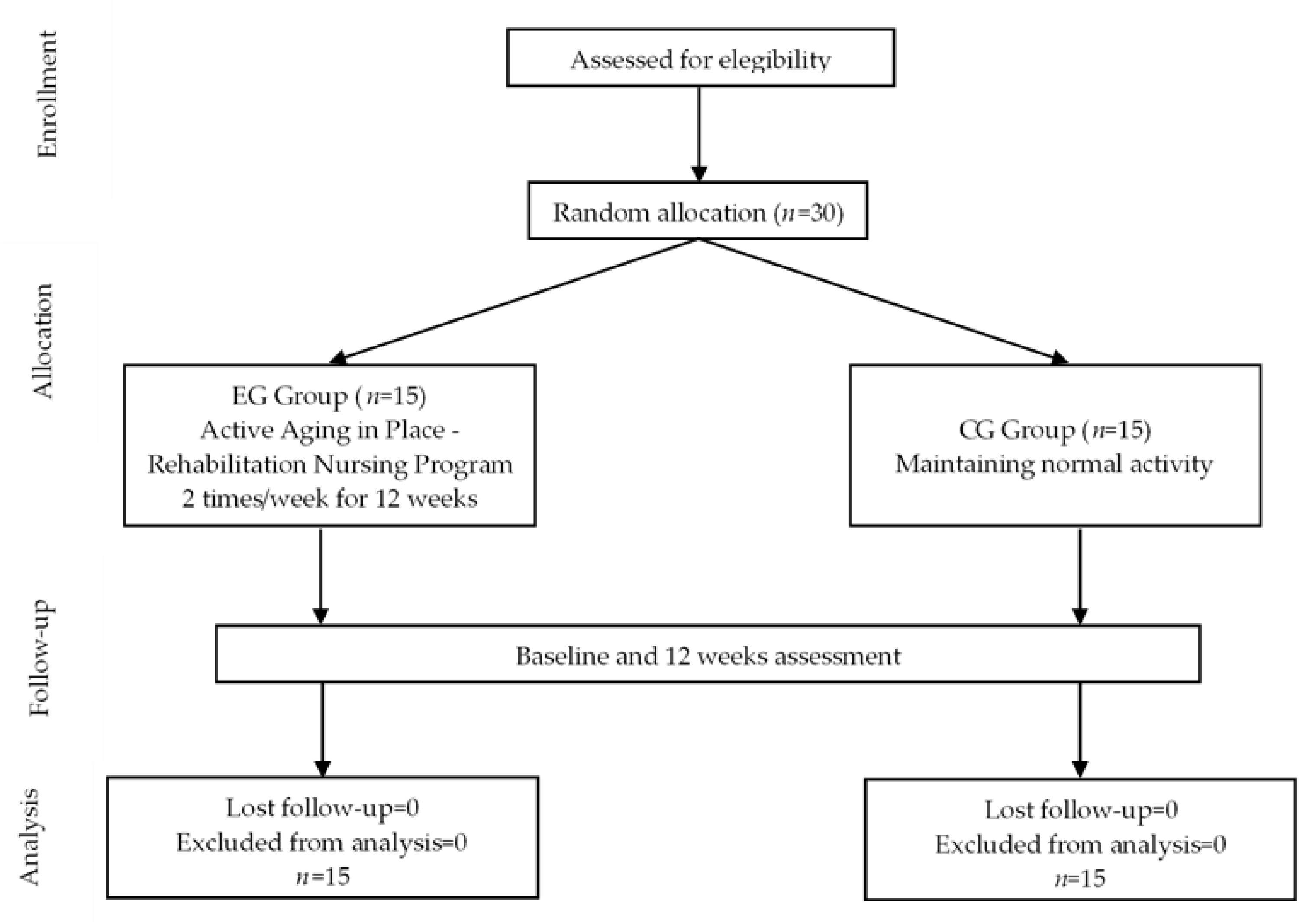
2.1. Study Design, Setting and Sample
2.2. Evaluation and Variables
- Frailty: We assessed multidimensional frailty using the TFI [33]. The TFI is a questionnaire that integrates 3 components (physical, psychological, and social) and is divided into 2 parts: the first part, where the determinants of frailty are recorded, and the second, which is composed of 15 questions divided into 3 components. All items in the second part are rated between 0 and 1, and the cut-off score of frailty was 6. We assessed physical frailty using Fried’s phenotype [35]. We can consider an individual frail if he/she has three or more of the criteria defined in Fried’s phenotype, i.e., 0 points, no frailty; 1 to 2 points, pre-frailty; and 3 to 5 points, frail.
- Functional Capacity: We used several tests to determine older adults’ functional capacity. The Barthel Index is a questionnaire that assesses dependence in basic activities of daily living (BADL) [34]. It is composed of 10 questions, and the higher the score, which is a maximum of 100 points, the greater the functional independence of the older adult. The Lawton Index assesses dependence on instrumental activities of daily living (IADL) and consists of 8 questions [36]. The score ranges from 0 to 16, and the cut-off points are: 0 to 5, severe or total dependence; 6 to 11, moderate dependence; and 12 to 16, mild dependence or independence. Functional fitness was assessed using Rikli and Jones’ Senior Fitness Test (SFT), a validated test battery for older adults that incorporates the following tests: the chair stand test, counting the number of repetitions in 30 s; the arm-curl test with dumbbells, counting the number of repetitions in 30 s; the back-scratch test, measured in cm; the chair sit-and-reach test, measured in cm; and the timed up-and-go test, recording the time in seconds [37]. For the first five SFT tests, a higher value indicates better performance, while for the last test, lower values indicate better performance. We measured handgrip strength, a predictor of functional capacity in older adults and incorporated in Fried’s phenotype, using a universal hydraulic dynamometer in the dominant hand, choosing the best result from three trials.
- Balance: We evaluated this parameter using the unipedal balance test and Tinetti’s Index [38]. The Tinetti Index is composed of 16 items, 9 for balance and 7 for gait. The scores range from 0 to 28 points, with low values being associated with decreased balance capacity and an increased risk of falling. A score > 24 points indicates a low fall risk; a score of 19 to 24 points indicates a moderate fall risk; and a score < 19 indicates a high fall risk.
- Subjective perception of effort was assessed using the Borg scale, which ranges from 0 to 10, with 10 representing maximal effort [39].
- Lifestyle: We assessed the lifestyle profiles of older people using the Individual Lifestyle Profile (ILP) scale, which is composed of 15 questions subdivided into 5 components, namely: nutrition; physical activity; preventive behavior; relational behavior; and stress control [40]. For each component, the interpretation follows the same logic, but it is suggested to classify the sum of the three questions in each component as follows: up to 3, negative profile; 4 to 6, intermediate (can improve); and 7 to 9, positive profile. The lower the score, the greater the need for behavioral change.
2.3. Ethical Procedures
2.4. Intervention
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Manfredi, G.; Midão, L.; Paúl, C.; Cena, C.; Duarte, M.; Costa, E. Prevalence of frailty status among the European elderly population: Findings from the Survey of Health, Aging and Retirement in Europe. Geriatr. Gerontol. Int. 2019, 19, 723–729. [Google Scholar] [CrossRef]
- Siriwardhana, D.D.; Hardoon, S.; Rait, G.; Weerasinghe, M.C.; Walters, K.R. Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: A systematic review and meta-analysis. BMJ Open 2018, 8, e018195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005, 173, 489–495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gobbens, R.J.; Luijkx, K.G.; Wijnen-Sponselee, M.T.; Schols, J.M. Toward a conceptual definition of frail community dwelling older people. Nurs. Outlook 2010, 58, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Sun, F.; Tang, Z. Social Frailty Is Associated with Physical Functioning, Cognition, and Depression, and Predicts Mortality. J. Nutr. Health Aging 2018, 22, 989–995. [Google Scholar] [CrossRef]
- Makizako, H.; Shimada, H.; Tsutsumimoto, K.; Lee, S.; Doi, T.; Nakakubo, S.; Hotta, R.; Suzuki, T. Social Frailty in Community-Dwelling Older Adults as a Risk Factor for Disability. J. Am. Med. Dir. Assoc. 2015, 16, 1003.e7–1003.e11. [Google Scholar] [CrossRef]
- Mehrabi, F.; Béland, F. Effects of social isolation, loneliness and frailty on health outcomes and their possible mediators and moderators in community-dwelling older adults: A scoping review. Arch. Gerontol. Geriatr. 2020, 90, 104119. [Google Scholar] [CrossRef] [PubMed]
- Cano, A.; Dargent, G.; Carriazo, A.; López-Samaniego, L.; Apostolo, J.; Campos, E.; Holland, C.; Varela-Nieto, I.; Sánchez-Sánchez, M.L.; Illario, M.; et al. Tackling frailty and functional decline: Background of the action group A3 of the European innovation partnership for active and healthy ageing. Maturitas 2018, 115, 69–73. [Google Scholar] [CrossRef] [Green Version]
- de Souza, L.F.; Canever, J.B.; Moreira, B.D.S.; Danielewicz, A.L.; de Avelar, N.C.P. Association Between Fear of Falling and Frailty in Community-Dwelling Older Adults: A Systematic Review. Clin. Interv. Aging 2022, 17, 129–140. [Google Scholar] [CrossRef]
- Apóstolo, J.; Cooke, R.; Bobrowicz-Campos, E.; Santana, S.; Marcucci, M.; Cano, A.; Vollenbroek-Hutten, M.; Germini, F.; Holland, C. Predicting risk and outcomes for frail older adults: An umbrella review of frailty screening tools. JBI Database Syst. Rev. Implement. Rep. 2017, 15, 1154–1208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jadczak, A.D.; Makwana, N.; Luscombe-Marsh, N.; Visvanathan, R.; Schultz, T.J. Effectiveness of exercise interventions on physical function in community-dwelling frail older people: An umbrella review of systematic reviews. JBI Database Syst. Rev. Implement. Rep. 2018, 16, 752–775. [Google Scholar] [CrossRef] [PubMed]
- Weng, W.-H.; Cheng, Y.-H.; Yang, T.-H.; Lee, S.-J.; Yang, Y.-R.; Wang, R.-Y. Effects of strength exercises combined with other training on physical performance in frail older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2022, 102, 104757. [Google Scholar] [CrossRef]
- Arc-Chagnaud, C.; Millan, F.; Salvador-Pascual, A.; Correas, A.G.; Olaso-Gonzalez, G.; De la Rosa, A.; Carretero, A.; Gomez-Cabrera, M.C.; Viña, J. Reversal of age-associated frailty by controlled physical exercise: The pre-clinical and clinical evidences. Sports Med. Heal. Sci. 2019, 1, 33–39. [Google Scholar] [CrossRef]
- Li, P.-S.; Hsieh, C.-J.; Tallutondok, E.B.; Peng, H.-J. The Dose-Response Efficacy of Physical Training on Frailty Status and Physical Performance in Community-Dwelling Elderly: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Healthcare 2022, 10, 586. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, Y.; Du, S.; Wang, Q.; Xia, H.; Sun, R. Exercise interventions for improving physical function, daily living activities and quality of life in community-dwelling frail older adults: A systematic review and meta-analysis of randomized controlled trials. Geriatr. Nurs. 2020, 41, 261–273. [Google Scholar] [CrossRef]
- Racey, M.; Ali, M.U.; Sherifali, D.; Fitzpatrick-Lewis, D.; Lewis, R.; Jovkovic, M.; Bouchard, D.R.; Giguère, A.; Holroyd-Leduc, J.; Tang, A.; et al. Effectiveness of physical activity interventions in older adults with frailty or prefrailty: A systematic review and meta-analysis. CMAJ Open 2021, 9, E728–E743. [Google Scholar] [CrossRef]
- Franco, M.R.; Tong, A.; Howard, K.; Sherrington, C.; Ferreira, P.H.; Pinto, R.Z.; Ferreira, M.L. Older people’s perspectives on participation in physical activity: A systematic review and thematic synthesis of qualitative literature. Br. J. Sports Med. 2015, 49, 1268–1276. [Google Scholar] [CrossRef]
- Moran, M.; Van Cauwenberg, J.; Hercky-Linnewiel, R.; Cerin, E.; Deforche, B.; Plaut, P. Understanding the relationships between the physical environment and physical activity in older adults: A systematic review of qualitative studies. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 79. [Google Scholar] [CrossRef] [Green Version]
- Moschny, A.; Platen, P.; Klaassen-Mielke, R.; Trampisch, U.; Hinrichs, T. Barriers to physical activity in older adults in Germany: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 121. [Google Scholar] [CrossRef]
- Burton, E.; Farrier, K.; Lewin, G.; Pettigrew, S.; Hill, A.-M.; Airey, P.; Bainbridge, L.; Hill, K.D. Motivators and Barriers for Older People Participating in Resistance Training: A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2017, 25, 311–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boulton, E.; Weber, M.; Hawley-Hague, H.; Bergquist, R.; Van Ancum, J.; Jonkman, N.H.; Taraldsen, K.; Helbostad, J.L.; Maier, A.B.; Becker, C.; et al. Attitudes Towards Adapted Lifestyle-Integrated Functional Exercise Developed for 60–70-Year-Olds: Perceptions of Participants and Trainers. Gerontology 2019, 65, 599–609. [Google Scholar] [CrossRef] [PubMed]
- Schwenk, M.; Bergquist, R.; Boulton, E.; Van Ancum, J.M.; Nerz, C.; Weber, M.; Barz, C.; Jonkman, N.H.; Taraldsen, K.; Helbostad, J.L.; et al. The Adapted Lifestyle-Integrated Functional Exercise Program for Preventing Functional Decline in Young Seniors: Development and Initial Evaluation. Gerontology 2019, 65, 362–374. [Google Scholar] [CrossRef]
- Weber, M.; Belala, N.; Clemson, L.; Boulton, E.; Hawley-Hague, H.; Becker, C.; Schwenk, M. Feasibility and effectiveness of intervention programmes integrating functional exercise into daily life of older adults: A systematic review. Gerontology 2018, 64, 172–187. [Google Scholar] [CrossRef] [PubMed]
- Suikkanen, S.; Soukkio, P.; Aartolahti, E.; Kääriä, S.; Kautiainen, H.; Hupli, M.T.; Pitkälä, K.; Sipilä, S.; Kukkonen-Harjula, K. Effect of 12-Month Supervised, Home-Based Physical Exercise on Functioning Among Persons With Signs of Frailty: A Randomized Controlled Trial. Arch. Phys. Med. Rehabilit. 2021, 102, 2283–2290. [Google Scholar] [CrossRef]
- Schwarzer, R.; Hamilton, K. Changing behavior using the health action process approach. In The Handbook of Behavior Change; Cambridge University Press: Cambridge, UK, 2020; pp. 89–103. [Google Scholar] [CrossRef]
- Pender, N.; Murdaugh, C.; Parsons, M. Health Promotion in Nursing Practice, 8th ed.; Pearson/Prentice-Hall: Upper Saddle River, NJ, USA, 2019. [Google Scholar]
- Gourlan, M.; Bernard, P.; Bortolon, C.; Romain, A.J.; Lareyre, O.; Carayol, M.; Ninot, G.; Boiché, J. Efficacy of theory-based interventions to promote physical activity. A meta-analysis of randomised controlled trials. Health Psychol. Rev. 2016, 10, 50–66. [Google Scholar] [CrossRef]
- French, D.P.; Olander, E.K.; Chisholm, A.; Mc Sharry, J. Which Behaviour Change Techniques Are Most Effective at Increasing Older Adults’ Self-Efficacy and Physical Activity Behaviour? A Systematic Review. Ann. Behav. Med. 2014, 48, 225–234. [Google Scholar] [CrossRef] [Green Version]
- Bárrios, M.J.; Marques, R.; Fernandes, A.A. Aging with health: Aging in place strategies of a Portuguese population aged 65 years or older. Rev. de Saude Publ. 2020, 54, 129. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; CONSORT Group. WITHDRAWN: CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2010, 152, 726–732. [Google Scholar] [CrossRef]
- Faria, A.d.C.A.; Martins, M.M.F.P.S.; Ribeiro, O.M.P.L.; Ventura-Silva, J.M.A.; Fonseca, E.F.; Ferreira, L.J.M.; Teles, P.J.F.C.; Laredo-Aguilera, J.A. Multidimensional Frailty and Lifestyles of Community-Dwelling Older Portuguese Adults. Int. J. Environ. Res. Public Health 2022, 19, 14723. [Google Scholar] [CrossRef]
- Coelho, T.; Santos, R.; Paúl, M.C.; Gobbens, R.J.; Fernandes, L. Portuguese version of the Tilburg Frailty Indicator: Transcultural adaptation and psychometric validation. Geriatr. Gerontol. Int. 2015, 15, 951–960. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sequeira, C.A.C. Cuidar de Idosos Dependentes, 1st ed.; Quarteto: Coimbra, Portugal, 2007. [Google Scholar]
- Duarte, M. Fragilidade em Idosos: Modelos, Medidas e Implicações Práticas; Coisas de Ler: Lisboa, Portugal, 2015; pp. 1–163. [Google Scholar]
- Azeredo, Z.; Matos, E. Grau de dependência em doentes que sofreram AVC. Rev. Facul. Med. Lisboa 2003, 8, 199–204. [Google Scholar]
- Baptista, F.; Sardinha, L. Avaliação de Aptidão Física e do Equilíbrio de Pessoas Idosas: Baterias de Fullerton; Faculdade de Motricidade Humana: Lisboa, Portugal, 2005; pp. 1–15. [Google Scholar]
- Petiz, E.M. A Actividade Física, Equilíbrio e Quedas. um Estudo em Idosos Institucionalizados. Unpublished Master’s Thesis, Faculdade de Ciências do Desporto e de Educação Física da Universidade do Porto, Porto, Portugal, 2002. [Google Scholar]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Both, J.; Borgatto, A.F.; do Nascimento, J.V.; Sonoo, C.N.; Lemos, C.A.F.; Nahas, M.V. Validação da escala perfil do estilo de vida individual. Rev. Bras. Ativ. Física Saúde 2008, 13, 5–14. [Google Scholar]
- Martins, A.C.; Santos, C.; Silva, C.; Baltazar, D.; Moreira, J.; Tavares, N. Does modified Otago Exercise Program improves balance in older people? A systematic review. Prev. Med. Rep. 2018, 11, 231–239. [Google Scholar] [CrossRef]
- Clemson, L.; Munro, J.; Singh, M.F. Lifestyle-Integrated Functional Exercise (LiFE) Program to Prevent Falls: Trainer’s Manual; Sydney University Press: Sydney, Australia, 2014. [Google Scholar]
- Chiu, T.-Y.; Yu, H.-W. Associations of multicomponent exercise and aspects of physical performance with frailty trajectory in older adults. BMC Geriatr. 2022, 22, 559. [Google Scholar] [CrossRef]
- Mulasso, A.; Roppolo, M.; Rainoldi, A.; Rabaglietti, E. Effects of a Multicomponent Exercise Program on Prevalence and Severity of the Frailty Syndrome in a Sample of Italian Community-Dwelling Older Adults. Healthcare 2022, 10, 911. [Google Scholar] [CrossRef]
- Ng, T.P.; Feng, L.; Nyunt, M.S.Z.; Feng, L.; Niti, M.; Tan, B.Y.; Chan, G.; Khoo, S.A.; Chan, S.M.; Yap, P.; et al. Nutritional, Physical, Cognitive, and Combination Interventions and Frailty Reversal Among Older Adults: A Randomized Controlled Trial. Am. J. Med. 2015, 128, 1225–1236.e1. [Google Scholar] [CrossRef] [Green Version]
- Cesari, M.; Vellas, B.; Hsu, F.-C.; Newman, A.B.; Doss, H.; King, A.C.; Manini, T.M.; Church, T.; Gill, T.M.; Miller, M.E.; et al. A physical activity intervention to treat the frailty syndrome in older persons-results from the LIFE-P study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2015, 70, 216–222. [Google Scholar] [CrossRef]
- Oliveira, J.S.; Pinheiro, M.B.; Fairhall, N.; Walsh, S.; Franks, T.C.; Kwok, W.; Bauman, A.; Sherrington, C. Evidence on physical activity and the prevention of frailty and sarcopenia among older people: A systematic review to inform the world health organization physical activity guidelines. J. Phys. Act. Health 2020, 17, 1247–1258. [Google Scholar] [CrossRef]
- Rogers, N.T.; Marshall, A.; Roberts, C.H.; Demakakos, P.; Steptoe, A.; Scholes, S. Physical activity and trajectories of frailty among older adults: Evidence from the English Longitudinal Study of Ageing. PLoS ONE 2017, 12, e0170878. [Google Scholar] [CrossRef] [PubMed]
- Souza, D.D.S.; Berlese, D.B.; Da Cunha, G.L.; Cabral, S.M.; Dos Santos, G.A. Análise da relação do suporte social e da síndrome de fragilidade em idosos. Psicol Saúde Doenças 2017, 18, 420–433. [Google Scholar] [CrossRef]
- Faller, J.W.; Pereira, D.D.N.; De Souza, S.; Nampo, F.K.; Orlandi, F.D.S.; Matumoto, S. Instruments for the detection of frailty syndrome in older adults: A systematic review. PLoS ONE 2019, 14, e0216166. [Google Scholar] [CrossRef] [Green Version]
- Rivas-Ruiz, F.; Machón, M.; Contreras-Fernández, E.; Vrotsou, K.; Padilla-Ruiz, M.; Ruiz, A.I.D.; Berenguer, Y.d.M.; Vergara, I.; Group GIFEA. Prevalence of frailty among community-dwelling elderly persons in Spain and factors associated with it. Eur. J. Gen. Pract. 2019, 25, 190–196. [Google Scholar] [CrossRef]
- Jung, H.; Kim, M.; Lee, Y.; Won, C.W. Prevalence of Physical Frailty and Its Multidimensional Risk Factors in Korean Community-Dwelling Older Adults: Findings from Korean Frailty and Aging Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 7883. [Google Scholar] [CrossRef]
- Blanco-Reina, E.; Aguilar-Cano, L.; García-Merino, M.R.; Ocaña-Riola, R.; Valdellós, J.; Bellido-Estévez, I.; Ariza-Zafra, G. Assessing Prevalence and Factors Related to Frailty in Community-Dwelling Older Adults: A Multinomial Logistic Analysis. J. Clin. Med. 2021, 10, 3576. [Google Scholar] [CrossRef]
- Zhang, X.; Tan, S.S.; Franse, C.B.; Bilajac, L.; Alhambra-Borrás, T.; Garcés-Ferrer, J.; Verma, A.; Williams, G.; Clough, G.; Koppelaar, E.; et al. Longitudinal Association Between Physical Activity and Frailty Among Community-Dwelling Older Adults. J. Am. Geriatr. Soc. 2020, 68, 1484–1493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tarazona-Santabalbina, F.J.; Gómez-Cabrera, M.C.; Pérez-Ros, P.; Martínez-Arnau, F.M.; Cabo, H.; Tsaparas, K.; Salvador-Pascual, A.; Rodriguez-Mañas, L.; Viña, J. A multicomponent exercise intervention that reverses frailty and improves cognition, emotion, and social networking in the community-dwelling frail elderly: A randomized clinical trial. J. Am. Med. Dir. Assoc. 2016, 17, 426–433. [Google Scholar] [CrossRef] [Green Version]
- Cadore, E.L.; de Asteasu, M.L.S.; Izquierdo, M. Multicomponent exercise and the hallmarks of frailty: Considerations on cognitive impairment and acute hospitalization. Exp. Gerontol. 2019, 122, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Casas-Herrero, Á.; de Asteasu, M.L.S.; Antón-Rodrigo, I.; Sánchez-Sánchez, J.L.; Montero-Odasso, M.; Marín-Epelde, I.; Ramón-Espinoza, F.; Zambom-Ferraresi, F.; Petidier-Torregrosa, R.; Elexpuru-Estomba, J.; et al. Effects of Vivifrail multicomponent intervention on functional capacity: A multicentre, randomized controlled trial. J. Cachex. Sarcopenia Muscle 2022, 13, 884–893. [Google Scholar] [CrossRef]
- Bohannon, R.W. Grip Strength: An Indispensable Biomarker For Older Adults. Clin. Interv. Aging 2019, 14, 1681–1691. [Google Scholar] [CrossRef] [PubMed]
- Forrest, K.Y.Z.; Williams, A.M.; Leeds, M.J.; Robare, J.F.; Bechard, T.J. Patterns and correlates of grip strength in older Americans. Curr. Aging Sci. 2018, 11, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Iconaru, E.I.; Ciucurel, M.M.; Georgescu, L.; Ciucurel, C. Hand grip strength as a physical biomarker of aging from the perspective of a Fibonacci mathematical modeling. BMC Geriatr. 2018, 18, 296. [Google Scholar] [CrossRef] [PubMed]
- Sayer, A.A.; Kirkwood, T.B.L. Grip strength and mortality: A biomarker of ageing? Lancet 2015, 386, 226–227. [Google Scholar] [CrossRef]
- Haider, S.; Dorner, T.E.; Luger, E.; Kapan, A.; Titze, S.; Lackinger, C.; Schindler, K.E. Impact of a Home-Based Physical and Nutritional Intervention Program Conducted by Lay-Volunteers on Handgrip Strength in Prefrail and Frail Older Adults: A Randomized Control Trial. PLoS ONE 2017, 12, e0169613. [Google Scholar] [CrossRef] [PubMed]
- Buch, A.; Kis, O.; Carmeli, E.; Keinan-Boker, L.; Berner, Y.; Barer, Y.; Shefer, G.; Marcus, Y.; Stern, N. Circuit resistance training is an effective means to enhance muscle strength in older and middle aged adults: A systematic review and meta-analysis. Ageing Res. Rev. 2017, 37, 16–27. [Google Scholar] [CrossRef]
- Lai, X.; Bo, L.; Zhu, H.; Chen, B.; Wu, Z.; Du, H.; Huo, X. Effects of lower limb resistance exercise on muscle strength, physical fitness, and metabolism in pre-frail elderly patients: A randomized controlled trial. BMC Geriatr. 2021, 21, 447. [Google Scholar] [CrossRef]
- Sobrinho, A.C.d.S.; Almeida, M.L.d.; Rodrigues, G.d.S.; Bertani, R.F.; Lima, J.G.R.; Junior, C.R.B. Stretching and Multicomponent Training to Functional Capacities of Older Women: A Randomized Study. Int. J. Environ. Res. Public Health 2022, 19, 27. [Google Scholar] [CrossRef]
- Carneiro, N.H.; Ribeiro, A.S.; Nascimento, M.A.; Gobbo, L.A.; Schoenfeld, B.J.; Júnior, A.A.; Gobbi, S.; Oliveira, A.R.; Cyrino, E.S. Effects of different resistance training frequencies on flexibility in older women. Clin. Interv. Aging 2015, 10, 531–538. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Gao, Y.; Hu, S.; Chen, H.; Zhang, M.; Yang, Y.; Liu, Y. Effects of multicomponent exercise on the muscle strength, muscle endurance and balance of frail older adults: A meta-analysis of randomised controlled trials. J. Clin. Nurs. 2022, 1–11. [Google Scholar] [CrossRef]
- Wakida, M.; Asai, T.; Kubota, R.; Kuwabara, T.; Fukumoto, Y.; Sato, H.; Nakano, J.; Mori, K.; Ikezoe, T.; Hase, K. Longitudinal effects of physical exercise on health-related outcomes based on frailty status in community-dwelling older adults. Geriatr. Gerontol. Int. 2022, 22, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Perez-Sousa, M.A.; Venegas-Sanabria, L.C.; Chavarro-Carvajal, D.A.; Cano-Gutierrez, C.A.; Izquierdo, M.; Correa-Bautista, J.E.; Ramírez-Vélez, R. Gait speed as a mediator of the effect of sarcopenia on dependency in activities of daily living. J. Cachex. Sarcopenia Muscle 2019, 10, 1009–1015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fain, R.S.; Hayat, S.A.; Luben, R.; Pari, A.A.; Yip, J.L.Y. Effects of social participation and physical activity on all-cause mortality among older adults in Norfolk, England: An investigation of the EPIC-Norfolk study. Public Health 2022, 202, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Bacanoiu, M.V.; Danoiu, M. New Strategies to Improve the Quality of Life for Normal Aging versus Pathological Aging. J. Clin. Med. 2022, 11, 4207. [Google Scholar] [CrossRef] [PubMed]
| Variables | Main Exercises | Duration | Intensity | Frequency | Progression | ||
|---|---|---|---|---|---|---|---|
| 1st Month | 2nd Month | 3rd Month | |||||
| Warm-up exercises |
| 10 min | Mild | Twice a week |
| ||
| Aerobic Endurance Training |
| 5 min | Mild (up to 4) to moderate (5–6) on a Borg rating scale of perceived exertion (0–10) | Twice a week | Longer distance and more unstable/irregular walking surface, with change of pace and direction | Climb up and down stairs, progressing according to the person’s tolerance | |
| Strength Training |
| 10 min | Mild-to-moderate | Twice a week | 2 sets of each exercise with 10 repetitions without load | 3 sets of each exercise with 12 repetitions with load adapted to each patient (40 to 50% of 1 RM) | 3 sets of each exercise with 15 repetitions with load adapted to each patient (60 to 70% of 1 RM) |
| Flexibility Training/ Workout |
| 5 min | Mild | Twice a week | Increase the range of motion | ||
| Balance and coordination training |
| 10 min | Moderate | Twice a week |
|
|
|
| ADL Training |
| 15 min | Moderate | Twice a week | Move on to more challenging tasks combined with strength, balance, coordination, and flexibility training, performing complex movements such as pronation/supination, cubital/radial deviation of the wrist, and fine motor skills by training thumb opposability, grip, and reach | ||
| Relaxing and stretching exercises |
| 5 min | Mild | Twice a week |
| ||
| Individual Counseling |
| ||||||
| Variables | EG | CG |
|---|---|---|
| Gender n; % Female Male | 11 (73.33%) 4 (26.67%) | 10 (66.67%) 5 (33.33%) |
| Age (Mean ± Std. Deviation) | 80.07 ± 4.91 | 81.8 ± 5 |
| Education (years) (Mean ± Std. Deviation) | 3.13 ± 0.92 | 2.067 ± 1.87 |
| Marital status n; % Married Widow(er) Single | 4 (26.70%) 11 (73.30%) 0 (0%) | 6 (40%) 8 (53.33%) 1(6.67%) |
| N.º. of household members (Mean ± Std. Deviation) | 2 ± 0.535 | 2.87 ± 1.41 |
| Nº of diseases (Mean ± Std. Deviation) | 4.75 ± 1.49 | 4.13 ± 1.92 |
| N.º. of daily medications/drugs (Mean ± Std. Deviation) | 6.42 ± 1.78 | 6.2 ± 2.11 |
| Variables | Baseline (Mean ± Std. Deviation) | Post-Program (Mean ± Std. Deviation) | z | p | |
|---|---|---|---|---|---|
| Multidimensional Frailty | Physical frailty (EG) | 6.27 ± 0.88 | 5.00 ± 2.27 | −2.39 | 0.017 |
| Physical frailty (CG) | 6.0 ± 1.69 | 6.07 ± 1.34 | −0.38 | 0.705 | |
| Psychological frailty (EG) | 3.53 ± 0.52 | 2.4 ± 1.18 | −2.89 | 0.004 | |
| Psychological frailty (CG) | 2.87 ± 1.06 | 3.13 ± 0.99 | −1.63 | 0.102 | |
| Social frailty (EG) | 1.6 ± 0.74 | 0.8 ± 0.78 | −3.46 | 0.001 | |
| Social frailty (CG) | 0.93 ± 0.89 | 1.07 ± 0.88 | −1.00 | 0.317 | |
| Total frailty (EG) | 11.4 ± 1.35 | 8.2 ± 3.43 | −3.19 | 0.001 | |
| Total frailty (CG) | 9.8 ± 3.03 | 10.27 ± 2.60 | −1.27 | 0.206 | |
| Physical frailty | Fried Frailty Phenotype Criteria (EG) | 3.07 ± 0.26 | 2.8 ± 0.56 | −2.00 | 0.046 |
| Fried Frailty Phenotype Criteria (CG) | 3.133 ± 0.35 | 3.133 ± 0.35 | 0 | 1 | |
| Variables | Baseline (Mean ± Std. Deviation) | Post-Program (Mean ± Std. Deviation) | z | p | |
|---|---|---|---|---|---|
| Functional Fitness | Chair stand test (EG) | 12.27 ± 3.59 | 15.00 ± 3.46 | −3.43 | 0.001 |
| Chair stand test (CG) | 11.53 ± 2.20 | 10.93 ± 1.39 | −1.78 | 0.075 | |
| Arm-curl test (EG) | 14.2 ± 2.14 | 17.77 ± 2.10 | −3.44 | <0.001 | |
| Arm-curl test (CG) | 13.53 ± 1.88 | 12.93 ± 1.34 | −2.08 | 0.037 | |
| Back scratch test (EG) | −37.73 ± 11.29 | −32.27 ± 13.02 | −2.79 | 0.005 | |
| Back scratch test (CG) | −39.07 ± 9.63 | −38.33 ± 10.27 | −1.21 | 0.228 | |
| Chair sit-and-reach test (EG) | −12.2 ± 7.58 | −8.33 ± 7.68 | −3.43 | 0.001 | |
| Chair sit-and-reach test (CG) | −10.07 ± 11.51 | −13.87 ± 5.69 | −0.73 | 0.465 | |
| Timed up-and-go test (EG) | 18.833 ± 3.68 | 15.657 ± 4.12 | −2.92 | 0.004 | |
| Timed up-and-go test (CG) | 19.133 ± 2.92 | 20.00 ± 2.92 | −2.38 | 0.018 | |
| Grip strength | Handgrip strength (EG) | 14.087 ± 4.49 | 17.693 ± 6.07 | −3.41 | <0.001 |
| Handgrip strength (CG) | 11.867 ± 2.10 | 11.5 ± 2.163 | −1.84 | 0.066 | |
| Dependence in BADL | Barthel Index (EG) | 77 ± 7.973 | 80.00 ± 9.45 | −2.71 | 0.007 |
| Barthel Index (CG) | 72.67 ± 7.528 | 71 ± 8.062 | −1.63 | 0.102 | |
| Dependence in IADL | Lawton Scale (EG) | 9.73 ± 1.033 | 10 ± 1 | −1.41 | 0.157 |
| Lawton Scale (CG) | 11.93 ± 2.815 | 11.8 ± 2.859 | −1.41 | 0.157 | |
| Balance | Single-leg balance (EG) | 3.8 ± 1.26 | 5.2 ± 1.612 | −3.31 | <0.001 |
| Single-leg balance (CG) | 3.5 ± 0.9636 | 3.267 ± 0.753 | −1.89 | 0.059 | |
| Tinetti Index (EG) | 17.87 ± 2.588 | 18.93 ± 2.52 | −2.32 | 0.020 | |
| Tinetti Index (CG) | 16.53 ± 4.103 | 16 ± 3.854 | −2.12 | 0.034 | |
| Subjective perception of effort | Borg Scale (EG) | 6.73 ± 1.033 | 5.53 ± 1.125 | −3.63 | <0.001 |
| Borg Scale (CG) | 6.07 ± 0.704 | 6 ± 0.756 | −1 | 0.317 | |
| Variables | Baseline (Mean ± Std. Deviation) | Post-Program (Mean ± Std. Deviation) | z | p | |
|---|---|---|---|---|---|
| Dimensions of the Individual Lifestyle Profile (ILP) | Relational behavior (EG) | 0.67 ± 0.724 | 4.53 ± 1.457 | −3.45 | 0.001 |
| Relational behavior (CG) | 1.6 ± 1.549 | 1.53 ± 1.506 | −1.00 | 0.317 | |
| Physical activity (EG) | 0.13 ± 0.352 | 3.73 ± 1.4.38 | −3.36 | 0.001 | |
| Physical activity (CG) | 1.33 ± 1.234 | 1.33 ± 1.234 | 0 | 1 | |
| Stress management (EG) | 5.07 ± 1.486 | 5.8 ± 1.320 | −3.05 | 0.002 | |
| Stress management (CG) | 3.87 ± 2.615 | 3.73 ± 2.52 | −1.41 | 0.157 | |
| Nutrition (EG) | 3.93 ± 1.100 | 4.27 ± 1.22 | −1.67 | 0.096 | |
| Nutrition (CG) | 5.4 ± 2.72 | 5.27 ± 2.549 | −3.42 | 0.001 | |
| Preventive behavior (EG) | 7.87 ± 1.06 | 7.87 ± 1.06 | 0.00 | 1 | |
| Preventive behavior (CG) | 6.4 ± 2.261 | 6.27 ± 2.219 | −1.00 | 0.317 | |
| Total ILP (EG) | 17.67 ± 3.13 | 26.8 ± 4.057 | −3.41 | <0.001 | |
| Total ILP (CG) | 17.27 ± 5.738 | 18.13 ± 5.693 | −1.93 | 0.053 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faria, A.d.C.A.; Martins, M.M.F.P.S.; Ribeiro, O.M.P.L.; Ventura-Silva, J.M.A.; Fonseca, E.F.; Ferreira, L.J.M.; Laredo-Aguilera, J.A. Effect of the Active Aging-in-Place–Rehabilitation Nursing Program: A Randomized Controlled Trial. Healthcare 2023, 11, 276. https://doi.org/10.3390/healthcare11020276
Faria AdCA, Martins MMFPS, Ribeiro OMPL, Ventura-Silva JMA, Fonseca EF, Ferreira LJM, Laredo-Aguilera JA. Effect of the Active Aging-in-Place–Rehabilitation Nursing Program: A Randomized Controlled Trial. Healthcare. 2023; 11(2):276. https://doi.org/10.3390/healthcare11020276
Chicago/Turabian StyleFaria, Ana da Conceição Alves, Maria Manuela F. P. S. Martins, Olga Maria Pimenta Lopes Ribeiro, João Miguel Almeida Ventura-Silva, Esmeralda Faria Fonseca, Luciano José Moreira Ferreira, and José Alberto Laredo-Aguilera. 2023. "Effect of the Active Aging-in-Place–Rehabilitation Nursing Program: A Randomized Controlled Trial" Healthcare 11, no. 2: 276. https://doi.org/10.3390/healthcare11020276
APA StyleFaria, A. d. C. A., Martins, M. M. F. P. S., Ribeiro, O. M. P. L., Ventura-Silva, J. M. A., Fonseca, E. F., Ferreira, L. J. M., & Laredo-Aguilera, J. A. (2023). Effect of the Active Aging-in-Place–Rehabilitation Nursing Program: A Randomized Controlled Trial. Healthcare, 11(2), 276. https://doi.org/10.3390/healthcare11020276








