Multiple Cesarean Section Outcomes and Complications: A Retrospective Study in Jazan, Saudi Arabia
Abstract
1. Introduction
2. Materials and Methods
2.1. Design Setting and Participants
2.2. Data Collection, Study Variables, and Their Definitions
2.3. Data Analysis
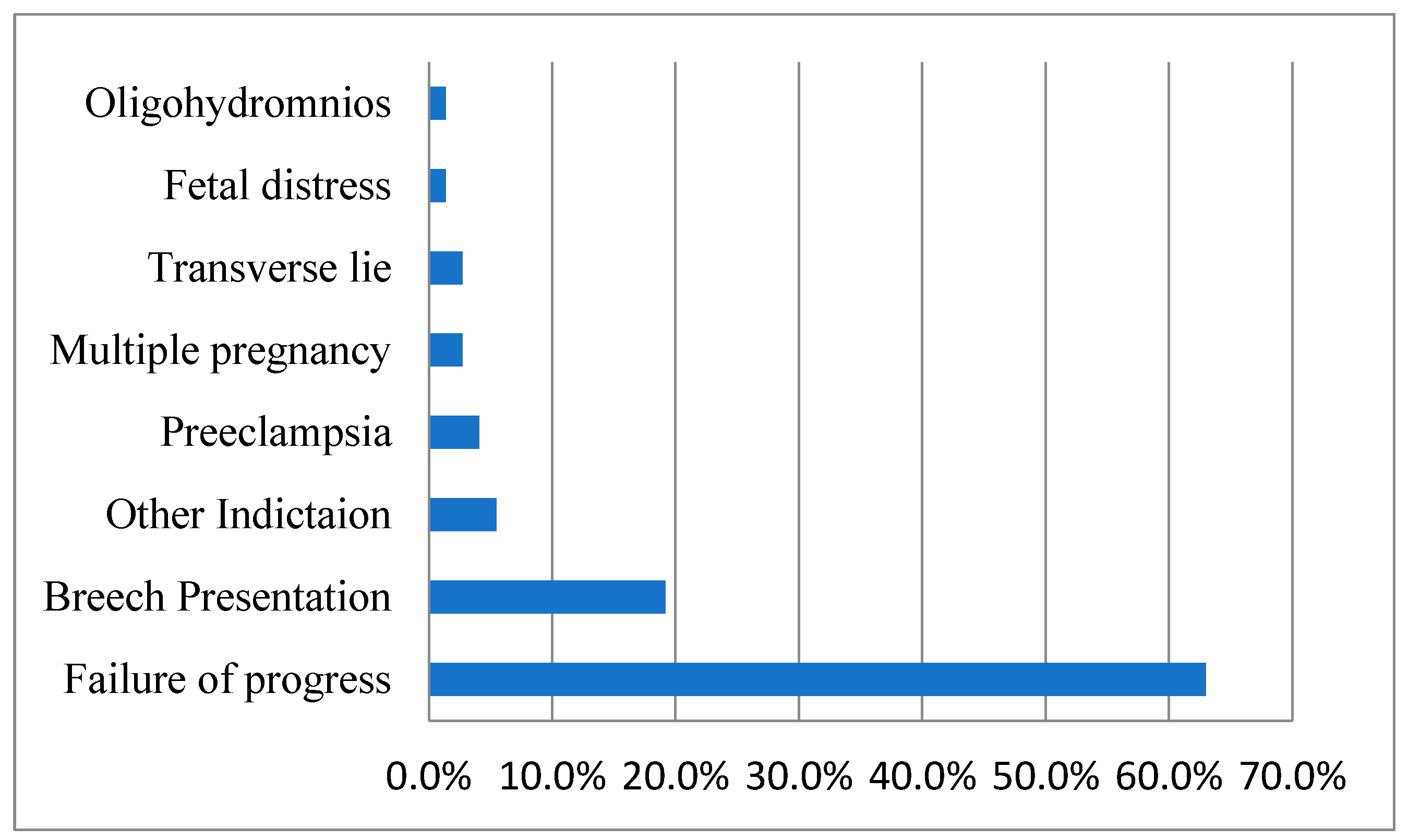
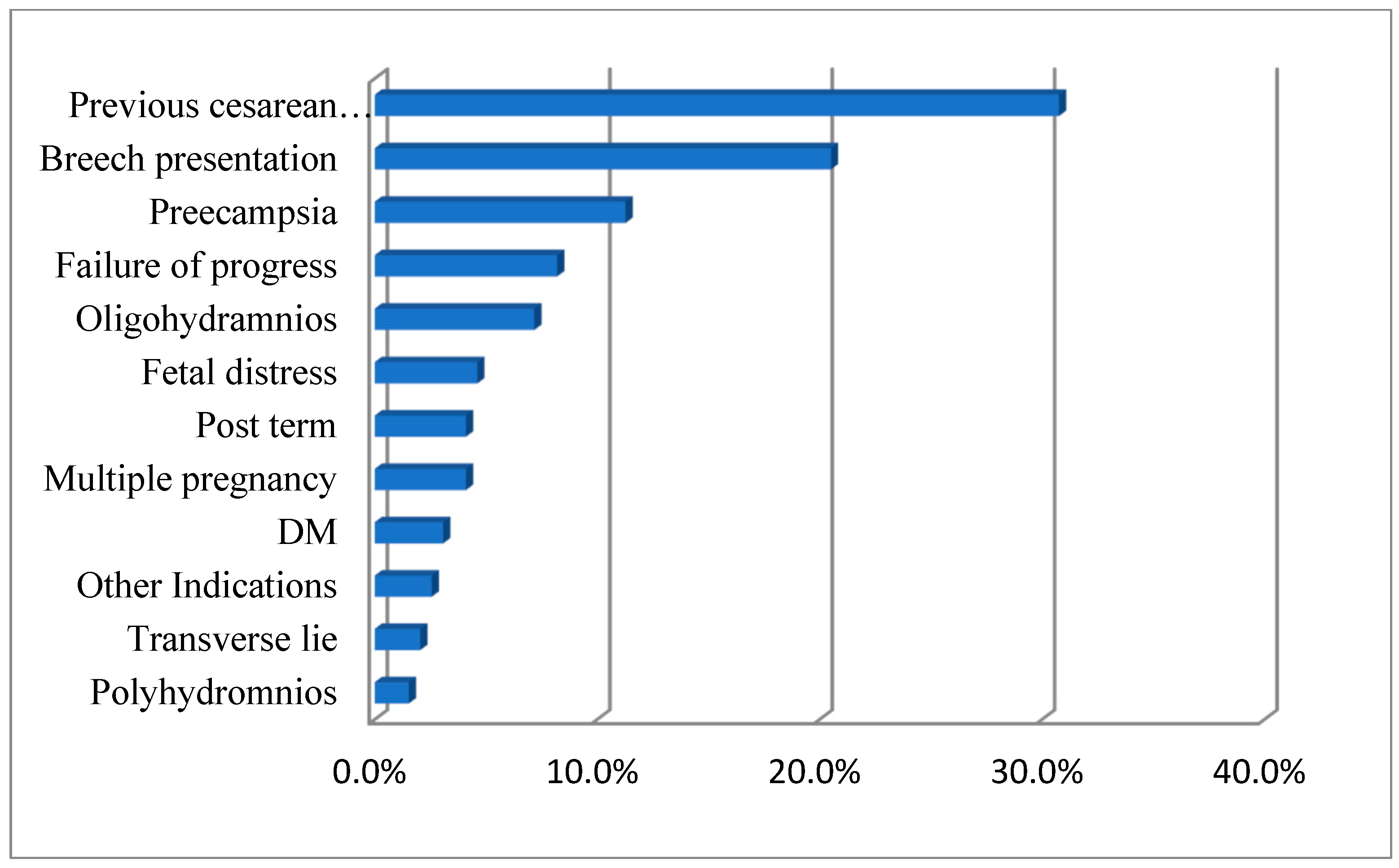
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| C/S | Caesarean section/cesarean section |
| P scar | Previous scar |
| HB | Hemoglobin |
| UTI | Urinary tract infection |
| APH | Ante partum hemorrhage |
| CD | Caesarean delivery |
| NICU | Neonatal Intensive Care Unit |
| DM | Diabetes mellitus |
| HPT | Hypertension |
| PROM | Premature rupture of membranes |
| ANC | Antenatal care |
| Fenestration | Small opening (window) in uterine muscles |
| Rectal muscle diastasis | Rectal muscles are separated |
| APGAR | Appearance, Pulse, Grimace, Activity, and Respiration (score 0, 1, or 2) |
References
- Yang, X.J.; Sun, S.S. Comparison of maternal and fetal complications in elective and emergency cesarean section: A systematic review and meta-analysis. Arch. Gynecol. Obstet. 2017, 296, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Arlier, S.; Seyfettinoğlu, S.; Yilmaz, E.; Nazik, H.; Adıgüzel, C.; Eskimez, E.; Hürriyetoğlu, Ş.; Yücel, O. Incidence of adhesions and maternal and neonatal morbidity after repeat cesarean section. Arch. Gynecol. Obstet. 2017, 295, 303–311. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Human Reproduction Programme. WHO statement on caesarean section rates. Reprod. Health Matters 2015, 23, 149–150. [Google Scholar] [CrossRef]
- Rochat, R.W.; Koonin, L.M.; Atrash, H.K.; Jewett, J.F. Maternal mortality in the United States: Report from the Maternal Mortality Collaborative. Obstet. Gynecol. 1988, 72, 91–97. [Google Scholar] [CrossRef]
- Gasim, T.; Al Jama, F.E.; Rahman, M.S.; Rahman, J. Multiple repeat cesarean sections: Operative difficulties, maternal complications and outcome. J. Reprod. Med. 2013, 58, 312–318. [Google Scholar]
- Guise, J.M.; Denman, M.A.; Emeis, C.; Marshall, N.; Walker, M.; Fu, R.; Janik, R.; Nygren, P.; Eden, K.B.; McDonagh, M. Vaginal birth after cesarean: New insights on maternal and neonatal outcomes. Obstet. Gynecol. 2010, 115, 1267–1278. [Google Scholar] [CrossRef] [PubMed]
- Al-Kadri, H.M.; Al-Anazi, S.A.; Tamim, H.M. Increased cesarean section rate in Central Saudi Arabia: A change in practice or different maternal characteristics. Int. J. Women’s Health 2015, 7, 685–692. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alsulami, S.M.; Ashmawi, M.T.; Jarwan, R.O.; Malli, I.A.; Albar, S.K.; Al-Jifree, H.M. The rates of cesarean section deliveries according to Robson Classification System during the year of 2018 among patients in King Abdul-Aziz Medical City, Jeddah, Saudi Arabia. Cureus 2020, 12, e11529. [Google Scholar] [CrossRef]
- Ba’aqeel, H.S. Cesarean delivery rates in Saudi Arabia: A ten-year review. Ann. Saudi Med. 2009, 29, 179–183. [Google Scholar] [CrossRef]
- Al Rowaily, M.A.; Alsalem, F.A.; Abolfotouh, M.A. Cesarean section in a high-parity community in Saudi Arabia: Clinical indications and obstetric outcomes. BMC Pregnancy Childbirth 2014, 14, 92. [Google Scholar] [CrossRef]
- Elnakib, S.; Abdel-Tawab, N.; Orbay, D.; Hassanein, N. Medical and non-medical reasons for cesarean section delivery in Egypt: A hospital-based retrospective study. BMC Pregnancy Childbirth 2019, 19, 411. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.M.; Namir, A.L. Rate and indications of cesarean section in the maternity teaching hospital in erbil city, kurdistan region, Iraq. Zanco J. Med. Sci. 2018, 22, 148–154. [Google Scholar] [CrossRef]
- Thakur, V.; Chiheriya, H.; Thakur, A.; Mourya, S. Study of maternal and fetal outcome in elective and emergency caesarean section. Emergency 2015, 2521, 1300–1305. [Google Scholar] [CrossRef]
- Biler, A.; Ekin, A.; Ozcan, A.; Inan, A.H.; Vural, T.; Toz, E. Is it safe to have multiple repeat cesarean sections? A high volume tertiary care center experience. Pak. J. Med. Sci. 2017, 33, 1074–1079. [Google Scholar] [CrossRef]
- Suwal, A.; Shrivastava, V.R.; Giri, A. Maternal and fetal outcome in elective versus emergency cesarean section. J. Nepal Med. Assoc. 2013, 52, 563–566. [Google Scholar] [CrossRef]
- Kolås, T.; Saugstad, O.D.; Daltveit, A.K.; Nilsen, S.T.; Øian, P. Planned cesarean versus planned vaginal delivery at term: Comparison of newborn infant outcomes. Am. J. Obstet. Gynecol. 2006, 195, 1538–1543. [Google Scholar] [CrossRef] [PubMed]
- Hook, B.; Kiwi, R.; Amini, S.B.; Fanaroff, A.; Hack, M. Neonatal morbidity after elective repeat cesarean section and trial of labor. Pediatrics 1997, 100, 348–353. [Google Scholar] [CrossRef]
- Bodner, K.; Wierrani, F.; Grünberger, W.; Bodner-Adler, B. Influence of the mode of delivery on maternal and neonatal outcomes: A comparison between elective cesarean section and planned vaginal delivery in a low-risk obstetric population. Arch. Gynecol. Obstet. 2011, 283, 1193–1198. [Google Scholar] [CrossRef] [PubMed]
- Prior, E.; Santhakumaran, S.; Gale, C.; Philipps, L.H.; Modi, N.; Hyde, M.J. Breastfeeding after cesarean delivery: A systematic review and meta-analysis of world literature. Am. J. Clin. Nutr. 2012, 95, 1113–1135. [Google Scholar] [CrossRef]
- Rollins, N.C.; Bhandari, N.; Hajeebhoy, N.; Horton, S.; Lutter, C.K.; Martines, J.C.; Piwoz, E.G.; Richter, L.M.; Victora, C.G. Why invest, and what it will take to improve breastfeeding practices? Lancet 2016, 387, 491–504. [Google Scholar] [CrossRef]
- Ponsiglione, A.M.; Trunfio, T.A.; Amato, F.; Improta, G. Predictive Analysis of Hospital Stay after Caesarean Section: A Single-Center Study. Bioengineering 2023, 10, 440. [Google Scholar] [CrossRef] [PubMed]
- Digenis, C.; Salter, A.; Cusack, L.; Koch, A.; Turnbull, D. Reduced length of hospital stay after caesarean section: A systematic review examining women’s experiences and psychosocial outcomes. Midwifery 2020, 91, 102855. [Google Scholar] [CrossRef] [PubMed]
- Maroufizadeh, S.; Amini, P.; Hosseini, M.; Almasi-Hashiani, A.; Mohammadi, M.; Navid, B.; Omani-Samani, R. Determinants of Cesarean Section among Primiparas: A Comparison of Classification Methods. Iran. J. Public Health 2018, 47, 1913–1922. [Google Scholar] [PubMed]
- Asfaw, T.; Tesema, A. Determinant factors, trend and outcomes of cesarean delivery in Debre Berhan referral hospital, North Shewa Zone, Ethiopia. Pediatr. Rep. 2020, 12, 8430. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Number | Percentage | |
|---|---|---|---|
| Age group (years) | 20–30 | 146 | 54.5% |
| 31–40 | 103 | 38.4% | |
| 41–50 | 19 | 7.1% | |
| Residence | Abuarish | 139 | 51.9% |
| Jazan | 88 | 32.8% | |
| Sabya | 41 | 15.3% | |
| Parity | 1 | 133 | 49.6% |
| 2 | 62 | 23.1% | |
| 3 | 49 | 18.3% | |
| 4 | 15 | 5.6% | |
| 5 | 9 | 3.4% | |
| Had regular antenatal care | Yes | 246 | 91.8% |
| No | 22 | 8.2% | |
| History of any chronic conditions | Yes | 34 | 12.7% |
| No | 234 | 87.3% | |
| History of DM | Yes | 14 | 5.2% |
| No | 254 | 94.8% | |
| History of HTN | Yes | 8 | 3.0% |
| No | 260 | 97.0% | |
| Number of previous CSs | 0 | 133 | 49.6% |
| 1 | 62 | 23.1% | |
| 2 | 49 | 18.3% | |
| 3 | 15 | 5.6% | |
| 4 | 9 | 3.4% | |
| Need of antenatal admission before operation | Yes | 24 | 9.0% |
| No | 244 | 91.0% | |
| Child gender | Female | 142 | 53.0% |
| Male | 126 | 47.0% | |
| Condition | All | Group I | Group II | p Value * | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |||
| Fenestration | No | 266 | (99.3) | 194 | (99.5) | 72 | (98.6) | 0.471 |
| Yes | 2 | (0.7) | 1 | (0.5) | 1 | (1.4) | ||
| Rectal muscle diastasis (separated) | No | 267 | (99.6) | 195 | (100.0) | 72 | (98.6) | 0.272 |
| Yes | 1 | (0.4) | 0 | (0.0) | 1 | (1.4) | ||
| Fused abdominal wall layers | No | 249 | (92.9) | 184 | (94.4) | 65 | (89.0) | 0.109 |
| Yes | 19 | (7.1) | 11 | (5.6) | 8 | (11.0) | ||
| Urinary bladder attached high in the anterior abdominal wall | No | 263 | (98.1) | 193 | (99.0) | 70 | (95.9) | 0.126 |
| Yes | 5 | (1.9) | 2 | (1.0) | 3 | (4.1) | ||
| Intra peritoneal adhesions | No | 248 | (92.5) | 184 | (94.4) | 64 | (87.7) | 0.060 |
| Yes | 20 | (7.5) | 11 | (5.6) | 9 | (12.3) | ||
| Intrapartum hemorrhage | No | 263 | (98.1) | 192 | (98.5) | 71 | (97.3) | 0.415 |
| Yes | 5 | (1.9) | 3 | (1.5) | 2 | (2.7) | ||
| Need for tubal ligation | No | 265 | (98.9) | 194 | (99.5) | 71 | (97.3) | 0.180 |
| Yes | 3 | (1.1) | 1 | (0.5) | 2 | (2.7) | ||
| Early mobilization within 24 h | No | 5 | (1.9) | 5 | (2.6) | 0 | (0.0) | 0.201 |
| Yes | 263 | (98.1) | 190 | (97.4) | 73 | (100.0) | ||
| Postoperative complications | No | 267 | (99.6) | 195 | (100.0) | 72 | (98.6) | 0.272 |
| Yes | 1 | (0.4) | 0 | (0.0) | 1 | (1.4) | ||
| Thromboembolism | No | 267 | (99.6) | 194 | (99.5) | 73 | (100.0) | 0.728 |
| Yes | 1 | (0.4) | 1 | (0.5) | 0 | (0.0) | ||
| Sepsis | No | 265 | (98.9) | 194 | (99.5) | 71 | (97.3) | 0.181 |
| Yes | 3 | (1.1) | 1 | (0.5) | 2 | (2.7) | ||
| Paralytic ileus | No | 267 | (99.6) | 194 | (99.5) | 73 | (100.0) | 0.728 |
| Yes | 1 | (0.4) | 1 | (0.5) | 0 | (0.0) | ||
| UTI | No | 260 | (97.0) | 188 | (96.4) | 72 | (98.6) | 0.130 |
| Yes | 8 | (3.0) | 7 | (3.6) | 1 | (1.4) | ||
| Fever | No | 256 | (95.5) | 185 | (94.9) | 71 | (97.3) | 0.319 |
| Yes | 8 | (3.0) | 7 | (3.6) | 1 | (1.4) | ||
| Need for blood transfusion | No | 209 | (78.0) | 149 | (76.4) | 60 | (82.2) | 0.198 |
| Yes | 59 | (22.0) | 46 | (23.6) | 13 | (17.8) | ||
| Start breastfeeding in the first 24 h | No | 10 | (3.7) | 7 | (3.6) | 3 | (4.1) | 0.543 |
| Yes | 258 | (96.3) | 188 | (96.4) | 70 | (95.9) | ||
| Needed resuscitation | No | 261 | (97.4) | 192 | (98.5) | 69 | (94.5) | 0.090 |
| Yes | 7 | (2.6) | 3 | (1.5) | 4 | (5.5) | ||
| Needed NICU admission | No | 260 | (97.0) | 189 | (96.9) | 71 | (97.3) | 0.623 |
| Yes | 8 | (3.0) | 6 | (3.1) | 2 | (2.7) | ||
| Type of abdominal incision | Midline | 19 | (7.1) | 13 | (6.7) | 6 | (8.2) | 0.418 |
| Pfannenstiel | 249 | (92.9) | 182 | (93.3) | 67 | (91.8) | ||
| Placental site | Lower | 80 | (29.9) | 58 | (29.7) | 22 | (30.1) | 0.531 |
| Upper | 188 | (70.1) | 137 | (70.3) | 51 | (69.9) | ||
| Type of operation | Elective | 106 | (39.6) | 59 | (30.3) | 47 | (64.4) | <0.001 |
| Emergency | 162 | (60.4) | 136 | (69.7) | 26 | (35.6) | ||
| Type of anesthesia | Epidural | 3 | (1.1) | 2 | (1.0) | 1 | (1.4) | 0.152 |
| GA | 74 | (27.6) | 48 | (24.6) | 26 | (35.6) | ||
| Spinal | 191 | (71.3) | 145 | (74.4) | 46 | (63.0) | ||
| Apgar score | Normal (10) | 217 | (81.0) | 149 | (76.4) | 68 | (93.2) | 0.001 |
| Low(5) | 51 | (19.0) | 46 | (23.6) | 5 | (6.8) | ||
| Factor | All | Group I | Group II | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | N | Mean | SD | ||
| Operating time (minutes) | 268 | 48.54 | 8.95 | 195 | 49.74 | 8.85 | 73 | 45.36 | 8.48 | <0.001 |
| Postoperative hospital stay(days) | 268 | 3.31 | 1.50 | 195 | 3.28 | 1.43 | 73 | 3.40 | 1.66 | 0.559 |
| Uterine incision to delivery time | 268 | 17.02 | 4.95 | 195 | 17.10 | 4.71 | 73 | 16.81 | 5.58 | 0671 |
| Hemoglobin on admission in g/L | 182 | 10.67 | 1.32 | 123 | 10.57 | 1.40 | 59 | 10.87 | 1.10 | 0.150 |
| Postoperative hemoglobin in g/L | 265 | 10.19 | 1.28 | 193 | 10.15 | 1.32 | 72 | 10.32 | 1.19 | 0.351 |
| Blood loss in mL | 230 | 0.97 | 0.93 | 169 | 1.09 | 1.01 | 61 | 0.66 | 0.53 | 0.002 |
| Blood units needed in mL | 60 | 730.00 | 315.32 | 48 | 704.17 | 327.44 | 12 | 833.33 | 246.18 | 0.207 |
| Birth weight in kg | 268 | 3.03 | 0.26 | 195 | 3.02 | 0.25 | 73 | 3.03 | 0.29 | 0.923 |
| Parity | 268 | 1.9 | 1.10 | 195 | 1.32 | 0.47 | 73 | 3.45 | 0.71 | <0.001 |
| Variable | COR | 95% CI | p Value | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Age group (years) | 20–30 (Ref) | 1 | |||
| 31–40 | 2.99 | 1.77 | 5.05 | <0.001 | |
| 41–50 | 2.76 | 1.02 | 7.41 | 0.045 | |
| Residence | Abuarish (Ref) | 1 | |||
| Jazan | 0.15 | 0.08 | 0.29 | <0.001 | |
| Sabya | 1.08 | 0.52 | 2.25 | 0.830 | |
| Had regular antenatal care | No (Ref) | 1 | |||
| Yes | 1.81 | 0.73 | 4.46 | 1.81 | |
| History of any chronic condition | No (Ref) | 1 | |||
| Yes | 1.33 | 0.65 | 2.75 | 0.436 | |
| Poor medical history | No (Ref) | 1 | |||
| Yes | 29.94 | 11.40 | 78.64 | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murtada, M.; Hakami, N.; Mahfouz, M.; Abdelmola, A.; Eltyeb, E.; Medani, I.; Maghfori, G.; Zakri, A.; Hakami, A.; Altraifi, A.; et al. Multiple Cesarean Section Outcomes and Complications: A Retrospective Study in Jazan, Saudi Arabia. Healthcare 2023, 11, 2799. https://doi.org/10.3390/healthcare11202799
Murtada M, Hakami N, Mahfouz M, Abdelmola A, Eltyeb E, Medani I, Maghfori G, Zakri A, Hakami A, Altraifi A, et al. Multiple Cesarean Section Outcomes and Complications: A Retrospective Study in Jazan, Saudi Arabia. Healthcare. 2023; 11(20):2799. https://doi.org/10.3390/healthcare11202799
Chicago/Turabian StyleMurtada, Maha, Nasser Hakami, Mohamed Mahfouz, Amani Abdelmola, Ebtihal Eltyeb, Isameldin Medani, Ghadah Maghfori, Atheer Zakri, Ahlam Hakami, Ahmed Altraifi, and et al. 2023. "Multiple Cesarean Section Outcomes and Complications: A Retrospective Study in Jazan, Saudi Arabia" Healthcare 11, no. 20: 2799. https://doi.org/10.3390/healthcare11202799
APA StyleMurtada, M., Hakami, N., Mahfouz, M., Abdelmola, A., Eltyeb, E., Medani, I., Maghfori, G., Zakri, A., Hakami, A., Altraifi, A., Khormi, A., & Chourasia, U. (2023). Multiple Cesarean Section Outcomes and Complications: A Retrospective Study in Jazan, Saudi Arabia. Healthcare, 11(20), 2799. https://doi.org/10.3390/healthcare11202799






