Short-Term Effects of Centralization of the Glenohumeral Joint and Dynamic Humeral Centering on Shoulder Pain, Disability, and Grip Strength in Patients with Secondary Subacromial Impingement Syndrome
Abstract
1. Introduction
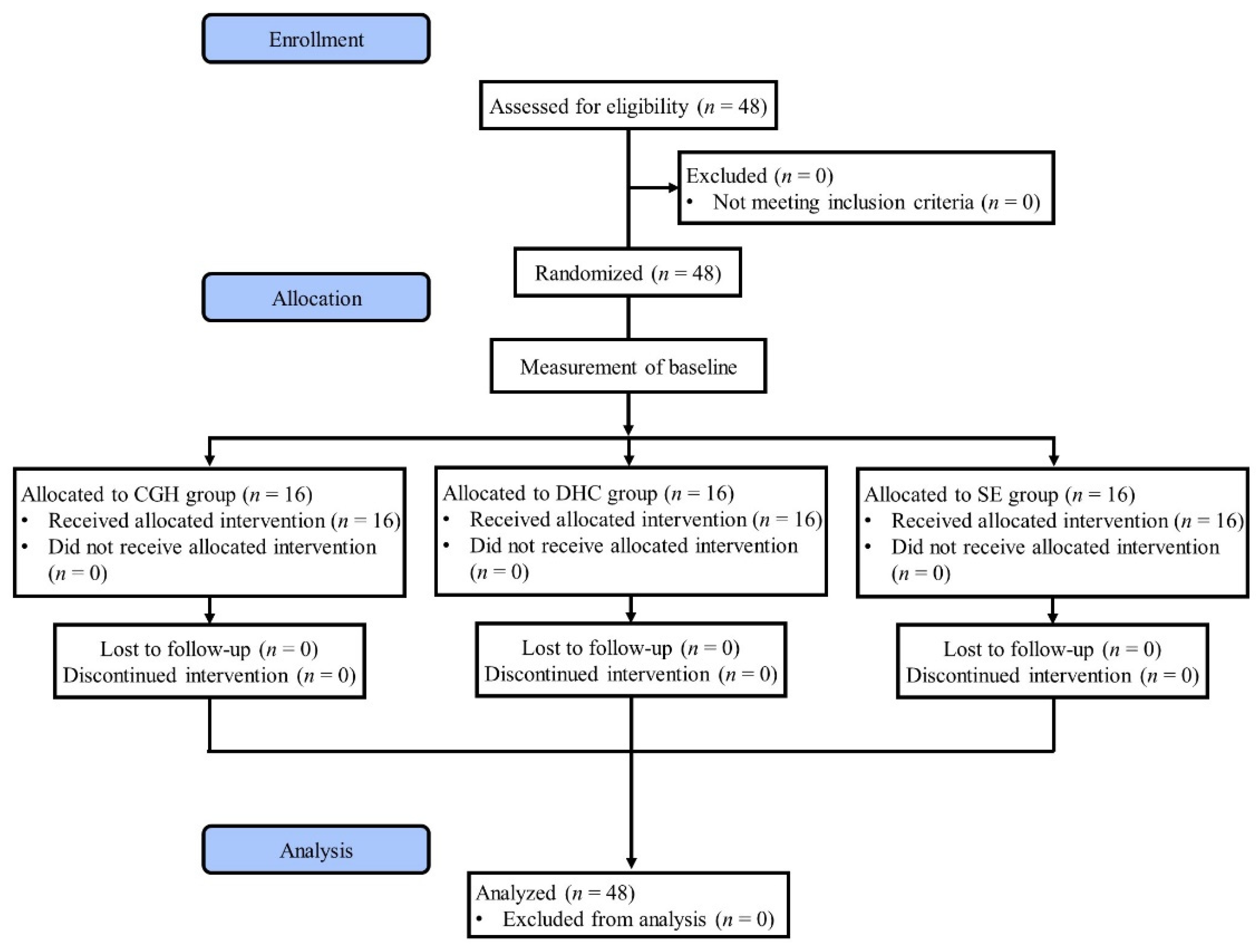
2. Materials and Methods
2.1. Participants
2.2. Study Design and Protocol
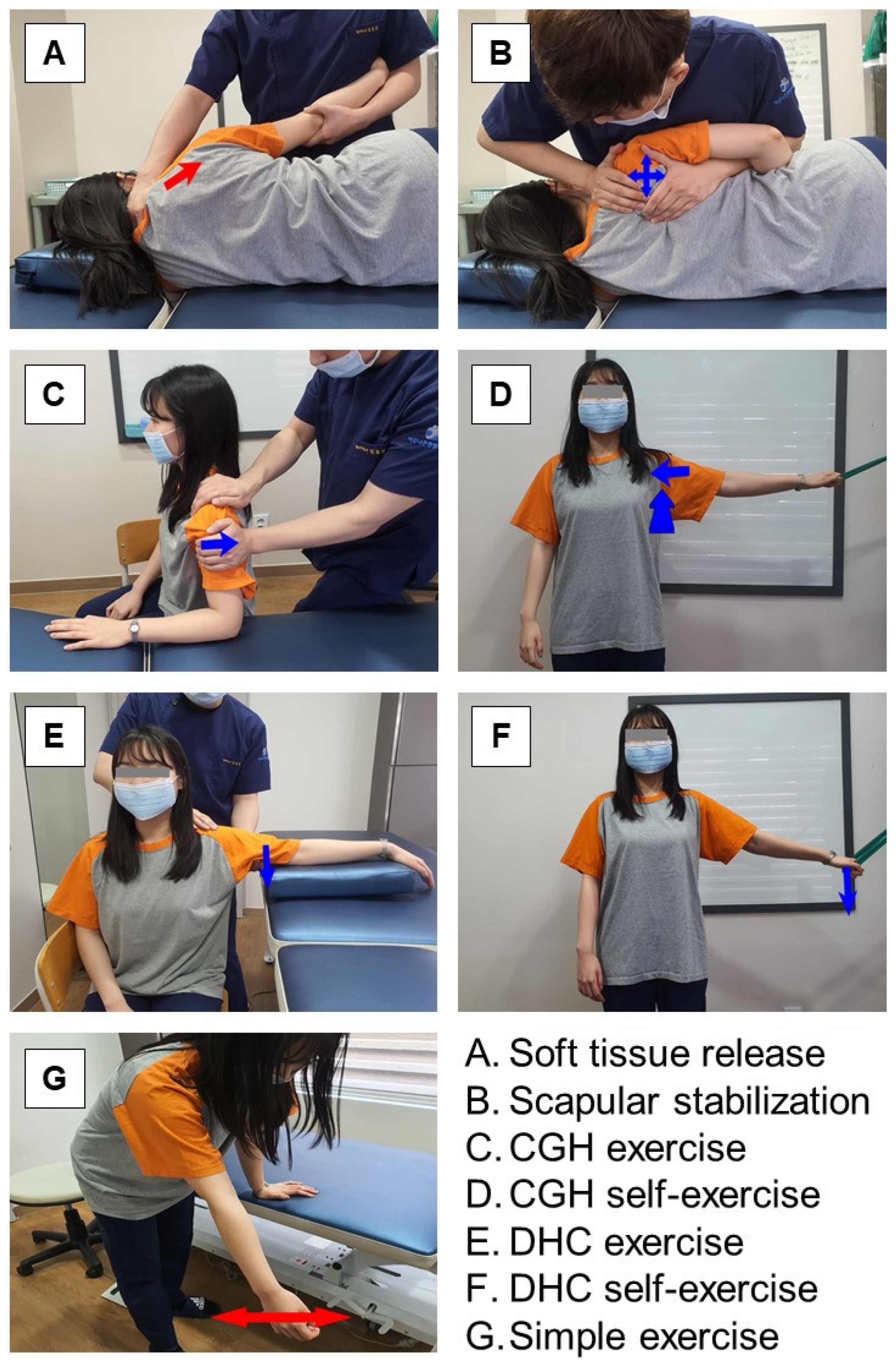
2.3. Intervention
2.3.1. Centralization of the Glenohumeral Joint Exercise
2.3.2. Dynamic Humeral Centering Exercise
2.3.3. Simple Exercise
2.4. Outcome Measurements
2.4.1. Constant–Murley Score
2.4.2. Grip Strength
2.5. Data Analysis
3. Results
3.1. Demographic and Clinical Profiles of the Study Participants
3.2. Constant–Murley Score
3.3. Grip Strength
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Imhoff, A.B.; Ledermann, T. Definition, Pathologische Befunde und Pathogenese; Das Impingement-syndrom der Schulter; Eulert, J., Hedtmann, A., Eds.; Thieme Verlag: New York, NY, USA, 1996; pp. 1–13. [Google Scholar]
- Feleus, A.; Bierma-Zeinstra, S.M.; Miedema, H.S.; Bernsen, R.M.; Verhaar, J.A.; Koes, B.W. Incidence of non-traumatic complaints of arm, neck and shoulder in general practice. Man. Ther. 2008, 13, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Luime, J.J.; Koes, B.W.; Hendriksen, I.J.; Burdorf, A.; Verhagen, A.P.; Miedema, H.S.; Verhaar, J.A. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand. J. Rheumatol. 2004, 33, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.S. Rotator cuff tendinopathy. Br. J. Sports Med. 2009, 43, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Jerosch, J.; Wüstner, P. Effect of a sensorimotor training program on patients with subacromial pain syndrome. Der Unfallchirurg. 2002, 105, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Joo, H.; Lee, Y.J.; Shin, J.S.; Lee, J.; Kim, M.R.; Koh, W.; Park, Y.; Song, Y.K.; Cho, J.H.; Ha, I.H. Medical service use and usual care of common shoulder disorders in Korea: A cross-sectional study using the Health Insurance Review and Assessment Service National Patient Sample. BMJ Open 2017, 7, e015848. [Google Scholar] [CrossRef] [PubMed]
- Viikari-Juntura, E.; Shiri, R.; Solovieva, S.; Karppinen, J.; Leino-Arjas, P.; Varonen, H.; Kalso, E.; Ukkola, O. Risk factors of atherosclerosis and shoulder pai—Is there an association? A systematic review. Eur. J. Pain 2008, 12, 412–426. [Google Scholar] [CrossRef] [PubMed]
- Walker-Bone, K.; Palmer, K.T.; Reading, I.; Coggon, D.; Cooper, C. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Rheum. 2004, 51, 642–651. [Google Scholar] [CrossRef]
- Koester, M.C.; George, M.S.; Kuhn, J.E. Shoulder impingement syndrome. Am. J. Med. 2005, 118, 452–455. [Google Scholar] [CrossRef]
- Natsis, K.; Tsikaras, P.; Totlis, T.; Gigis, I.; Skandalakis, P.; Appell, H.J.; Koebke, J. Correlation between the four types of acromion and the existence of enthesophytes: A study on 423 dried scapulas and review of the literature. Clin. Anat. 2007, 20, 267–272. [Google Scholar] [CrossRef]
- Chang, E.Y.; Moses, D.A.; Babb, J.S.; Schweitzer, M.E. Shoulder impingement: Objective 3D shape analysis of acromial morphologic features. Radiology 2006, 239, 497–505. [Google Scholar] [CrossRef]
- Blevins, F.T. Rotator cuff pathology in athletes. Sports Med. 1997, 24, 205–220. [Google Scholar] [CrossRef] [PubMed]
- Burkhart, S.S.; Morgan, C.D.; Kibler, W.B. The disabled throwing shoulder: Spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy 2003, 19, 641–661. [Google Scholar] [CrossRef] [PubMed]
- Cools, A.M.; Cambier, D.; Witvrouw, E.E. Screening the athlete’s shoulder for impingement symptoms: A clinical reasoning algorithm for early detection of shoulder pathology. Br. J. Sports Med. 2008, 42, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Kibler, W.B.; Sciascia, A.; Dome, D. Evaluation of apparent and absolute supraspinatus strength in patients with shoulder injury using the scapular retraction test. Am. J. Sports Med. 2006, 34, 1643–1647. [Google Scholar] [CrossRef] [PubMed]
- McClure, P.; Tate, A.R.; Kareha, S.; Irwin, D.; Zlupko, E. A clinical method for identifying scapular dyskinesis, part 1: Reliability. J. Athl. Train. 2009, 44, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, L.D.; McMahon, P.J.; Towers, J.; Irrgang, J.J.; Rodosky, M.W. Internal impingement: Findings on magnetic resonance imaging and arthroscopic evaluation. Arthroscopy 2004, 20, 701–704. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.S.; Green, A.; Wright, C. Subacromial impingement syndrome: The role of posture and muscle imbalance. J. Shoulder Elb. Surg. 2005, 14, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Wilk, K.E.; Obma, P.; Simpson, C.D.; Cain, E.L.; Dugas, J.R.; Andrews, J.R. Shoulder injuries in the overhead athlete. J. Orthop. Sports Phys. Ther. 2009, 39, 38–54. [Google Scholar] [CrossRef]
- Voight, M.L.; Thomson, B.C. The role of the scapula in the rehabilitation of shoulder injuries. J. Athl. Train. 2000, 35, 364–372. [Google Scholar]
- Bandholm, T.; Rasmussen, L.; Aagaard, P.; Jensen, B.R.; Diederichsen, L. Force steadiness, muscle activity, and maximal muscle strength in subjects with subacromial impingement syndrome. Muscle Nerve 2006, 34, 631–639. [Google Scholar] [CrossRef]
- Brumitt, J. Scapular-stabilization exercises: Early-intervention prescription. Athl. Ther. Today 2006, 11, 15–18. [Google Scholar] [CrossRef][Green Version]
- Horsley, I.; Herrington, L.; Hoyle, R.; Prescott, E.; Bellamy, N. Do changes in hand grip strength correlate with shoulder rotator cuff function? Shoulder Elb. 2016, 8, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Akyol, Y.; Ulus, Y.; Durmuş, D.; Tander, B.; Cantürk, F.; Bilgici, A.; Kuru, Ö.; Yüksel, B.E.K. Shoulder muscle strength in patients with subacromial impingement syndrome: Its relationship with duration of quality of life and emotional status. Turk. J. Phys. Med. Rehab. 2013, 59, 176–181. [Google Scholar]
- Ludewig, P.M.; Cook, T.M. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys. Ther. 2000, 80, 276–291. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, J.E. Exercise in the treatment of rotator cuff impingement: A systematic review and a synthesized evidence-based rehabilitation protocol. J. Shoulder Elb. Surg. 2009, 18, 138–160. [Google Scholar] [CrossRef] [PubMed]
- Green, S.; Buchbinder, R.; Glazier, R.; Forbes, A. Systematic review of randomised controlled trials of interventions for painful shoulder: Selection criteria, outcome assessment, and efficacy. BMJ 1998, 316, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Desmeules, F.; Côté, C.H.; Frémont, P. Therapeutic exercise and orthopedic manual therapy for impingement syndrome: A systematic review. Clin. J. Sport Med. 2003, 13, 176–182. [Google Scholar] [CrossRef]
- Faber, E.; Kuiper, J.I.; Burdorf, A.; Miedema, H.S.; Verhaar, J.A. Treatment of impingement syndrome: A systematic review of the effects on functional limitations and return to work. J. Occup. Rehabil. 2006, 16, 7–25. [Google Scholar] [CrossRef]
- Kromer, T.O.; Tautenhahn, U.G.; de Bie, R.A.; Staal, J.B.; Bastiaenen, C.H. Effects of physiotherapy in patients with shoulder impingement syndrome: A systematic review of the literature. J. Rehabil. Med. 2009, 41, 870–880. [Google Scholar] [CrossRef]
- Park, S.I.; Choi, Y.K.; Lee, J.H.; Kim, Y.M. Effects of shoulder stabilization exercise on pain and functional recovery of shoulder impingement syndrome patients. J. Phys. Ther. Sci. 2013, 25, 1359–1362. [Google Scholar] [CrossRef][Green Version]
- Giannakopoulos, K.; Beneka, A.; Malliou, P.; Godolias, G. Isolated vs. complex exercise in strengthening the rotator cuff muscle group. J. Strength Cond. Res. 2004, 18, 144–148. [Google Scholar] [PubMed]
- Werner, A.; Walther, M.; Ilg, A.; Stahlschmidt, T.; Gohlke, F. Self-training versus conventional physiotherapy in subacromial impingement syndrome. Z. Fur Orthop. Und Ihre Grenzgeb. 2002, 140, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Morrison, D.S.; Frogameni, A.D.; Woodworth, P. Non-operative treatment of subacromial impingement syndrome. J. Bone Jt. Surg. Am. 1997, 79, 732–737. [Google Scholar] [CrossRef] [PubMed]
- Myers, J.B.; Wassinger, C.A.; Lephart, S.M. Sensorimotor contribution to shoulder stability: Effect of injury and rehabilitation. Man Ther. 2006, 11, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Hess, S.A. Functional stability of the glenohumeral joint. Man. Ther. 2000, 5, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Jeon, N.Y.; Chon, S.C. Effect of glenohumeral stabilization exercises combined with scapular stabilization on shoulder function in patients with shoulder pain: A randomized controlled experimenter-blinded study. J. Back Musculoskelet. Rehabil. 2018, 31, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Beaudreuil, J.; Lasbleiz, S.; Richette, P.; Seguin, G.; Rastel, C.; Aout, M.; Vicaut, E.; Cohen-Solal, M.; Lioté, F.; de Vernejoul, M.C.; et al. Assessment of dynamic humeral centering in shoulder pain with impingement syndrome: A randomised clinical trial. Ann. Rheum. Dis. 2011, 70, 1613–1618. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- De Mey, K.; Cagnie, B.; Danneels, L.A.; Cools, A.M.; Van de Velde, A. Trapezius muscle timing during selected shoulder rehabilitation exercises. J. Orthop. Sports Phys. Ther. 2009, 39, 743–752. [Google Scholar] [CrossRef]
- Beaudreuil, J.; Lasbleiz, S.; Aout, M.; Vicaut, E.; Yelnik, A.; Bardin, T.; Orcel, P. Effect of dynamic humeral centring (DHC) treatment on painful active elevation of the arm in subacromial impingement syndrome. Secondary analysis of data from an RCT. Br. J. Sports Med. 2015, 49, 343–346. [Google Scholar] [CrossRef]
- Moeller, A.D.; Thorsen, R.R.; Torabi, T.P.; Bjoerkman, A.S.; Christensen, E.H.; Maribo, T.; Christiansen, D.H. The Danish version of the modified Constant-Murley shoulder score: Reliability, agreement, and construct validity. J. Orthop. Sports Phys. Ther. 2014, 44, 336–340. [Google Scholar] [CrossRef] [PubMed]
- De Smet, L.; Fabry, G. Grip force reduction in patients with tennis elbow: Influence of elbow position. J. Hand Ther. 1997, 10, 229–231. [Google Scholar] [CrossRef] [PubMed]
- Lindstrom-Hazel, D.; Kratt, A.; Bix, L. Interrater reliability of students using hand and pinch dynamometers. Am. J. Occup. Ther. 2009, 63, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Leroux, J.L.; Revel, M. Rehabilitation of rotator cuff disorders. Rev. Rhum. 1996, 63, S82–S87. [Google Scholar]
- Bohmer, A.S.; Staff, P.H.; Brox, J.I. Supervised exercises in relation to rotator cuff disease (impingement syndrome stages II and III): A treatment regimen and its rationale. Physiother. Theory Pract. 1998, 14, 93–105. [Google Scholar] [CrossRef]
- Neumann, D.A. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation; Elsevier Health Sciences: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Wuelker, N.; Korell, M.; Thren, K. Dynamic glenohumeral joint stability. J. Shoulder Elb. Surg. 1998, 7, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Moghadam, A.N.; Mohammadi, R.; Arab, A.M.; Kazamnajad, A. The effect of shoulder core exercises on isometric torque of glenohumeral joint movements in healthy young females. J. Res. Med. Sci. 2011, 16, 1555–1563. [Google Scholar]
| CGH | DHC | SE | Time | |
|---|---|---|---|---|
| Warm-up | Step 1: Stretching and massage of muscle and soft tissue of the neck and shoulder region Step 2: Scapular stabilization | Step 1: Stretching and massage of muscle and soft tissue of the neck and shoulder region Step 2: Scapular stabilization | Step 1: Stretching and massage of muscle and soft tissue of the neck and shoulder region Step 2: Scapular stabilization | 10 min |
| Main exercise | Step 1: Passive movement of the humeral head in four directions by the therapist Step 2: The participant holds a band or cushion ball, and, against resistance, positions the head of the humerus in the center of the glenohumeral joint | Step 1: Lowering of the humeral head during the passive abduction of the shoulder Step 2: Actively lowering the humeral head by co-contraction of the pectoralis major and latissimus dorsi during active abduction of the shoulder | Step 1: Active and passive range of motion exercise in the pain-free range of motion (flexion, extension, abduction, horizontal abduction, horizontal adduction, external rotation, and internal rotation) Step 2: Movement and pendulum exercise (anterior–posterior, medial–lateral, and rotation) | 30 min |
| Cool-down | Stretching Muscle and soft tissue of the neck and shoulder region | Stretching Muscle and soft tissue of the neck and shoulder region | Stretching Muscle and soft tissue of the neck and shoulder region | 10 min |
| Variables | CGH Group (n = 16) | DHC Group (n = 16) | SE Group (n = 16) | p-Value |
|---|---|---|---|---|
| Height (cm) * | 174.00 ± 8.29 | 168.75 ± 7.72 | 172.69 ± 10.62 | 0.353 † |
| Age (year) * | 35.66 ± 4.37 | 35.72 ± 5.65 | 37.08 ± 4.92 | 0.742 † |
| Weight (kg) * | 72.25 ± 13.49 | 64.41 ± 15.57 | 68.47 ± 13.66 | 0.383 † |
| Constant–Murley score (score) * | 53.27 ± 8.00 | 54.93 ± 8.02 | 55.86 ± 10.52 | 0.772 † |
| Pain (0–15 point) | 7.67 ± 2.23 | 8.25 ± 2.01 | 8.92 ± 2.11 | 0.362 † |
| ADL (0–20 point) | 13.00 ± 1.91 | 13.17 ± 2.41 | 12.42 ± 2.23 | 0.682 † |
| ROM (0–40 point) | 27.00 ± 4.55 | 27.83 ± 2.62 | 27.83 ± 4.47 | 0.840 † |
| Strength (0–25 point) | 5.60 ± 5.09 | 5.68 ± 4.41 | 6.70 ± 5.86 | 0.846 † |
| Rt side/Lt side (%) § | 10 (62.50)/6 (37.50) | 9 (56.25)/7 (43.75) | 9 (56.25)/7 (43.75) | 0.918 ‡ |
| Female/male (%) § | 8 (50.00)/8 (50.00) | 9 (56.25)/7 (43.75) | 8 (50.00)/8 (50.00) | 0.920 ‡ |
| Neer test positive (%) § | 10 (62.50) | 11 (68.75) | 10 (62.50) | 0.913 ‡ |
| Hawkins test positive (%) § | 15 (93.75) | 14 (87.50) | 14 (87.50) | 0.800 ‡ |
| Yocum test positive (%) § | 14 (87.50) | 15 (93.75) | 14 (87.50) | 0.800 ‡ |
| Parameters | Group | Pre-Treatment | Post-Treatment | Effect Size | p-Value |
|---|---|---|---|---|---|
| Primary Outcome | |||||
| Constant–Murley score (score) | CGH | 53.27 ± 8.00 | 67.62 ± 5.49 ***†† | 2.21 | <0.001 |
| DHC | 54.93 ± 8.02 | 64.25 ± 7.67 *** | 1.89 | ||
| SE | 55.86 ± 10.52 | 57.27 ± 10.04 | 0.28 | ||
| Pain (0–15 point) | CGH | 7.67 ± 2.23 | 11.08 ± 1.88 *** | 1.82 | 0.001 |
| DHC | 8.25 ± 2.01 | 10.92 ± 1.68 *** | 1.22 | ||
| SE | 8.92 ± 2.11 | 9.42 ± 1.93 | 0.96 | ||
| ADL (0–20 point) | CGH | 13.00 ± 1.91 | 13.5 ± 1.73 | 0.40 | 0.127 |
| DHC | 13.17 ± 2.41 | 13.08 ± 2.43 | 0.29 | ||
| SE | 12.42 ± 2.23 | 12.42 ± 2.23 | <0.001 | ||
| ROM (0–40 point) | CGH | 27.00 ± 4.55 | 35.00 ± 3.95 ***†† | 1.91 | <0.001 |
| DHC | 27.83 ± 2.62 | 33.83 ± 3.66 *** | 1.82 | ||
| SE | 27.83 ± 4.47 | 29.83 ± 4.55 * | 0.89 | ||
| Shoulder Strength (0–25 point) | CGH | 5.60 ± 5.09 | 8.03 ± 4.92 *** | 1.21 | 0.003 |
| DHC | 5.68 ± 4.41 | 6.42 ± 4.62 | 0.69 | ||
| SE | 6.70 ± 5.86 | 6.93 ± 6.57 | 0.18 | ||
| Secondary Outcome | |||||
| Grip Strength (lb) | CGH | 50.63 ± 14.95 | 57.90 ± 17.80 *** | 1.66 | <0.001 |
| DHC | 49.74 ± 14.58 | 50.92 ± 14.61 | 0.19 | ||
| SE | 56.63 ± 17.36 | 55.22 ± 16.96 | 0.36 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.-H.; Cho, H.-Y.; Kim, S.-H. Short-Term Effects of Centralization of the Glenohumeral Joint and Dynamic Humeral Centering on Shoulder Pain, Disability, and Grip Strength in Patients with Secondary Subacromial Impingement Syndrome. Healthcare 2023, 11, 2914. https://doi.org/10.3390/healthcare11222914
Kim Y-H, Cho H-Y, Kim S-H. Short-Term Effects of Centralization of the Glenohumeral Joint and Dynamic Humeral Centering on Shoulder Pain, Disability, and Grip Strength in Patients with Secondary Subacromial Impingement Syndrome. Healthcare. 2023; 11(22):2914. https://doi.org/10.3390/healthcare11222914
Chicago/Turabian StyleKim, Yong-Hee, Hwi-Young Cho, and Sung-Hyeon Kim. 2023. "Short-Term Effects of Centralization of the Glenohumeral Joint and Dynamic Humeral Centering on Shoulder Pain, Disability, and Grip Strength in Patients with Secondary Subacromial Impingement Syndrome" Healthcare 11, no. 22: 2914. https://doi.org/10.3390/healthcare11222914
APA StyleKim, Y.-H., Cho, H.-Y., & Kim, S.-H. (2023). Short-Term Effects of Centralization of the Glenohumeral Joint and Dynamic Humeral Centering on Shoulder Pain, Disability, and Grip Strength in Patients with Secondary Subacromial Impingement Syndrome. Healthcare, 11(22), 2914. https://doi.org/10.3390/healthcare11222914







