Ambient Noise in Candidate Rooms for User-Operated Audiometry
Abstract
1. Introduction
2. Methods
2.1. Rooms
2.2. Measurements
2.3. Data Analysis
3. Results
3.1. UAud-Candidate Rooms (Non-Sound Treated Rooms)
3.1.1. Rooms without Quasi-Constant Violations
3.1.2. Rooms with Quasi-Constant Violations
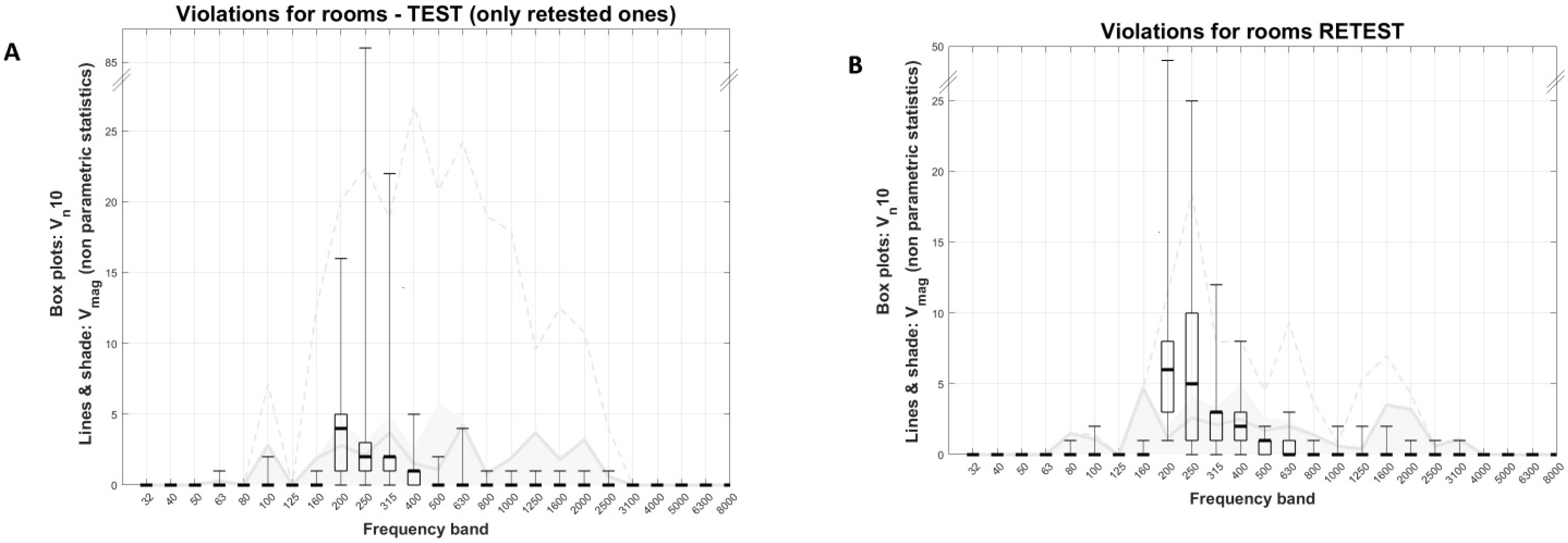
3.1.3. Test–Retest
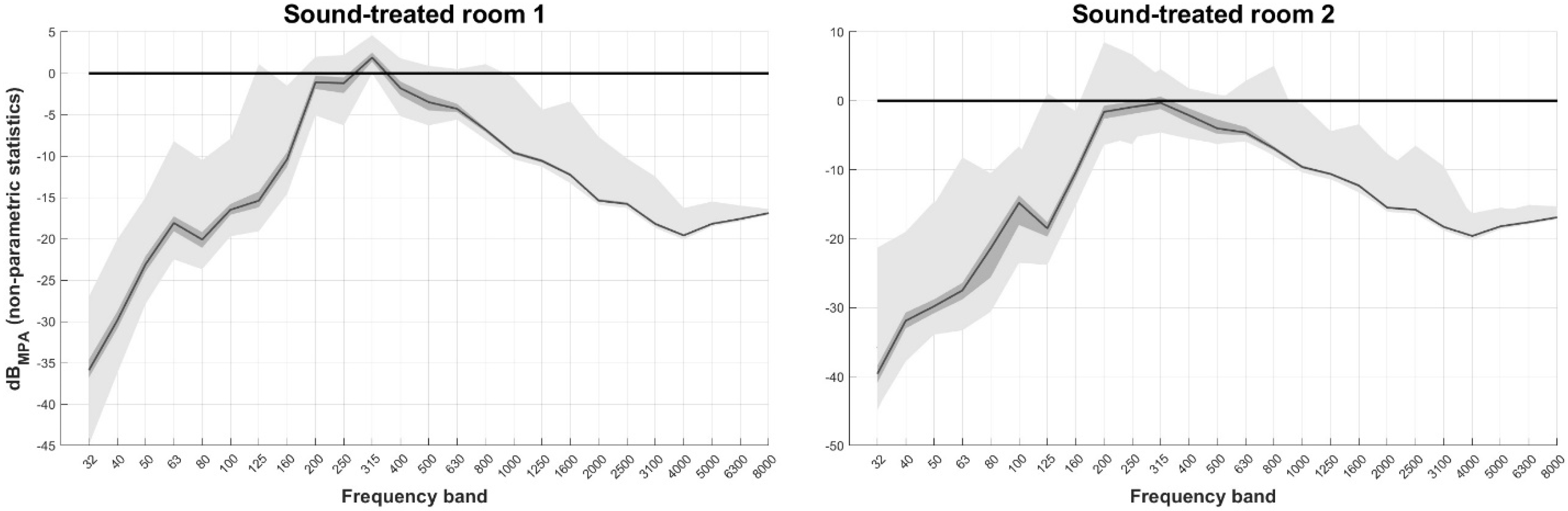
3.2. Standard Audiometry Rooms (Sound-Treated Rooms)
4. Discussion
4.1. MPA Violations—Overview
4.2. Test–Retest—Limitations and Generalizability of Results
4.3. Challenges in Predicting Ambient Noise Effects
- Does ambient noise effects depend on hearing loss?
- What is the effect of transient violations in audiometry?
- Are there any effects other than masking and is ambient noise’s semantic content relevant?
- Do patients’ characteristics, such as distractibility, discomfort to sound, and/or cognition play a role?
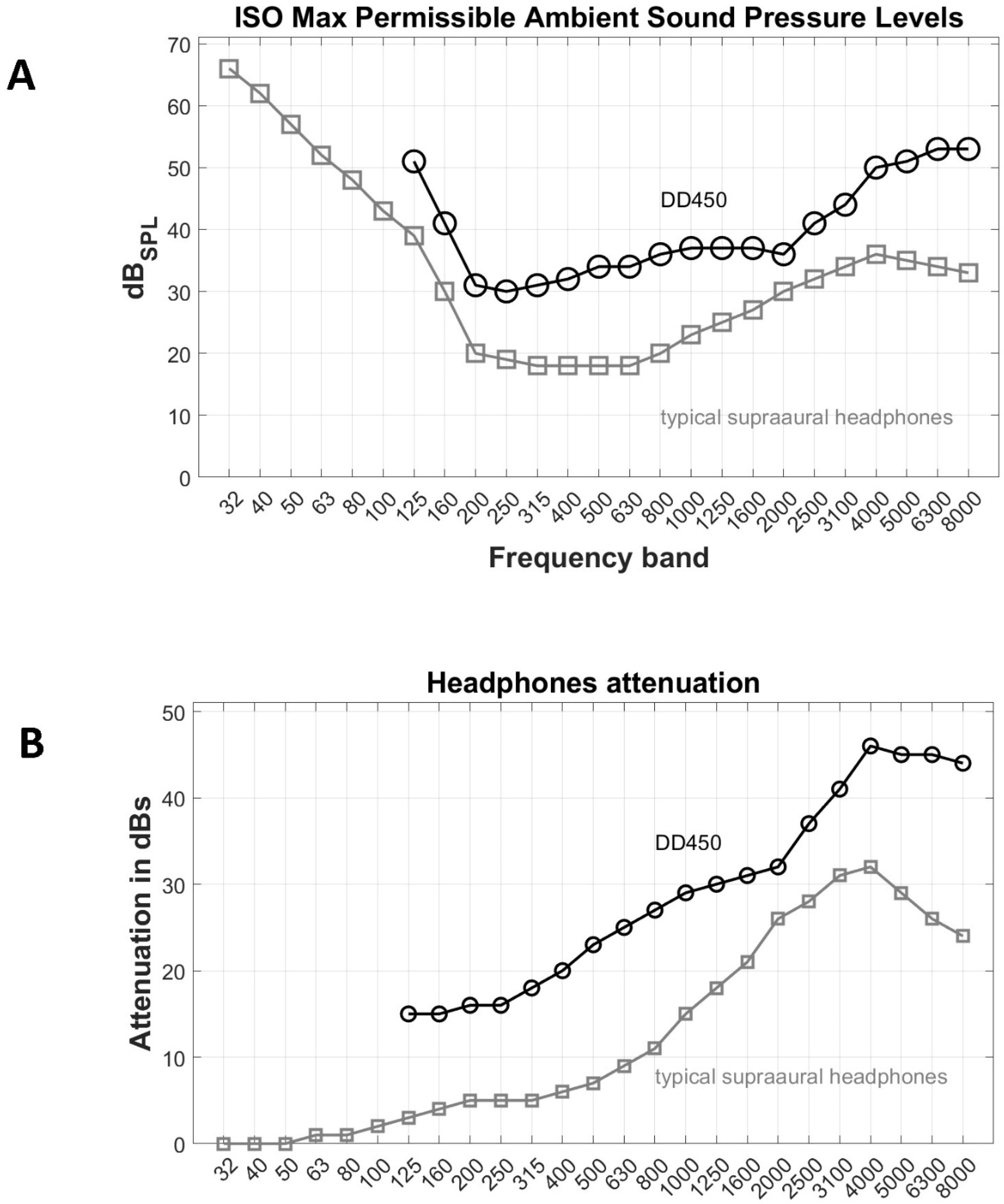
4.4. Ambient Noise Violations and Headphones Attenuation
4.5. Addressing Ambient Noise—Online Test Pause
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Amieva, H.; Ouvrard, C.; Giulioli, C.; Meillon, C.; Rullier, L.; Dartigues, J.-F. Self reported hearing loss, hearing aids, and cognitive decline in elderly adults: A 25-year study. J. Am. Geriatr. Soc. 2015, 63, 2099–2104. [Google Scholar] [CrossRef]
- Hardy, C.J.D.; Marshall, C.R.; Golden, H.L.; Clark, C.N.; Mummery, C.J.; Griffiths, T.D.; Bamiou, D.E.; Warren, J.D. Hearing and dementia. J. Neurol. 2016, 263, 2339–2354. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, T.D.; Lad, M.; Kumar, S.; Holmes, E.; McMurray, B.; Maguire, E.A.; Billig, A.J.; Sedley, W. How can hearing loss cause dementia? Neuron 2020, 108, 401–412. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Report on Hearing; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Danish Health and Medicines Authority, 2021. Available online: https://www.esundhed.dk/Emner/Patienter-og-sygehuse/MitSygehusvalgProfessionel?treatment_ids=336&organizationGroupId=undefined®ionId=1,2,3,4,5&postalFrom$=$undefined (accessed on 1 April 2021).
- Sidiras, C.; Sanchez-Lopez, R.; Pedersen, E.R.; Sørensen, C.B.; Nielsen, J.; Schmidt, J.H. User-Operated Audiometry Project (UAud)—Introducing an Automated User-Operated System for Audiometric Testing into Everyday Clinic Practice. Front. Digit. Health 2021, 3, 724748. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, C.; Pedersen, E.R.; Laugesen, S.; Sanchez-Lopez, R.; Nielsen, J.; Sørensen, C.B.; Sidiras, C.; Pedersen, R.G.; Schmidt, J.H. A validation of the UAud system for user-operated audiometry testing in a clinical setting: A study protocol for a blinded randomised controlled trial. BMJ Open 2023, 13, e065777. [Google Scholar] [CrossRef]
- Behar, A. Audiometric Tests without Booths. Int. J. Environ. Res. Public Health 2021, 18, 3073. [Google Scholar] [CrossRef]
- Sørensen, C.B.; Pedersen, R.G.; Nielsen, J.; Sidiras, C.; Schmidt, J.H.; Pedersen, E.R. User-operated audiometry – an evaluation of expert vs. non-expert headphone placement. Int. J. Audiol. 2022, 18, 1–8. [Google Scholar] [CrossRef]
- Margolis, R.H.; Saly, G.L.; Wilson, R.H. Ambient noise monitoring during pure-tone audiometry. J. Am. Acad. Audiol. 2022, 33, 45–56. [Google Scholar] [CrossRef] [PubMed]
- ANSI S3.1-1999; Maximum Permissible Ambient Noise Levels for Audiometric Test Rooms. American National Standards Institute: New York, NY, USA, 1999.
- 8231-1; Acoustics—Audiometric Test Methods. ISO: London, UK, 2010.
- British Society of Audiology. Practice Guidance Assessment Guidelines for the Distraction Test of Hearing. 2018. Available online: https://www.thebsa.org.uk/wp-content/uploads/2003/08/Practice-Guidance-Distraction-Test-for-Hearing-Final-copy-August-2018.pdf (accessed on 4 September 2019).
- Frank, T.; Williams, D.L. Ambient noise levels in audiometric test rooms used for clinical audiometry. Ear Hear. 1993, 14, 414–422. [Google Scholar] [CrossRef]
- Kim, K.S.; Choi, Y.H.; Won, Y.L.; Kang, S.K. Ambient Noise Levels in the Audiometric Test Rooms Used for Special Periodic Health Examination. Korean J. Occup. Environ. Med. 2004, 16, 316–328. [Google Scholar] [CrossRef]
- Coles, R.R.A. A noise-attenuating enclosure for audiometer earphones. Occup. Environ. Med. 1967, 24, 41–51. [Google Scholar] [CrossRef]
- Bromwich, M.A.; Parsa, V.; Lanthier, N.; Yoo, J.; Parnes, L.S. Active noise reduction audiometry: A prospective analysis of a new approach to noise management in audiometric testing. Laryngoscope 2008, 118, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Maclennan-Smith, F.; Swanepoel, D.W.; Hall, J.W., III. Validity of diagnostic pure-tone audiometry without a sound-treated environment in older adults. Int. J. Audiol. 2013, 52, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, D.W.; Maclennan-Smith, F.; Hall, J.W. Diagnostic pure-tone audiometry in schools: Mobile testing without a sound-treated environment. J. Am. Acad. Audiol. 2013, 24, 992–1000. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, D.W.; Matthysen, C.; Eikelboom, R.H.; Clark, J.L.; Hall, J.W. Pure-tone audiometry outside a sound booth using earphone attenuation, integrated noise monitoring, and automation. Int. J. Audiol. 2015, 54, 777–785. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.G.; Brady, M.; Earl, B.R.; Scheifele, P.M.; Snyder, L.; Clark, S.D. Use of noise cancellation earphones in out-of-booth audiometric evaluations. Int. J. Audiol. 2017, 56, 989–996. [Google Scholar] [CrossRef]
- Wong, T.W.; Yu, T.S.; Chen, W.Q.; Chiu, Y.L.; Wong, C.N.; Wong, A.H.S. Agreement between hearing thresholds measured in non-soundproof work environments and a soundproof booth. Occup. Environ. Med. 2003, 60, 667–671. [Google Scholar] [CrossRef]
- Storey, K.K.; Muñoz, K.; Nelson, L.; Larsen, J.; White, K. Ambient noise impact on accuracy of automated hearing assessment. Int. J. Audiol. 2014, 53, 730–736. [Google Scholar] [CrossRef]
- Chang, C.-Y.; Li, S.-T. Active noise control in headsets by using a low-cost microcontroller. IEEE Trans. Ind. Electron. 2010, 58, 1936–1942. [Google Scholar] [CrossRef]
- Wise, S.; Leventhall, G. Active noise control as a solution to low frequency noise problems. J. Low Freq. Noise Vib. Act. Control. 2010, 29, 129–137. [Google Scholar] [CrossRef]
- Saliba, J.; Al-Reefi, M.; Carriere, J.S.; Verma, N.; Provencal, C.; Rappaport, J.M. Accuracy of mobile-based audiometry in the evaluation of hearing loss in quiet and noisy environments. Otolaryngol. Head Neck Surg. 2017, 156, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, D.W.; Mngemane, S.; Molemong, S.; Mkwanazi, H.; Tutshini, S. Hearing assessment-reliability, accuracy, and efficiency of automated audiometry. Telemed. J. E Health 2010, 16, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Du, B.; Liu, B.; Fu, X.; Wang, Y. Clinical comparison of two automated audiometry procedures. Front. Neurosci. 2022, 16, 1011016. [Google Scholar] [CrossRef] [PubMed]



| Location | Room Number | Floor | Area (Approximately) | Retest | Quasi-Constant Violations |
|---|---|---|---|---|---|
| Audiology clinic, OUH | 1–13 | 3rd | ~5–10 m2 | Yes, 9 rooms | Absent |
| Private ENT clinic | 14 and 15 | ground | ~5–10 m2 | No | Absent |
| SDU hospital | 16 | ground | ~5–10 m2 | No | Absent |
| SDU library | 17 | 1st | >50 m2 | No No | Present |
| 18 | 2nd | ||||
| Odense public library | 19 | 1st | >50 m2 | No No | Present |
| 20 | 2nd | ||||
| TOTAL | 20 | 9 | Absent in 16 | ||
| Present in 4 |
| Most Frequently Violated Frequency Band | Rooms | N of Rooms |
|---|---|---|
| 200 Hz | 1, 3, 5, 9, 10, 11, 12, 13 | 9 |
| 250 Hz | 2, 4, 6, 15 | 4 |
| 315 Hz | 7, 8 | 2 |
| No violations | 14 | 1 |
| TOTAL | 16 |
| Room | Most Frequently Violated Frequency Band | Vn10 | Median (max) Vmag | ||||
|---|---|---|---|---|---|---|---|
| TEST | RETEST | Dif | TEST | RETEST | Dif | ||
| Room 1 | 200 Hz | 16 | 1 | 15 | 2.9 (20.1) | 0.4 (0.4) | 2.5 (19.7) |
| Room 2 | 250 Hz | 11 | 25 | 14 | 0.6 (3.7) | 2.2 (18.4) | 1.6 (14.7) |
| Room 4 | 200 Hz | 0 | 49 | 49 | 0 (0) | 1 (3.9) | 1 (3.9) |
| Room 5 | 200 Hz | 1 | 5 | 4 | 0.7 (0.7) | 3.1 (4.8) | 2.4 (4.1) |
| Room 6 | 250 Hz | 86 | 12 | 74 | 1.9 (7.5) | 2.8 (10.7) | 0.9 (3.2) |
| Room 7 | 200 Hz | 4 | 15 | 11 | 6.5 (8.5) | 1 (3.2) | 5.5 (5.3) |
| Room 10 | 250 Hz | 2 | 21 | 19 | 4.3 (6.9) | 2.2 (9.6) | 2.1 (2.7) |
| Room 11 | 200 Hz | 5 | 3 | 2 | 2.3 (3.4) | 0.5 (1.7) | 1.8 (1.7) |
| Room 12 | 250 Hz | 1 | 3 | 2 | 5.6 (5.6) | 3.9 (5.4) | 1.7 (0.2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sidiras, C.; Nielsen, J.; Sørensen, C.B.; Schmidt, J.H.; Pedersen, R.G.; Pedersen, E.R. Ambient Noise in Candidate Rooms for User-Operated Audiometry. Healthcare 2023, 11, 889. https://doi.org/10.3390/healthcare11060889
Sidiras C, Nielsen J, Sørensen CB, Schmidt JH, Pedersen RG, Pedersen ER. Ambient Noise in Candidate Rooms for User-Operated Audiometry. Healthcare. 2023; 11(6):889. https://doi.org/10.3390/healthcare11060889
Chicago/Turabian StyleSidiras, Christos, Jacob Nielsen, Chris Bang Sørensen, Jesper Hvass Schmidt, René Gyldenlund Pedersen, and Ellen Raben Pedersen. 2023. "Ambient Noise in Candidate Rooms for User-Operated Audiometry" Healthcare 11, no. 6: 889. https://doi.org/10.3390/healthcare11060889
APA StyleSidiras, C., Nielsen, J., Sørensen, C. B., Schmidt, J. H., Pedersen, R. G., & Pedersen, E. R. (2023). Ambient Noise in Candidate Rooms for User-Operated Audiometry. Healthcare, 11(6), 889. https://doi.org/10.3390/healthcare11060889






