Predicting Disability Using a Nomogram of the Tilburg Frailty Indicator (TFI)
Abstract
:1. Introduction
2. Methods
2.1. Study Population and Data Collection
2.2. Measures
2.2.1. Groningen Activity Restriction Scale (GARS)
2.2.2. Frailty
2.3. Statistical Analysis
2.4. Ethical Considerations
3. Results
3.1. Characteristics of the Participants
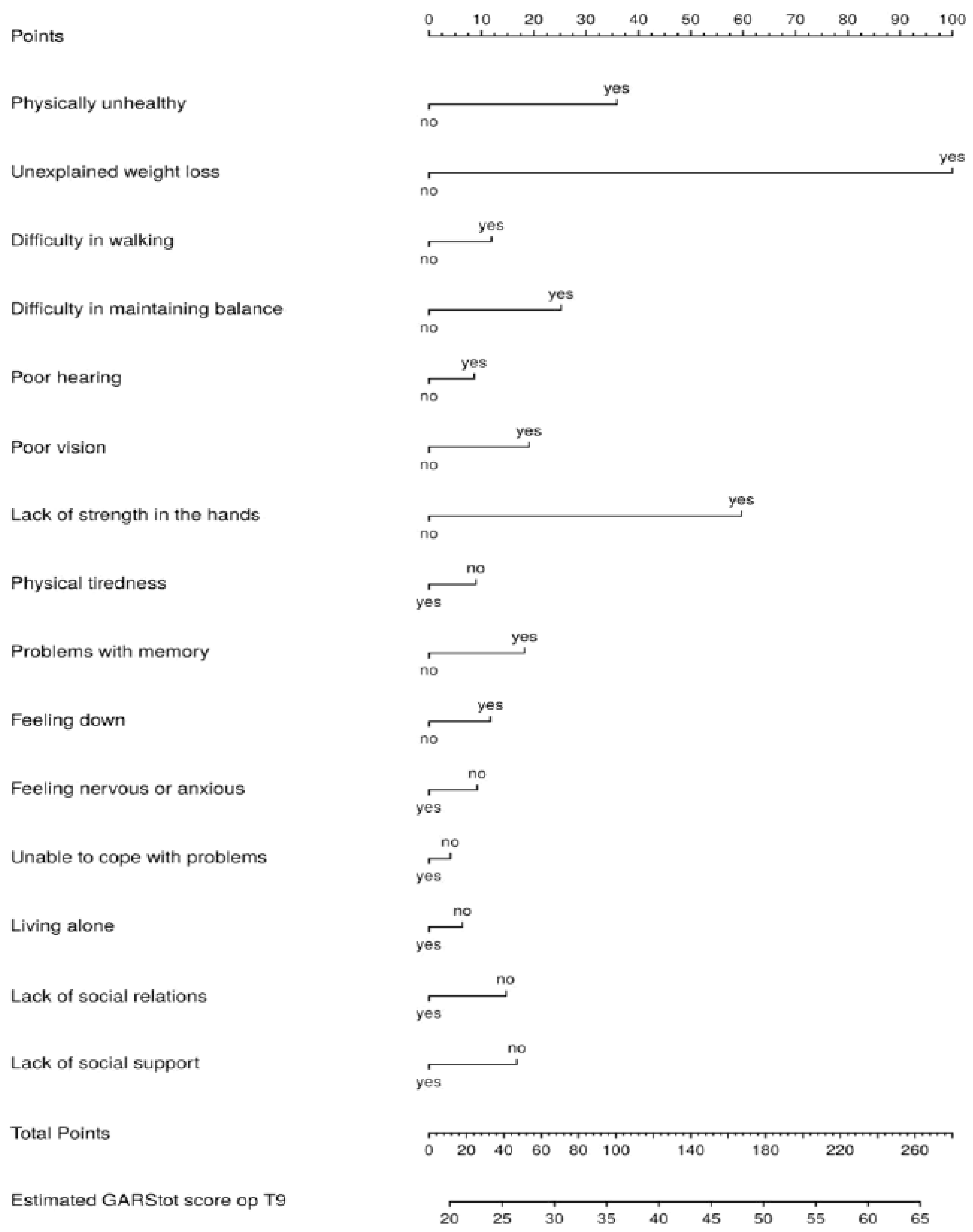
3.2. Prediction of Total Disability
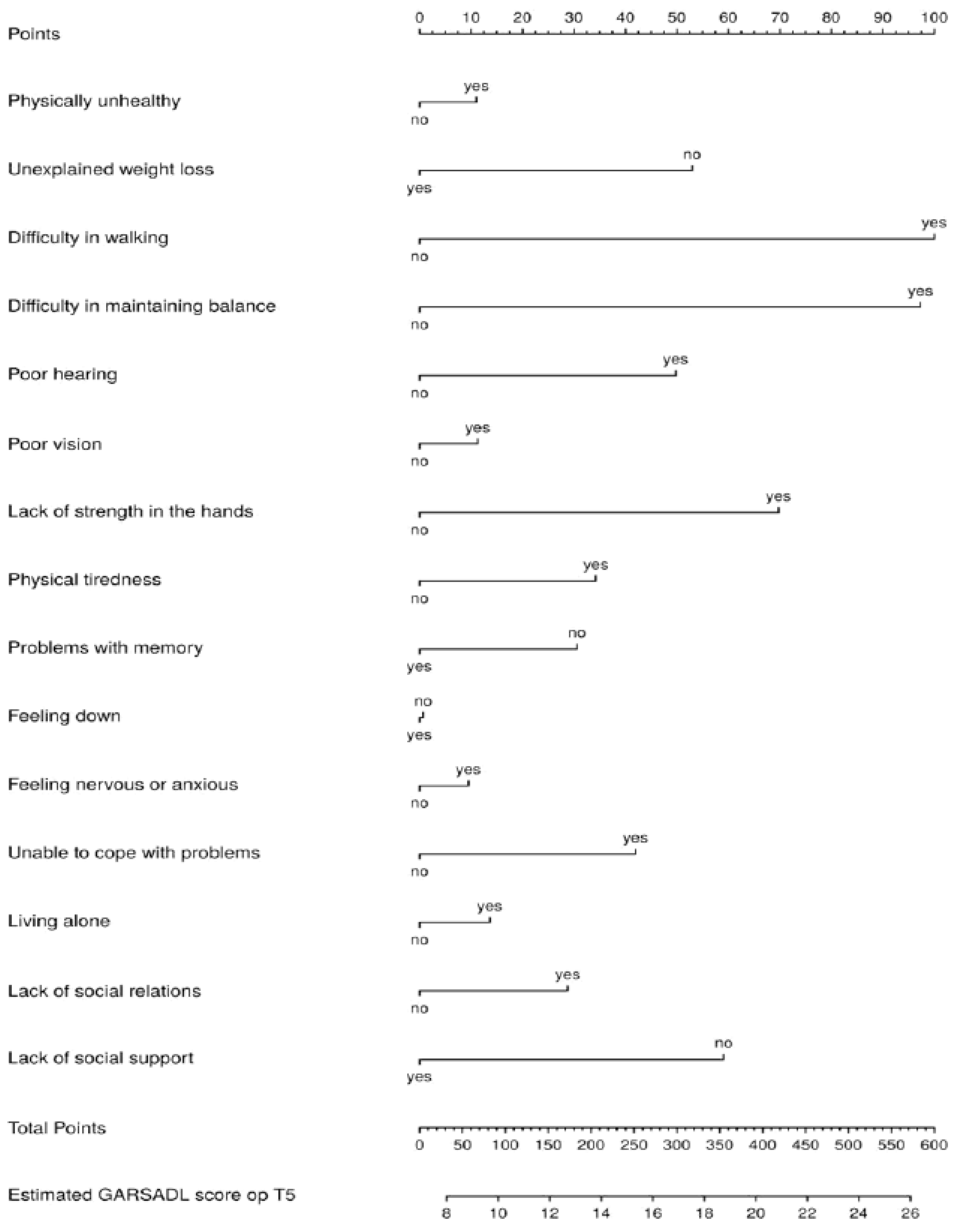
3.3. Prediction of ADL Disability
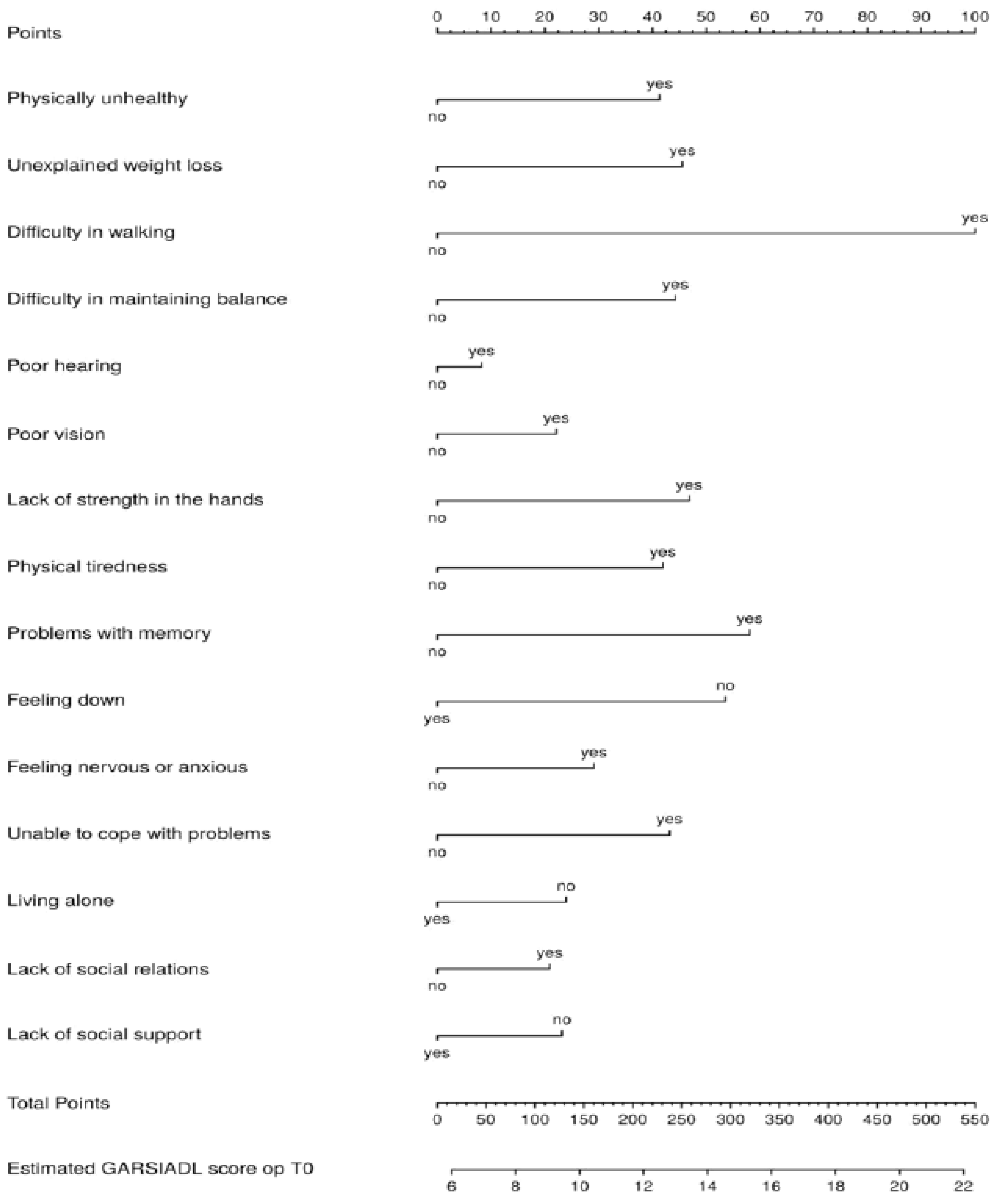
3.4. Prediction of IADL Disability
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A






References
- Kraus, L.; Lauer, E.; Coleman, R.; Houtenville, A. 2017 Disability Statistics Annual Report; University of New Hampshire: Durham, NH, USA, 2018. [Google Scholar]
- World Health Organization. International Classification of Functioning, Disability and Health (ICF); World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Tas, U.; Verhagen, A.P.; Bierma-Zeinstra, S.M.; Hofman, A.; Odding, E.; Pols, H.A.; Koes, B.W. Incidence and risk factors of disability in the elderly: The Rotterdam Study. Prev. Med. 2007, 44, 272–278. [Google Scholar] [CrossRef]
- Tas, U.; Verhagen, A.P.; Bierma-Zeinstra, S.M.; Odding, E.; Koes, B.W. Prognostic factors of disability in older people: A systematic review. Br. J. Gen. Pract. 2007, 57, 319–323. [Google Scholar] [PubMed]
- Kempen, G.I.; Miedema, I.; Ormel, J.; Molenaar, W. The assessment of disability with the Groningen Activity Restriction Scale. Conceptual framework and psychometric properties. Soc. Sci. Med. 1996, 43, 1601–1610. [Google Scholar] [CrossRef] [PubMed]
- Suurmeijer, T.P.; Doeglas, D.M.; Moum, T.; Briançon, S.; Krol, B.; Sanderman, R.; Guillemin, F.; Bjelle, A.; van den Heuvel, W.J. The Groningen Activity Restriction Scale for measuring disability: Its utility in international comparisons. Am. J. Public Health 1994, 84, 1270–1273. [Google Scholar] [CrossRef]
- Hardy, S.E.; Dubin, J.A.; Holford, T.R.; Gill, T.M. Transitions between states of disability and independence among older persons. Am. J. Epidemiol. 2005, 161, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.H.; Weiss, D.; Sourial, N.; Karunananthan, S.; Quail, J.M.; Wolfson, C.; Bergman, H. Frailty and its association with disability and comorbidity in a community-dwelling sample of seniors in Montreal: A cross-sectional study. Aging Clin. Exp. Res. 2010, 22, 54–62. [Google Scholar] [CrossRef]
- Ćwirlej-Sozańska, A.; Wiśniowska-Szurlej, A.; Wilmowska-Pietruszyńska, A.; Sozański, B. Determinants of ADL and IADL disability in older adults in southeastern Poland. BMC Geriatr. 2019, 19, 297. [Google Scholar] [CrossRef]
- Gobbens, R.J. Associations of ADL and IADL disability with physical and mental dimensions of quality of life in people aged 75 years and older. PeerJ 2018, 6, e5425. [Google Scholar] [CrossRef] [PubMed]
- Cheung, J.T.K.; Yu, R.; Wu, Z.; Wong, S.Y.S.; Woo, J. Geriatric syndromes, multimorbidity, and disability overlap and increase healthcare use among older Chinese. BMC Geriatr. 2018, 18, 147. [Google Scholar] [CrossRef]
- Fried, L.P.; Ferrucci, L.; Darer, J.; Williamson, J.D.; Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, 255–263. [Google Scholar] [CrossRef]
- Akosile, C.O.; Mgbeojedo, U.G.; Maruf, F.A.; Okoye, E.C.; Umeonwuka, I.C.; Ogunniyi, A. Depression, functional disability and quality of life among Nigerian older adults: Prevalences and relationships. Arch. Gerontol. Geriatr. 2018, 74, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Gobbens, R.J.J.; van der Ploeg, T. The Prediction of Mortality by Disability Among Dutch Community-Dwelling Older People. Clin. Interv. Aging 2020, 15, 1897–1906. [Google Scholar] [CrossRef] [PubMed]
- Hennessy, S.; Kurichi, J.E.; Pan, Q.; Streim, J.E.; Bogner, H.R.; Xie, D.; Stineman, M.G. Disability Stage is an Independent Risk Factor for Mortality in Medicare Beneficiaries Aged 65 Years and Older. PM&R J. Inj. Funct. Rehabil. 2015, 7, 1215–1225. [Google Scholar] [CrossRef]
- Nascimento, C.M.; Oliveira, C.; Firmo, J.O.A.; Lima-Costa, M.F.; Peixoto, S.V. Prognostic value of disability on mortality: 15-year follow-up of the Bambui cohort study of aging. Arch. Gerontol. Geriatr. 2018, 74, 112–117. [Google Scholar] [CrossRef]
- Picavet, H.S.; Hoeymans, N. Physical disability in The Netherlands: Prevalence, risk groups and time trends. Public Health 2002, 116, 231–237. [Google Scholar] [CrossRef]
- Chang, S.F.; Cheng, C.L.; Lin, H.C. Frail Phenotype and Disability Prediction in Community-Dwelling Older People: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. J. Nurs. Res. 2019, 27, e28. [Google Scholar] [CrossRef]
- Kojima, G. Frailty as a predictor of disabilities among community-dwelling older people: A systematic review and meta-analysis. Disabil. Rehabil. 2017, 39, 1897–1908. [Google Scholar] [CrossRef]
- Vermeulen, J.; Neyens, J.C.; van Rossum, E.; Spreeuwenberg, M.D.; de Witte, L.P. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: A systematic review. BMC Geriatr. 2011, 11, 33. [Google Scholar] [CrossRef]
- Gobbens, R.J.; Luijkx, K.G.; Wijnen-Sponselee, M.T.; Schols, J.M. Toward a conceptual definition of frail community dwelling older people. Nurs. Outlook 2010, 58, 76–86. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Mitnitski, A.B.; Mogilner, A.J.; Rockwood, K. Accumulation of deficits as a proxy measure of aging. Sci. World J. 2001, 1, 323–336. [Google Scholar] [CrossRef]
- Gobbens, R.J.; van Assen, M.A.; Luijkx, K.G.; Wijnen-Sponselee, M.T.; Schols, J.M. The Tilburg Frailty Indicator: Psychometric properties. J. Am. Med. Dir. Assoc. 2010, 11, 344–355. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Gobbens, R.J.; van Assen, M.A.; Luijkx, K.G.; Schols, J.M. The predictive validity of the Tilburg Frailty Indicator: Disability, health care utilization, and quality of life in a population at risk. Gerontologist 2012, 52, 619–631. [Google Scholar] [CrossRef] [PubMed]
- Kempen, G.I.; Suurmeijer, T.P. The development of a hierarchical polychotomous ADL-IADL scale for noninstitutionalized elders. Gerontologist 1990, 30, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Ormel, J.; Rijsdijk, F.V.; Sullivan, M.; van Sonderen, E.; Kempen, G.I. Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. J. Gerontol. B Psychol. Sci. Soc. Sci. 2002, 57, P338–P347. [Google Scholar] [CrossRef] [PubMed]
- Gobbens, R.J.; Uchmanowicz, I. Assessing Frailty with the Tilburg Frailty Indicator (TFI): A Review of Reliability and Validity. Clin. Interv. Aging 2021, 16, 863–875. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing. Available online: https://www.R-project.org/ (accessed on 14 October 2022).
- Central Committee on Research Involving Human Subjects. Available online: https://english.ccmo.nl/investigators/legal-framework-for-medical-scientic-research/your-research-is-it-subject-to-the-wmo-or-not (accessed on 15 January 2008).
- den Ouden, M.E.; Schuurmans, M.J.; Arts, I.E.; van der Schouw, Y.T. Physical performance characteristics related to disability in older persons: A systematic review. Maturitas 2011, 69, 208–219. [Google Scholar] [CrossRef]
- Neumann, J.T.; Thao, L.T.P.; Murray, A.M.; Callander, E.; Carr, P.R.; Nelson, M.R.; Wolfe, R.; Woods, R.L.; Reid, C.M.; Shah, R.C.; et al. Prediction of disability-free survival in healthy older people. Geroscience 2022, 44, 1641–1655. [Google Scholar] [CrossRef]
- Gobbens, R.J.; van Assen, M.A. The Prediction of ADL and IADL Disability Using Six Physical Indicators of Frailty: A Longitudinal Study in the Netherlands. Curr. Gerontol. Geriatr. Res. 2014, 2014, 358137. [Google Scholar] [CrossRef]
- Gobbens, R.J.; van Assen, M.A.; Schalk, M.J. The prediction of disability by self-reported physical frailty components of the Tilburg Frailty Indicator (TFI). Arch. Gerontol. Geriatr. 2014, 59, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Payette, H.; Coulombe, C.; Boutier, V.; Gray-Donald, K. Nutrition risk factors for institutionalization in a free-living functionally dependent elderly population. J. Clin. Epidemiol. 2000, 53, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Gaddey, H.L.; Holder, K.K. Unintentional Weight Loss in Older Adults. Am. Fam. Physician 2021, 104, 34–40. [Google Scholar]
- Alibhai, S.M.; Greenwood, C.; Payette, H. An approach to the management of unintentional weight loss in elderly people. CMAJ 2005, 172, 773–780. [Google Scholar] [CrossRef] [PubMed]
- Soysal, P.; Hurst, C.; Demurtas, J.; Firth, J.; Howden, R.; Yang, L.; Tully, M.A.; Koyanagi, A.; Ilie, P.C.; López-Sánchez, G.F.; et al. Handgrip strength and health outcomes: Umbrella review of systematic reviews with meta-analyses of observational studies. J. Sport Health Sci. 2021, 10, 290–295. [Google Scholar] [CrossRef]
- Shimada, H.; Makizako, H.; Doi, T.; Tsutsumimoto, K.; Lee, S.; Suzuki, T. Cognitive Impairment and Disability in Older Japanese Adults. PLoS ONE 2016, 11, e0158720. [Google Scholar] [CrossRef] [PubMed]
- St John, P.D.; Tyas, S.L.; Montgomery, P.R. Cognition, even in the normal range, predicts disability: Cross-sectional and prospective analyses of a population-based sample. Int. J. Geriatr. Psychiatry 2015, 30, 1008–1016. [Google Scholar] [CrossRef]
- Gobbens, R.J.J.; van Assen, M.; Augustijn, H.; Goumans, M.; van der Ploeg, T. Prediction of Mortality by the Tilburg Frailty Indicator (TFI). J. Am. Med. Dir. Assoc. 2021, 22, e601–e607. [Google Scholar] [CrossRef] [PubMed]
- Katz, S.; Downs, T.D.; Cash, H.R.; Grotz, R.C. Progress in development of the index of ADL. Gerontologist 1970, 10, 20–30. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
| Characteristics | T0 | T5 | T9 | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Gender | ||||||
| Man | 207 | 43.2 | 76 | 47.5 | 37 | 48.1 |
| Woman | 272 | 56.8 | 84 | 52.5 | 40 | 51.9 |
| Marital status | ||||||
| Married or cohabiting | 238 | 49.8 | 71 | 44.4 | 30 | 39.0 |
| Not married | 45 | 9.4 | 12 | 7.5 | 6 | 7.8 |
| Divorced | 15 | 3.1 | 9 | 5.6 | 5 | 6.5 |
| Widowed | 180 | 37.7 | 68 | 42.5 | 36 | 46.8 |
| Country of birth | ||||||
| The Netherlands | 461 | 96.6 | 159 | 99.4 | 75 | 97.4 |
| Other | 16 | 3.4 | 1 | 0.6 | 2 | 2.6 |
| Educational level | ||||||
| No or primary | 181 | 38.1 | 51 | 31.9 | 20 | 26.0 |
| Secondary education | 221 | 46.5 | 75 | 46.9 | 40 | 51.9 |
| Higher education | 73 | 15.4 | 34 | 21.2 | 17 | 22.1 |
| Monthly income in Euro * | ||||||
| Less than 600 | 12 | 2.7 | 2 | 1.3 | 2 | 2.7 |
| 601–900 | 71 | 16.2 | 6 | 4.0 | 3 | 4.1 |
| 901–1200 | 106 | 24.2 | 33 | 22.1 | 8 | 11.0 |
| 1201–1500 | 57 | 13.0 | 21 | 14.1 | 14 | 19.2 |
| 1501–1800 | 67 | 15.3 | 23 | 15.4 | 13 | 17.8 |
| 1801–2100 | 48 | 11.0 | 25 | 16.8 | 8 | 11.0 |
| 2101 or more | 77 | 17.6 | 39 | 26.2 | 25 | 34.2 |
| Continuous variables (mean, sd) | ||||||
| Age | 80.3 | 3.8 | 84.0 | 3.2 | 87.4 | 2.9 |
| Frailty score | 4.7 | 3.0 | 5.0 | 3.0 | 5.8 | 3.0 |
| Disability total | 26.7 | 9.6 | 28.7 | 10.1 | 33.3 | 12.5 |
| ADL disability | 14.6 | 4.8 | 15.6 | 5.5 | 17.8 | 6.8 |
| IADL disability | 12.2 | 5.4 | 13.1 | 5.5 | 15.5 | 6.6 |
| T0–T5 | T5–T9 | T0–T9 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Chi-square | df | p-value | Chi-square | df | p-value | Chi-square | df | p-value | |
| Gender | 1:197 | 1 | 0:274 | 0:009 | 1 | 0:923 | 0:734 | 1 | 0:392 |
| Marital status | 5:715 | 3 | 0:126 | 0:948 | 3 | 0:814 | 6:484 | 3 | 0:090 |
| Country of birth | 3:677 | 1 | 0:055 | 4:823 | 1 | 0:028 | 0:136 | 1 | 0:712 |
| Educational level | 5:235 | 2 | 0:073 | 1:289 | 2 | 0:525 | 5:716 | 2 | 0:057 |
| Monthly income in euro | 25:966 | 6 | 0:000 | 10:085 | 6 | 0:121 | 25:850 | 6 | 0:000 |
| Total | ||
|---|---|---|
| n | % | |
| Physically unhealthy | ||
| no | 334 | 70.8 |
| yes | 138 | 29.2 |
| Unexplained weight loss | ||
| no | 442 | 92.5 |
| yes | 36 | 7.5 |
| Difficulty in walking | ||
| no | 248 | 51.9 |
| yes | 230 | 48.1 |
| Difficulty in maintaining balance | ||
| no | 308 | 65.0 |
| yes | 166 | 35.0 |
| Poor hearing | ||
| no | 301 | 63.4 |
| yes | 174 | 36.6 |
| Poor vision | ||
| no | 372 | 78.6 |
| yes | 101 | 21.4 |
| Lack of strength in the hands | ||
| no | 315 | 65.8 |
| yes | 164 | 34.2 |
| Physical tiredness | ||
| no | 261 | 54.6 |
| yes | 217 | 45.4 |
| Problems with memory | ||
| no | 432 | 90.4 |
| yes | 46 | 9.6 |
| Feeling down | ||
| no | 286 | 59.8 |
| yes | 192 | 40.2 |
| Feeling nervous or anxious | ||
| no | 330 | 69.0 |
| yes | 148 | 31.0 |
| Unable to cope with problems | ||
| no | 401 | 85.0 |
| yes | 71 | 15.0 |
| Living alone | ||
| no | 250 | 52.2 |
| yes | 229 | 47.8 |
| Lack of social relations | ||
| no | 196 | 41.0 |
| yes | 282 | 59.0 |
| Lack of social support | ||
| no | 398 | 83.6 |
| yes | 78 | 16.4 |
| T0 | T5 | T9 | |
|---|---|---|---|
| Performance model | |||
| Rsq | 0.45 | 0.53 | 0.45 |
| Predictors | |||
| Physically unhealthy | 57 | 25 | 36 |
| Unexplained weight loss | 56 | 56 | 100 |
| Difficulty in walking | 100 | 84 | 12 |
| Difficulty in maintaining balance | 47 | 100 | 25 |
| Poor hearing | 3 | 60 | 9 |
| Poor vision | 14 | 24 | 19 |
| Lack of strength in the hands | 35 | 77 | 60 |
| Physical tiredness | 37 | 52 | 0 |
| Problems with memory | 35 | 7 | 18 |
| Feeling down | 0 | 9 | 12 |
| Feeling nervous or anxious | 28 | 6 | 0 |
| Unable to cope with problems | 30 | 34 | 0 |
| Living alone | 0 | 0 | 0 |
| Lack of social relations | 19 | 13 | 0 |
| Lack of social support | 0 | 0 | 0 |
| T0 | T5 | T9 | |
|---|---|---|---|
| Performance model | |||
| Rsq | 0.43 | 0.52 | 0.41 |
| Predictors | |||
| Physically unhealthy | 70 | 11 | 34 |
| Unexplained weight loss | 79 | 0 | 100 |
| Difficulty in walking | 100 | 100 | 28 |
| Difficulty in maintaining balance | 49 | 97 | 32 |
| Poor hearing | 0 | 50 | 0 |
| Poor vision | 4 | 11 | 5 |
| Lack of strength in the hands | 36 | 70 | 36 |
| Physical tiredness | 37 | 34 | 0 |
| Problems with memory | 5 | 0 | 0 |
| Feeling down | 0 | 0 | 25 |
| Feeling nervous or anxious | 30 | 10 | 0 |
| Unable to cope with problems | 10 | 42 | 0 |
| Living alone | 22 | 14 | 0 |
| Lack of social relations | 11 | 29 | 0 |
| Lack of social support | 0 | 0 | 0 |
| T0 | T5 | T9 | |
|---|---|---|---|
| Performance model | |||
| Rsq | 0.39 | 0.44 | 0.44 |
| Predictors | |||
| Physically unhealthy | 41 | 21 | 39 |
| Unexplained weight loss | 46 | 100 | 100 |
| Difficulty in walking | 100 | 31 | 0 |
| Difficulty in maintaining balance | 44 | 51 | 16 |
| Poor hearing | 8 | 36 | 22 |
| Poor vision | 22 | 20 | 38 |
| Lack of strength in the hands | 47 | 43 | 93 |
| Physical tiredness | 42 | 37 | 0 |
| Problems with memory | 58 | 28 | 84 |
| Feeling down | 0 | 11 | 0 |
| Feeling nervous or anxious | 29 | 1 | 1 |
| Unable to cope with problems | 43 | 12 | 0 |
| Living alone | 0 | 0 | 0 |
| Lack of social relations | 21 | 0 | 0 |
| Lack of social support | 0 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gobbens, R.J.; Santiago, L.M.; Uchmanowicz, I.; van der Ploeg, T. Predicting Disability Using a Nomogram of the Tilburg Frailty Indicator (TFI). Healthcare 2023, 11, 1150. https://doi.org/10.3390/healthcare11081150
Gobbens RJ, Santiago LM, Uchmanowicz I, van der Ploeg T. Predicting Disability Using a Nomogram of the Tilburg Frailty Indicator (TFI). Healthcare. 2023; 11(8):1150. https://doi.org/10.3390/healthcare11081150
Chicago/Turabian StyleGobbens, Robbert J., Livia M. Santiago, Izabella Uchmanowicz, and Tjeerd van der Ploeg. 2023. "Predicting Disability Using a Nomogram of the Tilburg Frailty Indicator (TFI)" Healthcare 11, no. 8: 1150. https://doi.org/10.3390/healthcare11081150
APA StyleGobbens, R. J., Santiago, L. M., Uchmanowicz, I., & van der Ploeg, T. (2023). Predicting Disability Using a Nomogram of the Tilburg Frailty Indicator (TFI). Healthcare, 11(8), 1150. https://doi.org/10.3390/healthcare11081150









