Development and Effectiveness of a Rapid Cycle Deliberate Practice Neonatal Resuscitation Simulation Program: A Quasi-Experimental Study
Abstract
1. Introduction
2. Materials and Methods
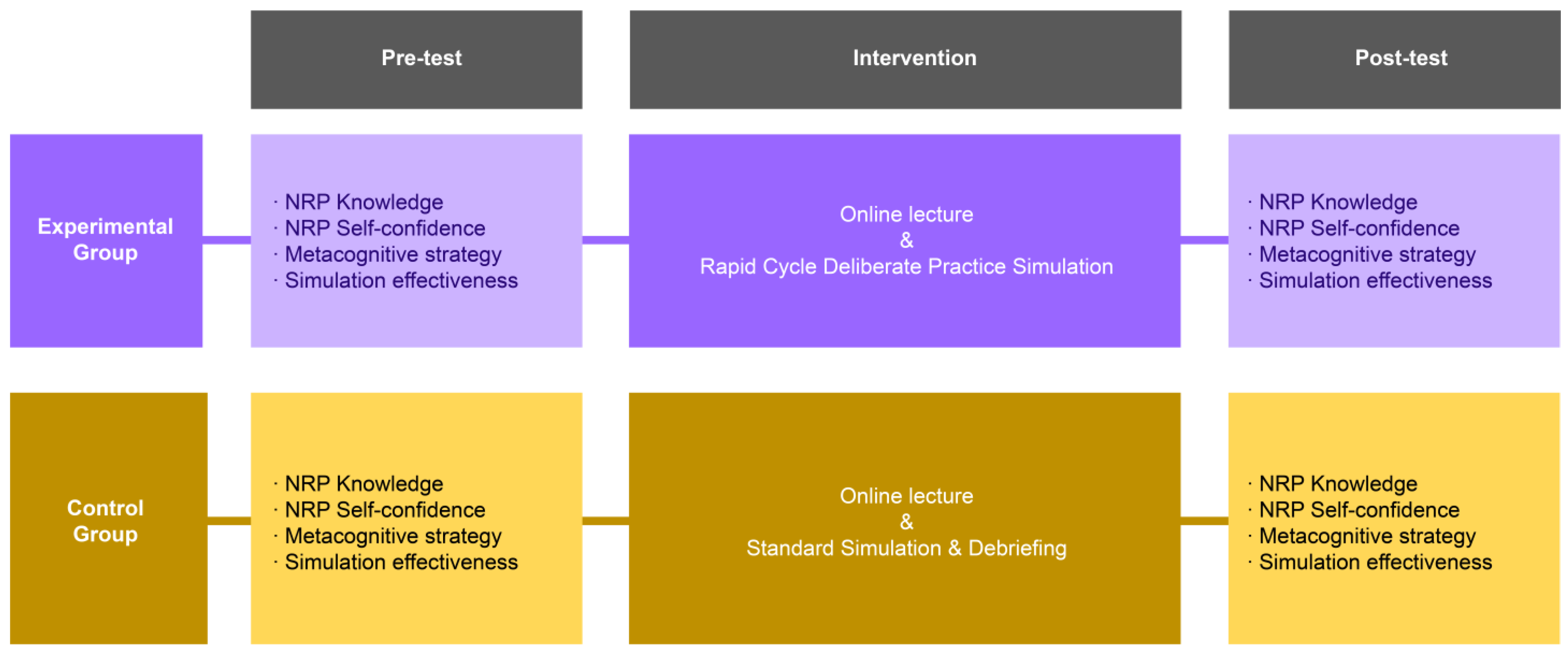
2.1. Research Design
2.2. Participants
2.3. Study Protocol
2.4. Data Collection
2.5. Research Tools
2.5.1. NRP Knowledge
2.5.2. NRP Self-Confidence
2.5.3. Clinical Decision-Making
2.5.4. Simulation Effectiveness
2.6. Data Analysis
3. Results
3.1. Validating the Pre-Homogeneity of Participants’ General Characteristics
3.2. Validating the Effectiveness of RCDP Simulation Based on the Self-Determination Theory Model
4. Discussion
5. Conclusions
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
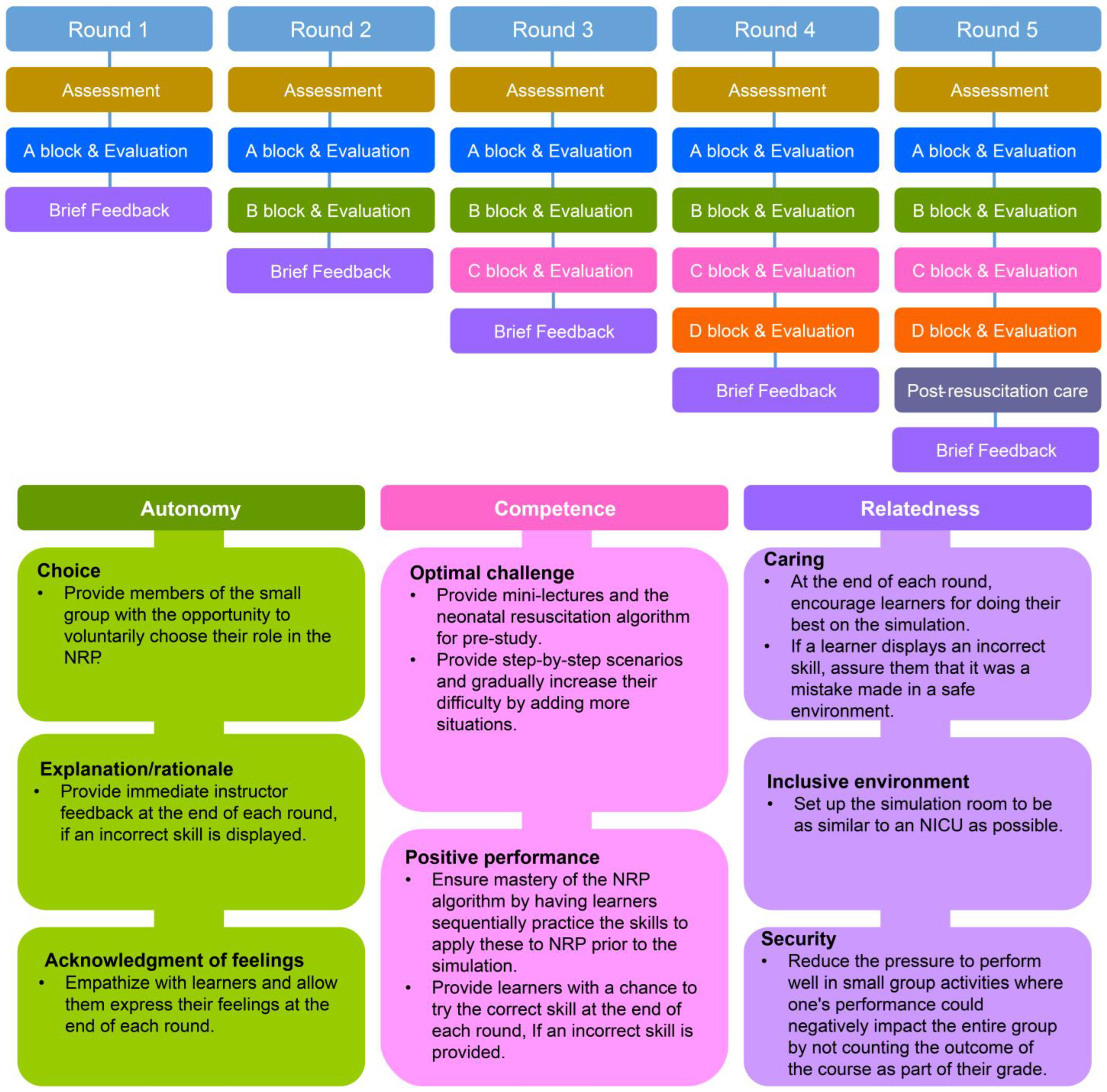
Appendix A. Experimental Group Debriefing Using RCDP
| Methods | □ Individual ■ Group □ Whole □ With video ■ Without video |
| Resources | □ Student simulation worksheet □ Article □ Handout □ Etc. (Self-reflection note) |
| Introduction explanation |
|
| Round 1 |
|
| Round 2 | During Round 2, if the interventions included in Round 1 are performed immaturely or incorrectly, a comment from Round 1 may be added.
|
| Round 3 | During Round 3, if the interventions included in Rounds 1 and 2 are performed immaturely or incorrectly, a comment from Rounds 1 and 2 may be added.
|
| Round 4 | During Round 4, if the interventions included in Rounds 1~3 are performed immaturely or incorrectly, a comment from Rounds 1–3 may be added.
|
| Round 5 | During Round 5, if the interventions included in Rounds 1~4 are performed immaturely or incorrectly, a comment from Rounds 1–4 may be added.
|
| Note. RCDP feedback is provided only when trainees perform incorrect assessments or incorrect or immature interventions in each round. Therefore, the content written is only an example, and the feedback may be edited depending on the situation. | |
Appendix B. Control Group Debriefing Using the PEARLS Model [35]
| Methods | □ Individual □ Group ■ Whole ■ With video □ Without video |
| Resources | □ Student simulation worksheet □ Article □ Handout □ Etc. (Self-reflection note) |
| Introduction explanation |
|
| Reaction |
|
| Description |
|
| Analysis |
|
| Application/Summary |
|
References
- Fogg, N.; Wilson, C.; Trinka, M.; Campell, R.; Thompson, A.; Merritt, L.; Tietze, M.; Prior, M. Transitioning from direct care to virtual clinical experiences during the COVID-19 pandemic. J. Prof. Nurs. 2020, 36, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Kwak, K.H.; Choi, H.M.; Hwang, S.W. The development and application of the alternative clinical practicum program for the delivery room and the newborn nursery in the non-face-to-face distance education environment. J. Korean Nurs. Res. 2021, 5, 49–61. [Google Scholar] [CrossRef]
- Mileder, L.P.; Bereiter, M.; Wegscheider, T. Telesimulation as a modality for neonatal resuscitation training. Med. Educ. Online 2021, 26, 1892017. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.H.; Kwak, Y.K. Differences of tradition and combining nursing process in simulation practice: Problem solving, critical thinking and clinical competency. AJMAHS 2016, 6, 125–134. [Google Scholar] [CrossRef]
- Capogna, G.; Ingrassia, P.L.; Capogna, E.; Bernardini, M.; Valteroni, E.; Pietrabissa, G.; Nardone, G. Essentials of debriefing. In Strategic Debriefing for Advanced Simulation; Springer: Cham, Switzerland, 2002; pp. 27–41. [Google Scholar] [CrossRef]
- Kandasamy, S.; Hua, T.K.; Sultan, F.M.M. The impact of a debriefing strategy in online ESL classrooms. Int. J. Learn. Teach. Educ. Res. 2002, 21, 247–262. [Google Scholar] [CrossRef]
- Nagle, A.; Foli, K. Student-centered reflection during debriefing: A mixed-methods study. Nurse Educ. 2022, 47, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Patricia, K.; Arnold, J.; Lemke, D. Rapid cycle deliberate practice: Application to neonatal resuscitation. MedEdPORTAL J. Teach. Learn. 2017, 13, 10534. [Google Scholar] [CrossRef] [PubMed]
- Blanchard, E.E.; Riesenberg, L.A.; Bergman, L.B.; Brown, M.R.; O’Hagan, E.C.; Patel, S.J.; Carter, T.R. Comparing traditional, immersive simulation with Rapid Cycle Deliberate Practice in postgraduate year 2 anesthesiology residents. Adv. Simul. 2021, 6, 20. [Google Scholar] [CrossRef]
- Taras, J.; Everett, T. Rapid cycle deliberate practice in medical education: A systematic review. Cureus 2017, 9, e1180. [Google Scholar] [CrossRef]
- Hunt, E.A.; Duval-Arnould, J.M.; Chime, N.O.; Jones, K.; Rosen, M.; Hollingsworth, M.; Aksamit, D.; Twilley, M.; Camacho, C.; Nogee, D.P.; et al. Integration of in-hospital cardiac arrest contextual curriculum into a basic life support course: A randomized, controlled simulation study. Resuscitation 2017, 114, 127–132. [Google Scholar] [CrossRef]
- Magee, M.J.; Farkouh-Karoleski, C.; Rosen, T.S. Improvement of immediate performance in neonatal resuscitation through Rapid Cycle Deliberate Practice Training. J. Grad. Med. Educ. 2018, 10, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Gross, I.T.; Abrahan, D.G.; Kumar, A.; Noether, J.; Shilkofski, N.A.; Pell, P.; Bahar-Posey, L. Rapid cycle deliberate practice (RCDP) as a method to improve airway management skills: A randomized controlled simulation study. Cureus 2019, 11, e5546. [Google Scholar] [CrossRef] [PubMed]
- de Castro, L.T.; Coriolano, A.M.; Burckart, K.; Soares, M.B.; Accorsi, T.A.D.; Rosa, V.E.E.; de Santis Andrade Lopes, A.S.; Couto, T.B. Rapid-cycle deliberate practice versus after-event debriefing clinical simulation in cardiopulmonary resuscitation: A cluster randomized trial. Adv. Simul. 2022, 7, 43. [Google Scholar] [CrossRef] [PubMed]
- Deci, E.L.; Ryan, R.M. Intrinsic Motivation and Self-Determination in Human Behavior; Plenum: New York, NY, USA, 1985. [Google Scholar]
- Guay, F. Applying self-determination theory to education: Regulations types, psychological needs, and autonomy supporting behaviors. Can. J. Sch. Psychol. 2021, 37, 75–92. [Google Scholar] [CrossRef]
- Kaplan, H.; Madjar, N. The motivational outcomes of psychological need-support among pre-service teachers: Multicultural and self-determination theory perspectives. Front. Educ. 2017, 2, 42. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. The support of autonomy and the control of behavior. J. Pers. Soc. Psychol. 1987, 53, 1024–1037. [Google Scholar] [CrossRef]
- Ayed, A.; Khalaf, I. The outcomes of integrating high fidelity simulation in nursing education: An integrative review. Open J. Nurs. 2018, 8, 292–302. [Google Scholar] [CrossRef]
- Shin, H.S.; Lee, Y.N.; Rim, D.H. Evaluation of algorithm-based simulation scenario for emergency measures with high-risk newborns presenting with apnea. Child Health Nurs. Res. 2015, 21, 98–106. [Google Scholar] [CrossRef]
- Zaichkin, J.; Kamath-Rayne, B.D.; Weiner, G.T. The NRP 8th edition: Innovation in education. Adv. Neonatal Care 2021, 21, 322–332. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Kim, M.J.; Kim, S.H. Development and effects a simulation-based airway management education program for nurses in a neonatal intensive care unit. Child Health Nurs. Res. 2019, 25, 518–527. [Google Scholar] [CrossRef] [PubMed]
- Page-Cutrara, K.; Turk, M. Impact of pre-briefing on competency performance, clinical judgment and experience in simulation: An experimental study. Nurse Educ. Today 2017, 48, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.Y. Development and effects of simulation-based education program for newborn emergency care. J. Korean Acad. Nurs. 2013, 43, 468–477. [Google Scholar] [CrossRef] [PubMed]
- Cory, M.J.; Colman, N.; McCracken, C.E.; Hebbar, K.B. Rapid cycle deliberate practice versus reflective debriefing for pediatric septic shock training. Pediatr. Crit. Care Med. 2019, 20, 481–489. [Google Scholar] [CrossRef]
- Hazinski, M.F.; Nolan, J.P.; Aickin, R.; Bhanji, F.; Billi, J.E.; Callaway, C.W.; Zideman, D.A. Part 1: Executive summary: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 2015, 132 (Suppl. S1), S2–S39. [Google Scholar] [CrossRef] [PubMed]
- Baek, M.K. Relationship between Level of Autonomy and Clinical Decision-Making in Nursing Scale of ET Nurse. Master’s Thesis, Yonsei University, Seoul, Republic of Korea, 2005. [Google Scholar]
- Jenkins, H.M. A research tool for measuring perceptions of clinical decision-making. J. Prof. Nurs. 1985, 1, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Leighton, K.; Ravert, P.; Mudra, V.; Macintosh, C. Update the simulation effectiveness tool: Item modifications and reevaluation of psychometric properties. Nurs. Educ. Perspect. 2015, 36, 317–323. [Google Scholar] [CrossRef]
- Kim, H.J.; Lee, H.C. Differences in advanced cardiac life support knowledge, confidence, satisfaction, and performance ability of paramedic students according to simulation education methods. Korean J. Emerg. Med. Serv. 2021, 25, 111–125. [Google Scholar] [CrossRef]
- Rosman, S.L.; Nyirasafari, R.; Bwiza, H.M.; Umuhoza, C.; Camp, E.A.; Weiner, D.L.; Rus, M.C. Rapid cycle deliberate practice vs. traditional simulation in resource-limited setting. BMC Med. Educ. 2019, 19, 314. [Google Scholar] [CrossRef]
- Gantt, L.T.; Overton, S.H.; Avery, J.; Swanson, M. Comparison of debriefing mthods and leaning outcomes in human patient simulation. J. Paediatr. Child Health 2018, 17, 7–13. [Google Scholar] [CrossRef]
- Brown, K.M.; Mudd, S.S.; Hunt, E.A.; Perretta, J.S.; Shilkofski, N.A.; Diddle, J.W.; Yurasek, G.; Bembea, M.; Duval-Arnould, J.; McMillan, K.N. A multi-institutional simulation boot camp for pediatric critical care nurse practitioners. Pediatr. Crit. Care Med. 2018, 19, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Eppich, W.; Cheng, A. Promoting excellence and reflective learning in simulation (PEARLS) de-velopment and rationale for a blended approach to health care simulation debriefing. Simul. Healthc. 2015, 10, 106–115. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Categories | Experimental Group (n = 29) | Control Group (n = 28) | χ2 or t | p |
|---|---|---|---|---|---|
| n (%) | n (%) | ||||
| Sex | Male | 9 (31.0) | 9 (32.1) | 0.01 | 0.928 |
| Female | 20 (69.0) | 19 (67.9) | |||
| Major satisfaction | Dissatisfied | 0 (0.0) | 2 (7.1) | 2.37 | 0.305 |
| Neutral | 13 (44.8) | 10 (35.7) | |||
| Very satisfied | 16 (55.2) | 16 (57.1) | |||
| Satisfaction with clinical practice | Neutral | 9 (31.0) | 13 (46.4) | 1.42 | 0.233 |
| Very satisfied | 20 (69.0) | 15 (53.6) | |||
| Satisfaction with simulation training | Neutral | 11 (37.9) | 18 (64.3) | 3.96 | 0.057 |
| Very satisfied | 18 (62.1) | 10 (35.7) | |||
| Demand for simulation training for nursing major | Yes | 28 (96.6) | 27 (96.4) | 0.746 * | |
| No | 1 (3.4) | 1 (3.6) | |||
| NRP knowledge, M (SD) | 9.59 (3.61) | 8.25 (4.01) | 1.32 | 0.191 | |
| NRP self-confidence, M (SD) | 50.17 (9.87) | 47.46 (13.96) | 0.02 | 0.400 | |
| Clinical decision-making skill, M (SD) | 147.86 (16.45) | 141.07 (12.72) | 1.72 | 0.091 | |
| Simulation effectiveness, M (SD) | 44.10 (7.24) | 42.21 (7.91) | 0.94 | 0.351 | |
| Variables | Groups | Pre-Test | Post-Test | Pre-Post Difference | ||
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | t (p) | M (SD) | t (p) | ||
| NRP knowledge | Experimental group | 9.59 (3.61) | 14.24 (3.20) | 2.25 (0.028) | 4.66 (4.37) | 0.38 (0.703) |
| Control group | 8.25 (4.01) | 12.46 (2.73) | 4.21 (4.31) | |||
| NRP self-confidence | Experimental group | 50.17 (9.87) | 65.66 (7.78) | 4.67 (<0.001) | 17.55 (7.86) | 1.45 (0.045) |
| Control group | 47.46 (13.96) | 57.86 (6.70) | 10.39 (17.15) | |||
| Clinical decision-making skill | Experimental group | 147.86 (16.45) | 156.86 (12.37) | 6.03 (<0.001) | 9.00 (12.74) | 3.13 (0.003) |
| Control group | 141.07 (12.72) | 137.57 (11.77) | −3.67 (17.39) | |||
| Simulation effectiveness | Experimental group | 44.10 (7.24) | 52.10 (5.49) | 3.51 (0.001) | 8.00 (6.46) | 1.99 (0.042) |
| Control group | 42.21 (7.91) | 46.61 (6.33) | 4.39 (7.25) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, S.-Y.; Oh, Y.-H. Development and Effectiveness of a Rapid Cycle Deliberate Practice Neonatal Resuscitation Simulation Program: A Quasi-Experimental Study. Healthcare 2024, 12, 104. https://doi.org/10.3390/healthcare12010104
Yang S-Y, Oh Y-H. Development and Effectiveness of a Rapid Cycle Deliberate Practice Neonatal Resuscitation Simulation Program: A Quasi-Experimental Study. Healthcare. 2024; 12(1):104. https://doi.org/10.3390/healthcare12010104
Chicago/Turabian StyleYang, Sun-Yi, and Yun-Hee Oh. 2024. "Development and Effectiveness of a Rapid Cycle Deliberate Practice Neonatal Resuscitation Simulation Program: A Quasi-Experimental Study" Healthcare 12, no. 1: 104. https://doi.org/10.3390/healthcare12010104
APA StyleYang, S.-Y., & Oh, Y.-H. (2024). Development and Effectiveness of a Rapid Cycle Deliberate Practice Neonatal Resuscitation Simulation Program: A Quasi-Experimental Study. Healthcare, 12(1), 104. https://doi.org/10.3390/healthcare12010104






