Social Media, Endometriosis, and Evidence-Based Information: An Analysis of Instagram Content
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Analysis
2.2.1. Content Categories
2.2.2. Post Accuracy
3. Results
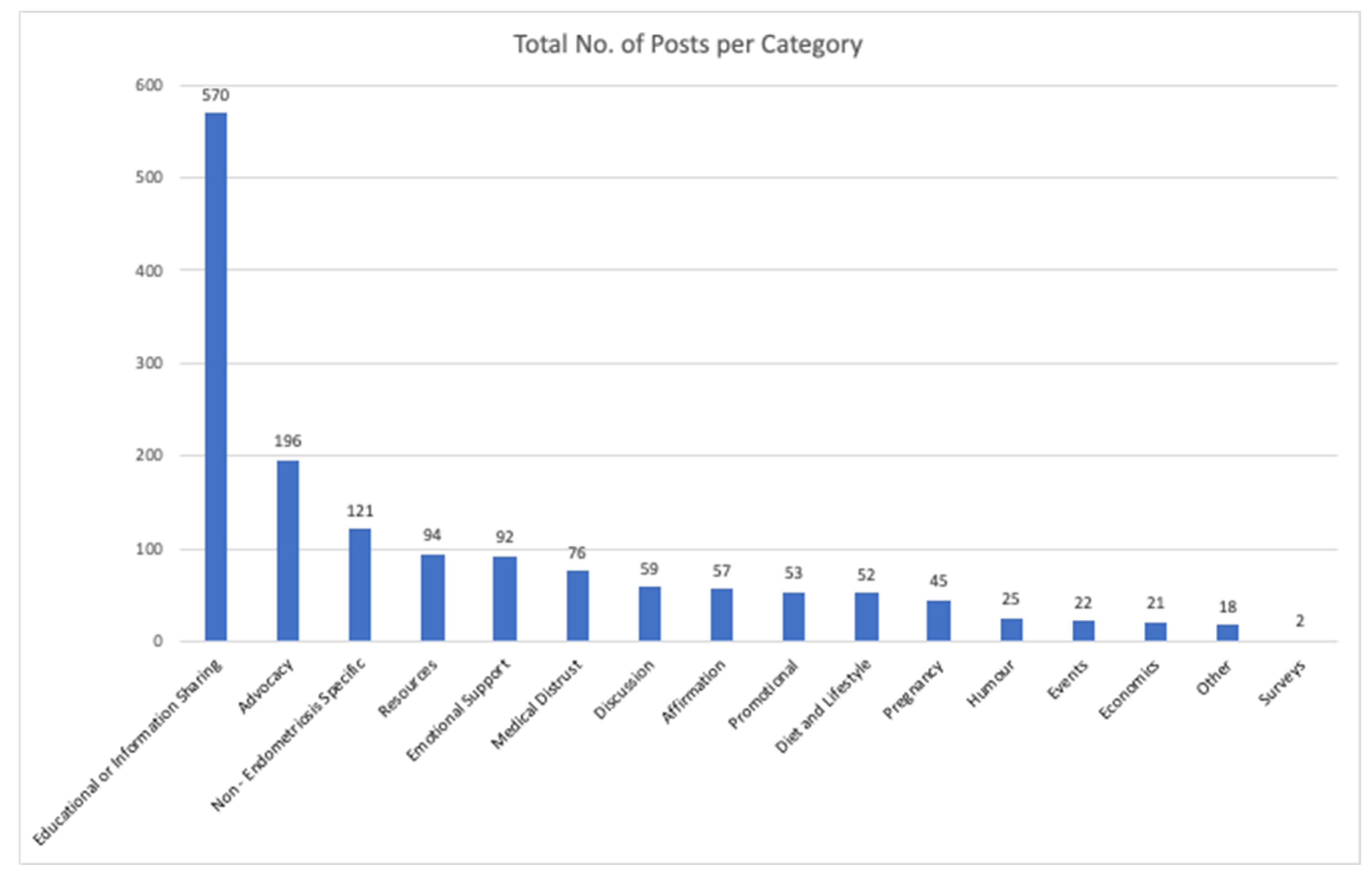
3.1. Content Categories
3.2. Evidence-Based Nature of Posts
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shafrir, A.L.; Farland, L.V.; Shah, D.K.; Harris, H.R.; Kvaskoff, M.; Zondervan, K.; Missmer, S.A. Risk for and consequences of endometriosis: A critical epidemiologic review. Best Pract. Res. Clin. Obstet. Gynecol. 2018, 51, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Rowlands, I.J.; Abbott, J.A.; Montgomery, G.W.; Hockey, R.; Rogers, P.; Mishra, G.D. Prevalence and incidence of endometriosis in Australian women: A data linkage cohort study. BJOG Int. J. Obstet. Gynaecol. 2021, 128, 657–665. [Google Scholar] [CrossRef] [PubMed]
- Armour, M.; Sinclair, J.; Ng, C.H.M.; Hyman, M.S.; Lawson, K.; Smith, C.A.; Abbott, J. Endometriosis and chronic pelvic pain have similar impact on women, but time to diagnosis is decreasing: An Australian survey. Sci. Rep. 2020, 10, 16253. [Google Scholar] [CrossRef] [PubMed]
- O’Hara, R.; Rowe, H.; Fisher, J. Managing endometriosis: A cross-sectional survey of women in Australia. J. Psychosom. Obstet. Gynaecol. 2022, 43, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, M.; Rocha, R.; Tun-Ismail, A.; Robledo, K.; Armour, M.; Condous, G. Assessing the knowledge of endometriosis diagnostic tools in a large, international lay population: An online survey. BJOG Int. J. Obstet. Gynaecol. 2021, 128, 2084–2090. [Google Scholar] [CrossRef] [PubMed]
- Metzler, J.M.; Kalaitzopoulos, D.R.; Burla, L.; Schaer, G.; Imesch, P. Examining the influence on perceptions of endometriosis via analysis of social media posts: Cross-sectional study. JMIR Form Res. 2022, 6, e31135. [Google Scholar] [CrossRef] [PubMed]
- Evans, S.; Villegas, V.; Dowding, C.; Druitt, M.; O’Hara, R.; Mikocka-Walus, A. Treatment use and satisfaction in Australian women with endometriosis: A mixed-methods study. Intern. Med. J. 2022, 52, 2096–2106. [Google Scholar] [CrossRef] [PubMed]
- All Party Parliamentary Group. Endometriosis in the UK: Time for Change: APPG on Endometriosis Inquiry Report 2020. Available online: https://www.endometriosis-uk.org/sites/default/files/files/Endometriosis%20APPG%20Report%20Oct%202020.pdf (accessed on 1 October 2023).
- Scottish Government. Women’s Health Plan: A Plan for 2021–2024. Available online: https://www.gov.scot/binaries/content/documents/govscot/publications/strategy-plan/2021/08/womens-health-plan/documents/womens-health-plan-plan-2021-2024/womens-health-plan-plan-2021-2024/govscot%3Adocument/womens-health-plan-plan-2021-2024.pdf?forceDownload=true (accessed on 2 October 2023).
- EndoAct Canada. Available online: https://endoact.ca/about/ (accessed on 1 October 2023).
- European Parliament. National Strategy to Combat Endometriosis. Available online: https://solidarites-sante.gouv.fr/IMG/pdf/10_01_2022_strategie_nationale_finale_chrysoula_zacharopoulou_vf.pdf (accessed on 1 October 2023).
- Royal Australia and New Zealand College of Obstetricians and Gynaecologists. Australian Clinical Practice Guideline for the Diagnosis and Management of Endometriosis. RANZCOG. 2021. Available online: https://ranzcog.edu.au/news/australian-endometriosis-guideline/ (accessed on 4 October 2023).
- Becker, C.M.; Bokor, A.; Heikinheimo, O.; Horne, A.; Jansen, F.; Kiesel, L.; King, K.; Kvaskoff, M.; Nap, A.; Petersen, K.; et al. ESHRE Endometriosis Guideline Group. ESHRE guideline: Endometriosis. Hum. Reprod. Open 2022, 2, hoac009. [Google Scholar]
- Nezhat, C. Endometriosis in Adolescents: A Comprehensive Guide to Diagnosis and Management, 1st ed.; Springer: Cham, Switzerland, 2020. [Google Scholar]
- Busque, B.L.; Mellish, S. Endometriosis awareness month on social media: A content analysis of images and captions on Instagram. Women 2023, 3, 82. [Google Scholar] [CrossRef]
- Arena, A.; Degli Esposti, E.; Orsini, B.; Verrelli, L.; Rodondi, G.; Lenzi, J.; Casadio, P.; Seracchioli, R. The social media effect: The impact of fake news on women affected by endometriosis. A prospective observational study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2022, 274, 101–105. [Google Scholar] [CrossRef]
- Carlson, S.; Coyne, K.; El-Nashar, S.; Billow, M. Analysis of endometriosis related hashtags on Instagram. J. Minim. Invasive Gynecol 2020, 27, 142. [Google Scholar] [CrossRef]
- Holowka, E.M. Mediating pain: Navigating endometriosis on social media. Front. Pain Res. 2022, 3, 889990. [Google Scholar] [CrossRef] [PubMed]
- Towne, J.; Suliman, Y.; Russell, K.A.; Stuparich, M.A.; Nahas, S.; Behbehani, S. Health information in the era of social media: An analysis of the nature and accuracy of posts made by public Facebook pages for patients with endometriosis. J. Minim. Invasive Gynecol. 2021, 28, 1637–1642. [Google Scholar] [CrossRef] [PubMed]
- Van den Haspel, K.; Reddington, C.; Healey, M.; Li, R.; Dior, U.; Cheng, C. The role of social media in management of individuals with endometriosis: A cross-sectional study. Aust. N. Z. J. Obstet. Gynaecol. 2022, 62, 701–706. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, M.; Aggarwal, S.; Barker, C.; Davis, C.J.; Duffy, J.M.N. Googling endometriosis: A systematic review of information available on the Internet. Am. J. Obstet. Gynecol. 2017, 216, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Stemler, S. An overview of content analysis. Pract. Assess. Res. Eval. 2001, 7, 1–6. [Google Scholar]
- Cherian, R.; Westbrook, M.; Ramo, D.; Sarkar, U. Representations of codeine misuse on Instagram: Content analysis. JMIR Public Health Surveill 2018, 4, e22. [Google Scholar] [CrossRef]
- Cohen, R.; Irwin, L.; Newton-John, T.; Slater, A. #bodypositivity: A content analysis of body positive accounts on Instagram. Body Image 2019, 29, 47–57. [Google Scholar]
- Lee, N.; Buchanan, K.; Yu, M. Each post matters: A content analysis of #mentalhealth images on Instagram. J. Vis. Commun. Med. 2020, 43, 128–138. [Google Scholar]
- Lucibello, K.M.; Vani, M.F.; Koulanova, A.; DeJonge, M.L.; Ashdown-Franks, G.; Sabiston, C.M. #quarantine15: A content analysis of Instagram posts during COVID-19. Body Image 2021, 38, 148–156. [Google Scholar]
- Tiggemann, M.; Zaccardo, M. ‘strong is the new skinny’: A content analysis of #fitspiration images on Instagram. J. Health Psychol. 2018, 23, 1003–1011. [Google Scholar]
- Webb, J.B.; Thomas, E.V.; Rogers, C.B.; Clark, V.N.; Hartsell, E.N.; Putz, D.Y. Fitspo at every size? A comparative content analysis of #curvyfit versus #curvyyoga Instagram images. Fat Stud. 2019, 8, 154–172. [Google Scholar]
- Mosseri, A. Instagram Ranking Explained. Available online: https://about.instagram.com/blog/announcements/instagram-ranking-explained (accessed on 1 October 2023).
- Adler, H.; Lewis, M. “Political cannabis” or “medicinal cannabis?”: An Australian news framing analysis. Int. J. Commun. 2023, 17, 5017–5038. [Google Scholar]
- Burns, P.B.; Rohrich, R.J.; Chung, K.C. The levels of evidence and their role in evidence-based medicine. Plast. Reconstr. Surg. 2011, 128, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Anampa-Guzmán, A.; Freeman-Daily, J.; Fisch, M.; Lou, E.; Pennell, N.A.; Painter, C.A.; Sparacio, D.; Lewis, M.A.; Karmo, M.; Anderson, P.F.; et al. Collaboration for outcomes using social media in oncology. The rise of the expert patient in cancer: From backseat passenger to co-navigator. JCO Oncol. Pract. 2022, 18, 578–583. [Google Scholar] [CrossRef] [PubMed]
- Becker, C.M.; Gattrell, W.T.; Gude, K.; Singh, S.S. Reevaluating response and failure of medical treatment of endometriosis: A systematic review. Fertil. Steril. 2017, 108, 125–136. [Google Scholar] [CrossRef]
- Berbic, M.; Hey-Cunningham, A.J.; Ng, C.; Tokushige, N.; Ganewatta, S.; Markham, R.; Russell, P.; Fraser, I.S. The role of Foxp3+ regulatory T-cells in endometriosis: A potential controlling mechanism for a complex, chronic immunological condition. Hum. Reprod. 2010, 25, 900–907. [Google Scholar] [CrossRef] [PubMed]
- Schulke, L.; Berbic, M.; Manconi, F.; Tokushige, N.; Markham, R.; Fraser, I.S. Dendritic cell populations in the eutopic and ectopic endometrium of women with endometriosis. Hum. Reprod. 2009, 24, 1695–1703. [Google Scholar] [CrossRef]
- Trapero, C.; Vidal, A.; Fernández-Montolí, M.E.; Coroleu, B.; Tresserra, F.; Barri, P.; Gómez de Aranda, I.; Sévigny, J.; Ponce, J.; Matias-Guiu, X.; et al. Impaired expression of ectonucleotidases in ectopic and eutopic endometrial tissue is in favor of ATP accumulation in the tissue microenvironment in endometriosis. Int. J. Mol. Sci. 2019, 20, 5532. [Google Scholar] [CrossRef]
- Wu, Y.; Strawn, E.; Basir, Z.; Wang, Y.; Halverson, G.; Jailwala, P.; Guo, S.W. Genomic alterations in ectopic and eutopic endometria of women with endometriosis. Gynecol. Obstet. Investig. 2006, 62, 148–159. [Google Scholar] [CrossRef]
- Zondervan, K.T.; Becker, C.M.; Missmer, S.A. Endometriosis. N. Engl. J. Med. 2020, 382, 1244–1256. [Google Scholar] [CrossRef]
- Cousins, F.L.; McKinnon, B.D.; Mortlock, S.; Fitzgerald, H.C.; Zhang, C.; Montgomery, G.W.; Gargett, C.E. New concepts on the etiology of endometriosis. J. Obstet. Gynaecol. Res. 2023, 49, 1090–1105. [Google Scholar] [CrossRef] [PubMed]
- Rizk, B.; Fischer, A.S.; Lotfy, H.A.; Turki, R.; Zahed, H.A.; Malik, R.; Holliday, C.P.; Glass, A.; Fishel, H.; Soliman, M.Y.; et al. Recurrence of endometriosis after hysterectomy. Facts Views Vis. ObGyn 2014, 6, 219–227. [Google Scholar] [PubMed]
- Ferrando, C.A.; Chapman, G.; Pollard, R. Preoperative pain symptoms and the incidence of endometriosis in transgender men undergoing hysterectomy for gender affirmation. J. Minim. Invasive Gynecol. 2021, 28, 1579–1584. [Google Scholar] [CrossRef] [PubMed]
- Ferrando, C.A. Endometriosis in transmasculine individuals. Reprod. Fertil. 2022, 3, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Rei, C.; Williams, T.; Feloney, M. Endometriosis in a man as a rare source of abdominal pain: A case report and review of the literature. Case Rep. Obstet. Gynecol. 2018, 2018, 2083121. [Google Scholar] [CrossRef] [PubMed]
- Zavestoski, S.; Morello-Frosch, R.; Brown, P.; Mayer, B.; McCormick, S.; Gasior Altman, R. Embodied health movements and challenges to the dominant epidemiological paradigm. In Authority in Contention (Research in Social Movements, Conflicts, and Change); Emerald Group Publishing Limited: Leeds, UK, 2004; Volume 25, pp. 253–278. [Google Scholar]
- Whelan, E. ‘No one agrees except for those of us who have it’: Endometriosis patients as an epistemological community. Sociol. Health Illn. 2007, 29, 957–982. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.; Mogan, S.; Kaur, K. Understanding the role of Facebook to support women with endometriosis: A Malaysian perspective. Int. J. Nurs. Pract. 2020, 26, e12833. [Google Scholar] [CrossRef]
- Fox, N.; Ward, K. Health identities: From expert patient to resisting consumer. Health 2006, 10, 461–479. [Google Scholar] [CrossRef]
- Driessen, S.R.; Janse, J.A.; Schreuder, H.W.; Jansen, F.W. Proficiency for advanced laparoscopic procedures in gynecologic residency program: Do all residents need to be trained? J. Surg. Educ. 2015, 72, 942–948. [Google Scholar] [CrossRef]
- Schulz, P.J.; Nakamoto, K. Health literacy and patient empowerment in health communication: The importance of separating conjoined twins. Patient Educ. Couns. 2013, 90, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.S.; Podolsky, S.H. The history and fate of the gold standard. Lancet 2015, 385, 1502–1503. [Google Scholar] [CrossRef] [PubMed]
- Bafort, C.; Beebeejaun, Y.; Tomassetti, C.; Bosteels, J.; Duffy, J.M. Laparoscopic surgery for endometriosis. Cochrane Database Syst. Rev. 2020, 10, CD011031. [Google Scholar] [PubMed]
- Burks, C.; Lee, M.; DeSarno, M.; Findley, J.; Flyckt, R. Excision versus ablation for management of minimal to mild endometriosis: A systematic review and meta-analysis. J. Minim. Invasive Gynecol. 2021, 28, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Healey, M.; Ang, W.C.; Cheng, C. Surgical treatment of endometriosis: A prospective randomized double-blinded trial comparing excision and ablation. Fertil. Steril. 2010, 94, 2536–2540. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, E.; Fitzgerald, A.; Clark, N. Evolving best practices in the surgical management of endometriosis—Examining the evidence and expert Opinion. Curr. Opin. Obstet. Gynecol. 2023, 35, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Hart, R.J.; Hickey, M.; Maouris, P.; Buckett, W. Excisional surgery versus ablative surgery for ovarian endometriomata. Cochrane Database Syst. Rev. 2008, 2, CD004992. [Google Scholar] [CrossRef]
- Johnson, N.P.; Hummelshoj, L. World Endometriosis Society Montpellier Consortium. Consensus on current management of endometriosis. Hum. Reprod. 2013, 28, 1552–1568. [Google Scholar] [CrossRef]
- Healey, M.; Cheng, C.; Kaur, H. To excise or ablate endometriosis? A prospective randomized double-blinded trial after 5-year follow-up. J. Minim. Invasive Gynecol. 2014, 21, 999–1004. [Google Scholar] [CrossRef]
- Riley, K.A.; Benton, A.S.; Deimling, T.A.; Kunselman, A.R.; Harkins, G.J. Surgical excision versus ablation for superficial endometriosis-associated pain: A randomized controlled trial. J. Minim. Invasive Gynecol. 2019, 26, 71–77. [Google Scholar] [CrossRef]
- Roman, H.; Chanavaz-Lacheray, I.; Hennetier, C.; Tuech, J.J.; Dennis, T.; Verspyck, E.; Merlot, B. Long-term risk of repeated surgeries in women managed for endometriosis: A 1092 Patient-series. Fertil. Steril. 2023, 120, 870–879. [Google Scholar] [CrossRef] [PubMed]
- Bafort, C.; Mourad Tawfic, N.; Meuleman, C.; Laenen, A.; Timmerman, D.; Van Schoubroeck, D.; Tomassetti, C. Similar long-term recurrence rates with cystectomy and CO2 laser vaporization for endometrioma: A retrospective study. Reprod. Biomed. Online 2022, 45, 101–108. [Google Scholar] [CrossRef]
- Butler, K. Have Endometriosis? Be Wary of that Popular Facebook Group. Mother Jones. Available online: https://www.motherjones.com/politics/2023/12/endometriosis-nancy-nook-facebook/?fbclid=IwAR0Wqge0rwkyThIWtOqIIAg-BAREpPW1fszA28Y51I8qOjApQ8Je78_aLdI#comment-container (accessed on 4 December 2023).
- Hawkey, A.; Chalmers, K.J.; Micheal, S.; Diezel, H.; Armour, M. “A day-to-day struggle”: A comparative qualitative study on experiences of women with endometriosis and chronic pelvic pain. Feminism Psychol. 2022, 32, 482–500. [Google Scholar] [CrossRef]
- Chou, W.Y.S.; Oh, A.; Klein, W.M.P. Addressing health-related misinformation on social media. JAMA 2018, 320, 2417–2418. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Song, Y. Viral misinformation and echo chambers: The diffusion of rumors about genetically modified organisms on social media. Internet Res. 2020, 30, 1547–1564. [Google Scholar] [CrossRef]
- Patrick, M.; Venkatesh, R.D.; Stukus, D.R. Social media and its impact on health care. Ann. Allergy Asthma Immunol. 2022, 128, 139–145. [Google Scholar] [CrossRef]
- Leonardi, M.; Robledo, K.P.; Goldstein, S.R.; Benacerraf, B.R.; Condous, G. International survey finds majority of gynecologists are not aware of and do not utilize ultrasound techniques to diagnose and map endometriosis. Ultrasound Obstet. Gynecol. 2020, 56, 324–328. [Google Scholar] [CrossRef]
- Lewis, M.; Govender, E.; Holland, K. (Eds.) Communicating COVID-19: Interdisciplinary Perspectives; Palgrave Macmillan: Cham, Switzerland, 2021; pp. 1–365. [Google Scholar]
- Hyland-Wood, B.; Gardner, J.; Leask, J.; Ecker, U.K.H. Toward effective government communication strategies in the era of COVID-19. Humanit. Soc. Sci. Commun. 2021, 8, 30. [Google Scholar] [CrossRef]
- Young, K.; Fisher, J.; Kirkman, M. Women’s experiences of endometriosis: A systematic review and synthesis of qualitative research. J. Fam. Plann. Reprod. Health Care 2015, 41, 225–234. [Google Scholar] [CrossRef]
- Sylvia Chou, W.Y.; Gaysynsky, A.; Cappella, J.N. Where we go from here: Health misinformation on social media. Am. J. Public Health 2020, 110, S273–S275. [Google Scholar] [CrossRef]
- Bode, L.; Vraga, E.K. See something, say something: Correction of global health misinformation on social media. Health Commun. 2018, 33, 1131–1140. [Google Scholar] [CrossRef] [PubMed]
- Vraga, E.K.; Bode, L. Using expert sources to correct health misinformation in social media. Sci. Commun. 2017, 39, 621–645. [Google Scholar] [CrossRef]
- Smith, C.N.; Seitz, H.H. Correcting misinformation about neuroscience via social media. Sci. Commun. 2019, 41, 790–819. [Google Scholar] [CrossRef]
- Maher, R.; Murphet, B. Community engagement in Australia’s COVID-19 communications response: Learning lessons from the humanitarian sector. Media Int. Australia 2020, 177, 113–118. [Google Scholar] [CrossRef]
- National Academies. Science Literacy for Communities. In Science Literacy: Concepts, Contexts, and Consequences; The National Academies Press: Washington, DC, USA, 2016. [Google Scholar]
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef]

| Category | Total No. of Posts | Total No. of Claims Overall | Total No. Evidenced Based Claims | Total No. Non-Evidenced-Based Claims | Total No. Mixed Claims |
|---|---|---|---|---|---|
| Cure | 38 | 45 | 31 (68.88%) | 10 (22.22%) | 4 (8.88%) |
| Scientific Article | 10 | 11 | 7 (63.63%) | 1 (9.09%) | 3 (27.27%) |
| Symptoms | 134 | 145 | 86 (59.31%) | 19 (13.10%) | 40 (27.5%) |
| Fertility | 44 | 44 | 24 (54.54%) | 8 (18.18%) | 12 (27.27%) |
| Other | 6 | 7 | 3 (42.85%) | 2 (28.57%) | 2 (28.57%) |
| Diagnosis | 65 | 76 | 28 (36.84%) | 21 (27.63%) | 27 (35.52%) |
| Orthodox Medicine | 38 | 50 | 17 (34%) | 17 (34%) | 16 (32%) |
| Epidemiology | 68 | 75 | 22 (29.33%) | 21 (28%) | 32 (42.66%) |
| Surgery | 50 | 58 | 11 (18.95%) | 35 (60.34%) | 12 (20.68%) |
| Pathophysiology | 86 | 114 | 21 (18.42%) | 10 (8.77%) | 83 (72.80%) |
| Alternative Medicine | 31 | 56 | 6 (10.71) | 18 (32.14%) | 32 (57.14%) |
| Example Claim | ||
|---|---|---|
| Evidence-Based | Non-Evidence-Based | Mixed |
| Endo[metriosis] can cause possible infertility (Fertility). | Physiotherapy, psychology, analgesics and surgery do not relieve much pain (Orthodox Medicine). | If a patient has suspected endo[metriosis], they MUST be referred to an excision specialist (Surgery). |
| For some, it [endometriosis] can prove to be excruciating, disrupting their normal routines and forcing them to plan their days around the pain (Symptoms). | The pill does not ‘fix’ anything and does not supress bleeding for those with endo[metriosis] (Orthodox Medicine.) | It’s [endometriosis] a chronic health issue that affects one in ten women and it’s hardly ever talked about (Epidemiology). |
| It takes on average eight years to get diagnosed (Diagnosis). | 20–25% of endo[metriosis] patients affected by infertility may be asymptomatic (Fertility). | Research has found that high levels of depression and anxiety can also exacerbate the symptoms of this condition. This is due to an increased pain perception which occurs with these psychological conditions (Scientific Article). |
| There is no cure for endometriosis (Cure). | We do not need research into alternative therapies, MRI studies are useless (Alternative Medicine). | If a patient has endo[metriosis] so severe it can be seen on a DIE scan, it should be removed to prevent frozen pelvis and organ dysfunction and a range of other potential comorbidities (Pathophysiology). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adler, H.; Lewis, M.; Ng, C.H.M.; Brooks, C.; Leonardi, M.; Mikocka-Walus, A.; Bush, D.; Semprini, A.; Wilkinson-Tomey, J.; Condous, G.; et al. Social Media, Endometriosis, and Evidence-Based Information: An Analysis of Instagram Content. Healthcare 2024, 12, 121. https://doi.org/10.3390/healthcare12010121
Adler H, Lewis M, Ng CHM, Brooks C, Leonardi M, Mikocka-Walus A, Bush D, Semprini A, Wilkinson-Tomey J, Condous G, et al. Social Media, Endometriosis, and Evidence-Based Information: An Analysis of Instagram Content. Healthcare. 2024; 12(1):121. https://doi.org/10.3390/healthcare12010121
Chicago/Turabian StyleAdler, Hannah, Monique Lewis, Cecilia Hoi Man Ng, Cristy Brooks, Mathew Leonardi, Antonina Mikocka-Walus, Deborah Bush, Alex Semprini, Jessica Wilkinson-Tomey, George Condous, and et al. 2024. "Social Media, Endometriosis, and Evidence-Based Information: An Analysis of Instagram Content" Healthcare 12, no. 1: 121. https://doi.org/10.3390/healthcare12010121
APA StyleAdler, H., Lewis, M., Ng, C. H. M., Brooks, C., Leonardi, M., Mikocka-Walus, A., Bush, D., Semprini, A., Wilkinson-Tomey, J., Condous, G., Patravali, N., Abbott, J., & Armour, M. (2024). Social Media, Endometriosis, and Evidence-Based Information: An Analysis of Instagram Content. Healthcare, 12(1), 121. https://doi.org/10.3390/healthcare12010121








