Abstract
Cystic fibrosis requires regular monitoring and intervention by healthcare teams; despite that, adherence to therapeutic measures is less than desired. The evolution of technology has allowed much of the care provided in person to be replaced by a telehealth delivery model, but studies on telerehabilitation are scarce and dispersed. This scoping review aimed to identify which domains of rehabilitation intervention are mediated by information and communication technologies and how they are developed in the provision of care to children and adolescents with cystic fibrosis. The data collection was conducted in February and June 2023, following the three steps recommended by the JBI for this type of review: (1) the search was conducted in MEDLINE, CINAHL, Scopus, JBI, and Web of Science; (2) the bibliographic references obtained from the included articles were analysed; and (3) the grey literature was checked. The eligibility criteria were children and adolescents and rehabilitation interventions mediated by information and communication technologies. The five studies included in this review were subjected to analysis, and a narrative synthesis of the results was carried out. The interventions identified included physical exercise programs (60%), management of the therapeutic regimen (40%), and symptom control (40%). The information and communication technologies were web-based platforms, video games, and telephones. The use of telerehabilitation included face-to-face meetings to ensure participants performed the exercises correctly, monitor their response to exercise, and teach them how to avoid risky situations during home workouts. In all studies, exercise sessions were supervised by the participants’ parents or caregivers.
1. Introduction
Cystic fibrosis (CF) is a chronic, progressive, genetic, and hereditary disease and autosomal recessive disorder that impairs normal chloride secretions, resulting in thick secretions that primarily affect breathing [1,2]. Respiratory impairment results from the presence of thick mucus, which causes airway obstruction, infection, lung damage, and pulmonary failure, shortening life expectancy [3,4].
Given the chronic, progressive, and disabling nature of CF, the therapeutic regimen is demanding and is based on multiple treatments, most of which are carried out on a daily basis [5]. Two of the pillars are airway clearance techniques (ACTs) and exercise training, within the scope of rehabilitation.
Airway clearance techniques have a positive impact on lung function decline. They clear secretions, but also improve lung function, increasing the percent predicted forced expiratory volume in one second (ppFEV1) [3,6,7]. Regular participation in physical activity and involvement in structured exercise training programs have also been shown to improve exercise tolerance, lung function, energy levels, and quality of life and are strongly encouraged [8,9].
Because the disease is diagnosed close to birth or in early childhood [5], support from families is essential to optimize the physical and psychosocial development of children living with CF [10]. Furthermore, childhood and adolescence (age >6 and <18 years) are fundamental stages for the development of skills related to understanding the disease and its management. As school-age children expand their cognitive and linguistic skills and can better communicate their beliefs and expectations about illness, psychoeducational interventions addressing misinformation and unfounded fears or concerns are more effective [5]. At this stage, it is also essential to encourage children’s sense of ownership and control, in order to develop skills and self-efficacy related to self-management of the disease and collaboration throughout their lifespan [5]. All these efforts should extend into adolescence, a phase that is characterized by persistent movement towards increasing autonomy, and in which self-concept continues to be refined through experiences such as “trying on” different roles and behaviours that could have implications for health [5].
Despite the tremendous physical and psychosocial development that occurs in these phases of the life cycle, CF typically worsens during adolescence with the presence of more frequent symptoms, like cough and fatigue, and pulmonary exacerbations, increasing the illness burden [11]. Research has shown that over time, overall adherence to CF treatment worsens with age, when children become adolescents [12,13].
There are several reasons that may explain problems related to adherence to the therapeutic regimen. In addition to the complexity and demands of treatment already mentioned, other problems have been reported, such as the accessibility of care, particularly that of reference centres, where disease management allows for better results, due to their distance from many patients or simply due to a lack of availability [14,15]. Contact isolation measures between patients with CF to prevent the onset of chronic airway infections when seeking healthcare cannot be excluded from this equation either [16,17].
The coronavirus disease 2019 (COVID-19) pandemic has exacerbated some of these problems and posed unique challenges for clinicians, researchers, and other healthcare professionals involved with CF patients [1]. Many of the activities based on a traditional in-person service model were quickly replaced by a telehealth delivery model, in a rapid adaptation to respond to the health needs of this population [18].
Telehealth, defined as the use of information and communication technologies (ICTs) to support distance-based health interventions like the assessment, education, monitoring, and delivery of healthcare interventions [19,20], has ensured timely remote healthcare and managed many chronic illnesses, with documented effectiveness [21]. Technology-based care delivery models are here to stay as a way to solve several problems, old and current, in accessing the best healthcare [22]. It also has the advantage of allowing easier access to reference centres in places where accessibility is limited, by distance or by service availability [14,15]. But telehealth also brings several challenges to multidisciplinary intervention, which also includes intervention in respiratory rehabilitation [14,15] with the need to design and test the effectiveness of telerehabilitation interventions for these patients and their families.
Objectives
To date, we have not found any systematic reviews, including scoping reviews, on the use of telehealth in the provision of rehabilitation care—telerehabilitation—in children and adolescents with CF. Therefore, the aim of this scoping review (ScR) is to identify which domains of rehabilitation intervention are mediated by ICT and how they are developed in the provision of care for children and adolescents with CF.
2. Materials and Methods
The study protocol was registered in the Open Science Framework (OSF) (DOI 10.17605/OSF.IO/B8TDW) with extended data at https://osf.io/wn2zd (accessed on 16 February 2023).
The protocol was designed according to the steps defined by the Joanna Briggs Institute (JBI) for the synthesis of evidence in a scoping review (ScR) [23]. It was structured as recommended by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist [24].
2.1. Study Design
After conducting an initial search in the various databases, we did not identify any systematic reviews, including scoping reviews, to answer the following research question: What interventions in the area of rehabilitation, mediated by ICT, are in use and how are they developed in cystic fibrosis management in children and adolescents?
Given the state of the art, the best type of systematic review to answer the research question is the ScR. A research strategy was implemented following the recommendations of the JBI 2021 and aimed to be as comprehensive as possible to answer the research question, based on the PCC mnemonic framework (Participants, Concept, Context) [23].
2.2. Eligibility Criteria
Each element of the acronym guided the definition of each specific inclusion criterion, presented in Table 1.

Table 1.
Eligibility criteria for bibliographic sample. Lisbon, 2023.
The following were considered for inclusion: primary studies, quantitative and qualitative studies, as well as secondary studies, specifically all types of literature reviews, guidelines indexed in databases, and any studies in the grey literature that could answer the research question. The studies were limited to full texts, in Portuguese, English, and Spanish, with a time limit of five years (2017–2022), due to the timeliness of the results and because exploratory research to identify studies showed that the research on the subject is recent.
2.3. Information Sources and Search Strategy
An initial exploratory study was carried out in February 2023 to identify the state of the art, check descriptors, and structure the study protocol. In June, a search was carried out, following the 3 steps recommended by the JBI for this type of systematic review [23]. First, an initial search was conducted in the MEDLINE (via PubMed) and CINAHL (via EBSCO) databases, using keywords built from natural language relative to the theme. This search allowed the identification of the words in the titles and abstracts, as well as the indexing terms used. A second search was carried out using the keywords and indexing terms identified in the previously included databases. The Boolean operators OR and AND were used to operationalize the search, and language filters were applied for full text, language, and time restriction. In this phase, the search was conducted in MEDLINE (via PubMed), CINAHL (via EBSCO), Scopus, JBI, and Web of Science. The descriptors were adjusted to each database, e.g., for Medline, MeSH terms were used; for CINAHL, subject headings; and so on.
After this stage, a search was conducted in the grey literature on websites about cystic fibrosis, in master’s and doctoral thesis repositories, and the bibliographic references obtained from the included articles were analysed. Table 2 shows the complete search strategy for the MEDLINE database.

Table 2.
Search strategy for MEDLINE (via PubMed). Lisbon, 2022.
The articles identified in each database/source were exported to Rayyan®. Two researchers independently screened the titles and abstracts (E.P., M.F.) according to the predefined inclusion criteria. A full-text evaluation of the retrieved studies was then carried out. Disagreements between reviewers were resolved by a third reviewer (C.L.B).
After this phase, the articles were read in full by each researcher, and this analysis was verified by the research team, increasing reliability.
2.4. Study Selection and Data Processing and Analysis
The researchers created an Excel table that was shared in the cloud to record the characteristics of the content extracted from the articles in the final bibliographic sample: identification of the title of the article/work; author(s), year of publication, and type of article; and objective(s), method, and main results/conclusions. Two reviewers (E.P. and C.L.B.) tested the extraction form in three sources to benchmark the decision-making process and ensure that relevant results were recorded, in line with Valaitis et al. [25].
The articles that answered the research question and met the inclusion criteria were subjected to analysis and a narrative synthesis of the results was carried out.
2.5. Ethical Issues
This study was carried out strictly following the study protocol to ensure its validity. The identification and referencing of the articles included in the bibliographic sample followed the recommendations of good academic and scientific practice. The extraction and analysis of data was carried out with evident respect for the research and results obtained by other researchers.
3. Results
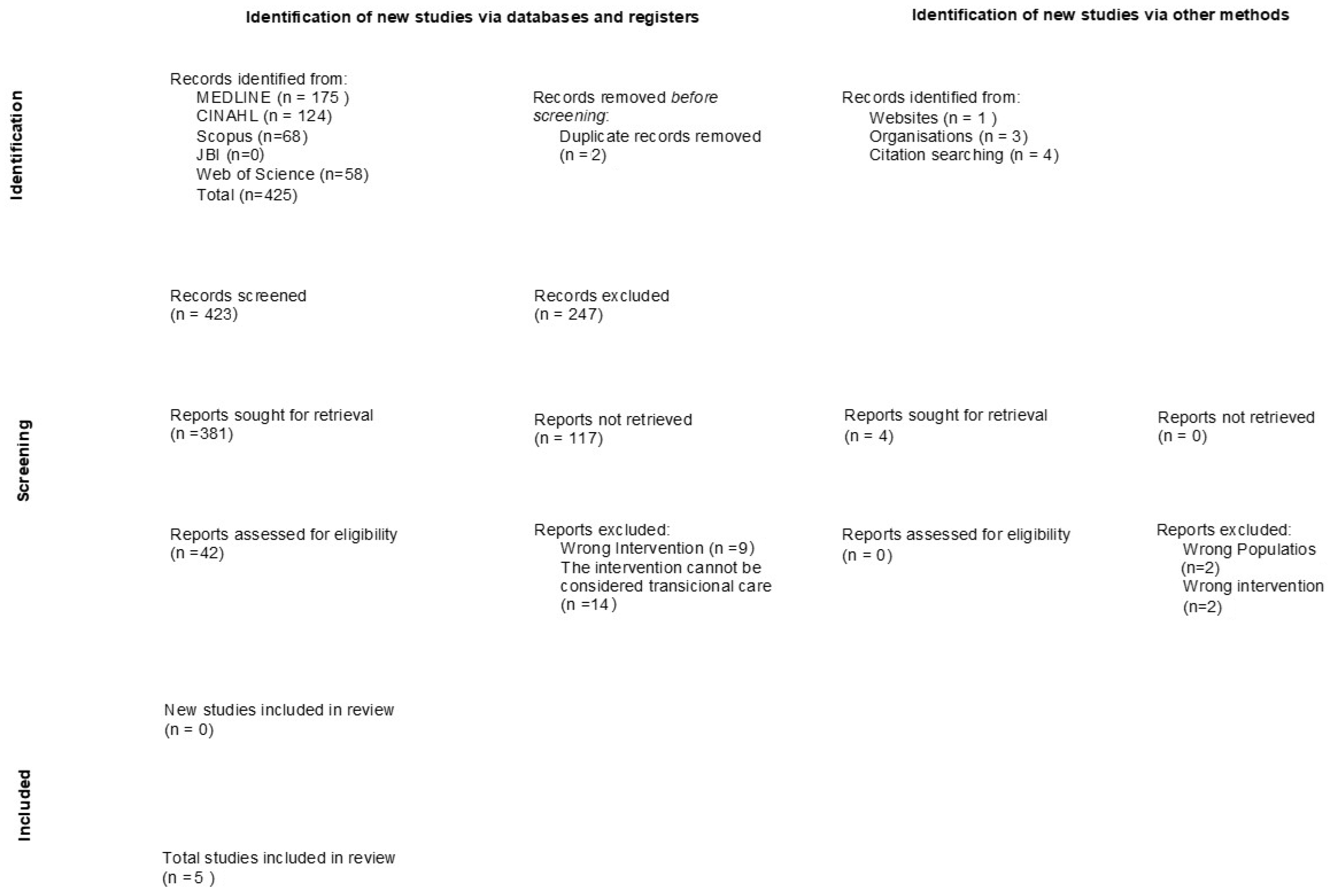
The search strategy initially generated 425 results, which, after screening and assessment for eligibility, resulted in the inclusion of 5 studies for review. The PRISMA flow diagram [24] is presented in Figure 1. Specifically, after the initial elimination of two duplicate results, the two reviewers analysed the titles and abstracts of the remaining articles against the inclusion/exclusion criteria. Forty-two full-text articles were reviewed, once again, against the inclusion and exclusion criteria, and five were included for review. The references of all included articles were selected, although they did not generate more articles. Searches were also carried out in repositories of academic institutions, as well as in organizations that work in CF, and four articles were identified.
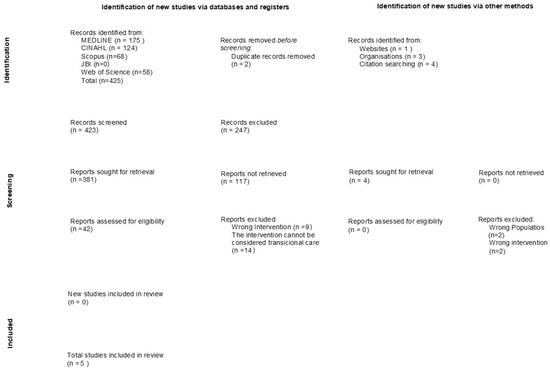
Figure 1.
PRISMA 2020 flow diagram. Lisbon, 2023.
The studies were heterogeneous and showed some geographic dispersion. They were conducted in the United States [1], Spain [26], Türkiye [27], Greece [28], and Brazil [29].
The included studies had different designs (Table 3). Two were RCTs [26,27], one a quasi-experimental study [28], one a feasibility/prospective study [1], and the other a cross-sectional study [29]. In the RCTs, the researchers who evaluated patients before and after the intervention were blinded to the participants’ treatment allocations. All studies were conducted as home-based interventions.

Table 3.
Telerehabilitation for children and adolescents with CF. Lisbon, 2023.
Three of the included studies were conducted with children and adolescents [26,28,29], one with children [27], and one with adolescents [1]. The number of participants ranged from 10 [1] to 184 [29]. With the exception of one study that did not report data on gender [28], in three studies the participants were mostly female [1,27,29], ranging from 53.7% to 71.4%, and in one study the participants were mostly male with 52.5% [26]. Three studies were conducted with participants with a stable clinical condition [1,26,27], one did not consider clinical stability as an inclusion criterion [29], and in another there were no data on this issue [28]. In three studies, participants were recruited from reference centres for the treatment of CF [1,28,29]; in one, from CF associations [26]; and in one, from a paediatric pulmonology clinic [27].
In three of the included studies, telerehabilitation programs consisted of home exercise training programs [1,26,27], and two of them addressed issues of the daily treatment routine or the control of signs and symptoms associated with CF in the form of teleconsultations or telemonitoring [28,29].
The studies that focused on physical exercise training used different strategies to develop the interventions. In one, an active video game (AVG) was used as a training modality (EA SPORTSTM ACTIVE 2 from Nintendo WiiTM platform), designed to include a combination of aerobic exercise, muscular strength exercise, body endurance, and flexibility [26]. The game was supervised by a virtual personal trainer and included a heart rate (HR) monitor to monitor daily exercise intensity and help patients to control their HR evolution. To increase patient adherence, weekly telephone check-ins were also provided. In another study, a trained researcher actively participated and supervised, via videoconferencing (web-based platform Zoom), an exercise training program based on a combination of high-intensity interval training, in the form of a letter game, and postural strengthening [27]. In another study, a personal trainer, via videoconference (Zoom), led, instructed, demonstrated, and encouraged participants to engage in a supervised resistance exercise training (RET) programme that consisted of whole-body exercise sessions, with the additional use of a set of adjustable-weight dumbbells, in individual sessions [1].
In these studies, it was possible to find information about the frequency, intensity, type of exercise, and duration of the programme. The frequency of the programs varied from three [1,27] to five [26] times a week. The exercise intensity was specified, according to the type of exercise performed, for example, 70–80% of the maximum HR for aerobic exercise [26] and 60% of one-repetition maximum for resistance exercise training [1]; one study did not specify these data [27]. Only one study specified the duration of the session, which varied between 30 and 60 min [26]. The programme duration ranged from 6 [26] to 12 weeks [1,27].
In two studies, games were used to implement the exercise programme: one used a video game [26] and the other a form of letter game [27]. In one, the exercises were also adapted to the age of the participants—≤12 years and >13 years [26].
These studies also described the security conditions underlying the development of the programme. In one study, the first sessions were held in person to ensure participants performed the exercises correctly, monitor their response to exercise, and teach them how to avoid risky situations during home workouts [27]. In two studies, rehabilitation sessions took place face-to-face, via videoconference, with the supervision of therapists [1,27]. In all studies, exercise sessions were supervised by the participants’ parents or caregivers.
The studies that focused on the implementation of routine teleconsultations and telemonitoring also used different strategies. One used a web-based platform (Skype®) or a telephone, depending on the patients’ availability, to address important issues of the daily treatment routine like treatment adherence, the proper use of prescribed drugs, the possibilities of performing techniques, and the use of physical therapy equipment for each patient individually [29]. The other based the intervention on telephone communication, dealing with questions about exacerbations, respiratory infections or symptoms, weight gain, medications, and treatment adherence [28].
4. Discussion
This scoping review allowed the mapping of telerehabilitation interventions, including telemonitoring, in children and adolescents with cystic fibrosis, identifying the intervention design, as well as the e-health modality, technological platforms, and other elements, used to delivere digital care.
Although the research strategy was comprehensive in answering the research question, the low number of studies identified stands out for showing that telerehabilitation is still in development and being adopted by reference centres for monitoring the disease, still without dissemination of the results of its implementation. Even so, the results corroborate the opinions of other authors, who suggest that supervised telerehabilitation with telemonitoring support is feasible and safe, without adverse events, and adherence is high, with a recruitment rate consistent with previous respiratory rehabilitation trials [30,31].
The information and communication technologies used for intervention were web-based platforms [1,27,29], video game consoles [26], and telephones [29]. Intervention monitoring was carried out by researchers via teleconsultation (telephone or web platform) [28,29] or by a heart rate (HR) monitor [26]. These virtual interventions eliminate the need for unnecessary in-person referrals to specialists, reduce wait times for specialist feedback, and eliminate the need for unnecessary travel [32]. They also simultaneously allow the timely identification of clinical changes, worsening of symptoms, and non-adherence to the therapeutic regimen [30,31,32].
The good adherence of children and adolescents to these programmes demonstrates their acceptability and allows us to predict the potential of e-health interventions for solving problems present in these chronically ill patients. Some studies have observed that adherence is unsatisfactory, especially in certain therapeutic modalities, such as nutritional guidelines, inhalation therapy, and respiratory physical therapy [1,7,9,33].
Researchers who implemented a video game intervention concluded that it can effectively improve exercise capacity, muscular strength, and quality of life in the short term in children and adolescents with CF [26]. Indeed, video games have been considered as a novel way of delivering healthcare interventions with the potential to motivate changes in health behaviours [34,35]. One systematic review that aimed to examine the effectiveness of game-based interventions on physiological outcome measures, as well as adherence and enjoyment, in subjects with chronic respiratory diseases observed that the use of videogame interventions, undertaken for several weeks, improved exercise capacity and other outcomes and was more enjoyable for subjects with chronic respiratory diseases [34].
Another study that used videogames with patients over 6 years old with CF reported that active video gaming in patients with CF, as well in healthy individuals, generated the required cardiorespiratory demand for moderate-intensity aerobic physical training. However, these effects depended on the game selection, with the games Wii Fit “Free Run” (Nintendo Wii) and “Just Dance 2015″ (Xbox One, song “Summer”) being the ones that produced greater responses [36]. More studies with children and adolescents are needed that include investigations of the effects in this age group.
The interventions implemented were home exercise training programs, and controlling the signs and symptoms and treatment adherence. Physical activity and exercise have numerous benefits in patients with CF, including improved FEV1, aerobic capacity, lung function, exercise capacity, and quality of life [37]. These patients show some difficulties in exercise, symptom management, and therapeutic adherence that are essential for controlling the disease, preventing exacerbations, and slowing progression [37,38]. Non-compliance with the therapeutic regimen has multiple clinical and economic consequences, with increased mortality or morbidity observed in non-compliant patients [38]. Further studies are needed to determine the effect of telerehabilitation in adherence to therapeutic regimes.
Although they mentioned that a reduction in hospital visits is an advantage of these interventions [32], the researchers did not evaluate the participants’ satisfaction in relation to this factor. We suggest that future studies explore this topic, especially because these patients are often exposed to invasive and painful procedures in the hospital, and the fact that they need to visit the hospital increases their fear and worry [39]. There is also a need to understand the meaning that children, adolescents, and their families give to the possibility of having the care at home and understanding their representations, beliefs, and behaviours [40], which can interfere with the delivery of and adherence to telerehabilitation. Although paediatric telerehabilitation has been considered feasible to provide clinical intervention, future research is needed to evaluate the impact of telerehabilitation services on patient care and its applications for the ongoing use of this delivery model [41].
Another recommendation is that studies include other non-pharmacological interventions in association with physical exercise, given the multicomponent nature of interventions in young people with CF.
This scoping review has limitations related to some methodological options, such as restrictions placed on the language and free access to full texts, which probably excluded some articles that answered the research question. It should also be noted that the studies are heterogeneous in terms of design, participants, and type of intervention.
5. Conclusions
This ScR was conducted in MEDLINE, CINAHL, Scopus, JBI, and Web of Science. Of 425 identified studies, 5 respected the eligibility criteria, 2 were RCTs, 1 was a quasi-experimental study, 1 a feasibility/prospective study, and the other a cross-sectional study.
Interventions within the scope of telerehabilitation included physical exercise programs (60%), management of the therapeutic regimen (40%), and control of symptoms (40%). In some studies, the use of telerehabilitation included face-to-face meetings to ensure participants performed the exercises correctly, monitor their response to exercise, and teach them how to avoid risky situations during home workouts. In all studies, exercise sessions were supervised by the participants’ parents or caregivers. The information and communication technologies used for intervention were web-based platforms, video game consoles, and telephones. Intervention monitoring was carried out via teleconsultation (telephone or web platform) or by a heart rate monitor.
Author Contributions
Conceptualization, E.P., M.F. and C.L.B.; methodology, E.P. and C.L.B.; software, M.F. and E.P.; validation, C.L.B.; formal analysis, E.P., M.F. and C.L.B.; investigation, E.P., M.F. and C.L.B.; resources, C.L.B.; data curation, E.P., M.F. and C.L.B.; writing—original draft preparation, E.P., M.F. and C.L.B.; writing—review and editing, E.P., M.F. and C.L.B.; visualization, E.P., M.F. and C.L.B.; supervision, C.L.B.; project administration, C.L.B.; funding acquisition, C.L.B. All authors have read and agreed to the published version of the manuscript.
Funding
The present study was funded by the Center for Research, Innovation, and Development in Nursing, in Portugal, by means of grants provided to some of the authors (CIDNUR, Psafe2transition_2021).
Data Availability Statement
The original contributions presented in the study are included in the article; further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflicts of interest.
References
- Holmes, C.J.; Racette, S.B.; Symonds, L.; Arbeláez, A.M.; Cao, C.; Granados, A. Feasibility and Efficacy of Telehealth-Based Resistance Exercise Training in Adolescents with Cystic Fibrosis and Glucose Intolerance. Int. J. Environ. Res. Public Health 2022, 19, 3297. [Google Scholar] [CrossRef]
- Reamer, C.; O’Malley, C.; Nufer, J.; Savant, A. Improved outcomes in cystic fibrosis using modified Re-Education of Airway Clearance Technique (REACT) programme. BMJ Open Qual. 2020, 9, e000890. [Google Scholar] [CrossRef]
- Elborn, J.S. Cystic fibrosis. Lancet 2016, 388, 2519–2531. [Google Scholar] [CrossRef]
- Scotet, V.; L’hostis, C.; Férec, C. The changing epidemiology of cystic fibrosis: Incidence, survival and impact of the CFTRGene discovery. Genes 2020, 11, 589. [Google Scholar] [CrossRef] [PubMed]
- Ernst, M.M.; Johnson, M.C.; Stark, L.J. Developmental and psychosocial issues in cystic fibrosis. Child Adolesc. Psychiatr. Clin. North Am. 2010, 19, 263–283. [Google Scholar] [CrossRef] [PubMed]
- Flume, P.A.; O’Sullivan, B.P.; Robinson, K.A.; Goss, C.H.; Mogayzel, P.J., Jr.; Willey-Courand, D.B.; Bujan, J.; Finder, J.; Lester, M.; Quittell, L.; et al. Cystic fibrosis pulmonary guidelines: Chronic medications for maintenance of lung health. Am. J. Respir. Crit. Care Med. 2007, 176, 957–969. [Google Scholar] [CrossRef] [PubMed]
- Mogayzel, P.J., Jr.; Naureckas, E.T.; Robinson, K.A.; Mueller, G.; Hadjiliadis, D.; Hoag, J.B.; Lubsch, L.; Hazle, L.; Sabadosa, K.; Marshall, B.; et al. Cystic fibrosis pulmonary guidelines: Chronic medications for maintenance of lung health. Am. J. Respir. Crit. Care Med. 2013, 187, 680–689. [Google Scholar] [CrossRef] [PubMed]
- Cerny, F. Exercise and cystic fibrosis (CF) 2.0. Pediatr. Exerc. Sci. 2013, 25, 616–623. [Google Scholar] [CrossRef]
- Radtke, T.; Smith, S.; Nevitt, S.J.; Hebestreit, H.; Kriemler, S. Physical activity and exercise training in cystic fibrosis. Cochrane Database Syst. Rev. 2022, 8, CD002768. [Google Scholar] [CrossRef]
- Li, S.; Douglas, T.; Fitzgerald, D.A. Psychosocial needs and interventions for young children with cystic fibrosis and their families. Paediatr. Respir. Rev. 2023, 46, 30–36. [Google Scholar] [CrossRef]
- Hegarty, M.; Macdonald, J.; Watter, P.; Wilson, C. Quality of life in young people with cystic fibrosis: Effects of hospitalization, age and gender, and differences in parent/child perceptions. Child Care Health Dev. 2009, 35, 462–468. [Google Scholar] [CrossRef] [PubMed]
- DiGirolamo, A.M.; Quittner, A.L.; Ackerman, V.; Stevens, J. Identification and assessment of ongoing stressors in adolescents with a chronic illness: An application of the behavior-analytic model. J. Clin. Child Psychol. 1997, 26, 53–66. [Google Scholar] [CrossRef] [PubMed]
- Goodfellow, N.A.; Hawwa, A.F.; Reid, A.J.M.; Horne, R.; Shields, M.D.; McElnay, J.C. Adherence to treatment in children and adolescents with cystic fibrosis: A cross-sectional, multi-method study investigating the influence of beliefs about treatment and parental depressive symptoms. BMC Pulm. Med. 2015, 15, 43. [Google Scholar] [CrossRef] [PubMed]
- Mahadeva, R.; Webb, K.; Westerbeek, R.C.; Carroll, N.R.; Dodd, M.E.; Bilton, D. Clinical outcome in relation to care in centres specialising in Cystic Fibrosis: Cross Sectional Study Commentary: Management in paediatric and adult cystic fibrosis centres improves clinical outcome. BMJ 1998, 316, 1771–1775. [Google Scholar] [CrossRef] [PubMed]
- Lebecque, P.; Leonard, A.; De Boeck, K.; De Baets, F.; Malfroot, A.; Casimir, G.; Desager, K.; Godding, V.; Leal, T. Early referral to cystic fibrosis specialist centre impacts on respiratory outcome. J. Cyst. Fibros. 2009, 8, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Rowbotham, N.J.; Palser, S.C.; Smith, S.J.; Smyth, A.R. Infection prevention and control in cystic fibrosis: A systematic review of interventions. Expert Rev. Respir. Med. 2019, 13, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Langton Hewer, S.C.; Smyth, A.R. Antibiotic strategies for eradicating Pseudomonas aeruginosa in people with cystic fibrosis. Cochrane Database Syst. Rev. 2014, 6, CD004197. [Google Scholar] [CrossRef] [PubMed]
- Jaclyn, D.; Andrew, N.; Ryan, P.; Julianna, B.; Christopher, S.; Nauman, C.; Powers, M.; Gregory, S.S.; George, M.S. Patient and family perceptions of telehealth as part of the cystic fibrosis care model during COVID-19. J. Cyst. Fibros. 2021, 20, e23–e28. [Google Scholar] [CrossRef] [PubMed]
- Serviços Partilhados do Ministério da Saúde. Plano Estratégico Nacional para a Telessaúde 2019–2022. 2019. Available online: https://www.spms.minsaude.pt/wp-content/uploads/2019/11/PENTS_português.pdf (accessed on 3 February 2024).
- Bland, K.A.; Bigaran, A.; Campbell, K.L.; Trevaskis, M.; Zopf, E.M. Exercising in Isolation? The Role of Telehealth in Exercise Oncology During the COVID-19 Pandemic and Beyond. Phys. Ther. 2020, 100, 1713–1716. [Google Scholar] [CrossRef]
- Omboni, S.; Campolo, L.; Panzeri, E. Telehealth in chronic disease management and the role of the Internet-of-Medical-Things: The Tholomeus® experience. Expert Rev. Med. Devices 2020, 17, 659–670. [Google Scholar] [CrossRef]
- Desimone, M.E.; Sherwood, J.; Soltman, S.C.; Moran, A. Telemedicine in cystic fibrosis. J. Clin. Transl. Endocrinol. 2021, 26, 100270. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.; Khalil, H. Chapter 11: Scoping Reviews (2020 version). In JBI Manual for Evidence Synthesis [Internet]; Aromataris, E., Munn, Z., Eds.; JBI Manual; JBI: Adelaide, SA, Australia, 2020; Available online: https://synthesismanual.jbi.global (accessed on 25 January 2024).
- Tricco, A.C.; Lillie, E.; Zarin, W. PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Valaitis, R.; Martin-Misener, R.; Wong, S.T.; MacDonald, M.; Meagher-Stewart, D.; Austin, P.; Kaczorowski, J.; Linda, O.; Savage, R. Methods, strategies and technologies used to conduct a scoping literature review of collaboration between primary care and public health. Prim. Health Care Res. Dev. 2012, 13, 219–236. [Google Scholar] [CrossRef] [PubMed]
- Del Corral, T.; Cebrià IIranzo, M.À.; López-de-Uralde-Villanueva, I.; Martínez-Alejos, R.; Blanco, I.; Vilaró, J. Effectiveness of a Home-Based Active Video Game Programme in Young Cystic Fibrosis Patients. Respiration 2018, 95, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Kenis-Coskun, Ö.; Aksoy, A.N.; Kumaş, E.N.; Yılmaz, A.; Güven, E.; Ayaz, H.H.; Sözer, T.; Ergenekon, A.P.; Karadağ-Saygı, E. The effect of telerehabilitation on quality of life, anxiety, and depression in children with cystic fibrosis and caregivers: A single-blind randomized trial. Pediatr. Pulmonol. 2022, 57, 1262–1271. [Google Scholar] [CrossRef] [PubMed]
- Chrysochoou, E.A.; Hatziagorou, E.; Kirvassilis, F.; Tsanakas, J. Telephone monitoring and home visits significantly improved the quality of life, treatment adherence and lung function in children with cystic fibrosis. Acta Paediatr. 2017, 106, 1882. [Google Scholar] [CrossRef] [PubMed]
- Costa, R.L.F.; Costa, R.F.; Gonçalves, C.P.; Cohen, R.W.F.; Santana, N.N. Telemedicine of patients with cystic fibrosis during the COVID-19 pandemic. Rev. Paul. Pediatr. 2022, 40, e2021118. [Google Scholar] [CrossRef] [PubMed]
- Seron, P.; Oliveros, M.-J.; Gutierrez-Arias, R.; Fuentes-Aspe, R.; Torres-Castro, R.C.; Merino-Osorio, C.; Nahuelhual, P.; Inostroza, J.; Jalil, Y.; Solano, R.; et al. Effectiveness of Telerehabilitation in Physical Therapy: A Rapid Overview. Phys. Ther. 2021, 101, pzab053. [Google Scholar] [CrossRef] [PubMed]
- Reis, N.; Costa Dias, M.J.; Sousa, L.; Canedo, F.; Rico, M.T.; Henriques, M.A.; Baixinho, C.L. Telerehabilitation Intervention in Transitional Care for People with COVID-19: Pre-Post Study with a Non-Equivalent Control Group. Healthcare 2023, 11, 2561. [Google Scholar] [CrossRef] [PubMed]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef]
- Bonfim, B.S.; Melo Filho, V.M.; Fontenelle, F.M.; Souza, E.L. Treatment adherence among children and adolescents in a cystic fibrosis reference center. Rev. Paul. Pediatr. 2020, 38, e2018338. [Google Scholar] [CrossRef] [PubMed]
- Simmich, J.; Deacon, A.J.; Russell, T.G. Active Video Games for Rehabilitation in Respiratory Conditions: Systematic Review and Meta-Analysis. JMIR Serious Games 2019, 7, e10116. [Google Scholar] [CrossRef] [PubMed]
- Pope, Z.; Zeng, N.; Gao, Z. The effects of active video games on patients’ rehabilitative outcomes: A meta-analysis. Prev. Med. 2017, 95, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Campos, N.E.; Heinzmann-Filho, J.P.; Becker, N.A.; Schiwe, D.; Gheller, M.F.; de Almeida, I.S.; Donadio, M.V.F. Evaluation of the exercise intensity generated by active video gaming in patients with cystic fibrosis and healthy individuals. J. Cyst. Fibros. 2020, 19, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Curran, M.; Tierney, A.; Button, B.; Collins, L.; Kennedy, L.; McDonnell, C.; Casserly, B.; Cahalan, R. The effectiveness of exercise interventions to increase physical activity in Cystic Fibrosis: A systematic review. J. Cyst. Fibros. 2022, 21, 272–281. [Google Scholar] [CrossRef] [PubMed]
- Girón, R.M.; Peláez, A.; Ibáñez, A.; Martínez-Besteiro, E.; Gómez-Punter, R.M.; Martínez-Vergara, A.; Ancochea, J.; Morell, A. Longitudinal Study of Therapeutic Adherence in a Cystic Fibrosis Unit: Identifying Potential Factors Associated with Medication Possession Ratio. Antibiotics 2022, 11, 1637. [Google Scholar] [CrossRef] [PubMed]
- Kimball, H.; Cobham, V.E.; Sanders, M.; Douglas, T. Procedural anxiety among children and adolescents with cystic fibrosis and their parents. Pediatr. Pulmonol. 2023, 58, 1967–1976. [Google Scholar] [CrossRef]
- Oliveira, E.S.F.; Baixinho, C.L.; Presado, M.H.C.V. Qualitative research in health: A reflexive approach. Rev. Bras. Enferm. 2019, 72, 830–831. [Google Scholar] [CrossRef]
- Tanner, K.; Bican, R.; Boster, J.; Christensen, C.; Coffman, C.; Fallieras, K.; Long, R.; Mansfield, C.; O’Rourke, S.; Pauline, L.; et al. Feasibility and Acceptability of Clinical Pediatric Telerehabilitation Services. Int. J. Telerehabilit. 2020, 12, 43–52. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).