Changes in MRI Workflow of Multiple Sclerosis after Introduction of an AI-Software: A Qualitative Study
Abstract
1. Introduction
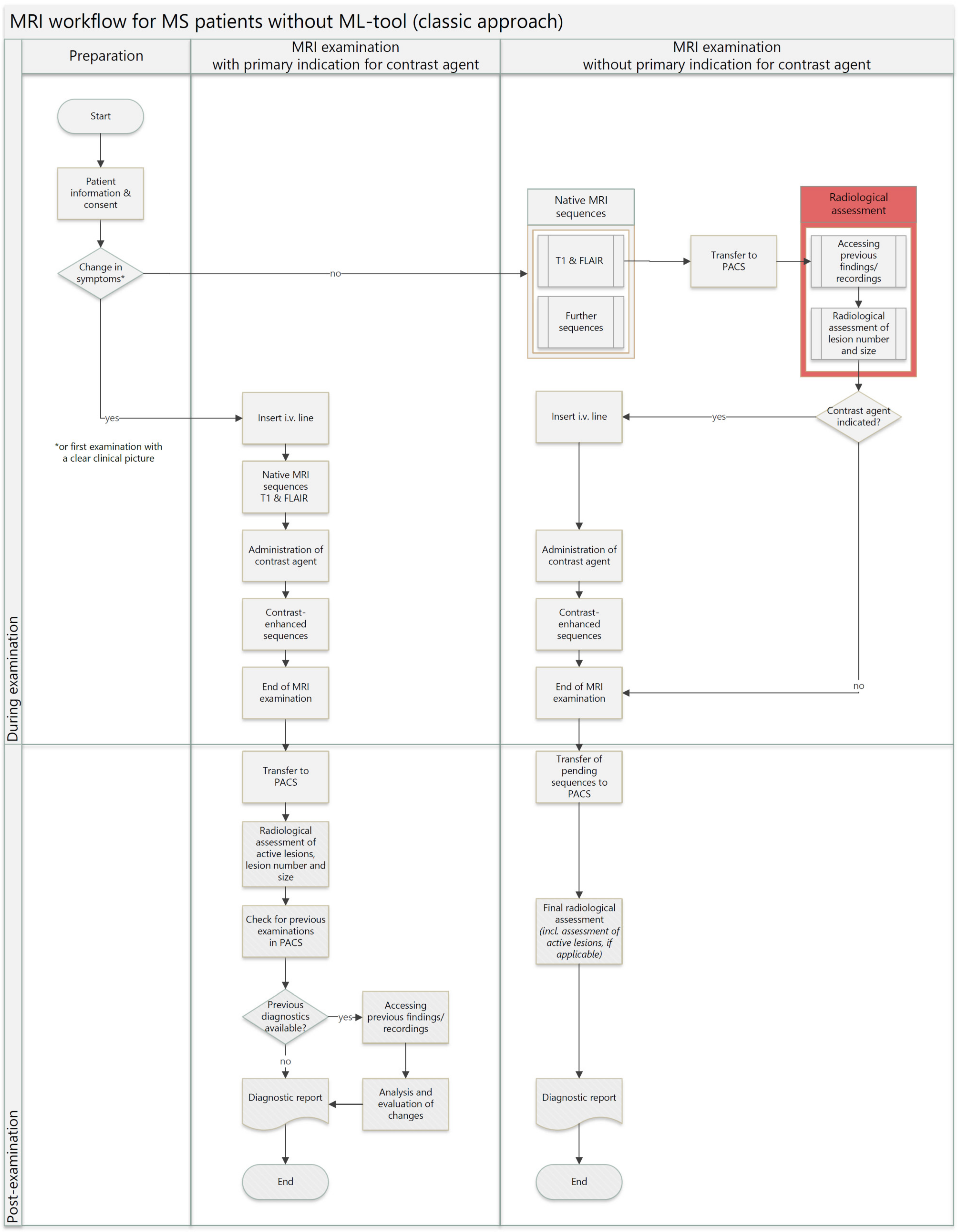
2. Materials and Methods
3. Results
- Workload and Efficiency:
Citation 1. “The process of decision-making is made significantly [...] less complicated. [The machine learning software] directs you as to which lesions to examine. [...] the task was shifted from ‘compare each and every spot’ to ‘check whether [the machine learning software] is correct in its assessment’.” (neuroradiologist)
Citation 2. “[...] For example, those lesions’ volumes are measured by [the machine learning software], which is simply impossible utilizing only examining them manually. [...] it, of course, alleviates having to do routine counting [of the lesions]. Whether they are really 52 or 54 small [lesions] in the brain, which you’d have to arduously count otherwise. […] It’s simply manual work which is taken over [by the machine learning software], and one therefore has more capability for other areas of work, which may require more physician expertise than counting lesions one by one.” (radiologist 1)
- 2.
- Systematic Errors vs. Human Interpretation:
Citation 3. “From my perspective, one would methodologically describe it as having a high negative predictive value. This algorithm detects many lesions that may not actually exist, but when the algorithm indicates ‘there is no new lesion’, there typically is indeed no new lesion. […] I always find that, at a qualitative level, there is a significant distinction when it comes to errors; [errors made by the machine learning software] tend to be systematic in nature. This is in contrast to a radiologist who might have good and bad days. The quality of their interpretation may differ when the radiologist writes the report first thing in the morning versus [...] at 10:30 p.m. in the evening. When [a patient] has 173 lesions, and now you’re [required] to find the 174th, it’s not ideal. In such cases, an algorithm ultimately proves to be not only faster but also more sensitive.” (neurologist)
- 3.
- Lesion Analysis and Communication:
Citation 4. “So, [the lesion load] is presented in a way that’s easy for patients to understand, which I think is excellent. I therefore believe the quality of communication between doctor and patient is improved through it. […] Communication between doctor and patient, in my opinion, seems to have decreased. This is because [communication] is not necessary in every case now. But communication now is perhaps a bit more targeted. […] I find the presentation of this report, as it is visually designed, to be very appealing, and it is some-thing that is highly accessible to patients.” (neurologist)
Citation 5. “Well, there’s less communication between doctor and patient before the MRI examination. However, if desired, communication after the examination is much faster and easier. […] The volume of the lesions measured by the machine-learning software is something I hadn’t previously noticed. [...] Measuring the volume of each individual lesion manually would be unrealistic and not feasible during the course of a shift.” (radiologist 2)
- 4.
- Time Savings and Workload Distribution:
Citation 6. “Additionally, the time it takes for the program to generate a report for me is roughly five minutes. [...] It would take [a reporting radiologist] significantly longer to manually do it at this level of thoroughness and conscientiousness. […] While the program is running in the background, the reporting radiologist is able to work, and then make an ad-hoc decision whether further MR sequences are necessary. This definitely saves a significant amount of time.” (radiologist 2)
Citation 7. “When new lesions are assessed by the machine-learning software, you can provide a precise description of their location, which wouldn’t be feasible with manual assessment. […] If you are familiar with the colors [which highlight each lesion’s location], the reporting radiologist can assess the report created by the program and form a preliminary result within less than ten seconds. Because it’s color-coded, you can immediately tell if a lesion is new or known. In clinical routine, the longest part [of the process] is usually waiting for the program’s report.” (radiologist 1)
- 5.
- Contrast Media
Citation 8. “[...] By allowing us to evaluate lesion load simultaneously [to the MRI], AI enables us to be more flexible in decision-making on whether we want to add contrast-enhanced sequences. [This] is advantageous in avoiding unnecessary placement of intravenous cannula and administration of medication.” (radiologist 1)
Citation 9. “The program quickly helps me decide whether to administer the contrast agent or not, and I believe this really does reduce the use of contrast-agent in general.” (physicians 2)
- 6.
- Drawbacks and Difficulties
Citation 10. “The ML software usually detects a little more than I do, but sometimes those are lesions that aren’t actually real; they’re just MRI artifacts that occur. So, I critically examine them to determine whether they’re genuine or not.” (radiologist 2)
Citation 11. “We had initial issues with the lesions located in the posterior cranial fossa. It’s already a bit better. It’s not yet optimal, but it has improved. So, I know I need to check ML findings here.” (radiologist 1)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Acronym | Full form |
| AI | artificial intelligence |
| HIS/RIS | hospital/radiologic imaging system |
| ML | machine learning |
| MR | magnet resonance |
| MRI | magnet resonance imaging |
| MS | multiple sclerosis |
| PACS | picture archiving and communication system |
| PPMS | primary-progressive multiple sclerosis |
| PRMS | progressive-relapsing multiple sclerosis |
| RRMS | relapsing-remitting multiple sclerosis |
| SPMS | secondary-progressive multiple sclerosis |
| TE | echo time |
| TR | repetition time |
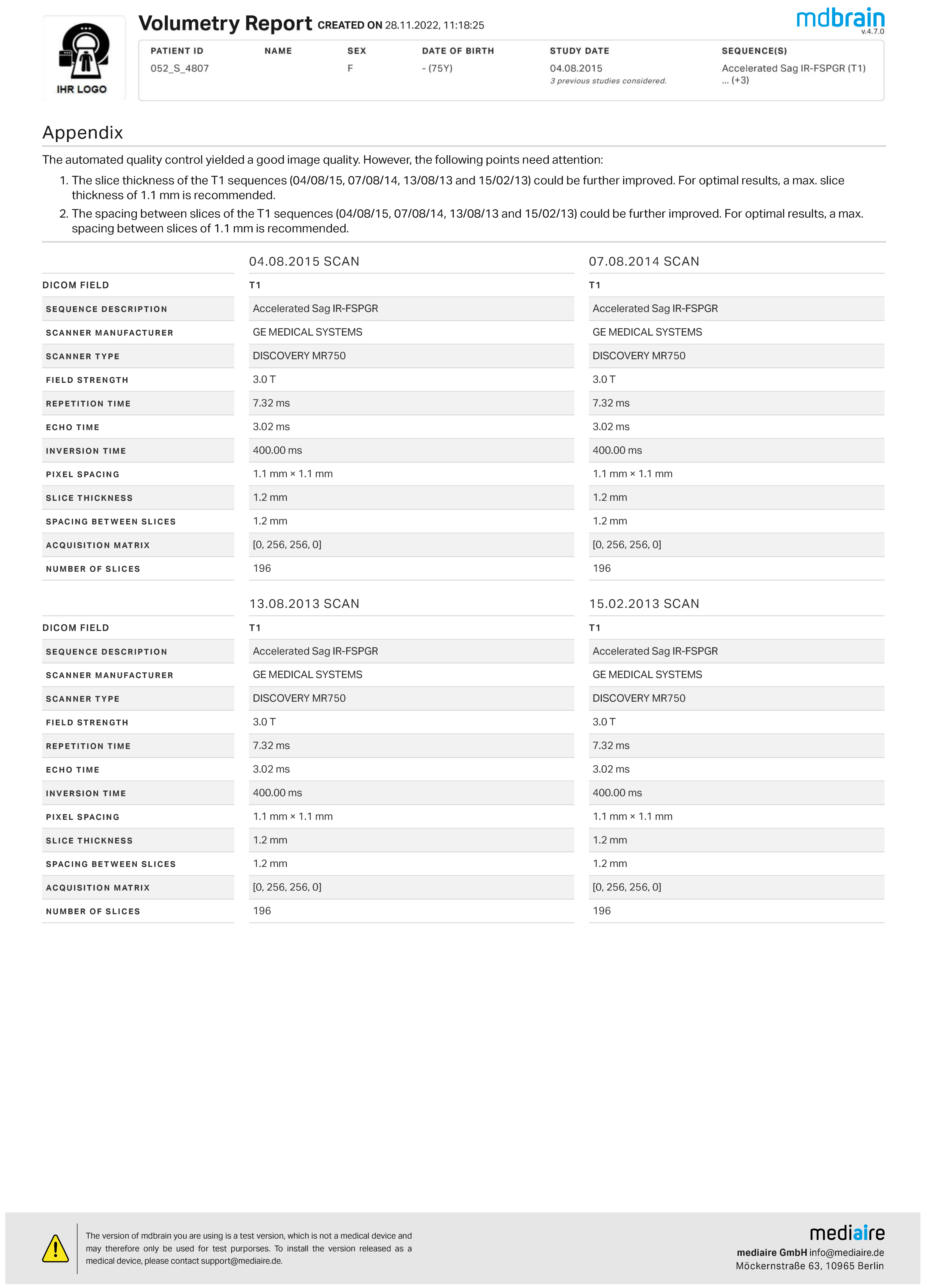
Appendix A. Volumetric Report Mdbrain


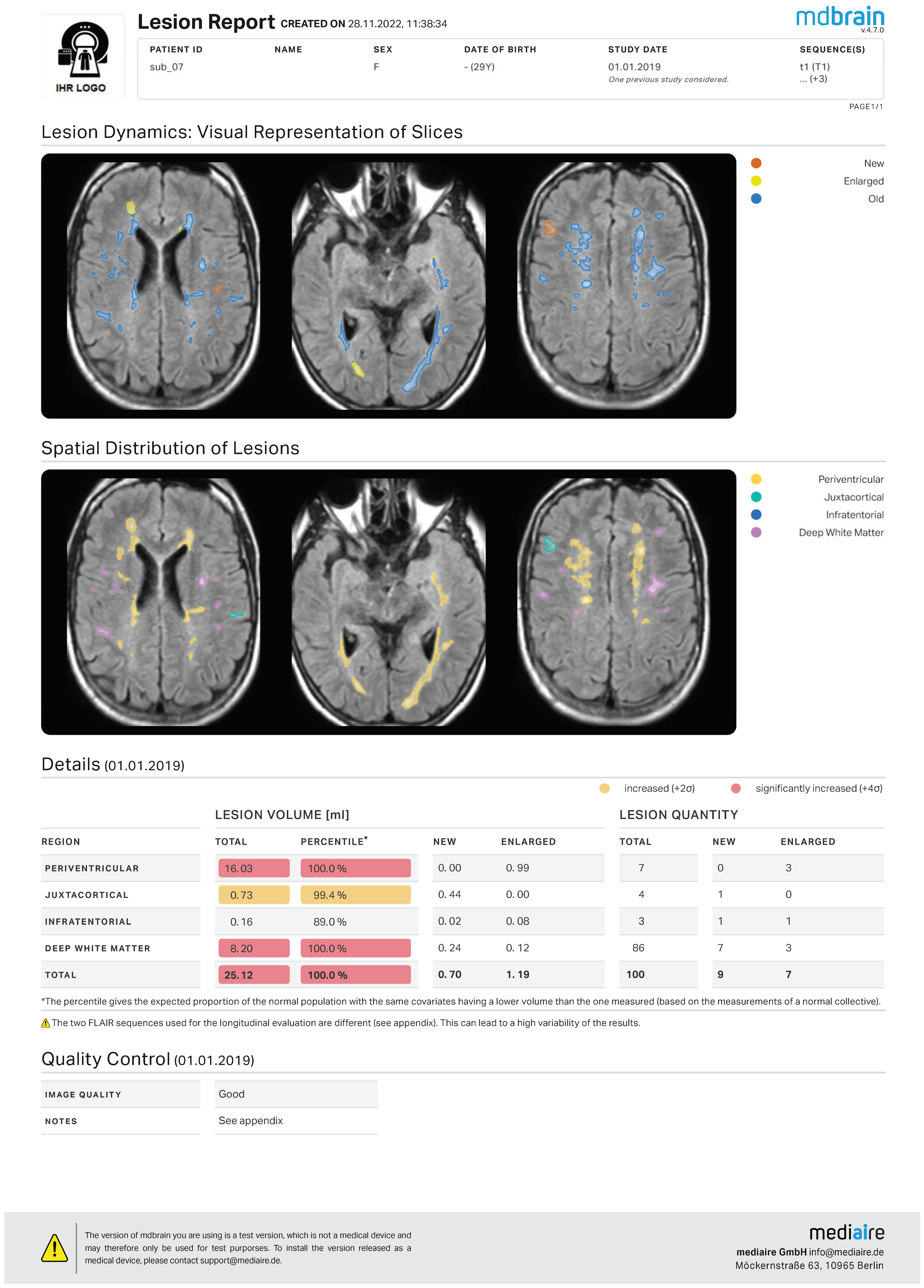
Appendix B. Lesion Report Mdbrain

References
- Thompson, A.J.; Baranzini, S.E.; Geurts, J.; Hemmer, B.; Ciccarelli, O. Multiple Sclerosis. Lancet 2018, 391, 1622–1636. [Google Scholar] [CrossRef] [PubMed]
- Lublin, F.D.; Reingold, S.C.; Cohen, J.A.; Cutter, G.R.; Sorensen, P.S.; Thompson, A.J.; Wolinsky, J.S.; Balcer, L.J.; Banwell, B.; Barkhof, F.; et al. Defining the Clinical Course of Multiple Sclerosis: The 2013 Revisions. Neurology 2014, 83, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Tafti, D.; Ehsan, M.; Xixis, K.L. Multiple Sclerosis. In Nbk499849; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Walton, C.; King, R.; Rechtman, L.; Kaye, W.; Leray, E.; Marrie, R.A.; Robertson, N.; La Rocca, N.; Uitdehaag, B.; Van Der Mei, I.; et al. Rising Prevalence of Multiple Sclerosis Worldwide: Insights from the Atlas of Ms, Third Edition. Mult. Scler. 2020, 26, 1816–1821. [Google Scholar] [CrossRef] [PubMed]
- Weidauer, S.; Raab, P.; Hattingen, E. Diagnostic Approach in Multiple Sclerosis with Mri: An Update. Clin. Imaging 2021, 78, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Wattjes, M.P.; Ciccarelli, O.; Reich, D.S.; Banwell, B.; de Stefano, N.; Enzinger, C.; Fazekas, F.; Filippi, M.; Frederiksen, J.; Gasperini, C.; et al. 2021 Magnims-Cmsc-Naims Consensus Recommendations on the Use of Mri in Patients with Multiple Sclerosis. Lancet Neurol. 2021, 20, 653–670. [Google Scholar] [CrossRef]
- Traboulsee, A.; Simon, J.; Stone, L.; Fisher, E.; Jones, D.; Malhotra, A.; Newsome, S.; Oh, J.; Reich, D.; Richert, N.; et al. Revised Recommendations of the Consortium of Ms Centers Task Force for a Standardized Mri Protocol and Clinical Guidelines for the Diagnosis and Follow-up of Multiple Sclerosis. AJNR Am. J. Neuroradiol. 2016, 37, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Holstiege, J.; Akmatov, M.K.; Klimke, K.; Dammertz, L.; Kohring, C.; Marx, C.; Frahm, N.; Peters, M.; Ellenberger, D.; Zettl, U.K.; et al. Trends in Administrative Prevalence of Multiple Sclerosis and Utilization Patterns of Disease Modifying Drugs in Germany. Mult. Scler. Relat. Disord. 2022, 59, 103534. [Google Scholar] [CrossRef] [PubMed]
- Molwitz, I.; Kemper, C.; Stahlmann, K.; Oechtering, T.H.; Sieren, M.M.; Afat, S.; Gerwing, M.; Bucher, A.M.; Storz, C.; Langenbach, M.C.; et al. Work Expectations, Their Fulfillment, and Exhaustion among Radiologists of All Career Levels: What Can Be Learned from the Example of Germany. Eur. Radiol. 2023, 33, 5664–5674. [Google Scholar] [CrossRef] [PubMed]
- Griffith, B.; Kadom, N.; Straus, C.M. Radiology Education in the 21st Century: Threats and Opportunities. J. Am. Coll. Radiol. 2019, 16, 1482–1487. [Google Scholar] [CrossRef]
- Aldoseri, A.; Al-Khalifa, K.N.; Hamouda, A.M. Re-Thinking Data Strategy and Integration for Artificial Intelligence: Concepts, Opportunities, and Challenges. Appl. Sci. 2023, 13, 7082. [Google Scholar] [CrossRef]
- Sorantin, E.; Grasser, M.G.; Hemmelmayr, A.; Tschauner, S.; Hrzic, F.; Weiss, V.; Lacekova, J.; Holzinger, A. The Augmented Radiologist: Artificial Intelligence in the Practice of Radiology. Pediatr. Radiol. 2022, 52, 2074–2086. [Google Scholar] [CrossRef]
- Duong, M.T.; Rauschecker, A.M.; Mohan, S. Diverse Applications of Artificial Intelligence in Neuroradiology. Neuroimaging Clin. N. Am. 2020, 30, 505–516. [Google Scholar] [CrossRef]
- Afzal, H.M.R.; Luo, S.; Ramadan, S.; Lechner-Scott, J. The Emerging Role of Artificial Intelligence in Multiple Sclerosis Imaging. Mult. Scler. 2022, 28, 849–858. [Google Scholar] [CrossRef]
- Mendelsohn, Z.; Pemberton, H.G.; Gray, J.; Goodkin, O.; Carrasco, F.P.; Scheel, M.; Nawabi, J.; Barkhof, F. Commercial Volumetric Mri Reporting Tools in Multiple Sclerosis: A Systematic Review of the Evidence. Neuroradiology 2023, 65, 5–24. [Google Scholar] [CrossRef]
- Aruci, M.; Dünnwald, M.; Schreiber, F.; Sciarra, A.; Maass, A.; Schreiber, S.; Oeltze-Jafra, S. Challenging Cases for Wmh Segmentation Comparatively Processed by Seven Automated Methods. Clin. Neuroradiol. 2021, 31, 40–41. [Google Scholar]
- Hock, S.; Marterstock, D.C.; Meyer, A.L.; Bettray, C.; Huhn, K.; Rothhammer, V.; Dörfler, A.; Schmidt, M. Latest Artificial Intelligence Provides Fast, Accurate and Consistent Detection of Multiple Sclerosis Lesions. Clin. Neuroradiol. 2021, 31, 41–42. [Google Scholar]
- Bruno, F.; Tommasino, E.; Catalucci, A.; Pastorelli, C.; Borea, F.; Caldarelli, G.; Bellini, M.; Badini, P.; Mancini, S.; Santobuono, C.; et al. Evaluation of Cerebral Volume Changes in Patients with Tremor Treated by Mrgfus Thalamotomy. Life 2022, 13, 16. [Google Scholar] [CrossRef]
- Bendella, Z.; Widmann, C.N.; Layer, J.P.; Layer, Y.L.; Haase, R.; Sauer, M.; Bieler, L.; Lehnen, N.C.; Paech, D.; Heneka, M.T.; et al. Brain Volume Changes after Covid-19 Compared to Healthy Controls by Artificial Intelligence-Based Mri Volumetry. Diagnostics 2023, 13, 1716. [Google Scholar] [CrossRef]
- Purrer, V.; Pohl, E.; Lueckel, J.M.; Borger, V.; Sauer, M.; Radbruch, A.; Wüllner, U.; Schmeel, F.C. Artificial-Intelligence-Based Mri Brain Volumetry in Patients with Essential Tremor and Tremor-Dominant Parkinson’s Disease. Brain Commun. 2023, 5, fcad271. [Google Scholar] [CrossRef]
- Mediaire. Mdbrain—Your Upgrade for Mri Diagnostics in Neuroradiology. Available online: https://mediaire.ai/en/mdbrain/ (accessed on 21 March 2024).
- Waller, J.; O’connor, A.; Raafat, E.; Amireh, A.; Dempsey, J.; Martin, C.; Umair, M. Applications and Challenges of Artificial Intelligence in Diagnostic and Interventional Radiology. Pol. J. Radiol. 2022, 87, e113–e117. [Google Scholar] [CrossRef]
- Bara, M.T.G.; Gallardo-Higueras, A.; Moreno, E.M.; Laffond, E.; Bellido, F.J.M.; Martin, C.; Sobrino, M.; Macias, E.; Arriba-Méndez, S.; Castillo, R.; et al. Hypersensitivity to Gadolinium-Based Contrast Media. Front. Allergy 2022, 3, 813927. [Google Scholar] [CrossRef] [PubMed]
- Khairinisa, M.A.; Ariyani, W.; Tsushima, Y.; Koibuchi, N. Effects of Gadolinium Deposits in the Cerebellum: Reviewing the Literature from in Vitro Laboratory Studies to in Vivo Human Investigations. Int. J. Environ. Res. Public Health 2021, 18, 7214. [Google Scholar] [CrossRef] [PubMed]
- Zivadinov, R.; Bergsland, N.; Hagemeier, J.; Ramasamy, D.P.; Dwyer, M.G.; Schweser, F.; Kolb, C.; Weinstock-Guttman, B.; Hojnacki, D. Cumulative Gadodiamide Administration Leads to Brain Gadolinium Deposition in Early Ms. Neurology 2019, 93, e611–e623. [Google Scholar] [CrossRef]
- Mattay, R.; Davtyan, K.; Bilello, M.; Mamourian, A. Do All Patients with Multiple Sclerosis Benefit from the Use of Contrast on Serial Follow-up Mr Imaging? A Retrospective Analysis. AJNR Am. J. Neuroradiol. 2018, 39, 2001–2006. [Google Scholar] [CrossRef] [PubMed]
- Loma, I.; Heyman, R. Multiple Sclerosis: Pathogenesis and Treatment. Curr. Neuropharmacol. 2011, 9, 409–416. [Google Scholar] [CrossRef]
- Beer, P.; Mulder, R.H. The Effects of Technological Developments on Work and Their Implications for Continuous Vocational Education and Training: A Systematic Review. Front. Psychol. 2020, 11, 918. [Google Scholar] [CrossRef]
- Tenny, S.; Brannan, J.M.; Brannan, G.D. Qualitative Study; Statpearls: Treasure Island, FL, USA, 2024. [Google Scholar]
- Council of the European Union. Council Directive 93/42/Eec of 14 June 1993 Concerning Medical Devices; Council of the European Union: Brussels, Belgium, 1993. [Google Scholar]
- DIN EN ISO 13485: 2021; Medical Devices—Quality Management Systems-Requirements for Regulatory Purposes (Iso 13485:2016) (Includes Corrigendum:2018). Deutsches Institut für Normung: Berlin, Germany, 2016.
- Hitziger, S.; Ling, W.X.; Fritz, T.; D’Albis, T.; Lemke, A.; Grilo, J. Triplanar U-Net with Lesion-Wise Voting for the Segmentation of New Lesions on Longitudinal Mri Studies. Front. Neurosci. 2022, 16, 964250. [Google Scholar] [CrossRef]
- M-Kis, Version 7.2.2; Meierhofer GmbH: Leipzig, Germany, 2019.
- Radcentre, Version 70.0.15115.0; Mesalvo: Freiburg, Germany, 2019.
- Bonacchi, R.; Filippi, M.; Rocca, M.A. Role of Artificial Intelligence in Ms Clinical Practice. Neuroimage Clin. 2022, 35, 103065. [Google Scholar] [CrossRef]
- Barnett, M.; Wang, D.; Beadnall, H.; Bischof, A.; Brunacci, D.; Butzkueven, H.; Brown, J.W.L.; Cabezas, M.; Das, T.; Dugal, T.; et al. A Real-World Clinical Validation for Ai-Based Mri Monitoring in Multiple Sclerosis. NPJ Digit. Med. 2023, 6, 196. [Google Scholar] [CrossRef] [PubMed]
- Haller, S.; Haacke, E.M.; Thurnher, M.M.; Barkhof, F. Susceptibility-Weighted Imaging: Technical Essentials and Clinical Neurologic Applications. Radiology 2021, 299, 3–26. [Google Scholar] [CrossRef]
- Sparacia, G.; Agnello, F.; Gambino, A.; Sciortino, M.; Midiri, M. Multiple Sclerosis: High Prevalence of the ‘Central Vein’ Sign in White Matter Lesions on Susceptibility-Weighted Images. Neuroradiol. J. 2018, 31, 356–361. [Google Scholar] [CrossRef]
- Elliott, C.; A Rudko, D.; Arnold, D.L.; Fetco, D.; Elkady, A.M.; Araujo, D.; Zhu, B.; Gafson, A.; Tian, Z.; Belachew, S.; et al. Lesion-Level Correspondence and Longitudinal Properties of Paramagnetic Rim and Slowly Expanding Lesions in Multiple Sclerosis. Mult. Scler. 2023, 29, 680–690. [Google Scholar] [CrossRef] [PubMed]
- Krajnc, N.; Schmidbauer, V.; Leinkauf, J.; Haider, L.; Bsteh, G.; Kasprian, G.; Leutmezer, F.; Kornek, B.; Rommer, P.S.; Berger, T.; et al. Paramagnetic Rim Lesions Lead to Pronounced Diffuse Periplaque White Matter Damage in Multiple Sclerosis. Mult. Scler. 2023, 29, 1406–1417. [Google Scholar] [CrossRef]
- Brand, J.; Kopke, S.; Kasper, J.; Rahn, A.; Backhus, I.; Poettgen, J.; Stellmann, J.P.; Siemonsen, S.; Heesen, C. Magnetic Resonance Imaging in Multiple Sclerosis—Patients’ Experiences, Information Interests and Responses to an Education Programme. PLoS ONE 2014, 9, e113252. [Google Scholar] [CrossRef] [PubMed]
- Van Hecke, W.; Costers, L.; Descamps, A.; Ribbens, A.; Nagels, G.; Smeets, D.; Sima, D.M. A Novel Digital Care Management Platform to Monitor Clinical and Subclinical Disease Activity in Multiple Sclerosis. Brain Sci. 2021, 11, 1171. [Google Scholar] [CrossRef] [PubMed]
- Nabizadeh, F.; Ramezannezhad, E.; Kargar, A.; Sharafi, A.M.; Ghaderi, A. Diagnostic Performance of Artificial Intelligence in Multiple Sclerosis: A Systematic Review and Meta-Analysis. Neurol. Sci. 2023, 44, 499–517. [Google Scholar] [CrossRef]
- Lang, K.; Josefsson, V.; Larsson, A.-M.; Larsson, S.; Högberg, C.; Sartor, H.; Hofvind, S.; Andersson, I.; Rosso, A. Artificial Intelligence-Supported Screen Reading Versus Standard Double Reading in the Mammography Screening with Artificial Intelligence Trial (Masai): A Clinical Safety Analysis of a Randomised, Controlled, Non-Inferiority, Single-Blinded, Screening Accuracy Study. Lancet Oncol. 2023, 24, 936–944. [Google Scholar]


| Variable | n | Mean | SD | Min | Median | Max | ∆Mean (95% CI) | p-Value |
|---|---|---|---|---|---|---|---|---|
| Number of lesions | 21 | 39.62 | 26.39 | 11 | 34 | 103 | - | - |
| w/o ML [s] | 25 | 295.5 | 149.2 | 73.0 | 283.0 | 625.0 | 0 | - |
| w ML (1) [s] | 21 | 101.60 | 44.32 | 53.00 | 90.00 | 221.00 | 193.88 ** (130.10–257.66) | <0.001 |
| w ML (2) [s] | 21 | 68.80 | 29.94 | 36.00 | 55.00 | 139.00 | 226.68 ** (163.88–289.48) | <0.001 |
| avg. w ML [s] | 21 | 82.40 | 34.70 | 49.00 | 68.00 | 180.00 | 210.28 ** (147.30–273.26) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rathmann, E.; Hemkemeier, P.; Raths, S.; Grothe, M.; Mankertz, F.; Hosten, N.; Flessa, S. Changes in MRI Workflow of Multiple Sclerosis after Introduction of an AI-Software: A Qualitative Study. Healthcare 2024, 12, 978. https://doi.org/10.3390/healthcare12100978
Rathmann E, Hemkemeier P, Raths S, Grothe M, Mankertz F, Hosten N, Flessa S. Changes in MRI Workflow of Multiple Sclerosis after Introduction of an AI-Software: A Qualitative Study. Healthcare. 2024; 12(10):978. https://doi.org/10.3390/healthcare12100978
Chicago/Turabian StyleRathmann, Eiko, Pia Hemkemeier, Susan Raths, Matthias Grothe, Fiona Mankertz, Norbert Hosten, and Steffen Flessa. 2024. "Changes in MRI Workflow of Multiple Sclerosis after Introduction of an AI-Software: A Qualitative Study" Healthcare 12, no. 10: 978. https://doi.org/10.3390/healthcare12100978
APA StyleRathmann, E., Hemkemeier, P., Raths, S., Grothe, M., Mankertz, F., Hosten, N., & Flessa, S. (2024). Changes in MRI Workflow of Multiple Sclerosis after Introduction of an AI-Software: A Qualitative Study. Healthcare, 12(10), 978. https://doi.org/10.3390/healthcare12100978









