Cost–Utility Analysis of 3-Month Telemedical Intervention for Heart Failure Patients: A Preliminary Study from Poland
Abstract
:1. Introduction
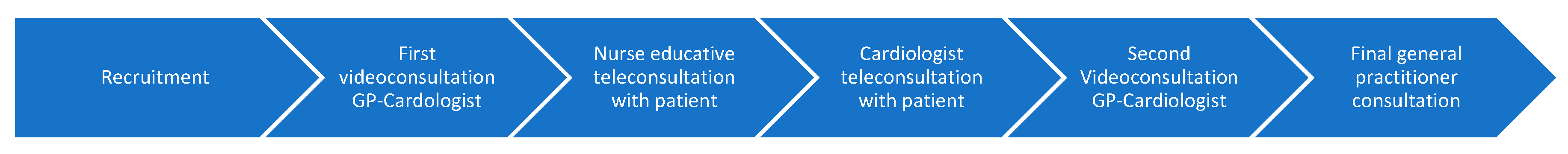
2. Materials and Methods
2.1. Resulting Study Pool and Variables
2.2. Data Analysis
2.3. Ethics
3. Results
3.1. Descriptive Characteristics
3.1.1. QALY Difference between Basic Supportive Care and Basic Supportive Care Aided by Telemedicine
3.1.2. Cost Comparison between Basic Supportive Care and Basic Supportive Care Aided by Telemedicine
3.2. Cost–Utility of Telemedical Intervention
4. Limitations
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bozkurt, B.; Coats, A.J.; Tsutsui, H.; Abdelhamid, M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Böhm, M.; Butler, J.; et al. Universal Definition and Classification of Heart Failure: A Report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J. Card Fail. 2021, 27, 387–413. [Google Scholar] [CrossRef]
- Lippi, G.; Fabián, S.G. Global epidemiology and future trends of heart failure. AME Med. J. 2020, 5, 15. [Google Scholar] [CrossRef]
- Krawczyk, K.; Nessler, J. Nowe praktyczne rozwiązania w leczeniu pacjentów z niewydolnością serca. Lekarz POZ 2023, 9, 61–70. [Google Scholar]
- Kałużna-Oleksy, M.; Bartoli, K.; Bukowski, H. Niewydolność Serca w Polsce. Realia, Koszty, Sugestie Poprawy Sytuacji; Instytut Innowacji i Odpowiedzialnego Rozwoju: Warszawa, Poland, 2020. [Google Scholar]
- OECD. Congestive heart failure hospital admission in adults, 2011, 2019 and 2021 (or nearest years). In Health at a Glance 2023: OECD Indicators; OECD Publishing: Paris, France, 2023. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef] [PubMed]
- Silva-Cardoso, J.; Juanatey, J.R.G.; Comin-Colet, J.; Sousa, J.M.; Cavalheiro, A.; Moreira, E. The Future of Telemedicine in the Management of Heart Failure Patients. Card. Fail. Rev. 2021, 7, e11. [Google Scholar] [CrossRef] [PubMed]
- Scherrenberg, M.; Vangenechten, G.; Janssen, A.; Dendale, P. What Is the Value of Digital Tools for Cardiovascular Patients? A Comprehensive Review of Evidence for Effectiveness and Cost-Effectiveness for Prevention and Management. European Heart Network. 12 July 2020. Available online: http://ehnheart.org/wp-content/uploads/2023/08/2020.07_Digital_tools_CVD_EHN-paper_long-version.pdf (accessed on 5 April 2024).
- Acheampong, F.; Vimarlund, V. Business models for telemedicine services: A literature review. Health Syst. 2015, 4, 189–203. [Google Scholar] [CrossRef]
- Velayati, F.; Ayatollahi, H.; Hemmat, M.; Dehghan, R. Telehealth Business Models and Their Components: Systematic Review. J. Med. Internet Res. 2022, 24, e33128. [Google Scholar] [CrossRef] [PubMed]
- Lundgren, K.M.; Langlo, K.A.R.; Salvesen, Ø.; Zanaboni, P.; Cittanti, E.; Mo, R.; Ellingsen, Ø.; Dalen, H.; Aksetøy, I.A. Feasibility of telerehabilitation for heart failure patients inaccessible for outpatient rehabilitation. ESC Heart Fail. 2023, 10, 2406–2417. [Google Scholar] [CrossRef]
- Golicki, D.; Jakubczyk, M.; Graczyk, K.; Niewada, M. Valuation of EQ-5D-5L Health States in Poland: The First EQ-VT-Based Study in Central and Eastern Europe. Pharmacoeconomics 2019, 37, 1165–1176. [Google Scholar] [CrossRef]
- Turner, H.C.; Archer, R.A.; Downey, L.E.; Isaranuwatchai, W.; Chalkidou, K.; Jit, M.; Teerawattananon, Y. An Introduction to the Main Types of Economic Evaluations Used for Informing Priority Setting and Resource Allocation in Healthcare: Key Features, Uses, and Limitations. Front. Public Health 2021, 9, 722927. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Obwieszczenie Ministra Zdrowia z dnia 30 sierpnia 2023 r. w sprawie wykazu refundowanych leków, środków spożywczych specjalnego przeznaczenia żywieniowego oraz wyrobów medycznych na 1 września 2023 r. 2023. Available online: https://www.gov.pl/web/zdrowie/obwieszczenie-ministra-zdrowia-z-dnia-30-sierpnia-2023-r-w-sprawie-wykazu-refundowanych-lekow-srodkow-spozywczych-specjalnego-przeznaczenia-zywieniowego-oraz-wyrobow-medycznych-na-1-wrzesnia-2023-r (accessed on 5 April 2024).
- Tallarida, R.J.; Murray, R.B. Area under a curve: Trapezoidal and Simpson’s rules. In Manual of Pharmacologic Calculations; Springer: London, UK, 1987; pp. 77–81. [Google Scholar] [CrossRef]
- Glory Apantaku B.Sc. HOME TELEMONITORING IN PATIENTS WITH HEART FAILURE A COST CONSEQUENCE ANALYSIS AND NARRATIVE SYSTEMATIC REVIEW, A THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE IN THE FACULTY OF GRADUATE AND POSTDOCTORAL STUDIES (Population and Public Health) THE UNIVERSITY OF BRITISH COLUMBIA. 2019. Available online: https://open.library.ubc.ca/media/stream/pdf/24/1.0380498/4 (accessed on 5 April 2024).
- Regan, J.A.; Kitzman, D.W.; Leifer, E.S.; Kraus, W.E.; Fleg, J.L.; Forman, D.E.; Whellan, D.J.; Wojdyla, D.; Parikh, K.; O’Connor, C.M.; et al. Impact of Age on Comorbidities and Outcomes in Heart Failure with Reduced Ejection Fraction. JACC Heart Fail. 2019, 7, 1056–1065. [Google Scholar] [CrossRef] [PubMed]
- Roalfe, A.K.; Taylor, C.J.; Hobbs, F.D.R. Long term changes in health-related quality of life for people with heart failure: The ECHOES study. ESC Heart Fail. 2023, 10, 211–222. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Calvin, A.D.; Alan; Berger, K.; Vazquez, G.; Susan; Duval, J.; Nelson, A.F.; Luepker, R.V. Effect of Age on Quality of Life in Heart Failure. J. Card. Fail. 2007, 13 (Supplement 2), S160–S161. [Google Scholar] [CrossRef]
- Jia, H.; Lubetkin, E.I. Time trends and seasonal patterns of health-related quality of life among U.S. adults. Public Health Rep. 2009, 124, 692–701. [Google Scholar] [CrossRef]
- Imberti, J.F.; Tosetti, A.; Mei, D.A.; Maisano, A.; Boriani, G. Remote monitoring and telemedicine in heart failure: Implementation and benefits. Curr. Cardiol. Rep. 2021, 23, 55. [Google Scholar] [CrossRef]
- Kruse, C.S.; Soma, M.; Pulluri, D.; Nemali, N.T.; Brooks, M. The effectiveness of telemedicine in the management of chronic heart disease—A systematic review. JRSM Open. 2017, 8. [Google Scholar] [CrossRef]
- Lin, M.; Yuan, W.; Huang, T.; Zhang, H.; Mai, J.; Wang, J. Clinical Effectiveness of Telemedicine for Chronic Heart Failure: A Systematic Review and Meta-Analysis. J. Investig. Med. 2017, 65, 899–911. [Google Scholar] [CrossRef]
- Hale, T.M.; Jethwani, K.; Kandola, M.S.; Saldana, F.; Kvedar, J.C. A remote medication monitoring system for chronic heart failure patients to reduce readmissions: A two-arm randomized pilot study. J. Med. Internet Res. 2016, 18, e5256. [Google Scholar] [CrossRef]
- Kotb, A.; Cameron, C.; Hsieh, S.; Wells, G. Comparative effectiveness of different forms of telemedicine for individuals with heart failure (HF): A systematic review and network meta-analysis. PLoS ONE 2015, 10, e0118681. [Google Scholar] [CrossRef]
- Ong, M.K.; Romano, P.S.; Edgington, S.; Aronow, H.U.; Auerbach, A.D.; Black, J.T.; De Marco, T.; Escarce, J.J.; Evangelista, L.S.; Hanna, B.; et al. Effectiveness of remote patient monitoring after discharge of hospital patients with heart failure: The better effectiveness after transition—Heart Failure (BEAT-HF) randomized clinical trial. J. Am. Med. Assoc. Intern. Med. 2016, 176, 310–318. [Google Scholar] [CrossRef]
- Koehler, F.; Koehler, K.; Deckwart, O.; Prescher, S.; Wegscheider, K.; Kirwan, B.-A.; Winkler, S.; Vettorazzi, E.; Bruch, C.; Oeff, M.; et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): A randomized controlled, parallel-group, unmasked trial. Lancet 2018, 392, 1047–1057. [Google Scholar] [CrossRef] [PubMed]
- Long, G.; Babbitt, A.; Cohn, T. Impact of home telemonitoring on 30-Day hospital readmission rates for patients with heart failure: A systematic review. MedSurg Nurs. 2017, 26, 337–348. [Google Scholar]
- Rabbe, S.; Blankart, C.R.; Franz, W.M.; Hager, L.; Schreyögg, J. Impact of a telemonitoring intervention in patients with chronic heart failure in Germany: A difference-in-difference matching approach using real-world data. J. Telemed Telecare 2023, 29, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Indraratna, P.; Biswas, U.; McVeigh, J.; Mamo, A.; Magdy, J.; Vickers, D.; Watkins, E.; Ziegl, A.; Liu, H.; Cholerton, N.; et al. A Smartphone-Based Model of Care to Support Patients with Cardiac Disease Transitioning From Hospital to the Community (TeleClinical Care): Pilot Randomized Controlled Trial. JMIR Mhealth Uhealth 2022, 10, e32554. [Google Scholar] [CrossRef]
- Kędzierski, K.; Radziejewska, J.; Sławuta, A.; Wawrzyńska, M.; Arkowski, J. Telemedicine in Cardiology: Modern Technologies to Improve Cardiovascular Patients’ Outcomes—A Narrative Review. Medicina 2022, 58, 210. [Google Scholar] [CrossRef]
- Grustam, A.S.; Severens, J.L.; van Nijnatten, J.; Koymans, R.; Vrijhoef, H.J.M. Cost-effectiveness of telehealth interventions for chronic heart failure patients: A literature review. Int. J. Technol. Assess. Health Care 2014, 30, 59–68. [Google Scholar] [CrossRef]
- Zanaboni, P.; Landolina, M.; Marzegalli, M.; Lunati, M.; Perego, G.B.; Guenzati, G.; Curnis, A.; Valsecchi, S.; Borghetti, F.; Borghi, G.; et al. Cost-Utility Analysis of the EVOLVO Study on Remote Monitoring for Heart Failure Patients with Implantable Defibrillators: Randomized Controlled Trial. J. Med. Internet Res. 2013, 15, e106. [Google Scholar] [CrossRef]
- Niewada, M.; Tabor, B.; Piotrowicz, E.; Piotrowicz, R.; Opolski, G.; Banach, M.; Jakubczyk, M. Cost-effectiveness of telerehabilitation in patients with heart failure in Poland: An analysis based on the results of Telerehabilitation in the Heart Failure Patients (TELEREH-HF) randomized clinical trial. Kardiol. Pol. 2021, 79, 510–516. [Google Scholar] [CrossRef]
- Hwang, R.; Morris, N.R.; Mandrusiak, A.; Bruning, J.; Peters, R.; Korczyk, D.; Russell, T. Cost-Utility Analysis of Home-Based Telerehabilitation Compared with Centre-Based Rehabilitation in Patients with Heart Failure. Heart Lung Circ. 2019, 28, 1795–1803. [Google Scholar] [CrossRef] [PubMed]
- Caillon, M.; Sabatier, R.; Legallois, D.; Courouve, L.; Donio, V.; Boudevin, F.; de Chalus, T.; Hauchard, K.; Belin, A.; Milliez, P. A telemonitoring programme in patients with heart failure in France: A cost-utility analysis. BMC Cardiovasc. Disord. 2022, 22, 441. [Google Scholar] [CrossRef]
- Boodoo, C.; Zhang, Q.; Ross, H.J.; Alba, A.C.; Laporte, A.; Seto, E. Evaluation of a Heart Failure Telemonitoring Program Through a Microsimulation Model: Cost-Utility Analysis. J. Med. Internet Res. 2020, 22, e18917. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque de Almeida, F.; Al, M.J.; Koymans, R.; Riistama, J.; Pauws, S.; Severens, J.L. Impact of hospitalization on health-related quality of life in patients with chronic heart failure. Health Qual Life Outcomes 2020, 18, 262. [Google Scholar] [CrossRef] [PubMed]
- Hasan, A.; Paul, V. Telemonitoring in chronic heart failure. Eur. Heart J. 2011, 32, 1457–1464. [Google Scholar] [CrossRef] [PubMed]
- Koehler, F.; Koehler, K.; Prescher, S.; Kirwan, B.A.; Wegscheider, K.; Vettorazzi, E.; Lezius, S.; Winkler, S.; Moeller, V.; Fiss, G.; et al. Mortality and morbidity 1 year after stopping a remote patient management intervention: Extended follow-up results from the telemedical interventional management in patients with heart failure II (TIM-HF2) randomized trial. Lancet Digit. Health 2020, 2, e16–e24. [Google Scholar] [CrossRef]
- Frederix, I.; Vanderlinden, L.; Verboven, A.S.; Welten, M.; Wouters, D.; De Keulenaer, G.; Ector, B.; Elegeert, I.; Troisfontaines, P.; Weytjens, C.; et al. Long-term impact of a six-month telemedical care programme on mortality, heart failure readmissions and healthcare costs in patients with chronic heart failure. J. Telemed. Telecare 2019, 25, 286–293. [Google Scholar] [CrossRef]
- Xie, L.; Li, S.; Yu, X.; Wei, Q.; Yu, F.; Tong, J. DAHOS Study: Efficacy of dapagliflozin in treating heart failure with reduced ejection fraction and obstructive sleep apnea syndrome—A 3-month, multicenter, randomized controlled clinical trial. Eur. J. Clin. Pharmacol. 2024, 80, 771–780. [Google Scholar] [CrossRef] [PubMed]
- Lynskey, M.T.; Schlag, A.K.; Athanasiou-Fragkouli, A.; Badcock, D.; Nutt, D.J. Characteristics of and 3-month health outcomes for people seeking treatment with prescribed cannabis: Real-world evidence from Project Twenty21. Drug Sci. Policy Law 2023, 9. [Google Scholar] [CrossRef]
- Zhao, Y.; Liao, X.; Gu, H.; Jiang, Y.; Jiang, Y.; Wang, Y.; Zhang, Y. Gait speed at the acute phase predicted health-related quality of life at 3 and 12 months after stroke: A prospective cohort study. J. Rehabil. Med. 2024, 56, 24102. [Google Scholar] [CrossRef]
- Xia, Q.; Campbell, J.A.; Ahmad, H.; Si, L.; de Graaff, B.; Otahal, P.; Palmer, A.J. Health state utilities for economic evaluation of bariatric surgery: A comprehensive systematic review and meta-analysis. Obes. Rev. 2020, 21, e13028. [Google Scholar] [CrossRef]

| n = 346 | |
|---|---|
| Age, mean (SD) | 69.8 (10.3) |
| Female gender, n (%) | 138 (39.9%) |
| Body mass in kg, mean (SD) | 85.2 (16.0) |
| DBP in mmHG, mean (SD) | 70.9 (10.9) |
| SBP in mmHG, mean (SD) | 133.5 (22.2) |
| HR, mean (SD) | 78.5 (12.2) |
| NYHA class, n (%) | |
| I | 27 (7.8%) |
| II | 214 (61.8%) |
| IIII | 87 (25.2%) |
| IV | 18 (5.2%) |
| Comorbidities, n (%) | |
| Hypertension | 261 (75.4%) |
| Dyslipidemia | 196 (56.6%) |
| Diabetes | 105 (30.3%) |
| Myocardial infarction history | 103 (29.8%) |
| Atrial fibrillation | 100 (28.9%) |
| Nicotinism | 36 (10.4%) |
| Hypothyroidism | 35 (10.1%) |
| Chronic kidney disease | 34 (9.8%) |
| Valvular defects | 33 (9.5%) |
| Asthma | 30 (8.7%) |
| Cancer | 27 (7.8%) |
| Stroke history | 23 (6.6%) |
| Thrombosis | 22 (6.4%) |
| Obstructive pulmonary disease | 21 (6.1%) |
| Other thyroid diseases | 19 (5.5%) |
| Hyperthyroidism | 9 (2.6%) |
| Cardiomyopathy | 6 (1.7%) |
| Previous cardiac procedures, n (%) | |
| Angioplasty | 85 (24.6%) |
| Coronary artery bypass grafting | 24 (6.9%) |
| Implanted cardioverter | 18 (5.2%) |
| Medications, n (%) | |
| Beta-blocker | 292 (84.4%) |
| Angiotensin-converting enzyme inhibitor | 215 (62.1%) |
| Loop diuretic | 161 (46.5%) |
| Oral anticoagulant | 133 (38.4%) |
| Thiazide diuretic | 121 (35.0%) |
| SGLT2 inhibitor | 86 (24.9%) |
| P2Y12 inhibitor | 34 (9.8%) |
| Sacubitril/valsartan | 13 (3.8%) |
| Variables | Initial HSUV | Final HSUV | HSUV Change |
|---|---|---|---|
| Mean | 0.853 | 0.923 | 0.070 * |
| Standard deviation | 0.176 | 0.123 | 0.180 |
| Upper quartile | 0.97 | 1 | 0.11 |
| Median | 0.925 | 0.952 | 0.023 |
| Lower quartile | 0.795 | 0.873 | −0.018 |
| Centile 95 | 1 | 1 | 0.448 |
| Centile 5 | 0.497 | 0.752 | −0.116 |
| Variables | Coefficient | SD | p-Value |
| Telemedical intervention intensiveness | |||
| Number of pharmacotherapy modifications | 0.0126 | 0.0068 | 0.0639 |
| Number of telemedical examinations | 0.0001 | 0.0001 | 0.2985 |
| Constant | 0.0366 | 0.0226 | 0.1051 |
| Patients’ basic characteristics | |||
| Age in years | 0.0004 | 0.0010 | 0.6469 |
| Sex (female = 1) | 0.0439 | 0.0207 | 0.0349 * |
| Constant | 0.0219 | 0.0672 | 0.7455 |
| Comorbidities, previous cardiac procedures, and selected health indicators | |||
| Hypertension | 0.0251 | 0.0220 | 0.2548 |
| Dyslipidemia | −0.0097 | 0.0165 | 0.5596 |
| Diabetes | −0.0203 | 0.0166 | 0.2217 |
| Myocardial infarction history | 0.0214 | 0.0205 | 0.2976 |
| Atrial fibrillation | −0.0056 | 0.0174 | 0.7479 |
| Nicotinism | 0.0124 | 0.0244 | 0.6118 |
| Hypothyroidism | −0.0192 | 0.0244 | 0.4319 |
| Chronic kidney disease | −0.0080 | 0.0259 | 0.7567 |
| Valvular defects | −0.0499 | 0.0264 | 0.0597 |
| Asthma | 0.0069 | 0.0276 | 0.8024 |
| Cancer | 0.0149 | 0.0277 | 0.5906 |
| Stroke history | −0.00108 | 0.0288 | 0.9702 |
| Thrombosis | −0.0277 | 0.0299 | 0.3543 |
| Obstructive pulmonary disease | 0.0167 | 0.0352 | 0.636 |
| Other thyroid diseases | 0.0112 | 0.0329 | 0.7346 |
| Hyperthyroidism | 0.0023 | 0.0502 | 0.9631 |
| Cardiomyopathy | 0.0564 | 0.0621 | 0.3652 |
| Angioplasty | 0.0062 | 0.0205 | 0.763 |
| Coronary artery bypass grafting | −0.0195 | 0.0296 | 0.5096 |
| Implanted cardioverter | 0.0047 | 0.0359 | 0.8955 |
| NYHA class at inclusion | −0.0487 | 0.0122 | 0.0001 * |
| Hospitalization in previous 3 months | 0.0391 | 0.0262 | 0.1371 |
| Constant | 1.0111 | 0.0359 | <0.0001 * |
| Type of Action | Cost in PLN |
|---|---|
| Recruitment | 10 |
| Recruitment visit | 100 |
| Teleconsultation with a cardiologist | 50 |
| Remuneration of a primary care physician, for conducting follow-up and final visits | 200 |
| Televisits with a primary care physician | 25 |
| Visits with a cardiologist | 250 |
| Final teleconsultation with a cardiologist | 50 |
| Primary care nurse | 150 |
| Operation of the information and registration desk at each primary healthcare facility during the medical event—recruitment stage | 59.04 |
| Telemonitoring | 60.61 |
| Helpline | 11.66 |
| Distribution | 6.14 |
| License for telemedicine platform | 0.81 |
| Scales | 41.82 |
| Blood pressure monitors | 81 |
| Programming of scales and blood pressure monitors and configuration for the telemedicine platform | 14.76 |
| Preparation of starter kits for patients ready to be dispensed by the medical personnel | 49.20 |
| Leaflets/Posters | 0.37 |
| Social media advertising and information | 0.65 |
| Maintaining an information profile on social media | 1.08 |
| Total | 1162.12 |
| 3-Month BSC Costs | 3-Month BSC + T Costs | Difference (BSC + T − BSC) | |
|---|---|---|---|
| Hospitalization | 250,283.1 | 29,010.8 | −221,272.3 |
| Medicines | 131,324.8 | 153,556.1 | 22,231.3 |
| Outpatient specialist care and primary care | 10,427.2 | 0 | −10,427.2 |
| Telemedical intervention | 538,841.6 | 538,841.6 | |
| Total | 392,035.1 | 721,408.5 | 329,373.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wańczura, P.; Aebisher, D.; Wiśniowski, M.; Kos, M.; Bukowski, H.; Golicki, D.; Przybylski, A. Cost–Utility Analysis of 3-Month Telemedical Intervention for Heart Failure Patients: A Preliminary Study from Poland. Healthcare 2024, 12, 1360. https://doi.org/10.3390/healthcare12131360
Wańczura P, Aebisher D, Wiśniowski M, Kos M, Bukowski H, Golicki D, Przybylski A. Cost–Utility Analysis of 3-Month Telemedical Intervention for Heart Failure Patients: A Preliminary Study from Poland. Healthcare. 2024; 12(13):1360. https://doi.org/10.3390/healthcare12131360
Chicago/Turabian StyleWańczura, Piotr, David Aebisher, Mateusz Wiśniowski, Marek Kos, Hubert Bukowski, Dominik Golicki, and Andrzej Przybylski. 2024. "Cost–Utility Analysis of 3-Month Telemedical Intervention for Heart Failure Patients: A Preliminary Study from Poland" Healthcare 12, no. 13: 1360. https://doi.org/10.3390/healthcare12131360







