Increased Risk of Fracture after Traumatic Amputation: A Nationwide Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
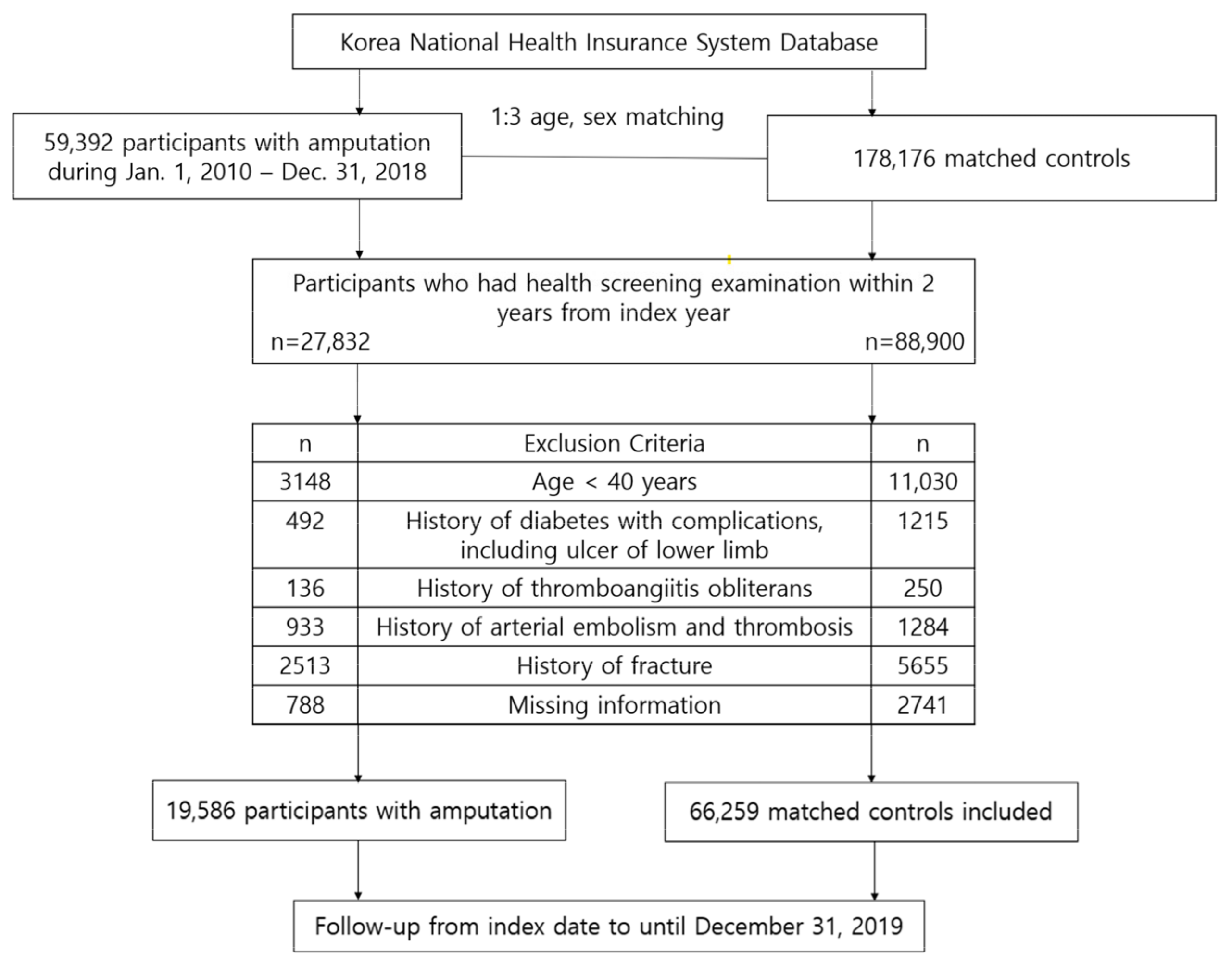
2.2. Study Population
2.3. Severity of Disability due to Amputation
2.4. Site of Amputation
2.5. Study Outcomes and Follow-Up
2.6. Covariates
2.7. Statistical Analysis
2.8. Equity, Diversity, and Inclusion Statement
3. Results
3.1. Baseline Characteristics
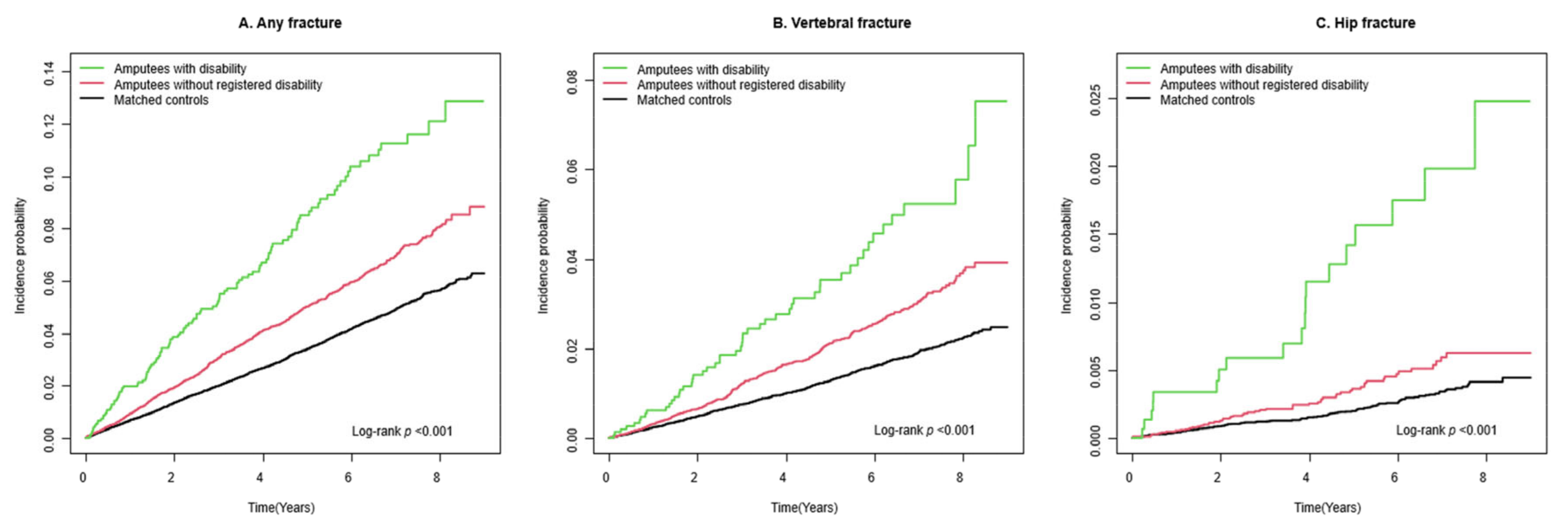
3.2. Risk of Fracture among Amputees
3.3. Risk of Fracture According to Site of Amputation
4. Discussion
5. Clinical Implications
6. Limitations
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bok, S.K.; Song, Y. Fact Sheet of Amputee 10-Year Trends in Korea: From 2011 to 2020. Ann. Rehabil. Med. 2022, 46, 221–227. [Google Scholar] [CrossRef]
- Sherk, V.D.; Bemben, M.G.; Bemben, D.A. BMD and bone geometry in transtibial and transfemoral amputees. J. Bone Miner. Res. 2008, 23, 1449–1457. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.C.; Deathe, A.B. A prospective study examining balance confidence among individuals with lower limb amputation. Disabil. Rehabil. 2004, 26, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Myers, A.M.; Fletcher, P.C.; Myers, A.H.; Sherk, W. Discriminative and evaluative properties of the activities-specific balance confidence (ABC) scale. J. Gerontol. A Biol. Sci. Med. Sci. 1998, 53, M287–M294. [Google Scholar] [CrossRef] [PubMed]
- Perry, S.D.; McIlroy, W.E.; Maki, B.E. The role of plantar cutaneous mechanoreceptors in the control of compensatory stepping reactions evoked by unpredictable, multi-directional perturbation. Brain Res. 2000, 877, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Hermodsson, Y.; Ekdahl, C.; Persson, B.M.; Roxendal, G. Standing balance in trans-tibial amputees following vascular disease or trauma: A comparative study with healthy subjects. Prosthet. Orthot. Int. 1994, 18, 150–158. [Google Scholar] [CrossRef]
- Miller, W.C.; Speechley, M.; Deathe, B. The prevalence and risk factors of falling and fear of falling among lower extremity amputees. Arch. Phys. Med. Rehabil. 2001, 82, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Bergen, G.; Stevens, M.R.; Burns, E.R. Falls and Fall Injuries Among Adults Aged ≥65 Years—United States, 2014. MMWR Morb. Mortal Wkly. Rep. 2016, 65, 993–998. [Google Scholar] [CrossRef]
- Finco, M.G.; Kim, S.; Ngo, W.; Menegaz, R.A. A review of musculoskeletal adaptations in individuals following major lower-limb amputation. J. Musculoskelet. Neuronal. Interact. 2022, 22, 269–283. [Google Scholar]
- Esquenazi, A. Gait analysis in lower-limb amputation and prosthetic rehabilitation. Phys. Med. Rehabil. Clin. N. Am. 2014, 25, 153–167. [Google Scholar] [CrossRef]
- de Oliveira, F.C.L.; Williamson, S.; Ardern, C.L.; Fagher, K.; Heron, N.; Janse van Rensburg, D.C.C.; Jansen, M.G.T.; Kolman, N.; O’Connor, S.R.; Saueressig, T.; et al. Association between the level of partial foot amputation and gait: A scoping review with implications for the minimum impairment criteria for wheelchair tennis. Br. J. Sports Med. 2022, 57, 237–248. [Google Scholar] [CrossRef]
- Haleem, S.; Yousaf, S.; Hamid, T.; Nagappa, S.; Parker, M.J. Characteristics and outcomes of hip fractures in lower limb amputees. Injury 2021, 52, 914–917. [Google Scholar] [CrossRef] [PubMed]
- Collins, S.H.; Adamczyk, P.G.; Kuo, A.D. Dynamic arm swinging in human walking. Proc. Biol. Sci. 2009, 276, 3679–3688. [Google Scholar] [CrossRef] [PubMed]
- Major, M.J.; Stine, R.; Shirvaikar, T.; Gard, S.A. Effects of Upper Limb Loss or Absence and Prosthesis Use on Postural Control of Standing Balance. Am. J. Phys. Med. Rehabil. 2020, 99, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, M.J.; Policha, A.; Maldonado, T.; Hiramoto, J.S.; Honig, S.; Conte, M.S.; Berger, J.; Rockman, C.B. Novel association between bone mineral density scores and the prevalence of peripheral artery disease in both sexes. Vasc. Med. 2017, 22, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Pasqualini, L.; Ministrini, S.; Macura, A.; Marini, E.; Leli, C.; Siepi, D.; Lombardini, R.; Kararoudi, M.N.; Scarponi, A.M.; Schillaci, G.; et al. Increased Bone Resorption: A Possible Pathophysiological Link Between Hypovitaminosis D and Peripheral Arterial Disease. Eur. J. Vasc. Endovasc. Surg. 2016, 52, 352–359. [Google Scholar] [CrossRef]
- Hyde, Z.; Mylankal, K.J.; Hankey, G.J.; Flicker, L.; Norman, P.E. Peripheral arterial disease increases the risk of subsequent hip fracture in older men: The Health in Men Study. Osteoporos. Int. 2013, 24, 1683–1688. [Google Scholar] [CrossRef] [PubMed]
- Jiao, H.; Xiao, E.; Graves, D.T. Diabetes and Its Effect on Bone and Fracture Healing. Curr. Osteoporos. Rep. 2015, 13, 327–335. [Google Scholar] [CrossRef]
- Krakauer, J.C.; Mckenna, M.J.; Fenn Buderer, N.; Rao, D.S.; Whitehouse, F.W.; Parfitt, A.M. Bone Loss and Bone Turnover in Diabetes. Diabetes 1995, 44, 775–782. [Google Scholar] [CrossRef]
- Wong, C.K.; Rissland, M.S.; Madagan, D.M.; Jones, K.N. A Scoping Review of Physical Activity in People With Lower-Limb Loss: 10,000 Steps Per Day? Phys. Ther. 2021, 101, pzab115. [Google Scholar] [CrossRef]
- Shin, D.W.; Cho, B.; Guallar, E. Korean National Health Insurance Database. JAMA Intern. Med. 2016, 176, 138. [Google Scholar] [CrossRef]
- Shin, D.W.; Cho, J.; Park, J.H.; Cho, B. National General Health Screening Program in Korea: History, current status, and future direction. Precis. Future Med. 2022, 6, 9–31. [Google Scholar] [CrossRef]
- Lee, S.W.; Lee, H.Y.; Ihm, S.H.; Park, S.H.; Kim, T.H.; Kim, H.C. Status of hypertension screening in the Korea National General Health Screening Program: A questionnaire survey on 210 screening centers in two metropolitan areas. Clin. Hypertens. 2017, 23, 23. [Google Scholar] [CrossRef]
- Cheol Seong, S.; Kim, Y.Y.; Khang, Y.H.; Heon Park, J.; Kang, H.J.; Lee, H.; Do, C.H.; Song, J.S.; Hyon Bang, J.; Ha, S.; et al. Data Resource Profile: The National Health Information Database of the National Health Insurance Service in South Korea. Int. J. Epidemiol. 2017, 46, 799–800. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Jung, W.; Kim, S.Y.; Park, J.H.; Shin, D.W. The Korea National Disability Registration System. Epidemiol. Health 2023, 45, e2023053. [Google Scholar] [CrossRef]
- Yoo, J.E.; Shin, D.W.; Han, K.; Kim, D.; Yoon, J.W.; Lee, D.Y. Association of Female Reproductive Factors With Incidence of Fracture Among Postmenopausal Women in Korea. JAMA Netw. Open 2021, 4, e2030405. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.B.; Park, H.S.; Yoo, J.E.; Han, K.; Park, S.H.; Shin, D.W.; Park, J. Risk of fracture incidence in prostate cancer survivors: A nationwide cohort study in South Korea. Arch. Osteoporos. 2020, 15, 110. [Google Scholar] [CrossRef]
- Shin, D.W.; Suh, B.; Lim, H.; Suh, Y.S.; Choi, Y.J.; Jeong, S.M.; Yun, J.M.; Song, S.O.; Park, Y. Increased Risk of Osteoporotic Fracture in Postgastrectomy Gastric Cancer Survivors Compared With Matched Controls: A Nationwide Cohort Study in Korea. Am. J. Gastroenterol. 2019, 114, 1735–1743. [Google Scholar] [CrossRef]
- Jung, S.Y.; Cho, E.B.; Han, K.D.; Jung, J.H.; Yeo, Y.; Kong, S.H.; Shin, D.W.; Min, J.H. Risk of fracture in neuromyelitis optica spectrum disorder and multiple sclerosis: A nationwide cohort study in South Korea. Osteoporos. Int. 2023, 34, 925–933. [Google Scholar] [CrossRef]
- Khan, N.F.; Perera, R.; Harper, S.; Rose, P.W. Adaptation and validation of the Charlson Index for Read/OXMIS coded databases. BMC Fam. Pract. 2010, 11, 1. [Google Scholar] [CrossRef]
- Huguet, J.; Mariscal, G.; Balfagón, A.; Mayorga, D.; Ulldemolins, P.; Guillot, A.; Barrés, M. Management and Outcomes of Hip Fractures in Lower Limb Amputees: A Case Series. Indian. J. Orthop. 2023, 57, 1063–1067. [Google Scholar] [CrossRef] [PubMed]
- Bowker, J.H.; Rills, B.M.; Ledbetter, C.A.; Hunter, G.A.; Holliday, P. Fractures in lower limbs with prior amputation. A study of ninety cases. J. Bone Jt. Surg. Am. 1981, 63, 915–920. [Google Scholar] [CrossRef]
- Ramachandran, V.S.; Hirstein, W. The perception of phantom limbs. The D. O. Hebb lecture. Brain 1998, 121 Pt 9, 1603–1630. [Google Scholar] [CrossRef] [PubMed]
- Saetta, G.; Cognolato, M.; Atzori, M.; Faccio, D.; Giacomino, K.; Mittaz Hager, A.G.; Tiengo, C.; Bassetto, F.; Müller, H.; Brugger, P. Gaze, behavioral, and clinical data for phantom limbs after hand amputation from 15 amputees and 29 controls. Sci. Data 2020, 7, 60. [Google Scholar] [CrossRef]
- Roșca, A.C.; Baciu, C.C.; Burtăverde, V.; Mateizer, A. Psychological Consequences in Patients With Amputation of a Limb. An Interpretative-Phenomenological Analysis. Front. Psychol. 2021, 12, 537493. [Google Scholar] [CrossRef] [PubMed]
- Nikander, R.; Sievänen, H.; Heinonen, A.; Daly, R.M.; Uusi-Rasi, K.; Kannus, P. Targeted exercise against osteoporosis: A systematic review and meta-analysis for optimising bone strength throughout life. BMC Med. 2010, 8, 47. [Google Scholar] [CrossRef] [PubMed]
- Thomson, S.; Lu, W.; Zreiqat, H.; Li, J.J.; Tetsworth, K.; Al Muderis, M. Proximal Bone Remodeling in Lower Limb Amputees Reconstructed With an Osseointegrated Prosthesis. J. Orthop. Res. 2019, 37, 2524–2530. [Google Scholar] [CrossRef]
- Cavedon, V.; Sandri, M.; Peluso, I.; Zancanaro, C.; Milanese, C. Body composition and bone mineral density in athletes with a physical impairment. PeerJ 2021, 9, e11296. [Google Scholar] [CrossRef]
- Yazicioglu, K.; Tugcu, I.; Yilmaz, B.; Goktepe, A.S.; Mohur, H. Osteoporosis: A factor on residual limb pain in traumatic trans-tibial amputations. Prosthet. Orthot. Int. 2008, 32, 172–178. [Google Scholar] [CrossRef][Green Version]
- Tugcu, I.; Safaz, I.; Yilmaz, B.; Göktepe, A.S.; Taskaynatan, M.A.; Yazicioglu, K. Muscle Strength and Bone Mineral Density in Mine Victims with Transtibial Amputation. Prosthet. Orthot. Int. 2009, 33, 299–306. [Google Scholar] [CrossRef]
- Smith, É.; Comiskey, C.; Carroll, Á.; Ryall, N. A Study of Bone Mineral Density in Lower Limb Amputees at a National Prosthetics Center. JPO: J. Prosthet. Orthot. 2011, 23, 14–20. [Google Scholar] [CrossRef]
- Bemben, D.A.; Sherk, V.D.; Ertl, W.J.J.; Bemben, M.G. Acute bone changes after lower limb amputation resulting from traumatic injury. Osteoporos. Int. 2017, 28, 2177–2186. [Google Scholar] [CrossRef]
- Pearson, O.M.; Lieberman, D.E. The aging of Wolff’s “law”: Ontogeny and responses to mechanical loading in cortical bone. Am. J. Phys. Anthropol. 2004, 125 (Suppl. S39), 63–99. [Google Scholar] [CrossRef]
- Tsai, S.; Pirruccio, K.; Ahn, J. The brief window of time comprising a wheelchair transfer confers a significant fracture risk on elderly Americans. Public Health 2020, 182, 1–6. [Google Scholar] [CrossRef]
- Major, M.J. Fall Prevalence and Contributors to the Likelihood of Falling in Persons with Upper Limb Loss. Phys. Ther. 2019, 99, 377–387. [Google Scholar] [CrossRef]
- Soyer, K.; Unver, B.; Tamer, S.; Ulger, O. The importance of rehabilitation concerning upper extremity amputees: A Systematic review. Pak. J. Med. Sci. 2016, 32, 1312–1319. [Google Scholar] [CrossRef] [PubMed]
- Abou, L.; Fliflet, A.; Zhao, L.; Du, Y.; Rice, L. The Effectiveness of Exercise Interventions to Improve Gait and Balance in Individuals with Lower Limb Amputations: A Systematic Review and Meta-analysis. Clin. Rehabil. 2022, 36, 857–872. [Google Scholar] [CrossRef]
- Yang, J.Y.; Suh, W.S. Factors Associated with Occurrence, Average Length of Stay(ALOS) and Average Daily Patient Revenues of Hand Injured Patients. J. Korea Contents Assoc. 2012, 12, 380–389. [Google Scholar] [CrossRef]
- Ko, K.J. Monthly Safety and Health, June Issue. Korea Occupational Safety & Health Agency, Ulsan, Republic of Korea, 2020; pp. 11–15. Available online: https://www.kosha.or.kr/ebook/fcatalog/include/monthly_detail.jsp?ccate=01010C0000&sdir=40&cimg= (accessed on 2 July 2024).


| Variables | Matched Controls (n = 66,259) | Amputees (n = 19,586) | p Value |
|---|---|---|---|
| Age (years) | 55.9 ± 9.5 | 56.3 ± 9.5 | <0.001 |
| Sex (male) | 51,470 (77.7) | 14,818 (75.7) | <0.001 |
| Income (lowest 20%) | 11,875 (17.9) | 3579 (18.3) | 0.261 |
| Place of residence (urban) | 30,447 (46.0) | 6755 (34.5) | <0.001 |
| Alcohol consumption | <0.001 | ||
| None | 29,967 (45.2) | 9088 (46.4) | |
| Mild to moderate | 29,508 (44.5) | 7958 (40.6) | |
| Heavy | 6784 (10.2) | 2540 (13.0) | |
| Smoking status | <0.001 | ||
| Never | 29,517 (44.6) | 8862 (45.3) | |
| Former | 17,816 (26.9) | 4523 (23.1) | |
| Current | 18,926 (28.6) | 6201 (31.7) | |
| Regular physical activity | 15,284 (23.1) | 3537 (18.1) | <0.001 |
| Body mass index (kg/m2) | 24.2 ± 3.0 | 24.1 ± 3.0 | <0.001 |
| Systolic blood pressure (mmHg) | 124.6 ± 14.4 | 124.6 ± 14.9 | 0.849 |
| Diastolic blood pressure (mmHg) | 77.7 ± 9.9 | 77.6± 10.0 | 0.197 |
| Fasting glucose (mg/dL) | 102.4 ± 25.4 | 102.9 ± 27.7 | 0.020 |
| Total cholesterol (mg/dL) | 197.6 ± 37.6 | 196.5 ± 37.6 | <0.001 |
| Comorbidities | |||
| Hypertension | 24,129 (36.4) | 7267 (37.1) | 0.080 |
| Type 2 diabetes | 8953 (13.5) | 2763 (14.1) | 0.033 |
| Dyslipidemia | 19,016 (28.7) | 5447 (27.8) | 0.016 |
| Charlson comorbidity index | 1.3 ± 1.6 | 1.6 ± 1.7 | <0.001 |
| N | Any Fracture | Vertebral Fracture | Hip Fracture | Other Fracture | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases/IR | Model 1 | Model 2 | Cases/IR | Model 1 | Model 2 | Cases/IR | Model 1 | Model 2 | Cases/IR | Model 1 | Model 2 | ||
| Matched controls | 66,259 | 2014/7.1 | 1 (ref.) | 1 (ref.) | 772/2.7 | 1 (Ref.) | 1 (Ref.) | 132/0.5 | 1 (Ref.) | 1 (Ref.) | 1,201/4.2 | 1 (Ref.) | 1 (Ref.) |
| Amputees | 19,586 | 883/10.8 | 1.54 (1.42–1.66) | 1.47 (1.36–1.60) | 374/4.5 | 1.69 (1.49–1.91) | 1.63 (1.44–1.85) | 76/0.9 | 2.00 (1.51–2.65) | 1.85 (1.39–2.46) | 482/5.8 | 1.40 (1.26–1.55) | 1.34 (1.20–1.49) |
| Presence of disability | |||||||||||||
| No disability | 18,061 | 769/10.3 | 1.45 (1.34–1.58) | 1.41 (1.30–1.54) | 323/4.2 | 1.59 (1.39–1.81) | 1.57 (1.38–1.79) | 57/0.7 | 1.63 (1.20–2.23) | 1.57 (1.14–2.15) | 42/7.5 | 1.36 (1.21–1.51) | 1.30 (1.17–1.45) |
| Disability | 1525 | 114/17.4 | 2.45 (2.03–2.96) | 2.07 (1.71–2.50) | 51/7.5 | 2.80 (2.11–3.72) | 2.16 (1.63–2.88) | 19/2.8 | 6.05 (3.74–9.79) | 3.98 (2.45–6.47) | 10/8.5 | 1.84 (1.40–2.43) | 1.70 (1.29–2.25) |
| Severity of disability | |||||||||||||
| Mild | 1249 | 90/16.6 | 2.34 (1.90–2.89) | 1.97 (1.59–2.43) | 41/7.3 | 2.72 (1.99–3.73) | 2.09 (1.53–2.87) | 13/2.3 | 5.00 (2.83–8.85) | 3.36 (1.89–5.95) | 42/7.5 | 1.80 (1.33–2.45) | 1.66 (1.22–2.26) |
| Severe | 276 | 24/21.0 | 2.99 (2.00–4.46) | 2.59 (1.73–3.87) | 10/8.4 | 3.17 (1.70–5.92) | 2.51 (1.34–4.69) | 6/5.0 | 11.02 (4.86–25.00) | 6.73 (2.95–15.35) | 10/8.5 | 2.03 (1.09–3.78) | 1.91 (1.02–3.56) |
| Location of amputation | |||||||||||||
| Shoulder/upper arm | 28 | 1 | 1.38 (0.19–9.78) | 1.25 (0.18–8.90) | 0/0 | - | - | 0/0 | - | - | 1/9.6 | 2.30 (0.32–16.35) | 2.22 (0.31–15.80) |
| Forearm | 68 | 7 | 3.30 (1.57–6.92) | 2.68 (1.28–5.63) | 3/9.7 | 3.62 (1.17–11.26) | 2.78 (0.89–8.65) | 1/3.2 | 6.93 (0.97–49.58) | 4.46 (0.62–32.09) | 5/16.3 | 3.91 (1.62–9.40) | 3.36 (1.40–8.10) |
| Wrist/hand | 18,935 | 842 | 1.51 (1.40–1.64) | 1.46 (1.34–1.58) | 357/4.4 | 1.66 (1.47–1.89) | 1.62 (1.42–1.83) | 66/0.8 | 1.79 (1.34–2.41) | 1.68 (1.24–2.26) | 464/5.8 | 1.39 (1.25–1.55) | 1.33 (1.19–1.48) |
| Hip/thigh | 27 | 2 | 2.44 (0.61–9.78) | 1.81 (0.45–7.26) | 1/8.3 | 3.14 (0.44–22.34) | 2.13 (0.30–15.13) | 1/8.5 | 18.96 (2.65–135.63) | 9.47 (1.31–68.43) | 0/0 | - | - |
| Lower leg | 87 | 6 | 2.22 (1.00–4.96) | 1.82 (0.82–4.05) | 2/5.1 | 1.89 (0.47–7.56) | 1.31 (0.33–5.27) | 3/7.7 | 17.27 (5.50–54.25) | 9.24 (2.92–29.18) | 1/2.5 | 0.60 (0.09–4.27) | 0.53 (0.08–3.77) |
| Ankle/foot | 410 | 23 | 1.94 (1.28–2.92) | 1.89 (1.25–2.85) | 10/5.8 | 2.18 (1.17–4.07) | 2.02 (1.08–3.76) | 5/2.9 | 6.28 (2.57–15.35) | 4.71 (1.92–11.54) | 10/5.8 | 1.39 (0.75–2.59) | 1.41 (0.76–2.64) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, H.; Park, J.; Kim, B.; Han, K.; Choi, H.L.; Shin, D.W. Increased Risk of Fracture after Traumatic Amputation: A Nationwide Retrospective Cohort Study. Healthcare 2024, 12, 1362. https://doi.org/10.3390/healthcare12131362
Cho H, Park J, Kim B, Han K, Choi HL, Shin DW. Increased Risk of Fracture after Traumatic Amputation: A Nationwide Retrospective Cohort Study. Healthcare. 2024; 12(13):1362. https://doi.org/10.3390/healthcare12131362
Chicago/Turabian StyleCho, Hyeonjin, Junhee Park, Bongseong Kim, Kyungdo Han, Hea Lim Choi, and Dong Wook Shin. 2024. "Increased Risk of Fracture after Traumatic Amputation: A Nationwide Retrospective Cohort Study" Healthcare 12, no. 13: 1362. https://doi.org/10.3390/healthcare12131362
APA StyleCho, H., Park, J., Kim, B., Han, K., Choi, H. L., & Shin, D. W. (2024). Increased Risk of Fracture after Traumatic Amputation: A Nationwide Retrospective Cohort Study. Healthcare, 12(13), 1362. https://doi.org/10.3390/healthcare12131362





