Understanding the Role of Technology Anxiety in the Adoption of Digital Health Technologies (DHTs) by Older Adults with Chronic Diseases in Shanghai: An Extension of the Unified Theory of Acceptance and Use of Technology (UTAUT) Model
Abstract
:1. Introduction
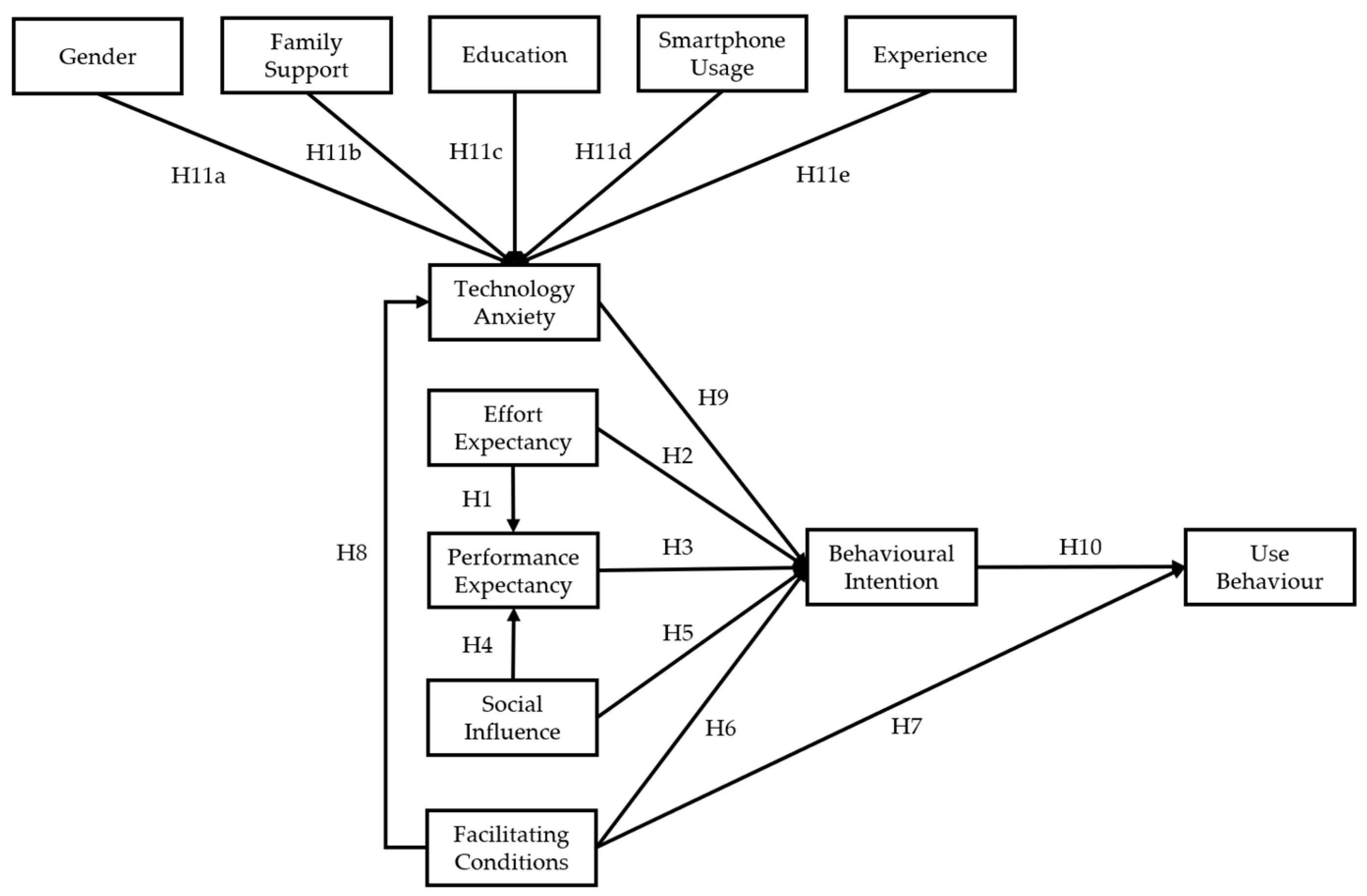
2. Theoretical Framework and hypotheses
2.1. Effort Expectancy (EE)
2.2. Performance Expectancy (PE)
2.3. Social Influence (SI)
2.4. Facilitating Conditions (FC)
2.5. Technology Anxiety (TA)
2.6. Behavioural Intention (BI)
2.7. Demographic Variables
3. Methodology
3.1. Questionnaire Design
3.2. Data Collection
3.3. Data Analysis
4. Results
4.1. Demographic Characteristics of Sample
4.2. Technology Anxiety Level
4.3. Measurement Model
4.4. Hypothesis Testing
5. Discussion
5.1. Principle Findings
5.1.1. Implications
5.1.2. Limitations and Future Research Directions
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Items | Source | |
|---|---|---|
| Performance Expectancy (PE) | PE1. Digital health technologies can be useful in managing my daily health. | [6] |
| PE2. Digital health technologies can help me receive medical treatment more conveniently. | ||
| PE3. Digital health technologies can improve my health level and quality of life. | ||
| PE4 *. Digital health technologies are useless for my health or medical services. | By authors | |
| Effort Expectancy (EE) | EE1. It is easy for me to accept digital health technologies. | [6] |
| EE2. Learning how to use digital health technologies is easy for me. | [13] | |
| EE3. Using digital health technologies is easy for me. | ||
| EE4. It is worth learning how to use digital health technologies (to help me). | ||
| Social Influence (SI) | SI1. Family members or relatives influence me to use digital health technologies. | |
| SI2. Teachers and colleagues influence me to use digital health technologies. | ||
| SI3. Friends (or fellow patients) influence me to use digital health technologies. | ||
| SI4. Medical staff influence me to use digital health technologies. | ||
| Facilitating Conditions (FC) | FC1. When I have difficulties using various digital health technologies, I can obtain help from others. | |
| FC2. When using digital health technologies, I have access to various resources to support me (software, network, equipment, hardware environmental conditions, etc.). | ||
| FC3. The use of digital health technologies does not contradict my use of other technologies, functions, services, needs, etc. | ||
| Technology Anxiety (TA) | TA1. Using digital health technologies may make me feel uneasy and confused. | [10] |
| TA2. Using digital health technologies would make me very nervous. | ||
| TA3. Using digital health technologies may make me feel uncomfortable. | ||
| TA4 *. I feel calm to use digital health technologies. | By authors | |
| Behavioural Intention (BI) | BI1. I plan to use digital health technologies frequently. | [6,13] |
| BI2. I am willing to recommend digital health technologies to others. | ||
| BI3 *. I do not intend to use digital health technologies for the next six months. | [48] | |
| BI4. I intend to use (more) digital health technologies as soon as possible. | ||
| User Behaviour (UB) | UB1. I have used digital health technologies. | [6,58] |
| UB2. Using digital health technologies is a pleasant experience. | ||
| UB3. When I need to seek healthcare service, digital health technologies will be very important options for me. | ||
| UB4. Using digital health technologies helps me to manage my selfcare and adequate behaviour. | ||
References
- Wang, X.; Luan, W. Research progress on digital health literacy of older adults: A scoping review. Front. Public Health 2022, 10, 906089. [Google Scholar] [CrossRef] [PubMed]
- Abernethy, A.; Adams, L.; Barrett, M.; Bechtel, C.; Brennan, P.; Butte, A.; Faulkner, J.; Fontaine, E.; Friedhoff, S.; Halamka, J.; et al. The Promise of Digital Health: Then, Now, and the Future. NAM Perspect. 2022. [Google Scholar] [CrossRef] [PubMed]
- Kainiemi, E.; Saukkonen, P.; Virtanen, L.; Vehko, T.; Kyytsönen, M.; Aaltonen, M.; Heponiemi, T. Perceived benefits of digital health and social services among older adults: A population-based cross-sectional survey. Digit. Health 2023, 9, 20552076231173559. [Google Scholar] [CrossRef] [PubMed]
- Peeples, M.; Maity, B. Digital Health in Chronic Care and Self-Management; Kiel, J.M., Ed.; Springer International Publishing: Cham, Switzerland, 2022; pp. 209–222. [Google Scholar]
- Kasoju, N.; Remya, N.S.; Sasi, R.; Sujesh, S.; Soman, B.; Kesavadas, C.; Muraleedharan, C.V.; Varma, P.R.H.; Behari, S. Digital health: Trends, opportunities and challenges in medical devices, pharma and bio-technology. CSI Trans. ICT 2023, 11, 11–30. [Google Scholar] [CrossRef]
- Li, W.; Gui, J.; Luo, X.; Yang, J.; Zhang, T.; Tang, Q. Determinants of intention with remote health management service among urban older adults: A Unified Theory of Acceptance and Use of Technology perspective. Front. Public Health 2023, 11, 1117518. [Google Scholar] [CrossRef]
- Wilson, J.; Heinsch, M.; Betts, D.; Booth, D.; Kay-Lambkin, F. Barriers and facilitators to the use of e-health by older adults: A scoping review. BMC Public Health 2021, 21, 1556. [Google Scholar] [CrossRef]
- Gould, C.E.; O’Hara, R.; Goldstein, M.K.; Beaudreau, S.A. Multimorbidity is associated with anxiety in older adults in the Health and Retirement Study. Int. J. Geriatr. Psychiatr. 2016, 31, 1105–1115. [Google Scholar] [CrossRef] [PubMed]
- He, Z.F.; Tan, W.Y.; Ma, H.; Shuai, Y.; Shan, Z.; Zhai, J.; Qiu, Y.; Zeng, H.; Chen, X.L.; Wang, S.B.; et al. Prevalence and factors associated with depression and anxiety among older adults: A large-scale cross-sectional study in China. J. Affect. Disord. 2024, 346, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Hoque, R.; Sorwar, G. Understanding factors influencing the adoption of mHealth by the elderly: An extension of the UTAUT model. Int. J. Med. Inform. 2017, 101, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Palas, J.U.; Sorwar, G.; Hoque, R.; Sivabalan, A. Factors influencing the elderly’s adoption of mHealth: An empirical study using extended UTAUT2 model. BMC Med. Inform. Decis. Mak. 2022, 22, 191. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Khan, S.; Khan, I.U.; Khan, S.U.; Xie, Y.; Li, X.; Zhang, G. Assessing the Adoption of e-Health Technology in a Developing Country: An Extension of the UTAUT Model. SAGE Open 2021, 11, 21582440211027565. [Google Scholar] [CrossRef]
- Cao, J.; Kurata, K.; Lim, Y.; Sengoku, S.; Kodama, K. Social Acceptance of Mobile Health among Young Adults in Japan: An Extension of the UTAUT Model. Int. J. Environ. Res. Public Health 2022, 19, 15156. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, A.; Díaz-Martín, A.M.; Guillén, M.J.Y. Modifying UTAUT2 for a cross-country comparison of telemedicine adoption. Comput. Human. Behav. 2022, 130, 107183. [Google Scholar] [CrossRef]
- Jewer, J. Patients’ intention to use online postings of ED wait times: A modified UTAUT model. Int. J. Med. Inform. 2018, 112, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Rogers, E.M. Simon and Schuster, Diffusion of Innovations, 5th ed.; Free Press: New York, NY, USA, 2003. [Google Scholar]
- Fishbein, M.; Ajzen, I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Philos. Rhetor. 1977, 10, 130–132. [Google Scholar]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Bandura, A. Social foundations of thought and action: A social cognitive theory. In Social Foundations of thought and Action: A Social Cognitive Theory; Prentice-Hall, Inc.: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. Extrinsic and Intrinsic Motivation to Use Computers in the Workplace1. J. Appl. Social. Psychol. 1992, 22, 1111–1132. [Google Scholar] [CrossRef]
- Thompson, R.L.; Higgins, C.A.; Howell, J.M. Personal Computing: Toward a Conceptual Model of Utilization. MIS Q. 1991, 15, 125–143. [Google Scholar] [CrossRef]
- Taylor, S.; Todd, P.A. Assessing IT Usage: The Role of Prior Experience. MIS Q. 1995, 19, 561–570. [Google Scholar] [CrossRef]
- Cimperman, M.; Brenčič, M.M.; Trkman, P. Analyzing older users’ home telehealth services acceptance behavior-applying an Extended UTAUT model. Int. J. Med. Inform. 2016, 90, 22–31. [Google Scholar] [CrossRef]
- Liu, J.Y.W.; Sorwar, G.; Rahman, M.S.; Hoque, R. The role of trust and habit in the adoption of mHealth by older adults in Hong Kong: A healthcare technology service acceptance (HTSA) model. BMC Geriatr. 2023, 23, 73. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, C.; Carlsson, J.; Hyvonen, K.; Puhakainen, J.; Walden, P. Adoption of Mobile Devices/Services—Searching for Answers with the UTAUT. In Proceedings of the 39th Annual Hawaii International Conference on System Sciences (HICSS’06), Kauai, HI, USA, 4–7 January 2006; p. 132a. [Google Scholar]
- Sen, K.; Prybutok, G.; Prybutok, V. The use of digital technology for social wellbeing reduces social isolation in older adults: A systematic review. SSM Popul. Health 2022, 17, 101020. [Google Scholar] [CrossRef] [PubMed]
- Meuter, M.L.; Ostrom, A.L.; Bitner, M.J.; Roundtree, R. The influence of technology anxiety on consumer use and experiences with self-service technologies. J. Bus. Res. 2003, 56, 899–906. [Google Scholar] [CrossRef]
- Xue, L.; Yen, C.C.; Chang, L.; Chan, H.C.; Tai, B.C.; Tan, S.B.; Duh, H.B.; Choolani, M. An exploratory study of ageing women’s perception on access to health informatics via a mobile phone-based intervention. Int. J. Med. Inform. 2012, 81, 637–648. [Google Scholar] [CrossRef] [PubMed]
- Ha-Neul Kim, P.P.F.; Greenhow, C. Older adults’ technology anxiety as a barrier to digital inclusion: A scoping review. Educ. Gerontol. 2023, 49, 1021–1038. [Google Scholar]
- Hsieh, Y.C.; Tsai, W.C.; Hsia, Y.C. A Study on Technology Anxiety among Different Ages and Genders; Springer International Publishing: Cham, Switzerland, 2020; pp. 241–254. [Google Scholar]
- Hänninen, R.; Taipale, S.; Luostari, R. Exploring heterogeneous ICT use among older adults: The warm experts’ perspective. New Media Soc. 2020, 23, 370089257. [Google Scholar] [CrossRef]
- Ma, Q.; Chan, A.H.; Chen, K. Personal and other factors affecting acceptance of smartphone technology by older Chinese adults. Appl. Ergon. 2016, 54, 62–71. [Google Scholar] [CrossRef]
- Dou, K.; Yu, P.; Deng, N.; Liu, F.; Guan, Y.; Li, Z.; Ji, Y.; Du, N.; Lu, X.; Duan, H. Patients’ Acceptance of Smartphone Health Technology for Chronic Disease Management: A Theoretical Model and Empirical Test. JMIR Mhealth Uhealth 2017, 5, e177. [Google Scholar] [CrossRef] [PubMed]
- Nymberg, V.M.; Bolmsjö, B.B.; Wolff, M.; Calling, S.; Gerward, S.; Sandberg, M. Having to learn this so late in our lives…’ Swedish elderly patients’ beliefs, experiences, attitudes and expectations of e-health in primary health care. Scand. J. Prim. Health Care 2019, 37, 41–52. [Google Scholar] [CrossRef] [PubMed]
- De Veer, A.J.; Peeters, J.M.; Brabers, A.E.; Schellevis, F.G.; Rademakers, J.J.; Francke, A.L. Determinants of the intention to use e-Health by community dwelling older people. BMC Health Serv. Res. 2015, 15, 103. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, T.D.; de Santana, V.F. Identifying Distractors for People with Computer Anxiety Based on Mouse Fixations. Interact. Comput. 2022, 35, 165–190. [Google Scholar] [CrossRef]
- Tompson, R.; Barclay, D.; Higgins, C. The partial least squares (PLS) approach to causal modeling: Personal computer adoption and use as an illustration. Technol. Stud. 1995, 2, 284–324. [Google Scholar]
- Hair, J.; Alamer, A. Partial Least Squares Structural Equation Modeling (PLS-SEM) in second language and education research: Guidelines using an applied example. Res. Methods Appl. Linguist. 2022, 1, 100027. [Google Scholar] [CrossRef]
- Peterson, R.A.; Kim, Y. On the relationship between coefficient alpha and composite reliability. J. Appl. Psychol. 2013, 98, 194–198. [Google Scholar] [CrossRef]
- Petter, S.; Straub, D.; Rai, A. Specifying Formative Constructs in Information Systems Research. MIS Q. 2007, 31, 623–656. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Nimrod, G. Technophobia among older Internet users. Educ. Gerontol. 2018, 44, 148–162. [Google Scholar] [CrossRef]
- Tennant, B.; Stellefson, M.; Dodd, V.; Chaney, B.; Chaney, D.; Paige, S.; Alber, J. eHealth literacy and Web 2.0 health information seeking behaviors among baby boomers and older adults. J. Med. Internet Res. 2015, 17, e70. [Google Scholar] [CrossRef]
- Kim, J.; Jeon, S.W.; Byun, H.; Yi, E. Exploring E-Health Literacy and Technology-Use Anxiety among Older Adults in Korea. Healthcare 2023, 11, 1556. [Google Scholar] [CrossRef]
- Hsu, C.W.; Peng, C.C. What drives older adults’ use of mobile registration apps in Taiwan? An investigation using the extended UTAUT model. Inform. Health Soc. Care 2022, 47, 258–273. [Google Scholar] [CrossRef]
- Akdur, G.; Aydin, M.N.; Akdur, G. Adoption of Mobile Health Apps in Dietetic Practice: Case Study of Diyetkolik. JMIR Mhealth Uhealth 2020, 8, e16911. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhang, R.; Lu, X.; Zhang, X. What drives the adoption of online health communities? An empirical study from patient-centric perspective. BMC Health Serv. Res. 2023, 23, 524. [Google Scholar] [CrossRef] [PubMed]
- Huygens, M.W.J.; Vermeulen, J.; Swinkels, I.C.S.; Friele, R.D.; van Schayck, O.C.P.; de Witte, L.P. Expectations and needs of patients with a chronic disease toward self-management and eHealth for self-management purposes. BMC Health Serv. Res. 2016, 16, 232. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Gong, X.; Weal, M.; Dai, W.; Hou, S.; Ma, J. Attitudes and associated factors of patients’ adoption of patient accessible electronic health records in China—A mixed methods study. Digit. Health 2023, 9, 20552076231174101. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Zhao, Z.; Guo, J.; Wang, Y.; Zhang, C.; Zheng, J.; Zou, Z.; Liu, W. Understanding Use Intention of mHealth Applications Based on the Unified Theory of Acceptance and Use of Technology 2 (UTAUT-2) Model in China. Int. J. Environ. Res. Public Health 2023, 20, 3139. [Google Scholar] [CrossRef] [PubMed]
- Portz, J.D.; Bayliss, E.A.; Bull, S.; Boxer, R.S.; Bekelman, D.B.; Gleason, K.; Czaja, S. Using the Technology Acceptance Model to Explore User Experience, Intent to Use, and Use Behavior of a Patient Portal among Older Adults with Multiple Chronic Conditions: Descriptive Qualitative Study. J. Med. Internet Res. 2019, 21, e11604. [Google Scholar] [CrossRef] [PubMed]
- Bi, L. Can Digital Feedback Promote the Use of Mobile Internet by the Elderly. In Proceedings of the 2023 International Seminar on Computer Science and Engineering Technology, New York, NY, USA, 29–30 April 2023; pp. 405–408. [Google Scholar]
- Bhukya, R.; Paul, J. Social influence research in consumer behavior: What we learned and what we need to learn?—A hybrid systematic literature review. J. Bus. Res. 2023, 162, 113870. [Google Scholar]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef] [PubMed]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digitization of healthcare sector: A study on privacy and security concerns. ICT Express 2023, 9, 571–588. [Google Scholar]
- Zhou, M.; Long, P.; Kong, N.; Campy, K.S. Characterizing Wuhan residents’ mask-wearing intention at early stages of the COVID-19 pandemic. Patient Educ. Couns. 2021, 104, 1868–1877. [Google Scholar] [CrossRef] [PubMed]

| Main Category | Exact Technologies Involved in the Study |
|---|---|
| eHealth | Electronic health reports, electronic health records, electronic discharge summaries |
| mHealth | Outpatient appointments, mobile health management applications |
| Telemedicine | Telesurgery, telemedicine services |
| Wearable devices | Smart wearable devices |
| Variable | Description | Frequency | Percentage |
|---|---|---|---|
| Source | General hospital | 104 | 33.66 |
| District hospital | 103 | 33.33 | |
| Community health centre (CHC) | 102 | 33.01 | |
| Gender | Male | 159 | 51.46 |
| Female | 150 | 48.54 | |
| Age | 60–69 | 121 | 39.16 |
| 70–79 | 144 | 46.60 | |
| ≥80 | 44 | 14.24 | |
| Chronic Disease | Hypertension | 128 | 41.42 |
| Cardiovascular disease | 82 | 26.54 | |
| Diabetes | 112 | 36.25 | |
| Stroke | 36 | 11.65 | |
| COPD | 33 | 10.68 | |
| Education | Elementary school or below | 2 | 0.65 |
| Junior high school | 96 | 31.07 | |
| High school | 204 | 66.02 | |
| University or beyond | 7 | 2.27 | |
| Family Support | Live alone | 50 | 16.18 |
| Live with partner | 154 | 49.84 | |
| Live with younger generation | 105 | 33.98 | |
| Smartphone Usage | Positive | 97 | 31.39 |
| Negative | 212 | 68.61 | |
| DHTs Experience | Yes | 98 | 31.72 |
| No | 211 | 68.28 |
| Technology Anxiety Level | Mean Value for Measurement Construct TA | n | % |
|---|---|---|---|
| Neutral or not anxious | ≤3 | 143 | 46.28 |
| Anxious | >3 | 166 | 53.72 |
| Constructs | Items | Mean (SD) | Loadings | Cronbach’s Alpha | CR | AVE |
|---|---|---|---|---|---|---|
| Behavioural Intention (BI) | BI1 | 2.97 (1.47) | 0.941 | 0.901 | 0.939 | 0.836 |
| BI2 | 2.14 (1.22) | 0.860 | ||||
| BI4 | 2.93 (1.47) | 0.939 | ||||
| Effort Expectancy (EE) | EE1 | 3.04 (1.44) | 0.877 | 0.946 | 0.961 | 0.861 |
| EE2 | 2.38 (1.35) | 0.945 | ||||
| EE3 | 2.19 (1.39) | 0.951 | ||||
| EE4 | 2.79 (1.43) | 0.935 | ||||
| Facilitating Conditions (FC) | FC1 | 3.98 (1.11) | 0.932 | 0.894 | 0.935 | 0.827 |
| FC2 | 4.02 (1.06) | 0.949 | ||||
| FC3 | 4.08 (0.94) | 0.844 | ||||
| Performance Expectancy (PE) | PE1 | 3.74 (1.21) | 0.940 | 0.947 | 0.966 | 0.904 |
| PE2 | 3.94 (1.26) | 0.952 | ||||
| PE3 | 3.88 (1.19) | 0.960 | ||||
| Social Influence (SI) | SI1 | 3.83 (1.14) | 0.825 | 0.900 | 0.927 | 0.761 |
| SI2 | 2.01 (1.68) | 0.889 | ||||
| SI3 | 2.25 (1.75) | 0.904 | ||||
| SI4 | 2.42 (1.76) | 0.869 | 0.929 | 0.955 | 0.876 | |
| Technology Anxiety (TA) | TA1 | 3.26 (1.41) | 0.951 | |||
| TA2 | 3.28 (1.46) | 0.963 | ||||
| TA3 | 2.64 (1.48) | 0.893 | ||||
| Use Behaviour (UB) | UB1 | 3.22 (1.50) | 0.831 | 0.917 | 0.941 | 0.801 |
| UB2 | 3.68 (1.29) | 0.909 | ||||
| UB3 | 3.82 (1.35) | 0.922 | ||||
| UB4 | 3.59 (1.23) | 0.915 |
| BI | EE | FC | PE | SI | TA | UB | |
|---|---|---|---|---|---|---|---|
| BI | 0.914 | ||||||
| EE | 0.820 | 0.928 | |||||
| FC | 0.151 | 0.214 | 0.909 | ||||
| PE | 0.413 | 0.452 | 0.606 | 0.951 | |||
| SI | 0.103 | 0.025 | 0.752 | 0.475 | 0.872 | ||
| TA | 0.772 | 0.827 | 0.169 | 0.371 | 0.018 | 0.936 | |
| UB | 0.336 | 0.427 | 0.712 | 0.780 | 0.630 | 0.376 | 0.895 |
| Hypothesis | Path | β | p-Value | Hypotheses |
|---|---|---|---|---|
| H1 | EE→PE | 0.441 | 0.000 | Supported |
| H2 | EE→BI | 0.522 | 0.000 | Supported |
| H3 | PE→BI | 0.135 | 0.000 | Supported |
| H4 | SI→PE | 0.464 | 0.000 | Supported |
| H5 | SI→BI | −0.250 | 0.000 | Not supported |
| H6 | FC→BI | 0.100 | 0.073 | Not supported |
| H7 | FC→UB | 0.677 | 0.000 | Supported |
| H8 | FC→TA | −0.158 | 0.000 | Supported |
| H9 | TA→BI | −0.269 | 0.002 | Supported |
| H10 | BI→UB | 0.234 | 0.000 | Supported |
| H11a | Gender→TA | 0.064 | 0.400 | Not supported |
| H11b | FS→TA | 0.007 | 0.865 | Not supported |
| H11c | Education→TA | −0.281 | 0.000 | Supported |
| H11d | SU→TA | 0.860 | 0.005 | Supported |
| H11e | Experience→TA | 0.635 | 0.041 | Supported |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.; Yuan, J.; Shi, L.; Zhou, J.; Wang, H.; Li, C.; Dong, E.; Zhao, L. Understanding the Role of Technology Anxiety in the Adoption of Digital Health Technologies (DHTs) by Older Adults with Chronic Diseases in Shanghai: An Extension of the Unified Theory of Acceptance and Use of Technology (UTAUT) Model. Healthcare 2024, 12, 1421. https://doi.org/10.3390/healthcare12141421
Chen Y, Yuan J, Shi L, Zhou J, Wang H, Li C, Dong E, Zhao L. Understanding the Role of Technology Anxiety in the Adoption of Digital Health Technologies (DHTs) by Older Adults with Chronic Diseases in Shanghai: An Extension of the Unified Theory of Acceptance and Use of Technology (UTAUT) Model. Healthcare. 2024; 12(14):1421. https://doi.org/10.3390/healthcare12141421
Chicago/Turabian StyleChen, Yunhao, Jiajun Yuan, Lili Shi, Jiayun Zhou, Hansong Wang, Chengjin Li, Enhong Dong, and Liebin Zhao. 2024. "Understanding the Role of Technology Anxiety in the Adoption of Digital Health Technologies (DHTs) by Older Adults with Chronic Diseases in Shanghai: An Extension of the Unified Theory of Acceptance and Use of Technology (UTAUT) Model" Healthcare 12, no. 14: 1421. https://doi.org/10.3390/healthcare12141421
APA StyleChen, Y., Yuan, J., Shi, L., Zhou, J., Wang, H., Li, C., Dong, E., & Zhao, L. (2024). Understanding the Role of Technology Anxiety in the Adoption of Digital Health Technologies (DHTs) by Older Adults with Chronic Diseases in Shanghai: An Extension of the Unified Theory of Acceptance and Use of Technology (UTAUT) Model. Healthcare, 12(14), 1421. https://doi.org/10.3390/healthcare12141421





