Recommendations for Upper Limb Motor Recovery: An Overview of the UK and European Rehabilitation after Stroke Guidelines (2023)
Abstract
1. Introduction
1.1. Pathophysiology of Motor Deficit after Stroke
1.2. Upper Limb Impairment after Stroke
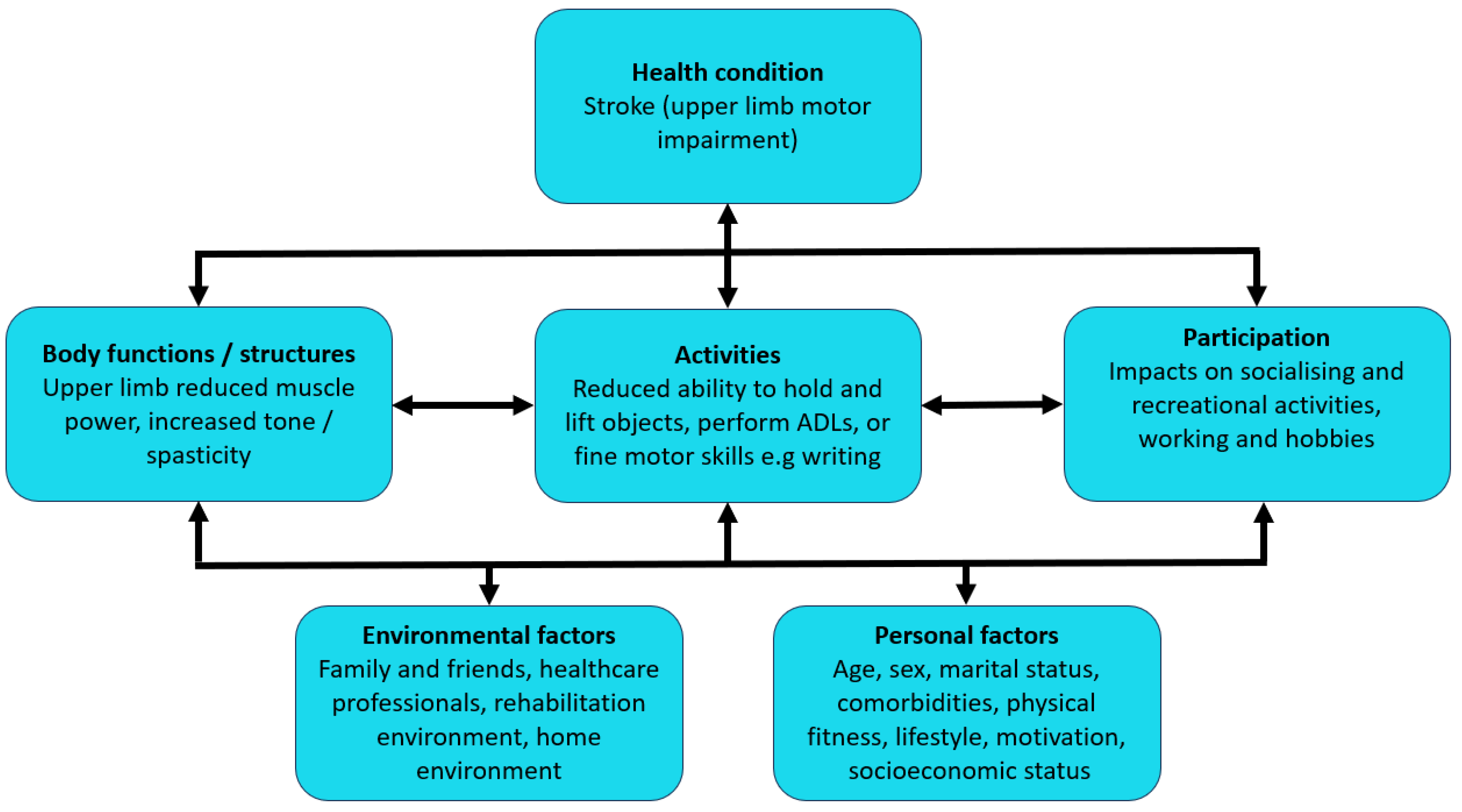
1.3. Upper Limb Impairment and Quality of Life
1.4. Management Approaches for Upper Limb Impairment
1.5. Stroke Rehabilitation Guidelines
1.6. Aims and Objectives
2. Materials and Methods
3. Results
3.1. Upper Limb Stroke Guidelines
3.2. General Approaches to Upper Limb Rehabilitation after Stroke
3.2.1. Therapeutic Intensity
3.2.2. Strength Training
3.2.3. Task-Specific Training/Repetitive Task Training
3.2.4. Mental Practice
3.3. Technology- and Device-Assisted Upper Limb Rehabilitation after Stroke
3.3.1. Constraint-Induced Movement Therapy
3.3.2. Splinting/Orthoses
3.3.3. Electrical Stimulation
3.3.4. Vagus Nerve Stimulation
3.3.5. Mirror Therapy
3.3.6. Robotic Therapy
3.3.7. Virtual Reality/Telerehabilitation
3.3.8. Other Approaches and Therapeutic Interventions
3.4. Management of Spasticity in the Upper Limb after Stroke
3.4.1. General Principles and Splinting
3.4.2. Drug Therapies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abedi, V.; et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 79–820. [Google Scholar] [CrossRef] [PubMed]
- Steel, N.; Ford, J.A.; Newton, J.N.; Davis, A.C.J.; Vos, T.; Naghavi, M.; Glenn, S.; Hughes, A.; Dalton, A.M.; Stockton, D.; et al. Changes in health in the countries of the UK and 150 English Local Authority areas 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018, 392, 1647–1661. [Google Scholar] [CrossRef] [PubMed]
- Stroke Association. State of the Nation: Stroke Statistics. 2016. Available online: www.stroke.org.uk/sites/default/files/stroke_statistics_2015.pdf (accessed on 2 March 2022).
- Wafa, H.A.; Wolfe, C.D.A.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of Stroke in Europe. Stroke 2020, 51, 2418–2427. [Google Scholar] [CrossRef] [PubMed]
- Purves, D.; Augustine, G.J.; Fitzpatrick, D.; Katz, L.C.; LaMantia, A.S.; McNamara, J.O.; Williams, S.M. Functional Organization of the Primary Motor Cortex. In Neuroscience, 2nd ed.; Sinauer Associates: Sunderland, MA, USA, 2001. Available online: https://www.ncbi.nlm.nih.gov/books/NBK11095/ (accessed on 27 June 2024).
- Hui, C.; Tadi, P.; Patti, L. Ischemic Stroke. In MEDSURG Nursing; StatPearls Publishing: Treasure Island, FL, USA, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK499997/ (accessed on 10 August 2021).
- Unnithan, A.K.A.; Das, J.M.; Mehta, P. Hemorrhagic Stroke. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK559173/ (accessed on 27 June 2024).
- Persson, H.C.; Opheim, A.; Lundgren-Nilsson, Å.; Alt Murphy, M.; Danielsson, A.; Sunnerhagen, K.S. Upper extremity recovery after ischaemic and haemorrhagic stroke: Part of the SALGOT study. Eur. Stroke J. 2016, 1, 310–319. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, H.; Stig Jørgensen, H.; Otto Raaschou, H.; Skyhøj Olsen, T. Recovery of upper extremity function in stroke patients: The Copenhagen stroke study. Arch. Phys. Med. Rehabil. 1994, 75, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Persson, H.C.; Parziali, M.; Danielsson, A.; Sunnerhagen, K.S. Outcome and upper extremity function within 72 hours after first occasion of stroke in an unselected population at a stroke unit. A part of the SALGOT study. BMC Neurol. 2012, 12, 162. [Google Scholar] [CrossRef]
- Lawrence, E.; Coshall, C.; Dundas, R.; Stewart, J.; Rudd, A.; Howard, R.; Wolfe, C.D.A. Estimates of the prevalence of acute stroke impairments and disability in a multiethnic population. Stroke 2001, 32, 1279–1284. [Google Scholar] [CrossRef]
- Soo, Y.; Leung, H.; Wong, L.K. What are this patient’s problems? A problem-based approach to the general management of stroke. In Warlow’s Stroke: Practical Management, 4th ed.; Hankey, G.J., Macleod, M., Gorelick, P.B., Chen, C., Caprio, F.Z., Mattle, H., Eds.; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2019; pp. 481–529. [Google Scholar] [CrossRef]
- Friedman, P. Gait recovery after hemiplegic stroke. Int. Disabil. Stud. 1990, 12, 119–122. [Google Scholar] [CrossRef] [PubMed]
- Tomita, Y.; Rodrigues, M.R.M.; Levin, M.F. Upper Limb Coordination in Individuals With Stroke: Poorly Defined and Poorly Quantified. Neurorehabil. Neural. Repair. 2017, 31, 885–897. [Google Scholar] [CrossRef]
- Kessner, S.S.; Schlemm, E.; Cheng, B.; Bingel, U.; Fiehler, J.; Gerloff, C.; Thomalla, G. Somatosensory Deficits after Ischemic Stroke: Time Course and Association with Infarct Location. Stroke 2019, 50, 1116–1123. [Google Scholar] [CrossRef]
- Borisova, Y.; Bohannon, R.W. Positioning to prevent or reduce shoulder range of motion impairments after stroke: A meta-analysis. Clin. Rehabil. 2009, 23, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Yong, J.; MacDermid, J.C.; Packham, T.; Bobos, P.; Richardson, J.; Moll, S. Performance-based outcome measures of dexterity and hand function in person with hands and wrist injuries: A scoping review of measured constructs. J. Hand Ther. 2022, 35, 200–214. [Google Scholar] [CrossRef] [PubMed]
- Marciniak, C. Poststroke Hypertonicity: Upper Limb Assessment and Treatment. Top. Stroke Rehabil. 2011, 18, 179–194. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J.; Hallett, M.; Okun, M.S.; Comella, C.; Fahn, S.; Goldman, J.G. Stiffness syndromes. In Principles and Practice of Movement Disorders, 3rd ed.; Elsevier: Amsterdam, The Netherlands, 2021; pp. 537–542. Available online: www.sciencedirect.com/book/9780323310710/principles-and-practice-of-movement-disorders (accessed on 8 March 2022).
- Lang, C.E. Impaired motor control. In Geriatric Physical Therapy, 3rd ed.; Elsevier: Amsterdam, The Netherlands, 2012; pp. 272–291. [Google Scholar] [CrossRef]
- Gowda, S.N.; Schneider, L.K. Apraxia. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK585110/ (accessed on 27 June 2024).
- Broeks, J.; Lankhorst, G.; Rumping, K.; Prevo, A. The long-term outcome of arm function after stroke: Results of a follow-up study. Disabil. Rehabil. 1999, 21, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Egbert, N.; Koch, L.; Coeling, H.; Ayers, D. The Role of Social Support in the Family and Community Integration of Right-Hemisphere Stroke Survivors. Health Commun. 2009, 20, 45–55. [Google Scholar] [CrossRef] [PubMed]
- van der Kemp, J.; Kruithof, W.J.; Nijboer, T.C.W.; van Bennekom, C.A.M.; van Heugten, C.; Visser-Meily, J.M.A. Return to work after mild-to-moderate stroke: Work satisfaction and predictive factors. Neuropsychol. Rehabil. 2019, 29, 638–653. [Google Scholar] [CrossRef] [PubMed]
- van Lieshout, E.C.C.; van de Port, I.G.; Dijkhuizen, R.M.; Visser-Meily, J.M.A. Does upper limb strength play a prominent role in health-related quality of life in stroke patients discharged from inpatient rehabilitation? Top. Stroke Rehabil. 2020, 27, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Martinsen, R.; Kirkevold, M.; Sveen, U. Younger Stroke Survivors’ Experiences of Family Life in a Long-Term Perspective: A Narrative Hermeneutic Phenomenological Study. Nurs. Res. Pr. 2012, 2012, 948791. [Google Scholar] [CrossRef]
- Dowswell, G.; Lawler, J.; Dowswell, T.; Young, J.; Forster, A.; Hearn, J. Investigating recovery from stroke: A qualitative study. J. Clin. Nurs. 2000, 9, 507–515. [Google Scholar] [CrossRef]
- Pallesen, H. Body, coping and self-identity. A qualitative 5-year follow-up study of stroke. Disabil. Rehabil. 2013, 36, 232–241. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Towards a Common Language for Functioning, Disability and Health; World Health Organization (WHO): Geneva, Switzerland, 2002; Available online: https://cdn.who.int/media/docs/default-source/classification/icf/icfbeginnersguide.pdf (accessed on 30 June 2024).
- Aguiar de Sousa, D.; von Martial, R.; Abilleira, S.; Gattringer, T.; Kobayashi, A.; Gallofré, M.; Fazekas, F.; Szikora, I.; Feigin, V.; Caso, V.; et al. Access to and delivery of acute ischaemic stroke treatments: A survey of national scientific societies and stroke experts in 44 European countries. Eur. Stroke J. 2019, 4, 13–28. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Stroke Rehabilitation in Adults. 2023. Available online: https://www.nice.org.uk/guidance/ng236 (accessed on 24 April 2024).
- Intercollegiate Stroke Working Party. National Clinical Guideline for Stroke. 2023. Available online: www.strokeguideline.org (accessed on 25 April 2024).
- National Institute for Health and Care Excellence. Stroke Rehabilitation in Adults Clinical Guideline; NICE: London, UK, 2013; pp. 6–37. Available online: www.nice.org.uk/guidance/cg162 (accessed on 22 July 2021).
- Intercollegiate Stroke Working Party. National Clinical guideline for Stroke, 5th ed.; Royal College of Physicians: London, UK, 2016; Available online: https://www.strokeaudit.org/Guideline/Full-Guideline.aspx (accessed on 19 March 2022).
- National Institute for Health and Care Excellence. Our Charter: Who We Are and What We Do. Available online: https://www.nice.org.uk/about/who-we-are/our-charter#:~:text=The%20National%20Institute%20for%20Health,ensuring%20value%20for%20the%20taxpayer (accessed on 10 May 2024).
- National Institute for Health and Care Excellence. Developing NICE Guidelines: The Manual. 2014. Available online: https://www.nice.org.uk/process/pmg20 (accessed on 27 June 2024).
- Kwakkel, G.; Stinear, C.; Essers, B.; Munoz-Novoa, M.; Branscheidt, M.; Cabanas-Valdés, R.; Lakičević, S.; Lampropoulou, S.; Luft, A.R.; Marque, P.; et al. Motor rehabilitation after stroke: European Stroke Organisation (ESO) consensus-based definition and guiding framework. Eur. Stroke J. 2023, 8, 880–894. [Google Scholar] [CrossRef] [PubMed]
- Scottish Intercollegiate Guidelines Network. Management of Patients with Stroke: Rehabilitation, Prevention and Management of Complications, and Discharge Planning. 2010. Available online: https://digirepo.nlm.nih.gov/master/borndig/101609293/sign118.pdf (accessed on 17 March 2022).
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Deruyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L.; et al. Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef] [PubMed]
- Intercollegiate Stroke Working Party. National Clinical Guideline for Stroke: Scope. 2023. Available online: https://www.strokeguideline.org/app/uploads/2023/03/Scope.pdf (accessed on 20 May 2024).
- Norrving, B.; Barrick, J.; Davalos, A.; Dichgans, M.; Cordonnier, C.; Guekht, A.; Kutluk, K.; Mikulik, R.; Wardlaw, J.; Richard, E.; et al. Action Plan for Stroke in Europe 2018–2030. Eur. Stroke J. 2018, 3, 309–336. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Stroke Rehabilitation in Adults: Visual Summary. 2023. Available online: https://www.nice.org.uk/guidance/ng236/resources/visual-summary-pdf-13193478253 (accessed on 20 May 2024).
- Intercollegiate Stroke Working Party. Care after Stroke or Transient Ischaemic Attack: What, When and Why? Plain Language Summary for People Affected by Stroke. London. 2023. Available online: https://www.strokeguideline.org/app/uploads/2023/03/Plain-language-summary.pdf?_gl=1*1v2xu89*_up*MQ..*_ga*MTI5ODMwNTgwMi4xNzE2MjAzNTQx*_ga_EE3BZMVLRT*MTcxNjIwMzU0MC4xLjAuMTcxNjIwMzU0MC4wLjAuMA (accessed on 20 May 2024).
| Impairment | Features |
|---|---|
| Incoordination | Inability to execute motor responses with appropriate accuracy, speed and smoothness |
| Paresis | Partial loss of skeletal muscle strength, reducing voluntary movement ability in the affected region |
| Paralysis | Complete loss of skeletal muscle strength; voluntary movement will be absent in the affected region |
| Somatosensory loss | Reduced sensation in modalities such as light touch, pressure, sharp–dull discrimination, temperature, pain, two-point discrimination and proprioception |
| Reduced range of movement | Decreased extent to which a limb or body part can be rotated around a joint |
| Reduced dexterity | Diminished ability to perform fine motor skills to achieve a task in an accurate and timely manner, while adapting to any environmental changes that occur |
| Hypertonia/spasticity | Increased muscular tone; resistance to passive movement may or may not be velocity-dependent |
| General Approaches to Upper Limb Rehabilitation after Stroke | NICE | ISWP | ESO |
|---|---|---|---|
| Therapeutic intensity |
|
|
|
| Strength training |
|
|
|
| Task-specific training/repetitive task training (TST/RTT) |
|
|
|
| Mental practice (MP) |
|
|
|
| Technology-/Device-Assisted Rehabilitation | NICE | ISWP | ESO |
|---|---|---|---|
| Constraint-induced movement therapy (CIMT) |
|
|
|
| Splinting/orthoses |
|
|
|
| Electrical stimulation (ES) |
|
|
|
| Vagus nerve stimulation (VNS) |
|
|
|
| Mirror therapy |
|
|
|
| Robotic therapy |
|
|
|
| Virtual reality (VR)/telerehabilitation |
|
|
|
| Spasticity Management | NICE | ISWP | ESO |
|---|---|---|---|
| General recommendations and splinting |
|
|
|
| Drug therapies |
|
|
|
| Electrical stimulation (ES) |
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Flaherty, D.; Ali, K. Recommendations for Upper Limb Motor Recovery: An Overview of the UK and European Rehabilitation after Stroke Guidelines (2023). Healthcare 2024, 12, 1433. https://doi.org/10.3390/healthcare12141433
O’Flaherty D, Ali K. Recommendations for Upper Limb Motor Recovery: An Overview of the UK and European Rehabilitation after Stroke Guidelines (2023). Healthcare. 2024; 12(14):1433. https://doi.org/10.3390/healthcare12141433
Chicago/Turabian StyleO’Flaherty, Daniel, and Khalid Ali. 2024. "Recommendations for Upper Limb Motor Recovery: An Overview of the UK and European Rehabilitation after Stroke Guidelines (2023)" Healthcare 12, no. 14: 1433. https://doi.org/10.3390/healthcare12141433
APA StyleO’Flaherty, D., & Ali, K. (2024). Recommendations for Upper Limb Motor Recovery: An Overview of the UK and European Rehabilitation after Stroke Guidelines (2023). Healthcare, 12(14), 1433. https://doi.org/10.3390/healthcare12141433






