Cybernetic Principles in Psychophysiology: Their Significance and Conclusions for Palliative Care
Abstract
:1. Introduction
1.1. Cybernetic Systems Offer Three Advantages
1.2. The Role of Psychophysiology
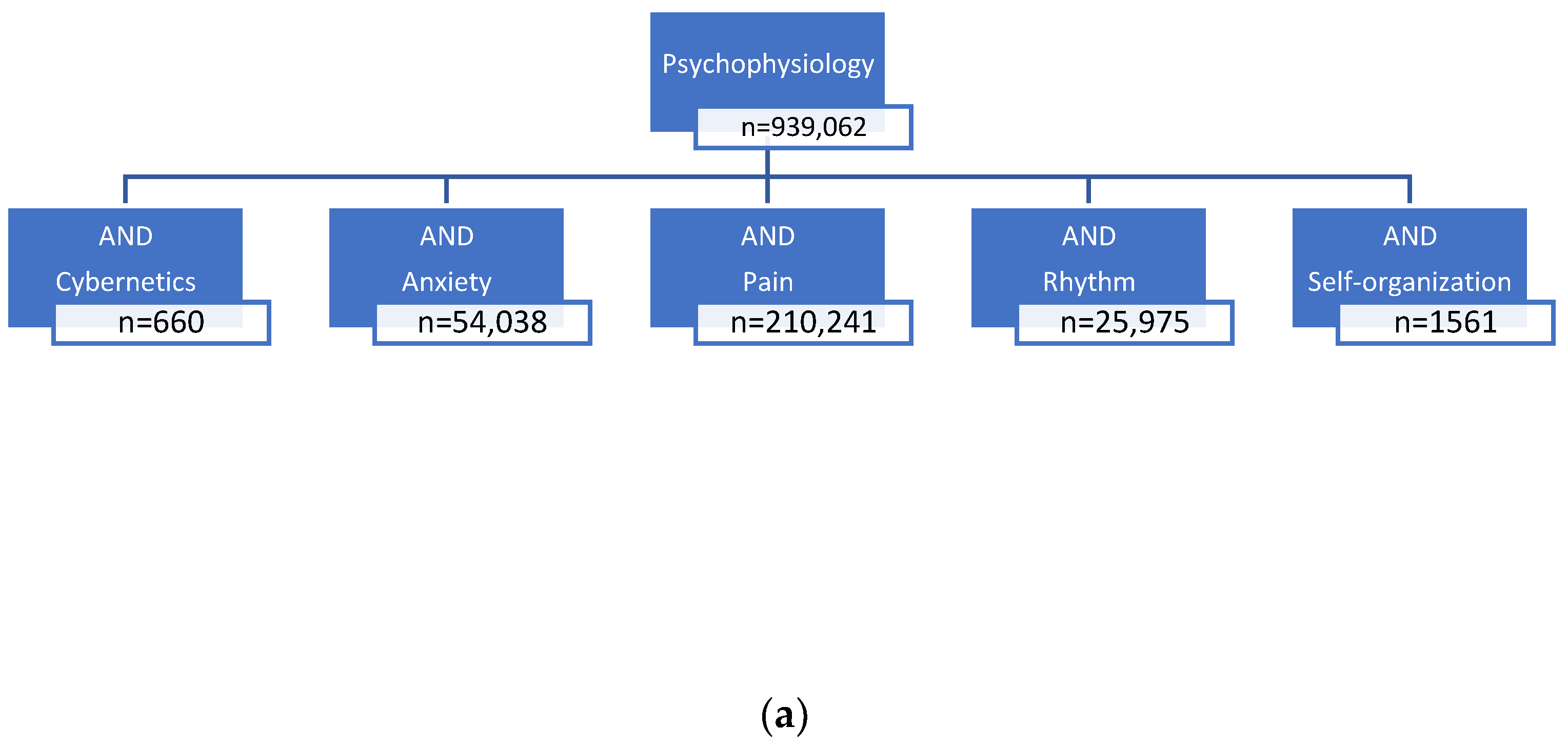
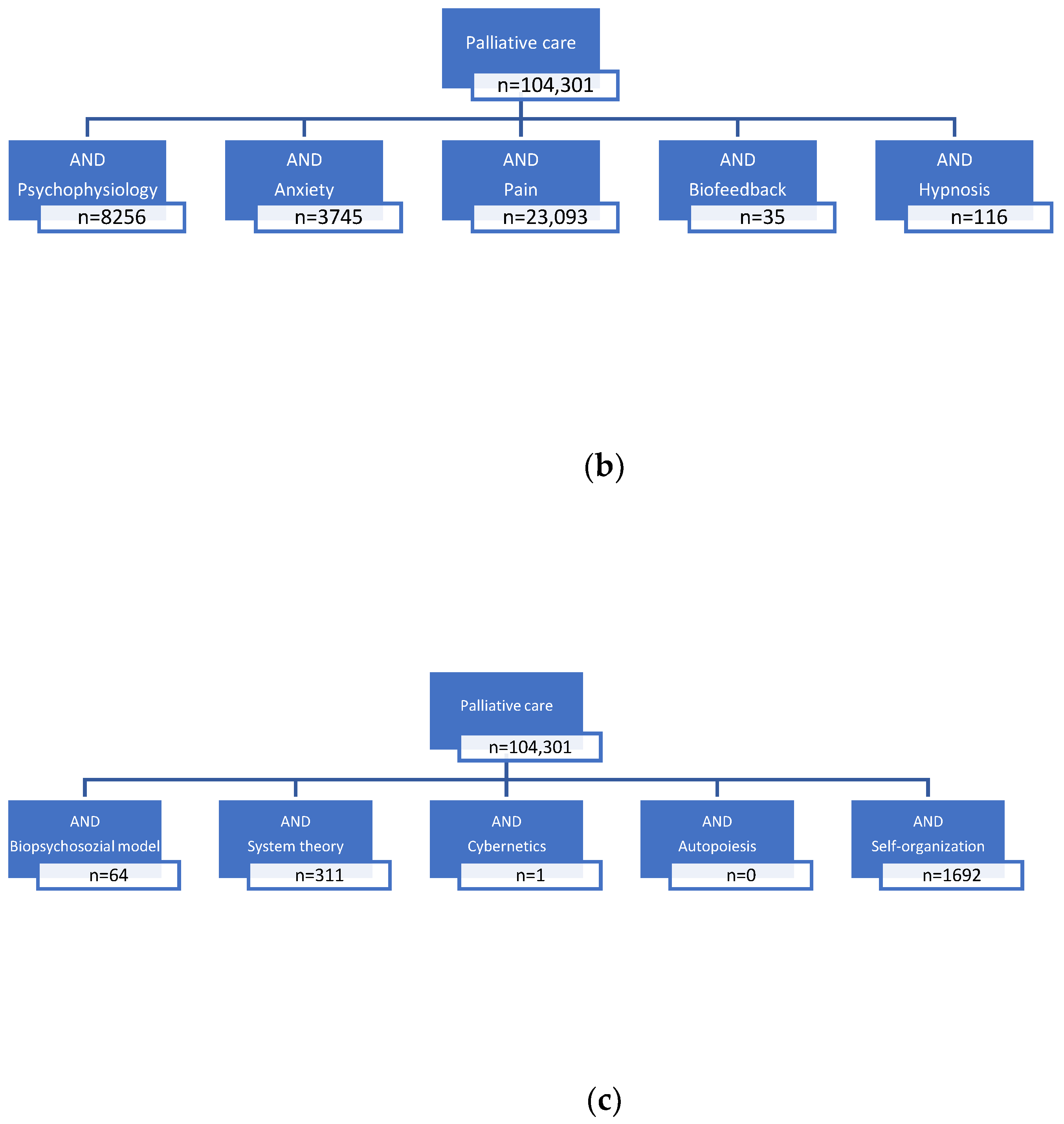
2. Materials and Methods
3. Results
3.1. Cybernetics Principles in Psychophysiology
3.1.1. Cybernetic Principles of Psychophysiological Terms
3.1.2. Further Common Themes of Psychophysiology and Cybernetics
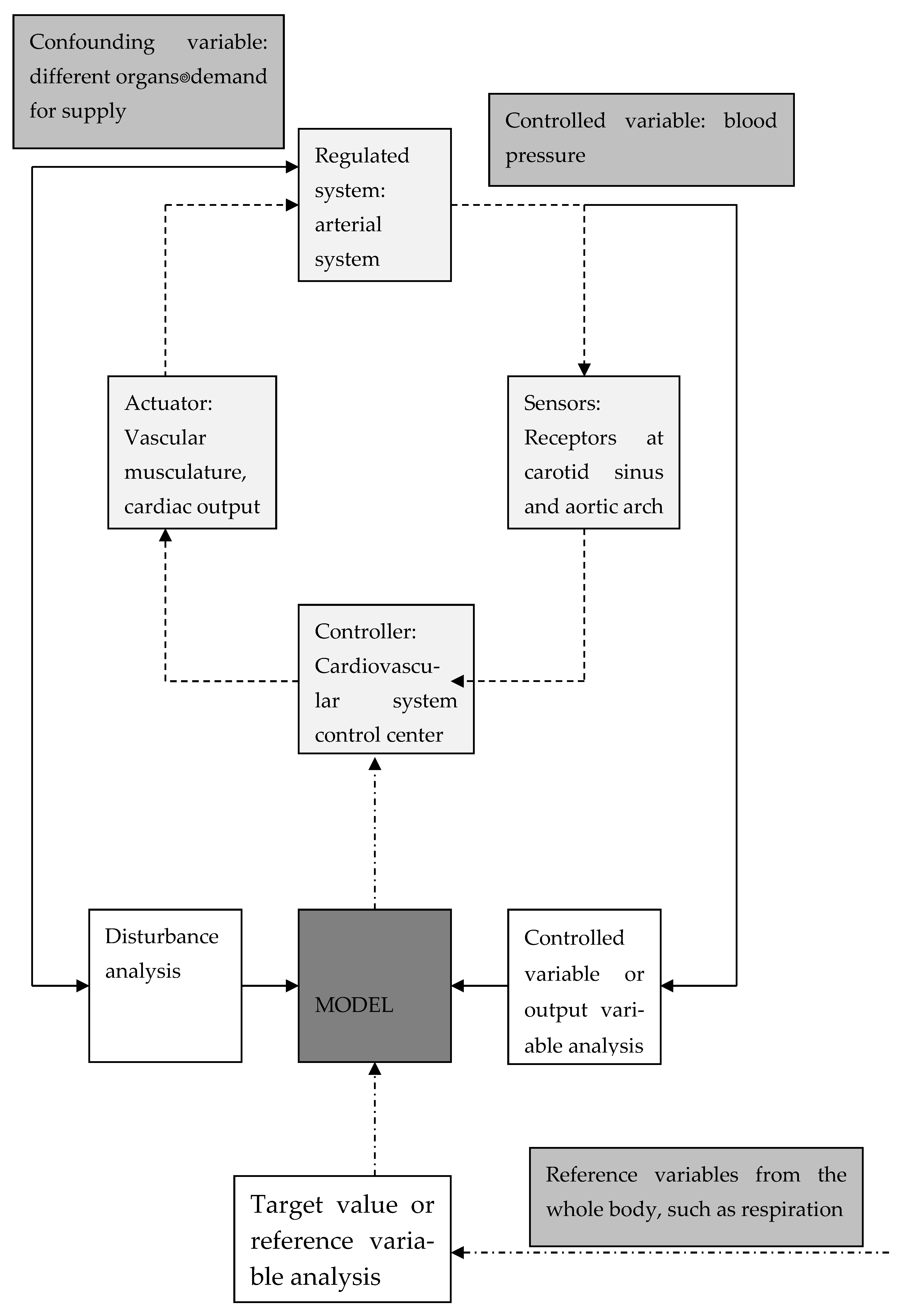
3.1.3. Circulatory Model
3.2. Cybernetics of Living Systems (Circulatory Model)
4. Discussion
4.1. Cybernetic Principles in Psychophysiology
4.1.1. The Subjectivity
Circulatory Model
The Counter-Regulation: Cybernetics of Psychophysiology in Illnesses/Diseases
4.1.2. Psychophysiological Therapies of Illnesses/Diseases
4.2. Cybernetics in Palliative Care
- Section 4.2.1 discusses palliative care concepts and their cybernetic equivalents;
- Section 4.2.2 debates cybernetic terms without corresponding palliative medicine equivalents.
4.2.1. Palliative Care Concepts and Their Cybernetic Equivalents
4.2.2. Cybernetic Terms without Corresponding Palliative Care Equivalents
- Activity. Actions are provided by me.
- Unity of the “I”: I can never break down into several independent ego parts.
- Continuity of “I”: Yesterday I was me. Today I am, too.
- Independence of the “I”: I am no one other than myself.
4.3. The Role of Psychophysiology in Palliative Care
- Physiological processes are measurable (EEG, 24-h ECG);
- They are not identical in all people, but are individual;
- There is no compelling relationship between observable/observable physiological parameters and the conditions perceived by the patient.
- Interoception is the perception of one’s own psychophysical states.
- Personality traits.
- Tipping Point/Overload
- (a)
- A preliminary phase or rehabilitation phase:
- (b)
- Preterminal phase:
- (c)
- Terminal phase:
- (d)
- Final phase:
4.3.1. Symptom Burden (of Anxiety and Pain) in General
4.3.2. Anxiety and Pain
4.3.3. Consciousness
4.4. Strengths, Limitations, and Criticism of the Narrative Review
4.4.1. Strengths
4.4.2. Limitations
4.4.3. Criticism
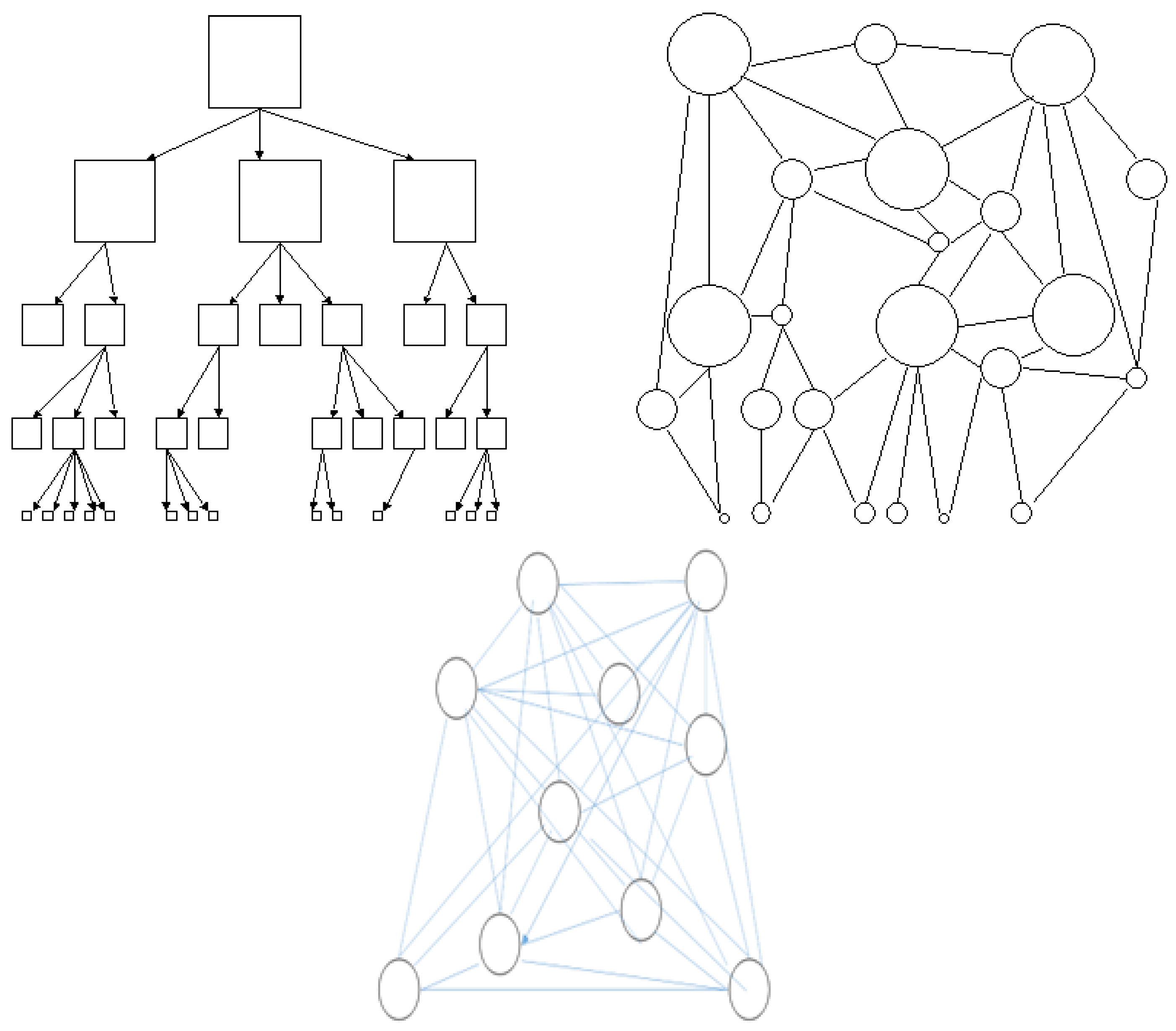
5. Conclusions
- The common theme of cybernetic thinking, psychophysiology, and palliative care is the concept of subjectivity.
- Cybernetics and psychophysiology are significant for palliative care within the concepts of quality of life, autonomy, and symptom control.
- Works on applied cybernetics in biology, psychophysiology, and business management demonstrate the practical applicability of the notions of complexity, identity, rhythmicity, and temporal behavior. However, these have not yet been formally used in palliative care.
- Concrete measures and therapies for the subjective benefit of palliative patients are based in particular on psychophysiology (bio-feedback, hypnosis).
- Cybernetics teaches that networked systems are superior to hierarchical structures in solving problems. This is a consequence of pattern recognition rather than data accumulation and the rejection of local solutions. For palliative care, the comparison with cybernetic thinking means that therapy is not a matter of exhausting the maximum or restitutio ad integrum, but of “going with the flow” in recognition of what is still possible for the patient, regardless of what has determined the sense of the limits of life. This is a central demand not only of psychophysiology, but of palliative care in general.
- The assumption of a cybernetic biopsychosocial system would pay more attention to the remaining possibilities, dispositions, and subjective requirements of the individual. All of this is the basis of psychophysiology in particular.
- It would be advisable for palliative care to take a closer look at these issues.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schmidgen, H. Cybernetic times: Norbert Wiener, John Stroud, and the ‘brain clock’ hypothesis. Hist. Hum. Sci. 2020, 33, 80–108. [Google Scholar] [CrossRef]
- Rösler, F. (Ed.) Results and Applications of Psychophysiology [Ergebnisse und Anwendungen der Psychophysiologie]; Hogrefe: Göttingen, Germany, 1998; ISBN 3801705455. [Google Scholar]
- Bissonnette, J.; Pierre, S.; Duong, A.T.J.; Pinard, A.-M.; Rainville, P.; Ogez, D. Development of a Mixed Hypnosis and Music Intervention Program for the Management of Pain, Anxiety, and Wellbeing in End-of-Life Palliative Care. Front. Pain Res. 2022, 3, 926584. [Google Scholar] [CrossRef] [PubMed]
- von Uexküll, T.; Wesiak, W. Theory of Human Medicine [Theorie der Humanmedizin]; Urban und Schwarzenberg: München, Germany; Wien, Austria; Balimore, MD, USA, 1991. [Google Scholar]
- Vossius, G. Fundamentals of biological cybernetics [Grundlagen der biologischen Kybernetik]. In Human Physiology [Physiologie des Menschen], 10th ed.; Gauer, O.H., Kramer, K., Jung, R., Eds.; Urban und Schwarzenberg: München, Germany; Wien, Austria; Balimore, MD, USA, 1980; pp. 224–240. [Google Scholar]
- Weiner, H. Is the “biopsychosocial model” a helpful construct? [Das biopsychosoziale Modell” ein hilfreiches Konstrukt?]. Psychother. Psychosom. Med. Psychol. 1994, 44, 73–83. [Google Scholar] [PubMed]
- Böckelmann, I.; Sammito, S. Heart rate variability [Herzfrequenzvariabilität]. In Handbook of Occupational Medicine [Handbuch der Arbeitsmedizin]; 41. Ergänzungslieferung, 06/2016; Letzel, S., Nowak, D., Eds.; Ecomed Medizin: Landsberg, Germany, 2016; pp. 1–32. [Google Scholar]
- Sammito, S.; Thielmann, B.; Klussmann, A.; Deußen, A.; Braumann, K.-M.; Böckelmann, I. Guideline for the application of heart rate and heart rate variability in occupational medicine and occupational health science. J. Occup. Med. Toxicol. 2024, 19, 15. [Google Scholar] [CrossRef] [PubMed]
- Böckelmann, I.; Pohl, R.; Darius, S.; Thielmann, B.; Sammito, S.; Riesemann, M.; Jarczok, M.N.; Glomb, S.; Delhey, M.; Gündel, H.; et al. Assessment of autonomic nervous system activation in pain patients using heart rate variability [Beurteilung der Aktivierung des autonomen Nervensystems bei Schmerzpatienten anhand der Herzfrequenzvariabilität]. In Heart Rate Variability: Applications in Research and Practice [Herzfrequenzvariabilität: Anwendungen in Forschung und Praxis]; Hottenrott, K., Böckelmann, I., Schmidt, H., Eds.; Feldhaus Edition Czwalina: Hamburg, Germany, 2021. [Google Scholar]
- Trappe, H.-J. Music and health--what kind of music is helpful for whom? What music not? Dtsch. Med. Wochenschr. 2009, 134, 2601–2606. [Google Scholar] [CrossRef] [PubMed]
- Goepfert, M.; Liebl, P.; Herth, N.; Ciarlo, G.; Buentzel, J.; Huebner, J. Aroma oil therapy in palliative care: A pilot study with physiological parameters in conscious as well as unconscious patients. J. Cancer Res. Clin. Oncol. 2017, 143, 2123–2129. [Google Scholar] [CrossRef] [PubMed]
- Wagner, B.; Steiner, M.; Huber, D.F.X.; Crevenna, R. The effect of biofeedback interventions on pain, overall symptoms, quality of life and physiological parameters in patients with pelvic pain: A systematic review. Wien. Klin. Wochenschr. 2022, 134, 11–48. [Google Scholar] [CrossRef] [PubMed]
- Groß, M.; Demmer, T. (Eds.) Interdisciplinary Palliative Medicine [Interdisziplinäre Palliativmedizin]; Springer: Berlin/Heidelberg, Germany, 2021; ISBN 978-3-662-62011-3. [Google Scholar]
- Abbass, A.; Schubiner, H. Psychophysiological Disorders [Psychophysiologische Störungen]: A Guide to Diagnosis, Psychotherapy and Basic Psychosomatic Care [Ein Leitfaden für Diagnose, Psychotherapie und Psychosomatische Grundversorgung]; Kohlhammer Verlag: Stuttgart, Germany, 2020; ISBN 9783170367333. [Google Scholar]
- Brinkers, M. Bio-psycho-social aspects of movement function [Bio-psycho-soziale Aspekte der Bewegungsfunktion]. In Functional Medicine of the Musculoskeletal System [Funktionsmedizin des Bewegungssystems]; Beyer, L., Liefring, V., Niemier, K., Seidel, E.J., Eds.; KIENER: München, Germany, 2023; pp. 69–76. ISBN 9783948442248. [Google Scholar]
- Popkirov, S. General pathophysiological models of explanation [Allgemeine pathophysiologische Erklärungsmodelle]. In Functional Neurological Disorders: Recognize, Understand, Treat [Funktionelle Neurologische Störungen: Erkennen, Verstehen, Behandeln]; Popkirov, S., Ed.; Springer: Berlin/Heidelberg, Germany, 2020; pp. 9–15. ISBN 978-3-662-61272-9. [Google Scholar]
- Doering, S.; Söllner, W. The psychosomatics of chronic pain [Zur Psychosomatik chronischer Schmerzen]. Orthopade 1997, 26, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Vogelzang, N.J.; Breitbart, W.; Cella, D.; Curt, G.A.; Groopman, J.E.; Horning, S.J.; Itri, L.M.; Johnson, D.H.; Scherr, S.L.; Portenoy, R.K. Patient, caregiver, and oncologist perceptions of cancer-related fatigue: Results of a tripart assessment survey. The Fatigue Coalition. Semin. Hematol. 1997, 34, 4–12. [Google Scholar] [PubMed]
- Williams, L.A.; Bohac, C.; Hunter, S.; Cella, D. Patient and health care provider perceptions of cancer-related fatigue and pain. Support. Care Cancer 2016, 24, 4357–4363. [Google Scholar] [CrossRef]
- Houska, A.; Loučka, M. Patients’ Autonomy at the End of Life: A Critical Review. J. Pain Symptom Manag. 2019, 57, 835–845. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, A.A. Development and Evaluation of Self-Instructive Body-Mindfulness Programs for Health Promotion and Recovery in the Workplace [Entwicklung und Evaluation Selbstinstruktiver Körper-Achtsamkeitsprogramme zur Gesundheitsförderung und Erholung am Arbeitsplatz]; Fakultät III, Pädagogische Hochschule Karlsruhe: Karlsruhe, Germany, 2017. [Google Scholar]
- Stepken, G. Cybernetics of Cybernetics—Laws of Networks [Kybernetik der Kybernetik—Gesetze der Netze]. Available online: https://silo.tips/download/kybernetik-der-kybernetik-gesetze-der-netze (accessed on 31 December 2023).
- Meyer, N.; Harvey, A.G.; Lockley, S.W.; Dijk, D.-J. Circadian rhythms and disorders of the timing of sleep. Lancet 2022, 400, 1061–1078. [Google Scholar] [CrossRef]
- Schwartz, G.E. Biofeedback and the behavioral treatment of disorders of disregulation. Yale J. Biol. Med. 1979, 52, 581–596. [Google Scholar]
- Geissner, E. Psychological models of pain and pain processing [Psychologische Modelle des Schmerzens und der Schmerzverarbeitung]. In Psychology of Pain [Psychologie des Schmerzes]; Geissner, E., Jungnitsch, G., Eds.; Psychologie-Verl.-Union: Weinheim, Germany, 1992; pp. 25–41. ISBN 3621271252. [Google Scholar]
- Hürter, A. The bio-psycho-social model [Das bio-psycho-soziale Modell]. In Interdisciplinary Pain Therapy [Schmerztherapie Interdisziplinär]; Gralow, I., Berger, K., Eds.; Schattauer: Stuttgart, Germany, 2002; pp. 47–50. ISBN 3-7945-2118-8. [Google Scholar]
- Luisi, P.L. Autopoiesis: A review and a reappraisal. Naturwissenschaften 2003, 90, 49–59. [Google Scholar] [CrossRef]
- Maturana, H.R.; Varela, F.J.; Beer, S. Autopoiesis and Cognition: The Realization of the Living; Reidel: Dordrecht, The Netherlands, 1980; ISBN 9027710155. [Google Scholar]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef]
- Vester, F. The Art of Networked Thinking. Ideas and Tools for a New Approach to Complexity; a Report to the Club of Rome [Die Kunst Vernetzt zu Denken. Ideen und Werkzeuge für Einen Neuen Umgang mit Komplexität; ein Bericht an den Club of Rome], 10. Aufl.; Dt. Taschenbuch-Verl.: München, Germany, 2015; ISBN 9783423330770. [Google Scholar]
- Wolf, G. Shaping complexity through network management [Gestalten von Komplexität durch Netzwerk-Management]. In Basic Principles of Self-Organization [Grundprinzipien der Selbstorganisation]; Kratky, K.W., Wallner, F., Eds.; Wissenschaftliche Buchgesellschaft: Darmstadt, Germany, 1990; pp. 103–126. [Google Scholar]
- Bertschinger, N.; Olbrich, E.; Ay, N.; Jost, J. Autonomy: An information theoretic perspective. Biosystems 2008, 91, 331–345. [Google Scholar] [CrossRef] [PubMed]
- Luhmann, N. Sociological Education 6 Sociology and the Human Being [Soziologische Aufklärung 6. Die Soziologie under der Mensch]; Verlag für Sozialwissenschaften: Opladen, Germany, 1995. [Google Scholar]
- Moreno, A.; Etxeberria, A.; Umerez, J. The autonomy of biological individuals and artificial models. Biosystems 2008, 91, 309–319. [Google Scholar] [CrossRef]
- Schipek, G. Self-reference in psychological and social systems [Selbstreferenz in psychischen und sozialen Systemen]. In Basic Principles of Self-Organization [Grundprinzipien der Selbstorganisation]; Kratky, K.W., Wallner, F., Eds.; Wissenschaftliche Buchgesellschaft: Darmstadt, Germany, 1990; pp. 182–200. [Google Scholar]
- Niedermüller, H.; Hofecker, G. Possible applications of the principle of autopoiesis to physiological and gerontological issues [Anwendungsmöglichkeiten des Prinzips der Autopoiese auf physiologische und gerontologische Fragestellungen]. In Basic Principles of Self-Organization [Grundprinzipien der Selbstorganisation]; Kratky, K.W., Wallner, F., Eds.; Wissenschaftliche Buchgesellschaft: Darmstadt, Germany, 1990; pp. 201–218. [Google Scholar]
- Etxeberria, A. Autopoiesis and natural drift: Genetic information, reproduction, and evolution revisited. Artif. Life 2004, 10, 347–360. [Google Scholar] [CrossRef] [PubMed]
- Luhmann, N. The Society of Society. First and Second Volumes [Die Gesellschaft der Gesellschaft. Erster und Zweiter Teilband]; Suhrkamp: Frankfurt am Main, Germany, 1997. [Google Scholar]
- Miltner, W.H.R. Psychophysiology of pain [Psychophysiologie des Schmerzes]. In Results and Applications of Psychophysiology [Ergebnisse und Anwendungen der Psychophysiologie; Rösler, F., Ed.; Hogrefe: Göttingen, Germany, 1998; pp. 479–523. ISBN 3801705455. [Google Scholar]
- Frone, M.R.; McFarlin, D.B. Chronic occupational stressors, self-focused attention, and well-being: Testing a cybernetic model of stress. J. Appl. Psychol. 1989, 74, 876–883. [Google Scholar] [CrossRef]
- Brinkers, M.; Pfau, G.; Niemier, K. Lack of functional examination in patients with chronic pain—And now? A case series on functional, manual therapeutic, psychiatric, and cybernetic aspects [Fehlende funktionelle Untersuchung bei Patienten mit chronischen Schmerzen—Und nun?]. Manuelle Medizin 2023, 61, 165–172. [Google Scholar] [CrossRef]
- Baltissen, R.; Sartory, G. Orientation, defensive and startle reactions [Orientierungs-, Defensiv- und Schreckreaktionen]. In Results and Applications of Psychophysiology [Ergebnisse und Anwendungen der Psychophysiologie]; Rösler, F., Ed.; Hogrefe: Göttingen, Germany, 1998; pp. 29–31. ISBN 3801705455. [Google Scholar]
- Dankert, A.; Duran, G.; Engst-Hastreiter, U.; Keller, M.; Waadt, S.; Henrich, G.; Herschbach, P. Fear of progression in patients with cancer, diabetes mellitus and chronic arthritis. Rehabilitation 2003, 42, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Facco, E.; Casiglia, E.; Zanette, G.; Testoni, I. On the way of liberation from suffering and pain: Role of hypnosis in palliative care. Ann. Palliat. Med. 2018, 7, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Herschbach, P.; Dankert, A.; Duran-Atzinger, G.; Waadt, S.; Engst-Hastreiter, U.; Keller, M.; Henrich, G. Wissenschaftliche Darstellung Diagnostik von Progredienzangst—Entwicklung eines Fragebogens zur Erfassung von Progredienzangst bei Patienten mit Krebserkrankungen, Diabetes Mellitus und Entzündlich-Rheumatischen Erkrankungenin der Rehabilitation: RFB—Wissenschaftliche Darstellung Projekt A2: Progredienzangst. Available online: https://docplayer.org/35426953-Diagnostik-von-progredienzangst.html (accessed on 20 January 2024).
- Krooupa, A.-M.; Vivat, B.; McKeever, S.; Marcus, E.; Sawyer, J.; Stone, P. Identification and evaluation of observational measures for the assessment and/or monitoring of level of consciousness in adult palliative care patients: A systematic review for I-CAN-CARE. Palliat. Med. 2020, 34, 83–113. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, G. Cybernetics and Biology [Kybernetik und Biologie]; Metzler: Stuttgart, Germany, 1972; ISBN 3476300056. [Google Scholar]
- ben-Aaron, M. Sudden infant death syndrome: A cybernetic etiology. Med. Hypotheses 2003, 61, 601–604. [Google Scholar] [CrossRef] [PubMed]
- Hasenbring, M. Chronification of Disc-Related Pain: Risk Factors and Health-Promoting Behavior [Chronifizierung Bandscheibenbedingter Schmerzen: Risikofaktoren und Gesundheitsförderndes Verhalten]; Schattauer: Stuttgart, Germany, 1992. [Google Scholar]
- Niemier, K.; Schulz, J.; Emmerich, J.; Liefring, V.; Beyer, L. Chronic Muscular Skeletal Pain Syndromes, New Models for an Old Problem. Specific and Nonspecific Pain-Time to Move on. J. Orthop. Sports Med. 2020, 2, 42–54. [Google Scholar] [CrossRef]
- Tsai, P.-S.; Chen, P.-L.; Lai, Y.-L.; Lee, M.-B.; Lin, C.-C. Effects of electromyography biofeedback-assisted relaxation on pain in patients with advanced cancer in a palliative care unit. Cancer Nurs. 2007, 30, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Brugnoli, M.P.; Pesce, G.; Pasin, E.; Basile, M.F.; Tamburin, S.; Polati, E. The role of clinical hypnosis and self-hypnosis to relief pain and anxiety in severe chronic diseases in palliative care: A 2-year long-term follow-up of treatment in a nonrandomized clinical trial. Ann. Palliat. Med. 2018, 7, 17–31. [Google Scholar] [CrossRef] [PubMed]
- Loew, T.H. Breathe Slower, Live Better [Langsamer Atmen, Besser Leben]: Eine Anleitung zur Stressbewältigung; Psychosozial Verlag: Gießen, Germany, 2019; ISBN 9783837973693. [Google Scholar]
- Loew, T.; Leinberger, B. “Decelerated breathing”—Central psychosomatic offer in order therapy [“Entschleunigtes Atmen“—Zentrales psychosomatisches Angebot in der Ordnungstherapie]. Erfahrungsheilkunde 2019, 68, 67–72. [Google Scholar] [CrossRef]
- Rösel, S.; Burian, R. Working with cognitions, emotions and behavior in chronic pain therapy [Arbeit mit Kognitionen, Emotionen und Verhalten in der Therapie chronischer Schmerzen]. Man. Med. 2023, 61, 153–159. [Google Scholar] [CrossRef]
- Allmer, H. Recovery and Health—Basics, Results and Measures [Erholung und Gesundheit—Grundlagen, Ergebnisse und Maßnahmen]; Hogrefe: Göttingen, Germany, 1996. [Google Scholar]
- Wolfe, C.; Page, P.; Voight, M.; Norman, C.; Draovitch, P. The Deceleration Index—Is it the Missing Link in Rehabilitation? Int. J. Sports Phys. Ther. 2023, 18, 73799. [Google Scholar] [CrossRef]
- Husebø, S.; Mathis, G. What is palliative care? [Was ist Palliative Care?]. In Palliative Medicine: Co-Founded by E. Klaschik [Palliativmedizin: Mitbegründet von E. Klaschik]; Husebø, S., Mathis, G., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; pp. 1–9. ISBN 978-3-662-49039-6. [Google Scholar]
- Latimer, E.J.; Dawson, H.R. Palliative care: Principles and pracice. Section of Palliative Care, Ontario Medical Association. CMAJ 1993, 148, 933–936. [Google Scholar] [PubMed]
- Mounsey, L.; Ferres, M.; Eastman, P. Palliative care for the patient without cancer. Aust. J. Gen. Pract. 2018, 47, 765–769. [Google Scholar] [CrossRef] [PubMed]
- Wille, A.; Mühlenbrock, J.; Groß, M. Concepts of cooperation between the various professional groups [Konzepte der Zusammenarbeit der verschiedenen Berufsgruppen]. In Interdisciplinary Palliative Medicine [Interdisziplinäre Palliativmedizin]; Groß, M., Demmer, T., Eds.; Springer: Berlin/Heidelberg, Germany, 2021; pp. 63–71. ISBN 978-3-662-62011-3. [Google Scholar]
- Yerkes, R.M.; Dodson, J.D. The relation of strength of stimulus to rapidity of habit-formation. J. Comp. Neurol. Psychol. 1908, 18, 459–482. [Google Scholar] [CrossRef]
- Hatt, H.E. Kybernetik und Menschenbild: Freiheit und Verantwortung im Zeitalter der Denkmaschinen; Theologischer Verlag: Zürich, Switzerland, 1972; ISBN 3290113000. [Google Scholar]
- Bäuml, J. Psychoses—From the Schizophrenic Spectrum [Psychosen—Aus Dem Schizophrenen Formenkreis]; Springer: Dordrecht, The Netherlands, 2008; ISBN 978-3-540-43646-1. [Google Scholar]
- Roenn, J.H. von. Palliative care and the cancer patient: Current state and state of the art. J. Pediatr. Hematol. Oncol. 2011, 33 (Suppl. 2), S87–S89. [Google Scholar] [CrossRef]
- Knaus, C. The Total Pain Concept in the Scientific Literature—A Literature Review [Das Total Pain Konzept in der Wissenschaftlichen Literatur—Ein Literaturreview]. Bachelor’s Thesis, Medizinische Universität, Graz, Austria, 2020. [Google Scholar]
- Husebø, S. Psychosoziale Fragen. In Palliativmedizin; von E. Klaschik, M., Husebø, S., Mathis, G., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; pp. 349–416. ISBN 978-3-662-49039-6. [Google Scholar]
- Henningsen, P.; Zipfel, S.; Herzog, W. Management of functional somatic syndromes. Lancet 2007, 369, 946–955. [Google Scholar] [CrossRef]
- Glaser, W.R. Systems theory [Systemtheorie]. In Psychologie [Psychology]; Straub, J., Kempf, W., Werbik, H., Eds.; DTV: München, Germany, 1997. [Google Scholar]
- Timm, H. Transformation of the concepts and practice of total pain and total care: 30 years of Danish hospices. Front. Sociol. 2023, 8, 1145131. [Google Scholar] [CrossRef]
- Borrell-Carrió, F.; Suchman, A.L.; Epstein, R.M. The biopsychosocial model 25 years later: Principles, practice, and scientific inquiry. Ann. Fam. Med. 2004, 2, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Egger, J.W. Are there “psychosomatic” diseases? In Psychology in Medicine. Medical Psychology, Psychotherapy, Psychosomatics [Psychologie in der Medizin. Medizinische Psychologie, Psychotherapie, Psychosomatik]; Egger, J.W., Ed.; WUV: Wien, Austria, 1993; pp. 106–123. [Google Scholar]
- Egger, J.W. Body-mind unity theory: The expanded biopsychosocial model of illness—Toward a scientifically based holistic understanding of illness. Integr. Ther.—Z. Für Vgl. Psychother. Und Methodenintegration 2008, 33, 497–520. [Google Scholar]
- Egger, J.W. Biopsychosocial Medicine: The Theoretical Basis of Multidimensional Parallel Diagnosis and Therapy. Psychol. Med. 2012, 23, 45–49. [Google Scholar]
- Egger, J.W. Integrative Behavioral Therapy and Psychotherapeutic Medicine. A Biopsychosocial Model [Integrative Verhaltenstherapie und Psychotherapeutische Medizin. Ein Biopsychosoziales Modell]; Springer Fachmedien-Verl.: Wiesbaden, Germany, 2015; ISBN 978-3-658-06802-8. [Google Scholar]
- Ghaemi, S.N. The rise and fall of the biopsychosocial model. Br. J. Psychiatry 2009, 195, 3–4. [Google Scholar] [CrossRef]
- Ghaemi, S.N. The Biopsychosocial Model in Psychiatry: A Critique. Existenz 2011, 6, 1. [Google Scholar]
- Descartes, R. On the Human Being. (Translation of “L‘Homme” 1664, introduction by K. Rotschuh) [Über den Menschen. (Übersetzung von “L’Homme“ 1664, Einführung von K. Rotschuh)]; Lambert Schneider: Heidelberg, Germany, 1969. [Google Scholar]
- Chapman, R.C.; Wykoff, M. The problem of pain: A psychobiological perspective. In Psychosomatic Disorders; Haynes, S.N., Gannon, L., Eds.; Praeger: New York, NY, USA, 1981; pp. 32–78. [Google Scholar]
- Kapfhammer, H. Somatoform disorders [Somatoforme Störungen]. Nervenarzt 2007, 79, 99–117. [Google Scholar] [CrossRef]
- McLaren, N. A critical review of the biopsychosocial model. Aust. N. Z. J. Psychiatry 1998, 32, 86–92; discussion 93–96. [Google Scholar] [CrossRef]
- Berghaus, M. Luhmann Made Easy—An Introduction to Systems Theory [Luhmann Leicht Gemacht—Eine Einführung in Die Systemtheorie], 4., Überarbeitete und Ergänzte Auflage; Böhlau Verlag: Köln, Germany; Wien, Austria, 2022; ISBN 9783838557731. [Google Scholar]
- Watzke, H. Symptom control [Symptomkontrolle]. In Palliative Medicine: Co-Founded by E. Klaschik [Palliativmedizin: Mitbegründet von E. Klaschik]; Husebø, S., Mathis, G., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; pp. 215–255. ISBN 978-3-662-49039-6. [Google Scholar]
- Hearson, B.; Sawatzky, J.-A.V. Sleep disturbance in patients with advanced cancer. Int. J. Palliat. Nurs. 2008, 14, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Nabal, M.; Pascual, A.; Llombart, A. General evaluation of patients with advanced cancer. Principles of symtom control. Aten. Primaria 2006, 38, 21–28. [Google Scholar] [CrossRef]
- Chang, C.-H.; Boni-Saenz, A.A.; Durazo-Arvizu, R.A.; DesHarnais, S.; Lau, D.T.; Emanuel, L.L. A system for interactive assessment and management in palliative care. J. Pain Symptom Manag. 2007, 33, 745–755. [Google Scholar] [CrossRef]
- Falckenberg, M. Multiprofessional cooperation in palliative care. Anasthesiol. Intensivmed. Notfallmed. Schmerzther. 2007, 42, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Curtis Nickel, J.; Baranowski, A.P.; Pontari, M.; Berger, R.E.; Tripp, D.A. Management of men diagnosed with chronic prostatitis/chronic pelvic pain syndrome who have failed traditional management. Rev. Urol. 2007, 9, 63–72. [Google Scholar] [PubMed]
- Nicolis, G.; Prigogine, I.; Rebhan, E. Exploring the Complex. Towards a New Understanding of the Natural Sciences [Die Erforschung des Komplexen. Auf dem Weg zu Einem Neuen Verständnis der Naturwissenschaften]; Piper: München, Germany, 1987; ISBN 3492030750. [Google Scholar]
- Zimmermann, M. New concepts of pain and pain treatment [Neue Konzepte von Schmerz und Schmerzbehandlung]. In Theory of Medicine: Dialog between Basic Disciplines and Clinical Practice [Theorie der Medizin: Dialoge Zwischen Grundlagenfächern und Klinik]; Bauer, A., Ed.; Barth Verlag: Heidelberg, Germany; Leipzig, Germany, 1995; pp. 46–59. [Google Scholar]
- Feuerstein, M.; Papciak, A.S.; Hoon, P.E. Biobehavioral mechanisms of chronic low back pain. Clin. Psychol. Rev. 1987, 7, 243–273. [Google Scholar] [CrossRef]
- Wright, A.R.; Gatchel, R.J.; Wildenstein, L.; Riggs, R.; Buschang, P.; Ellis, E., III. Biopsychosocial differences between high-risk and low-risk patients with acute TMD-related pain. J. Am. Dent. Assoc. 2004, 135, 474–483. [Google Scholar] [CrossRef]
- Seemann, H.; Zimmermann, M. Regulatory model of pain from a system-theoretical perspective—An assessment of the situation [Regulationsmodell des Schmerzes aus systemtheoretischer Sicht—Eine Standortbestimmung]. In Psychological Pain Therapy: Basics—Diagnostics—Clinical Pictures—Treatment [Psychologische Schmerztherapie: Grundlagen Diagnostik Krankheitsbilder Behandlung]; Basler, H.-D., Franz, C., Kröner-Herwig, B., Rehfisch, H.P., Seemann, H., Eds.; Springer: Berlin/Heidelberg, Germany, 1996; pp. 23–57. ISBN 978-3-662-09591-1. [Google Scholar]
- Reindl, M.S. The Living Will [Die Patientenverfügung]; JBZ: Salzburg, Austria, 2012. [Google Scholar]
- Hochwarter, M. Wenn Kinder Sterben Müssen: Heranwachsende Kinder als Expertinnen und Experten Persönlicher Bedürfnisse in der Interaktion mit Pflegepersonen. Ph.D. Thesis, Universtiät Wien, Wien, Austria, 2011. [Google Scholar]
- Daneault, S.; Lussier, V.; Mongeau, S.; Hudon, E.; Paillé, P.; Dion, D.; Yelle, L. Primum non nocere: Could the health care system contribute to suffering? In-depth study from the perspective of terminally ill cancer patients. Can. Fam. Physician 2006, 52, 1574–1575. [Google Scholar]
- Sullivan, A.M.; Lakoma, M.D.; Billings, J.A.; Peters, A.S.; Block, S.D. Creating enduring change: Demonstrating the long-term impact of a faculty development program in palliative care. J. Gen. Intern. Med. 2006, 21, 907–914. [Google Scholar] [CrossRef]
- Whelton, B.J.B. Human nature: A foundation for palliative care. Nurs. Philos. 2008, 9, 77–88. [Google Scholar] [CrossRef]
- Hodiamont, F. Komplexität verstehen—Die Palliative Care Versorgungssituation als komplexes adaptives System. Ph.D. Thesis, Ludwig-Maximilians-Universität München, München, Germany, 2018. [Google Scholar]
- Malik, F. Self-organization in management [Selbstorganisation im Management]. In Basic Principles of Self-Organization [Grundprinzipien der Selbstorganisation]; Kratky, K.W., Wallner, F., Eds.; Wissenschaftliche Buchgesellschaft: Darmstadt, Germany, 1990; pp. 96–102. [Google Scholar]
- Bionity. Self-Organization [Selbstorganisation]. Available online: https://www.bionity.com/de/lexikon/Selbstorganisation.html (accessed on 10 July 2023).
- Barz, H. Psychopathology and Its Psychological Foundations [Psychopathologie und Ihre Psychologischen Grundlagen]; Huber: Bern, Switzerland, 1997. [Google Scholar]
- Luhmann, N. The Reality of the Mass Media. 376th Meeting on July 13, 1994 in Düsseldorf [Die Realität der Massenmedien. 376. Sitzung am 13. Juli 1994 in Düsseldorf]; Westdt. Verl.: Opladen, Germany, 1995; ISBN 978-3-531-07333-0. [Google Scholar]
- Wallner, F. Renouncing ultimate justification: Autopoiesis as a way out? [Verzicht auf Letztbegründung: Autopoiesis als Ausweg?]. In Basic Principles of Self-Organization [Grundprinzipien der Selbstorganisation]; Kratky, K.W., Wallner, F., Eds.; Wissenschaftliche Buchgesellschaft: Darmstadt, Germany, 1990; pp. 129–139. [Google Scholar]
- Rosen, R. Feedforwards and global system failure: A general mechanism for senescence. J. Theor. Biol. 1978, 74, 579–590. [Google Scholar] [CrossRef] [PubMed]
- Sittl, R.; Griessinger, N. Circadian rhythm in neuropathic tumor pain [Zirkadiane Rhythmik bei neuropathischen Tumorschmerzen]. Z. Fur Allg. 1995, 71, 206. [Google Scholar]
- Jonen-Thielemann, I. The terminal phase [Die Terminalphase]. In Textbook of Palliative Medicine [Lehrbuch der Palliativmedizin]; Aulbert, E., Zech, D., Eds.; Schattauer: Stuttgart, Germany; New York, NY, USA, 1997; pp. 678–686. [Google Scholar]
- Koesel, N.; Tocchi, C.; Burke, L.; Yap, T.; Harrison, A. Symptom Distress: Implementation of Palliative Care Guidelines to Improve Pain, Fatigue, and Anxiety in Patients with Advanced Cancer. Clin. J. Oncol. Nurs. 2019, 23, 149–155. [Google Scholar] [CrossRef]
- Mramor, K.M. Music therapy with persons who are indigent and terminally ill. J. Palliat. Care 2001, 17, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Falkensteiner, M.; Mantovan, F.; Müller, I.; Them, C. The use of massage therapy for reducing pain, anxiety, and depression in oncological palliative care patients: A narrative review of the literature. ISRN Nurs. 2011, 2011, 929868. [Google Scholar] [CrossRef]
- Jane, S.-W.; Wilkie, D.J.; Gallucci, B.B.; Beaton, R.D.; Huang, H.-Y. Effects of a full-body massage on pain intensity, anxiety, and physiological relaxation in Taiwanese patients with metastatic bone pain: A pilot study. J. Pain Symptom Manag. 2009, 37, 754–763. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brinkers, M.; Pfau, G.; Thielmann, B.; Böckelmann, I. Cybernetic Principles in Psychophysiology: Their Significance and Conclusions for Palliative Care. Healthcare 2024, 12, 1510. https://doi.org/10.3390/healthcare12151510
Brinkers M, Pfau G, Thielmann B, Böckelmann I. Cybernetic Principles in Psychophysiology: Their Significance and Conclusions for Palliative Care. Healthcare. 2024; 12(15):1510. https://doi.org/10.3390/healthcare12151510
Chicago/Turabian StyleBrinkers, Michael, Giselher Pfau, Beatrice Thielmann, and Irina Böckelmann. 2024. "Cybernetic Principles in Psychophysiology: Their Significance and Conclusions for Palliative Care" Healthcare 12, no. 15: 1510. https://doi.org/10.3390/healthcare12151510






