Investigating Physicians’ Adoption of Telemedicine in Romania Using Technology Acceptance Model (TAM)
Abstract
1. Introduction
2. Literature Review
2.1. Telemedicine in the Healthcare Sector
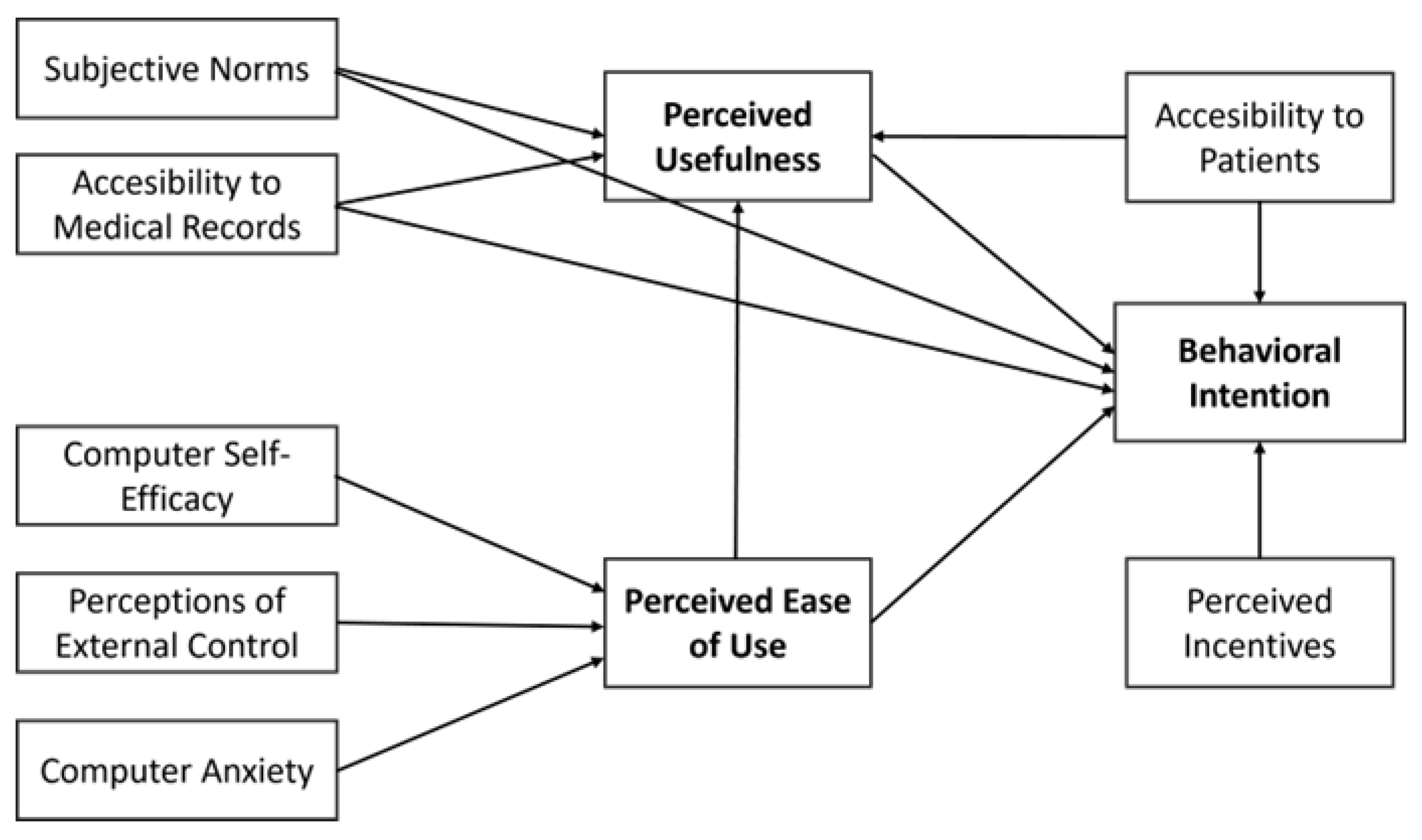
2.2. Technology Acceptance Model
2.3. Hypotheses Development
3. Materials and Methods
3.1. Data
3.2. Measurement
3.3. Method
4. Results
4.1. The Measurement (Outer) Model
4.2. The Inner Model
4.2.1. Predictors of Behavioral Intention
4.2.2. Predictors of Perceived Usefulness
4.2.3. Predictors of Perceived Ease of Use
5. Discussion
6. Limitations and Future Directions
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Estimated Coef. | Direct Effects | Indirect Effects | Total Effects | |||||
|---|---|---|---|---|---|---|---|---|
| Model | BI | PU | PEOU | BI | PU | BI | PU | PEOU |
| BI | - | - | - | - | - | - | - | |
| PU | 0.179 *** (p < 0.001) | - | - | - | 0.179 *** (p < 0.001) | - | - | |
| PEOU | 0.047 (p = 0.059) | 0.283 *** (p < 0.001) | 0.051 ** (p = 0.009) | - | 0.098 *** (p < 0.001) | 0.283 *** (p < 0.001) | - | |
| CSE | - | - | 0.280 *** (p < 0.001) | 0.013 (p = 0.268) | 0.079 *** (p < 0.001) | 0.027 (p = 0.100) | 0.079 *** (p < 0.001) | 0.280 *** (p < 0.001) |
| PEC | - | - | 0.613 *** (p < 0.001) | 0.029 (p = 0.088) | 0.173 *** (p < 0.001) | 0.060 ** (p = 0.002) | 0.173 *** (p < 0.001) | 0.613 *** (p < 0.001) |
| AMR | 0.209 *** (p < 0.001) | 0.255 *** (p < 0.001) | 0.046 * (p = 0.016) | 0.254 *** (p < 0.001) | 0.255 *** (p < 0.001) | |||
| AP | 0.252 *** (p < 0.001) | 0.142 *** (p < 0.001) | 0.025 (p = 0.117) | 0.278 *** (p < 0.001) | 0.142 *** (p < 0.001) | |||
| PI | 0.120 *** (p < 0.001) | - | 0.120 *** (p < 0.001) | |||||
| CANX | - | - | −0.078 ** (p = 0.005) | −0.004 (p = 0.432) | −0.022 (p = 0.151) | −0.008 (p = 0.361) | −0.022 (p = 0.151) | −0.078 ** (p = 0.005) |
| SN | 0.252 *** (p < 0.001) | 0.287 *** (p < 0.001) | 0.051 ** (p = 0.008) | 0.303 *** (p < 0.001) | 0.287 *** (p < 0.001) | |||
| Age | 0.007 (p = 0.406) | - | 0.007 (p = 0.406) | |||||
| Gender | −0.005 (p = 0.430) | - | −0.005 (p = 0.430) | |||||
| Telemed | 0.033 (p = 0.135) | 0.033 (p = 0.135) | ||||||
| R2/ Adjusted R2 | 84.6%/ 84.4% | 71.5%/ 71.4% | 72.7%/ 72.6% | |||||
| Tenehaus GoF | 0.821 (large) | |||||||
Appendix B
| Estimated Coef. | Direct Effects | Indirect Effects | Total Effects | |||||
|---|---|---|---|---|---|---|---|---|
| Model | BI | PU | PEOU | BI | PU | BI | PU | PEOU |
| BI | - | - | - | - | - | - | - | - |
| PU | 0.146 | - | - | - | - | 0.146 | - | - |
| PEOU | 0.035 | 0.211 | - | 0.038 | - | 0.073 | 0.211 | - |
| CSE | - | - | 0.198 | 0.008 | 0.043 | 0.017 | 0.043 | 0.198 |
| PEC | - | - | 0.505 | 0.021 | 0.125 | 0.044 | 0.125 | 0.505 |
| AMR | 0.168 | 0.191 | - | 0.037 | - | 0.204 | 0.191 | - |
| AP | 0.207 | 0.103 | - | 0.021 | - | 0.228 | 0.103 | - |
| PI | 0.073 | - | - | - | - | 0.073 | - | - |
| CANX | - | - | 0.024 | 0.001 | 0.003 | 0.002 | 0.003 | 0.024 |
| SN | 0.202 | 0.211 | - | 0.041 | - | 0.243 | 0.211 | - |
| Age | 0.000 | - | - | - | - | 0.000 | - | - |
| Gender | 0.000 | - | - | - | - | 0.000 | - | - |
| Telemed | 0.009 | - | - | - | - | 0.009 | - | - |
Appendix C
| Construct | Items | |
|---|---|---|
| Behavioral Intention | BI1. I have a positive intention to adopt the telemedicine service. BI2. I will care for my patients through telemedicine service. BI3. I will gain accurate patient information and treatment histories. BI4. I will provide telemedicine services and share the information through this service. | [51] |
| Perceived Usefulness | PU1. It will positively affect the treatment plan. PU2. It is possible to provide a more comprehensive care service. PU3. It is efficient for diagnosing patients and scheduling. PU4. I can precisely monitor the patient’s condition. | |
| Perceived Ease of Use | PEOU1. It is easy to use the device for telemedicine service. PEOU2. It is easy to learn how to use the new device for telemedicine. PEOU3. It is easy to perform my job by using the telemedicine service. | |
| Computer Self−Efficacy | I could complete the job using a software package. CSE1. if there was no one around to tell me what to do as I go. CSE2. if I had just the built−in help facility for assistance. CSE3. if someone showed me how to do it first. CSE4. if I had used similar packages before this one to do the same job | [33] |
| Perceptions of External Control | PEC1. I have control over using the system. PEC2. I have the resources necessary to use the system. PEC3. Given the resources. opportunities. and knowledge it takes to use the system. it would be easy for me to use the system. PEC4. The system is not compatible with other systems I use. | |
| Accessibility to Medical Records | AMR1. I can gather correct information about the patient. AMR2. I can easily record a patient’s health condition. AMR3. Because of the precise record of the patients. it enables me to provide proper healthcare service to my patients. | [51] |
| Accessibility to Patients | AP1. I am able to care for patients living at further distances. AP2. I am able to be in contact with patients who seldom come to the clinic. AP3. I am able to be in contact with patients who cannot be easily delivered to the clinic. | |
| Perceived Incentives | PI1. This service needs proper government policy and support. PI2. It needs monetary incentives. PI3. It would be meaningful. if financial support were given. | |
| Computer Anxiety | CANX1. Computers do not scare me at all. CANX2. Working with a computer makes me nervous. CANX3. Computers make me feel uncomfortable. CANX4. Computers make me feel uneasy. | [33] |
| Subjective Norms | SN1.People who influence my behavior think that I should use the system. SN2. People who are important to me think that I should use the system. SN3. The senior management of this business has been helpful in the use of the system. SN4. In general. the organization has supported the use of the system. |
Appendix D
| BI | PU | PEOU | CSE | PEC | AMR | AP | PI | CANX | SN | |
|---|---|---|---|---|---|---|---|---|---|---|
| BI1 | 0.950 | 0.008 | 0.042 | 0.017 | 0.011 | −0.169 | −0.037 | 0.020 | −0.007 | 0.019 |
| BI2 | 0.955 | −0.064 | 0.026 | 0.000 | 0.067 | −0.196 | 0.072 | −0.022 | 0.005 | 0.030 |
| BI3 | 0.892 | 0.043 | −0.110 | 0.040 | −0.089 | 0.469 | −0.150 | 0.039 | −0.010 | −0.056 |
| BI4 | 0.952 | 0.016 | 0.035 | −0.055 | 0.005 | −0.074 | 0.106 | −0.035 | 0.010 | 0.004 |
| PU1 | 0.044 | 0.927 | 0.129 | −0.009 | −0.086 | −0.049 | −0.009 | −0.005 | 0.006 | 0.003 |
| PU2 | 0.085 | 0.931 | −0.022 | 0.010 | −0.091 | −0.024 | −0.056 | −0.022 | −0.010 | −0.023 |
| PU3 | −0.130 | 0.881 | 0.024 | −0.019 | −0.012 | 0.065 | −0.060 | 0.081 | −0.002 | 0.045 |
| PU4 | −0.006 | 0.868 | −0.138 | 0.018 | 0.203 | 0.012 | 0.131 | −0.053 | 0.006 | −0.024 |
| PEOU1 | −0.084 | −0.190 | 0.931 | 0.008 | 0.079 | 0.048 | 0.009 | 0.002 | −0.012 | −0.008 |
| PEOU2 | −0.130 | −0.244 | 0.914 | 0.037 | 0.041 | −0.006 | 0.067 | 0.089 | −0.031 | −0.044 |
| PEOU3 | 0.242 | 0.491 | 0.814 | −0.050 | −0.136 | −0.047 | −0.086 | −0.102 | 0.048 | 0.060 |
| CSE1 | 0.034 | −0.174 | 0.427 | 0.753 | 0.330 | −0.140 | 0.037 | −0.133 | −0.045 | 0.063 |
| CSE2 | −0.029 | 0.007 | 0.134 | 0.888 | 0.027 | −0.083 | 0.061 | −0.046 | −0.016 | 0.020 |
| CSE3 | 0.047 | 0.027 | −0.204 | 0.869 | −0.172 | 0.112 | 0.002 | 0.058 | 0.037 | −0.078 |
| CSE4 | −0.051 | 0.124 | −0.324 | 0.815 | −0.151 | 0.100 | −0.102 | 0.111 | 0.020 | 0.003 |
| PEC1 | 0.012 | 0.094 | 0.067 | 0.045 | 0.926 | −0.010 | −0.027 | −0.010 | −0.006 | −0.004 |
| PEC2 | −0.005 | −0.053 | −0.149 | −0.059 | 0.937 | 0.007 | 0.024 | −0.023 | 0.035 | 0.012 |
| PEC3 | −0.006 | −0.040 | 0.083 | 0.014 | 0.940 | 0.004 | 0.003 | 0.033 | −0.029 | −0.009 |
| AMR1 | −0.010 | 0.012 | −0.044 | 0.041 | −0.037 | 0.934 | −0.075 | −0.005 | 0.030 | −0.036 |
| AMR2 | −0.073 | −0.134 | 0.072 | −0.012 | 0.075 | 0.938 | 0.067 | −0.010 | −0.036 | 0.036 |
| AMR3 | 0.084 | 0.123 | −0.028 | −0.028 | −0.039 | 0.935 | 0.007 | 0.016 | 0.006 | 0.000 |
| AP1 | 0.014 | 0.127 | −0.055 | 0.005 | −0.011 | 0.003 | 0.942 | −0.019 | 0.020 | 0.006 |
| AP2 | −0.035 | −0.064 | 0.026 | −0.006 | 0.000 | 0.031 | 0.968 | 0.005 | −0.015 | 0.021 |
| AP3 | 0.022 | −0.060 | 0.028 | 0.002 | 0.010 | −0.034 | 0.962 | 0.013 | −0.005 | −0.026 |
| PI1 | −0.105 | −0.243 | 0.227 | 0.057 | −0.017 | 0.015 | 0.086 | 0.804 | −0.067 | −0.047 |
| PI2 | −0.379 | 0.096 | −0.207 | −0.004 | 0.060 | 0.025 | 0.043 | 0.838 | 0.037 | 0.062 |
| PI3 | 0.480 | 0.137 | −0.011 | −0.050 | −0.044 | −0.039 | −0.126 | 0.837 | 0.027 | −0.017 |
| CANX2 | 0.037 | −0.020 | −0.050 | −0.029 | −0.017 | 0.006 | 0.012 | 0.000 | 0.905 | 0.037 |
| CANX3 | −0.029 | 0.005 | 0.041 | 0.011 | −0.005 | 0.000 | 0.012 | 0.025 | 0.939 | −0.024 |
| CANX4 | −0.007 | 0.014 | 0.007 | 0.016 | 0.021 | −0.005 | −0.023 | −0.025 | 0.947 | −0.012 |
| SN1 | −0.665 | 0.028 | −0.198 | 0.003 | 0.217 | 0.091 | 0.061 | 0.000 | 0.014 | 0.812 |
| SN2 | −0.478 | 0.042 | −0.072 | −0.054 | 0.128 | 0.129 | 0.040 | −0.005 | 0.010 | 0.879 |
| SN3 | 0.445 | −0.015 | 0.099 | 0.022 | −0.153 | −0.115 | −0.008 | 0.018 | 0.000 | 0.879 |
| SN4 | 0.653 | −0.053 | 0.158 | 0.029 | −0.176 | −0.100 | −0.089 | −0.013 | −0.023 | 0.871 |
References
- Wang, J.; Xu, Y. Digitalization, Income Inequality, and Public Health: Evidence from Developing Countries. Technol. Soc. 2023, 73, 102210. [Google Scholar] [CrossRef]
- Guzel, A.E.; Arslan, U.; Acaravci, A. The Impact of Economic, Social, and Political Globalization and Democracy on Life Expectancy in Low-Income Countries: Are Sustainable Development Goals Contradictory? Environ. Dev. Sustain. 2021, 23, 13508–13525. [Google Scholar] [CrossRef]
- Huang, S.; Zhou, T.; Xu, C.; Zheng, J. Does Public Health Influence Economic Performance? Investigating the Role of Governance and Greener Energies for the Case of China. Front. Public Health 2022, 10, 864736. [Google Scholar] [CrossRef]
- Paunov, C.; Planes-Satorra, S. What Future for Science, Technology and Innovation after COVID-19? OECD Science, Technology and Industry Policy Papers; OECD: Paris, France, 2021; Volume 107. [Google Scholar]
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for Global Emergencies: Implications for Coronavirus Disease 2019 (COVID-19). J. Telemed. Telecare 2020, 26, 309–313. [Google Scholar] [CrossRef]
- Golinelli, D.; Boetto, E.; Carullo, G.; Nuzzolese, A.G.; Landini, M.P.; Fantini, M.P. Adoption of Digital Technologies in Health Care During the COVID-19 Pandemic: Systematic Review of Early Scientific Literature. J. Med. Internet Res. 2020, 22, e22280. [Google Scholar] [CrossRef]
- How Digital Transformation in Healthcare Improves Efficiency and Patient Care. 2021. Available online: https://sidebench.com/digital-transformation-healthcare-improves-efficiency-patient-care/ (accessed on 12 June 2024).
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef]
- Gjellebæk, C.; Svensson, A.; Bjørkquist, C.; Fladeby, N.; Grundén, K. Management Challenges for Future Digitalization of Healthcare Services. Futures 2020, 124, 102636. [Google Scholar] [CrossRef]
- CVSHealth. 2022 Health Care Insights Study. Available online: https://www.cvshealth.com/content/dam/enterprise/cvs-enterprise/pdfs/cvs-health-care-insights-study-2022-report-executive-summary.pdf (accessed on 12 June 2024).
- Hyder, M.A.; Razzak, J. Telemedicine in the United States: An Introduction for Students and Residents. J. Med. Internet Res. 2020, 22, e20839. [Google Scholar] [CrossRef]
- Omboni, S.; Padwal, R.S.; Alessa, T.; Benczúr, B.; Green, B.B.; Hubbard, I.; Kario, K.; Khan, N.A.; Konradi, A.; Logan, A.G.; et al. The Worldwide Impact of Telemedicine during COVID-19: Current Evidence and Recommendations for the Future. Connect. Health 2022, 1, 7. [Google Scholar] [CrossRef]
- Li, J. Telemedicine and Telehealth in 2023 and beyond: From Leveling Out to Leveling Up. 2022. Available online: https://www.forbes.com/sites/forbestechcouncil/2022/12/27/telemedicine-and-telehealth-in-2023-and-beyond-from-leveling-out-to-leveling-up/ (accessed on 12 June 2024).
- Barbosa, W.; Zhou, K.; Waddell, E.; Myers, T.; Dorsey, E.R. Improving Access to Care: Telemedicine Across Medical Domains. Annu. Rev. Public Health 2021, 42, 463–481. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for Healthcare: Capabilities, Features, Barriers, and Applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef]
- Atmojo, J.T.; Sudaryanto, W.T.; Widiyanto, A.; Ernawati; Arradini, D. Telemedicine, Cost Effectiveness, and Patients Satisfaction: A Systematic Review. J. Health Policy Manag. 2020, 5, 103–107. [Google Scholar] [CrossRef]
- Lasslo, J.A.; Anthony, K.E.; Reif, C.E.; Bell, N.H. Overcoming Health Disparities. In Health Professionals’ Education in the Age of Clinical Information Systems, Mobile Computing and Social Networks; Elsevier: London, UK, 2017; pp. 35–62. ISBN 978-0-12-805362-1. [Google Scholar]
- Williams, R.M. The Costs of Visits to Emergency Departments. N. Engl. J. Med. 1996, 334, 642–646. [Google Scholar] [CrossRef]
- Tapia, A.D.; Howard, J.T.; Bebo, N.L.; Pfaff, J.A.; Chin, E.J.; Trueblood, W.A.; April, M.D.; Long, B.J.; Long, A.N.; Fernandez, W.G.; et al. A Retrospective Review of Emergency Department Visits That May Be Appropriate for Management in Non-Emergency Settings. Mil. Med. 2022, 187, e1153–e1159. [Google Scholar] [CrossRef]
- Hazarika, I. Artificial Intelligence: Opportunities and Implications for the Health Workforce. Int. Health 2020, 12, 241–245. [Google Scholar] [CrossRef]
- Ramanauskas, B. Better and Cheaper Public Services 2018. Available online: https://d3n8a8pro7vhmx.cloudfront.net/taxpayersalliance/pages/9468/attachments/original/1529499259/Automation_Paper_1.pdf?1529499259 (accessed on 10 June 2024).
- Batko, K.; Ślęzak, A. The Use of Big Data Analytics in Healthcare. J. Big Data 2022, 9, 3. [Google Scholar] [CrossRef]
- Koff, D.A.; Doyle, T.E. Imaging Informatics. In Encyclopedia of Biomedical Engineering; Elsevier: Amsterdam, The Netherlands, 2019; pp. 551–560. ISBN 978-0-12-805144-3. [Google Scholar]
- Hasselberg, M.J. The Digital Revolution in Behavioral Health. J. Am. Psychiatr. Nurses Assoc. 2020, 26, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Robeznieks, A. Which Medical Specialties Use Telemedicine the Most? 2019. Available online: https://www.ama-assn.org/practice-management/digital/which-medical-specialties-use-telemedicine-most (accessed on 30 May 2024).
- Scîntee, S.G.; Vlădescu, C. Implementation of Telemedicine in Romania. European Observatory of Health Systems and Policies. 30 September 2022. Available online: https://eurohealthobservatory.who.int/monitors/health-systems-monitor/updates/hspm/romania-2016/implementation-of-telemedicine-in-romania (accessed on 12 June 2024).
- Market Data Forecast Telemedicine Market. Market Data Forecast. 2023. Available online: https://www.marketdataforecast.com/market-reports/telemedicine-market (accessed on 4 May 2024).
- Observatoire Cetelem. Contactless Solutions Are Taking Hold Of Our Lives: Telemedicine 2021. Available online: https://observatoirecetelem.com/en/lobservatoire-cetelem-de-la-consommation/contactless-solutions-are-taking-hold-of-our-lives/telemedicine (accessed on 12 June 2024).
- Bagchi, A.D. Telemedicine Delivery for Urban Seniors with Low Computer Literacy: A Pilot Study. Online J. Nurs. Inform. 2018, 22, 1–7. [Google Scholar]
- Florea, M.; Lazea, C.; Gaga, R.; Sur, G.; Lotrean, L.; Puia, A.; Stanescu, A.M.A.; Lupsor-Platon, M.; Florea, H.; Sur, M.L. Lights and Shadows of the Perception of the Use of Telemedicine by Romanian Family Doctors During the COVID-19 Pandemic. IJGM 2021, 14, 1575–1587. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319. [Google Scholar] [CrossRef]
- Help University, Malaysia; Lai, P. The Literature Review of Technology Adoption Models and Theories for the Novelty Technology. JISTEM 2017, 14, 21–38. [Google Scholar] [CrossRef]
- Venkatesh, V.; Bala, H. Technology Acceptance Model 3 and a Research Agenda on Interventions. Decis. Sci. 2008, 39, 273–315. [Google Scholar] [CrossRef]
- Venkatesh, V.; Davis, F.D. A Theoretical Extension of the Technology Acceptance Model: Four Longitudinal Field Studies. Manag. Sci. 2000, 46, 186–204. [Google Scholar] [CrossRef]
- Venkatesh, V. Determinants of Perceived Ease of Use: Integrating Control, Intrinsic Motivation, and Emotion into the Technology Acceptance Model. Inf. Syst. Res. 2000, 11, 342–365. [Google Scholar] [CrossRef]
- Chen, S.-C.; Li, S.-H.; Li, C.-Y. Recent related research in technology acceptance model: A literature review. AJBMR 2012, 1, 124–127. [Google Scholar] [CrossRef]
- Elshafey, A.; Saar, C.C.; Aminudin, E.B.; Gheisari, M.; Usmani, A. Technology Acceptance Model for Augmented Reality and Building Information Modeling Integration in the Construction Industry. ITcon 2020, 25, 161–172. [Google Scholar] [CrossRef]
- Musyaffi, A.M.; Mulyani, S.; Suraida, I.; Sukmadilaga, C. Lack of readiness of digital banking channel acceptance: Study on TAM 3 and technology readiness. Acad. Strateg. Manag. J. 2021, 20, 1–18. [Google Scholar]
- Barabadi, S.A.; Shams, A.; Wise, N. Social Network Sites Impact on Learning: Extending the TAM3 Model to Assess Academic Performance in Higher Education. JAST 2022, 24, 1073–1086. [Google Scholar]
- Mayasari, R.; Febriantoko, J.; Putra, R.R.; Hadiwijaya, H.; Kurniawan, D. Analysis of Behavioral Intention Towards the Use of Smart Village Ogan Ilir (SVOI) Using Technology Acceptance Model (TAM) 3 Method. In Proceedings of the International Conference of Economics, Business, and Entrepreneur (ICEBE 2022), Palembang, Indonesia, 26 October 2022; Nairobi, Yuliansyah, Jimad, H., Perdana, R., Putrawan, G.E., Septiawan, T.Y., Eds.; Advances in Economics, Business and Management Research. Atlantis Press SARL: Paris, France, 2023; Volume 241, pp. 545–553, ISBN 978-2-38476-063-3. [Google Scholar]
- Salimon, M.G.; Kareem, O.; Mokhtar, S.S.M.; Aliyu, O.A.; Bamgbade, J.A.; Adeleke, A.Q. Malaysian SMEs M-Commerce Adoption: TAM 3, UTAUT 2 and TOE Approach. JSTPM 2023, 14, 98–126. [Google Scholar] [CrossRef]
- Ebnehoseini, Z.; Tara, M.; Tabesh, H.; Dindar, F.; Hasibian, S. Understanding Key Factors Affecting on Hospital Electronic Health Record (EHR) Adoption. J. Fam. Med. Prim. Care 2020, 9, 4348. [Google Scholar] [CrossRef]
- Klaic, M.; Galea, M.P. Using the Technology Acceptance Model to Identify Factors That Predict Likelihood to Adopt Tele-Neurorehabilitation. Front. Neurol. 2020, 11, 580832. [Google Scholar] [CrossRef] [PubMed]
- Barzegari, S.; Arpaci, I.; Marznaki, Z.H. Determining Factors Affecting Nurses’ Acceptance of a Hospital Information System Using a Modified Technology Acceptance Model 3. In International Conference on Information Systems and Intelligent Applications; Al-Emran, M., Al-Sharafi, M.A., Shaalan, K., Eds.; Lecture Notes in Networks and Systems; Springer International Publishing: Cham, Switzerland, 2023; Volume 550, pp. 449–456. ISBN 978-3-031-16864-2. [Google Scholar]
- Yazdanpanahi, F.; Shahi, M.; Vossoughi, M. Investigating the Effective Factors on the Acceptance of Teleorthodontic Technology Based on the Technology Acceptance Model 3 (TAM3). J. Dent. 2024, 25. [Google Scholar] [CrossRef]
- Holden, R.J.; Karsh, B.-T. The Technology Acceptance Model: Its Past and Its Future in Health Care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef] [PubMed]
- AlQudah, A.A.; Al-Emran, M.; Shaalan, K. Technology Acceptance in Healthcare: A Systematic Review. Appl. Sci. 2021, 11, 10537. [Google Scholar] [CrossRef]
- Rahimi, B.; Nadri, H.; Lotfnezhad Afshar, H.; Timpka, T. A Systematic Review of the Technology Acceptance Model in Health Informatics. Appl. Clin. Inf. 2018, 9, 604–634. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Chen, Q.; Kitkuakul, S. Regulatory Focus and Technology Acceptance: Perceived Ease of Use and Usefulness as Efficacy. Cogent Bus. Manag. 2018, 5, 1459006. [Google Scholar] [CrossRef]
- Martínez, A.; Everss, E.; Rojo-Álvarez, J.L.; Figal, D.P.; García-Alberola, A. A Systematic Review of the Literature on Home Monitoring for Patients with Heart Failure. J. Telemed. Telecare 2006, 12, 234–241. [Google Scholar] [CrossRef]
- Rho, M.J.; Choi, I.Y.; Lee, J. Predictive Factors of Telemedicine Service Acceptance and Behavioral Intention of Physicians. Int. J. Med. Inform. 2014, 83, 559–571. [Google Scholar] [CrossRef] [PubMed]
- Whitten, P.; Doolittle, G.; Mackert, M. Providers’ Acceptance of Telehospice. J. Palliat. Med. 2005, 8, 730–735. [Google Scholar] [CrossRef]
- Gagnon, M.P.; Orruño, E.; Asua, J.; Abdeljelil, A.B.; Emparanza, J. Using a Modified Technology Acceptance Model to Evaluate Healthcare Professionals’ Adoption of a New Telemonitoring System. Telemed. E-Health 2012, 18, 54–59. [Google Scholar] [CrossRef]
- Kowitlawakul, Y. The Technology Acceptance Model: Predicting Nurses’ Intention to Use Telemedicine Technology (eICU). CIN Comput. Inform. Nurs. 2011, 29, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Molfenter, T.; Roget, N.; Chaple, M.; Behlman, S.; Cody, O.; Hartzler, B.; Johnson, E.; Nichols, M.; Stilen, P.; Becker, S. Use of Telehealth in Substance Use Disorder Services During and After COVID-19: Online Survey Study. JMIR Ment. Health 2021, 8, e25835. [Google Scholar] [CrossRef] [PubMed]
- Croteau, A.-M.; Vieru, D. Telemedicine Adoption by Different Groups of Physicians. In Proceedings of the 35th Annual Hawaii International Conference on System Sciences, Big Island, HI, USA, 10 January 2002; pp. 1985–1993. [Google Scholar]
- Cilliers, L.; Flowerday, S. User Acceptance of Telemedicine by Health Care Workers A Case of the Eastern Cape Province, South Africa. Electron. J. Inf. Syst. Dev. Ctries. 2014, 65, 1–10. [Google Scholar] [CrossRef]
- Mohammed, R.; Elmajid, E.A.; Amine, H.; Khadija, C. Acceptance Factors of Telemedicine Technology during COVID-19 Pandemic among Health Professionals: A Qualitative Study. Healthc. Technol. Lett. 2023, 10, 23–33. [Google Scholar] [CrossRef]
- Olver, I.N.; Selva-Nayagam, S. Evaluation of a Telemedicine Link Between Darwin and Adelaide to Facilitate Cancer Management. Telemed. J. 2000, 6, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Achim, N.; Kassim, A.A. Computer Usage: The Impact of Computer Anxiety and Computer Self-Efficacy. Procedia Soc. Behav. Sci. 2015, 172, 701–708. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425. [Google Scholar] [CrossRef]
- Korkut Altuna, O.; Arslan, F.M. Impact of the Number of Scale Points on Data Characteristics and Respondents’ Evaluations: An Experimental Design Approach Using 5-Point and 7-Point Likert-Type Scales. İstanbul Üniversitesi Siyasal Bilgiler Fakültesi Derg. 2016. [Google Scholar] [CrossRef]
- Finstad, K. Response Interpolation and Scale Sensitivity: Evidence Against 5-Point Scales. J. Usability Stud. 2010, 5, 104–110. [Google Scholar]
- Jöreskog, K.G.; Wold, H.O.A. (Eds.) Systems under Indirect Observation: Causality, Structure, Prediction; Contributions to economic analysis; North-Holland: Amsterdam, The Netherlands; Sole distributors for the U.S.A. and Canada: New York, NY, USA; Elsevier Science Publishers: New York, NY, USA, 1982; ISBN 978-0-444-86301-0. [Google Scholar]
- Ioniță, A.; Rădoi, M.F.; Gusicov, D.M.; Anca, M. Activitatea Rețelei Sanitare Și de Ocrotire a Sănătății 2023. Available online: https://insse.ro/cms/ro/content/activitatea-re%C8%9Belei-sanitare-%C8%99i-de-ocrotire-s%C4%83n%C4%83t%C4%83%C8%9Bii-%C3%AEn-anul-2023 (accessed on 12 June 2024).
- lege5.ro. ANEXA Nr II | Lege 153/2017. 2023. Available online: https://lege5.ro/Gratuit/ge3dkmzyga3a/anexa-nr-ii-lege-153-2017?dp=giydanzzga3dmny (accessed on 13 June 2024).
- Shrestha, N. Factor Analysis as a Tool for Survey Analysis. AJAMS 2021, 9, 4–11. [Google Scholar] [CrossRef]
- Cortina, J.M. What Is Coefficient Alpha? An Examination of Theory and Applications. J. Appl. Psychol. 1993, 78, 98–104. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Kennedy, P. A Guide to Econometrics, 6th ed.; Blackwell Pub: Malden, MA, USA, 2008; ISBN 978-1-4051-8258-4. [Google Scholar]
- Rönkkö, M.; Cho, E. An Updated Guideline for Assessing Discriminant Validity. Organ. Res. Methods 2022, 25, 6–14. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sinkovics, R.R. The Use of Partial Least Squares Path Modeling in International Marketing. In Advances in International Marketing; Sinkovics, R.R., Ghauri, P.N., Eds.; Emerald Group Publishing Limited: Bingley, UK, 2009; Volume 20, pp. 277–319. ISBN 978-1-84855-468-9. [Google Scholar]
- Hair, J.F. (Ed.) Multivariate Data Analysis, 7th ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2010; ISBN 978-0-13-813263-7. [Google Scholar]
- Hair, J.F.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M.; Danks, N.P.; Ray, S. Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R: A Workbook; Classroom Companion: Business; Springer International Publishing: Cham, Switzerland, 2021; ISBN 978-3-030-80518-0. [Google Scholar]
- Kock, N.; Lynn, G. Lateral Collinearity and Misleading Results in Variance-Based SEM: An Illustration and Recommendations. JAIS 2012, 13, 546–580. [Google Scholar] [CrossRef]
- Kock, N. WarpPLS User Manual: Version 8.0. Laredo. 2023. Available online: https://scriptwarp.com/warppls/UserManual_v_8_0.pdf (accessed on 24 April 2023).
- Kock, N. Common Structural Variation Reduction in PLS-SEM: Replacement Analytic Composites and the One Fourth Rule. Data Anal. Perspect. J. 2021, 2, 1–6. [Google Scholar]
- Zin, K.S.L.T.; Kim, S.; Kim, H.-S.; Feyissa, I.F. A Study on Technology Acceptance of Digital Healthcare among Older Korean Adults Using Extended Tam (Extended Technology Acceptance Model). Adm. Sci. 2023, 13, 42. [Google Scholar] [CrossRef]
- Kohnke, A.; Cole, M.L.; Bush, R. Incorporating UTAUT Predictors for Understanding Home Care Patients’ and Clinician’s Acceptance of Healthcare Telemedicine Equipment. J. Technol. Manag. Innov. 2014, 9, 29–41. [Google Scholar] [CrossRef]
- Ruiz Morilla, M.D.; Sans, M.; Casasa, A.; Giménez, N. Implementing Technology in Healthcare: Insights from Physicians. BMC Med. Inf. Decis. Mak. 2017, 17, 92. [Google Scholar] [CrossRef] [PubMed]
- Ly, B.A.; Kristjansson, E.; Labonté, R.; Bourgeault, I.L. Determinants of the Intention of Senegal’s Physicians to Use Telemedicine in Their Professional Activities. Telemed. E-Health 2018, 24, 897–898. [Google Scholar] [CrossRef] [PubMed]
- Conner, M.; Armitage, C.J. Extending the Theory of Planned Behavior: A Review and Avenues for Further Research. J. Appl. Soc. Pyschol. 1998, 28, 1429–1464. [Google Scholar] [CrossRef]
- Garavand, A.; Samadbeik, M.; Nadri, H.; Rahimi, B.; Asadi, H. Effective Factors in Adoption of Mobile Health Applications between Medical Sciences Students Using the UTAUT Model. Methods Inf. Med. 2019, 58, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.; Bancilhon, J.-M.; Jones, M. South African Physicians’ Acceptance of e-Prescribing Technology: An Empirical Test of a Modified UTAUT Model. SACJ 2013, 50, 43–54. [Google Scholar] [CrossRef]
- Lee, C.; Wan, G. Including Subjective Norm and Technology Trust in the Technology Acceptance Model: A Case of e-Ticketing in China. SIGMIS Database 2010, 41, 40–51. [Google Scholar] [CrossRef]
- Hofstede Insights. Country Comparison Tool 2023. Available online: https://www.hofstede-insights.com/country-comparison-tool (accessed on 30 May 2024).
- Hofstede, G.; Hofstede, G.J.; Minkov, M. Cultures and Organizations: Software of the Mind: Intercultural Cooperation and Its Importance for Survival; Revised and expanded third edition; McGraw-Hill: New York, NY, USA, 2010; ISBN 978-0-07-177015-6. [Google Scholar]
- European Observatory on Health Systems and Policies State of Health in the EU: Romania; The European Commission: Brussels, Belgium, 2017.
- Alhur, A. An Exploration of Nurses’ Perceptions of the Usefulness and Easiness of Using EMRs. J. Public Health Sci. 2023, 2, 20–31. [Google Scholar] [CrossRef]
- CNAS Ce Este Dosarul Electronic de Sănatate? 2023. Available online: http://www.des-cnas.ro/pub/ (accessed on 12 June 2024).
- Constitutional Court of Romania. Decizia Nr.498 Din 17 Iulie 2018 Referitoare La Excepția de Neconstituționalitate a Dispozițiilor Art.30 Alin.(2) Și (3), Precum Și a Sintagmei “sistemul Dosarului Electronic de Sănătate al Pacientului” Din Cuprinsul Art.280 Alin.(2) Din Legea Nr.95/2006. 2018. Available online: https://legislatie.just.ro/Public/DetaliiDocumentAfis/203149 (accessed on 13 June 2024).
- Șomănescu, C. Dosarul Electronic de Sănătate, Un Şir Lung de Rateuri la Doi Ani Şi Jumătate de Când e Obligatoriu. Economica.net. 2019. Available online: https://www.economica.net/dosar-electronic-de-sanatate-al-pacietului-probleme-si-beneficii_168361.html (accessed on 12 June 2024).
- CNAS COMUNICAT. Dosarul Electronic de Sănătate a Redevenit Funcțional. CNAS. 2021. Available online: https://cnas.ro/2021/12/22/comunicat-dosarul-electronic-de-sanatate-a-redevenit-functional/ (accessed on 12 June 2024).
- Borcea, Ș. Dosarul Electronic al Pacientului, Un Instrument Util, Dar Ignorat de Spitale. Ce Spun Autoritățile. adevarul.ro. 26 November 2022. Available online: https://adevarul.ro/stiri-interne/societate/dosarul-electronic-al-pacientului-un-instrument-2223162.html (accessed on 12 June 2024).
- European Commission. Commission Staff Working Document: 2023 Country Report—Romania; European Commission: Brussels, Belgium, 2023. [Google Scholar]
- Ajzen, I. From Intentions to Actions: A Theory of Planned Behavior. In Action Control; Kuhl, J., Beckmann, J., Eds.; Springer: Berlin/Heidelberg, Germany, 1985; pp. 11–39. ISBN 978-3-642-69748-7. [Google Scholar]
- Nov, O.; Ye, C. Resistance to Change and the Adoption of Digital Libraries: An Integrative Model. J. Am. Soc. Inf. Sci. 2009, 60, 1702–1708. [Google Scholar] [CrossRef]
- Adenuga, K.I.; Iahad, N.A.; Miskon, S. Towards Reinforcing Telemedicine Adoption amongst Clinicians in Nigeria. Int. J. Med. Inform. 2017, 104, 84–96. [Google Scholar] [CrossRef] [PubMed]
- Glaser, J. Financial Incentives for Healthcare IT Adoption. Healthc. Financ. Manag. 2007, 61, 118–120. [Google Scholar]
- Chaix-Couturier, C.; Durand-Zaleski, I.; Jolly, D.; Durieux, P. Effects of Financial Incentives on Medical Practice: Results from a Systematic Review of the Literature and Methodological Issues. Int. J. Qual. Health Care 2000, 12, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Gagnon, M.-P.; Desmartis, M.; Labrecque, M.; Car, J.; Pagliari, C.; Pluye, P.; Frémont, P.; Gagnon, J.; Tremblay, N.; Légaré, F. Systematic Review of Factors Influencing the Adoption of Information and Communication Technologies by Healthcare Professionals. J. Med. Syst. 2012, 36, 241–277. [Google Scholar] [CrossRef]
- Iftimoaei, C. Aspecte Sociodemografice Privind Calitatea Vieții În Mediul Rural. In Provocări Rurale Contemporane. Studii de Agro-economie și Antropologie Rurală; Presa Universitară Clujeană: Cluj-Napoca, Romania, 2021; pp. 39–55. ISBN 978-606-37-1280-7. [Google Scholar]
- Lee, H.Y.; Kanthawala, S.; Choi, E.Y.; Kim, Y.S. Rural and Non-Rural Digital Divide Persists in Older Adults: Internet Access, Usage, and Attitudes toward Technology. Gerontechnology 2021, 20, 1–9. [Google Scholar] [CrossRef]
- MINISTERUL SĂNĂTĂȚII. 131 de Spitale Dotate Cu Sistem de Telemedicină Pentru Serviciul de Urgență. 2023. Available online: https://www.ms.ro/ro/centrul-de-presa/131-de-spitale-dotate-cu-sistem-de-telemedicin%C4%83-pentru-serviciul-de-urgen%C8%9B%C4%83/ (accessed on 19 May 2024).
| Participants in Current Study N = 1093 (%) | |
|---|---|
| Sex | |
| Male | 334 (30.6%) |
| Female | 759 (69.4%) |
| Age | |
| 18–29 years old | 14 (1.3%) |
| 30–39 years old | 311 (28.5%) |
| 40–49 years old | 365 (33.4%) |
| 50–59 years old | 274 (25.1%) |
| 60–69 years old | 119 (10.9%) |
| 70–79 years old | 10 (0.9%) |
| Over 80 years old | None |
| Provenience | |
| Rural | 113 (10.3%) |
| Urban | 980 (89.7%) |
| Education | |
| Medical school | 161 (14.7%) |
| Medical Residency | 343 (31.4%) |
| Ph.D. in medicine | 285 (26.1%) |
| Post-university studies | 282 (25.8%) |
| Income | |
| Under RON 4000 (EUR 806) | 2 (0.2%) |
| RON 4000–6000 (EUR 807–1208 euro) | 48 (4.4%) |
| RON 6001–8000 (EUR 1209–1610) | 100 (9.1%) |
| RON 8001–10,000 (EUR 1611–2013) | 172 (15.7%) |
| RON 10,001–12,000 (EUR 2014–2416) | 234 (21.4%) |
| RON 12,001–14,000 (EUR 2417–2819) | 161 (14.7%) |
| RON 14,001–16,000 (EUR 2820–3221) | 149 (13.6%) |
| Above RON 16,000 (EUR 3221) | 212 (19.4%) |
| Refuse to answer | 15 (1.4%) |
| Specialization | |
| Resident physician | 21 (1.9%) |
| Specialist physician | 315 (28.8%) |
| Primary care physician | 622 (56.9%) |
| Doctor in medical sciences | 135 (12.4%) |
| Variable | Composite Reliability | Cronbach’s Alpha | Average Variance Extracted (AVE) |
|---|---|---|---|
| Behavioral Intention | 0.967 | 0.954 | 0.879 |
| Perceived Usefulness | 0.946 | 0.923 | 0.814 |
| Perceived Ease of Use | 0.918 | 0.864 | 0.788 |
| Computer Self-Efficacy | 0.900 | 0.851 | 0.694 |
| Perceptions of External Control | 0.954 | 0.927 | 0.873 |
| Accessibility of Medical Records | 0.955 | 0.929 | 0.875 |
| Accessibility of Patients | 0.971 | 0.955 | 0.917 |
| Perceived Incentives | 0.866 | 0.768 | 0.683 |
| Computer Anxiety | 0.951 | 0.922 | 0.865 |
| Subjective Norms | 0.920 | 0.883 | 0.741 |
| BI | PU | PEOU | CSE | PEC | AMR | AP | PI | CANX | SN | |
|---|---|---|---|---|---|---|---|---|---|---|
| BI | 0.937 | 0.802 | 0.745 | 0.614 | 0.729 | 0.802 | 0.819 | 0.600 | −0.229 | 0.780 |
| PU | 0.802 | 0.902 | 0.739 | 0.547 | 0.721 | 0.750 | 0.716 | 0.481 | −0.158 | 0.729 |
| PEOU | 0.745 | 0.739 | 0.888 | 0.703 | 0.814 | 0.695 | 0.720 | 0.517 | −0.283 | 0.629 |
| CSE | 0.614 | 0.547 | 0.703 | 0.833 | 0.637 | 0.555 | 0.601 | 0.469 | −0.188 | 0.548 |
| PEC | 0.729 | 0.721 | 0.814 | 0.637 | 0.934 | 0.724 | 0.702 | 0.480 | −0.286 | 0.617 |
| AMR | 0.802 | 0.750 | 0.695 | 0.555 | 0.724 | 0.935 | 0.726 | 0.489 | −0.204 | 0.676 |
| AP | 0.819 | 0.716 | 0.720 | 0.601 | 0.702 | 0.726 | 0.958 | 0.533 | −0.255 | 0.660 |
| PI | 0.600 | 0.481 | 0.517 | 0.469 | 0.480 | 0.489 | 0.533 | 0.827 | −0.177 | 0.484 |
| CANX | −0.229 | −0.158 | −0.283 | −0.188 | −0.286 | −0.204 | −0.225 | −0.177 | 0.930 | −0.108 |
| SN | 0.780 | 0.729 | 0.629 | 0.548 | 0.617 | 0.676 | 0.660 | 0.484 | −0.108 | 0.861 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bîlbîie, A.; Puiu, A.-I.; Mihăilă, V.; Burcea, M. Investigating Physicians’ Adoption of Telemedicine in Romania Using Technology Acceptance Model (TAM). Healthcare 2024, 12, 1531. https://doi.org/10.3390/healthcare12151531
Bîlbîie A, Puiu A-I, Mihăilă V, Burcea M. Investigating Physicians’ Adoption of Telemedicine in Romania Using Technology Acceptance Model (TAM). Healthcare. 2024; 12(15):1531. https://doi.org/10.3390/healthcare12151531
Chicago/Turabian StyleBîlbîie, Abigaela, Andreea-Ionela Puiu, Viorel Mihăilă, and Marin Burcea. 2024. "Investigating Physicians’ Adoption of Telemedicine in Romania Using Technology Acceptance Model (TAM)" Healthcare 12, no. 15: 1531. https://doi.org/10.3390/healthcare12151531
APA StyleBîlbîie, A., Puiu, A.-I., Mihăilă, V., & Burcea, M. (2024). Investigating Physicians’ Adoption of Telemedicine in Romania Using Technology Acceptance Model (TAM). Healthcare, 12(15), 1531. https://doi.org/10.3390/healthcare12151531









