The Methodological Quality of Studies on Physical Exercise in Adolescents with Cerebral Palsy: A Scoping Review of Systematic Reviews and Meta-Analyses
Abstract
1. Introduction
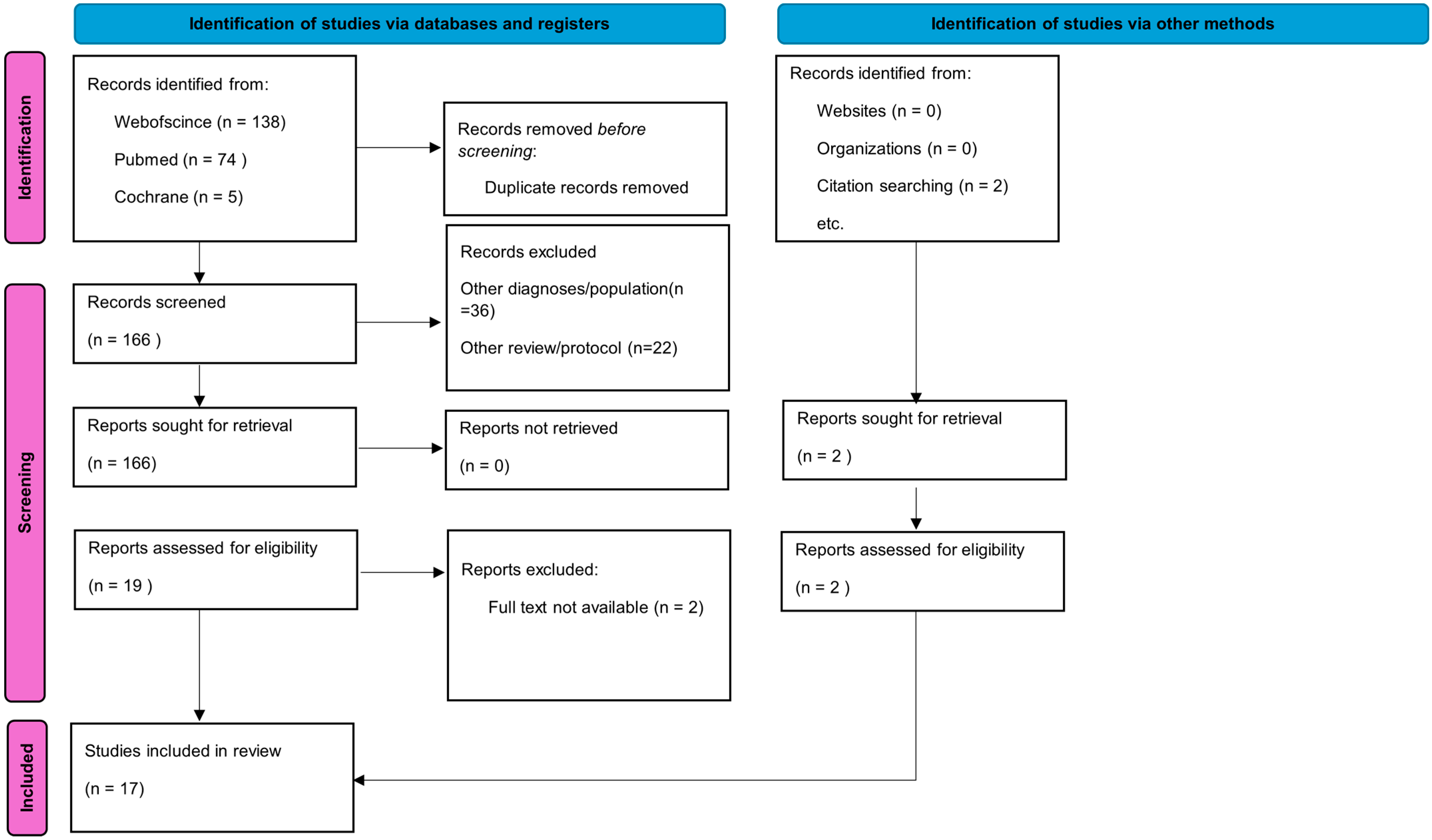
2. Materials and Methods
2.1. Protocol and Guidelines
2.2. Search Strategy
2.3. Selection Criteria
- Patients: Systematic reviews or meta-analyses in which at least 50% of the included articles had a sample composed of adolescents (10–19 years old).
- Intervention: Physical exercise. In this study, physical exercise was defined as any activity that is planned, structured, repetitive, and purposefully completed to improve physical fitness [1].
- Comparison: Comparison before and after the intervention or comparison with any other intervention, as long as the target population received intervention with some physical exercise program.
- Results: Physical fitness. For this study, physical fitness was considered a set of attributes related to health or skills, with the health-related components of physical fitness being cardiorespiratory endurance, muscular endurance, muscular strength, body composition, and flexibility [1]. Programs with physical exercise, which had other domains as outcome measures, in addition to physical fitness, were also considered, as long as physical fitness was one of the outcome measures.
- Of-Study Design: Systematic review or meta-analysis only.
2.4. Data Collection
2.5. Methodological Quality Assessment
2.6. Summary and Quality of Evidence (GRADE)
3. Results
3.1. Characteristics of the Studies
3.2. Evaluation of Methodological Quality
3.2.1. Analysis of Negative Responses
3.2.2. Analysis of Critical Items
3.3. Description of Reviews of High Methodological Quality
3.3.1. Intervention: Power Exercise
- Quality of evidence (GRADE): MODERATE
- Risk of bias: moderate
- Inconsistency: no information
- Indirectness: high
- Imprecision: moderate
- Publication bias: low
3.3.2. Intervention: Aerobic Exercise
- Quality of evidence (GRADE): MODERATE-LOW
- Risk of bias: low
- Inconsistency: low
- Indirectness: high
- Imprecision: moderate
- Publication bias: moderate
3.3.3. Intervention: Resistive Therapy
- Quality of evidence (GRADE): MODERATE
- Risk of bias: moderate
- Inconsistency: moderate
- Indirectness: high
- Imprecision: moderate to high
- Publication bias: low
3.4. Description of Reviews of Moderate Methodological Quality
3.4.1. Intervention: Nintendo Wii Therapy (NWT) with Balance Board
- Quality of evidence (GRADE): LOW
- Risk of bias: moderate
- Inconsistency: low
- Indirectness: low
- Imprecision: low
- Publication bias: moderate
3.4.2. Intervention: VRT (Virtual Reality Therapy)
- Quality of evidence (GRADE): MODERATE TO HIGH
- Risk of bias: moderate
- Inconsistency: moderate
- Indirectness: high
- Imprecision: high
- Publication bias: moderate
3.4.3. Intervention: Aerobic Exercise
- Quality of evidence (GRADE): MODERATE TO LOW
- Risk of bias: high
- Inconsistency: moderate
- Indirectness: high
- Imprecision: low
- Publication bias: low
4. Discussion
4.1. Main Findings
4.2. Other Considerations
5. Conclusions
- -
- The systematic reviews and meta-analyses on the effects of physical exercise in adolescents with CP were diverse regarding the exercises studied, the number of studies included, the type of studies included (randomized/non-randomized), and the number of participants in each study.
- -
- The number of studies included in each review, whether the review included only randomized studies, and the number of participants included in each review were not factors that interfered with the result in assessing methodological quality.
- -
- The methodological quality of systematic reviews and meta-analyses on the effects of physical exercise in adolescents with CP is variable, but only 15.78% have high methodological quality.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical Activity, Exercise, and Physical Fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- Hosker, D.K.; Elkins, R.M.; Potter, M.P. Promoting Mental Health and Wellness in Youth through Physical Activity, Nutrition, and Sleep. Child Adolesc. Psychiatr. Clin. N. Am. 2019, 28, 171–193. [Google Scholar] [CrossRef] [PubMed]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020. [Google Scholar] [CrossRef]
- Tian, D.; Meng, J. Exercise for Prevention and Relief of Cardiovascular Disease: Prognoses, Mechanisms, and Approaches. Oxidative Med. Cell. Longev. 2019, 2019, 3756750. [Google Scholar] [CrossRef] [PubMed]
- Nystoriak, M.A.; Bhatnagar, A. Cardiovascular Effects and Benefits of Exercise. Front. Cardiovasc. Med. 2018, 5, 408204. [Google Scholar] [CrossRef] [PubMed]
- Schultchen, D.; Reichenberger, J.; Mittl, T.; Weh, T.R.M.; Smyth, J.M.; Blechert, J.; Pollatos, O. Bidirectional Relationship of Stress and Affect with Physical Activity and Healthy Eating. Br. J. Health Psychol. 2019, 24, 315–333. [Google Scholar] [CrossRef]
- McMahon, E.M.; Corcoran, P.; O’Regan, G.; Keeley, H.; Cannon, M.; Carli, V.; Wasserman, C.; Hadlaczky, G.; Sarchiapone, M.; Apter, A.; et al. Physical Activity in European Adolescents and Associations with Anxiety, Depression and Well-Being. Eur. Child Adolesc. Psychiatry 2016, 26, 111–122. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, G.; Liu, C.; Guan, J.; Zhang, Y.; Shi, Z. Comparing the Efficacy of Different Types of Exercise for the Treatment and Prevention of Depression in Youths: A Systematic Review and Network Meta-Analysis. Front. Psychiatry 2023, 14, 1199510. [Google Scholar] [CrossRef]
- Bell, S.L.; Audrey, S.; Gunnell, D.; Cooper, A.; Campbell, R. The Relationship between Physical Activity, Mental Wellbeing and Symptoms of Mental Health Disorder in Adolescents: A Cohort Study. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 138. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Saltin, B. Exercise as Medicine—Evidence for Prescribing Exercise as Therapy in 26 Different Chronic Diseases. Scand. J. Med. Sci. Sports 2015, 25, 1–72. [Google Scholar] [CrossRef]
- Abdelhaleem, N.; Taher, S.; Mahmoud, M.; Hendawy, A.; Hamed, M.; Mortada, H.; Magdy, A.; Raafat Ezz El-Din, M.; Zoukiem, I.; Elshennawy, S. Effect of Action Observation Therapy on Motor Function in Children with Cerebral Palsy: A Systematic Review of Randomized Controlled Trials with Meta-Analysis. Clin. Rehabil. 2020, 35, 51–63. [Google Scholar] [CrossRef] [PubMed]
- Sadowska, M.; Sarecka-Hujar, B.; Kopyta, I. Cerebral Palsy: Current Opinions on Definition, Epidemiology, Risk Factors, Classification and Treatment Options. Neuropsychiatr. Dis. Treat. 2020, 16, 1505–1518. [Google Scholar] [CrossRef] [PubMed]
- Verschuren, O.; Peterson, M.D.; Balemans, A.C.J.; Hurvitz, E.A. Exercise and Physical Activity Recommendations for People with Cerebral Palsy. Dev. Med. Child Neurol. 2016, 58, 798–808. [Google Scholar] [CrossRef] [PubMed]
- Novak, I.; Honan, I. Effectiveness of Paediatric Occupational Therapy for Children with Disabilities: A Systematic Review. Aust. Occup. Ther. J. 2019, 66, 258–273. [Google Scholar] [CrossRef] [PubMed]
- Hjalmarsson, E.; Fernandez-Gonzalo, R.; Lidbeck, C.; Palmcrantz, A.; Jia, A.; Kvist, O.; Pontén, E.; von Walden, F. RaceRunning Training Improves Stamina and Promotes Skeletal Muscle Hypertrophy in Young Individuals with Cerebral Palsy. BMC Musculoskelet. Disord. 2020, 21, 193. [Google Scholar] [CrossRef]
- Park, E.-Y.; Kim, W.-H. Structural Equation Modeling of Motor Impairment, Gross Motor Function, and the Functional Outcome in Children with Cerebral Palsy. Res. Dev. Disabil. 2013, 34, 1731–1739. [Google Scholar] [CrossRef]
- González, L.; Argüelles, J.; González, V.; Winge, K.; Iscar, M.; Olmedillas, H.; Blanco, M.; Valenzuela, P.L.; Lucia, A.; Federolf, P.A.; et al. Slackline Training in Children with Spastic Cerebral Palsy: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2020, 17, 8649. [Google Scholar] [CrossRef]
- Minghetti, A.; Widmer, M.; Viehweger, E.; Roth, R.; Gysin, R.; Keller, M. Translating Scientific Recommendations into Reality: A Feasibility Study Using Group-Based High-Intensity Functional Exercise Training in Adolescents with Cerebral Palsy. Disabil. Rehabil. 2023, 46, 4787–4796. [Google Scholar] [CrossRef]
- Smith, K.J.; Peterson, M.D.; O’Connell, N.E.; Victor, C.; Liverani, S.; Anokye, N.; Ryan, J.M. Risk of Depression and Anxiety in Adults with Cerebral Palsy. JAMA Neurol. 2019, 76, 294. [Google Scholar] [CrossRef]
- Toldi, J.; Escobar, J.; Brown, A. Cerebral Palsy: Sport and Exercise Considerations. Curr. Sports Med. Rep. 2021, 20, 19–25. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A Critical Appraisal Tool for Systematic Reviews That Include Randomised or Non-Randomised Studies of Healthcare Interventions, or Both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef] [PubMed]
- Atkins, D. Grading Quality of Evidence and Strength of Recommendations. BMJ 2004, 328, 1490. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, E.L.; Boyd, R.N.; Kentish, M.J.; Carty, C.P.; Horan, S.A. Effects of a Training Programme of Functional Electrical Stimulation (FES) Powered Cycling, Recreational Cycling and Goal-Directed Exercise Training on Children with Cerebral Palsy: A Randomised Controlled Trial Protocol. BMJ Open 2019, 9, e024881. [Google Scholar] [CrossRef]
- Duarte Machado, E.; Cole, M.H.; Miller, L.; McGuckian, T.B.; Wilson, P.H. The Efficacy of Dance Interventions for the Activity and Participation of Individuals with Cerebral Palsy—A Systematic Review and Meta-Analysis. Disabil. Rehabil. 2023, 46, 1485–1501. [Google Scholar] [CrossRef]
- Roostaei, M.; Baharlouei, H.; Azadi, H.; Fragala-Pinkham, M.A. Effects of Aquatic Intervention on Gross Motor Skills in Children with Cerebral Palsy: A Systematic Review. Phys. Occup. Ther. Pediatr. 2016, 37, 496–515. [Google Scholar] [CrossRef]
- Mujawar, M.M. A Systematic Review of the Effects of Aquatic Therapy on Motor Functions in Children with Cerebral Palsy. Reabil. Moksl. Slauga Kineziter. Ergoter. 2022, 2, 51–67. [Google Scholar] [CrossRef]
- Montoro-Cárdenas, D.; Cortés-Pérez, I.; Zagalaz-Anula, N.; Osuna-Pérez, M.C.; Obrero-Gaitán, E.; Lomas-Vega, R. Nintendo Wii Balance Board Therapy for Postural Control in Children with Cerebral Palsy: A Systematic Review and Meta-Analysis. Dev. Med. Child Neurol. 2021, 63, 1262–1275. [Google Scholar] [CrossRef]
- Warnier, N.; Lambregts, S.; Port, I.V.D. Effect of Virtual Reality Therapy on Balance and Walking in Children with Cerebral Palsy: A Systematic Review. Dev. Neurorehabilit. 2020, 23, 502–518. [Google Scholar] [CrossRef]
- Ravi, D.K.; Kumar, N.; Singhi, P. Effectiveness of Virtual Reality Rehabilitation for Children and Adolescents with Cerebral Palsy: An Updated Evidence-Based Systematic Review. Physiotherapy 2017, 103, 245–258. [Google Scholar] [CrossRef]
- Wu, J.; Loprinzi, P.D.; Ren, Z. The Rehabilitative Effects of Virtual Reality Games on Balance Performance among Children with Cerebral Palsy: A Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2019, 16, 4161. [Google Scholar] [CrossRef] [PubMed]
- Merino-Andrés, J.; García de Mateos-López, A.; Damiano, D.L.; Sánchez-Sierra, A. Effect of Muscle Strength Training in Children and Adolescents with Spastic Cerebral Palsy: A Systematic Review and Meta-Analysis. Clin. Rehabil. 2021, 36, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Santos, K.P.; da SiIva, V.M.M.; dos Reis, I.F.; de Aquino, M.R.C.; Lana, M.R.V.; de Freitas Teixeira, C.M.M. Physical Conditioning in Children and Adolescents with Cerebral Palsy: Systematic Review and Meta-Analysis. J. Bodyw. Mov. Ther. 2023, 25, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Kara, Ö.K.; Gursen, C.; Cetin, S.Y.; Tascioglu, E.N.; Muftuoglu, S.; Damiano, D.L. The Effects of Power Exercises on Body Structure and Function, Activity and Participation in Children with Cerebral Palsy: An ICF-Based Systematic Review. Disabil. Rehabil. 2023, 45, 3705–3718. [Google Scholar] [CrossRef] [PubMed]
- Booth, A.T.C.; Buizer, A.I.; Meyns, P.; Oude Lansink, I.L.B.; Steenbrink, F.; van der Krogt, M.M. The Efficacy of Functional Gait Training in Children and Young Adults with Cerebral Palsy: A Systematic Review and Meta-Analysis. Dev. Med. Child Neurol. 2018, 60, 866–883. [Google Scholar] [CrossRef]
- Collado Garrido, L.; Parás Bravo, P.; Calvo Martín, P.; Santibáñez Margüello, M. Impacto de La Terapia Resistida Sobre Los Parámetros de La Marcha En Niños Con Parálisis Cerebral: Revisión Sistemática Y Metaanálisis. Rev. Neurol. 2019, 69, 307. [Google Scholar] [CrossRef]
- Soares, E.G.; Gusmão, C.H.V.; Souto, D.O. Efficacy of Aerobic Exercise on the Functioning and Quality of Life of Children and Adolescents with Cerebral Palsy: A Systematic Review and Meta-Analysis. Dev. Med. Child Neurol. 2023, 65, 1292–1307. [Google Scholar] [CrossRef]
- Czencz, J.; Shields, N.; Wallen, M.; Wilson, P.H.; McGuckian, T.B.; Imms, C. Does Exercise Affect Quality of Life and Participation of Adolescents and Adults with Cerebral Palsy: A Systematic Review. Disabil. Rehabil. 2023, 45, 4190–4206. [Google Scholar] [CrossRef]
- Bania, T.; Chiu, H.-C.; Billis, E. Activity Training on the Ground in Children with Cerebral Palsy: Systematic Review and Meta-Analysis. Physiother. Theory Pract. 2018, 35, 810–821. [Google Scholar] [CrossRef]
- Bania, T.A.; Taylor, N.F.; Chiu, H.-C.; Charitaki, G. What Are the Optimum Training Parameters of Progressive Resistance Exercise for Changes in Muscle Function, Activity and Participation in People with Cerebral Palsy? A Systematic Review and Meta-Regression. Physiotherapy 2023, 119, 1–16. [Google Scholar] [CrossRef]
- Liang, X.; Tan, Z.; Yun, G.; Cao, J.; Wang, J.; Liu, Q.; Chen, T. Effectiveness of Exercise Interventions for Children with Cerebral Palsy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Rehabil. Med. 2021, 53, jrm00176. [Google Scholar] [CrossRef] [PubMed]
- de Sousa Junior, R.R.; Souto, D.O.; Camargos, A.C.R.; Clutterbuck, G.L.; Leite, H.R. Moving Together Is Better: A Systematic Review with Meta-Analysis of Sports-Focused Interventions Aiming to Improve Physical Activity Participation in Children and Adolescents with Cerebral Palsy. Disabil. Rehabil. 2023, 45, 2398–2408. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen-Barr, E.; Halvorsen, M.; Bohman, T.; Boström, C.; Dedering, Å.; Kuster, R.; Olsson, C.; Rovner, G.; Tseli, E.; Nilsson-Wikmar, L.; et al. Summarizing the Effects of Different Exercise Types in Chronic Neck Pain—A Systematic Review and Meta-Analysis of Systematic Reviews. BMC Musculoskelet. Disord. 2023, 24, 806. [Google Scholar] [CrossRef] [PubMed]
- Lai, B.; Lee, E.; Wagatsuma, M.; Frey, G.; Stanish, H.; Jung, T.; Rimmer, J.H. Research Trends and Recommendations for Physical Activity Interventions among Children and Youth with Disabilities: A Review of Reviews. Adapt. Phys. Act. Q. 2020, 37, 211–234. [Google Scholar] [CrossRef]
- Posadzki, P.; Pieper, D.; Bajpai, R.; Makaruk, H.; Könsgen, N.; Neuhaus, A.L.; Semwal, M. Exercise/Physical Activity and Health Outcomes: An Overview of Cochrane Systematic Reviews. BMC Public Health 2020, 20, 1724. [Google Scholar] [CrossRef]
- Wassenaar, T.M.; Williamson, W.; Johansen-Berg, H.; Dawes, H.; Roberts, N.; Foster, C.; Sexton, C.E. A Critical Evaluation of Systematic Reviews Assessing the Effect of Chronic Physical Activity on Academic Achievement, Cognition and the Brain in Children and Adolescents: A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 79. [Google Scholar] [CrossRef]
| Reference Number | Database | Studies | Population | Exercise | Outcome | Measure | Conclusion |
|---|---|---|---|---|---|---|---|
| [24] | SCOPUS, PubMed, CINAHL, EMBASE, SPORTDiscus, and Cochrane. | Nine articles in qualitative and four in quantitative synthesis; 1 to 62 participants per study. | Cerebral palsy, 6–14 years. | Cycling | To improve muscle strength, balance, and gross motor function in children with cerebral palsy. | GMFM; PEDALS; PODCI; PEDI-CAT. | Significant improvements were reported for hamstring strength (effect size = 0.77–0.93), cardiorespiratory fitness (effect size = 1.13–1.77), balance (effect size = 1.03–1.29), 3 min walk test distance (effect size = 1.14), and gross motor function (effect size = 0.91). Conclusions were limited by small sample sizes, inconsistent outcome measures, and lack of follow-up testing. |
| [42] | EMBASE, PubMed, Scielo, PEDro, and CINAHL. | Ten articles (RCTs); 19 to 68 participants per study. | Cerebral palsy, 5–24 years. | Aerobic training, progressive resistive exercises, and treadmill training. | Improve participation in exercise, sport, and physical activity. | PEM-CY; Life-H; Participation in physical activities: CAPE; COPM. | Positive pooled effects on leisure time participation were seen only in group interventions at short-term follow-up compared with control. Sports-focused interventions did not improve overall participation. |
| [34] | MEDLINE (PubMed), Cochrane, and Web of Science. | Ten articles; 10 to 42 participants per study. | Cerebral palsy, 4–20 years. | Power training. | Walking speed, activities of daily living, muscle strength, and gross motor function. | 1MFWT; 6MWT; TUG; GMFM; PODC; ASK; MMT; FMS; Goal Attainment Scale; 3D Gait analysis; PEM-CY; dynamometer. | Moderate evidence was found that strength exercises increased walking speed, activities of daily living, and muscle strength and improved gross motor function more than a routine physical therapy program. The lack of stronger evidence might be explained by the differences in training protocols and the degree to which these met the physiological definition of power, the different methods of measuring power, limited durations of training, and the relative effectiveness of control interventions. |
| [35] | PubMed, Embase, CINAHL, and Web of Science. | Forty-one studies (11 RCTs); 1 to 95 participants per study. | Cerebral palsy, 5–25 years. | Functional gait training. | Walking speed was the most commonly reported gait outcome. | 2MFWT; 6MWT; 10MWT; GMFM, TUG; PEDI. | There is promising evidence that functional gait training is a safe, feasible, and effective intervention to target improved walking ability in children and young adults with CP. The addition of virtual reality and biofeedback can increase patient engagement and magnify effects. |
| [36] | Medline, ISI Web of Knowledge, and PEDro. | Ten articles (nine controlled studies and one single-arm study); 6 to 62 participants per study. | Cerebral palsy, 4–18 years. | Resistive therapy. | Impact on strength, motor function, and gait (at least one gait parameter). | GMFM; STS; LSU; MobQue; TUG. | The results concluded that resistive therapy improves muscle strength and gait parameters, and the study established an intervention protocol of 40–50 min for three days a week. |
| [41] | PubMed, Embase, and Cochrane. | Twenty-seven studies; 12 to 101 participants per study. | Cerebral palsy, 6–16 years. | Aerobic or resistance training. | Gross motor function, gait speed, and muscular strength. | ICF; GMFM; Three-dimensional gait analysis; Biodex dynamometer; The Biodex Gait Trainer 2TM; WeeFIM; Bruininks– Oseretsity test; Lateral step up Test; 6MWT; GAS. | The meta-analysis revealed that exercise interventions are not associated with improved gross motor function in children with CP, but were associated with increased gait speed and muscle strength. |
| [39] | PubMed, Cochrane, Science Direct, OVID, ERIC, Dare, and PEDro. | Nine studies (RCTs); 8 to 30 participants per study. | Cerebral palsy, 10–12 years. | Activity training on the ground (such as sit-to-stand, walking, or stepping). | Most of the studies used either the Gross Motor Function Measure or the Timed Up and Go. | 1MFWT; GMFM; TUG; MAS; Wee-FIM. | The available evidence shows little effect of activity training on the ground on activity or participation in children with CP, suggesting that rigorous trials with larger samples and a larger “dosage” of activity training on the ground are needed in the future. |
| [38] | Cochrane, MEDLINE, Embase, CINAHL, Pedro, Science Web, Otseeker, SCOPUS, and PubMed. | Seventeen studies; 6 to 95 participants per study. | Cerebral palsy, age ≥ 16 years. | Strength, aerobic, or treadmill training; dance; and swimming. | Quality of life, participation, pain, mood, and fatigue. | LIFE-H; SF-36; WHOQOF-BREF; 10WMT, FIM; GMFM. | The review could not answer the primary questions about the effect of an exercise intervention on quality of life and participation nor the secondary questions about pain, mood, fatigue, and self-efficacy. A limited number of studies suggest that exercise may improve fatigue and mental health in adults with CP, but more research is needed to confirm these findings. |
| [37] | Embase, PubMed, CINAHL, and PEDro. | Fifteen RCTs; 6 to 34 participants per study. | Cerebral palsy, 4–21 years. | Aerobic exercise. | Aerobic capacity, muscle strength, spasticity, balance, gait parameters, gross motor function, mobility, quality of life, and participation. | 6MWT; 10MWT; Shuttle Run Tests; Muscle Power Sprint Test; computerized dynamometer; Second Sit to Stand Test; MAS; BBS; Biodex Gait; three-dimensional motion analysis; GMFM. | Aerobic exercise improves gross motor function but not gait parameters in cerebral palsy (CP). It improves participation, but not quality of life in children and adolescents with CP. It is more effective than usual care or other interventions in improving mobility, aerobic capacity, and balance in CP. It is no more effective than usual care or other interventions in improving muscle strength and spasticity. |
| [40] | PubMed, Web of Science, Scopus, OVID, Science Direct, PEDro, ERIC and ClinicalTrials.gov. | Twenty reports (16 RCTs); 12 to 64 participants per study. | Cerebral palsy, age ≤18 years. | Progressive resistance exercise. | Muscle strength was the primary outcome. | GMFM; MAS; FMS; PedsQL; 6MWT; MobQue; LifeHABITS; Harris Children’s SelfConcept Scale; PODCI; MTS; SPPC. | When PRE was compared with another therapy, there were no differences between groups. PRE is safe and increases muscle strength in young people with CP, which is maintained after training stops. The increase in muscle strength is unrelated to the PRE intensity or dose. |
| [33] | PubMed, SciELO, PEDro, ERIC, and Cochrane. | Five studies (four RCTs); 13 to 29 participants per study. | Cerebral palsy, 7–18 years. | Aerobic training. | Improve walk distance and VO2max. | 6MWD or VO2max (maximum oxygen volume). | Positive effects on the cardiorespiratory fitness system in CP. Aerobic training statistically increased VO2 max in CP. Aerobic training increased the distance covered during the 6MWT. |
| [26] | PubMed, Web of Science, Scopus, Physiotherapy Evidence Database (PEDro), Google Scholar, and Proquest. | Eleven studies; 1 to 29 participants per study. | Cerebral palsy, 3–21 years. | Aquatic exercise. | Main outcomes: gross motor skills (walking speed or distance). | GMFM; COPM; Timed walk tests; PEDI; mobility and self-care domains. | The findings indicate that the effects of aquatic intervention on gross motor skills and walking speed are variable in children with CP who are ambulatory. The level of evidence is low for the majority of studies, especially for children classified according to GMFCS levels III–V, and further research is needed. |
| [32] | MEDLINE-PubMed, Cochrane, PEDro, CINAHL, and SPORTDiscus. | Twenty-seven studies; 873 participants. | Cerebral palsy, 3–22 years. | Strength training. | Strength, spasticity, gait, balance, energy expenditure, and motor function. | GMFM; daily step; Sitting time MAS; Dynamic Balance (FRT, PBS); WB-SI; CAPE; FEF; PedsQoLCP; PierrsHarris Self Concept Scale; MobQues28; COPM; STS; LSU; MAS; MMT; TUG; PEDI; FMS; FWT; 1MFWT; 6MWT; 10MWT;TST; NNcost. | Strength training programs appear to improve the strength of trained muscles, balance, gait, and motor function in CP, without increasing spasticity, but this type of intervention may demonstrate different effects in different neurological conditions. |
| [29] | PubMed and Embase. | Twenty-six studies; 3 to 40 participants per study. | Cerebral palsy, 6–18 years. | Virtual reality. | Balance, walking speed, and walking distance. | mABC-2; 1MFWT; 2MFWT; 6MWT; 10MWT; Quiet stance (force plate); Romberg test; CB&M TUDS; BOTMP; PBS; BBS; TUG; FAB; Dynamic stance (force plate); PRT; BOT 2; Msot; Reactive balance (force plate); Rhythmic weight shift test; FFRT; FSRT; TGGT. | VRT appears to be a promising intervention for rehabilitation in children with CP. Meta-analysis confirmed this positive effect. These results should be interpreted with caution due to differences in the interventions used, the lack of randomized controlled trials, and the relatively small groups. |
| [28] | PubMed, MEDLINE, Scopus, Web of Science, PEDro (Physioterapia Evidence Database), and SciELO. | Eleven RCTs; 16 to 40 participants per study. | Cerebral palsy, 5–16 years. | Nintendo Wii therapy. | Balance. | TGUGT; PBS; OLST. | NWT can be considered an effective treatment for improving functional and dynamic balance in children with CP, especially when combined with CPT in 30 min sessions, with interventions lasting longer than 3 weeks. Moderate-quality evidence. |
| [31] | CNKI, Wanfang Data, Web of Science, PubMed, EBSCOhost, Informit, Scopus, Science Direct, and ProQuest. | Eleven studies; 16 to 48 participants per study. | Cerebral palsy, ≤14 years. | Virtual reality. | Balance. | M-ABC; PBS; BBS; Nintendo Wii Fit Balance; Board Score; TUG; PBM. | VR games played a positive role in improving the balance of children with CP, but these results should be viewed with caution due to current methodological defects (measurement difference, heterogeneity of control groups, intervention combined with other treatments). |
| [25] | CINAHL, Embase, PubMed, Informações Psicológicas, Escopo, and Web of Science. | Sixteen studies; 1 to 27 participants per study. | Cerebral palsy, 7–18 years. | Movement and step-based dance practice. | Impact on walking/gait, balance/postural control, and range of motion. | PBS; PRT; 10MWT; GMFM; BCS; BBS; TUG; DGI; K-MBI; FGA; GAITRite system; TUDS; QUEST. | The review suggested a positive impact on the main outcomes but the findings should be interpreted with caution (limitations). |
| [30] | PubMed, PEDro, Web of Science, OTseeker, PsycINFO, and Cochrane. | Thirty-one studies; 1 to 32 participants per study. | Cerebral palsy, mean age 6–16. | Virtual reality. | Balance and motor skills. | GMFM; TUG; PBS; PEDI; Modified UE Functional Targeting Reach Test; TUDS; WeeFIM–The; QUEST; STST; PRT, RSA; AMPS; BBS; FMA; GAS; PSA. | Moderate evidence that VRT is a promising intervention to improve balance and motor skills in children and adolescents with CP. The technique is growing, so long-term follow-up and further research are required to determine its exact place in the management of cerebral palsy. |
| [27] | Google Acadêmico, PubMed and PEDRO | 11 studies (6 RCTs). 5 to 17 participants per study | Cerebral palsy, 3–15 years | Aquatic interventions | Motor function, quality of life, fatigue, spasticity, balance, enjoyment, behaviour, activities of daily living, strength, endurance and aerobic capacity. | GMFM | The review suggest that aquatic therapy has the potential to achieve better motor functions in CP patient with GMFCS levels between I–III when compared with conventional land-based therapy or to no intervention. |
| Reference Number | Design | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [24] | MA | Y | Y | Y | PY | N | Y | Y | Y | PY | N | Y | N | N | Y | N | Y | CL |
| [42] | MA | Y | Y | Y | PY | Y | Y | N | Y | Y | N | N | N | N | N | N | Y | CL |
| [34] | SR | Y | Y | Y | Y | Y | Y | Y | PY | Y | N | NM | NM | Y | Y | NM | Y | H |
| [35] | MA | Y | PY | N | PY | Y | Y | Y | PY | N | N | Y | N | N | Y | N | Y | CL |
| [36] | MA | Y | Y | Y | PY | Y | Y | Y | PY | Y | N | Y | Y | Y | Y | Y | Y | H |
| [41] | MA | Y | Y | Y | PY | Y | Y | N | PY | Y | N | N | N | N | N | N | Y | CL |
| [39] | MA | Y | PY | Y | PY | Y | Y | Y | PY | Y | N | N | Y | N | N | N | Y | CL |
| [38] | SR | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | NM | NM | Y | Y | NM | Y | H |
| [37] | MA | Y | Y | Y | PY | Y | Y | Y | N | Y | N | Y | Y | Y | Y | Y | N | M |
| [40] | MA | Y | PY | N | PY | Y | Y | Y | PY | Y | N | N | N | N | N | N | Y | CL |
| [33] | MA | Y | Y | Y | PY | Y | Y | N | PY | Y | N | Y | Y | N | N | N | Y | CL |
| [26] | SR | Y | PY | Y | PY | Y | Y | Y | PY | Y | N | NM | NM | N | N | NM | Y | L |
| [32] | MA | Y | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | Y | Y | N | Y | CL |
| [29] | MA | Y | PY | Y | PY | Y | Y | Y | Y | PY | N | Y | N | Y | Y | N | Y | L |
| [28] | MA | Y | Y | Y | Y | Y | Y | Y | PY | Y | Y | Y | N | Y | Y | Y | N | M |
| [31] | MA | Y | Y | Y | PY | Y | Y | Y | Y | Y | N | Y | N | Y | N | Y | Y | M |
| [25] | MA | Y | Y | N | PY | Y | Y | Y | PY | Y | N | N | N | N | N | N | Y | CL |
| [30] | SR | Y | Y | N | PY | Y | Y | N | Y | Y | Y | NM | NM | Y | Y | NM | Y | L |
| [27] | SR | Y | PY | N | PY | N | N | Y | Y | N | N | NM | NM | N | N | NM | Y | CL |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nitz, A.C.R.; Campos, M.J.; Antunes, A.A.M.; da Silva Freitas, E.; Toscano, C.V.A.; Ferreira, J.P. The Methodological Quality of Studies on Physical Exercise in Adolescents with Cerebral Palsy: A Scoping Review of Systematic Reviews and Meta-Analyses. Healthcare 2024, 12, 2039. https://doi.org/10.3390/healthcare12202039
Nitz ACR, Campos MJ, Antunes AAM, da Silva Freitas E, Toscano CVA, Ferreira JP. The Methodological Quality of Studies on Physical Exercise in Adolescents with Cerebral Palsy: A Scoping Review of Systematic Reviews and Meta-Analyses. Healthcare. 2024; 12(20):2039. https://doi.org/10.3390/healthcare12202039
Chicago/Turabian StyleNitz, Alexandrina Cavalcante Rodrigues, Maria João Campos, Ana Amélia Moraes Antunes, Emilly da Silva Freitas, Chrystiane Vasconcelos Andrade Toscano, and José Pedro Ferreira. 2024. "The Methodological Quality of Studies on Physical Exercise in Adolescents with Cerebral Palsy: A Scoping Review of Systematic Reviews and Meta-Analyses" Healthcare 12, no. 20: 2039. https://doi.org/10.3390/healthcare12202039
APA StyleNitz, A. C. R., Campos, M. J., Antunes, A. A. M., da Silva Freitas, E., Toscano, C. V. A., & Ferreira, J. P. (2024). The Methodological Quality of Studies on Physical Exercise in Adolescents with Cerebral Palsy: A Scoping Review of Systematic Reviews and Meta-Analyses. Healthcare, 12(20), 2039. https://doi.org/10.3390/healthcare12202039








