Association between Quality of Life, Confinement, and Sex in Adults: A Multigroup Structural Equation Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Variables and Instruments
2.3. Procedure
2.4. Data Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lehmann, S.; Haug, E.; Bjørknes, R.; Mjeldheim Sandal, G.; Fadnes, L.T.; Skogen, J.C. Quality of life among young people in Norway during the COVID-19 pandemic. A longitudinal study. Eur. Child. Adolesc. Psychiatry 2023, 32, 1061–1071. [Google Scholar] [CrossRef] [PubMed]
- Hawi, N.S.; Samaha, M. The relations among social media addiction, self-esteem, and life satisfaction in university students. Soc. Sci. Comput. Rev. 2017, 35, 576–586. [Google Scholar] [CrossRef]
- Kaya, G.; Zeren, M. Age-related differences in functional capacity, physical activity, life satisfaction, well-being and quality of life in turkish adult population during COVID-19. J. Basic. Clin. Health Sci. 2022, 6, 128–138. [Google Scholar] [CrossRef]
- Peterson, N.E.; Sirard, J.R.; Kulbok, P.A.; DeBoer, M.D.; Erickson, J.M. Sedentary behavior and physical activity of young adult university students. Res. Nurs. Health 2018, 41, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Karageorgou, A.; Kokaridas, D.; Theodorakis, Y.; Goudas, M.; Krommidas, C.; Mousiolis, S. The effect of exercise and goal setting strategies on improving quality of life of multiple sclerosis patients. J. Sport. Health Res. 2024, 16, 67–82. [Google Scholar] [CrossRef]
- Choi, J.I.; Cho, Y.H.; Kim, Y.J.; Lee, S.Y.; Lee, J.G.; Yi, Y.H.; Tak, Y.J.; Hwang, H.R.; Lee, S.H.; Park, E.J.; et al. The Relationship of Sitting Time and Physical Activity on the Quality of Life in Elderly People. Int. J. Environ. Res. Public Health 2021, 18, 1459. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Lee, E. The association between elderly people’s sedentary behaviors and their health-related quality of life: Focusing on comparing the young-old and the old-old. Health Qual. Life Outcomes 2019, 17, 131. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, A.R.; Murad, H.R. The Impact of Social Media on Panic During the COVID-19 Pandemic in Iraqi Kurdistan: Online Questionnaire Study. J. Med. Internet Res. 2020, 22, e19556. [Google Scholar] [CrossRef] [PubMed]
- Oura, M.J.; Moreira, A.R.; Santos, P. Stress among Portuguese Medical Students: A National Cross-Sectional Study. J. Environ. Public Health 2020, 2020, 6183757. [Google Scholar] [CrossRef]
- Pinillos, Y.P.; Cobos, R.R.; de Ávila Quintana, L.; Egea, S.A.; Montero, L.V.; Beltrán, Y.H.; Cueto, D.; Baena, S.G.; Racha, C.R. Caracterización de hábitos alimentarios y de actividad física en jóvenes de la Región Caribe Colombiana. Nutr. Clín Diet. Hosp. 2022, 42, 12–21. [Google Scholar]
- Zurita-Ortega, F.; Castro-Sánchez, M.; Álvaro-Rodríguez, J.I.; Rodríguez-Fernández, S.; Pérez-Cortés, A. Self-concept, physical activity and family: Analysis of a structural equation model. Sports Psychol. J. 2016, 25, 97–101. [Google Scholar]
- Hewitt, B.; Deranek, K.; McLeod, A.; Gudi, A. Exercise motives impact on physical activities measured using wearable devices. Health Promot. Int. 2022, 37, daac071. [Google Scholar] [CrossRef] [PubMed]
- Flores Paredes, A.; Pino Vanegas, Y.M.; Yupanqui Pino, E.H.; Yupanqui Pino, A.; Mamani, S.; Coila Pancca, D.; Atencio Ayma, L.J.; Manzaneda Peña, M.A.; Lavalle Gonzales, A.K. Estilos de vida y el índice de masa corporal en estudiantes universitarios. Retos 2023, 50, 950–957. [Google Scholar] [CrossRef]
- Valladares, M.; Ramírez-Tagle, R.; Muñoz, M.A.; Obregón, A.M. Individual differences in chronotypes associated with academic performance among Chilean University students. Chronobiol. Int. 2018, 35, 578–583. [Google Scholar] [CrossRef] [PubMed]
- Ilic, M.; Pang, H.W.; Vlaski, T.; Grujicic, M.; Novakovic, B. Motives and barriers for regular physical activity among medical students from the Western Balkans (South-East Europe Region). Int. J. Environ. Res. Public Health 2022, 19, 16240. [Google Scholar] [CrossRef]
- Chen, E.; Brody, G.H.; Miller, G.E. Childhood close family relationships and health. Am. Psychol. 2017, 72, 555. [Google Scholar] [CrossRef] [PubMed]
- Grønhøj, A.; Thøgersen, J. Why young people do things for the environment: The role of parenting for adolescents’ motivation to engage in pro-environmental behaviour. J. Environ. Psychol. 2017, 54, 11–19. [Google Scholar] [CrossRef]
- Arnason, A.; Langarica, N.; Dugas, L.R.; Mora, N.; Luke, A.; Markossian, T. Family-based lifestyle interventions: What makes them successful? A systematic literature review. Prev. Med. 2020, 21, 101299. [Google Scholar] [CrossRef] [PubMed]
- Hryniewicz, A.; Gmiat, A.; Jaroch-Lidzbarska, M.; Lipowski, M. Actividad física en el manejo del estrés entre los gerentes durante la pandemia de COVID-19: Una revisión sistemática. Ley Balt. J. Health Phys. 2023, 15. [Google Scholar] [CrossRef]
- Kadam, A.B.; Atre, S.R. Negative impact of social media panic during the COVID-19 outbreak in India. J. Travel. Med. 2020, 27, taaa057. [Google Scholar] [CrossRef]
- Srinivasan Raj, S.; Kuduruthullah, S.; Al Moutassem Billah, K.; Al Shayeb, M.; Elkaseh, A.; Sudhir Rama, V.; Gulrez, N.; Issameldin, E.; Ashekhi, A. Impact of pain, psychological-distress, SARS-CoV-2 fear on adults’ OHRQOL during COVID-19 pandemic. Saudi J. Biol. Sci. 2021, 28, 492–494. [Google Scholar] [CrossRef]
- Dalbudak, İ.; Yiğit, Ş.; Yılmaz, T. La relación entre la calidad de vida y la nutrición de los estudiantes universitarios. Prog. Nutr. 2020, 22, 112–121. [Google Scholar] [CrossRef]
- García, S.; Herrera, N.; Rodríguez, C.; Nissensohn, M.; Román, B.; Serra-Majem, L. KIDMED test; prevalence of low adherence to the Mediterranean diet in children and young; a systematic review. Nutr. Hosp. 2015, 32, 2390–2399. [Google Scholar]
- Aguilar-Cordero, M.J.; León-Ríos, X.A.; Rojas-Carvajal, A.M.; Latorre-García, J.; Pérez Castillo, I.M.; Sánchez-López, A.M. Effects of physical activity on quality of life in overweight and obese children. Nutr. Hosp. 2021, 38, 736–741. [Google Scholar] [CrossRef]
- Mosconi, L.; Walters, M.; Sterling, J.; Quinn, C.; McHugh, P.; Andrews, R.E.; Matthews, D.C.; Ganzer, C.; Osorio, R.S.; Isaacson, R.S.; et al. Lifestyle and vascular risk effects on MRI- based biomarkers of Alzheimer’s disease: A cross-sectional study of middle-aged adults from the broader New York City area. BMJ Open 2018, 8, e019362. [Google Scholar] [CrossRef]
- Dentale, F.; Vecchione, M.; Alessandri, G.; Barbaranelli, C. Investigating the protective role of global self-esteem on the relationship between stressful life events and depression: A longitudinal moderated regression model. Curr. Psychol. 2020, 39, 2096–2107. [Google Scholar] [CrossRef]
- Numans, W.; Regenmortel, T.; Schalk, R.; y Boog, J. Vulnerable persons in society: An insider’s perspective. Int. J. Qual. Stud. Health Well-Being 2021, 16, 1863598. [Google Scholar] [CrossRef] [PubMed]
- Füzéki, E.; Engeroff, T.; Banzer, W. Health benefits of light-intensity physical activity: A systematic review of accelerometer data of the national health and nutrition examination survey (NHANES). Sports Med. 2017, 47, 1769–1793. [Google Scholar] [CrossRef]
- Warburton, D.E.; Bredin, S.S. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef]
- McMahon, E.M.; Corcoran, P.; O’Regan, G.; Keeley, H.; Cannon, M.; Carli, V.; Wasserman, C.; Hadlaczky, G.; Sarchiapone, M.; Apter, A.; et al. Physical activity in European adolescents and associations with anxiety, depression and well-being. Eur. Child. Adolesc. Psychiatry 2017, 26, 111–122. [Google Scholar] [CrossRef]
- Nixdorf, R.; Beckmann, J.; Oberhoffer, R.; Weberrub, H.; Nixdorf, I. Associations between Physical Fitness and Mental Health Among German Adolescents. J. Sport. Health Res. 2021, 13, 125–138. [Google Scholar]
- Amornsriwatanakul, A.; Rahman, H.A.; Katewongsa, P.; Chaiyasong, S.; Charoenwattana, S.; Chupradit, S.; Ivanovitch, K.; Rodjarkpai, Y.; Sriboonma, K.; Sudnongbua, S.; et al. Multilevel factors associated with physical activity participation among Thai university students. Prev. Med. Rep. 2023, 36, 102510. [Google Scholar] [CrossRef] [PubMed]
- Hesketh, K.R.; Lakshman, R.; van Sluijs, E.M.F. Barriers and facilitators to young children’s physical activity and sedentary behavior: A systematic review and synthesis of qualitative literature. Obes. Rev. 2017, 18, 987–1017. [Google Scholar] [CrossRef]
- Hootman, K.C.; Guertin, K.A.; Cassano, P.A. Stress and psychological constructs related to eating behavior are associated with anthropometry and body composition in young adults. Appetite 2018, 125, 287–294. [Google Scholar] [CrossRef]
- O’Regan, A.; Hannigan, A.; Glynn, L.; Garcia Bengoechea, E.; Donnelly, A.; Hayes, G.; Murphy, A.W.; Clifford, A.M.; Gallagher, S.; Woods, C.B. A cluster analysis of device-measured physical activity behaviours and the association with chronic conditions, multi-morbidity and healthcare utilisation in adults aged 45 years and older. Prev. Med. Rep. 2021, 24, 101641. [Google Scholar] [CrossRef]
- Walsh, A.; Taylor, C.; Brennick, D. Factors that influence campus dwelling University Student’s facility to practice healthy living guidelines. Can. J. Nurs. Res. 2018, 50, 57–63. [Google Scholar] [CrossRef]
- Davis, H.A.; Riley, E.N.; Smith, G.T.; Milich, R.; Burris, J.L. Alcohol use and strenuous physical activity in college students: A longitudinal test of 2 explanatory models of health behavior. J. Am. Coll. Health 2017, 65, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Badau, A.; Rachita, A.; Radu-Sasu, C.; Clipa, A. Motivations and the Level of Practicing Physical Activities by Physio-Kinetotherapy Students. Educ. Sci. 2018, 8, 97. [Google Scholar] [CrossRef]
- Sharratt, J.; Sharratt, M.T.; Smith, D.; Howell, M.; Davenport, L. FANTASTIC Lifestyle Survey of University of Waterloo Employees. Can. Fam. Physician 1984, 30, 1869–1872. [Google Scholar]
- Ramírez-Vélez, R.; Agredo, R.A. Fiabilidad y validez del instrumento “Fantástico” para medir el estilo de vida en adultos colombianos. Rev. De. Salud Pública 2012, 14, 226–237. [Google Scholar] [CrossRef]
- Barrón, V.; Rodríguez, A.; Chavarría, P. Eating habits, nutritional status and lifestyles in active older adults in the city of Chillán, Chile. Chil. J. Nutr. 2017, 44, 57–62. [Google Scholar] [CrossRef]
- Marsh, H.W. Application of Confirmatory Factor Analysis and Structural Equation Modeling in Sport and Exercise Psychology. In Handbook of Sport Psychology, 3rd ed.; Tenenbaum, G., Eklund, R.C., Eds.; Sons Inc.: Hoboken, NJ, USA, 2007. [Google Scholar]
- Khomsi, K.; Najmi, H.; Amghar, H.; Chelhaoui, Y.; Souhaili, Z. COVID-19 national lockdown in morocco: Impacts on air quality and public health. One Health 2021, 11, 100200. [Google Scholar] [CrossRef] [PubMed]
- Guida, C.; Carpentieri, G. Quality of life in the urban environment and primary health services for the elderly during the Covid-19 pandemic: An application to the city of Milan (Italy). Cities 2021, 110, 103038. [Google Scholar] [CrossRef]
- Wyche, K.P.; Nichols, M.; Parfitt, H.; Beckett, P.; Gregg, D.J.; Smallbone, K.L.; Monks, P.S. Changes in ambient air quality and atmospheric composition and reactivity in the South East of the UK as a result of the COVID-19 lockdown. Sci. Total Environ. 2021, 755, 142526. [Google Scholar] [CrossRef] [PubMed]
- Sieczkowska, S.M.; de Lima, A.P.; Swinton, P.A.; Dolan, E.; Roschel, H.; Gualano, B. Health Coaching Strategies for Weight Loss: A Systematic Review and Meta-Analysis. Adv. Nutr. 2021, 12, 1449–1460. [Google Scholar] [CrossRef] [PubMed]
- Merlo, G.; Vela, A. Mental Health in Lifestyle Medicine: A Call to Action. Am. J. Lifestyle Med. 2022, 16, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Merced-Len, S.; Velázquez-Cintra, A.; Ramírez-González, M.; Coll-Costa, J.L. La actividad física en la formación de hábitos y estilos de vida saludables: Experiencia con universitarios cubanos en COVID-19. Luz 2022, 21, 114–128. [Google Scholar]
- Weber, M.; Schnorr, T.; Morat, M.; Morat, T.; Donath, L. Effects of Mind-Body Interventions Involving Meditative Movements on Quality of Life, Depressive Symptoms, Fear of Falling and Sleep Quality in Older Adults: A Systematic Review with Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6556. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Lan, M.; Li, H.; Yang, J. Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: A moderated mediation model. Sleep Med. 2021, 77, 339–345. [Google Scholar] [CrossRef]
- Martins, J.; Costa, J.; Sarmento, H.; Marques, A.; Farias, C.; Onofre, M.; Valeiro, M.G. Adolescents’ Perspectives on the Barriers and Facilitators of Physical Activity: An Updated Systematic Review of Qualitative Studies. Int. J. Environ. Res. Public Health 2021, 18, 4954. [Google Scholar] [CrossRef]
- Geigl, C.; Loss, J.; Leitzmann, M.; Janssen, C. Social factors of health-related quality of life in older adults: A multivariable analysis. Qual. Life Res. 2023, 32, 3257–3268. [Google Scholar] [CrossRef]
- Sarla, E.; Lambrinou, E.; Galanis, P.; Kalokairinou, A.; Sourtzi, P. Factors That Influence the Relationship between Social Support and Health-Related Quality of Life of Older People Living in the Community. Gerontol. Geriatr. Med. 2020, 6, 2333721420911474. [Google Scholar] [CrossRef] [PubMed]
- Sawa, S.; Sekine, M.; Yamada, M.; Fukazawa, Y.; Hiraku, Y. Social and family factors as determinants of exercise habits in Japanese elementary school children: A cross-sectional study from the Super Shokuiku School Project. Env. Health Prev. Med. 2020, 25, 54. [Google Scholar] [CrossRef]
- Valdés-Badilla, P.; Herrera-Valenzuela, T.; Guzmán-Muñoz, E.; Delgado-Floody, P.; Núñez-Espinosa, C.; Monsalves-Álvarez, M.; Andrade, D.C. Effects of Olympic Combat Sports on Health-Related Quality of Life in Middle-Aged and Older People: A Systematic Review. Front. Psychol. 2022, 12, 797537. [Google Scholar] [CrossRef]
- Harwood, C.G.; Keegan, R.J.; Smith, J.M.; Raine, A.S. A systematic review of the intrapersonal correlates of motivational climate perceptions in sport and physical activity. Psychol. Sport. Exerc. 2015, 18, 9–25. [Google Scholar] [CrossRef]
- Robinson, E.; Boyland, E.; Chisholm, A.; Harrold, J.; Maloney, N.G.; Marty, L.; Mead, B.R.; Noonan, R.; Hardman, C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite 2021, 156, 104853. [Google Scholar] [CrossRef]
- Flanagan, E.W.; Beyl, R.A.; Fearnbach, S.N.; Altazan, A.D.; Martin, C.K.; Redman, L.M. The Impact of COVID-19 Stay- At-Home Orders on Health Behaviors in Adults. Obesity 2021, 29, 438–445. [Google Scholar] [CrossRef]
- López-Moreno, M.; Lopez, M.T.; Miguel, M.; Garces-Rimon, M. Physical and Psychological Effects Related to Food Habits and Lifestyle Changes Derived from COVID-19 Home Confinement in the Spanish Population. Nutrients 2020, 12, 3445. [Google Scholar] [CrossRef]
- Álvaro-González, J.I.; Zurita Ortega, F.; Castro Sánchez, M.; Martínez, A.; García Sánchez, S. Relationship between tobacco and alcohol consumption and self-concept in Spanish adolescents. Rev. Complut. Educ. 2015, 27, 533–550. [Google Scholar] [CrossRef]
- Öztürk Çopur, E.; Karasu, F. The impact of the COVID-19 pandemic on the quality of life and depression, anxiety, and stress levels of individuals above the age of eighteen. Perspect. Psychiatr. Care 2021, 57, 1645–1655. [Google Scholar] [CrossRef] [PubMed]
- Szabo, C.; Pukanszky, J.; Kemeny, L. Psychological Effects of the COVID-19 Pandemic on Hungarian Adults. Int. J. Environ. Res. Public Health 2020, 17, 9565. [Google Scholar] [CrossRef] [PubMed]
- Havnen, A.; Anyan, F.; Hjemdal, O.; Solem, S.; Gurigard Riksfjord, M.; Hagen, K. Resilience Moderates Negative Outcome from stress during the COVID-19 Pandemic: A Moderated-Mediation Approach. Int. J. Environ. Res. Public Health 2020, 17, 6461. [Google Scholar] [CrossRef] [PubMed]
- Muller, J.; Siefken, K.; Parfitt, G.; Dollman, J. Exploring the social conditions of physical activity participation amongst rural South Australian women: A qualitative study. Health Promot. J. Aust. 2020, 32 (Suppl. S2), 54–64. [Google Scholar] [CrossRef] [PubMed]
- Qi, M.L.; Li, P.; Moyle, W.; Weeks, B.; Jones, C. Physical Activity, Health-Related Quality of Life, and Stress among the Chinese Adult Population during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6494. [Google Scholar] [CrossRef]
- Suzuki, Y.; Maeda, N.; Hirado, D.; Shirakawa, T.; Urabe, Y. Physical Activity Changes and Its Risk Factors among Community-Dwelling Japanese Older Adults during the COVID-19 Epidemic: Associations with Subjective Well-Being and Health-Related Quality of Life. Int. J. Environ. Res. Public Health 2020, 17, 6591. [Google Scholar] [CrossRef]




| Confinement Status | Total | ||||
|---|---|---|---|---|---|
| Yes | No | ||||
| Sex | Male | Count | 254 | 277 | 531 |
| % Sex | 47.8% | 52.2% | 100.0% | ||
| % Confinement | 54.5% | 68.2% | 60.9% | ||
| Female | Count | 212 | 129 | 341 | |
| % Sex | 62.2% | 37.8% | 100.0% | ||
| % Confinement | 45.5% | 31.8% | 39.1% | ||
| Total | Count | 466 | 406 | 872 | |
| % Sex | 53.4% | 46.6% | 100% | ||
| % Confinement | 100% | 100% | 100% | ||
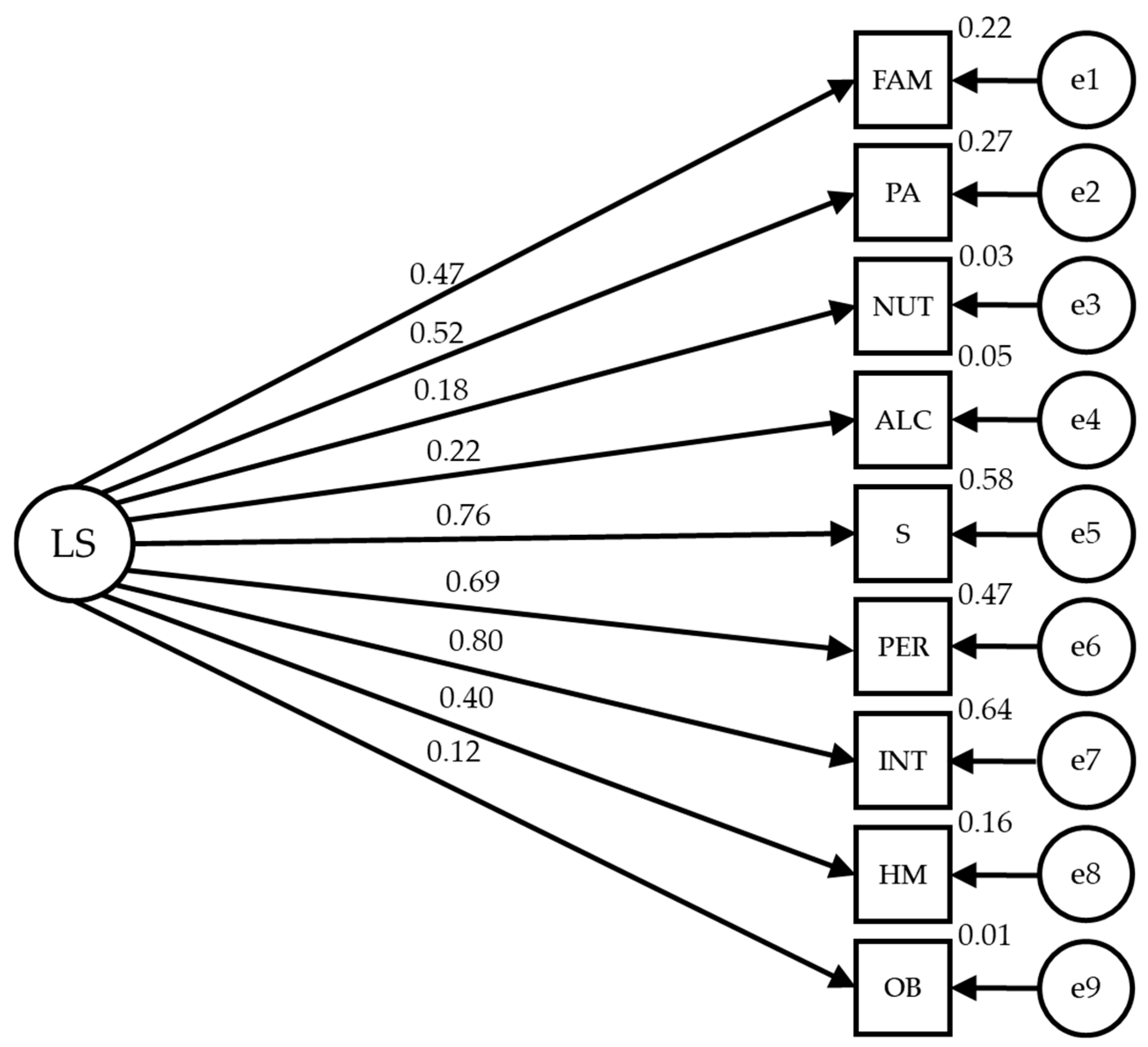
| Relationships between Variables | R.W. | S.R.W. | |||||
|---|---|---|---|---|---|---|---|
| Estimates | E.E. | C.R. | p | Estimates | |||
| FAM | ← | LS | 1.002 | 0.113 | 7.631 | *** | 0.498 |
| PA | ← | LS | 0.580 | 0.118 | 4.923 | *** | 0.310 |
| NUT | ← | LS | 0.551 | 0.116 | 4.752 | *** | 0.297 |
| ALC | ← | LS | 0.489 | 0.101 | 4.822 | *** | 0.302 |
| S | ← | LS | 1.203 | 0.149 | 8.064 | *** | 0.663 |
| PER | ← | LS | 1.037 | 0.134 | 7.762 | *** | 0.609 |
| INT | ← | LS | 1.119 | 0.137 | 8.186 | *** | 0.690 |
| HM | ← | LS | 0.902 | 0.142 | 6.356 | *** | 0.435 |
| OB | ← | LS | 0.484 | 0.108 | 4.493 | *** | 0.278 |
| Relationships between Variables | R.W. | S.R.W. | |||||
|---|---|---|---|---|---|---|---|
| Estimates | E.E. | C.R. | p | Estimates | |||
| FAM | ← | LS | 1.490 | 0.026 | 7.622 | *** | 0.430 |
| PA | ← | LS | 0.984 | 0.149 | 6.594 | *** | 0.439 |
| NUT | ← | LS | 0.375 | 0.090 | 4.184 | *** | 0.234 |
| ALC | ← | LS | 0.050 | 0.050 | 1.000 | 0.317 | 0.051 |
| S | ← | LS | 1.682 | 0.201 | 8.388 | *** | 0.757 |
| PER | ← | LS | 1.247 | 0.155 | 8.028 | *** | 0.659 |
| INT | ← | LS | 1.670 | 0.197 | 8.482 | *** | 0.803 |
| HM | ← | LS | 0.464 | 0.099 | 4.707 | *** | 0.271 |
| OB | ← | LS | 0.199 | 0.082 | 2.420 | 0.016 | 0.128 |
| Relationships between Variables | R.W. | S.R.W. | |||||
|---|---|---|---|---|---|---|---|
| Estimates | E.E. | C.R. | p | Estimates | |||
| FAM | ← | LS | 0.984 | 0.076 | 7.622 | *** | 0.466 |
| PA | ← | LS | 0.803 | 0.121 | 6.636 | *** | 0.387 |
| NUT | ← | LS | 0.373 | 0.087 | 4.272 | *** | 0.223 |
| ALC | ← | LS | 0.245 | 0.069 | 3.557 | *** | 0.182 |
| S | ← | LS | 1.407 | 0.152 | 9.243 | *** | 0.718 |
| PER | ← | LS | 1.111 | 0.126 | 8.842 | *** | 0.638 |
| INT | ← | LS | 1.346 | 0.144 | 9.358 | *** | 0.752 |
| HM | ← | LS | 0.703 | 0.107 | 6.578 | *** | 0.383 |
| OB | ← | LS | 0.185 | 0.080 | 2.306 | 0.021 | 0.115 |
| Relationships between Variables | R.W. | S.R.W. | |||||
|---|---|---|---|---|---|---|---|
| Estimates | E.E. | C.R. | p | Estimates | |||
| FAM | ← | LS | 0.954 | 0.078 | 7.622 | *** | 0.472 |
| PA | ← | LS | 1.191 | 0.178 | 6.676 | *** | 0.519 |
| NUT | ← | LS | 0.303 | 0.102 | 2.962 | 0.003 | 0.184 |
| ALC | ← | LS | 0.254 | 0.072 | 3.535 | *** | 0.223 |
| S | ← | LS | 1.520 | 0.190 | 8.003 | *** | 0.761 |
| PER | ← | LS | 1.258 | 0.163 | 7.693 | *** | 0.686 |
| INT | ← | LS | 1.617 | 0.199 | 8.123 | *** | 0.802 |
| HM | ← | LS | 0.738 | 0.132 | 5.613 | *** | 0.396 |
| OB | ← | LS | 0.198 | 0.098 | 2.019 | 0.044 | 0.122 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zurita-Ortega, F.; Galeano-Rojas, D.; Tenelanda-López, D.; Cresp-Barria, M.; Farias-Valenzuela, C.; Valdivia-Moral, P. Association between Quality of Life, Confinement, and Sex in Adults: A Multigroup Structural Equation Analysis. Healthcare 2024, 12, 774. https://doi.org/10.3390/healthcare12070774
Zurita-Ortega F, Galeano-Rojas D, Tenelanda-López D, Cresp-Barria M, Farias-Valenzuela C, Valdivia-Moral P. Association between Quality of Life, Confinement, and Sex in Adults: A Multigroup Structural Equation Analysis. Healthcare. 2024; 12(7):774. https://doi.org/10.3390/healthcare12070774
Chicago/Turabian StyleZurita-Ortega, Félix, Dilan Galeano-Rojas, Dennys Tenelanda-López, Mauricio Cresp-Barria, Claudio Farias-Valenzuela, and Pedro Valdivia-Moral. 2024. "Association between Quality of Life, Confinement, and Sex in Adults: A Multigroup Structural Equation Analysis" Healthcare 12, no. 7: 774. https://doi.org/10.3390/healthcare12070774
APA StyleZurita-Ortega, F., Galeano-Rojas, D., Tenelanda-López, D., Cresp-Barria, M., Farias-Valenzuela, C., & Valdivia-Moral, P. (2024). Association between Quality of Life, Confinement, and Sex in Adults: A Multigroup Structural Equation Analysis. Healthcare, 12(7), 774. https://doi.org/10.3390/healthcare12070774








