Potential Applications of Artificial Intelligence (AI) in Managing Polypharmacy in Saudi Arabia: A Narrative Review
Abstract
:1. Introduction
2. Methods and Materials
3. Results
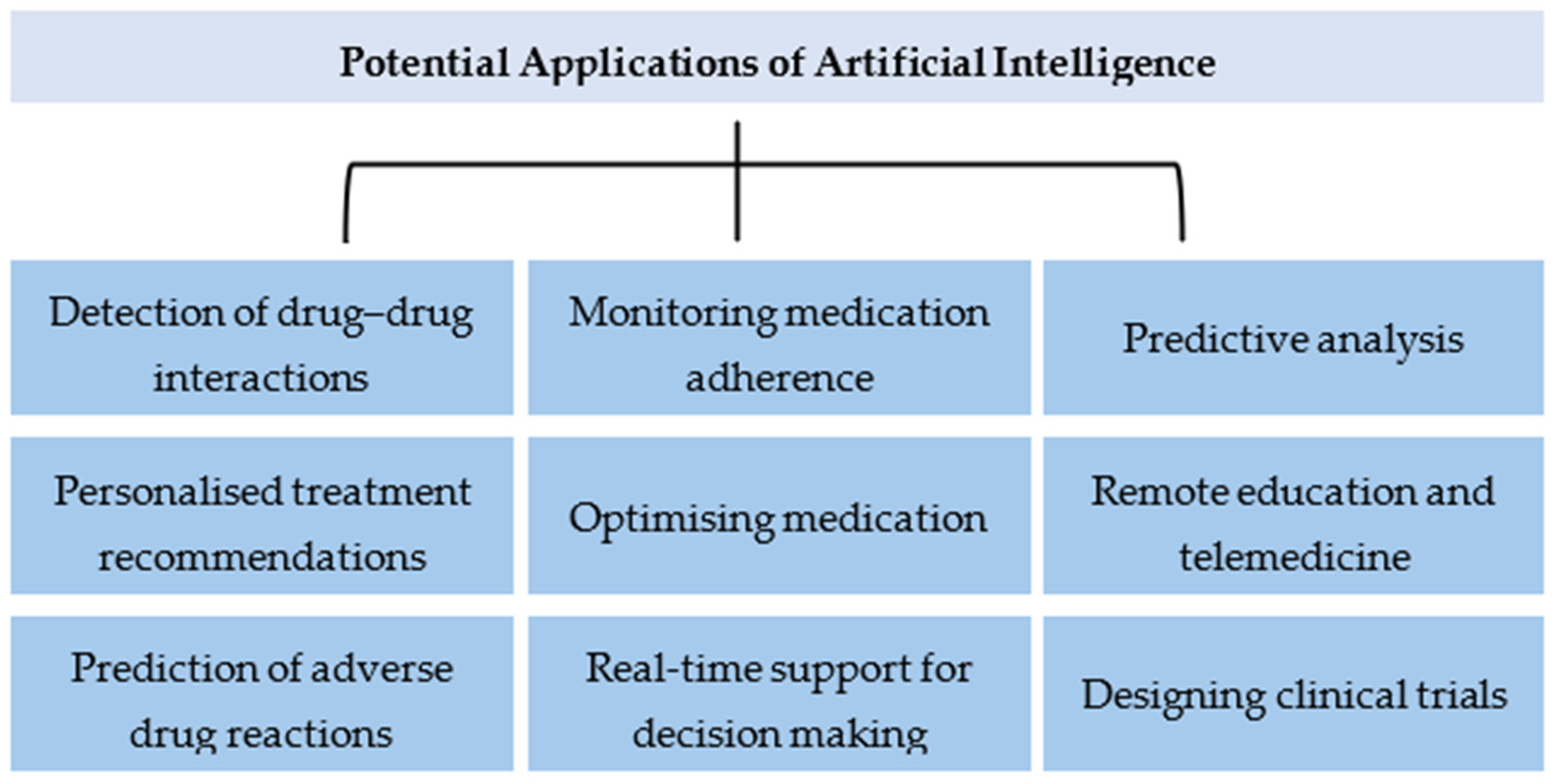
3.1. Main Applications of AI in Polypharmacy
- Drug–Drug Interaction Detection: AI algorithms can sift through extensive databases to identify potential adverse interactions between medications, reducing the risk of harmful side effects in patients with complex medication regimens.
- Personalised Medicine: By analysing genetic data, patient histories and current medications, ML models can help healthcare providers to tailor treatment plans to individuals, improving their efficacy and minimising unnecessary polypharmacy.
- Predictive Analytics: AI can forecast which patients are at risk of polypharmacy complications, allowing for pre-emptive adjustments to their treatment plans.
- Medication Adherence: AI-powered apps and devices can monitor patients’ adherence to medication schedules, providing reminders and alerts to both patients and healthcare providers to prevent the underuse or overuse of prescribed drugs.
3.2. Detection of Drug–Drug Interactions
3.3. Personalised Treatment Recommendations
3.4. Prediction of Adverse Drug Reactions
3.5. Monitoring Medication Adherence
3.6. Optimising Medication
3.7. Real-Time Support for Decision Making
- Interoperability: The system must be compatible with the existing EHR and healthcare IT infrastructure.
- User Interface: Alerts and recommendations should be presented in a user-friendly manner that integrates seamlessly into healthcare professionals’ workflows.
- Privacy and Security: Patient data used in the training and operation of the model must be handled according to strict privacy and security standards.
- Regulatory Compliance: The development and deployment of the system must comply with the relevant healthcare regulations and standards.
3.8. Predictive Analysis
3.9. Remote Education and Telemedicine
3.10. Designing Clinical Trials
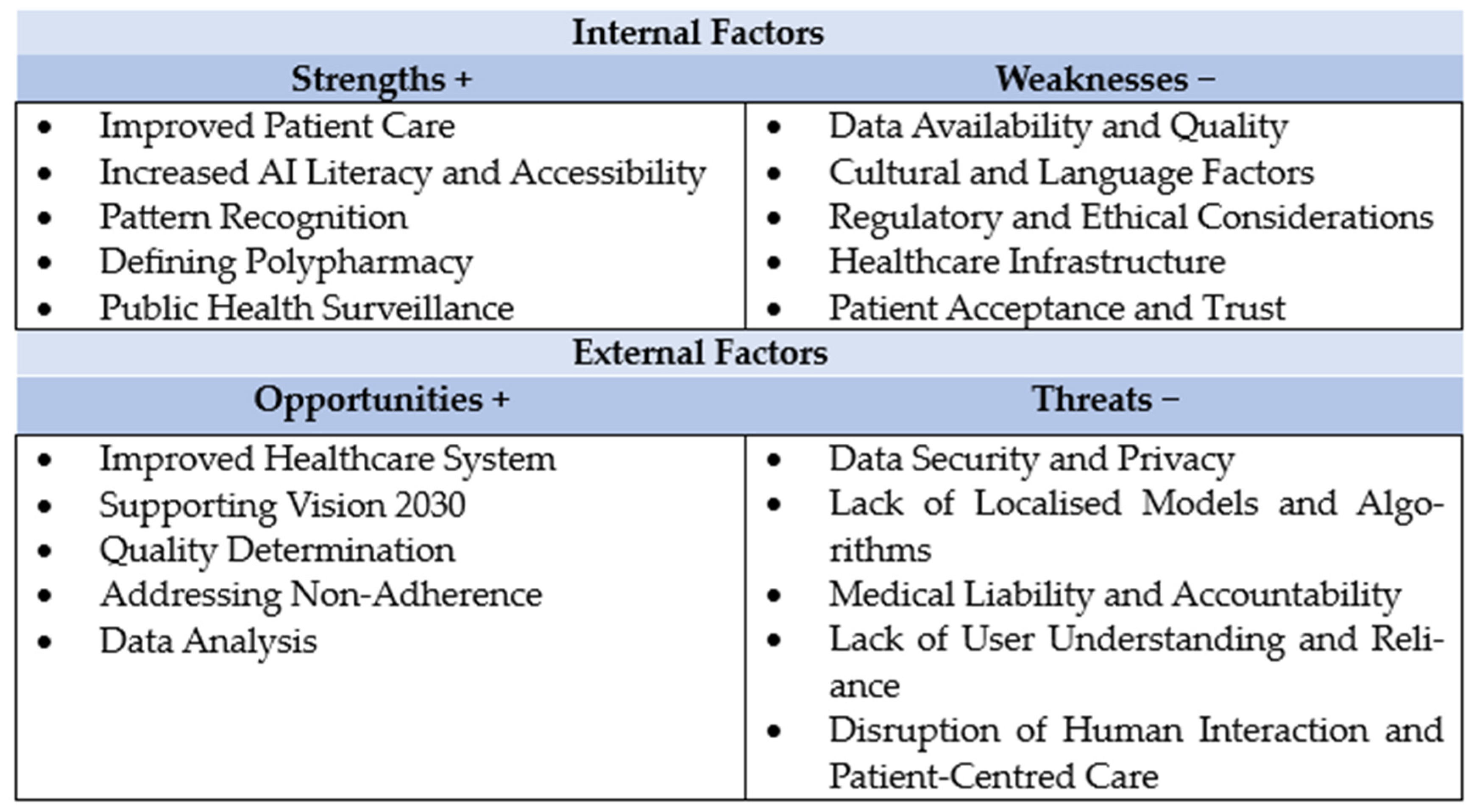
4. Discussion
- Enhanced Personalisation: AI will drive the shift towards more personalised medicine, where treatments and medication regimens are tailored to the individual’s genetic makeup, lifestyle and specific health conditions.
- Interoperability and Integration: The seamless integration of AI tools with existing EHRs and healthcare systems will be crucial. This will ensure that AI-driven insights are readily accessible to healthcare providers, facilitating informed decision making.
- Ethical AI Use: As AI takes on a more prominent role in healthcare, ethical considerations, including patient privacy, data security and algorithmic transparency, will become increasingly important. It will be essential to establish guidelines and standards for the ethical use of AI to maintain trust and protect patient rights.
- Education and Collaboration: Educating healthcare professionals about AI and its potential applications in polypharmacy management will be key to AI’s successful implementation. Furthermore, fostering collaboration between AI researchers, healthcare providers and patients will ensure that the AI solutions are effectively tailored to meet the needs of those whom they aim to serve.
- Continuous Innovation and Research: Ongoing research and innovation will be vital in expanding the capabilities of AI in healthcare. This includes developing new algorithms, refining existing models and exploring novel applications to address the complexities of polypharmacy and medication adherence.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aljawadi, M.H.; Khoja, A.T.; Alaboud, N.M.; AlEnazi, M.E.; Al-Shammari, S.A.; Khoja, T.A.; AlMuqbil, M.S.; Alsheikh, A.M.; Alwhaibi, M. Prevalence of Polypharmacy and Factors Associated with it among Saudi Older Adults—Results from the Saudi National Survey for Elderly Health (SNSEH). Saudi Pharm. J. 2022, 30, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Alosaimi, K.; Alwafi, H.; Alhindi, Y.; Falemban, A.; Alshanberi, A.; Ayoub, N.; Alsanosi, S. Medication Adherence among Patients with Chronic Diseases in Saudi Arabia. Int. J. Environ. Res. Public Health 2022, 19, 10053. [Google Scholar] [CrossRef] [PubMed]
- Alasiri, A.A.; Mohammed, V. Healthcare Transformation in Saudi Arabia: An Overview Since the Launch of Vision 2030. Health Serv Insights 2022, 15, 11786329221121214. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, S.R. Rational prescribing: The principles of drug selection. Clin. Med. 2016, 16, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Johansson, T.; Abuzahra, M.E.; Keller, S.; Mann, E.; Faller, B.; Sommerauer, C.; Höck, J.; Löffler, C.; Köchling, A.; Schuler, J.; et al. Impact of strategies to reduce polypharmacy on clinically relevant endpoints: A systematic review and meta-analysis. Br. J. Clin. Pharmacol. 2016, 82, 532–548. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.T.; Bussell, J.K. Medication adherence: WHO cares? Mayo Clin. Proc. 2011, 86, 304–314. [Google Scholar] [CrossRef] [PubMed]
- WHO Centre for Health Development. A Glossary of Terms for Community Health Care and Services for Older Persons; World Health Organization: Geneva, Switzerland, 2004.
- Mortazavi, S.S.; Shati, M.; Keshtkar, A.; Malakouti, S.K.; Bazargan, M.; Assari, S. Defining polypharmacy in the elderly: A systematic review protocol. BMJ Open 2016, 6, e010989. [Google Scholar] [CrossRef]
- Nishtala, P.S.; Salahudeen, M.S. Temporal Trends in Polypharmacy and Hyperpolypharmacy in Older New Zealanders over a 9-Year Period: 2005–2013. Gerontology 2015, 61, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Januário, B.D.; Mafra, N.S.; de Souza Silva, H.; Carvalho, I.M.; Sena, A.L.S.; Pereira, A.; Júnior, N.S.d.F.; Campos, H.O. Worldwide Prevalence of Polypharmacy: A Systematic Review. Curr. Drug Metab. 2023, 24, 568–586. [Google Scholar] [CrossRef]
- Chowdhury, S.; Mok, D.; Leenen, L. Transformation of health care and the new model of care in Saudi Arabia: Kingdom’s Vision 2030. J. Med. Life 2021, 14, 347–354. [Google Scholar]
- Rahman, R. The Privatization of Health Care System in Saudi Arabia. Health Serv. Insights 2020, 13, 1178632920934497. [Google Scholar] [CrossRef] [PubMed]
- Alkhamis, A.; Miraj, S.A. Access to health care in Saudi Arabia: Development in the context of vision 2030. In Handbook of Healthcare in the Arab World; Springer: Berlin/Heidelberg, Germany, 2021; pp. 1629–1660. [Google Scholar]
- Rahman, R.; Al-Borie, H.M. Strengthening the Saudi Arabian healthcare system: Role of vision 2030. Int. J. Healthc. Manag. 2021, 14, 1483–1491. [Google Scholar] [CrossRef]
- Sarker, I.H. AI-Based Modeling: Techniques, Applications and Research Issues Towards Automation, Intelligent and Smart Systems. SN Comput. Sci. 2022, 3, 158. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Liu, X.; Cao, X.; Huang, C.; Liu, E.; Qian, S.; Liu, X.; Wu, Y.; Dong, F.; Qiu, C.-W.; et al. Artificial intelligence: A powerful paradigm for scientific research. Innovation 2021, 2, 100179. [Google Scholar] [CrossRef] [PubMed]
- Bellini, V.; Cascella, M.; Cutugno, F.; Russo, M.; Lanza, R.; Compagnone, C.; Bignami, E.G. Understanding basic principles of Artificial Intelligence: A practical guide for intensivists. Acta Biomed. 2022, 93, e2022297. [Google Scholar]
- Datta, S.D.; Islam, M.; Rahman Sobuz, M.H.; Ahmed, S.; Kar, M. Artificial intelligence and machine learning applications in the project lifecycle of the construction industry: A comprehensive review. Heliyon 2024, 10, e26888. [Google Scholar] [CrossRef]
- Sarker, I.H. Deep Learning: A Comprehensive Overview on Techniques, Taxonomy, Applications and Research Directions. SN Comput. Sci. 2021, 2, 420. [Google Scholar] [CrossRef] [PubMed]
- Lepakshi, V.A. Machine Learning and Deep Learning based AI Tools for Development of Diagnostic Tools. In Computational Approaches for Novel Therapeutic and Diagnostic Designing to Mitigate SARS-CoV-2 Infection; Academic Press: Cambridge, MA, USA, 2022; pp. 399–420. [Google Scholar] [CrossRef]
- Kufel, J.; Bargieł-Łączek, K.; Kocot, S.; Koźlik, M.; Bartnikowska, W.; Janik, M.; Czogalik, Ł.; Dudek, P.; Magiera, M.; Lis, A.; et al. What Is Machine Learning, Artificial Neural Networks and Deep Learning?-Examples of Practical Applications in Medicine. Diagnostics 2023, 13, 2582. [Google Scholar] [CrossRef] [PubMed]
- Van Veen, D.; Van Uden, C.; Blankemeier, L.; Delbrouck, J.B.; Aali, A.; Bluethgen, C.; Pareek, A.; Polacin, M.; Reis, E.P.; Seehofnerova, A.; et al. Clinical Text Summarization: Adapting Large Language Models Can Outperform Human Experts. Res. Sq. 2023. [Google Scholar] [CrossRef]
- Saeed, A.; Bin Saeed, A.; AlAhmri, F.A. Saudi Arabia Health Systems: Challenging and Future Transformations with Artificial Intelligence. Cureus 2023, 15, e37826. [Google Scholar] [CrossRef]
- Bohr, A.; Memarzadeh, K. The rise of artificial intelligence in healthcare applications. In Artificial Intelligence in Healthcare; Academic Press: Cambridge, MA, USA, 2020; pp. 25–60. [Google Scholar] [CrossRef]
- Lee, D.; Yoon, S.N. Application of Artificial Intelligence-Based Technologies in the Healthcare Industry: Opportunities and Challenges. Int. J. Environ. Res. Public Health 2021, 18, 271. [Google Scholar] [CrossRef]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing healthcare: The role of artificial intelligence in clinical practice. BMC Med. Educ. 2023, 23, 689. [Google Scholar] [CrossRef] [PubMed]
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Future Healthc. J. 2019, 6, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Mirza, A.H.; Alqasomi, A.; El-Dahiyat, F.; Babar, Z.U. Access to Medicines and Pharmaceutical Policy in Saudi Arabia: A Scoping Review. Integr. Pharm. Res. Pract. 2023, 12, 137–155. [Google Scholar] [CrossRef] [PubMed]
- Alfahmi, A.A.; Curtain, C.M.; Salahudeen, M.S. Assessment of Knowledge, Attitude and Practices of the Hospital and Community Pharmacists in Saudi Arabia (Jeddah) towards Inappropriate Medication Use in Older Adults. Int. J. Environ. Res. Public Health 2023, 20, 1635. [Google Scholar] [CrossRef] [PubMed]
- Alsuwaidan, A.; Almedlej, N.; Alsabti, S.; Daftardar, O.; Al Deaji, F.; Al Amri, A.; Alsuwaidan, S. A Comprehensive Overview of Polypharmacy in Elderly Patients in Saudi Arabia. Geriatrics 2019, 4, 36. [Google Scholar] [CrossRef] [PubMed]
- Maher, R.L.; Hanlon, J.; Hajjar, E.R. Clinical consequences of polypharmacy in elderly. Expert Opin. Drug Saf. 2014, 13, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Salive, M.E. Multimorbidity in older adults. Epidemiol. Rev. 2013, 35, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Balkhi, B.; AlQahtani, N.; Alwhaibi, M.; Alshammari, T.M.; Alhawassi, T.M.; Mahmoud, M.A.; Almetwazi, M.; Ata, S.; Basyoni, M.; Aljadhey, H. Prevalence and factors associated with polypharmacy use among adult patients in Saudi Arabia. J. Patient Saf. 2021, 17, e1119–e1124. [Google Scholar] [CrossRef]
- Almalki, Z.S.; Alqahtani, N.; Salway, N.T.; Alharbi, M.M.; Alqahtani, A.; Alotaibi, N.; Alotaibi, T.M.; Alshammari, T. Evaluation of medication error rates in Saudi Arabia: A protocol for systematic review and meta-analysis. Medicine 2021, 100, e24956. [Google Scholar] [CrossRef]
- Choudhury, A.; Asan, O. Role of Artificial Intelligence in Patient Safety Outcomes: Systematic Literature Review. JMIR Med. Inform. 2020, 8, e18599. [Google Scholar] [CrossRef] [PubMed]
- Poly, T.N.; Islam, M.M.; Muhtar, M.S.; Yang, H.C.; Nguyen, P.A.A.; Li, Y.J. Machine Learning Approach to Reduce Alert Fatigue Using a Disease Medication-Related Clinical Decision Support System: Model Development and Validation. JMIR Med. Inform. 2020, 8, e19489. [Google Scholar] [CrossRef] [PubMed]
- Vora, L.K.; Gholap, A.D.; Jetha, K.; Thakur, R.R.S.; Solanki, H.K.; Chavda, V.P. Artificial Intelligence in Pharmaceutical Technology and Drug Delivery Design. Pharmaceutics 2023, 15, 1916. [Google Scholar] [CrossRef] [PubMed]
- Cheng, F.; Zhao, Z. Machine learning-based prediction of drug–drug interactions by integrating drug phenotypic, therapeutic, chemical, and genomic properties. J. Am. Med. Inform. Assoc. 2014, 21, e278–e286. [Google Scholar] [CrossRef] [PubMed]
- Temsah, M.H.; Aljamaan, F.; Malki, K.H.; Alhasan, K.; Altamimi, I.; Aljarbou, R.; Bazuhair, F.; Alsubaihin, A.; Abdulmajeed, N.; Alshahrani, F.S.; et al. ChatGPT and the Future of Digital Health: A Study on Healthcare Workers’ Perceptions and Expectations. Healthcare 2023, 11, 1812. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, Z.; Rahim, S.; Zubair, M.; Abdul-Ghafar, J. Artificial intelligence (AI) in medicine, current applications and future role with special emphasis on its potential and promise in pathology: Present and future impact, obstacles including costs and acceptance among pathologists, practical and philosophical considerations. A comprehensive review. Diagn. Pathol. 2021, 16, 24. [Google Scholar] [PubMed]
- Rezayi, S.; Sharareh, R.N.K.; Saeedi, S. Effectiveness of Artificial Intelligence for Personalized Medicine in Neoplasms: A Systematic Review. Biomed. Res. Int. 2022, 2022, 7842566. [Google Scholar] [CrossRef] [PubMed]
- Chekroud, A.M.; Bondar, J.; Delgadillo, J.; Doherty, G.; Wasil, A.; Fokkema, M.; Cohen, Z.; Belgrave, D.; DeRubeis, R.; Iniesta, R.; et al. The promise of machine learning in predicting treatment outcomes in psychiatry. World Psychiatry 2021, 20, 154–170. [Google Scholar] [CrossRef]
- Al Kuwaiti, A.; Nazer, K.; Al-Reedy, A.; Al-Shehri, S.; Al-Muhanna, A.; Subbarayalu, A.V.; Al Muhanna, D.; Al-Muhanna, F.A. A Review of the Role of Artificial Intelligence in Healthcare. J. Pers. Med. 2023, 13, 951. [Google Scholar] [CrossRef]
- Kumar, Y.; Koul, A.; Singla, R.; Ijaz, M.F. Artificial intelligence in disease diagnosis: A systematic literature review, synthesizing framework and future research agenda. J. Ambient. Intell. Humaniz. Comput. 2023, 14, 8459–8486. [Google Scholar] [CrossRef]
- Schmider, J.; Kumar, K.; LaForest, C.; Swankoski, B.; Naim, K.; Caubel, P.M. Innovation in Pharmacovigilance: Use of Artificial Intelligence in Adverse Event Case Processing. Clin. Pharmacol. Ther. 2019, 105, 954–961. [Google Scholar] [CrossRef] [PubMed]
- Mohsen, A.; Tripathi, L.P.; Mizuguchi, K. Deep learning prediction of adverse drug reactions in drug discovery using open TG–GATEs and FAERS databases. Front. Drug Discov. 2021, 1, 768792. [Google Scholar] [CrossRef]
- Ahmed, Z.; Mohamed, K.; Zeeshan, S.; Dong, X. Artificial intelligence with multi-functional machine learning platform development for better healthcare and precision medicine. Database 2020, 2020, baaa010. [Google Scholar] [CrossRef] [PubMed]
- Biehl, J.T.; Patel, R.; Lee, A.J. Toward the Design of Sensing-Based Medication Adherence Aids That Support Individualized Activities of Daily Living: Survey and Interviews with Patients and Providers. JMIR Hum. Factors 2023, 10, e40173. [Google Scholar] [CrossRef] [PubMed]
- Flores, A.M.; Demsas, F.; Leeper, N.J.; Ross, E.G. Leveraging Machine Learning and Artificial Intelligence to Improve Peripheral Artery Disease Detection, Treatment, and Outcomes. Circ. Res. 2021, 128, 1833–1850. [Google Scholar] [CrossRef]
- Liang, L.; Hu, J.; Sun, G.; Hong, N.; Wu, G.; He, Y.; Li, Y.; Hao, T.; Liu, L.; Gong, M. Artificial Intelligence-Based Pharmacovigilance in the Setting of Limited Resources. Drug Saf. 2022, 45, 511–519. [Google Scholar] [CrossRef]
- Murali, K.; Kaur, S.; Prakash, A.; Medhi, B. Artificial intelligence in pharmacovigilance: Practical utility. Indian J. Pharmacol. 2019, 51, 373–376. [Google Scholar]
- Melton, G.B.; Hripcsak, G. Automated detection of adverse events using natural language processing of discharge summaries. J. Am. Med. Inform. Assoc. 2005, 12, 448–457. [Google Scholar] [CrossRef]
- Babel, A.; Taneja, R.; Mondello Malvestiti, F.; Monaco, A.; Donde, S. Artificial Intelligence Solutions to Increase Medication Adherence in Patients with Non-communicable Diseases. Front. Digit. Health 2021, 3, 669869. [Google Scholar] [CrossRef]
- Sekandi, J.N.; Shi, W.; Zhu, R.; Kaggwa, P.; Mwebaze, E.; Li, S. Application of Artificial Intelligence to the Monitoring of Medication Adherence for Tuberculosis Treatment in Africa: Algorithm Development and Validation. JMIR AI 2023, 2, e40167. [Google Scholar] [CrossRef]
- Chun-Yun Kang, G. Technology-based interventions to improve adherence to antihypertensive medications—An evidence-based review. Digit. Health 2022, 8, 20552076221089725. [Google Scholar] [CrossRef] [PubMed]
- van der Sijs, H.; Aarts, J.; Vulto, A.; Berg, M. Overriding of drug safety alerts in computerized physician order entry. J. Am. Med. Inform. Assoc. 2006, 13, 138–147. [Google Scholar] [CrossRef]
- Barrio-Cortes, J.; Benito-Sánchez, B.; Villimar-Rodriguez, A.I.; Rujas, M.; Arroyo-Gallego, P.; Carlson, J.; Merino-Barbancho, B.; Roca-Umbert, A.; Castillo-Sanz, A.; Lupiáñez-Villanueva, F.; et al. Differences in healthcare service utilization in patients with polypharmacy according to their risk level by adjusted morbidity groups: A population-based cross-sectional study. J. Pharm. Policy Pract. 2023, 16, 161. [Google Scholar] [CrossRef]
- Alshammari, F.M.; Alanazi, E.J.; Alanazi, A.M.; Alturifi, A.K.; Alshammari, T.M. Medication Error Concept and Reporting Practices in Saudi Arabia: A Multiregional Study among Healthcare Professionals. Risk Manag. Healthc. Policy 2021, 14, 2395–2406. [Google Scholar] [CrossRef]
- Poweleit, E.A.; Vinks, A.A.; Mizuno, T. Artificial Intelligence and Machine Learning Approaches to Facilitate Therapeutic Drug Management and Model-Informed Precision Dosing. Ther. Drug Monit. 2023, 45, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Alhumaidi, R.M.; Bamagous, G.A.; Alsanosi, S.M.; Alqashqari, H.S.; Qadhi, R.S.; Alhindi, Y.Z.; Ayoub, N.; Falemban, A.H. Risk of Polypharmacy and Its Outcome in Terms of Drug Interaction in an Elderly Population: A Retrospective Cross-Sectional Study. J. Clin. Med. 2023, 12, 3960. [Google Scholar] [CrossRef]
- Chalasani, S.H.; Syed, J.; Ramesh, M.; Patil, V.; Pramod Kumar, T.M. Artificial intelligence in the field of pharmacy practice: A literature review. Explor. Res. Clin. Soc. Pharm. 2023, 12, 100346. [Google Scholar] [CrossRef]
- Shahmoradi, L.; Safdari, R.; Ahmadi, H.; Zahmatkeshan, M. Clinical decision support systems-based interventions to improve medication outcomes: A systematic literature review on features and effects. Med. J. Islam. Repub. Iran. 2021, 35, 27. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.W.; Levine, D.; Syrowatka, A.; Kuznetsova, M.; Craig, K.J.T.; Rui, A.; Jackson, G.P.; Rhee, K. The potential of artificial intelligence to improve patient safety: A scoping review. NPJ Digit. Med. 2021, 4, 54. [Google Scholar] [CrossRef]
- Sirois, C.; Khoury, R.; Durand, A.; Deziel, P.L.; Bukhtiyarova, O.; Chiu, Y.; Talbot, D.; Bureau, A.; Després, P.; Gagné, C.; et al. Exploring polypharmacy with artificial intelligence: Data analysis protocol. BMC Med. Inform. Decis. Mak. 2021, 21, 219. [Google Scholar] [CrossRef]
- Ryan, R.; Santesso, N.; Lowe, D.; Hill, S.; Grimshaw, J.; Prictor, M.; Kaufman, C.; Cowie, G.; Taylor, M. Interventions to improve safe and effective medicines use by consumers: An overview of systematic reviews. Cochrane Database Syst. Rev. 2014, 2014, Cd007768. [Google Scholar] [PubMed]
- Khan, B.; Fatima, H.; Qureshi, A.; Kumar, S.; Hanan, A.; Hussain, J.; Abdullah, S. Drawbacks of Artificial Intelligence and Their Potential Solutions in the Healthcare Sector. Biomed. Mater. Devices 2023, 1, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Murri, R.; Masciocchi, C.; Lenkowicz, J.; Fantoni, M.; Damiani, A.; Marchetti, A.; Sergi, P.D.A.; Arcuri, G.; Cesario, A.; Patarnello, S.; et al. A real-time integrated framework to support clinical decision making for COVID-19 patients. Comput. Methods Programs Biomed. 2022, 217, 106655. [Google Scholar] [CrossRef] [PubMed]
- Seliaman, M.E.; Albahly, M.S. The Reasons for Physicians and Pharmacists’ Acceptance of Clinical Support Systems in Saudi Arabia. Int. J. Environ. Res. Public Health 2023, 20, 3132. [Google Scholar] [CrossRef] [PubMed]
- Raza, M.A.; Aziz, S. Transformative potential of Artificial Intelligence in pharmacy practice. Saudi Pharm. J. 2023, 31, 101706. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, G.; Singh, S.; Pathania, M.; Gosavi, S.; Abhishek, S.; Parchani, A.; Dhar, M. Artificial intelligence in clinical medicine: Catalyzing a sustainable global healthcare paradigm. Front. Artif. Intell. 2023, 6, 1227091. [Google Scholar] [CrossRef] [PubMed]
- Meid, A.D.; Wirbka, L.; Groll, A.; Haefeli, W.E. Can Machine Learning from Real-World Data Support Drug Treatment Decisions? A Prediction Modeling Case for Direct Oral Anticoagulants. Med. Decis. Mak. 2022, 42, 587–598. [Google Scholar] [CrossRef] [PubMed]
- Chong, L.R.; Tsai, K.T.; Lee, L.L.; Foo, S.G.; Chang, P.C. Artificial Intelligence Predictive Analytics in the Management of Outpatient MRI Appointment No-Shows. Am. J. Roentgenol. 2020, 215, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- Batko, K.; Ślęzak, A. The use of Big Data Analytics in healthcare. J. Big Data 2022, 9, 3. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef]
- Sharma, S.; Rawal, R.; Shah, D. Addressing the challenges of AI-based telemedicine: Best practices and lessons learned. J. Educ. Health Promot. 2023, 12, 338. [Google Scholar] [CrossRef]
- Robinson, C.L.; D’Souza, R.S.; Yazdi, C.; Diejomaoh, E.M.; Schatman, M.E.; Emerick, T.; Orhurhu, V. Reviewing the Potential Role of Artificial Intelligence in Delivering Personalized and Interactive Pain Medicine Education for Chronic Pain Patients. J. Pain. Res. 2024, 17, 923–929. [Google Scholar] [CrossRef]
- Alzahrani, S.A.; Khouja, J.H.; Ghamd, I.S.; Alotaybi, M.; Bargawi, A.; Alghamdi, A.A.; Fayraq, A.; Ghamdi, S. Telemedicine Acceptability among Patients of Primary Health Care Clinics in the Western Region, Saudi Arabia. Cureus 2023, 15, e40857. [Google Scholar] [CrossRef]
- Zhang, X.; Ma, L.; Sun, D.; Yi, M.; Wang, Z. Artificial Intelligence in Telemedicine: A Global Perspective Visualization Analysis. Telemed. J. e-Health 2024. ahead of print. [Google Scholar] [CrossRef]
- Ftouni, R.; AlJardali, B.; Hamdanieh, M.; Ftouni, L.; Salem, N. Challenges of Telemedicine during the COVID-19 pandemic: A systematic review. BMC Med. Inform. Decis. Mak. 2022, 22, 207. [Google Scholar] [CrossRef] [PubMed]
- Alotaibi, F.M.; Bukhamsin, Z.M.; Alsharafaa, A.N.; Asiri, I.M.; Kurdi, S.M.; Alshayban, D.M.; Alsultan, M.M.; Almalki, B.A.; Alzlaiq, W.A.; Alotaibi, M.M. Knowledge, Attitude, and Perception of Health Care Providers Providing Medication Therapy Management (MTM) Services to Older Adults in Saudi Arabia. Healthcare 2023, 11, 2936. [Google Scholar] [CrossRef]
- Damiani, G.; Altamura, G.; Zedda, M.; Nurchis, M.C.; Aulino, G.; Heidar Alizadeh, A.; Cazzato, F.; Della Morte, G.; Caputo, M.; Grassi, S.; et al. Potentiality of algorithms and artificial intelligence adoption to improve medication management in primary care: A systematic review. BMJ Open 2023, 13, e065301. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, T.; Ceyhan, Ş.; Akyön, Ş.H.; Yılmaz, T.E. Enhancing Primary Care for Nursing Home Patients with an Artificial Intelligence-Aided Rational Drug Use Web Assistant. J. Clin. Med. 2023, 12, 6549. [Google Scholar] [CrossRef] [PubMed]
- Al-Baity, H.H. The artificial intelligence revolution in digital finance in Saudi Arabia: A comprehensive review and proposed framework. Sustainability 2023, 15, 13725. [Google Scholar] [CrossRef]
- Yelne, S.; Chaudhary, M.; Dod, K.; Sayyad, A.; Sharma, R. Harnessing the Power of AI: A Comprehensive Review of Its Impact and Challenges in Nursing Science and Healthcare. Cureus 2023, 15, e49252. [Google Scholar] [CrossRef]
- Akyon, S.H.; Akyon, F.C.; Yılmaz, T.E. Artificial intelligence-supported web application design and development for reducing polypharmacy side effects and supporting rational drug use in geriatric patients. Front. Med. 2023, 10, 1029198. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsanosi, S.M.; Padmanabhan, S. Potential Applications of Artificial Intelligence (AI) in Managing Polypharmacy in Saudi Arabia: A Narrative Review. Healthcare 2024, 12, 788. https://doi.org/10.3390/healthcare12070788
Alsanosi SM, Padmanabhan S. Potential Applications of Artificial Intelligence (AI) in Managing Polypharmacy in Saudi Arabia: A Narrative Review. Healthcare. 2024; 12(7):788. https://doi.org/10.3390/healthcare12070788
Chicago/Turabian StyleAlsanosi, Safaa M., and Sandosh Padmanabhan. 2024. "Potential Applications of Artificial Intelligence (AI) in Managing Polypharmacy in Saudi Arabia: A Narrative Review" Healthcare 12, no. 7: 788. https://doi.org/10.3390/healthcare12070788




