Abstract
Interprofessional collaborative practice is a core competency and is the key to strengthening health practice systems in order to deliver safe and high-quality nursing practice. However, there is no Interprofessional Collaboration Practice Competency Scale (IPCPCS) for clinical nurses in Taiwan. Therefore, the purposes of this study were to develop an IPCPCS and to verify its reliability and validity. This was a psychometric study with a cross-sectional survey using convenience sampling to recruit nurses from the seven hospitals of a medical foundation. A self-designed structured IPCPCS was rolled out via a Google survey. The data were analyzed using descriptive statistics, principal-axis factoring (PAF) with Promax rotation, Pearson correlation, reliability analysis, and one-way ANOVA. PAF analysis found that three factors could explain 77.76% of cumulative variance. These were collaborative leadership and interprofessional conflict resolution, interprofessional communication and team functioning, and role clarification and client-centered care. The internal consistency of the three factors (Cronbach’s α) was between 0.970 to 0.978, and the Pearson correlation coefficients were between 0.814 to 0.883. Significant differences were presented in the IPCPCS score by age, education level, total years of work experience, position on the nursing clinical ladder, and participation in interprofessional education. In conclusion, the three factors used in the IPCPCS have good reliability and construct validity. This scale can be used as an evaluation tool of in-service interprofessional education courses for clinical nurses.
1. Introduction
The ultimate goal of modern healthcare is to deliver patient-centered, holistic care of the highest quality. Interprofessional collaborative practice (IPCP) has emerged as the premier strategy for achieving this goal. The Institute of Medicine (IOM), in its 2003 report, underscored the importance of IPCP in enhancing patient safety and healthcare quality [1]. This focus was amplified by the IOM’s 1999 report, “To Err is Human”, which identified medical errors as a major global healthcare challenge, thereby stressing the need for safer healthcare practices [2]. A pivotal change required in healthcare institutions is the promotion of interprofessional collaboration. Training healthcare professionals in teamwork is essential in efforts to foster interprofessional collaborative care, which in turn improves patient safety [2].
The IOM has delineated five core competencies necessary for healthcare professionals to deliver standard medical care: patient-centered care, evidence-based practice, information technology, quality improvement, and interprofessional teamwork [1]. IPCP fosters communication across different professional domains, facilitating mutual learning and the development of innovative problem-solving strategies. This approach promotes a patient-centered care ethos, minimizes resource wastage, and enhances the quality of medical care [3].
Furthermore, in 2010, the World Health Organization (WHO) defined IPCP as a collaborative effort involving healthcare workers from diverse backgrounds, along with patients, families, caregivers, and communities, with an aim to provide comprehensive, high-quality care [4]. This innovative model necessitates a clear understanding of each participant’s role, encouraging learning from and contribution to the team, as well as the sharing of responsibilities, and is considered the core and soul of healthcare [5,6].
IPCP plays a crucial role in improving the accessibility of health interventions, strengthening interdepartmental coordination, and enhancing the job satisfaction of healthcare professionals [4,5]. For patients, IPCP has numerous positive health-related outcomes. According to a scoping review by Lutfiyya et al. (2019) [7], these benefits include well-managed chronic diseases, reduced surgery costs, improved communication between care providers, and increased patient satisfaction, among others [7]. For nursing staff, effective teamwork and communication can increase job satisfaction [8].
The identification of competencies, as highlighted by Ten Cate O (2006), is a crucial initial step in preparing future healthcare providers to deliver high-quality care [9]. In response, the World Health Organization, along with the Interprofessional Education Collaborative (IPEC) and the Canadian Interprofessional Health Collaborative (CIHC), proposed core IPCP competencies for adoption by medical education-related research institutions [1,5,10,11]. IPEC’s four IPCP core competencies are values/ethics for interprofessional practice, roles/responsibilities, interprofessional communication, and teams and teamwork [1,10]. The six dimensions proposed by CIHC are role clarification (RC), patient/client/family/community-centered care (CC), interprofessional communication (IC), team functioning (TF), collaborative leadership (CL), and interprofessional conflict resolution (ICR) [5,11].
Working based on the concepts of IPEC or CIHC, many international scholars have continued to develop IPCP assessment tools. The assessment targets different clinical practitioners or single professions, diverse clinical practitioners and healthcare professional students, and students in different healthcare professions. The scale is mainly used for self-assessment but rarely for observer use in the assessment of clinical practitioners. Even the IPCP assessments among different clinical practitioners or patients within an organization are also scarce (Table S1) [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47]. Furthermore, there are several outcome measurement instruments for evaluating competency in interprofessional collaboration practice [48,49]. These IPCP assessment tools, depending on their measurement purposes, are used in different healthcare contexts and for different subjects. Although each tool has advantages and disadvantages, earlier tools had methodological issues related to psychometric tests. For instance, Peltonen et al. (20) pointed out in their scoping review that the psychometric parameters of 29 tools were non-systematic, focusing primarily on construct validity and internal consistency. They suggested that further extensive testing and confirmatory studies should be performed to strengthen the evidence of the reliability and validity of these tools [48]. Moreover, Glover et al. (2022) identified similar issues in their systematic review of outcome measurement instruments. Only ATICS-II was rated as having sufficient measurement characteristics, with low- to moderate-quality evidence, and further validation of each outcome measurement instrument, including relevance, comprehensibility, and comprehensiveness, is needed [49]. Considering the differences in healthcare contexts and cultures across countries, Edelbring et al. (2018) argue that caution should be exercised in the conceptualization and wording of scales during localization and translation [43].
Cultivating competence in “interprofessional collaborative practice” and examining the implementation of IPCP among healthcare personnel are the best educational and summative assessment methods for interprofessional education (IPE) [50], leading to the best outcomes in terms of patient-centered care [1]. Since 2007, Taiwan’s Ministry of Health and Welfare has promoted a subsidy program for teaching hospitals to train novice medical personnel in IOM core competencies. Undergoing continuous medical-quality education in teaching hospitals, particularly in the “Two-Year Nurse Post-Graduate Year (NPGY) Training Program” [51], mandates participation in interprofessional team collaboration care-related activities (IPE) during the second (4–12 months) and third stages (13–24 months) of the program. This policy fosters the effective implementation of IPCP, laying the groundwork for Taiwanese medical care institutions to aim for patient-centered holistic medical care. Although the importance of IPCP in medical care has been noted, there is still a lack of valid and reliable tools for assessing IPCP competencies among clinical nurses on different clinical nursing ladders in Taiwan. The dimensions of leadership and conflict management are missed by many IPCP scales [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47]. Since the importance and necessity of IPCP competencies among nursing staff are acknowledged, clinical nurses, as members of interprofessional teams, should possess IPCP capabilities [42], promote patient safety and care quality [7], and achieve the goal of holistic care as a crucial aspect of nursing practice. Considering these challenges, our study aims to develop and validate a theoretically based self-assessment tool for evaluating the “Interprofessional Collaborative Practice Competency” among clinical nurses in Taiwan. This initiative addresses the critical need for a valid and reliable IPCP competency assessment tool in the Taiwanese healthcare context, supporting the advancement of patient safety and care quality through enhanced nursing practice.
2. Materials and Methods
2.1. Study Design
This was a psychometric study with a cross-sectional survey using a self-designed structured scale.
2.2. Participants and Setting
The study was based on a convenience sample of clinical nurses from seven hospital districts of a medical foundation in Taiwan. The inclusion criteria were registered nurses who were willing to fill out the questionnaire and agreed to participate in the study program. The exclusion criteria were medical personnel in non-nursing occupations. The sample size was calculated using the Creative Research System (2012) sample-size estimator with a confidence interval set at 95%, a confidence level set at 4, and a population of 566 based on approximately 10,000 registered professional nurses [52].
2.3. Instruments
The tools used in this study consisted of two parts. The first part was sociodemographic and professional characteristics, including gender, age, education level, hospital district, years of work experience, place on the nursing clinical ladder, qualification as a clinical instructor, and training experience in interprofessional education (IPE). The second part was the score achieved on the Interprofessional Collaborative Practice Competence Scale (IPCPCS) based on the six competency structures of the CIHC [5,11], as shown in Table S2. After receiving approval from the CIHC team, two experts with nursing backgrounds and doctoral degrees, who had lived in English-speaking countries for more than 5 years, conducted English-to-Chinese forward translation and Chinese-to-English back translation of the questionnaires [53,54], considering the cultural and language differences between Chinese and English questions. The original IPCPCS has 41 questions with 6 dimensions, including role clarification, patient/client/family/community-centered practice, interprofessional communication, team functioning, collaborative leadership, and interprofessional conflict resolution. A 7-point Likert scale was used, with responses on a scale with 1 indicating “No ability”; 2 indicating “Inadequate ability”; 3 designating “Somewhat inadequate ability”; 4 indicating “Ability satisfied or meeting minimal requirements”; 5 indicating “Fair ability”; 6 showing “Good ability”; and 7 sjowing “Excellent ability”. Possible total scores ranged from 42 to 210, with higher scores indicating greater holistic practice competence in terms of interprofessional collaboration.
After the questionnaire was drafted, a total of five experts in related fields in Taiwan (1 physician, 1 associate professor, 1 director of the Nursing Department, and 2 experts specializing in nursing and health practice education) were invited to perform expert content validity evaluation. The experts rated the relevance of the questions to the study’s purpose by using a four-point Likert scale (4 = appropriate; 3 = requiring minor modification; 2 = requiring major modification; and 1 = inappropriate) to calculate the content validity index (CVI) and quantify expert validity [53]. The questionnaire was modified according to the expert’s recommendations and the modified research tools had 41 questions.
2.4. Procedure
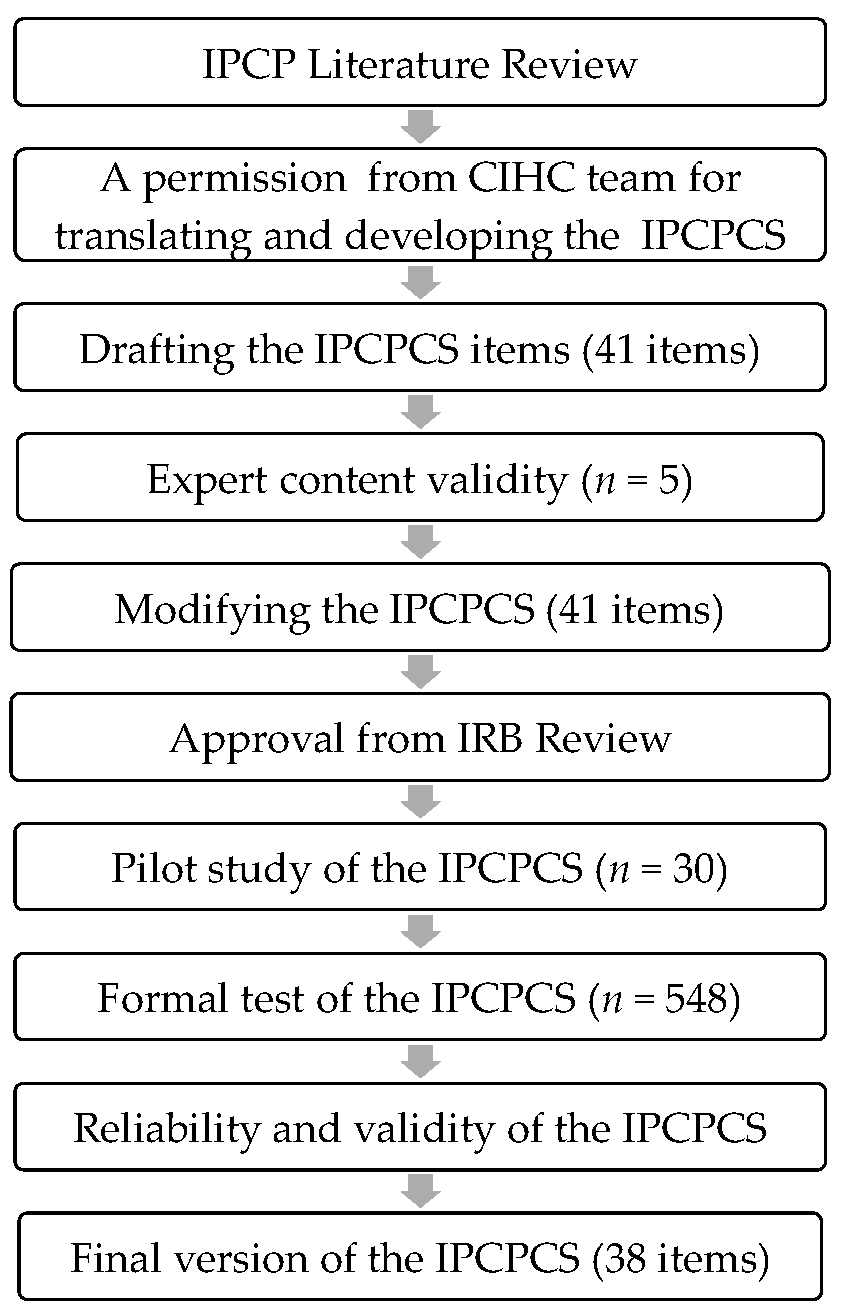
Figure 1 presents the flow of this study. Based on the literature [53,54], the English-to-Chinese and Chinese-to-English translations took cultural differences into consideration. A 41-question survey was constructed along six dimensions. Five experts were commissioned to conduct an expert content validity evaluation, and the content of the questions was modified according to their comments. After obtaining approval from the IRB, a pilot test was conducted in a hospital district. As there were no changes in the content of the questionnaires, the project investigator (PI) of the study sent a study recruitment poster and a QR code link to the responsible supervisors of seven hospital districts. After obtaining approval from supervisors, the poster and link were forwarded to the head nurses, and then the head nurses distributed the study’s instructions and the survey QR code URL to the clinical nurses. The Google online link-based questionnaire was distributed from 5 February 2022 to 30 November 2022 to conduct a formal test. Then, the reliability and validity of this tool were analyzed.
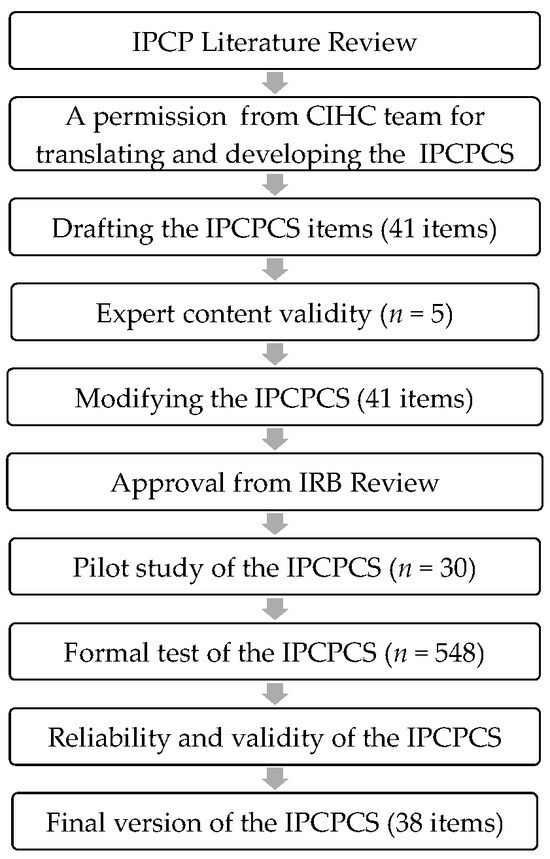
Figure 1.
Study procedure.
2.5. Ethical Considerations
This study was conducted in compliance with the basic human rights of the participants, safety standards, and research ethics and was approved by the Institutional Review Board of the Chang Gung Medical Foundation (202102065A3). Consent was obtained from all participants. Personal information was handled with anonymous numbering and kept strictly confidential to protect the privacy of the subjects.
2.6. Data Processing and Statistical Analysis
The results of the questionnaire were automatically saved in Google Forms and downloaded into the 2016 version of our Excel database after the study’s deadline date to examine the accuracy of the data. The SPSS 22.0 Statistical Package (IBM, Armonk, NY, USA) was used for the assumption testing and data analysis. Assumption testing included normality, linearity, outliers, and multicollinearity. Data analysis used descriptive statistics to present the sociodemographic and professional characteristics of participants and the distribution of scales in terms of value, percentage, mean, median, and standard deviation. Reliability analysis was performed to assess the internal consistency of the IPCPCS. Principal-axis factoring analysis was conducted with Promax rotation to determine validity based on initial eigenvalues (≥1), factor loadings (>0.40), and scree plots [55,56,57]. One-way analysis of variance (ANOVA) was applied to check the mean differences between the total IPCPCS scores by examining the sociodemographic and professional characteristics of the participants, with a p < 0.05 two-tailed test result indicating statistical significance. Pearson correlation was applied to analyze the relationship between the factors for the IPCPCS.
3. Results
In this study, 578 questionnaires were collected. The fill-in rate was 97.9%. Winsorizing was used to remove 5 extreme values, and the final statistical analysis was conducted with 548 valid questionnaires.
3.1. Sociodemographic and Professional Characteristics of the Participants
Most of the participants were female (96.7%). The most common age group was 26 to 30 years (22.6%), with a mean age of 34.48 (SD = 7.87). Moreover, 84.3% of the participants had a bachelor’s degree in nursing. The most common work experience group was 5.1 to 10 years (29.9%), with a mean of 11.08 (SD = 7.80). Most of the participants (25.0%) were of rank N2. Of all the nurses, 74.3% had clinical teaching qualifications, and 51.1% had experience with IPE, as shown in Table 1.

Table 1.
Sociodemographic and professional characteristics of the participants (n = 548).
3.2. Content Validity
The S-CVI of this research tool was 0.76 and its I-CVI was 0.94.
3.3. Construct Validity—Principal-Axis Factoring of the Exploratory Factor Analysis
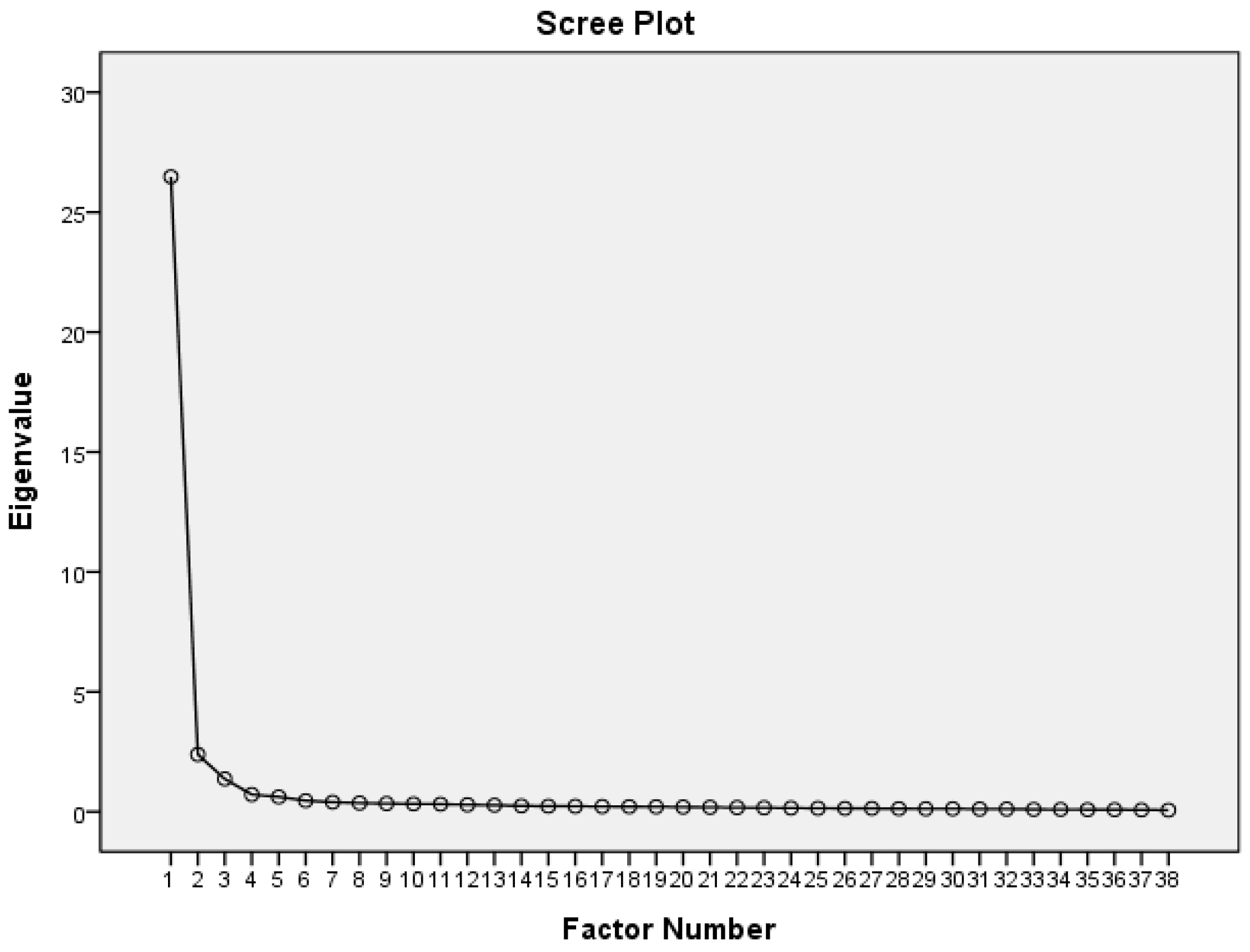
We employed principal-axis factoring analysis for factor extraction of the scale, followed by a Promax rotation. After the sequential removal of one item due to multicollinearity (ICR5) and two items with factor loadings below 0.40 (TF1 and TF3), the final scale comprised 38 items. The overall Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy was exceptionally high at 0.983, and Bartlett’s test of sphericity was significant (χ2(703) = 29, 303.47, p < 0.001). The measure of sampling adequacy (MSA) of individual items ranged from 0.975 to 0.989. The scree plot illustrates three factors (Figure 2).
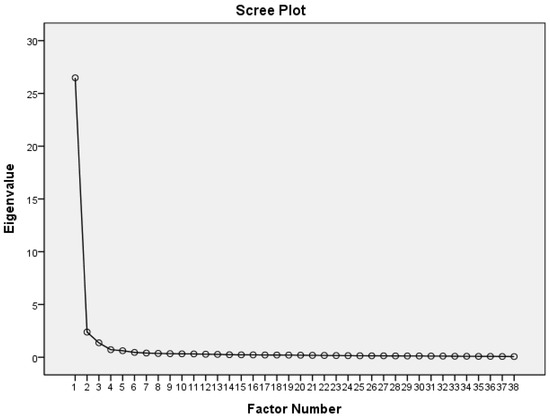
Figure 2.
Scree plot of the IPCPCS.
Table 2 shows that the eigenvalues of Factor 1 to Factor 3 after Promax rotation were 26.26, 2.16, and 1.13, respectively, explaining 69.11%, 5.69%, and 2.97% of the variance. The explainable cumulatively variance was 77.76%. As delineated in Appendix A (Table A1), the three factors of the scale were termed: Factor 1—collaborative leadership and interprofessional conflict resolution (CLICR, 13 items); Factor 2—interprofessional communication and team functioning (ICTF, 12 items); and Factor 3—role clarification and client-centered care (RCCC, 13 items).

Table 2.
Total variance explained by the three factors of the IPCPCS (n = 548).
3.4. Construct Validity—Contrasted Groups Methods
Assessed using ANOVA, age (p = 0.001), education level (p = 0.002), total years of work experience (p < 0.000), nursing clinical ladder (p < 0.000), and prior participation in an interprofessional education (p < 0.000) by clinical nurses produced significant differences in the IPCPCS score (Appendix A, Table A2).
3.5. Internal Consistency Reliability
Table A1 (Appendix A) shows that Cronbach’s for the three factors and the overall scale was greater than 0.970, with Cronbach’s of the overall scale being 0.988. Table 3 displays Pearson’s two-tailed correlation analysis, showing significant positive correlations among the three factors (p < 0.01).

Table 3.
Pearson correlation coefficients between the three factors of the IPCPCS (n = 548).
4. Discussion
The primary aim of this study was to develop and validate the Interprofessional Collaborative Practice Competency Scale (IPCPCS). This study was grounded in the Canadian Interprofessional Health Collaborative (CIHC) framework, which outlines six major areas of competency regarding interprofessional collaboration. The process of scale development encompassed the confirmation of the core competency framework, the design of scale items, and the assessment of content validity, construct validity, and internal consistency. The results validated the scale as a reliable and effective tool for assessing nurses’ IPCPCS scores.
4.1. Sociodemographic and Professional Characteristics of the Participants
The participants in our study were all clinical nurses, with an average age of 34.48. Most of the participants had a bachelor’s degree, and the average years of work experience was 11.08. Approximately 63% of the nurses held level N3 or above, and the majority of participants were qualified as clinical nursing instructors (74.3%). However, only 51.1% had participated in IPE training, indicating the necessity of IPCP training regardless of work experience.
4.2. Content Validity
For content validity, the appropriateness of each item content and direction was assessed by experts, and the results achieved an ideal level (S-CVI = 0.76 & I-CVI = 0.94), indicating good individual item values and the overall validity of the scale’s content [54].
4.3. Construct Validity—Principal-Axis Factoring of the Exploratory Factor Analysis
Construct validity was examined using principal-axis factoring from exploratory factor analysis with Promax rotation. The overall Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy, individual Measures of Sampling Adequacy (MSA), and Bartlett’s test of sphericity were significant, indicating that the data were highly suitable for use in factor analysis [57]. The factor loadings of the items in the scale ranged from 0.44 to 0.97. For exploratory factors, the minimum standard for factor loading should be greater than 0.3, and a score above 0.55 is considered good [56].
In the literature, the validation of IPCP competencies predominantly references the IPEC and CIHC competency frameworks. Our analysis indicates that the various dimensions of interprofessional collaboration competencies, initially encompassed by six dimensions, were reduced to three factors after factor analysis, which is supported by other scholars’ research findings [5,11,18,21,26,28,39,43,44,47]. Our study found that nurses’ self-assessment based the three dimensions of the IPCPCS were highest in ICTF, which is followed by RCCC, and lowest in CLICR. Unlike IPC [22], CICS29 [25,30], JASSIC [34], and IPC-Thailand [32], the factors of leadership and conflict management were not mentioned. Recent empirical literature found that clear role functions and leadership, which have significant implications for IPCP core competencies, are influential factors in effective team collaboration [59]. Nursing education should incorporate basic concepts of IPCP core competencies, such as leadership and management skills in clinical nursing education. Understanding roles and responsibilities in IPCP is crucial for enabling novice nurses to perform leadership roles within collaborative teams, advocate for patients, and promote patient safety and care quality [60,61].
4.4. Construct Validity—Contrasted Groups Methods
The study found significant differences in IPCPCS values among nurses based on age, educational level, total years of work experience, clinical nursing ladder, and IPE participation. The differences may be due to nurses being aged ≥ 46 years, holding senior positions or being higher up the nursing ladder, and having participated in the IPE, resulting in their scoring higher in the IPCPCS. Nurses with postgraduate degrees were caring and possessed critical thinking and reasoning aptitudes, professional nursing skills, communication and teamwork abilities, ethics, the attribute of responsibility, and lifelong learning capabilities. Therefore, they had higher IPCPCS scores. The literature confirms that learning experiences, age, participation in IPE training, and management experience positively affect the IPCP [62], and scholars point out that interprofessional education (IPE) programs are the first step in implementing the IPCP [63]. Recent intervention studies have shown that interprofessional simulation education can help novice nurses to improve core nursing competencies [64]. Moreover, scholars have noted that current nursing educators are still underprepared for teaching IPCP, which affects the IPCP capabilities of novice nurses [65]. The ability to engage in interprofessional collaborative practice is a dynamic development for learners and practitioners, with each competency continuously evolving throughout an individual’s professional career and being honed in the ever-changing practice/learning environment [66]. Therefore, prospective nursing undergraduate teachers, curricula, and newly graduated clinical trainees should implement interprofessional simulation training programs to enhance clinical performance and effective collaboration in the healthcare system, thus providing quality and safe care.
4.5. Internal Consistency Reliability
Regarding reliability testing, the reliabilities of the internal consistency of the three core competencies of the IPCPCS were 0.978, 0.976, and 0.970, respectively, with all values exceeding the high-reliability threshold of 0.8. Scholars have noted that Cronbach’s α is the most commonly referenced value, with higher values indicating better reliability, which is generally recommended to maintain values above 0.70 [67]. Thus, the scale used in this study had good internal consistency, demonstrating the reliability of the scale.
4.6. Limitations
This study has some limitations. First, this study was a preliminary psychometric validation of a questionnaire. Although the sample size was sufficient for exploratory factor analysis (EFA), the sample size was inadequate for use in confirmatory factor analysis (CFA) testing [68,69]. Future research could conduct CFA to confirm the domains and the overall model fit to determine construct validity. Second, the fact that the overwhelming majority of participants were female could limit the generalizability of the findings when applied to a more gender-diverse population. Third, the self-reported nature of the questionnaire could introduce bias, as participants might provide socially desirable answers. Fourth, the study’s cross-sectional design also prevents causal inferences, and the specific context of Taiwan’s healthcare system may limit the applicability of its findings in different cultural or healthcare settings. Finally, the 38-item questionnaire might affect participants’ willingness to complete the scale and the authenticity of their responses.
5. Conclusions
This study has demonstrated the IPCPCS’s validity and reliability in assessing the competencies essential to achieving effective interprofessional collaboration. The three identified core competencies, including collaborative leadership and interprofessional conflict resolution (CLICR), interprofessional communication and team functioning (ICTF), and role clarification and client-centered care (RCCC), explained 77.76% of the total cumulative variance, providing a comprehensive framework for understanding and enhancing interprofessional collaboration among clinical nurses.
Given the scale’s robust psychometric properties, it can serve as a valuable tool in both educational and clinical settings, assisting in efforts to foster a culture of collaborative practice. Future research should conduct criterion-related validity, convergent validity, and discriminant validity studies, and the development of a shorter IPCPC scale for use in nursing is needed. There is also a need for qualitative analysis and long-term tracking to better understand the trends of nurses in IPCP in overall nursing, which may confirm the teaching and learning effectiveness of interprofessional education (IPE). Moreover, we should aim to validate the IPCPCS across different contexts and explore interventions to improve IPCPCS scores, thereby enhancing patient care quality through improved interprofessional collaboration.
In conclusion, the IPCPCS offers a theoretically grounded and empirically validated tool for use in measuring and improving interprofessional collaboration competencies, paving the way for more effective, patient-centered healthcare delivery.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare12070806/s1, Table S1: IPCP instruments; Table S2: IPCP six competency domains and definitions vs. IPCPCS three domains.
Author Contributions
Conceptualization, Y.-F.C., Y.-P.T. and S.-I.H.; methodology, Y.-F.C. and S.-I.H.; formal analysis, Y.-F.C. and S.-I.H.; investigation, Y.-F.C. and Y.-P.T.; resources, Y.-P.T., S.-L.Y., M.-C.C., C.-C.H., C.-T.L., S.-T.H., S.-H.C. and M.-N.L.; data curation, Y.-P.T., S.-L.Y., M.-C.C., C.-C.H., C.-T.L., S.-T.H. and S.-H.C.; writing—original draft preparation, Y.-F.C. and S.-I.H.; writing—review and editing, Y.-F.C. and S.-I.H.; project administration, Y.-F.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Chang Gung Medical Foundation (No. 202102065A3, 2 February 2022) for studies involving humans.
Informed Consent Statement
The purpose, procedures, and methods of data collection were presented in an easily comprehensible manner on the first page of the online survey site. The website also clearly stated that participation was entirely voluntary, and the participants had the right to discontinue taking the survey or refuse to respond to the questionnaire. The page also included the contact details of the researchers and explained that no data would be included in the analysis if the subject dropped out of the survey, and that there would be no disadvantage caused by withdrawal from or rejection of the survey.
Data Availability Statement
The data are not publicly available due to ethical restrictions.
Acknowledgments
We thank the registered professional nurses who participated in this study. We thank ICHC & Carole Orchard for contributing to IPCP.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Results of exploratory factor analysis using principal-axis factoring analysis with Promax rotation (n = 548).
Table A1.
Results of exploratory factor analysis using principal-axis factoring analysis with Promax rotation (n = 548).
| Factors and Items | Mean | SD | Min | Max | Pattern Matrix | Structure Matrix | Corrected Item—Total Correlation |
|---|---|---|---|---|---|---|---|
| Factor 1: Collaborative leadership and interprofessional conflict resolution (Cronbach α = 0.978) | 72.52 | 10.63 | 38 | 91 | |||
| ICR6. I can effectively solve disputes among teammates, including analyzing causes of conflict and achieving acceptable solutions. | 5.58 | 0.90 | 3 | 7 | 1.029 | 0.885 | 0.853 |
| ICR3. I can identify common scenes which may lead to disputes or conflicts, including roles, ambiguity, power gradients and different goals. | 5.45 | 0.93 | 3 | 7 | 0.973 | 0.905 | 0.881 |
| ICR4. I understand conflict-solving strategies. | 5.43 | 0.96 | 2 | 7 | 0.955 | 0.900 | 0.877 |
| ICR7. I can arrange atmosphere allowing for different feedback. | 5.40 | 0.97 | 1 | 7 | 0.940 | 0.860 | 0.833 |
| ICR8. I can make all members listen to others’ viewpoints to form a consensus. | 5.39 | 0.98 | 2 | 7 | 0.819 | 0.862 | 0.848 |
| ICR2. I am aware of the possibility of conflict and take informed steps to solve it. | 5.53 | 0.93 | 2 | 7 | 0.800 | 0.895 | 0.891 |
| CL4. I can enable effective decision making by members. | 5.60 | 0.93 | 2 | 7 | 0.746 | 0.894 | 0.897 |
| CL7. I can apply skills of coordination/integrative strategies. | 5.62 | 0.92 | 1 | 7 | 0.705 | 0.874 | 0.876 |
| CL8. I can make use of continuous quality-improving principles in the process of interprofessional practice. | 5.66 | 0.92 | 2 | 7 | 0.698 | 0.877 | 0.880 |
| CL3. I can facilitate effective operation among teammates. | 5.67 | 0.88 | 2 | 7 | 0.651 | 0.889 | 0.895 |
| CL6. I can create ways of sharing work with teammates. | 5.74 | 0.87 | 3 | 7 | 0.597 | 0.866 | 0.875 |
| ICR1. I find positive implications behind the conflict of a team. | 5.72 | 0.88 | 3 | 7 | 0.580 | 0.834 | 0.841 |
| CL2. I can facilitate working relationships via collaboration with teammates. | 5.75 | 0.87 | 3 | 7 | 0.536 | 0.861 | 0.871 |
| Factor 2: Interprofessional communication and team functioning (Cronbach α = 0.976) | 70.92 | 8.92 | 45 | 84 | |||
| IC2. I can listen teammates’ opinions on caring for clients. | 6.04 | 0.81 | 4 | 7 | 0.944 | 0.914 | 0.890 |
| IC1. I can abide by teamwork communication principles. | 6.07 | 0.83 | 4 | 7 | 0.917 | 0.895 | 0.882 |
| TF7. I follow the ethical principles of a team (such as confidentiality). | 6.17 | 0.86 | 4 | 7 | 0.914 | 0.818 | 0.783 |
| IC4. I can develop trusted relationships with cases/families and other interprofessional members. | 5.92 | 0.83 | 3 | 7 | 0.785 | 0.913 | 0.911 |
| TF2. I can show respect to the ethical values of teammates during work as a team. | 5.94 | 0.84 | 3 | 7 | 0.768 | 0.861 | 0.855 |
| IC3. I can communicate with interprofessional teammates to come to agreement on practice strategy for application to clients. | 5.91 | 0.83 | 2 | 7 | 0.709 | 0.891 | 0.893 |
| TF4. I show my respect for any practice strategies coordinated/integrated by teammates. | 5.85 | 0.83 | 4 | 7 | 0.707 | 0.873 | 0.872 |
| IC5. I can effectively make use of information and communication skills to improve client-centered practice. | 5.84 | 0.83 | 3 | 7 | 0.600 | 0.871 | 0.884 |
| TF6. I can build and maintain trustful relationships with teammates, clients, and families. | 5.83 | 0.84 | 3 | 7 | 0.543 | 0.863 | 0.876 |
| CL1. I can cooperate with teammates to show client outcomes on caring for clients. | 5.82 | 0.82 | 3 | 7 | 0.523 | 0.855 | 0.860 |
| CL5. I can build a cooperative atmosphere with teammates. | 5.81 | 0.86 | 3 | 7 | 0.494 | 0.830 | 0.826 |
| TF5. I can reflect on interactions among teammates, clients and families. | 5.72 | 0.85 | 3 | 7 | 0.444 | 0.832 | 0.855 |
| Factor 3: Role clarification and client-centered care (Cronbach α = 0.970) | 74.61 | 9.82 | 48 | 91 | |||
| RC1. I am clear that interprofessional teammates provide care for individual cases. | 5.54 | 0.93 | 3 | 7 | 0.756 | 0.798 | 0.776 |
| RC4. I can clarify roles and functions with appropriate language. | 5.70 | 0.87 | 3 | 7 | 0.754 | 0.845 | 0.830 |
| RC5. I can learn from other teammates’ knowledge and capabilities through discussion. | 5.73 | 0.88 | 3 | 7 | 0.750 | 0.872 | 0.861 |
| RC6. I can consider other teammates’ roles to make sure the professional roles in this team are filled. | 5.74 | 0.89 | 3 | 7 | 0.749 | 0.878 | 0.868 |
| RC2. I show my respect for the difference of roles and function among teammates. | 5.94 | 0.91 | 3 | 7 | 0.693 | 0.799 | 0.783 |
| RC3. I can perform my own roles in a way that shows respect for the culture. | 5.93 | 0.88 | 3 | 7 | 0.684 | 0.834 | 0.821 |
| RC7. I can integrate roles and capabilities in a service capacity. | 5.47 | 0.94 | 3 | 7 | 0.656 | 0.801 | 0.787 |
| CC1. I can cooperate with teammates to provide care planning, execution, and evaluation. | 5.65 | 0.87 | 3 | 7 | 0.577 | 0.845 | 0.857 |
| CC2. I can show my respect for and encourage clients and their families to express their choices of strategy. | 5.85 | 0.85 | 4 | 7 | 0.561 | 0.839 | 0.853 |
| CC4. I can provide care by listening to all teammates as they express their opinions on care. | 5.90 | 0.86 | 3 | 7 | 0.558 | 0.838 | 0.852 |
| CC3. I can ensure that other teammates provide appropriate education and support to clients and their families involved in care. | 5.65 | 0.88 | 3 | 7 | 0.539 | 0.835 | 0.852 |
| CC5. The care that I have provided is based on continuous therapeutic relationships. | 5.79 | 0.83 | 3 | 7 | 0.471 | 0.815 | 0.839 |
| CC6. I can provide individualized care based on individual needs and values. | 5.73 | 0.85 | 3 | 7 | 0.445 | 0.811 | 0.837 |
| Total score | 218.06 | 27.83 | 137 | 266 |
Note. Factor > 0.40, SD, Standard Deviation; Min, Minimum; Max, Maximum.

Table A2.
Mean differences in the IPCPCS scores by participants’ background characteristics (n = 548).
Table A2.
Mean differences in the IPCPCS scores by participants’ background characteristics (n = 548).
| Variables | n (%) | Mean (SD) | One-Way ANOVA | p Value | Scheff Post Hoc Analysis | p Value |
|---|---|---|---|---|---|---|
| Age (full) | F(5, 542) = 4.29 | 0.001 | ||||
| ➀ 20–25 | 77 (14.1) | 214.86 (27.97) | ➅ > ➂ | 0.044 | ||
| ➁ 26–30 | 124 (22.6) | 219.68 (28.06) | ➅ > ➃ | 0.012 | ||
| ➂ 31–35 | 117 (21.4) | 214.50 (27.69) | ||||
| ➃ 36–40 | 100 (18.2) | 212.03 (26.12) | ||||
| ➄ 41–45 | 77 (14.1) | 223.73 (27.52) | ||||
| ➅ 46–60 | 53 (9.7) | 229.91 (26.74) | ||||
| Educational level | F(2, 545) = 6.35 | 0.002 | ||||
| ➀ Occupational high school/junior college | 56 (10.2) | 214.45 (29.63) | ➂ > ➀ | 0.004 | ||
| ➁ University | 462 (84.3) | 217.39 (27.54) | ➂ > ➁ | 0.003 | ||
| ➂ ≥ Master’s degree | 30 (5.5) | 235.10 (23.65) | ||||
| Years of working experience | F(4, 543) = 6.29 | <0.001 | ||||
| ➀ <5 years | 133 (24.3) | 215.35 (30.15) | ➄ > ➀ | 0.001 | ||
| ➁ 5.1–10 years | 164 (29.9) | 216.99 (26.98) | ➄ > ➁ | 0.004 | ||
| ➂ 10.1–15 years | 106 (19.3) | 213.70 (26.06) | ➄ > ➂ | 0.001 | ||
| ➃ 15.1–20 years | 62 (11.3) | 215.97 (29.05) | ➄ > ➃ | 0.021 | ||
| ➄ ≥21 years | 83 (15.1) | 231.64 (23.03) | ||||
| Nursing clinical ladder | F(6, 541) = 4.69 | <0.001 | ||||
| ➀ ≤N1 | 67 (12.2) | 212.85 (28.25) | ➅ > ➀ | 0.004 | ||
| ➁ N2 | 137 (25.0) | 215.29 (30.66) | ➅ > ➁ | 0.003 | ||
| ➂ N3 | 122 (22.3) | 215.75 (28.76) | ➅ > ➂ | 0.006 | ||
| ➃ N4 | 108 (19.7) | 216.34 (25.38) | ➅ > ➃ | 0.011 | ||
| ➄ AHN | 52 (9.5) | 224.13 (19.88) | ||||
| ➅ HN | 50 (9.1) | 235.48 (21.40) | ||||
| ➆ NP | 12 (2.2) | 218.67 (31.08) | ||||
| Has ever joined interprofessional collaborative practice trainings? | F(1, 546) = 13.96 | <0.001 | ||||
| 🄋 No | 268 (48.9) | 213.57 (28.74) | ||||
| ➀ Yes | 280 (51.1) | 222.35 (26.28) |
References
- Ann, C.G.; Knebel, E. Health Professions Education: A Bridge to Quality; National Academies Press: Washington, DC, USA, 2003. [Google Scholar]
- Institute of Medicine. To Err Is Human: Building a Safer Health System; The National Academies Press: Washington, DC, USA, 2000. [Google Scholar]
- Green, B.N.; Johnson, C.D. Interprofessional Collaboration in Research, Education, and Clinical Practice: Working Together for a Better Future. J. Chiropr. Educ. 2015, 29, 1–10. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization [WHO]. Framework for Action on Interprofessional Education & Collaborative Practice (WHO/HRH/HPN/10.3). 2010. Available online: http://www.who.int/hrh/nursing_midwifery/en/ (accessed on 15 September 2023).
- Canadian Interprofessional Health Collaborative [CIHC]. A National Interprofessional Competency Framework. Available online: http://ipcontherun.ca/wp-content/uploads/2014/06/National-Framework.pdf (accessed on 15 September 2023).
- Yeager, S. Interdisciplinary Collaboration: The Heart and Soul of Health Practice. Crit. Pract. Nurs. Clin. N. Am. 2005, 17, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Lutfiyya, M.N.; Chang, L.F.; McGrath, C.; Dana, C.; Lipsky, M.S. The State of the Science of Interprofessional Collaborative Practice: A Scoping Review of the Patient Health-Related Outcomes Based Literature Published between 2010 and 2018. PLoS ONE 2019, 14, e0218578. [Google Scholar] [CrossRef] [PubMed]
- Baik, D.; Zierler, B. Clinical Nurses’ Experiences and Perceptions after the Implementation of an Interprofessional Team Intervention: A Qualitative Study. J. Clin. Nurs. 2019, 28, 430–443. [Google Scholar] [CrossRef] [PubMed]
- Ten Cate, O. Trust, Competence, and the Supervisor’s Role in Postgraduate Training. BMJ 2006, 333, 748–751. [Google Scholar] [CrossRef] [PubMed]
- Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel; Interprofessional Education Collaborative: Washington, DC, USA, 2011. [Google Scholar]
- Bainbridge, L.; Nasmith, L.; Orchard, C.; Wood, V. Competencies for Interprofessional Collaboration. J. Phys. Ther. Educ. 2010, 24, 6–11. [Google Scholar] [CrossRef]
- Baggs, J.G. Development of an Instrument to Measure Collaboration and Satisfaction About Care Decisions. J. Adv. Nurs. 1994, 20, 176–182. [Google Scholar] [PubMed]
- Ushiro, R. Nurse-Physician Collaboration Scale: Development and Psychometric Testing. J. Adv. Nurs. 2009, 65, 1497–1508. [Google Scholar] [CrossRef] [PubMed]
- Kenaszchuk, C.; Reeves, S.; Nicholas, D.; Zwarenstein, M. Validity and Reliability of a Multiple-Group Measurement Scale for Interprofessional Collaboration. BMC Health Serv. Res. 2010, 10, 83. [Google Scholar] [CrossRef] [PubMed]
- Hull, L.; Arora, S.; Kassab, E.; Kneebone, R.; Sevdalis, N. Observational Teamwork Assessment for Surgery: Content Validation and Tool Refinement. J. Am. Coll. Surg. 2011, 212, 234–243.e1-5. [Google Scholar] [CrossRef]
- Schroder, C.; Medves, J.; Paterson, M.; Byrnes, V.; Chapman, C.; O’Riordan, A.; Pichora, D.; Kelly, C. Development and Pilot Testing Of The Collaborative Practice Assessment Tool. J. Interprofessional Care 2011, 25, 189. [Google Scholar] [CrossRef] [PubMed]
- Sutton, G.; Liao, J.; Jimmieson, N.L.; Restubog, S.L. Measuring Multidisciplinary Team Effectiveness in a Ward-Based Healthcare Setting: Development of the Team Functioning Assessment Tool. J. Heal. Qual. 2011, 33, 10–23. [Google Scholar] [CrossRef] [PubMed]
- Orchard, C.A.; King, G.A.; Khalili, H.; Bezzina, M.B. Assessment of Interprofessional Team Collaboration Scale (AITCS): Development and Testing of the Instrument. J. Contin. Educ. Health Prof. 2012, 32, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Van, C.; Costa, D.; Mitchell, B.; Abbott, P.; Krass, I. Development and Initial Validation of the Pharmacist Frequency of Interprofessional Collaboration Instrument (FICI-P) in Primary Care. Res. Soc. Adm. Pharm. 2012, 8, 397. [Google Scholar] [CrossRef] [PubMed]
- Van, C.; Costa, D.; Mitchell, B.; Abbott, P.; Krass, I. Development and Validation of the GP Frequency of Interprofessional Collaboration Instrument (FICI-GP) in Primary Care. J. Interprofessional Care 2012, 26, 297. [Google Scholar] [CrossRef] [PubMed]
- Jones, E.D.; Letvak, S.; McCoy, T.P. Reliability and Validity of the Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration for Nurse Practitioners. J. Nurs. Meas. 2013, 21, 463–476. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Sakai, I.; Takahashi, Y.; Maeda, T.; Kunii, Y.; Kurokochi, K. Development of a new Measurement Scale for Interprofessional Collaborative Competency: A Pilot Study in Japan. J. Interprofessional Care 2014, 28, 45. [Google Scholar] [CrossRef] [PubMed]
- Tilden, V.P.; Eckstrom, E.; Dieckmann, N.F. Development of the Assessment for Collaborative Environments (ACE-15): A tool to Measure Perceptions of Interprofessional “Teamness”. J. Interprofessional Care 2016, 30, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Jadotte, Y.T.; Chase, S.M.; Qureshi, R.I.; Holly, C.; Salmond, S. The HCAHPS Survey as a Potential Tool for Measuring Organizational Interprofessional Competency at American Hospitals Nationwide: A Content Analysis Study of Concept Validity. Health Interprofessional Pract. 2017, 3, eP1119. [Google Scholar] [CrossRef]
- Sakai, I.; Yamamoto, T.; Takahashi, Y.; Maeda, T.; Kunii, Y.; Kurokochi, K. Development of a new Measurement Scale for Interprofessional Collaborative Competency: The Chiba Interprofessional Competency Scale (CICS29). J. Interprofessional Care 2017, 31, 59–65. [Google Scholar] [CrossRef]
- Shimmura, K.; Tadaka, E. Development of an Interprofessional Collaboration Competency Scale for Children with Medical Complexity. BMJ Open 2018, 8, e019415. [Google Scholar] [CrossRef] [PubMed]
- Meijer, L.J.; de Groot, E.; van Smeden, M.; Schellevis, F.G.; Damoiseaux, R.A. Challenges in measuring Interprofessional–Interorganisational Collaboration with a Questionnaire. BJGP Open 2018, 2, bjgpopen18X101385. [Google Scholar] [CrossRef] [PubMed]
- Orchard, C.; Pederson, L.L.; Read, E.; Mahler, C.; Laschinger, H. Assessment of Interprofessional Team Collaboration Scale (AITCS): Further Testing and Instrument Revision. J. Contin. Educ. Health Prof. 2018, 38, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Haruta, J.; Goto, R. Development of a Japanese version of the Self-assessment Scale of Interprofessional Competency (JASSIC). J. Interprofessional Care 2022, 36, 599. [Google Scholar] [CrossRef] [PubMed]
- Soemantri, D.; Findyartini, A.; Werdhani, R.A.; Koesnoe, S.; Dahlia, D. Are we ready to collaborate? The interprofessional Collaborative Competencies of Healthcare Professionals in the Global South context. Front. Med. 2022, 9, 904658. [Google Scholar] [CrossRef] [PubMed]
- Hanskamp-Sebregts, M.; van Gurp, P.J.; Braspenning, J. Design and Validation of a Questionnaire to Measure Interprofessional Collaborative Practice for Auditing Integrated Hospital Care: Empirical Research. J. Contin. Educ. Health Prof. 2023. [Google Scholar] [CrossRef] [PubMed]
- Prasitanarapun, R.; Kitreerawutiwong, N. The Development of An Instrument to Measure Interprofessional Collaboration Competency for Primary Care Teams In The District Health System Of Health Region 2, Thailand. BMC Prim. Care 2023, 24, 55. [Google Scholar] [CrossRef] [PubMed]
- Archibald, D.; Trumpower, D.; MacDonald, C.J. Validation of the Interprofessional Collaborative Competency Attainment Survey (ICCAS). J. Interprofessional Care 2014, 28, 553–558. [Google Scholar] [CrossRef]
- Hojat, M.; Fields, S.K.; Veloski, J.J.; Griffiths, M.; Cohen, M.J.; Plumb, J.D. Psychometric Properties of an Attitude Scale Measuring Physician-Nurse Collaboration. Eval. Health Prof. 1999, 22, 208–220. [Google Scholar] [CrossRef]
- Ward, J.; Schaal, M.; Sullivan, J.; Bowen, M.E.; Erdmann, J.B.; Hojat, M. The Jefferson Scale of Attitudes toward Physician-Nurse Collaboration: A study with Undergraduate Nursing Students. J. Interprofessional Care 2008, 22, 375–386. [Google Scholar] [CrossRef]
- Curran, V.; Hollett, A.; Casimiro, L.M.; McCarthy, P.; Banfield, V.; Hall, P.; Lackie, K.; Oandasan, I.; Simmons, B.; Wagner, S. Development and Validation of the Interprofessional Collaborator Assessment Rubric (ICAR). J. Interprofessional Care 2011, 25, 339. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.J. Development and Validation of Performance Assessment Tools for Interprofessional Communication and Teamwork (PACT). Ph.D. Thesis, University of Washington, Seattle, WA, USA, 2014. [Google Scholar]
- Dow, A.W.; DiazGranados, D.; Mazmanian, P.E.; Retchin, S.M. An Exploratory Study of an Assessment tool Derived from the Competencies of the Interprofessional Education Collaborative. J. Interprofessional Care 2014, 28, 299. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, D.G.; Fike, D.S.; MacLaughlin, E.J.; Zorek, J.A. A Comparison of The Validity of Two Instruments Assessing Health Professional Student Perceptions of Interprofessional Education and Practice. J. Interprofessional Care 2015, 29, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Lockeman, K.S.; Dow, A.W.; DiazGranados, D.; McNeilly, D.P.; Nickol, D.; Koehn, M.L.; Knab, M.S. Refinement of the IPEC Competency Self-Assessment Survey: Results from a Multi-institutional Study. J. Interprofessional Care 2016, 30, 726. [Google Scholar] [CrossRef] [PubMed]
- Hasnain, M.; Gruss, V.; Keehn, M.; Peterson, E.; Valenta, A.L.; Kottorp, A. Development and Validation of a Tool to Assess Self-Efficacy for Competence in Interprofessional Collaborative Practice. J. Interprofessional Care 2017, 31, 255. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, M.; Blue, A.; Aschenbrener, C.A.; Viggiano, T.R. Core Competencies for Interprofessional Collaborative Practice: Reforming Health Practice by Transforming Health Professionals’ Education. Acad. Med. 2011, 86, 1351. [Google Scholar] [CrossRef]
- Edelbring, S.; Dahlgren, M.A.; Wiegleb Edström, D. Characteristics of Two Questionnaires Used to Assess Interprofessional Learning: Psychometrics and Expert Panel Evaluations. BMC Med. Educ. 2018, 18, 40. [Google Scholar] [CrossRef] [PubMed]
- Hinyard, L.; Toomey, E.; Eliot, K.; Breitbach, A. Student Perceptions of Collaboration Skills in an Interprofessional Context: Development and Initial Validation of the Self-Assessed Collaboration Skills Instrument. Eval. Health Prof. 2019, 42, 450. [Google Scholar] [CrossRef] [PubMed]
- Kottorp, A.; Keehn, M.; Hasnain, M.; Gruss, V.; Peterson, E. Instrument Refinement for Measuring Self-Efficacy for Competence in Interprofessional Collaborative Practice: Development and Psychometric Analysis of IPECC-SET 27 and IPECC-SET 9. J. Interprofessional Care 2019, 33, 47. [Google Scholar] [CrossRef]
- Violato, E.M.; King, S. A Validity Study of the Interprofessional Collaborative Competency Attainment Survey: An Interprofessional Collaborative Competency Measure. J. Nurs. Educ. 2019, 58, 454. [Google Scholar] [CrossRef]
- Braathen, K. Measuring Outcomes of Interprofessional Education: A Validation Study of the Self-Assessment of Collaboration Skills Measure. Prof. Prof. 2022, 12. [Google Scholar] [CrossRef]
- Peltonen, J.; Leino-Kilpi, H.; Heikkilä, H.; Rautava, P.; Tuomela, K.; Siekkinen, M.; Sulosaari, V.; Stolt, M. Instruments measuring interprofessional collaboration in healthcare—A scoping review. J. Interprofessional Care 2020, 34, 147. [Google Scholar] [CrossRef]
- Glover, P.D.; Gray, H.; Shanmugam, S.; McFadyen, A.K. Evaluating collaborative practice within community-based integrated health and social care teams: A systematic review of outcome measurement instruments. J. Interprofessional Care 2022, 36, 458–472. [Google Scholar] [CrossRef] [PubMed]
- Vaseghi, F.; Yarmohammadian, M.H.; Raeisi, A. Interprofessional Collaboration Competencies in the Health System: A Systematic Review. Iran. J. Nurs. Midwifery Res. 2022, 27, 496–504. [Google Scholar] [PubMed]
- Minstry of Health and Welfar, Taiwan, ROC. Clinical Medical Personnel Training Program- Biennial Training Course Guidelines. Department of Medical Affairs. 2007. Available online: https://dep.mohw.gov.tw/DOMA/cp-2713-46862-106.html (accessed on 15 January 2024).
- Creative Research Systems. Sample Size Calculator. Available online: https://www.surveysystem.com/sscalc.htm (accessed on 15 September 2023).
- Wu, M.L.; Zhang, Y. Quick Start Tips for SPSS Questionnaire Statistical Analysis; Wunan Publishing: Taipei, Taiwan, 2018. [Google Scholar]
- Polit, D.F.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice, 11th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2021. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed.; Allyn & Bacon/Pearson Education: Boston, MA, USA, 2007. [Google Scholar]
- Watkins, M.W. Exploratory Factor Analysis: A Guide to Best Practice. J. Black Psychol. 2018, 44, 219–246. [Google Scholar] [CrossRef]
- Taherdoost, H.; Sahibuddin, S.H.; Jalaliyoon, N.E. Exploratory Factor Analysis Concepts and Theory. Adv. Appl. Pure Math. 2022, 27, 375–382. [Google Scholar]
- Taiwan Nurses Association [TWNA]. Guidelines for Advanced Planning of Primary Care Nursing Ability. Available online: https://www.twna.org.tw/WebPad/WebPad.aspx?1x8jyHnXeNSHfBGHev4mkg%3d%3d (accessed on 18 December 2023).
- West, C.; Veronin, M.; Landry, K.; Kurz, T.; Watzak, B.; Quiram, B.; Graham, L. Tools to Investigate How Interprofessional Education Activities Link to Competencies. Med. Educ. Online 2015, 20, 28627. [Google Scholar] [CrossRef] [PubMed]
- Wynarczuk, K.D.; Hadley, D.E.; Sen, S.; Ward, J.F.; Ganetsky, V.S.; Sen, S. Pharmacy, Physical Therapy, Occupational Therapy, and Physician Assistant Professional Students’ Perspectives on Interprofessional Roles and Responsibilities. J. Interprofessional Care 2019, 33, 832–835. [Google Scholar] [CrossRef] [PubMed]
- Goldsberry, J.W. Advanced Practice Nurses Leading the Way: Interprofessional Collaboration. Nurse Educ. Today 2018, 65, 1–3. [Google Scholar] [CrossRef]
- Goto, R.; Haruta, J. Current Status of Interprofessional Competency among Healthcare Professions in Japan: A Cross-Sectional Web-Based Survey. J. Gen. Fam. Med. 2023, 24, 119–125. [Google Scholar] [CrossRef]
- Kaba, A.; Dubé, M.; Charania, I.; Donahue, M. Collaborative Practice in Action: Building Interprofessional Competencies through Simulation Based Education and Novel Approaches to Team Training. Health Educ. Care 2018, 3, 1–9. [Google Scholar] [CrossRef]
- Yeh, S.L.; Lin, C.T.; Wang, L.H.; Lin, C.C.; Ma, C.T.; Han, C.Y. The Outcomes of an Interprofessional Simulation Program for New Graduate Nurses. Int. J. Environ. Res. Public Health 2022, 19, 13839. [Google Scholar] [CrossRef]
- Berghout, T. How Are Nurse Educators Prepared to Teach Interprofessional Practice? Nurse Educ. Today 2021, 98, 104745. [Google Scholar] [CrossRef] [PubMed]
- Orchard, C.; Bainbridge, L. Competent for Collaborative Practice: What Does a Collaborative Practitioner Look Like and How Does the Practice Context Influence Interprofessional Education? J. Taibah Univ. Med. Sci. 2016, 11, 526–532. [Google Scholar] [CrossRef]
- Bolarinwa, O.A. Principles and Methods of Validity and Reliability Testing of Questionnaires Used in Social and Health Science Researches. Niger. Postgrad. Med. J. 2015, 22, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Knekta, E.; Runyon, C.; Eddy, S. One Size Doesn’t Fit All: Using Factor Analysis to Gather Validity Evidence When Using Surveys in Your Research. CBE Life Sci Educ. 2019, 18, rm1. [Google Scholar] [CrossRef]
- Gunawan, J.; Marzilli, C.; Aungsuroch, Y. Establishing Appropriate Sample Size for Developing and Validating A Questionnaire in Nursing Research. Belitung Nurs. J. 2021, 7, 356–360. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).