Perceived Well-Being among Adults with Diabetes and Hypertension: A National Study
Abstract
:1. Introduction
Aims
2. Materials and Methods
2.1. Data Sources
2.2. Study Population
2.3. Outcome Variables
2.3.1. Sociodemographic Variables
2.3.2. Perceived Health and Distresses
2.4. Data Analysis and Visualization
3. Results
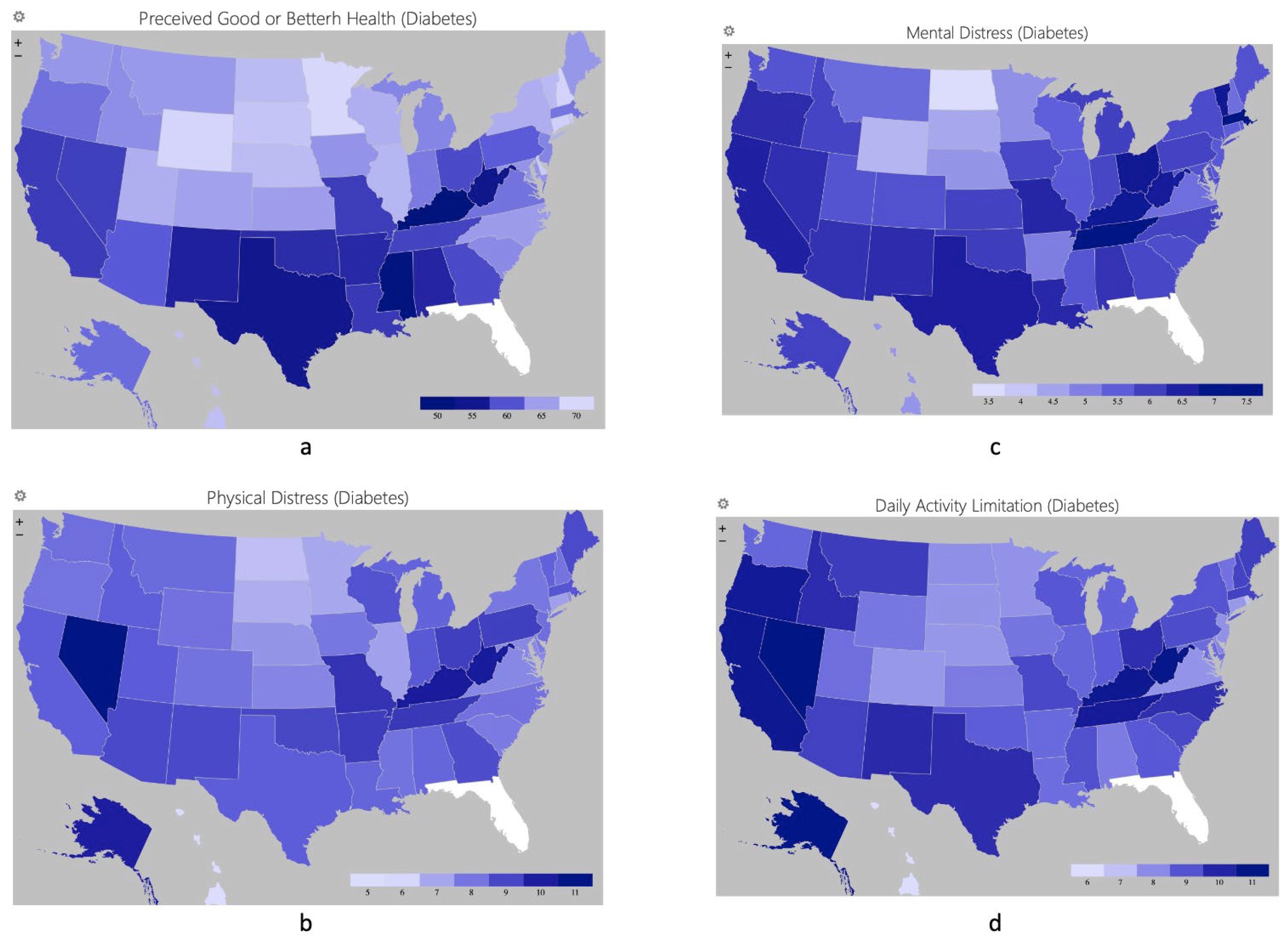
3.1. Perceived Health and Distresses in Different States
3.2. Factors Associated with Perceived Health and Distress
4. Discussion
4.1. Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 20 February 2024).
- GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- Wierzejska, E.; Giernas, B.; Lipiak, A.; Karasiewicz, M.; Cofta, M.; Staszewski, R. A global perspective on the costs of hypertension: A systematic review. Arch. Med. Sci. 2020, 16, 1078–1091. [Google Scholar] [CrossRef]
- Seuring, T.; Archangelidi, O.; Suhrcke, M. The Economic Costs of Type 2 Diabetes: A Global Systematic Review. Pharmacoeconomics 2015, 33, 811–831. [Google Scholar] [CrossRef]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of Medical Care in Diabetes—2022 Abridged for Primary Care Providers. Clin. Diabetes 2022, 40, 10–38. [Google Scholar] [CrossRef]
- de Boer, I.H.; Bangalore, S.; Benetos, A.; Davis, A.M.; Michos, E.D.; Muntner, P.; Rossing, P.; Zoungas, S.; Bakris, G. Diabetes and Hypertension: A Position Statement by the American Diabetes Association. Diabetes Care 2017, 40, 1273–1284. [Google Scholar] [CrossRef]
- WHO. Noncommunicable Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 20 February 2024).
- Tam, H.L.; Chair, S.Y.; Leung, I.S.H.; Leung, L.Y.L.; Chan, A.S.W. US Adults Practicing Healthy Lifestyles before and during COVID-19: Comparative Analysis of National Surveys. JMIR Public Health Surveill. 2023, 9, e45697. [Google Scholar] [CrossRef]
- Axon, D.R.; Jang, A.; Son, L.; Pham, T. Determining the association of perceived health status among united states older adults with self-reported pain. Aging Health Res. 2022, 2, 100051. [Google Scholar] [CrossRef]
- Tinajero-Chávez, L.I.; Mora-Romo, J.F.; Bravo-Doddoli, A.; Cruz-Narciso, B.V.; Calleja, N.; Toledano-Toledano, F. Design, Development, and Validation of the Self-Perceived Health Scale (SPHS). Healthcare 2023, 11, 2007. [Google Scholar] [CrossRef]
- Perrin, N.E.; Davies, M.J.; Robertson, N.; Snoek, F.J.; Khunti, K. The prevalence of diabetes-specific emotional distress in people with Type 2 diabetes: A systematic review and meta-analysis. Diabet. Med. 2017, 34, 1508–1520. [Google Scholar] [CrossRef]
- Young-Hyman, D.; de Groot, M.; Hill-Briggs, F.; Gonzalez, J.S.; Hood, K.; Peyrot, M. Psychosocial Care for People with Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016, 39, 2126–2140. [Google Scholar] [CrossRef]
- Ojike, N.; Sowers, J.R.; Seixas, A.; Ravenell, J.; Rodriguez-Figueroa, G.; Awadallah, M.; Zizi, F.; Jean-Louis, G.; Ogedegbe, O.; McFarlane, S.I. Psychological Distress and Hypertension: Results from the National Health Interview Survey for 2004–2013. Cardiorenal Med. 2016, 6, 198–208. [Google Scholar] [CrossRef]
- Duenas, M.; Salazar, A.; de Sola, H.; Failde, I. Limitations in Activities of Daily Living in People with Chronic Pain: Identification of Groups Using Clusters Analysis. Pain. Pract. 2020, 20, 179–187. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; STORBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Prev. Med. 2007, 45, 247–251. [Google Scholar] [CrossRef]
- 2021 BRFSS Survey Data and Documentation. Available online: https://www.cdc.gov/brfss/annual_data/annual_2021.html (accessed on 20 February 2024).
- Li, Y.; Schoufour, J.; Wang, D.D.; Dhana, K.; Pan, A.; Liu, X.; Song, M.; Liu, G.; Shin, H.J.; Sun, Q.; et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: Prospective cohort study. BMJ 2020, 368, l6669. [Google Scholar] [CrossRef]
- WHO. The Global Network for Age-Friendly Cities and Communities. Available online: https://www.who.int/publications/i/item/WHO-FWC-ALC-18.4 (accessed on 20 February 2024).
- Hong, A.; Welch-Stockton, J.; Kim, J.Y.; Canham, S.L.; Greer, V.; Sorweid, M. Age-Friendly Community Interventions for Health and Social Outcomes: A Scoping Review. Int. J. Environ. Res. Public. Health 2023, 20, 2554. [Google Scholar] [CrossRef]
- Schmidt, C.B.; van Loon, B.J.P.; Vergouwen, A.C.M.; Snoek, F.J.; Honig, A. Systematic review and meta-analysis of psychological interventions in people with diabetes and elevated diabetes-distress. Diabet. Med. 2018, 35, 1157–1172. [Google Scholar] [CrossRef]
- Ngan, H.Y.; Chong, Y.Y.; Chien, W.T. Effects of mindfulness- and acceptance-based interventions on diabetes distress and glycaemic level in people with type 2 diabetes: Systematic review and meta-analysis. Diabet. Med. 2021, 38, e14525. [Google Scholar] [CrossRef]
- Park, S.; Chan, K.C.; Williams, E.C. Gain of employment and perceived health status among previously unemployed persons: Evidence from a longitudinal study in the United States. Public. Health 2016, 133, 83–90. [Google Scholar] [CrossRef]
- Zhou, Y.F.; Chen, S.; Wang, G.; Chen, S.; Zhang, Y.B.; Chen, J.X.; Tu, Z.Z.; Liu, G.; Wu, S.; Pan, A. Effectiveness of a Workplace-Based, Multicomponent Hypertension Management Program in Real-World Practice: A Propensity-Matched Analysis. Hypertension 2022, 79, 230–240. [Google Scholar] [CrossRef]
- Mulchandani, R.; Chandrasekaran, A.M.; Shivashankar, R.; Kondal, D.; Agrawal, A.; Panniyammakal, J.; Tandon, N.; Prabhakaran, D.; Sharma, M.; Goenka, S. Effect of workplace physical activity interventions on the cardio-metabolic health of working adults: Systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 134. [Google Scholar] [CrossRef]
- Hosseinzadeh, R.; Goharrizi, M.; Bahardoust, M.; Alvanegh, A.G.; Ataee, M.R.; Bagheri, M.; Navidiyan, E.S.; Zijoud, S.R.H.; Heiat, M. Should all patients with hypertension be worried about developing severe coronavirus disease 2019 (COVID-19)? Clin. Hypertens. 2021, 27, 3. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Zhang, D.; Son, H.; Shen, Y.; Chen, Z.; Rajbhandari-Thapa, J.; Li, Y.; Eom, H.; Bu, D.; Mu, L.; Li, G.; et al. Assessment of Changes in Rural and Urban Primary Care Workforce in the United States from 2009 to 2017. JAMA Netw. Open 2020, 3, e2022914. [Google Scholar] [CrossRef]
- Tam, H.L.; Chung, S.F.; Wang, Q. Urban-rural disparities in hypertension management among middle-aged and older patients: Results of a 2018 Chinese national study. Chronic Illn. 2023, 19, 581–590. [Google Scholar] [CrossRef]
- Pew Research Center. Smartphone Ownership Is Growing Rapidly around the World, but Not Always Equally. Available online: https://www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally (accessed on 20 February 2024).
- Babbage, C.M.; Jackson, G.M.; Davies, E.B.; Nixon, E. Self-help Digital Interventions Targeted at Improving Psychological Well-being in Young People with Perceived or Clinically Diagnosed Reduced Well-being: Systematic Review. JMIR Ment. Health 2022, 9, e25716. [Google Scholar] [CrossRef] [PubMed]
- Nicholl, B.I.; Sandal, L.F.; Stochkendahl, M.J.; McCallum, M.; Suresh, N.; Vasseljen, O.; Hartvigsen, J.; Mork, P.J.; Kjaer, P.; Søgaard, K.; et al. Digital Support Interventions for the Self-Management of Low Back Pain: A Systematic Review. J. Med. Internet Res. 2017, 19, e179. [Google Scholar] [CrossRef]
- Russell, D.; Mathew, S.; Fitts, M.; Liddle, Z.; Murakami-Gold, L.; Campbell, N.; Ramjan, M.; Zhao, Y.; Hines, S.; Humphreys, J.S.; et al. Interventions for health workforce retention in rural and remote areas: A systematic review. Hum. Resour. Health 2021, 19, 103. [Google Scholar] [CrossRef]
- Ngan, H.Y.; Chong, Y.Y.; Loo, K.M.; Chien, W.T. Preliminary efficacy of an acceptance-based diabetes education (ACT-DE) programme for people with type 2 diabetes on diabetes distress and self-care behaviours: A pilot randomised controlled trial. J. Context. Behav. 2023, 30, 50–60. [Google Scholar] [CrossRef]
- Lazar, M.; Davenport, L. Barriers to Health Care Access for Low Income Families: A Review of Literature. J. Community Health Nurs. 2018, 35, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Terlizzi, E.P.; Cohen, R.A. Geographic Variation in Health Insurance Coverage: United States, 2021. Natl. Health Stat. Rep. 2022, 176, 1–19. [Google Scholar]
- Sanadgol, A.; Doshmangir, L.; Majdzadeh, R.; Gordeev, V.S. Engagement of non-governmental organisations in moving towards universal health coverage: A scoping review. Glob. Health 2021, 17, 129. [Google Scholar] [CrossRef] [PubMed]

| All | Diabetes | Hypertension | |
|---|---|---|---|
| N = 333,316 | N = 43,911 | N = 130,960 | |
| Sex | |||
| Male | 159,355 (47.8%) | 22,400 (51.0%) | 66,956 (51.1%) |
| Female | 173,961 (52.2%) | 21,511 (49.0%) | 64,004 (48.9%) |
| Age range (years) | |||
| 18 to 24 | 17,124 (5.1%) | 198 (0.5%) | 1343 (1.0%) |
| 25 to 34 | 38,404 (11.6%) | 820 (1.9%) | 4825 (3.7%) |
| 35 to 44 | 48,309 (14.5%) | 2466 (5.6%) | 10,172 (7.8%) |
| 45 to 54 | 51,345 (15.4%) | 5704 (13.0%) | 17,084 (13.0%) |
| 55 to 64 | 65,719 (19.7%) | 11,186 (25.4%) | 30,378 (23.2%) |
| 65 to 74 | 67,757 (20.3%) | 14,141 (32.2%) | 38,704 (29.6%) |
| 75 up | 44,658 (13.4%) | 9396 (21.4%) | 28,454 (21.7%) |
| Residential area | |||
| Urban | 284,944 (85.5%) | 36,604 (83.4%) | 109,565 (83.7%) |
| Rural | 48,372 (14.5%) | 7307 (16.6%) | 21,395 (16.3%) |
| Education level | |||
| Attended high school or less | 17,652 (5.3%) | 3551 (8.1%) | 7930 (6.1%) |
| Graduated from high school | 81,692 (24.5%) | 12,715 (29.0%) | 35,861 (27.4%) |
| Attended college or above | 93,203 (28.0%) | 13,622 (31.0%) | 38,598 (29.5%) |
| Graduated from college or above | 140,769 (42.2%) | 14,023 (31.9%) | 48,571 (37.0%) |
| Employment status | |||
| Employed | 182,528 (54.7%) | 14,453 (32.9%) | 52,282 (39.9%) |
| Unemployed | 34,854 (10.5%) | 3320 (7.6%) | 9778 (7.5%) |
| Retired or unable to work | 115,934 (34.8%) | 26,138 (59.5%) | 68,900 (52.6%) |
| Household income (US dollars) | |||
| Less than 15,000 | 20,616 (6.2%) | 4580 (10.4%) | 10,088 (7.7%) |
| 15,000 to <25,000 | 34,237 (10.3%) | 6825 (15.5%) | 16,730 (12.8%) |
| 25,000 to <35,000 | 42,321 (12.7%) | 7040 (16.0%) | 18,492 (14.2%) |
| 35,000 to <50,000 | 46,834 (14.1%) | 6919 (15.8%) | 20,089 (15.3%) |
| 50,000 to <100,000 | 104,756 (31.4%) | 12,077 (27.5%) | 39,664 (30.3%) |
| 100,000 to <200,000 | 66,017 (19.8%) | 5430 (12.4%) | 20,995 (16.0%) |
| 200,000 or more | 18,535 (5.5%) | 1040 (2.4%) | 4902 (3.7%) |
| Perceived health | |||
| Excellent | 58,798 (17.6%) | 1656 (3.8%) | 10,722 (8.2%) |
| Very good | 116,103 (34.8%) | 8400 (19.1%) | 38,373 (29.3%) |
| Good | 103,882 (31.2%) | 17,086 (38.9%) | 48,439 (37.0%) |
| Fair | 40,593 (12.2%) | 11,867 (27.0%) | 24,242 (18.5%) |
| Poor | 13,940 (4.2%) | 4902 (11.2%) | 9184 (7.0%) |
| Perceived unhealthy day, mean (SD) | |||
| Physical distress | 3.80 (8.32) | 7.25 (11.05) | 5.37 (9.79) |
| Mental distress | 4.23 (8.20) | 4.79 (9.05) | 4.28 (8.52) |
| Daily activity limitation | 5.18 (8.94) | 7.89 (10.96) | 6.52 (10.12) |
| Perceived Good or Better Health a | Physical Distress b | Mental Distress b | Daily Activity Limitation b | |
|---|---|---|---|---|
| Odds Ratio (95% CI) | Beta (95% CI) | Beta (95% CI) | Beta (95% CI) | |
| Sex: male | 0.97 (0.93, 1.01) | 0.01 (−0.19, 0.22) | −1.30 (−1.47, −1.14) * | 0.69 (0.43, 0.95) * |
| Age range (years) | ||||
| 18 to 24 | Reference | Reference | Reference | Reference |
| 25 to 34 | 0.78 | 1.14 | −1.40 | 0.95 |
| (0.55, 1.10) | (−0.51, 2.80) | (−2.75, −0.06) * | (−0.88, 2.78) | |
| 35 to 44 | 0.61 | 2.83 | −2.27 | 1.10 |
| (0.44, 0.85) * | (1.28, 4.37) * | (−3.52, −1.01) * | (−0.60, 2.81) | |
| 45 to 54 | 0.63 | 3.27 | −3.47 | 1.14 |
| (0.46, 0.87) * | (1.76, 4.78) * | (−4.70, −2.24) * | (−0.53, 2.80) | |
| 55 to 64 | 0.72 | 3.00 | −5.09 | 0.74 |
| (0.52, 0.98) * | (1.50, 4.50) * | (−6.31, −3.87) * | (−0.91, 2.40) | |
| 65 to 74 | 1.13 | 0.07 | −7.93 | −2.29 |
| (0.82, 1.69) | (−1.44, 1.57) | (−9.16, −6.71) * | (−3.95, −0.63) | |
| 75 up | 1.23 | −0.36 | −9.09 | −2.99 |
| (0.89, 1.69) | (−1.88, 1.15) | (−10.33, −7.86) * | (−4.67, −1.32) | |
| Residence in urban areas | 1.06 | −0.09 | 0.29 | −0.20 |
| (1.01, 1.12) * | (−0.36, 0.18) | (0.07, 0.50) * | (−0.54, 0.14) | |
| Education level | ||||
| Attended high school or less | 0.47 | 0.87 | −0.22 | 0.54 |
| (0.43, 0.51) * | (0.44, 1.30) * | (−0.57, 0.12) | (0.02, 1.06) * | |
| Graduated from high school | 0.73 | 0.46 | −0.24 | 0.23 |
| (0.69, 0.77) * | (0.19, 0.74) * | (−0.47, −0.02) * | (−0.12, 0.59) | |
| Attended college or above | 0.79 | 0.76 | 0.34 | 0.42 |
| (0.75, 0.84) * | (0.50, 1.02) * | (0.13, 0.55) * | (0.08, 0.75) * | |
| Graduated from college or above | Reference | Reference | Reference | Reference |
| Employment status | ||||
| Employed | 2.22 | −5.04 | −2.44 | −6.34 |
| (2.09, 2.35) * | (−5.31, −4.76) * | (−2.66, −2.21) * | (−6.69, −5.99) * | |
| Unemployed | 1.40 | −2.41 | −0.60 | −2.06 |
| (1.30, 1.52) * | (−2.82, −2.01) * | (−0.93, −0.27) * | (−2.54, −1.58) * | |
| Retired or unable to work | Reference | Reference | Reference | Reference |
| Household income (US dollars) | ||||
| Less than 15,000 | 0.22 | 6.21 | 4.84 | 4.78 |
| (0.19, 0.27) * | (5.46, 6.97) * | (4.22, 5.46) * | (3.72, 5.83) * | |
| 15,000 to <25,000 | 0.29 | 4.47 | 2.97 | 3.15 |
| (0.25, 0.35) * | (3.74, 5.19) * | (2.37, 3.56) * | (2.12, 4.18) * | |
| 25,000 to <35,000 | 0.37 | 3.15 | 2.01 | 2.08 |
| (0.31, 0.44) * | (2.43, 3.86) * | (1.43, 2.60) * | (1.06, 3.10) * | |
| 35,000 to <50,000 | 0.46 | 1.95 | 1.50 | 1.36 |
| (0.39, 0.55) * | (1.25, 2.66) * | (0.92, 2.08) * | (0.34, 2.38) * | |
| 50,000 to <100,000 | 0.65 | 1.07 | 0.61 | 0.54 |
| (0.54, 0.77) * | (0.39, 1.75) * | (0.06, 1.17) * | (−0.45, 1.53) | |
| 100,000 to <200,000 | 0.86 | 0.07 | 0.01 | 0.21 |
| (0.71, 1.02) | (−0.64, 0.77) | (−0.56, 0.59) | (−0.82, 1.24) | |
| 200,000 or more | Reference | Reference | Reference | Reference |
| Perceived Good or Better Health a | Physical Distress b | Mental Distress b | Daily Activity Limitation b | |
|---|---|---|---|---|
| Odds Ratio (95% CI) | Beta (95% CI) | Beta (95% CI) | Beta (95% CI) | |
| Sex: male | 0.97 | 0.01 | −1.30 | 0.69 |
| (0.93, 1.01) | (−0.19, 0.22) | (−1.47, −1.14) * | (0.43, 0.95) * | |
| Age range (years) | ||||
| 18 to 24 | Reference | Reference | Reference | Reference |
| 25 to 34 | 0.78 | 1.14 | −1.40 | 0.95 |
| (0.55, 1.10) | (−0.51, 2.80) | (−2.75, −0.06) * | (−0.88, 2.78) | |
| 35 to 44 | 0.61 | 2.83 | −2.27 | 1.10 |
| (0.44, 0.85) * | (1.28, 4.37) * | (−3.52, −1.01) * | (−0.60, 2.81) | |
| 45 to 54 | 0.63 | 3.27 | −3.47 | 1.14 |
| (0.46, 0.87) * | (1.76, 4.78) * | (−4.70, −2.24) * | (−0.53, 2.80) | |
| 55 to 64 | 0.72 | 3.00 | −5.09 | 0.74 |
| (0.52, 0.98) * | (1.50, 4.50) * | (−6.31, −3.87) * | (−0.91, 2.40) | |
| 65 to 74 | 1.13 | 0.07 | −7.93 | −2.29 |
| (0.82, 1.69) | (−1.44, 1.57) | (−9.16, −6.71) * | (−3.95, −0.63) * | |
| 75 up | 1.23 | −0.36 | −9.09 | −2.99 |
| (0.89, 1.69) | (−1.88, 1.15) | (−10.33, −7.86) * | (−4.67, −1.32) * | |
| Residence in urban areas | 1.06 | −0.09 | 0.29 | −0.20 |
| (1.01, 1.12) * | (−0.36, 0.18) | (0.07, 0.50) * | (−0.54, 0.14) | |
| Education level | ||||
| Attended high school or less | 0.47 | 0.87 | −0.22 | 0.54 |
| (0.43, 0.51) * | (0.44, 1.30) * | (−0.57, 0.12) | (0.02, 1.06) * | |
| Graduated from high school | 0.73 | 0.46 | −0.24 | 0.23 |
| (0.69, 0.77) * | (0.19, 0.74) * | (−0.47, −0.02) * | (−0.12, 0.59) | |
| Attended college or above | 0.79 | 0.76 | 0.34 | 0.42 |
| (0.75, 0.84) * | (0.50, 1.02) * | (0.13, 0.55) * | (0.08, 0.75) * | |
| Graduated from college or above | Reference | Reference | Reference | Reference |
| Employment status | ||||
| Employed | 2.22 | −5.04 | −2.44 | −6.34 |
| (2.09, 2.35) * | (−5.31, −4.76) * | (−2.66, −2.21) * | (−6.69, −5.99) * | |
| Unemployed | 1.40 | −2.41 | −0.60 | −2.06 |
| (1.30, 1.52) * | (−2.82, −2.01) * | (−0.93, −0.27) * | (−2.54, −1.58) * | |
| Retired or unable to work | Reference | Reference | Reference | Reference |
| Household income (US dollars) | ||||
| Less than 15,000 | 0.22 | 6.21 | 4.84 | 4.78 |
| (0.19, 0.27) * | (5.46, 6.97) * | (4.22, 5.46) * | (3.72, 5.83) * | |
| 15,000 to <25,000 | 0.29 | 4.47 | 2.97 | 3.15 |
| (0.25, 0.35) * | (3.74, 5.19) * | (2.37, 3.56) * | (2.12, 4.18) * | |
| 25,000 to <35,000 | 0.37 | 3.15 | 2.01 | 2.08 |
| (0.31, 0.44) * | (2.43, 3.86) * | (1.43, 2.60) * | (1.06, 3.10) * | |
| 35,000 to <50,000 | 0.46 | 1.95 | 1.50 | 1.36 |
| (0.39, 0.55) * | (1.25, 2.66) * | (0.92, 2.08) * | (0.34, 2.38) * | |
| 50,000 to <100,000 | 0.65 | 1.07 | 0.61 | 0.54 |
| (0.54, 0.77) * | (0.39, 1.75) * | (0.06, 1.17) * | (−0.45, 1.53) | |
| 100,000 to <200,000 | 0.86 | 0.07 | 0.01 | 0.21 |
| (0.71, 1.02) | (22120.64, 0.77) | (−0.56, 0.59) | (−0.82, 1.24) | |
| 200,000 or more | Reference | Reference | Reference | Reference |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leung, L.Y.-L.; Tam, H.-L.; Leung, I.S.-H.; Chan, A.S.-W.; Yin, Y.; Zhang, X.; Mao, A.; Cheong, P.-L. Perceived Well-Being among Adults with Diabetes and Hypertension: A National Study. Healthcare 2024, 12, 844. https://doi.org/10.3390/healthcare12080844
Leung LY-L, Tam H-L, Leung IS-H, Chan AS-W, Yin Y, Zhang X, Mao A, Cheong P-L. Perceived Well-Being among Adults with Diabetes and Hypertension: A National Study. Healthcare. 2024; 12(8):844. https://doi.org/10.3390/healthcare12080844
Chicago/Turabian StyleLeung, Leona Yuen-Ling, Hon-Lon Tam, Isaac Sze-Him Leung, Alex Siu-Wing Chan, Yueheng Yin, Xiubin Zhang, Aimei Mao, and Pak-Leng Cheong. 2024. "Perceived Well-Being among Adults with Diabetes and Hypertension: A National Study" Healthcare 12, no. 8: 844. https://doi.org/10.3390/healthcare12080844









