Artificial Intelligence as a Tool for Self-Care in Patients with Type 1 and Type 2 Diabetes—An Integrative Literature Review
Abstract
:1. Background
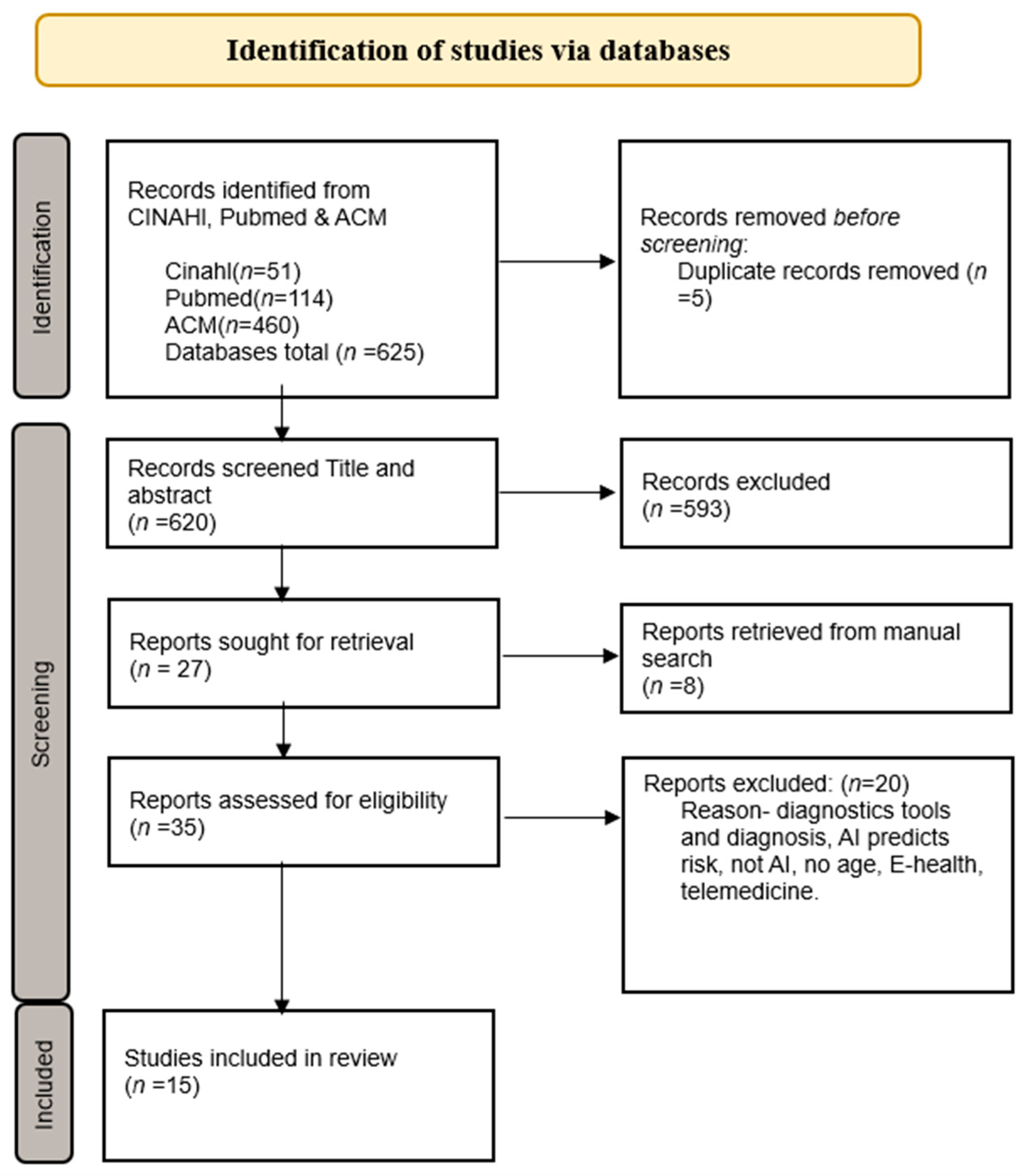
2. Methods
2.1. Design
2.2. Eligible Criteria and Data Collection
2.3. Quality Appraisal
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Artificial Intelligence as a Tool for Blood Sugar Monitoring for Patients with Diabetes Mellitus
3.2. Artificial Intelligence as a Decision Support for Diabetic Wounds and Complications
3.3. Patients’ Requests for Artificial Intelligence Capabilities in Relation to Tools
4. Discussion
Strengths and Limitations
5. Conclusions
6. Clinical Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Artificial intelligence |
| XGBoost | Extreme Gradient Boosting |
| MMAT | Mixed Methods Appraisal Tool |
| ML | Machine Learning |
| REFS | Reverse Engineering and Forward Simulation |
| RF | Random forest |
| TPGE | Treatment Pathway Graph-Based Estimation |
| MLP | Multi-layer perception |
Appendix A
Search Terms
| Search Action | CINAHL | ACM | Pubmed |
| “Telemedicine” OR “Digital health” OR “Artificial Intelligence” OR “computational intelligence” OR “machine intelligence” (“artificial intelligence” [Title/Abstract] OR “computational intelligence” [Title/Abstract] OR “machine intelligence” [Title/Abstract]) | 36,812 | 161,607 | 254,611 |
| “Diabetes mellitus” OR “Diabetes mellitus type 1” OR “diabetes mellitus type 2” OR “Diabetes” OR “type 2 diabetes” OR “diabetes type 2” OR “type 1 diabetes” OR “diabetes type 1” | 258,392 | 5977 | 842,844 |
| “Patient Centered Care” OR “Nurses Com-munity Health” OR Nurses OR “patient centered nursing” OR “patient focused care” OR “person centered care” OR “home health nurse” OR “nurse home health” OR “district nurse” OR “nursing staff” OR “Nursing” OR “nursing personnel” OR “nurses” OR “nurse s role” OR “nurses role” | 970,454 | 13,763 | 492,126 |
| #1 AND #2 AND #3 | 159 | 538 | 350 |
| Filter: English language | 104 | 538 | 212 |
| Limitation 10 year (2014–2024) | 51 | 460 | 216 |
| Adult patients | 51 | 460 | 114 |
References
- Okafor, C.N.; Akosile, C.O.; Nkechi, C.E.; Okonkwo, U.P.; Nwankwo, C.M.; Okoronkwo, I.L.; Okpala, P.U.; Afonne, A.J. Effect of educational intervention programme on the health-related quality of life (HRQOL) of individuals with type 2 diabetes mellitus in South-East, Nigeria. BMC Endocr. Disord. 2023, 23, 75. [Google Scholar] [CrossRef] [PubMed]
- Dailah, H.G. The Influence of Nurse-Led Interventions on Diseases Management in Patients with Diabetes Mellitus: A Narrative Review. Healthcare 2024, 12, 352. [Google Scholar] [CrossRef] [PubMed]
- Woldaregay, A.Z.; Årsand, E.; Walderhaug, S.; Albers, D.; Mamykina, L.; Botsis, T.; Hartvigsen, G. Data-driven modeling and prediction of blood glucose dynamics: Machine learning applications in type 1 diabetes. Artif. Intell. Med. 2019, 98, 109–134. [Google Scholar] [CrossRef] [PubMed]
- Tsalamandris, S.; Antonopoulos, A.S.; Oikonomou, E.; Papamikroulis, G.A.; Vogiatzi, G.; Papaioannou, S.; Deftereos, S.; Tousoulis, D. The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives. Eur. Cardiol. 2019, 14, 50–59. [Google Scholar] [CrossRef]
- Vehi, J.; Mujahid, O.; Contreras, I. Aim and Diabetes. In Artificial Intelligence in Medicine; Lidströmer, N., Ashrafian, H., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 701–709. [Google Scholar]
- Kaze, A.D.; Santhanam, P.; Erqou, S.; Bertoni, A.G.; Ahima, R.S.; Echouffo-Tcheugui, J.B. Microvascular disease and cardiovascular outcomes among individuals with type 2 diabetes. Diabetes Res. Clin. Pract. 2021, 176, 108859. [Google Scholar] [CrossRef]
- Khan, R.M.M.; Chua, Z.J.Y.; Tan, J.C.; Yang, Y.; Liao, Z.; Zhao, Y. From Pre-Diabetes to Diabetes: Diagnosis, Treatments and Translational Research. Medicina 2019, 55, 546. [Google Scholar] [CrossRef]
- Cho, M.K.; Kim, M.Y. Self-Management Nursing Intervention for Controlling Glucose among Diabetes: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 2750. [Google Scholar] [CrossRef]
- Deng, P.; Shi, H.; Pan, X.; Liang, H.; Wang, S.; Wu, J.; Zhang, W.; Huang, F.; Sun, X.; Zhu, H.; et al. Worldwide Research Trends on Diabetic Foot Ulcers (2004–2020): Suggestions for Researchers. J. Diabetes Res. 2022, 2022, 7991031. [Google Scholar] [CrossRef]
- Yang, H.; Li, J.; Liu, S.; Yang, X.; Liu, J. Predicting Risk of Hypoglycemia in Patients with Type 2 Diabetes by Electronic Health Record-Based Machine Learning: Development and Validation. JMIR Med. Inform. 2022, 10, e36958. [Google Scholar] [CrossRef]
- Yang, L.; Rong, G.C.; Wu, Q.N. Diabetic foot ulcer: Challenges and future. World J. Diabetes 2022, 13, 1014–1034. [Google Scholar] [CrossRef]
- Habib, S.; Sangaraju, S.L.; Yepez, D.; Grandes, X.A.; Talanki Manjunatha, R. The Nexus Between Diabetes and Depression: A Narrative Review. Cureus 2022, 14, e25611. [Google Scholar] [CrossRef]
- Franquez, R.T.; de Souza, I.M.; Bergamaschi, C.C. Interventions for depression and anxiety among people with diabetes mellitus: Review of systematic reviews. PLoS ONE 2023, 18, e0281376. [Google Scholar] [CrossRef] [PubMed]
- Skinner, T.C.; Joensen, L.; Parkin, T. Twenty-five years of diabetes distress research. Diabet. Med. 2020, 37, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Bertachi, A.; Viñals, C.; Biagi, L.; Contreras, I.; Vehí, J.; Conget, I.; Giménez, M. Prediction of Nocturnal Hypoglycemia in Adults with Type 1 Diabetes under Multiple Daily Injections Using Continuous Glucose Monitoring and Physical Activity Monitor. Sensors 2020, 20, 1705. [Google Scholar] [CrossRef] [PubMed]
- Ansari, R.M.; Harris, M.F.; Hosseinzadeh, H.; Zwar, N. Application of Artificial Intelligence in Assessing the Self-Management Practices of Patients with Type 2 Diabetes. Healthcare 2023, 11, 903. [Google Scholar] [CrossRef]
- Dankwa-Mullan, I.; Rivo, M.; Sepulveda, M.; Park, Y.; Snowdon, J.; Rhee, K. Transforming Diabetes Care Through Artificial Intelligence: The Future Is Here. Popul. Health Manag. 2019, 22, 229–242. [Google Scholar] [CrossRef]
- Ellahham, S. Artificial Intelligence: The Future for Diabetes Care. Am. J. Med. 2020, 133, 895–900. [Google Scholar] [CrossRef]
- Sridhar, G.; Lakshmi, G. Ethical Issues of Artificial Intelligence in Diabetes Mellitus. Med. Res. Arch. 2023, 11, 1–8. [Google Scholar] [CrossRef]
- Lag om egenvård. SFS 2022:1250. Available online: https://www.riksdagen.se/sv/dokument-och-lagar/dokument/svensk-forfattningssamling/lag-20221250-om-egenvard_sfs-2022-1250/ (accessed on 1 March 2025).
- Riegel, B.; Jaarsma, T.; Strömberg, A. A middle-range theory of self-care of chronic illness. ANS Adv. Nurs. Sci. 2012, 35, 194–204. [Google Scholar] [CrossRef]
- Asmat, K.; Dhamani, K.; Gul, R.; Froelicher, E.S. The effectiveness of patient-centered care vs. usual care in type 2 diabetes self-management: A systematic review and meta-analysis. Front. Public Health 2022, 10, 994766. [Google Scholar] [CrossRef]
- Toobert, D.J.; Hampson, S.E.; Glasgow, R.E. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care 2000, 23, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Weinger, K.; Butler, H.A.; Welch, G.W.; La Greca, A.M. Measuring diabetes self-care: A psychometric analysis of the Self-Care Inventory-Revised with adults. Diabetes Care 2005, 28, 1346–1352. [Google Scholar] [CrossRef]
- Ausili, D.; Barbaranelli, C.; Rossi, E.; Rebora, P.; Fabrizi, D.; Coghi, C.; Luciani, M.; Vellone, E.; Di Mauro, S.; Riegel, B. Development and psychometric testing of a theory-based tool to measure self-care in diabetes patients: The Self-Care of Diabetes Inventory. BMC Endocr. Disord. 2017, 17, 66. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.J.; Aroda, V.R.; Collins, B.S.; Gabbay, R.A.; Green, J.; Maruthur, N.M.; Rosas, S.E.; Del Prato, S.; Mathieu, C.; Mingrone, G.; et al. Management of Hyperglycemia in Type 2 Diabetes, 2022. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2022, 45, 2753–2786. [Google Scholar] [CrossRef]
- Petersson, L.; Larsson, I.; Nygren, J.M.; Nilsen, P.; Neher, M.; Reed, J.E.; Tyskbo, D.; Svedberg, P. Challenges to implementing artificial intelligence in healthcare: A qualitative interview study with healthcare leaders in Sweden. BMC Health Serv. Serv. Res. 2022, 22, 850. [Google Scholar] [CrossRef] [PubMed]
- Gautier, T.; Ziegler, L.B.; Gerber, M.S.; Campos-Náñez, E.; Patek, S.D. Artificial intelligence and diabetes technology: A review. Metabolism 2021, 124, 154872. [Google Scholar] [CrossRef]
- Zhang, J. Artificial Intelligence and Machine Learning Algorithm Optimization Applied in Health Big Data Digitization. In Proceedings of the 2021 3rd International Conference on Artificial Intelligence and Advanced Manufacture, Manchester, UK, 23–25 October 2022; Association for Computing Machinery: New York, NY, USA, 2022; pp. 2477–2480. [Google Scholar]
- Lidströmer, N.; Aresu, F.; Ashrafian, H. Introductory Approaches for Applying Artificial Intelligence in Clinical Medicine. In Artificial Intelligence in Medicine; Lidströmer, N., Ashrafian, H., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 57–74. [Google Scholar]
- Topol, E.J. Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again; Basic Books: New York, NY, USA, 2019. [Google Scholar]
- Meetoo, D.D.; Ochieng, B. AIM in Nursing Practice. In Artificial Intelligence in Medicine; Lidströmer, N., Ashrafian, H., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 743–757. [Google Scholar]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice; Wolters Kluwer Health/Lippincott Williams & Wilkins: Waltham, MA, USA, 2021. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Chan, K.S.; Chan, Y.M.; Tan, A.H.M.; Liang, S.; Cho, Y.T.; Hong, Q.; Yong, E.; Chong, L.R.C.; Zhang, L.; Tan, G.W.L.; et al. Clinical validation of an artificial intelligence-enabled wound imaging mobile application in diabetic foot ulcers. Int. Wound J. 2022, 19, 114–124. [Google Scholar] [CrossRef]
- Elhadd, T.; Mall, R.; Bashir, M.; Palotti, J.; Fernandez-Luque, L.; Farooq, F.; Mohanadi, D.A.; Dabbous, Z.; Malik, R.A.; Abou-Samra, A.B. Artificial Intelligence (AI) based machine learning models predict glucose variability and hypoglycaemia risk in patients with type 2 diabetes on a multiple drug regimen who fast during ramadan (The PROFAST—IT Ramadan study). Diabetes Res. Clin. Pract. 2020, 169, 108388. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Kao, Y.; Hsu, C.-C.; Chen, C.-J.; Hsu, S.-L.; Liu, T.-L.; Lin, H.-J.; Wang, J.-J.; Liu, C.-F.; Huang, C.-C. Using artificial intelligence to predict adverse outcomes in emergency department patients with hyperglycemic crises in real time. BMC Endocr. Disord. 2023, 23, 234. [Google Scholar] [CrossRef] [PubMed]
- James, S.; Armstrong, M.; Abdallah, Z.; O’Kane, A.A. Chronic Care in a Life Transition: Challenges and Oppor-tunities for Artificial Intelligence to Support Young Adults with Type 1 Diabetes Moving to University. In Proceedings of the 2023 CHI Conference on Human Factors in Computing Systems (CHI ‘23), Hamburg, Germany, 23–28 April 2023; Association for Computing Machinery: New York, NY, USA, 2023; pp. 1–16. [Google Scholar]
- Kozinetz, R.M.; Berikov, V.B.; Semenova, J.F.; Klimontov, V.V. Machine Learning and Deep Learning Models for Nocturnal High- and Low-Glucose Prediction in Adults with Type 1 Diabetes. Diagnostics 2024, 14, 740. [Google Scholar] [CrossRef] [PubMed]
- Mert, M.; Vahabi, A.; Daştan, A.E.; Kuyucu, A.; Ünal, Y.C.; Tezgel, O.; Öztürk, A.M.; Taşbakan, M.; Aktuğlu, K. Artificial intelligence’s suggestions for level of amputation in diabetic foot ulcers are highly correlated with those of clinicians, only with exception of hindfoot amputations. Int. Wound J. 2024, 21, e70055. [Google Scholar] [CrossRef] [PubMed]
- Mueller, L.; Berhanu, P.; Bouchard, J.; Alas, V.; Elder, K.; Thai, N.; Hitchcock, C.; Hadzi, T.; Khalil, I.; Miller-Wilson, L.A. Application of Machine Learning Models to Evaluate Hypoglycemia Risk in Type 2 Diabetes. Diabetes Ther. 2020, 11, 681–699. [Google Scholar] [CrossRef]
- Reddy, R.; Resalat, N.; Wilson, L.M.; Castle, J.R.; El Youssef, J.; Jacobs, P.G. Prediction of Hypoglycemia During Aerobic Exercise in Adults with Type 1 Diabetes. J. Diabetes Sci. Technol. 2019, 13, 919–927. [Google Scholar] [CrossRef]
- Robinson, R.; Liday, C.; Lee, S.; Williams, I.C.; Wright, M.; An, S.; Nguyen, E. Artificial Intelligence in Health Care—Understanding Patient Information Needs and Designing Comprehensible Transparency: Qualitative Study. JMIR AI 2023, 2, e46487. [Google Scholar] [CrossRef]
- Ruan, Y.; Bellot, A.; Moysova, Z.; Tan, G.D.; Lumb, A.; Davies, J.; van der Schaar, M.; Rea, R. Predicting the Risk of Inpatient Hypoglycemia with Machine Learning Using Electronic Health Records. Diabetes Care 2020, 43, 1504–1511. [Google Scholar] [CrossRef]
- Shi, M.; Yang, A.; Lau, E.S.H.; Luk, A.O.Y.; Ma, R.C.W.; Kong, A.P.S.; Wong, R.S.M.; Chan, J.C.M.; Chan, J.C.N.; Chow, E. A novel electronic health record-based, machine-learning model to predict severe hypoglycemia leading to hospitalizations in older adults with diabetes: A territory-wide cohort and modeling study. PLoS Med. 2024, 21, e1004369. [Google Scholar] [CrossRef]
- Tao, X.; Jiang, M.; Liu, Y.; Hu, Q.; Zhu, B.; Hu, J.; Guo, W.; Wu, X.; Xiong, Y.; Shi, X.; et al. Predicting three-month fasting blood glucose and glycated hemoglobin changes in patients with type 2 diabetes mellitus based on multiple machine learning algorithms. Sci. Rep. 2023, 13, 16437. [Google Scholar] [CrossRef]
- Tarumi, S.; Takeuchi, W.; Chalkidis, G.; Rodriguez-Loya, S.; Kuwata, J.; Flynn, M.; Turner, K.M.; Sakaguchi, F.H.; Weir, C.; Kramer, H.; et al. Leveraging Artificial Intelligence to Improve Chronic Disease Care: Methods and Application to Pharmacotherapy Decision Support for Type-2 Diabetes Mellitus. Methods Inf. Med. 2021, 60 (Suppl. S01), e32–e43. [Google Scholar] [CrossRef]
- Wang, S.; Wang, J.; Zhu, M.X.; Tan, Q. Machine learning for the prediction of minor amputation in University of Texas grade 3 diabetic foot ulcers. PLoS ONE 2022, 17, e0278445. [Google Scholar] [CrossRef]
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018, 34, 285–291. [Google Scholar] [CrossRef]
- Europeiska Kommisionen. Etiska Riktlinjer för Tillförlitlig AI. 2019. Available online: https://www.europarl.europa.eu/meetdocs/2014_2019/plmrep/COMMITTEES/JURI/DV/2019/11-06/Ethics-guidelines-AI_SV.pdf (accessed on 1 March 2025).
- Shi, L.; Fonseca, V.; Childs, B. Economic burden of diabetes-related hypoglycemia on patients, payors, and employers. J. Diabetes Complicat. 2021, 35, 107916. [Google Scholar] [CrossRef]
- Kulzer, B.; Freckmann, G.; Ziegler, R.; Schnell, O.; Glatzer, T.; Heinemann, L. Nocturnal Hypoglycemia in the Era of Continuous Glucose Monitoring. J. Diabetes Sci. Technol. 2024, 18, 1052–1060. [Google Scholar] [CrossRef] [PubMed]
- Kodama, S.; Fujihara, K.; Shiozaki, H.; Horikawa, C.; Yamada, M.H.; Sato, T.; Yaguchi, Y.; Yamamoto, M.; Kitazawa, M.; Iwanaga, M.; et al. Ability of Current Machine Learning Algorithms to Predict and Detect Hypoglycemia in Patients with Diabetes Mellitus: Meta-analysis. JMIR Diabetes 2021, 6, e22458. [Google Scholar] [CrossRef] [PubMed]
- Sudharsan, B.; Peeples, M.; Shomali, M. Hypoglycemia prediction using machine learning models for patients with type 2 diabetes. J. Diabetes Sci. Technol. 2015, 9, 86–90. [Google Scholar] [CrossRef]
- Battelino, T.; Danne, T.; Bergenstal, R.M.; Amiel, S.A.; Beck, R.; Biester, T.; Bosi, E.; Buckingham, B.A.; Cefalu, W.T.; Close, K.L.; et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations From the International Consensus on Time in Range. Diabetes Care 2019, 42, 1593–1603. [Google Scholar] [CrossRef]
- Vettoretti, M.; Cappon, G.; Facchinetti, A.; Sparacino, G. Advanced Diabetes Management Using Artificial Intelligence and Continuous Glucose Monitoring Sensors. Sensors 2020, 20, 3870. [Google Scholar] [CrossRef] [PubMed]
- McCormack, B.; McCance, T.V. Development of a framework for person-centred nursing. J. Adv. Nurs. 2006, 56, 472–479. [Google Scholar] [CrossRef]
- Lundin Gurné, F.; Jakobsson, S.; Lidén, E.; Björkman, I. District nurses’ perspectives on health-promotive and disease-preventive work at primary health care centres: A qualitative study. Scand. J. Caring Sci. 2023, 37, 153–162. [Google Scholar] [CrossRef]
- Guan, Z.; Li, H.; Liu, R.; Cai, C.; Liu, Y.; Li, J.; Wang, X.; Huang, S.; Wu, L.; Liu, D.; et al. Artificial intelligence in diabetes management: Advancements, opportunities, and challenges. Cell Rep. Med. 2023, 4, 101213. [Google Scholar] [CrossRef] [PubMed]
- Norori, N.; Hu, Q.; Aellen, F.M.; Faraci, F.D.; Tzovara, A. Addressing bias in big data and AI for health care: A call for open science. Patterns 2021, 2, 100347. [Google Scholar] [CrossRef] [PubMed]
| Author(s)/Title Year, Country | Title | Method | Artificial Intelligence | Quality Score |
|---|---|---|---|---|
| 1. Chan et al. (2022) [36] Singapore | Clinical validation of an artificial intelligence-enabled wound imaging mobile application in diabetic foot ulcers | Prospective cross-sectional study | Artificial intelligence-enabled wound imaging mobile application (CARES4WOUNDS [C4W]-system | High |
| 2. Elhadd et al. (2020) [37] United States | Artificial Intelligence (AI) based machine learning models predict glucose variability and hypoglycaemia risk in patients with type 2 diabetes. on a multiple drug regimen who fast during ramadan | Prospective observational cohort study | XGBoost, a machine learning algorithm for AI, achieves high predictive performance for normal and hyperglycemic deviations | High |
| 3. Hsu et al. (2023). [38] Taiwan | Using artificial intelligence to predict adverse outcomes in emergency department patients with hyperglycemic crises in real time | Quantitative | MLP to predict negative outcomes of hyperglycemic crises in real-time | High |
| 4. James, S. et al. (2023) [39] United Kingdom | Chronic Care in a Life Transition: Challenges and Opportunities for Artificial Intelligence to Support Young Adults with Type 1 Diabetes Moving to University. | Qualitative interview study | Patients with type 1 diabetes who move out and start university described their support from technology | High |
| 5. Kozinetz, R.M. et al. (2024) [40] Russia | Machine Learning and Deep Learning Models for Nocturnal High- and Low-Glucose Prediction in Adults with Type 1 | Quantitative | MLP predicts hypoglycemia in patients with type 1 diabetes at night | High |
| 6. Mert et al. (2024) [41] Turkey | Artificial intelligence’s suggestions for level of amputation in diabetic foot ulcers are highly correlated with those of clinicians, only with exception of hindfoot amputations | Quantitative | The AI tool ChatGPT-4.0 provides recommendations for amputation. | High |
| 7. Mueller, L. et al. (2020) [42] United States | Application of Machine Learning Models to Evaluate Hypoglycemia Risk in Type 2 Diabetes. | Quantitative | Application of Machine Learning Models | High |
| 8. Reddy, R. et al. (2019) [43] United States | Prediction of Hypoglycemia During Aerobic Exercise in Adults with Type 1 Diabetes | Randomized clinical study, Quantitative | Machine learning, RF model, predicts hypoglycemia during exercise in patients with type 1 diabetes | High |
| 9. Robinson, R. et al. (2023) [44] United States | Artificial Intelligence in Health Care-Understanding Patient Information Needs and Designing Comprehensible Transparency | Qualitative study | Preferences for education and information when using AI | High |
| 10. Ruan et al. (2020) [45] United Kingdom | Predicting the Risk of Inpatient Hypoglycemia with Machine | Retrospective cohort study, Quantitative | The machine learning model with the best performance was the XGBoost model, which predicts the risk of hypoglycemia | High |
| 11. Shi et al. (2024) [46] China | Electronic health record-based, machine-learning model to predict severe hypoglycemia leading to hospitalizations in older adults with diabetes | Cohort and modeling study/case-control design for a retrospective cohort. | ML predicts the risk of hypoglycemia in patients with diabetes | High |
| 12. Tao et al. (2023) [47] China | Predicting three-month fasting blood glucose and glycated hemoglobin changes in patients with type 2 diabetes mellitus based on multiple machine learning algorithms | Prospective observational cohort study | XGBoost and ensemble learning prediction models for compliance with two blood glucose indicators in T2DM patients | High |
| 13. Tarumi et al. (2021) [48] United States | Leveraging Artificial Intelligence to Improve Chronic Disease Care: Methods and Application to Pharmacotherapy Decision Support for Type-2 Diabetes Mellitus | A quantitative analysis method was validated | The TPGE model predicts HbA1c levels in patients with type 2 diabetes | High |
| 14. Wang, S. et al. (2022) [49] China | Machine learning for the prediction of minor amputation in University of Texas grade 3 diabetic foot ulcers | Retrospective observational study | Machine learning XGBoost predicts minor amputations in diabetic foot ulcers (DFU3) | High |
| 15. Yang, H. et al. (2022) [10] China | Predicting Risk of Hypoglycemia in Patients with Type 2 Diabetes by Electronic Health Record-Based Machine Learning: Development and Validation | Retrospective cohort study, Quantitative | The XGBoost machine learning model is used based on electronic health record (EHR) to predict hypoglycemia | High |
| Artificial Intelligence as a Tool for Blood Sugar Monitoring for Patients with Diabetes |
| Artificial Intelligence as a Decision Support for Diabetic Wounds and Complications |
| Patients’ Requests for Artificial Intelligence Capabilities in Relation to Tools |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Persson, V.; Lovén Wickman, U. Artificial Intelligence as a Tool for Self-Care in Patients with Type 1 and Type 2 Diabetes—An Integrative Literature Review. Healthcare 2025, 13, 950. https://doi.org/10.3390/healthcare13080950
Persson V, Lovén Wickman U. Artificial Intelligence as a Tool for Self-Care in Patients with Type 1 and Type 2 Diabetes—An Integrative Literature Review. Healthcare. 2025; 13(8):950. https://doi.org/10.3390/healthcare13080950
Chicago/Turabian StylePersson, Vera, and Ulrica Lovén Wickman. 2025. "Artificial Intelligence as a Tool for Self-Care in Patients with Type 1 and Type 2 Diabetes—An Integrative Literature Review" Healthcare 13, no. 8: 950. https://doi.org/10.3390/healthcare13080950
APA StylePersson, V., & Lovén Wickman, U. (2025). Artificial Intelligence as a Tool for Self-Care in Patients with Type 1 and Type 2 Diabetes—An Integrative Literature Review. Healthcare, 13(8), 950. https://doi.org/10.3390/healthcare13080950






