Factors Associated with Disparities in Appropriate Statin Therapy in an Outpatient Inner City Population
Abstract
1. Introduction
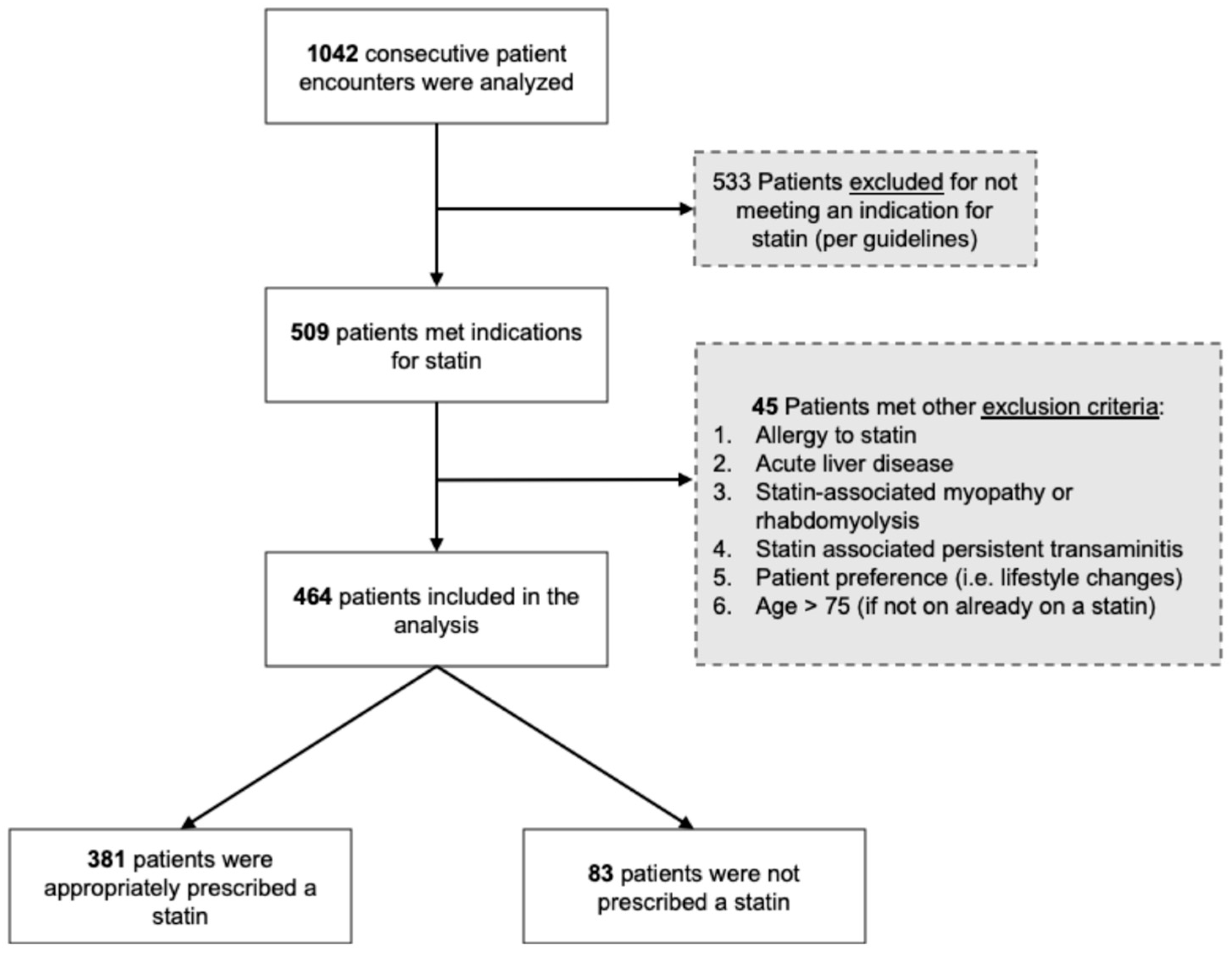
2. Materials and Methods
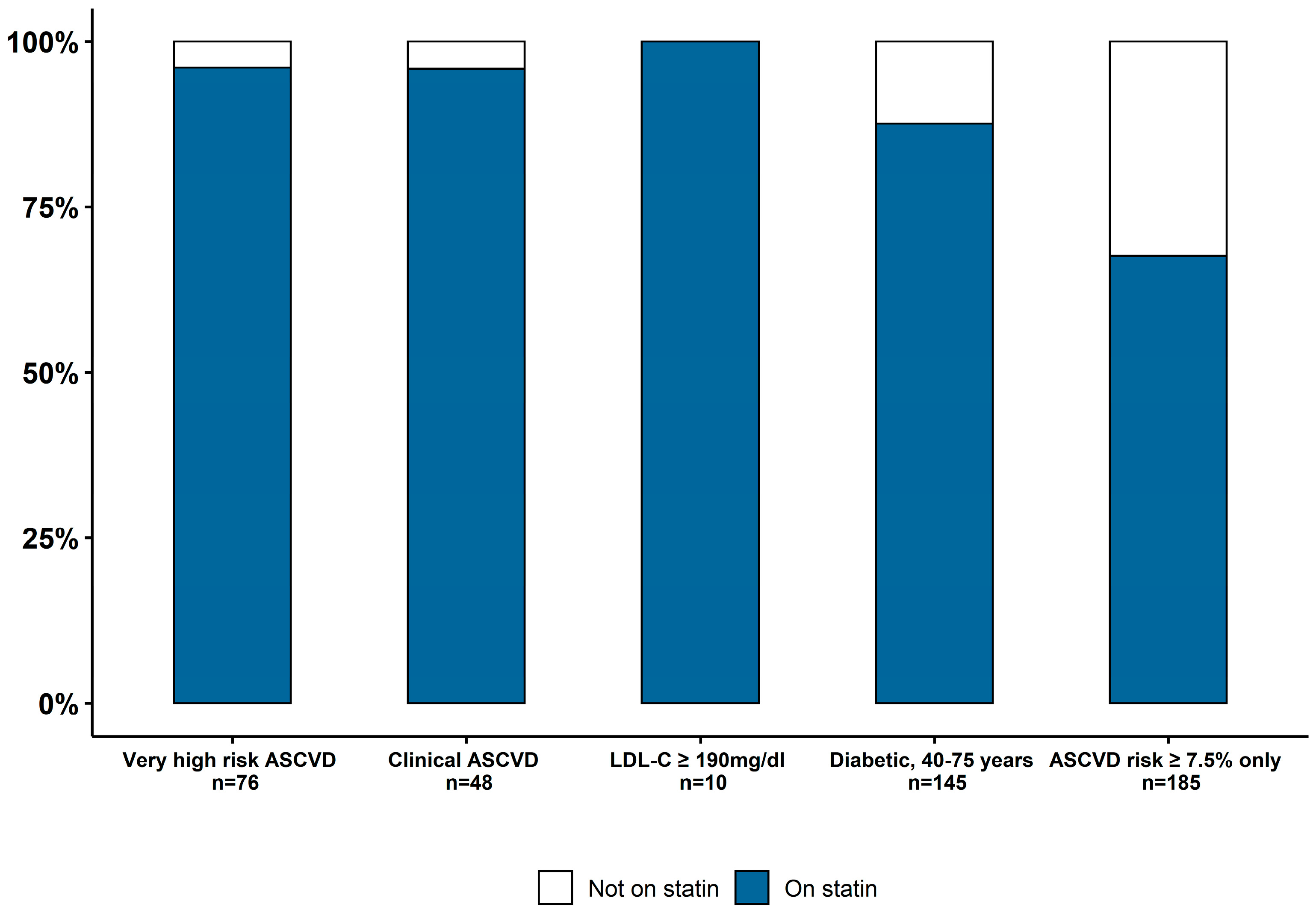
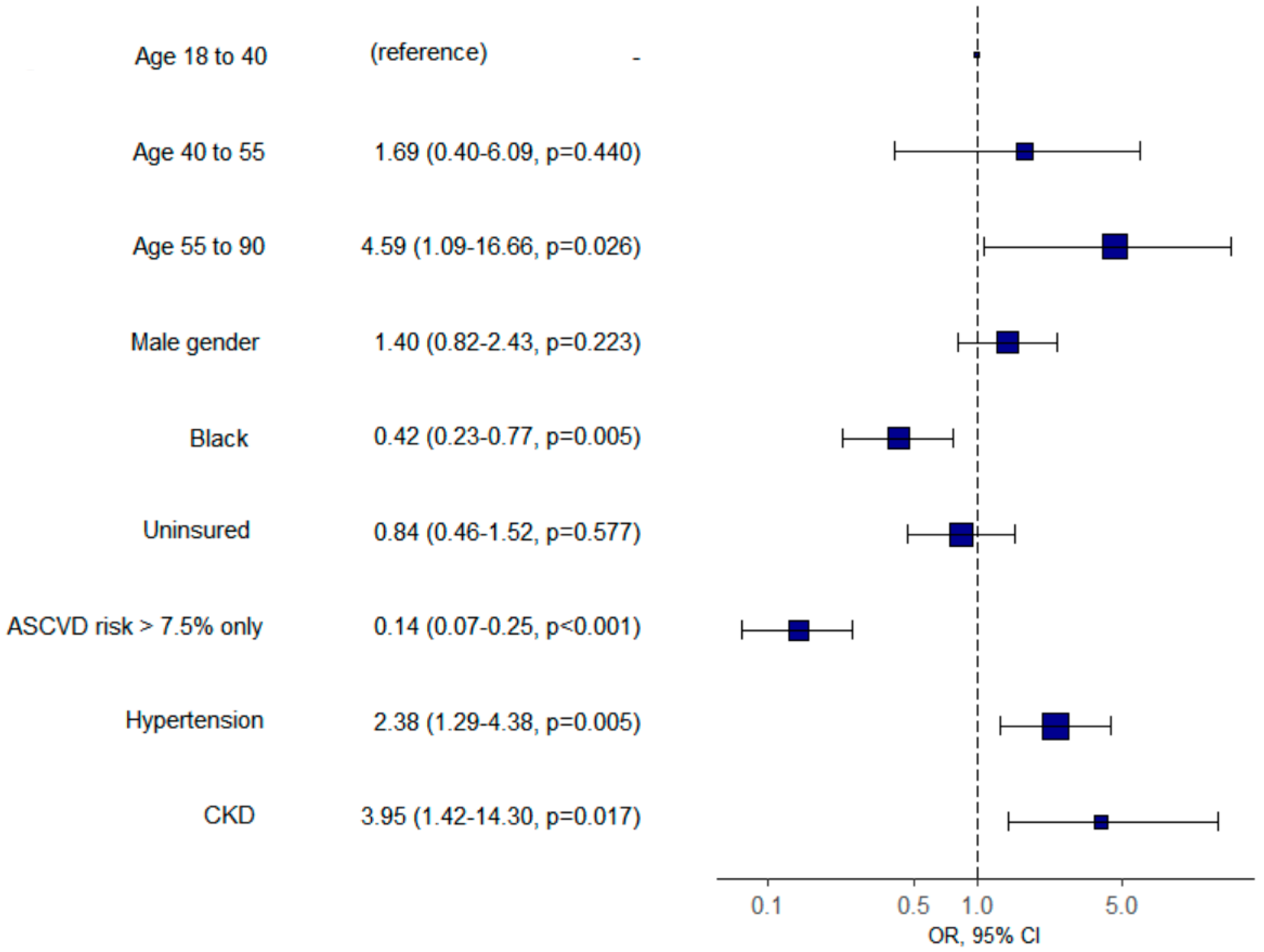
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ASCVD | atherosclerotic cardiovascular disease |
| CVD | cardiovascular disease |
| ACC | American College of Cardiology |
| AHA | American Heart Association (only 5–6 abbreviations) |
| LLT | lipid lowering therapy |
| LDL | low density lipoprotein |
References
- Heron, M. Deaths: Leading Causes for 2017; National vital statistics reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System; DHHS Publication: Atlanta, GA, USA, 2019; Volume 68, pp. 1–77. [Google Scholar]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart disease and stroke statistics-2019 update: A report from the american heart association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef] [PubMed]
- Mihaylova, B.; Emberson, J.; Blackwell, L.; Keech, A.; Simes, J.; Barnes, E.H.; Voysey, M.; Gray, A.; Collins, R.; Baigent, C. The effects of lowering ldl cholesterol with statin therapy in people at low risk of vascular disease: Meta-analysis of individual data from 27 randomised trials. Lancet 2012, 380, 581–590. [Google Scholar] [PubMed]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 aha/acc/aacvpr/aapa/abc/acpm/ada/ags/apha/aspc/nla/pcna guideline on the management of blood cholesterol: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. Circulation 2019, 139, e1082–e1143. [Google Scholar] [PubMed]
- Graham, G. Disparities in cardiovascular disease risk in the united states. Curr. Cardiol. Rev. 2015, 11, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Dorsch, M.P.; Lester, C.A.; Ding, Y.; Joseph, M.; Brook, R.D. Effects of race on statin prescribing for primary prevention with high atherosclerotic cardiovascular disease risk in a large healthcare system. J. Am. Heart Assoc. 2019, 8, e014709. [Google Scholar] [CrossRef] [PubMed]
- Vander Schaaf, E.B.; Seashore, C.J.; Randolph, G.D. Translating clinical guidelines into practice: Challenges and opportunities in a dynamic health care environment. N C Med J. 2015, 76, 230–234. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (redcap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- López-Melgar, B.; Fernández-Friera, L.; Oliva, B.; García-Ruiz, J.M.; Sánchez-Cabo, F.; Bueno, H.; Mendiguren, J.M.; Lara-Pezzi, E.; Andrés, V.; Ibáñez, B.; et al. Short-term progression of multiterritorial subclinical atherosclerosis. J. Am. Coll. Cardiol. 2020, 75, 1617–1627. [Google Scholar] [CrossRef] [PubMed]
- Hozawa, A.; Folsom, A.R.; Sharrett, A.R.; Chambless, L.E. Absolute and attributable risks of cardiovascular disease incidence in relation to optimal and borderline risk factors: Comparison of african american with white subjects—Atherosclerosis risk in communities study. Arch. Intern. Med. 2007, 167, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Schroff, P.; Gamboa, C.M.; Durant, R.W.; Oikeh, A.; Richman, J.S.; Safford, M.M. Vulnerabilities to health disparities and statin use in the regards (reasons for geographic and racial differences in stroke) study. J. Am. Heart Assoc. 2017, 6, e005449. [Google Scholar] [CrossRef] [PubMed]
- Nanna, M.G.; Navar, A.M.; Zakroysky, P.; Xiang, Q.; Goldberg, A.C.; Robinson, J.; Roger, V.L.; Virani, S.S.; Wilson, P.W.F.; Elassal, J.; et al. Association of patient perceptions of cardiovascular risk and beliefs on statin drugs with racial differences in statin use: Insights from the patient and provider assessment of lipid management registry. JAMA Cardiol. 2018, 3, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, C.J.; Daviglus, M.L.; Swett, K.; González, H.M.; Gallo, L.C.; Wassertheil-Smoller, S.; Giachello, A.L.; Teng, Y.; Schneiderman, N.; Talavera, G.A.; et al. Dyslipidemia patterns among hispanics/latinos of diverse background in the united states. Am. J. Med. 2014, 127, 1186–1194. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, C.J.; Cai, J.; Swett, K.; González, H.M.; Talavera, G.A.; Wruck, L.M.; Wassertheil-Smoller, S.; Lloyd-Jones, D.; Kaplan, R.; Daviglus, M.L. High cholesterol awareness, treatment, and control among hispanic/latinos: Results from the hispanic community health study/study of latinos. J. Am. Heart Assoc. 2015, 4, e001867. [Google Scholar]
- Qato, D.M.; Lee, T.A.; Durazo-Arvizu, R.; Wu, D.; Wilder, J.; Reina, S.A.; Cai, J.; Gonzalez, F., 2nd; Talavera, G.A.; Ostfeld, R.J.; et al. Statin and aspirin use among hispanic and latino adults at high cardiovascular risk: Findings from the hispanic community health study/study of latinos. J. Am. Heart Assoc. 2016, 5, e002905. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 464) | Statin Prescribed (n = 381) | Statin Not Prescribed (n = 83) | p | |
|---|---|---|---|---|
| Demographics | ||||
| Age, years | 61.0 (10.4) | 61.8 (10.5) | 57.2 (9.1) | 0.0001 |
| Males, n (%) | 214 (46.1) | 177 (46.5) | 37 (44.6) | |
| Race/Ethnicity, n (%) | 0.12 | |||
| Black or African American | 219 (47.2) | 169 (44.4) | 50 (60.2) | |
| Hispanic or Latino | 212 (45.7) | 184 (48.3) | 28 (33.7) | |
| White | 23 (5.0) | 19 (5.0) | 4 (4.8) | |
| Asian | 9 (1.9) | 8 (2.1) | 1 (1.2) | |
| Native Hawaiian/Pacific Islander | 1 (0.2) | 1 (0.3) | 0 (0.0) | |
| Primary Language, n (%) | 0.500 | |||
| English | 284 (61.2) | 227 (59.6) | 57 (68.7) | |
| Spanish | 130 (28.0) | 111 (29.1) | 19 (22.9) | |
| Portuguese | 31 (6.7) | 26 (6.8) | 5 (6.0) | |
| Other | 15 (3.2) | 14 (3.7) | 1 (1.2) | |
| French Creole | 4 (0.9) | 3 (0.8) | 1 (1.2) | |
| Translator utilized/Physician fluent | 127 (27.4) | 107 (28.1) | 20 (24.1) | 0.656 |
| Uninsured, n (%) | 254 (54.7) | 207 (54.3) | 47 (56.6) | 0.796 |
| BMI, kg/m2 | 29.4 [25.7–33.4] | 29.4 [25.8–33.3] | 29.0 [25.2–35.1] | 0.875 |
| Comorbidities, n (%) | ||||
| Hypertension | 376 (81.0) | 320 (84.0) | 56 (67.5) | 0.001 |
| Systolic BP | 142.0 (65.3) | 142.1 (71.5) | 141.7 (21.0) | 0.956 |
| Diastolic BP | 73.7 (12.0) | 73.0 (11.5) | 77.0 (13.5) | 0.006 |
| Diabetes Mellitus | 209 (45.0) | 209 (45.0) | 209 (45.0) | 0.0001 |
| Hemoglobin A1c | 7.2 [6.5–8.9] | 7.2 [6.5–8.9] | 7.2 [6.5–8.9] | 0.063 |
| Chronic kidney disease | 71 (15.3) | 67 (17.6) | 4 (4.8) | 0.006 |
| Congestive heart failure | 60 (12.9) | 56 (14.7) | 4 (4.8) | 0.024 |
| Coronary artery disease | 67 (14.4) | 67 (17.6) | 0 (0.0) | 0.0001 |
| History of MI | 32 (6.9) | 31 (8.2) | 1 (1.2) | 0.043 |
| History of PCI | 30 (6.5) | 30 (7.9) | 0 (0.0) | 0.017 |
| History of CABG | 15 (3.2) | 15 (3.9) | 0 (0.0) | 0.135 |
| Cerebrovascular disease | 68 (14.7) | 65 (17.1) | 3 (3.6) | 0.003 |
| Peripheral artery disease | 13 (2.8) | 12 (3.1) | 1 (1.2) | 0.545 |
| Current smoker | 83 (17.9) | 63 (16.5) | 20 (24.1) | 0.206 |
| Lipid profile, mg/dL | ||||
| LDL-C | 87.0 [64.0–120.0] | 84.0 [62.5–121.0] | 93.0 [72.0–112.5] | 0.339 |
| HDL-C | 50.0 [41.0–59.0] | 49.0 [40.0–58.0] | 52.0 [43.8–63.8] | 0.048 |
| Triglycerides | 103.0 [78.0–149.0] | 104.5 [80.2–150.0] | 95.5 [69.5–135.8] | 0.056 |
| Statin Indications, n (%) | 0.0001 | |||
| Very high-risk ASCVD | 76 (16.4) | 73 (19.2) | 3 (3.6) | |
| Clinical ASCVD | 48 (10.3) | 46 (12.1) | 2 (2.4) | |
| 10-year ASCVD risk >7.5 | 185 (39.9) | 125 (32.8) | 60 (72.3) | |
| Diabetes, age 40–75 | 145 (31.2) | 127 (33.3) | 18 (21.7) | |
| LDL-C >190mg/dL | 10 (2.2) | 10 (2.6) | 0 (0.0) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suero-Abreu, G.A.; Karatasakis, A.; Rashid, S.; Tysarowski, M.; Douglas, A.; Patel, R.; Siddiqui, E.; Bhardwaj, A.; Gerula, C.M.; Matassa, D. Factors Associated with Disparities in Appropriate Statin Therapy in an Outpatient Inner City Population. Healthcare 2020, 8, 361. https://doi.org/10.3390/healthcare8040361
Suero-Abreu GA, Karatasakis A, Rashid S, Tysarowski M, Douglas A, Patel R, Siddiqui E, Bhardwaj A, Gerula CM, Matassa D. Factors Associated with Disparities in Appropriate Statin Therapy in an Outpatient Inner City Population. Healthcare. 2020; 8(4):361. https://doi.org/10.3390/healthcare8040361
Chicago/Turabian StyleSuero-Abreu, Giselle Alexandra, Aris Karatasakis, Sana Rashid, Maciej Tysarowski, Analise Douglas, Richa Patel, Emaad Siddiqui, Aishwarya Bhardwaj, Christine M. Gerula, and Daniel Matassa. 2020. "Factors Associated with Disparities in Appropriate Statin Therapy in an Outpatient Inner City Population" Healthcare 8, no. 4: 361. https://doi.org/10.3390/healthcare8040361
APA StyleSuero-Abreu, G. A., Karatasakis, A., Rashid, S., Tysarowski, M., Douglas, A., Patel, R., Siddiqui, E., Bhardwaj, A., Gerula, C. M., & Matassa, D. (2020). Factors Associated with Disparities in Appropriate Statin Therapy in an Outpatient Inner City Population. Healthcare, 8(4), 361. https://doi.org/10.3390/healthcare8040361





