Abstract
Nursing home placement after stroke indicates a poor outcome but numbers placed vary between hospitals. The aim of this study is to determine whether between-hospital variations in new nursing home placements post-stroke are reliant solely on case-mix differences or whether service heterogeneity plays a role. A prospective, multi-center cohort study of acute stroke patients admitted to eight National Health Service acute hospitals within the Anglia Stroke and Heart Clinical Network between 2009 and 2011 was conducted. We modeled the association between hospitals (as a fixed-effect) and rates of new discharges to nursing homes using multiple logistic regression, adjusting for important patient risk factors. Descriptive and graphical data analyses were undertaken to explore the role of hospital characteristics. Of 1335 stroke admissions, 135 (10%) were discharged to a nursing home but rates varied considerably from 6% to 19% between hospitals. The hospital with the highest adjusted odds ratio of nursing home discharges (OR 4.26; 95% CI 1.69 to 10.73), was the only hospital that did not provide rehabilitation beds in the stroke unit. Increasing hospital size appeared to be related to an increased odds of nursing home placement, although attenuated by the number of hospital stroke admissions. Our results highlight the potential influence of hospital characteristics on this important outcome, independently of patient-level factors.
Keywords:
nursing home; institutionalization; acute hospitals; health services research; stroke; UK; NHS 1. Introduction
Stroke is the second leading cause of mortality and the third leading cause of disability worldwide [1]. Given the significant impact that a stroke can have on the ability to perform daily tasks, many patients require institutionalization. In the UK, for example, 8.2% of patients surviving stroke are discharged to a care home [2]. However, changing demographics, improvements in stroke care and post-acute care provision (i.e., widespread incorporation of early supported discharge policies) have led to a significant reduction in institutionalization rates since 1995 [3].
Home discharge is the most desirable outcome following stroke; 85% of patients in a previous study favored returning home for reasons such as increased autonomy and privacy [4]. Furthermore, greater long-term improvements have been observed in patients that return home [5].
Understanding what determines a patient’s discharge destination after stroke can provide invaluable information to identify factors that can be modified to prevent the need for nursing home placement. This information is also important in ensuring efficient discharge planning. If discharge to a nursing home can be anticipated then communication between different health care providers can be initiated early, as well as discussions with the patient and their family. In UK hospitals, the decision as to the patient’s discharge destination following stroke is arrived at collaboratively following input from the patient, the patient’s family, the leading physician, social work, and other allied health professionals.
To date, most studies have focused on what patient characteristics drive the need for nursing home placement after stroke. Other important factors, such as differences in service provision and resources, may impact the need for institutionalization. However, few have researched this specifically, despite a wealth of research showing the importance of hospital factors such as staffing levels and hospital stroke volume on other outcomes [6,7,8,9,10].
The aim of this study, therefore, was to examine whether variations in discharge to nursing homes after stroke could, in part, be explained by heterogeneities in hospital-related factors.
2. Materials and Methods
2.1. Study Design
A multi-centre, prospective cohort study conducted at eight acute NHS hospitals within the Anglia Stroke and Heart Clinical Network (AS&HCN) which participated in the Anglia Stroke Clinical Network Evaluation Study (ASCNES). The network covers three counties in the East of England, UK, with a catchment population of approximately 2.5 million. The ASCNES primary outcome of interest was one-year mortality, whereas discharge destination, the focus of this paper, was one of the secondary outcomes of interest. The detailed study protocol has been previously published [11].
2.2. Participants
The study population included all patients, aged 18 years or older, admitted to any of the eight hospitals (which spanned both urban and rural regions) within the ASCNES group diagnosed with stroke by an accredited stroke physician. Diagnoses by the stroke physician were coded using International Classification of Diseases-10 (ICD-10) and were confirmed through cerebral imaging. Stroke was defined as a focal neurological impairment of sudden onset and lasting more than 24 h (or leading to death) because of an intracerebral ischemic or hemorrhagic event. This definition was used in order to exclude diagnoses of transient ischaemic stroke, subdural hematomas, and subarachnoid hemorrhages. The study sample was systematically selected to include all patients with stroke admitted every third month of a two-year period (October 2009 to September 2011), resulting in a total of eight study months; the robustness of this sampling technique has been verified [12]. Patients who were previously resident in a nursing home prior to their admission for stroke, patients who died as an inpatient or those who were discharged to an interim or rehabilitation setting were all excluded from the final study population.
2.3. Data Collection
This study made use of prospectively collected anonymized data that were routinely sent to the AS&HCN for performance assessment, in addition to baseline patient and outcome data retrieved from case records and discharge summaries by clinical teams. Any identifiable patient information was held only at the individual hospitals—the network and investigators did not have access to these details.
Data on hospital-level characteristics were collected from clinical leads or service managers at each hospital and updated every six months over the two-year study period by research staff [11].
2.4. Statistical Analyses
We performed a single-level multiple logistic regression model using maximum likelihood with the hospital as a fixed-effect. Our outcome measure was new nursing home placement at discharge from acute hospitalization for stroke amongst those who were not previously institutionalized. Cases discharged to a nursing home were treated as the event group, whilst those who were discharged back home (including those living in sheltered accommodation or retirement home) constituted the non-event group.
Patient risk factors of institutionalization following stroke were identified a priori from a literature review (see Supplementary Table S1). The distribution of the patient risk factors available in the dataset was examined between hospitals using hypothesis testing. Factors that were unevenly distributed amongst the hospitals (p-value set at 0.05 significance level) were included in the main model as they were considered potential confounders of the relationship between our independent variable (hospital) and outcome of interest (institutionalization). These included a patient’s pre-stroke modified Rankin Scale (mRS) score, discharge mRS score, acute hospital length of stay, and whether the patient had a total anterior circulation stroke (TACS), history of myocardial infarction or ischemic heart disease, or developed an inpatient complication (see Supplementary Table S2). For the interest of the reader, we provide Supplementary Table S3 with a breakdown of the different types of complications recorded and the proportion of patients that were reported to have developed them. Furthermore, although we identified stroke severity as an important risk factor, 73% of cases had missing data on The National Institutes of Health Stroke Scale (NIHSS) score, and we believe that this variable was only collected in patients that were eligible for thrombolysis. Therefore, we did not multiply impute this variable due to the potential for introducing information bias. Instead, we adjusted for proxy variables of stroke severity, such as discharge mRS score [13], whether the patient had a TACS [14,15], or showed symptoms of brain lateralization. We hypothesized that patients with no symptoms of brain lateralization are likely to be those with more severe stroke where the whole brain is affected.
Processes of care measures such as the delivery of acute treatment therapies were not accounted for in our study as we believe they are mediator variables that lie on the causal pathway between hospital-level factors and stroke patient outcomes [16]. Their inclusion in our regression model could otherwise lead to over-adjustment bias by obscuring the overall effect of the hospital [17,18].
To explore hospital-level factors we first compared, descriptively, service variations between hospitals. We also plotted the adjusted odds ratio of new nursing home placement (estimated from the regression model) against the hospital characteristics of interest for each hospital. This is the favored approach when the sample size of hospitals is below the suggested critical number required to reliably estimate hospital effects through multi-level modelling [19,20]. Hospital characteristics included hospital size (number of hospital beds), hospital type (secondary or tertiary), hospital stroke volume (number of stroke admissions per month), presence of vascular surgery onsite, distance to a neurosurgical facility, number of full-time-equivalent (fte) staff per five beds (including doctors, nurses, occupational therapists, speech and language therapists, physiotherapists and dieticians), number of stroke unit beds per 100 admissions, number of hospital beds per CT scanner, number of non-stroke patients treated on the stroke unit per five beds, and number of patients with stroke treated outside the stroke unit per five beds.
The index of multiple deprivation (IMD) score was also explored graphically to assess whether the socio-economic status of the hospital catchment area may explain any differences in outcome observed between hospitals. This is an aggregate measure and is based on several domains, including income, employment, education, health, crime, barriers to housing and services and the living environment, that are believed to provide an indication of deprivation. England is subdivided into 32, 844 smaller areas, with an IMD score of 1 representing the area in England that is considered to be the most deprived and a score of 32, 844 the least deprived [21]. Here we assigned the mean 2010 IMD scores of the areas that make up the counties of Suffolk, Norfolk and Cambridgeshire and assigned these to each of the hospitals to which they are located [22].
We carried out multiple imputations by chained equations using the Multivariate Imputation by Chained Equations (MICE) package in R and pooled the results using Rubin’s rules [23] (see Supplementary Table S4 for details on variables used to inform multiple imputations). The inclusion of auxiliary variables for the imputation increased the casewise missingness to 43%, thus 43 datasets were imputed. The distribution of sample characteristics between individuals with complete and incomplete data was compared using the appropriate statistical tests (Supplementary Table S5). Findings from the complete case analysis are presented in Supplementary Table S6.
2.5. Sensitivity Analyses
We performed two sensitivity analyses to check the robustness of our findings. The first of these included all patient risk factors identified a priori in a literature review that were available in our dataset irrespective of whether they were evenly distributed between hospitals or not, and the second excluded hospital 2 which did not contribute data after January 2010.
All analyses were performed using R version 3.3.1 (R, Vienna, Austria) for Windows [24].
2.6. Ethics Approval
Ethical approval was obtained from the NRES Committee East of England—Norfolk (REC Reference number 10/H0310/44).
3. Results
Of the 2656 patients admitted during the inclusion period, 179 were eventually diagnosed with a condition other than stroke. After exclusions (see Supplementary Figure S1), a total of 1335 cases were available for analyses (median age (IQR) 79 (70 to 86 years), 52% males, 83% ischemic stroke).
A total of 135 (10%) patients were placed in a nursing home at discharge, with the remaining 90% discharged home. The proportion of patients discharged to a nursing home varied between hospitals (6% in hospital 1 to 19% in hospital 3). The unadjusted odds of being discharged to a nursing home in hospital 3 were 3.84 times that of hospital 1; the highest odds of all hospitals in the study (p < 0.001). All other hospitals were associated with greater odds of nursing home placement than hospital 1, although none reached statistical significance.
To note, when examining the original study population (including those who were discharged to settings other than home or nursing homes) the hospitals with the lowest rates of nursing home placements were not the hospitals with the highest proportion of patients discharged to an interim or rehabilitation setting, or who died as an inpatient (Supplementary Figure S2).
Between-hospital variations in rates of nursing home placement remained after the adjustment of patient confounders (Table 1). Hospital 3 still had the highest odds of discharges to nursing homes (Odds Ratio (OR) 4.26; 95% confidence interval (CI) 1.69 to 10.73). Due to low event numbers in the other hospitals, none of these were statistically significantly different from hospital 1, and all had wide confidence intervals. Findings were similar for the complete case analysis (Supplementary Table S6) and sensitivity analyses (Table 2).

Table 1.
Frequency of patients with stroke admitted and discharged to a nursing home placement (NHP) per hospital, and unadjusted odds ratio (OR) and 95% confidence intervals (CI) for new nursing home placement according to hospital (n = 1335).

Table 2.
Results of the sensitivity analyses with adjusted odds ratio (OR) and 95% confidence intervals (CI) for new nursing home placement according to hospital presented.
Table 3 outlines the service characteristics of each hospital, including standardized staffing levels, bed capacity, and the availability of onsite facilities. There is notable heterogeneity in service provision and resource levels. For example, only hospital 1 had a neurosurgical facility onsite and only hospitals 1, 3, 5 and 6 had onsite vascular surgery.

Table 3.
Hospital characteristics per individual hospital.
Hospital 3, with the highest odds ratio, and the only hospital that showed a statistically significant difference compared to hospital 1, was the study’s largest secondary hospital and was the only hospital that did not have any rehabilitation beds within the stroke unit. It also had the highest number of junior doctors and occupational therapists per five beds but one of the lowest number of nurses per five beds. Compared to hospital 1, hospital 3 was smaller, had a lower volume, had less stroke unit beds per 100 admissions, fewer hospital beds per CT scanner, had more senior doctors, junior doctors, physiotherapists and occupational therapists per fives beds, had fewer nurses, speech and language therapists and dieticians per five beds, less non-stroke patients treated on the stroke unit and fewer patients with stroke treated outside the stroke unit.
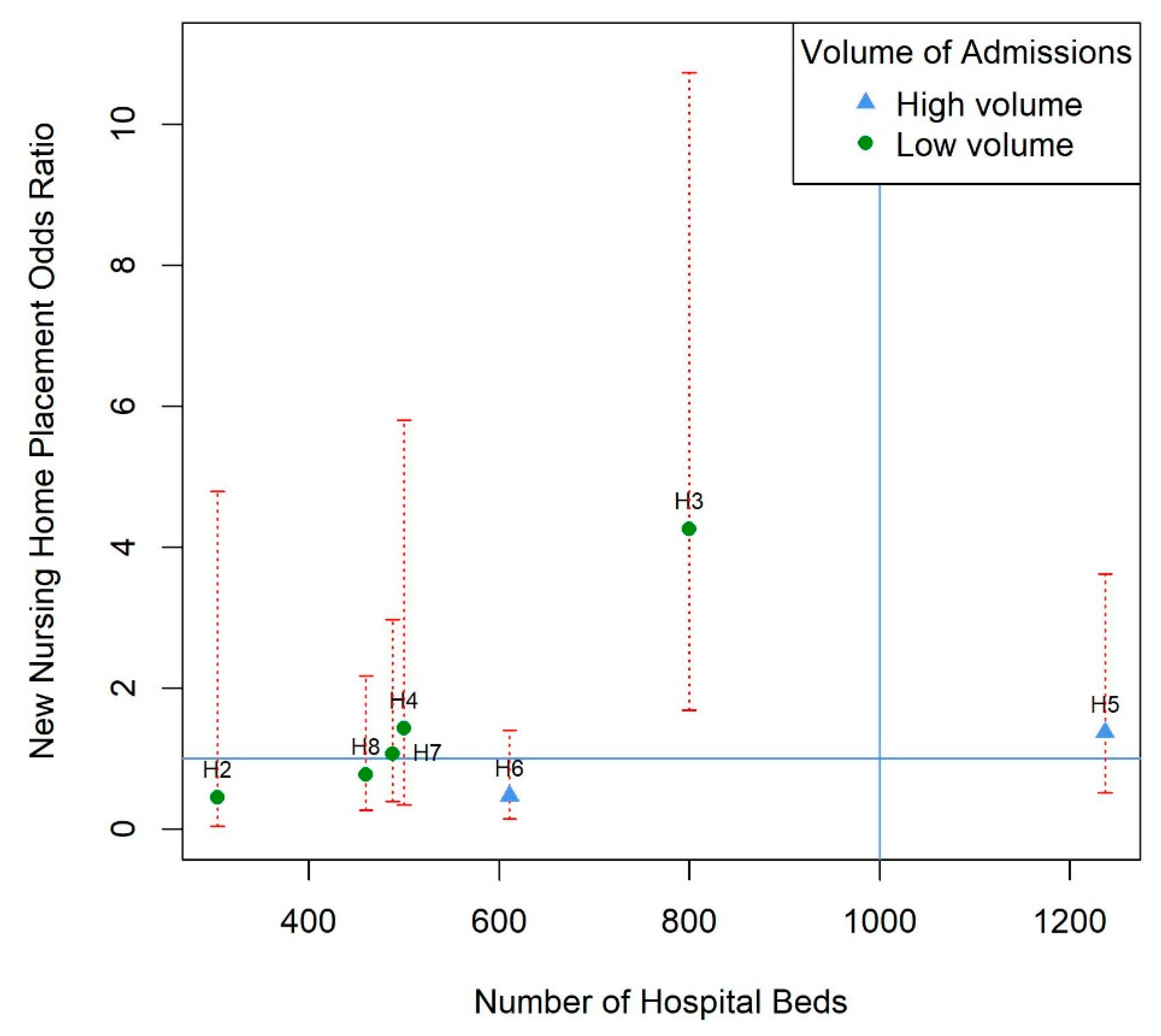
No obvious patterns emerged for any of the hospital characteristics in our graphical analysis (Supplementary Figures S3–S20). However, when we plotted hospital size against the adjusted odds ratio of nursing home placement, and grouped by hospital stroke volume, there was a clear positive linear trend in point estimates, although confidence intervals were wide. The increased odds ratio with hospital size was much more attenuated in the group of hospitals that admitted more than 50 patients with stroke a month (see Figure 1).
Figure 1.
Model estimates of new nursing home placement odds ratio for each hospital against the size of the hospital (total number of hospital beds) and grouped by hospital stroke volume with 95% confidence intervals (red dotted lines). Volume is categorized into high (more than 50 admissions per month) and low (less than 50 admissions per month). Horizontal line represents an odds ratio of 1 for reference hospital 1. Vertical line represents the hospital size in hospital 1. This line is blue because the volume of stroke admissions is more than 50 admissions per month for this hospital. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, total anterior circulation stroke (TACS), myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputations for missing covariate data. H2–H8: hospital 2 to 8, consecutively.
4. Discussion
Considerable variations in rates of new nursing home placements after stroke exist between hospitals in the UK NHS setting even after the adjustment of case-mix differences. These variations cannot be explained in terms of differences in rates of discharges to interim or rehabilitation settings, or inpatient deaths. Instead, they appear to reflect heterogeneities in service provision and resource levels between hospitals. Our exploratory analyses indicated the potential importance of the provision of rehabilitation beds within the stroke unit, hospital size and volume.
Our main finding agrees with a previous study conducted across health regions in the UK [25]. Here, we suggest that differences in hospital characteristics may partly explain these between-hospital variations. The superiority of stroke rehabilitation that is provided within a comprehensive stroke unit (i.e., where patients receive acute treatment and rehabilitation in combination) compared to rehabilitation provided outside the unit has been previously demonstrated [26,27,28]. Therefore, we surmise that this may be one driving force behind the high rate of nursing home placements in hospital 3 as this was the only hospital that did not provide rehabilitation beds in the stroke unit. It is unclear why this would have an effect on discharge destination; although it has been suggested that early mobilization and rehabilitation on these wards may lead to better functional gains in patients, allowing them to safely return home [28], a recent systematic review was unable to find conclusive evidence that early mobilization leads to improved outcomes after stroke [29].
This study also highlights the potential importance of hospital size and the volume of stroke admissions. In addition to hospital 3 being the study’s largest, secondary hospital, our graphical exploration demonstrated a strong positive trend between hospital size and our outcome, for low volume hospitals. This finding may reflect heightened resource pressure in larger hospitals. Indeed, out of all the other secondary hospitals, hospital 3 had the highest ratio of hospital beds to CT scanners. Pressure on CT scanners may lead to a delay in a confirmatory diagnosis and treatment, subsequently hindering recovery and making a safe discharge home less probable [30].
Larger patient volumes have been linked to improved outcomes in stroke [6,10]. This may be because physicians in high volume hospitals gain more experience in dealing with certain conditions and are therefore better placed at providing effective care [31,32]. Our finding that the effect of hospital size appears to be attenuated by hospital stroke volume appears to align with this and studies that have shown that whilst larger hospitals are associated with poorer outcomes, higher volume hospitals produce better results [33,34].
The main strength of our study is its prospective design which facilitated the collection of detailed and accurate patient and hospital-level data. This minimized residual confounding by case-mix differences and allowed us to explore several hospital characteristics. We did not restrict our analysis to certain sub-populations, meaning our results are generalizable to the wider stroke population. Multiple imputations also minimized any biases that would have arisen from the complete case analysis. Another strength was that our statistical approach was the most robust and economical way to use the data available. The sensitivity analyses conducted further confirmed the vigor of our findings. Very few other studies have looked at the influence of hospital characteristics on this outcome. This study, by appropriately adjusting for patient confounders and clustering of observations at the hospital-level is novel in its approach and clearly demonstrates the importance of hospital characteristics.
It should be noted, however, that this study did have some limitations. The small number of hospitals sampled prevented us from carrying out a multi-level model which would have enabled us to calculate direct estimates of hospital-level effects. Furthermore, the small event numbers per hospital led to wide confidence intervals and difficulty in interpreting our results for most hospitals. This limitation arose because the sample size calculation for the ASCNES study was arrived at partly pragmatically due to its exploratory nature, and was based on the primary outcome of one-year mortality. Therefore, it did not account for the low event size of this secondary outcome, and the exclusion criteria of this present study. A larger sample size would have allowed us to statistically test for the interaction between hospital size and hospital stroke volume in influencing nursing home placement. As service characteristics were self-reported by hospital managers and service providers, information bias may also have been introduced. Moreover, we were unable to adjust for stroke severity and other established risk factors of institutionalization after strokes, such as ethnicity [35,36] and socio-economic status. However, we adjusted for proxy variables of stroke severity, such as whether the patient had a TACS [14] or showed symptoms of brain lateralization. Additionally, the region where the study was conducted serves mainly a white British Caucasian population [37], and hence any potential confounding by race will have been limited. Furthermore, although we used an aggregate measure of socio-economic status and did not find an obvious pattern in our graphical exploration of hospital factors, we cannot be sure whether this resulted in some residual confounding.
Finally, advances in stroke management over the past decade have occurred since the collection of the ASCNES data, and this has likely led to differences in the discharge destinations of patients. However, variations in rates of nursing home placements still exist between hospitals [2], which may be partly due to differences in hospital characteristics. Our study supports that variations in patient outcomes are influenced, in part, by hospital characteristics. This is still relevant despite changes in acute therapy and post-acute care, and thus should be explored further in the current context.
5. Conclusions
Overall, this study furthers the knowledge of nursing home discharges after strokes, an important outcome for patients, relatives, and health care providers, by illustrating that hospital characteristics do seem to play an important role in driving variations between hospitals. Further confirmatory work could lead to the development and implementation of health services research in this area.
Supplementary Materials
The following are available online at https://www.mdpi.com/2227-9032/8/4/390/s1, Table S1 Summary of findings from a priori literature review evaluating what patient factors influence nursing home placement (institutionalization) after acute hospitalization for stroke, Table S2 Distribution of patient risk factors of the 1335 patients included in analysis per individual hospital (n [%] unless otherwise stated), Table S3 Breakdown of the type of inpatient complications recorded and the proportion of patients recorded with each, Table S4 Variables used to inform multiple imputation of missing data, Table S5 Comparison of patient characteristics between complete cases and those with at least one missing variable, Table S6 Multiple logistic regression complete case analysis for new nursing home placement after hospitalization for stroke (n = 972), Figure S1 Flow chart of cases included for the analysis, illustrating the reasons for exclusion, Figure S2 Stacked bar chart showing the proportion of patients that were discharged either to a nursing home (red), back home (blue), to an interim/rehabilitation setting (grey) or died as an inpatient (white), per hospital. H1 to H8 represent hospitals 1 to 8 inclusively, Figure S3 Model estimates of new nursing home placement odds ratio for each hospital and hospital type. Horizontal line represents an odds ratio of 1 for reference hospital 1; its green colour represents that it is a tertiary hospital. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data Figure S4 Model estimates of new nursing home placement odds ratio for each hospital against size of hospital (represented as number of total hospital beds). Horizontal line represents an odds ratio of 1 for reference hospital 1. Vertical line represents the size of hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S5 Model estimates of new nursing home placment odds ratio for each hospital against hospital stroke volume (mean number of stroke patients admitted and treated in each hospital per month). Horizontal line represents an odds ratio of 1 for reference hospital 1. Vertical line represents the stroke volume of hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S6 Model estimates of new nursing home placement odds ratio for each hospital against distance to neurosurgical facilities (in miles). Horizontal line represents an odds ratio of 1 for reference hospital 1. Vertical line illustrates that neurosurgery was available onsite at hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S7 Model estimates of new nursing home placement odds ratio for each hospital against presence of vascular surgery onsite. Horizontal line represents an odds ratio of 1 for reference hospital 1; its blue colour represents that it does not have a vascular surgery onsite. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, S8 Model estimates of new nursing home placement odds ratio for each hospital against number of senior doctors per five stroke unit beds. Horizontal line represents an odds ratio of 1 for reference hospital 1. Vertical line represents the senior doctor staffing level for the hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S9 Model estimates of new nursing home placement odds ratio for each hospital against number of junior doctors per five stroke unit beds. Horizontal line represents an odds ratio of 1 for reference hospital 1. Vertical line represents the junior doctor staffing level for hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S10 Model estimates of new nursing home placement odds ratio for each hospital against number of nurses per five stroke unit beds. Horizontal line represents an odds ratio of 1 for reference hospital 1. Vertical line represents the nurse staffing levels for hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S11 Model estimates of new nursing home placement odds ratio for each hospital against number of occupational therapists per five bed days. Horizontal line represents an odds ratio of 1 for reference hospital 1. Veritical line represents the staffing levels of occupational therapists in hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S12 Model estimates of new nursing home placement odds ratio for each hospital against the number of physiotherapists per five stroke unit beds. Horizontal line represents an odds ratio of 1 for reference hospital 1. Vertical line represents the staffing levels of physiotherapists in hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S13 Model estimates of new nursing home placement odds ratio for each hospital against the number of speech and language therapists per five stroke unit beds. Horizontal line represents an odds ratio of 1 for reference hospital 1. Vertical line represents the staffing levels of speech and language therapists in hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S14 Model estimates of new nursing home placement odds ratio for each hospital against the number of dieticians per five stroke unit beds. Horizontal line represents an odds ratio of 1 for reference hospital 1. Vertical line represents the staffing levels of dieticians in hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S15 Model estimates of new nursing home placement odds ratio for each hospital against number of hospital beds per CT scanner. Horizontal line represents an odds ratio of 1 for reference hospital 1. Vertical line represents the numer of hospital beds per CT scanner in hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S16 Model estimates of new nursing home placement odds ratio for each hospital against number of stroke unit beds per 100 admissions. Horizontal line represents an odds ratio of 1 for reference hospital 1. Verical line represents the number of stroke unit beds for hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S17 Model estimates of new nursing home placement odds ratio for each hospital against number of non-stroke patients treated daily on the stroke unit per five beds. Horizontal line represents an odds ratio of 1 for hospital 1. Verical line represents the number of non-stroke patients treated daily on the stroke unit of hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S18 Model estimates of new nursing home placement odds ratio for each hospital against number of patients with stroke treated daily outside the stroke unit per five beds. Horizontal line represents an odds ratio of 1 for reference hospital 1. Verical line represents the number of patients with stroke treated outside the stroke unit per five beds for hospital 1. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S19 Model estimates of new nursing home placement odds ratio for each hospital against presence of early supported discharge (ESD) policy. Horizontal line represents an odds ratio of 1 for reference hospital 1; its blue colour represents that it does not have an ESD policy. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data, Figure S20 Model estimates of new nursing home placement odds ratio for each hospital against mean Index of Multiple Deprivation (IMD) score of the counties in which the hospital services, with 95% confidence intervals. Horizontal line represents an odds ratio of 1 for reference hospital 1; its blue colour represents that hospital 1 is located in a county with an IMD mean score of 13.89. Multivariable regression model was adjusted for pre-stroke mRS score, discharge mRS score, TACS, myocardial infarction or ischemic heart disease, complication, brain lateralization, and acute hospital length of stay, after multiple imputation for missing covariate data.
Author Contributions
Conceptualization, P.K.M., D.J.D., M.O.B., E.A.W. and J.F.P.; methodology, P.K.M., D.J.D., M.O.B., E.A.W., J.F.P., D.M. and M.T.; formal analysis, M.T. and D.M.; data curation, S.D.M., M.T. and P.K.M.; writing—original draft preparation, M.T.; writing—review and editing, M.T., P.K.M., and D.M.; visualization, M.T.; supervision, P.K.M. and D.M.; project administration, S.D.M. and P.K.M.; funding acquisition, P.K.M., D.J.D., M.O.B., E.A.W., and J.F.P. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the National Institute For Health Research (NIHR) Research For Patient Benefit Programme, grant number PB-PG-1208-18240. E.A.W. receives funding support from the NIHR Biomedical Research Centre award to Cambridge. MT received a PhD studentship funded by the College Of Life Sciences & Medicine, University Aberdeen, grant number CF10109–38.
Acknowledgments
We thank the stroke database team and stroke research team staff from all participating sites who contributed to data collection. We also would like to acknowledge the contribution of Anglia Stroke Clinical Network Evaluation Study (ASCNES) Group. ASCNES Group (alphabetical order): Max O Bachmann (UEA); Garry R Barton (UEA); Fiona Cummings (ASHCN); Genevieve Dalton (ASHCN); Diana J Day (ASHCN/AH); Abraham George (JPUH); Rachel Hale (UEA); Anthony Kneale Metcalf (NNUH/UEA); Stanley D Musgrave (UEA); Phyo Kyaw Myint (UoA/UEA); Joseph Ngeh (IPH); Anne Nicholson (WSH); Peter Owusu-Agyei (PH); John F Potter (UEA/NNUH) and Gill M Price (UEA).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- World Health Organization. Global Health Estimates 2016: Disease Burden by Cause, Age, Sex, by Country and by Region, 2000–2016; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Royal College of Physicians Sentinel Stroke National Audit Programme (SSNAP). SSNAP Annual Portfolio for April 2018–March 2019 Admissions and Discharges; National Results; SSNAP: London, UK, 2019. [Google Scholar]
- Clery, A.; Bhalla, A.; Bisquera, A.; Skolarus, L.E.; Marshall, I.; McKevitt, C.; Wolfe, C. Long-Term Trends in Stroke Survivors Discharged to Care Homes. Stroke 2020, 51, 179–185. [Google Scholar] [CrossRef]
- Proot, I.M.; Crebolder, H.F.J.M.; Abu-Saad, H.; Macor, T.H.G.M.; Meulen, R.H.J.T. Facilitating and Constraining Factors on Autonomy: The Views of Stroke Patients on Admission Into Nursing Homes. Clin. Nurs. Res. 2000, 9, 460–478. [Google Scholar] [CrossRef] [PubMed]
- Leeds, L.; Meara, J.; Hobson, P. The impact of discharge to a care home on longer term stroke outcomes. Clin. Rehabil. 2004, 18, 924–928. [Google Scholar] [CrossRef] [PubMed]
- Tsugawa, Y.; Kumamaru, H.; Yasunaga, H.; Hashimoto, H.; Horiguchi, H.; Ayanian, J.Z. The association of hospital volume with mortality and costs of care for stroke in Japan. Med. Care 2013, 51, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Myint, P.K.; OBachmann, M.; Loke, Y.K.; DMusgrave, S.; Price, G.M.; Hale, R.; Potter, J.F. Important factors in predicting mortality outcome from stroke: Findings from the Anglia Stroke Clinical Network Evaluation Study. Age Ageing 2017, 46, 83–90. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Paley, L.; Williamson, E.; Bray, B.D.; Hoffman, A.; James, M.A.; Rudd, A.G. Associations Between 30-Day Mortality, Specialist Nursing, and Daily Physician Ward Rounds in a National Stroke Registry. Stroke 2018, 49, 2155–2162. [Google Scholar] [CrossRef] [PubMed]
- Fujino, Y.; Kubo, T.; Muramatsu, K.; Murata, A.; Hayashida, K.; Tomioka, S.; Matsuda, S. Impact of regional clinical pathways on the length of stay in hospital among stroke patients in Japan. Med. Care 2014, 52, 634–640. [Google Scholar] [CrossRef]
- Svendsen, M.L.; Ehlers, L.H.; Ingeman, A.; Johnsen, S.P. Higher stroke unit volume associated with improved quality of early stroke care and reduced length of stay. Stroke 2012, 43, 3041–3045. [Google Scholar] [CrossRef]
- Myint, P.K.; Potter, J.F.; Price, G.M.; Barton, G.R.; Metcalf, A.K.; Hale, R.; Owusu-Agyei, P. Evaluation of stroke services in Anglia Stroke Clinical Network to examine the variation in acute services and stroke outcomes. BMC Health Serv. Res. 2011, 11. [Google Scholar] [CrossRef]
- Kwok, C.S.; Musgrave, S.D.; Price, G.M.; Dalton, G.; Myint, P.K. Similarity of patient characteristics and outcomes in consecutive data collection on stroke admissions over one month compared to longer periods. BMC Res. Notes 2014, 7, 342. [Google Scholar] [CrossRef]
- Saver, J.L.; Altman, H.A. Relation between neurologic deficit severity and final functional outcome shifts and strengthens during first hours after onset. Stroke 2012, 43, 1537–1541. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, K.C.; Bhattacharya, R.L.; Ghosh, S.; Mahata, M.K.; Das, S.; Mondal, G.P. Predictors of severity and outcome and roles of intravenous thrombolysis and biomarkers in first ischemic stroke. Neuroimmunol. Neuroinflamm. 2018, 5. [Google Scholar] [CrossRef]
- Nedeltchev, K.; der Maur, T.A.; Georgiadis, D.; Arnold, M.; Caso, V.; Mattle, H.; Schroth, G.; Remonda, L.; Sturzenegger, M.; Fischer, U.; et al. Ischaemic stroke in young adults: Predictors of outcome and recurrence. J. Neurol. Neurosurg. Psychiatry 2005, 76, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Tung, Y.; Chang, G. The relationships among regionalization, processes, and outcomes for stroke care: A nationwide population-based study. Medicine 2016, 95, e3327. [Google Scholar] [CrossRef]
- Schisterman, E.F.; Cole, S.R.; Platt, R.W. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 2009, 20, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Staplin, N.; Herrington, W.G.; Judge, P.K.; Reith, C.A.; Haynes, R.; Landray, M.J.; Baigent, C.; Emberson, J. Use of causal diagrams to inform the design and interpretation of observational studies: An example from the Study of Heart and Renal Protection (SHARP). Clin. J. Am. Soc. Nephrol. 2017, 12, 546–552. [Google Scholar] [CrossRef]
- Bryan, M.L.; Jenkins, S.P. Multilevel Modelling of Country Effects: A Cautionary Tale. Eur. Sociol. Rev. 2015, 32, 3–22. [Google Scholar] [CrossRef]
- Bowers, J.; Drake, K.W. EDA for HLM: Visualization when Probabilistic Inference Fails. Political Anal. 2005, 13, 301–326. [Google Scholar] [CrossRef]
- Department for Communities and Local Government. English Indices of Deprivation 2010; Department for Communities and Local Government: London, UK, 2011. Available online: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed on 11 August 2020).
- Ministry of Housing, Communities & Local Government. Official Statistics English Indices of Deprivation 2010: Overall; Ministry of Housing, Communities & Local Government: London, UK, 2011. Available online: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010 (accessed on 11 August 2020).
- Van Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45. [Google Scholar] [CrossRef]
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Development Core Team: Vienna, Austria, 2017. [Google Scholar]
- Rudd, A.G.; Irwin, P.; Rutledge, Z.; Lowe, D.; Wade, D.T.; Pearson, M. Regional variations in stroke care in England, Wales and Northern Ireland: Results from the National Sentinel Audit of Stroke. Royal College of Physicians Intercollegiate Stroke Working Party. Clin. Rehabil. 2001, 15, 562–572. [Google Scholar] [CrossRef]
- Ang, Y.H.; Chan, D.K.Y.; Heng, D.M.K.; Shen, Q. Patient outcomes and length of stay in a stroke unit offering both acute and rehabilitation services. Med. J. Aust. 2003, 178, 333–336. [Google Scholar] [CrossRef] [PubMed]
- Kalra, L. The influence of stroke unit rehabilitation on functional recovery from stroke. Stroke 1994, 25, 821–825. [Google Scholar] [CrossRef] [PubMed]
- West, T.; Churilov, L.; Bernhardt, J. Early physical activity and discharge destination after stroke: A comparison of acute and comprehensive stroke unit care. Rehabil. Res. Pract. 2013. [Google Scholar] [CrossRef]
- Langhorne, P.; Collier, J.M.; Bate, P.J.; Thuy, M.; Bernhardt, J. Very early versus delayed mobilisation after stroke. Cochrane Database Syst. Rev. 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Hill, M.D.; Hachinski, V. Stroke treatment: Time is brain. Lancet 1998, 352. [Google Scholar] [CrossRef]
- Lyman, S. Higher hospital volume and specialisation. BMJ 2010, 340. [Google Scholar] [CrossRef] [PubMed]
- Urbach, D.R.; Baxter, N.N. Does it matter what a hospital is “high volume” for? Specificity of hospital volume-outcome associations for surgical procedures: Analysis of administrative data. BMJ 2004, 328, 737–740. [Google Scholar] [CrossRef]
- Carretta, H.J.; Chukmaitov, A.; Tang, A.; Shin, J. Examination of Hospital Characteristics and Patient Quality Outcomes Using Four Inpatient Quality Indicators and 30-Day All-Cause Mortality. Am. J. Med. Qual. 2013, 28, 46–55. [Google Scholar] [CrossRef]
- Flood, A.B.; Scott, W.R.; Ewy, W. Does Practice Make Perfect? Part II: The Relation between Volume and and Outcomes and Other Hospital Characteristics. Med. Care 1984, 22, 115–125. [Google Scholar] [CrossRef]
- Schlegel, D.J.; Tanne, D.; Demchuk, A.M.; Levine, S.R.; Kasner, S.E. Prediction of hospital disposition after thrombolysis for acute ischemic stroke using the National Institutes of Health Stroke Scale. Arch. Neurol. 2004, 61, 1061–1064. [Google Scholar] [CrossRef]
- Schlegel, D.; Kolb, S.J.; Luciano, J.M.; Tovar, J.M.; Cucchiara, B.L.; Liebeskind, D.S.; Kasner, S.E. Utility of the NIH stroke scale as a predictor of hospital disposition. Stroke 2003, 34, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. Dataset(s): 2011 Census: Key Statistics and Quick Statistics for Local Authorities in the United Kingdom-Part 1. KS201UK Ethnic Group, Local Authorities in the United Kingdom. 2013. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/2011censuskeystatisticsandquickstatisticsforlocalauthoritiesintheunitedkingdompart1 (accessed on 12 October 2018).
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).