Developing an Integrated Caregiver Patient-Portal System
Abstract
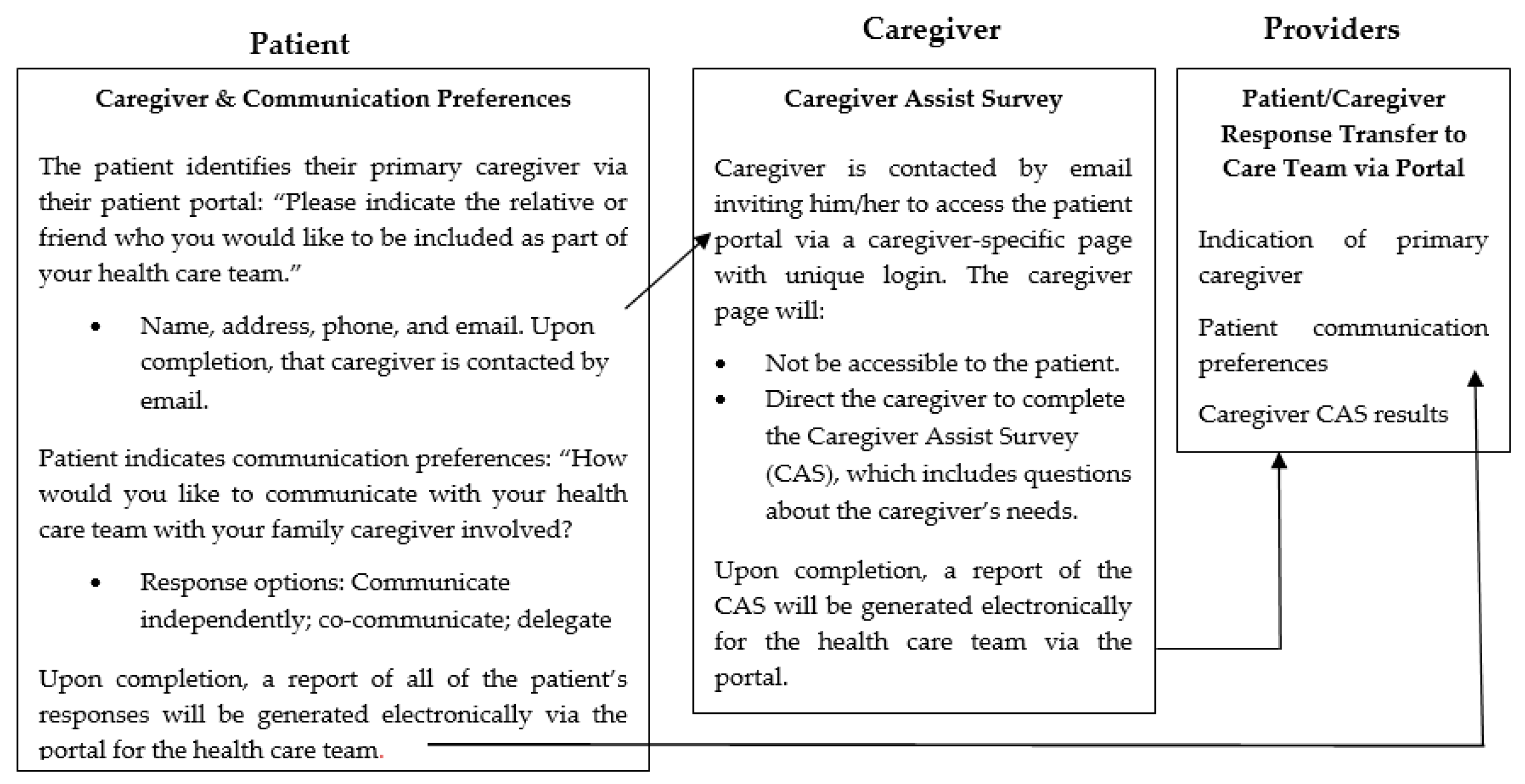
:1. Introduction
2. Materials and Methods
2.1. Phase I: Potential Barriers in the Development and Implementation of an Integrated Caregiver Patient-Portal System
2.2. Phase II: Stakeholders’ Reactions to the System
2.2.1. Sample and Recruitment
2.2.2. Procedures and Measurement
2.2.3. Analysis
3. Results
3.1. Phase I: Potential Barriers in the Development and Implementation of an Integrated Caregiver Patient-Portal System
| Rating | |||
|---|---|---|---|
| Domain and Questions | Simple | Complicated | Complex |
| The Condition or Illness | |||
| What is the nature of the condition? | Well-characterized, well-understood, predictable | Not fully characterized, understood, or predictable | Poorly characterized, poorly understood, unpredictable, or high risk |
| What are the relevant socio-cultural factors and comorbidities? | Unlikely to affect care significantly | Must be factored into care plan and service model | Pose significant challenges to care planning and service provision |
| The Technology | |||
| What are the key features of the technology? | Off-the-shelf or already installed, freestanding, dependable | Not yet developed or fully interoperable; not 100% dependable | Requires close embedding in complex technical systems; significant dependability issues |
| What kind of knowledge does the technology bring into play? | Directly and transparently measures [changes in] the condition. | Partially and indirectly measures [changes in] the condition | Link between data generated and [changes in] the condition is currently unpredictable or contested |
| What knowledge and/or support is required to use the technology? | None or a simple set of instructions | Detailed instruction and training needed, perhaps with ongoing helpdesk support | Effective use of technology requires advanced training and/or support to adjust to new identity or organizational role |
| What is the technology supply model? | Generic, “plug and play”, or COTS solutions requiring minimal customization, easily substitutable if supplier withdraws | COTS solutions requiring significant customization or bespoke solutions; substitution difficult if suppliers withdraw | Solutions requiring significant organizational reconfiguration or medium-to-large scale-bespoke solutions, highly vulnerable to supplier withdraw |
| The Value Proposition | |||
| What is the developer’s business case for the technology (supply-side value)? | Clear business case with strong chance of return on investment. | Business case underdeveloped; potential risk to investors | Business case implausible; significant risk to investors |
| What is its desirability, efficacy, safety, and cost-effectiveness (demand-side value)? | Technology is desirable for patients, effective, safe, and cost-effective. | Technology’s desirability, efficacy, safety, or cost-effectiveness is unknown or contested | |
| The Adopter System | |||
| What changes in staff roles, practices, and identities are implied? | None | Existing staff must learn new skills and/or new staff be appointed. | Threat to professional identity, values, or scope of practice, risk of job loss |
| What is expected of the patient (and/or immediate caregiver)—and is this achievable by, and acceptable to, them? | Nothing | Routine task, e.g., log on, enter data, converse | Complex tasks, e.g., initiate changes in therapy, make judgments, organize |
| What is assumed about the extended network of lay caregivers? | None | Assumes caregiver will be available when needed | Assumes a network of caregivers with the ability to coordinate their input |
| The Wider Context | |||
| What is the political, economic, regulatory, professional, and sociocultural context for program rollout | Financial and regulatory requirements already in place nationally; professional bodies and civil society supportive | Financial and regulatory requirements being negotiated nationally; professional and lay stakeholders not yet committed | Financial and regulatory requirements raise tricky legal or other challenges; professional bodies and lay stakeholders unsupportive or opposed |
| Embedding and Adaptation Over Time | |||
| How much scope is there for adapting and coevolving the technology and the service over time?” | Strong scope for adapting and embedding the technology as local need or context changes | Potential for adapting and coevolving the technology and service is limited or uncertain | Significant barriers to further adaptation and/or coevolution of the technology or service |
3.1.1. The Condition
3.1.2. The Technology
3.1.3. The Value Proposition
3.1.4. The Adopter System
3.1.5. The Organization
3.1.6. The Wider Context
3.1.7. Embedding and Adaptation Over Time
3.2. Phase II: Stakeholders’ Reactions to the System
3.2.1. Sample Characteristics
3.2.2. Concerns and Benefits
| Subtheme | Description | # Of Patients Referencing | Patient Exemplar Quote | # Of Caregivers Referencing | Caregiver Exemplar Quote |
|---|---|---|---|---|---|
| Connects Caregiver | Identifies and connects caregiver with the patient’s care team | 4 | I like the caregivers to be totally involved. | 5 | [I like that] It identifies a caregiver. |
| Gives Voice | Allows caregiver to express needs | 2 | She may have questions of her own that she really doesn’t want to talk to me about, she can you know go [to the system] because it’s stressful on her and she might want to say something | 4 | There may be things that I am thinking that I may not want to put stress on him about then I can ask questions to and receive answers back |
| Learn Caregiver Barriers | Helps the care team recognize barriers, feelings, or needs related to caregiving | 4 | When you fill out the forms they [care team] kind of get to know you and you know one of the questions may be how comfortable are you [providing care] just like you asked [in the demonstration] … or questions like how do you feel doing this. | 2 | You can get the support needed and without guessing or trying to figure out who you need to go to—people [care team] will see it and recommend what you need. |
| Patient Autonomy | Considers or improves patient autonomy | 3 | Well it’s ultimately up to the patient to decide how he really wants or she wants her, their case managed—and how much help they want from the caregiver and you can’t do it without that input. | 0 | (Not referenced by caregivers) |
| Ease of Use of Integrated Portal System | Perception that the integrated portal system is easy to use or beneficial than standard of care | 3 | Seemed pretty straight forward. | 4 | It looked okay to me. I am sure it’s doable for someone who’s used to doing the portal if you can do the patient portal then it should be okay to do this. |
| Portal Use Among Patient | Currently or previously comfortable using the patient portal | 3 | The patient portal is a great feature for those who are capable enough to use it. | 0 | (Not referenced by caregivers) |
| Simplifies Communication | Simplifies communication with care team | 1 | It seems to be easier than trying you know to explain everything over again and like I said I might forget something; she might have a question instead of asking me she can just go [to the system]. | 3 | It gets you involved, you know when the appointments are, what the treatment plans are, you can help interpret everything for her and know for sure what is going on and not just hear it or be told second hand what is going on. |
| Privacy | Protects patient or caregiver privacy within the system | 0 | (Not referenced by patients) | 2 | I think the easy use of the system if he has, he can limit what I need to see or what I’m allowed to use on the system which is good but it’s also good because I think it’s important for the caregiver to have that access with the team. |
| Avoids Assumptions | Avoids making assumptions about who the caregiver is for the patient | 0 | (Not referenced by patients) | 3 | It communicates how much she wants me to be involved. |
| Subtheme | Description | # of Patients Referencing | Patient Exemplar Quote | # of Caregivers Referencing | Caregiver Exemplar Quote |
|---|---|---|---|---|---|
| Adaptability | Suggested additions/changes to system now or in future | 0 | (Not referenced by patient) | 4 | Letting there be more than one person [as caregiver]. |
| Expectations | Expectations for the system not aligning with beta functioning | 1 | Integration with… asking a live (question), not that it’s urgent but get back to me, or whatever… | 3 | Yeah, because then I don’t have to place the phone call I can type it in—hey, I got a question about this, or can somebody contact me—you know I can just put it in the system and it will go through to his care team. |
| Need for User Testing | Need to use the system “hands-on” | 1 | I would have to use it a few times. | 3 | I still think it should be rolled out and then used. |
| Overwhelming | Cancer treatment and diagnosis involves high volume of information | 1 | I think somebody needs to walk them through it… when you get in there you’re in shock. | 1 | I [caregiver has a nursing background] have an edge above the typical lay person who’s coming in here in a whirlwind of emotions and what the heck do we do next… oh my god it’s information overload. |
| Lack of Portal Use | Patient does not use the current portal system or have previous experience | 3 | I never used it. She [caregiver] is very computer literate and she has no problem at all going on there you know. | 0 | (Not referenced by a caregiver) |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- IOM. Retooling for an Aging America: Building the Health Care Workforce; The National Academies Press: Washington, DC, USA, 2008. [Google Scholar]
- Redfoot, D.; Feinberg, L.; Houser, A. The Aging of the Baby Boom and the Growing Care Gap: A Look at Future Declines in the Availability of Family Caregivers; AARP: Washington, DC, USA, 2013. [Google Scholar]
- NAC; AARP. Caregiving in the U.S. 2020 Report; National Alliance for Caregiving and AARP: Washington, DC, USA, 2020. [Google Scholar]
- Kim, Y.; Schulz, R. Family caregivers’ strains: Comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. J. Aging Health 2008, 20, 483–503. [Google Scholar] [CrossRef]
- NAC; AARP. Caregiving in the U.S. 2015 Report; National Alliance for Caregiving and AARP: Washington, DC, USA, 2015. [Google Scholar]
- Kent, E.; Dionne-Odom, J.N. Population-based profile of mental health and support service need among family caregivers of adults with cancer. J. Oncol. Pract. 2019, 15, e122–e131. [Google Scholar] [CrossRef]
- Hopps, M.; Iadeluca, L.; McDonald, M.; Makinson, G.T. The burden of family caregiving in the United States: Work productivity, health care resource utilization, and mental health among employed adults. J. Multidiscip. Healthc. 2017, 10, 437–444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bevans, M.; Sternberg, E.M. Caregiving Burden, Stress, and Health Effects Among Family Caregivers of Adult Cancer Patients. J. Am. Med Assoc. 2012, 307, 398–403. [Google Scholar] [CrossRef]
- Schulz, R.; Beach, S.R. Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. J. Am. Med Assoc. 1999, 282, 2215–2219. [Google Scholar] [CrossRef] [Green Version]
- Hunt, G.H.; Longacre, M.L.; Kent, E.E.; Weber-Raley, L. Cancer Caregiving in the U.S.: An Intense, Episodic, and Challenging Care Experience; National Alliance for Caregiving: Washington, DC, USA, 2016. [Google Scholar]
- Stenberg, U.; Ruland, C.M.; Miaskowski, C. Review of the literature on the effects of caring for a patient with cancer. Pyschooncology 2010, 19, 1013–1025. [Google Scholar] [CrossRef] [PubMed]
- Litzelman, K.; Yabroff, K.R. How are spousal depressed mood, distress, and quality of life associated with risk of depressed mood in cancer survivors? Longitudinal findings from a national sample. Cancer Epidemiol. Biomark. Prev. 2015, 24, 969–977. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milbury, K.; Badr, H.; Fossella, F.; Pisters, K.M.; Carmack, C.L. Longitudinal associations between caregiver burden and patient and spouse distress in couples coping with lung cancer. Supportive Care Cancer 2013, 21, 2371–2379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kent, E.; Rowland, J.H.; Northouse, L.; Litzelman, K.; Chou, W.Y.; Shelburne, N.; Timura, C.; OSMara, A.; Huss, K. Caring for caregivers and patients: Research and clinical priorities for informal cancer caregiving. Cancer 2016, 122, 1987–1995. [Google Scholar] [CrossRef]
- Ryn, M.; Sanders, S.; Kahn, K.; van Houtven, C.H.; Griffin, J.M.; Martin, M.; Atienza, A.; Phelan, S.; Finstad, D.; Rowland, J. Objective burden, resources, and other stressors among informal cancer caregivers: A hidden quality issue? Psychooncology 2011, 20, 44–52. [Google Scholar] [CrossRef]
- Bevan, J.L.; Pecchioni, L.L. Understanding the impact of family caregiver cancer literacy on patient health outcomes. Patient Educ. Couns. 2008, 21, 356–364. [Google Scholar] [CrossRef]
- Longacre, M.L.; Galloway, T.J.; Parvanta, C.F.; Fang, C.Y. Medical Communication-related Informational Need and Resource Preferences Among Family Caregivers for Head and Neck Cancer Patients. J. Cancer Educ. 2015, 30, 786–791. [Google Scholar] [CrossRef] [Green Version]
- Alfano, C.M.; Leach, C.R.; Smith, T.G.; Miller, K.D.; Alcaraz, K.I.; Cannady, R.S.; Wender, R.C.; Brawley, O.W. Equitably Improving Outcomes for Cancer Survivors and Supporting Caregivers: A Blueprint for Care Delivery, Research, Education, and Policy. CA Cancer J. Clin. 2019, 69, 35–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolff, J.L.; Feder, J.; Schulz, R. Supporting family Caregivers of older americans. N. Engl. J. Med. 2016, 375, 2513–2515. [Google Scholar] [CrossRef] [PubMed]
- Coleman, E.A. Family Caregivers as Partners in Care Transitions: The Caregiver Advise Record and Enable Act. J. Hosptial Med. 2016, 11, 883–885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldsmith, J.; Wittenberg, E.; Platt, C.S.; Iannarino, N.T.; Reno, J. Family caregiver communication in oncology: Advancing a typology. Pyschooncology 2016, 25, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.L.; Guan, Y.; Boyd, C.M.; Vick, J.; Amjad, H.; Roth, D.L.; Gitlin, L.N.; Roter, D.L. Examining the context and helpfulness of family companion contributions to older adults’ primary care visits. Patient Educ. Couns. 2017, 100, 487–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Longacre, M.L.; Miller, M.F.; Zaleta, A.K.; Golant, M.; Buzaglo, J. Care and treatment decisions in cancer: The role of the family caregiver. J. Oncol. Navig. Surviv. 2018, 9, 354–362. [Google Scholar]
- Clayman, M.L.; Roter, D.; Wissow, L.S.; Bandeen-Roche, K. Autonomy-related behaviors of patient companions and their effect on decision-making activity in geriatric primary care visits. Soc. Sci. Med. 2005, 60, 1583–1591. [Google Scholar] [CrossRef]
- Wolff, J.L.; Roter, D.L. Older adults’ mental health function and patient-centered care: Does the presence of a family companion help or hinder communication? J. Gen. Intern. Med. 2012, 27, 661–668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wittenberg, E.; Buller, H.; Ferrell, B.; Koczywas, M.; Borneman, T. Understanding Family Caregiver Communication to Provide Family-Centered Cancer Care. Semin. Oncol. Nurs. 2017, 33, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Frampton, S.B.; Guastello, S.; Hoy, L.; Naylor, M.; Sheridan, S.; Johnston-Fleece, M. Harnessing Evidence and Experience to Change Culture: A Guiding Framework for Patient and Family Engaged Care; National Academy of Medicine: New Delhi, India, 2017. [Google Scholar]
- Carman, K.L.; Dardess, P.; Maurer, M.E.; Workman, T.; Ganachari, D.; Pathak-Sen, E.A. Roadmap for Patient and Family Engagement in Healthcare Practice and Research; The American Institutes for Research: Austin, TX, USA, 2014. [Google Scholar]
- Greenhalgh, T. How to improve success of technology projects in health and social care. Public Health Res. Pract. 2018, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenhalgh, T.; Wherton, J.; Papoutsi, C.; Lynch, J.; Hughes, G.; A’Court, C.; Hinder, S.; Fahy, N.; Procter, R.; Shaw, S. Beyond adoption: A new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J. Med. Internet Res. 2017, 19, e367. [Google Scholar] [CrossRef] [Green Version]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Draugalis, J.R.; Coons, S.J.; Plaza, C.M. Best practices for survey research reports: A synopsis for authors and reviewers. Am. J. Pharm. Educ. 2008, 72, 11. [Google Scholar] [CrossRef]
- Bradley, E.H.; Curry, L.A.; Devers, K.J. Qualitative data analysis for health services research: Developing taxonomy, themes, and theory. Health Serv. Res. 2007, 42, 1758–1772. [Google Scholar] [CrossRef] [Green Version]
- Curry, L.A.; Nembhard, I.M.; Bradley, E.H. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation 2009, 119, 1442–1452. [Google Scholar] [CrossRef] [Green Version]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Fang, C.Y.; Longacre, M.L.; Manne, S.L.; Ridge, J.A.; Lango, M.N.; Burtness, B.A. Informational needs of head and neck cancer patients. Health Technol. 2012, 2, 57–62. [Google Scholar] [CrossRef] [Green Version]
- Longacre, M.L.; Ridge, J.A.; Burtness, B.A.; Galloway, T.J.; Fang, C.Y. Psychological functioning of caregivers for head and neck cancer patients. Oral Oncol. 2012, 48, 18–25. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.; Ryoo, J.H.; Campbell, C.; Hollen, P.J.; Williams, I.C. Exploring the challenges of medical/nursing tasks in home care experienced by caregivers of older adults with dementia: An integrative review. J. Clin. Nurs. 2019, 28, 4177–4189. [Google Scholar] [CrossRef]
- Backhouse, T.; Camino, J.; Mioshi, E. What Do We Know About Behavioral Crises in Dementia? A Systematic Review. J. Alzheimer’s Dis. 2018, 62, 99–113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Longacre, M.L.; Ross, E.A.; Fang, C.Y. Caregiving choice and emotional stress among cancer caregivers. West. J. Nurs. Res. 2014, 36, 806–824. [Google Scholar] [CrossRef] [PubMed]
- Schulz, R.; Beach, S.R.; Cook, T.B.; Martire, L.M.; Tomlinson, J.M.; Monin, J.K. Predictors and consequences of perceived lack of choice in becoming an informal caregiver. Aging Ment. Health 2012, 16, 712–721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santoro, M.S.; Van Liew, C.; Holloway, B.; McKinnon, S.; Little, T.; Cronan, T.A. Honor thy parents: An ethnic multigroup analysis of filial responsibility, health perceptions, and caregiving decisions. Res. Aging 2016, 38, 665–688. [Google Scholar] [CrossRef]
- Longacre, M.L.; Applebaum, A.J.; Buzaglo, J.S.; Miller, M.F.; Golant, M.; Rowland, J.H.; Given, B.; Dockham, B.; Northouse, L. Reducing informal caregiver burden in cancer: Evidence-based programs in practice. Transl. Behav. Med. 2018, 8, 145–155. [Google Scholar] [CrossRef] [Green Version]
- Casado, B.L.; van Vulpen, K.S.; Davis, S.L. Unmet Needs for Home and Community-Based Services Among Frail Older Americans and Their Caregivers. J. Aging Health 2011, 23, 529–553. [Google Scholar] [CrossRef]
- Gordon, N.P.; Hornbrook, M.C. Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: A database and survey study of seniors in a large health plan. J. Med. Internet Res. 2016, 18, e50. [Google Scholar] [CrossRef]
- Northouse, L.; Williams, A.L.; Given, B.; McCorkle, R. Psychosocial care for family caregivers of patients with cancer. J. Clin. Oncol. 2012, 30, 1227–1234. [Google Scholar] [CrossRef]
- Vandepitte, S.; Van Den Noortgate, N.; Putman, K.; Verhaeghe, S.; Faes, K.; Annemans, L. Effectiveness of supporting informal caregivers of people with dementia: A systematic review of randomized and non-randomized controlled trials. J. Alzheimer’s Dis. 2016, 52, 929–965. [Google Scholar] [CrossRef] [Green Version]
- Mittelman, M.S.; Ferris, S.H.; Steinberg, G.; Shulman, E.; Mackell, J.A.; Ambinder, A.; Cohen, J. An intervention that delays institutionalization of Alzheimer’s disease patients: Treatment of spouse-caregivers. Gerontologist 1993, 33, 730–740. [Google Scholar] [CrossRef] [PubMed]
- Mittelman, M.S.; Haley, W.E.; Clay, O.J.; Roth, D.L. Improving caregiver well-being delays nursing home placement of patients with Alzheimer disease. Neurology 2006, 67, 1592–1599. [Google Scholar] [CrossRef] [PubMed]
- Woods, S.S.; Forsberg, C.W.; Schwartz, E.C.; Nazi, K.M.; Hibbard, J.H.; Houston, T.K.; Gerrity, M. The Association of Patient Factors, Digital Access, and Online Behavior on Sustained Patient Portal Use: A Prospective Cohort of Enrolled Users. J. Med Internet Res. 2017, 19, e345. [Google Scholar] [CrossRef]
- Irizarry, T.; DeVito Dabbs, A.; Curran, C.R. Patient portals and patient engagement: A state of the science review. J. Med Internet Res. 2015, 17, e148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- IOM. Crossing the Quality Chasm: A New Health System for the 21st Century; The National Academies Press: Washington, DC, USA, 2001. [Google Scholar]
- Gillick, M.R. The critical role of caregivers in achieving patient-centered care. J. Am. Med. Assoc. 2013, 10, 575–576. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longacre, M.L.; Keleher, C.; Chwistek, M.; Odelberg, M.; Siemon, M.; Collins, M.; Fang, C.Y. Developing an Integrated Caregiver Patient-Portal System. Healthcare 2021, 9, 193. https://doi.org/10.3390/healthcare9020193
Longacre ML, Keleher C, Chwistek M, Odelberg M, Siemon M, Collins M, Fang CY. Developing an Integrated Caregiver Patient-Portal System. Healthcare. 2021; 9(2):193. https://doi.org/10.3390/healthcare9020193
Chicago/Turabian StyleLongacre, Margaret L., Cynthia Keleher, Marcin Chwistek, Michelle Odelberg, Mark Siemon, Molly Collins, and Carolyn Y. Fang. 2021. "Developing an Integrated Caregiver Patient-Portal System" Healthcare 9, no. 2: 193. https://doi.org/10.3390/healthcare9020193
APA StyleLongacre, M. L., Keleher, C., Chwistek, M., Odelberg, M., Siemon, M., Collins, M., & Fang, C. Y. (2021). Developing an Integrated Caregiver Patient-Portal System. Healthcare, 9(2), 193. https://doi.org/10.3390/healthcare9020193





