Spinal Orthoses Prescription for Vertebral Fragility Fractures by Italian Physical and Rehabilitation Medicine Physicians: The SPIN-VER Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Survey
2.3. Statistical Analysis
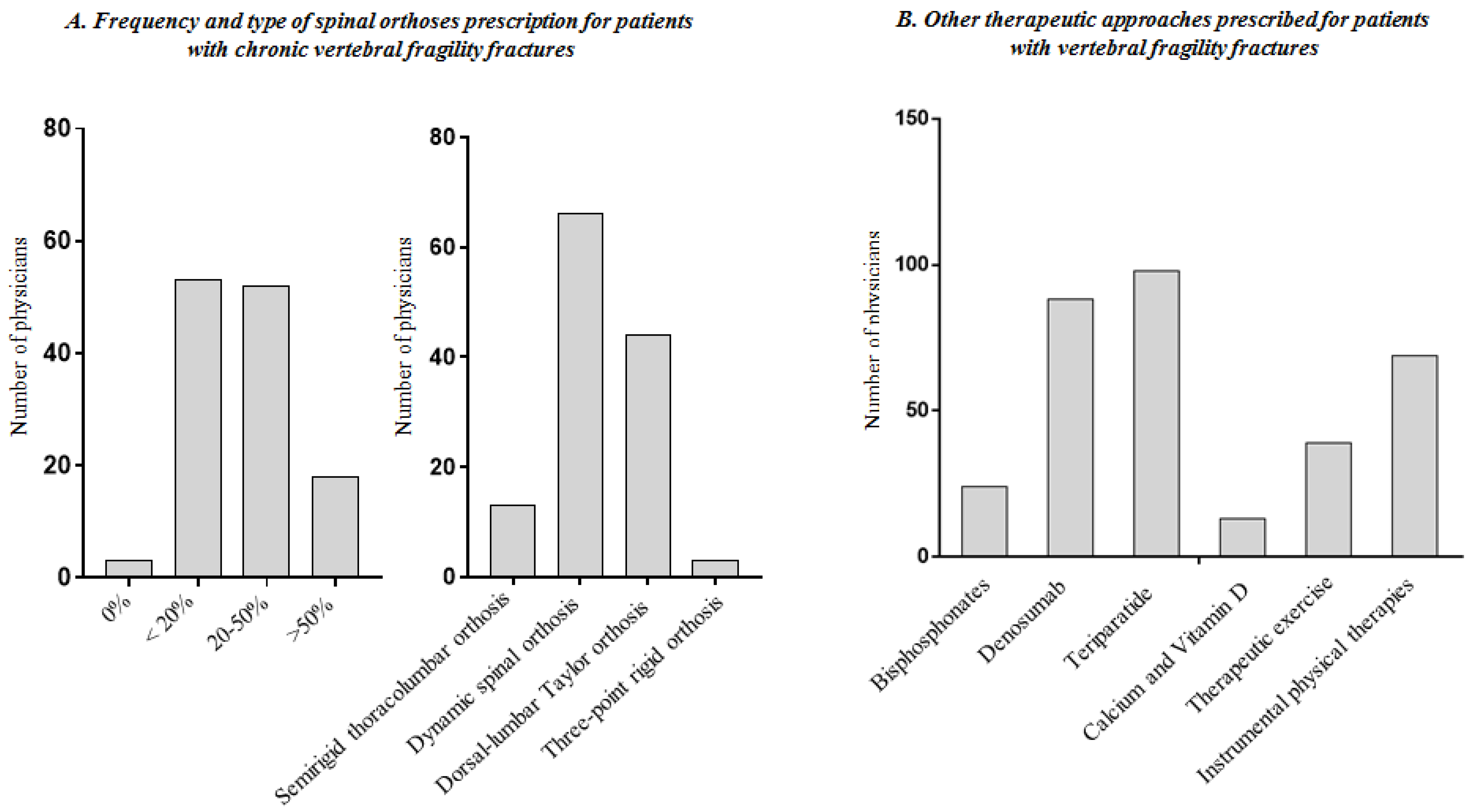
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jin, K.; Simpkins, J.W.; Ji, X.; Leis, M.; Stambler, I. The Critical Need to Promote Research of Aging and Aging-related Diseases to Improve Health and Longevity of the Elderly Population. Aging Dis. 2014, 6, 1–5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirk, B.; Zanker, J.; Duque, G. Osteosarcopenia: Epidemiology, diagnosis, and treatment-facts and numbers. J. Cachexia Sarcopenia Muscle 2020, 11, 609–618. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Sire, A.; Baricich, A.; Renò, F.; Cisari, C.; Fusco, N.; Invernizzi, M. Myostatin as a potential biomarker to monitor sarcopenia in hip fracture patients undergoing a multidisciplinary rehabilitation and nutritional treatment: A preliminary study. Aging Clin. Exp. Res. 2020, 32, 959–962. [Google Scholar] [CrossRef]
- de Sire, A.; Ferrillo, M.; Gennari, A.; Cisari, C.; Pasqua, S.; Foglio Bonda, P.L.; Invernizzi, M.; Migliario, M. Bone health, vitamin D status and oral hygiene screening in breast cancer women before starting osteoporosis treatment: A cross-sectional study. J. Biol. Regul. Homeost. Agents 2021, 35, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Aspray, T.J.; Hill, T.R. Osteoporosis and the Ageing Skeleton. Subcell. Biochem. 2019, 91, 453–476. [Google Scholar] [CrossRef]
- de Sire, A.; Baricich, A.; Minetto, M.A.; Cisari, C.; Invernizzi, M. Low back pain related to a sacral insufficiency fracture: Role of paravertebral oxygen-ozone therapy in a paradigmatic case of nociplastic pain. Funct. Neurol. 2019, 34, 119–122. [Google Scholar]
- Biver, E.; Pepe, J.; de Sire, A.; Chevalley, T.; Ferrari, S. Associations between radius low-frequency axial ultrasound velocity and bone fragility in elderly men and women. Osteoporos. Int. 2019, 30, 411–421. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence (NICE). Clinical Guideline 146. In Osteoporosis: Assessing the Risk of Fragility Fracture; National Institute for Health and Care Excellence: London, UK, 2012. [Google Scholar]
- Kelly, M.A.; McCabe, E.; Bergin, D.; Kearns, S.R.; McCabe, J.P.; Armstrong, C.; Heaney, F.; Carey, J.J. Osteoporotic Vertebral Fractures are Common in Hip Fracture Patients and are Under-recognized. J. Clin. Densitom. 2021, 24, 183–189. [Google Scholar] [CrossRef]
- Ballane, G.; Cauley, J.A.; Luckey, M.M.; Fuleihan, G.E.H. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos. Int. 2017, 28, 1531–1542. [Google Scholar] [CrossRef]
- Lunt, M.; O’Neill, T.W.; Felsenberg, D.; Reeve, J.; Kanis, J.A.; Cooper, C.; Silman, A.J. Characteristics of a prevalent vertebral deformity predict subsequent vertebral fracture: Results from the European prospective osteoporosis study (EPOS). Bone 2003, 33, 505–513. [Google Scholar] [CrossRef]
- Balasubramanian, A.; Zhang, J.; Chen, L.; Wenkert, D.; Daigle, S.G.; Grauer, A.; Curtis, J.R. Risk of subsequent fracture after prior fracture among older women. Osteoporos. Int. 2019, 30, 79–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gimigliano, F.; de Sire, A.; Gastaldo, M.; Maghini, I.; Paoletta, M.; Pasquini, A.; Boldrini, P.; Selb, M.; Prodinger, B.; SIMFER Residents Section Group. Use of the International Classification of Functioning, Disability and Health Generic-30 Set for the characterization of outpatients: Italian Society of Physical and Rehabilitative Medicine Residents Section Project. Eur. J. Phys. Rehabil. Med. 2019, 55, 258–264. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A. Are Individual Recovery Expectations Associated with Future Work Participation and Functional Recovery in Adults with Non-specific Low Back Pain? A Cochrane Review Summary with Commentary. PM R 2021, 13, 105–107. [Google Scholar] [CrossRef] [PubMed]
- Pietri, M.; Lucarini, S. The orthopaedic treatment of fragility fractures. Clin. Cases Miner. Bone Metab. 2007, 4, 108–116. [Google Scholar] [PubMed]
- Shi, L.; Min, N.; Wang, F.; Xue, Q.Y. Bisphosphonates for Secondary Prevention of Osteoporotic Fractures: A Bayesian Network Meta-Analysis of Randomized Controlled Trials. BioMed Res. Int. 2019, 2019, 2594149. [Google Scholar] [CrossRef] [Green Version]
- Moretti, A.; de Sire, A.; Curci, C.; Toro, G.; Gimigliano, F.; Iolascon, G. Effectiveness of denosumab on back pain-related disability and quality-of-life in patients with vertebral fragility fractures. Curr. Med. Res. Opin. 2019, 35, 151–155. [Google Scholar] [CrossRef]
- de Waure, C.; Specchia, M.L.; Cadeddu, C.; Capizzi, S.; Capri, S.; Di Pietro, M.L.; Veneziano, M.A.; Gualano, M.R.; Kheiraoui, F.; La Torre, G.; et al. The prevention of postmenopausal osteoporotic fractures: Results of the Health Technology Assessment of a new antiosteoporotic drug. BioMed Res. Int. 2014, 2014, 975927. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Migliaccio, S.; Francomano, D.; Romagnoli, E.; Marocco, C.; Fornari, R.; Resmini, G.; Buffa, A.; Di Pietro, G.; Corvaglia, S.; Gimigliano, F.; et al. Persistence with denosumab therapy in women affected by osteoporosis with fragility fractures: A multicenter observational real practice study in Italy. J. Endocrinol. Investig. 2017, 40, 1321–1326. [Google Scholar] [CrossRef] [PubMed]
- Perracini, M.R.; Kristensen, M.T.; Cunningham, C.; Sherrington, C. Physiotherapy following fragility fractures. Injury 2018, 49, 1413–1417. [Google Scholar] [CrossRef] [PubMed]
- Benedetti, M.G.; Furlini, G.; Zati, A.; Mauro, G.L. The Effectiveness of Physical Exercise on Bone Density in Osteoporotic Patients. BioMed Res. Int. 2018, 2018, 4840531. [Google Scholar] [CrossRef] [PubMed]
- Caitriona, C.; Mark, M.G.; Elaine, H.; Claire, G.; Michelle, F.; Persson, U.M.; Sherrington, C.; Blake, C. Management of hospitalised osteoporotic vertebral fractures. Arch. Osteoporos. 2020, 15, 14. [Google Scholar] [CrossRef] [PubMed]
- Newman, M.; Lowe, C.M.; Barker, K. Spinal Orthoses for Vertebral Osteoporosis and Osteoporotic Vertebral Fracture: A Systematic Review. Arch. Phys. Med. Rehabil. 2016, 97, 1013–1025. [Google Scholar] [CrossRef] [PubMed]
- Alin, C.K.; Uzunel, E.; Kronhed, A.C.G.; Alinaghizadeh, H.; Salminen, H. Effect of treatment on back pain and back extensor strength with a spinal orthosis in older women with osteoporosis: A randomized controlled trial. Arch. Osteoporos. 2019, 14, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pfeifer, M.; Kohlwey, L.; Begerow, B.; Minne, H.W. Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: A randomized trial. Am. J. Phys. Med. Rehabil. 2011, 90, 805–815. [Google Scholar] [CrossRef]
- Briggs, A.M.; van Dieën, J.H.; Wrigley, T.V.; Greig, A.M.; Phillips, B.; Lo, S.K.; Bennell, K. Thoracic kyphosis affects spinal loads and trunk muscle force. Phys. Ther. 2007, 87, 595–607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dionyssiotis, Y.; Trovas, G.; Thoma, S.; Lyritis, G.; Papaioannou, N. Prospective study of spinal orthoses in women. Prosthet. Orthot. Int. 2015, 39, 487–495. [Google Scholar] [CrossRef]
- Valentin, G.H.; Pedersen, L.N.; Maribo, T. Wearing an active spinal orthosis improves back extensor strength in women with osteoporotic vertebral fractures. Prosthet. Orthot. Int. 2014, 38, 232–238. [Google Scholar] [CrossRef]
- Meccariello, L.; Muzii, V.F.; Falzarano, G.; Medici, A.; Carta, S.; Fortina, M.; Ferrata, P. Dynamic corset versus three-point brace in the treatment of osteoporotic compression fractures of the thoracic and lumbar spine: A prospective, comparative study. Aging Clin. Exp. Res. 2017, 29, 443–449. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.H.; Kang, S.M. Effect of belt pressure and breath held on trunk electromyography. Spine 2002, 27, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Granata, K.P.; Marras, W.S.; Davis, K.G. Biomechanical assessment of lifting dynamics, muscle activity and spinal loads while using three different styles of lifting belt. Clin. Biomech. 1997, 12, 107–115. [Google Scholar] [CrossRef]
- Rostami, M.; Noormohammadpour, P.; Sadeghian, A.H.; Mansournia, M.A.; Kordi, R. The effect of lumbar support on the ultrasound measurements of trunk muscles: A single-blinded randomized controlled trial. PM R 2014, 6, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Rzewuska, M.; Ferreira, M.; McLachlan, A.J.; Machado, G.C.; Maher, C.G. The efficacy of conservative treatment of osteoporotic compression fractures on acute pain relief: A systematic review with meta-analysis. Eur. Spine J. 2015, 24, 702–714. [Google Scholar] [CrossRef]
- Li, M.; Law, S.W.; Cheng, J.; Kee, H.M.; Wong, M.S. A comparison study on the efficacy of SpinoMed® and soft lumbar orthosis for osteoporotic vertebral fracture. Prosthet. Orthot. Int. 2015, 39, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Azadinia, F.; Kamyab, M.; Behtash, H.; Maroufi, N.; Larijani, B. The effects of two spinal orthoses on balance in elderly people with thoracic kyphosis. Prosthet. Orthot. Int. 2013, 37, 404–410. [Google Scholar] [CrossRef] [PubMed]
- Viceconti, A.; Geri, T.; De Luca, S.; Maselli, F.; Rossettini, G.; Sulli, A.; Schenone, A.; Testa, M. Neuropathic pain and symptoms of potential small-fiber neuropathy in fibromyalgic patients: A national on-line survey. Jt. Bone Spine 2021, 88, 105153. [Google Scholar] [CrossRef]
- Rossettini, G.; Palese, A.; Geri, T.; Fiorio, M.; Colloca, L.; Testa, M. Physical therapists’ perspectives on using contextual factors in clinical practice: Findings from an Italian national survey. PLoS ONE 2018, 13, e0208159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brindisino, F.; Ristori, D.; Lorusso, M.; Miele, S.; Pellicciari, L.; Rossettini, G.; Bonetti, F.; Heick, J.D.; Testa, M. Subacromial impingement syndrome: A survey of Italian physiotherapists and orthopaedics on diagnostic strategies and management modalities. Arch. Physiother. 2020, 10, 16. [Google Scholar] [CrossRef]
- Maselli, F.; Rossettini, G.; Storari, L.; Barbari, V.; Viceconti, A.; Geri, T.; Testa, M. Knowledge and management of low back pain as running-related injuries among Italian physical therapists: Findings from a national survey. Physician Sportsmed. 2020, 1–11. [Google Scholar] [CrossRef]
- Jacobs, E.; Senden, R.; McCrum, C.; van Rhijn, L.W.; Meijer, K.; Willems, P.C. Effect of a semirigid thoracolumbar orthosis on gait and sagittal alignment in patients with an osteoporotic vertebral compression fracture. Clin. Interv. Aging 2019, 14, 671–680. [Google Scholar] [CrossRef] [Green Version]
- Jin, Y.Z.; Lee, J.H. Effect of Brace to Osteoporotic Vertebral Fracture: A Meta-Analysis. J. Korean Med. Sci. 2016, 31, 1641–1649. [Google Scholar] [CrossRef] [Green Version]
- Sahota, O.; Ong, T.; Salem, K. Vertebral Fragility Fractures (VFF)-Who, when and how to operate. Injury 2018, 49, 1430–1435. [Google Scholar] [CrossRef] [PubMed]
- Shamji, M.F.; Roffey, D.M.; Young, D.K.; Reindl, R.; Wai, E.K. A pilot evaluation of the role of bracing in stable thoracolumbar burst fractures without neurologic deficit. J. Spinal Disord. Tech. 2014, 27, 370–375. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.S.; Urquhart, J.C.; Dvorak, M.F.; Nadeau, M.; Boyd, M.C.; Thomas, K.C.; Kwon, B.K.; Gurr, K.R.; Bailey, S.I.; Fisher, C.G. Orthosis versus no orthosis for the treatment of thoracolumbar burst fractures without neurologic injury: A multicenter prospective randomized equivalence trial. Spine J. 2013, 14, 2557–2564. [Google Scholar] [CrossRef]
- Kim, H.J.; Yi, J.M.; Cho, H.G.; Chang, B.S.; Lee, C.K.; Kim, J.H.; Yeom, J.S. Comparative study of the treatment outcomes of osteoporotic compression fractures without neurologic injury using a rigid brace, a soft brace, and no brace: A prospective randomized controlled non-inferiority trial. J. Bone Jt. Surg Am. 2014, 96, 1959–1966. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patwardhan, A.G.; Li, S.P.; Gavin, T.; Lorenz, M.; Meade, K.P.; Zindrick, M. Orthotic stabilization of thoracolumbar injuries: A biomechanical analysis of the Jewett hyperextension orthosis. Spine 1990, 15, 654–661. [Google Scholar] [CrossRef] [PubMed]
- Alexandru, D.; So, W. Evaluation and management of vertebral compression fractures. Perm. J. 2012, 16, 46–51. [Google Scholar] [CrossRef] [Green Version]
- Kim, D.H.; Vaccaro, A.R. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J. 2006, 6, 479–487. [Google Scholar] [CrossRef]
- Agostini, F.; Bernetti, A.; Di Giacomo, G.; Viva, M.G.; Paoloni, M.; Mangone, M.; Santilli, V.; Masiero, S. Rehabilitative Good Practices in the Treatment of Sarcopenia: A Narrative Review. Am. J. Phys. Med. Rehabil. 2021, 100, 280–287. [Google Scholar] [CrossRef]
- Harvey, N.C.; Biver, E.; Kaufman, J.M.; Bauer, J.; Branco, J.; Brandi, M.L.; Bruyere, O.; Coxam, V.; Cruz-Jentoft, A.J.; Czerwinski, E.; et al. The role of calcium supplementation in healthy musculoskeletal ageing: An expert consensus meeting of the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) and the International Foundation for Osteoporosis (IOF). Osteoporos. Int. 2017, 28, 447–462. [Google Scholar] [CrossRef] [Green Version]
- Martone, A.M.; Marzetti, E.; Calvani, R.; Picca, A.; Tosato, M.; Santoro, L.; Di Giorgio, A.; Nesci, A.; Sisto, A.; Santoliquido, A.; et al. Exercise and Protein Intake: A Synergistic Approach against Sarcopenia. Biomed. Res. Int. 2017, 2017, 2672435. [Google Scholar] [CrossRef] [PubMed]
- Invernizzi, M.; de Sire, A.; D’Andrea, F.; Carrera, D.; Renò, F.; Migliaccio, S.; Iolascon, G.; Cisari, C. Effects of essential amino acid supplementation and rehabilitation on functioning in hip fracture patients: A pilot randomized controlled trial. Aging Clin. Exp. Res. 2019, 31, 1517–1524. [Google Scholar] [CrossRef]
- Giangregorio, L.M.; Macintyre, N.J.; Thabane, L.; Skidmore, C.J.; Papaioannou, A. Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst. Rev. 2013, 1, CD008618. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.D.; Kim, E.H.; Lee, J.C.; Choi, S.W.; Kim, K.; Shin, B.J. Current Concepts in the Management of Osteoporotic Vertebral Fractures: A Narrative Review. Asian Spine J. 2020, 14, 898–909. [Google Scholar] [CrossRef] [PubMed]
- Bernetti, A.; Agostini, F.; Cacchio, A.; Santilli, V.; Ruiu, P.; Paolucci, T.; Paoloni, M.; Mangone, M. Postural Evaluation in Sports and Sedentary Subjects by Rasterstereographic Back Shape Analysis. Appl. Sci. 2020, 10, 8838. [Google Scholar] [CrossRef]
- Stanghelle, B.; Bentzen, H.; Giangregorio, L.; Pripp, A.H.; Skelton, D.A.; Bergland, A. Physical fitness in older women with osteoporosis and vertebral fracture after a resistance and balance exercise programme: 3-month post-intervention follow-up of a randomised controlled trial. BMC Musculoskelet. Disord. 2020, 21, 471. [Google Scholar] [CrossRef]
- Hoke, M.; Omar, N.B.; Amburgy, J.W.; Self, D.M.; Schnell, A.; Morgan, S.; Larios, E.A.; Chambers, M.R. Impact of exercise on bone mineral density, fall prevention, and vertebral fragility fractures in postmenopausal osteoporotic women. J. Clin. Neurosci. 2020, 76, 261–263. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, J.C.; MacIntyre, N.J.; Ponzano, M.; Templeton, J.A.; Thabane, L.; Papaioannou, A.; Giangregorio, L.M. Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst. Rev. 2019, 7, CD008618. [Google Scholar] [CrossRef] [PubMed]
- Evidence Service to Support the COVID-19 Response. Available online: http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/ (accessed on 1 January 2021).

| Domain A |
| 1. How many patients do you visit in your outpatient monthly? |
| 2. What percentage of patients with osteoporosis do you visit in your outpatient? |
| 3. What percentage of patients with back pain do you visit in your outpatient? |
| 4. What percentage of patients with acute vertebral fragility fractures do you visit in your outpatient? |
| 5. What percentage of patients with chronic vertebral fragility fractures do you visit in your outpatient? |
| Domain B |
| 6. What percentage of patients with back pain without vertebral fragility fractures do you prescribe with spinal orthoses? |
| 7. Which is the spinal orthosis most prescribed by you in the above-mentioned patients? |
| Domain C |
| 8. What percentage of patients with acute vertebral fragility fractures do you prescribe with spinal orthoses? |
| 9. Which is the spinal orthosis most prescribed by you in the above-mentioned patients? |
| 10. What is the timing of spinal orthosis dismission that you suggest in the above-mentioned patients? |
| Domain D |
| 11. What percentage of patients with chronic vertebral fragility fractures do you prescribe with spinal orthoses? |
| 12. What is the spinal orthosis most prescribed in these patients? |
| Domain E |
| 13. Which treatment do you mostly prescribe in patients with vertebral fragility fractures? |
| PRM Physicians (n = 126) | |
|---|---|
| Number of outpatients assessed per month | |
| <50 | 32 (25.4) |
| 50–100 | 35 (27.8) |
| 100–200 | 41 (32.5) |
| >200 | 18 (14.3) |
| Patients with diagnosis of osteoporosis | |
| 0% | 1 (0.8) |
| <20% | 41 (32.5) |
| 20–50% | 71 (56.3) |
| >50% | 13 (10.3) |
| Patients with back pain without VFFs | |
| 0% | 0 (0.0) |
| <20% | 23 (18.3) |
| 20–50% | 64 (50.8) |
| >50% | 39 (30.9) |
| Patients with acute VFFs | |
| 0% | 8 (6.3) |
| <20% | 105 (83.3) |
| 20–50% | 12 (9.5) |
| >50% | 1 (0.8) |
| Patients with chronic VFFs | |
| 0% | 0 (0.0) |
| <20% | 49 (38.9) |
| 20–50% | 61 (48.4) |
| >50% | 16 (12.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Sire, A.; Ammendolia, A.; Gimigliano, A.; Tiberi, R.; Cisari, C.; Invernizzi, M. Spinal Orthoses Prescription for Vertebral Fragility Fractures by Italian Physical and Rehabilitation Medicine Physicians: The SPIN-VER Survey. Healthcare 2021, 9, 892. https://doi.org/10.3390/healthcare9070892
de Sire A, Ammendolia A, Gimigliano A, Tiberi R, Cisari C, Invernizzi M. Spinal Orthoses Prescription for Vertebral Fragility Fractures by Italian Physical and Rehabilitation Medicine Physicians: The SPIN-VER Survey. Healthcare. 2021; 9(7):892. https://doi.org/10.3390/healthcare9070892
Chicago/Turabian Stylede Sire, Alessandro, Antonio Ammendolia, Alessandra Gimigliano, Roberto Tiberi, Carlo Cisari, and Marco Invernizzi. 2021. "Spinal Orthoses Prescription for Vertebral Fragility Fractures by Italian Physical and Rehabilitation Medicine Physicians: The SPIN-VER Survey" Healthcare 9, no. 7: 892. https://doi.org/10.3390/healthcare9070892
APA Stylede Sire, A., Ammendolia, A., Gimigliano, A., Tiberi, R., Cisari, C., & Invernizzi, M. (2021). Spinal Orthoses Prescription for Vertebral Fragility Fractures by Italian Physical and Rehabilitation Medicine Physicians: The SPIN-VER Survey. Healthcare, 9(7), 892. https://doi.org/10.3390/healthcare9070892









