Association of Primary Hypertension and Risk of Cerebrovascular Diseases with Overweight and Physical Activity in Korean Women: A Longitudinal Study
Abstract
1. Introduction
2. Methods
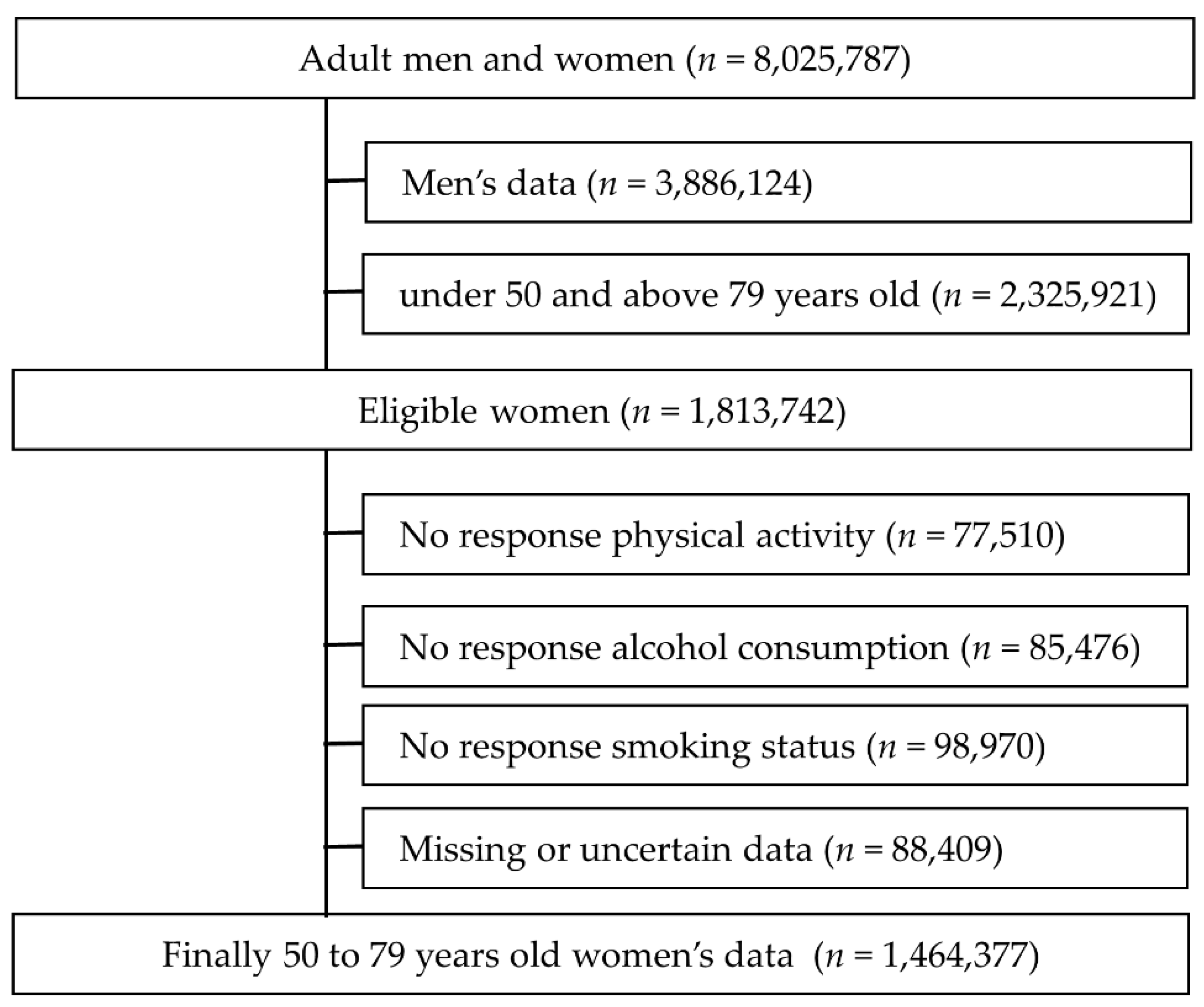
2.1. Participants and Data Sources
2.2. Diagnosis and Follow-Up
2.3. Health Screening
2.4. BMI: Normal, Overweight and Obese
2.5. Physical Activity, Smoking Status, and Alcohol Consumption Risk, Family Monthly Income
2.6. Data Analysis
3. Results
3.1. General Characteristics of Participants
3.2. Incidence of Cerebrovascular Diseases and Adjusted Relative Risk According to BMI and Physical Activity Classifications
3.3. Incidence of Primary Hypertension and Adjusted Relative Risk According to BMI and Physical Activity Classifications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Magalhães, J.E.; Sampaio Rocha-Filho, P.A. Migraine and cerebrovascular diseases: Epidemiology, pathophysiological, and clinical considerations. Headache J. Head Face Pain 2018, 58, 1277–1286. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R. Heart disease and stroke statistics—2019 update: A report from the American Heart Association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef] [PubMed]
- Hermida, R.C.; Ayala, D.E.; Fernandez, J.R.; Mojon, A.; Smolensky, M.H. Hypertension: New perspective on its definition and clinical management by bedtime therapy substantially reduces cardiovascular disease risk. Eur. J. Clin. Investig. 2018, 48, e12909. [Google Scholar] [CrossRef]
- Johnson, W.; Onuma, O.; Owolabi, M.; Sachdev, S. Bull World Health Organ. Bull. World Health Organ. 2016, 94, 634. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kang, K.; Kang, J.; Koo, J.; Kim, D.-H.; Kim, B.J.; Kim, W.-J.; Kim, E.-G.; Kim, J.G.; Kim, J.-M. Executive summary of stroke statistics in Korea 2018: A report from the epidemiology research council of the Korean Stroke Society. J. Stroke 2019, 21, 42. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Tong, X.; Schieb, L.; Vaughan, A.; Gillespie, C.; Wiltz, J.L.; King, S.C.; Odom, E.; Merritt, R.; Hong, Y. Vital signs: Recent trends in stroke death rates—United States, 2000–2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 933. [Google Scholar] [CrossRef] [PubMed]
- İçağasıoğlu, A.; Baklacıoğlu, H.Ş.; Mesci, E.; Yumuşakhuylu, Y.; Murat, S.; Mesci, N. Economic burden of stroke. Turk. J. Phys. Med. Rehabil. 2017, 63, 155. [Google Scholar] [CrossRef]
- Boehme, A.K.; Esenwa, C.; Elkind, M.S. Stroke risk factors, genetics, and prevention. Circ. Res. 2017, 120, 472–495. [Google Scholar] [CrossRef]
- Wang, J.; Wen, X.; Li, W.; Li, X.; Wang, Y.; Lu, W. Risk factors for stroke in the Chinese population: A systematic review and meta-analysis. J. Stroke Cerebrovasc. Dis. 2017, 26, 509–517. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P. Physical Activity Guidelines for Americans From the US Department of Health and Human Services. Circ. Cardiovasc. Qual. Outcomes 2018, 11, e005263. [Google Scholar] [CrossRef]
- Falkstedt, D.; Wolff, V.; Allebeck, P.; Hemmingsson, T.; Danielsson, A.-K. Cannabis, tobacco, alcohol use, and the risk of early stroke: A population-based cohort study of 45,000 Swedish men. Stroke 2017, 48, 265–270. [Google Scholar] [CrossRef]
- Bots, S.H.; Peters, S.A.; Woodward, M. Sex differences in coronary heart disease and stroke mortality: A global assessment of the effect of ageing between 1980 and 2010. BMJ Glob. Health 2017, 2, e000298. [Google Scholar] [CrossRef]
- Hong, K.-S.; Bang, O.Y.; Kang, D.-W.; Yu, K.-H.; Bae, H.-J.; Lee, J.S.; Heo, J.H.; Kwon, S.U.; Oh, C.W.; Lee, B.-C. Stroke statistics in Korea: Part I. Epidemiology and risk factors: A report from the korean stroke society and clinical research center for stroke. J. Stroke 2013, 15, 2. [Google Scholar] [CrossRef]
- Kang, Y.W.; Ko, Y.S.; Kim, K.Y.; Sung, C.; Lee, D.H.; Jeong, E. Trends in health-related behaviors of Korean adults: Study based on data from the 2008-2014 Community Health Surveys. Epidemiol. Health 2015, 37, e2015042. [Google Scholar] [CrossRef] [PubMed]
- Seo, M.H.; Kim, Y.-H.; Han, K.; Jung, J.-H.; Park, Y.-G.; Lee, S.-S.; Kwon, H.-S.; Lee, W.-Y.; Yoo, S.J. Prevalence of obesity and incidence of obesity-related comorbidities in Koreans based on National Health Insurance Service health checkup data 2006–2015. J. Obes. Metab. Syndr. 2018, 27, 46. [Google Scholar] [CrossRef]
- KCDC. 2016 Health Behavior and Chronic Diseases Statitics; Seventh Korea National Health and Nutrition Examination Survey (KNHANES VII-1); Korean Centers for Disease Control and Prevention Osong: Osong-eup, Korea, 2017. [Google Scholar]
- Nguyen, N.T.; Magno, C.P.; Lane, K.T.; Hinojosa, M.W.; Lane, J.S. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: Findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J. Am. Coll. Surg. 2008, 207, 928–934. [Google Scholar] [CrossRef] [PubMed]
- Services USDoHaH. Physical Activity and Health: A Report of the Surgeon General; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion: Atlanta, GA, USA, 1996.
- Azevedo, M.R.; Araújo, C.L.P.; Reichert, F.F.; Siqueira, F.V.; da Silva, M.C.; Hallal, P.C. Gender differences in leisure-time physical activity. Int. J. Public Health 2007, 52, 8. [Google Scholar] [CrossRef]
- Harelick, L.; Viola, D.; Tahara, D. Preconception health of low socioeconomic status women: Assessing knowledge and behaviors. Women’s Health Issues 2011, 21, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.h.; Kwon, S.o.; Kim, D.w.; Kim, Y.h.; Kim, C.i.; Lyu, H.r.; Lee, L.d.; Lee, J.w.; Seo, S.y.; Cho, K.h.; et al. Development of High-Obesity Reality Analysis and Management Measures; KNHI Service, Ed.; Korean National Health Insurance Service: Seoul, Korea, 2015. [Google Scholar]
- Statistics Korea. Korean Standard Classification of Diseases; Statistics Korea: Daejeon, Korea, 2010. [Google Scholar]
- Lenfant, C.; Chobanian, A.V.; Jones, D.W.; Roccella, E.J. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) resetting the hypertension sails. Circulation 2003, 107, 2993–2994. [Google Scholar] [CrossRef][Green Version]
- Donahue, M.J.; Achten, E.; Cogswell, P.M.; De Leeuw, F.-E.; Derdeyn, C.P.; Dijkhuizen, R.M.; Fan, A.P.; Ghaznawi, R.; Heit, J.J.; Ikram, M.A. Consensus statement on current and emerging methods for the diagnosis and evaluation of cerebrovascular disease. J. Cereb. Blood Flow Metab. 2018, 38, 1391–1417. [Google Scholar] [CrossRef] [PubMed]
- Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: Executive Summary. Expert panel on the identification, evaluation, and treatment of overweight in adults. Am. J. Clin. Nutr. 1998, 68, 899–917. [CrossRef] [PubMed]
- Paffenbarger, R.; Wing, A.; Hyde, R. Paffenbarger physical activity questionnaire. Am. J. Epidemiol. 1978, 108, 161–175. [Google Scholar] [CrossRef]
- Washburn, R.A.; Goldfield, S.R.; Smith, K.W.; McKinlay, J.B. The validity of self-reported exercise-induced sweating as a measure of physical activity. Am. J. Epidemiol. 1990, 132, 107–113. [Google Scholar] [CrossRef] [PubMed]
- ACSM. American College Sports Medicine, ACSM’s Guidelines for Exercise Testing and Prescription, 10th ed.; Lippincott Williams & Wilkins: Philadephia, PA, USA, 2017. [Google Scholar]
- World Health Organization. Tobacco or Health: A Global Status Report; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- World Health Organization. International Guide for Monitoring Alcohol Consumption and Related Harm; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Gillespie, C.D.; Hurvitz, K.A.; Centers for Disease Control and Prevention (CDC). Prevalence of hypertension and controlled hypertension—United States, 2007–2010. MMWR Suppl. 2013, 62, 144–148. [Google Scholar]
- Statistics, K. Causes of Death Statitics in 2017; Statistics Korea: Daejeon, Korea, 2018. [Google Scholar]
- Bushnell, C.D.; Chaturvedi, S.; Gage, K.R.; Herson, P.S.; Hurn, P.D.; Jiménez, M.C.; Kittner, S.J.; Madsen, T.E.; McCullough, L.D.; McDermott, M. Sex differences in stroke: Challenges and opportunities. J. Cereb. Blood Flow Metab. 2018, 38, 2179–2191. [Google Scholar] [CrossRef]
- Barengo, N.C.; Antikainen, R.; Borodulin, K.; Harald, K.; Jousilahti, P. Leisure-time physical activity reduces total and cardiovascular mortality and cardiovascular disease incidence in older adults. J. Am. Geriatr. Soc. 2017, 65, 504–510. [Google Scholar] [CrossRef]
- Ellekjær, H.; Holmen, J.; Ellekjær, E.; Vatten, L. Physical activity and stroke mortality in women: Ten-year follow-up of the Nord-Trøndelag health survey, 1984–1986. Stroke 2000, 31, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Kubota, Y.; Iso, H.; Yamagishi, K.; Sawada, N.; Tsugane, S. Daily total physical activity and incident stroke: The Japan public health Center–Based prospective study. Stroke 2017, 48, 1730–1736. [Google Scholar] [CrossRef]
- Wen, C.P.; Liu, C.H.; Jeng, J.S.; Hsu, S.P.; Chen, C.H.; Lien, L.M.; Chen, A.C.; Lee, J.T.; Chen, P.K.; Hsu, C.S. Pre-stroke physical activity is associated with fewer post-stroke complications, lower mortality and a better long-term outcome. Eur. J. Neurol. 2017, 24, 1525–1531. [Google Scholar] [CrossRef]
- McDonnell, M.N.; Hillier, S.L.; Hooker, S.P.; Le, A.; Judd, S.E.; Howard, V.J. Physical activity frequency and risk of incident stroke in a national US study of blacks and whites. Stroke 2013, 44, 2519–2524. [Google Scholar] [CrossRef] [PubMed]
- Chase, N.L.; Sui, X.; Lee, D.-c.; Blair, S.N. The association of cardiorespiratory fitness and physical activity with incidence of hypertension in men. Am. J. Hypertens. 2009, 22, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhang, D.; Liu, Y.; Sun, X.; Han, C.; Wang, B.; Ren, Y.; Zhou, J.; Zhao, Y.; Shi, Y. Dose–response association between physical activity and incident hypertension: A systematic review and meta-analysis of cohort studies. Hypertension 2017, 69, 813–820. [Google Scholar] [CrossRef] [PubMed]
- Huai, P.; Xun, H.; Reilly, K.H.; Wang, Y.; Ma, W.; Xi, B. Physical activity and risk of hypertension: A meta-analysis of prospective cohort studies. Hypertension 2013, 62, 1021–1026. [Google Scholar] [CrossRef]
- Camões, M.; Oliveira, A.; Pereira, M.; Severo, M.; Lopes, C. Role of physical activity and diet in incidence of hypertension: A population-based study in Portuguese adults. Eur. J. Clin. Nutr. 2010, 64, 1441. [Google Scholar] [CrossRef] [PubMed]
- Diaz, K.M.; Booth III, J.N.; Seals, S.R.; Abdalla, M.; Dubbert, P.M.; Sims, M.; Ladapo, J.A.; Redmond, N.; Muntner, P.; Shimbo, D. Physical activity and incident hypertension in African Americans: The Jackson Heart Study. Hypertension 2017, 69, 421–427. [Google Scholar] [CrossRef]
- Joseph, G.; Marott, J.L.; Torp-Pedersen, C.; Biering-Sørensen, T.; Nielsen, G.; Christensen, A.-E.; Johansen, M.B.; Schnohr, P.; Sogaard, P.; Mogelvang, R. Dose-response association between level of physical activity and mortality in normal, elevated, and high blood pressure. Hypertension 2019, 74, 1307–1315. [Google Scholar] [CrossRef]
- Lu, Y.; Lu, M.; Dai, H.; Yang, P.; Smith-Gagen, J.; Miao, R.; Zhong, H.; Chen, R.; Liu, X.; Huang, Z.; et al. Lifestyle and Risk of Hypertension: Follow-Up of a Young Pre-Hypertensive Cohort. Int. J. Med. Sci. 2015, 12, 605–612. [Google Scholar] [CrossRef][Green Version]
- Zambrana, R.E.; Lopez, L.; Dinwiddie, G.Y.; Ray, R.M.; Phillips, L.S.; Trevisan, M.; Wassertheil-Smoller, S. Prevalence and incident prehypertension and hypertension in postmenopausal Hispanic women: Results from the Women’s Health Initiative. Am. J. Hypertens. 2014, 27, 372–381. [Google Scholar] [CrossRef][Green Version]
- Nakayama, T.; Date, C.; Yokoyama, T.; Yoshiike, N.; Yamaguchi, M.; Tanaka, H. A 15.5-year follow-up study of stroke in a Japanese provincial city: The Shibata Study. Stroke 1997, 28, 45–52. [Google Scholar] [CrossRef]
- Sattelmair, J.R.; Kurth, T.; Buring, J.E.; Lee, I.-M. Physical activity and risk of stroke in women. Stroke 2010, 41, 1243–1250. [Google Scholar] [CrossRef]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo Jr, J.L.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright Jr, J.T. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef]
- Scholes, S.; Mindell, J. Health Survey for England 2016: Physical Activity in Adults; Health and Social Care Information Centre, UK: Richmond, VA, USA, 2013. [Google Scholar]
- Liu, F.; Wang, W.; Ma, J.; Sa, R.; Zhuang, G. Different associations of sufficient and vigorous physical activity with BMI in Northwest China. Sci. Rep. 2018, 8, 13120. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Recommendations on Physical Activity for Health; Geneva World Health Organization: Geneva, Switzerland, 2010; Volume 60. [Google Scholar]
- Lee, J.Y.; Lee, K.; Choi, Y.C. Relative Grip Strength Cut-Off Values and Metabolic Syndrome in the Elderly: The Korea National Health and Nutrition Examination Survey 2014–2017. J. Men’s Health 2019, 15, e47–e57. [Google Scholar]
- Miller, S.L.; Reber, R.J.; Chapman-Novakofski, K. Prevalence of CVD risk factors and impact of a two-year education program for premenopausal women. Women’s Health Issues 2001, 11, 486–493. [Google Scholar] [CrossRef]
- Conway-Phillips, R.; Dagadu, H.; Motley, D.; Shawahin, L.; Janusek, L.W.; Klonowski, S.; Saban, K.L. Qualitative evidence for Resilience, Stress, and Ethnicity (RiSE): A program to address race-based stress among Black women at risk for cardiovascular disease. Complement. Ther. Med. 2020, 48, 102277. [Google Scholar] [CrossRef]
| Normal | Overweight | Obese | p-Value | |
|---|---|---|---|---|
| n, (%) | 837,623 (57.2%) | 575,500 (39.3%) | 51,253 (3.5%) | |
| Age, years | 59.2 ± 7.3 | 66.4 ± 6.5 a | 67.1 ± 7.1 b,c | <0.001 * |
| Height, cm | 157.9 ± 6.3 | 155.3 ± 5.6 a | 154.1 ± 5.1 b | <0.001 * |
| Weight, kg | 55.2 ± 6.2 | 66.1 ± 6.8 a | 79.9 ± 8.3 b,c | <0.001 * |
| BMI, kg/m2 | 22.1 ± 2.4 | 27.4 ± 1.7 a | 33.6 ± 2.3 b,c | <0.001 * |
| SBP, mmHg | 115.3 ± 11.3 | 119.3 ± 11.8 a | 123.4 ± 12.5 b,c | <0.001 * |
| DBP, mmHg | 75.7 ± 6.1 | 77.1 ± 7.9 a | 81.6 ± 8.3 b,c | <0.001 * |
| Total cholesterol, mg/dL | 192.7 ± 41.3 | 217.3 ± 59.6 a | 219.1 ± 60.1 b,c | <0.001 * |
| Fasting glucose, mg/dL | 92.2 ± 23.5 | 99.7 ± 32.7 a | 109.5 ± 37.1 b,c | <0.001 * |
| AST, U/L | 22.9 ± 18.3 | 26.7 ± 21.7 a | 29.3 ± 27.7 b,c | <0.001 * |
| ALT, U/L | 20.1 ± 21.3 | 24.7 ± 22.6 a | 30.4 ± 26.1 b,c | <0.001 * |
| Normal | Overweight | Obese | p-Value | p-Value | |
|---|---|---|---|---|---|
| Physical Activity, (%) | |||||
| Low | 86.2 | 83.4 | 85.6 | normal vs. overweight, p < 0.001 * normal vs. obese, p < 0.001 * overweight vs. obese, p = 0.003 | <0.001 * |
| Medium | 7.3 | 8.0 | 6.5 | ||
| High | 6.5 | 8.6 | 7.9 | ||
| Smoking status, (%) | |||||
| Never | 94.3 | 95.6 | 94.5 | normal vs. overweight, p < 0.001 * normal vs. obese, p < 0.001 * overweight vs. obese, p < 0.001 * | <0.001 * |
| Quit smoking | 2.0 | 1.4 | 1.6 | ||
| Current smoker | 3.7 | 3.0 | 3.9 | ||
| Alcohol consumption risk, (%) | |||||
| None | 90.9 | 91.0 | 91.3 | normal vs. overweight, p < 0.001 * normal vs. obese, p < 0.001 * overweight vs. obese, p = 0.007 | <0.001 * |
| Low risk | 7.4 | 6.6 | 5.9 | ||
| medium risk | 1.1 | 1.6 | 1.9 | ||
| High risk | 0.6 | 0.8 | 0.9 | ||
| Family monthly income, KW | 2,799,315 | 2,710,819 a | 2,594,100 b,c | - | <0.001 * |
| P.A | Incidence (%) | Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|---|---|
| ARR (95% CI) | p | ARR (95% CI) | p | ARR (95% CI) | p | |||
| Normal BMI 18.5–24.9 | Low | 5.7 | 1 | 1 | 1 | |||
| Medium | 5.4 | 0.931 (0.913–0.959) | <0.001 * | 0.896 (0.860–0.933) | <0.001 * | 0.889 (0.854–0.919) | <0.001 * | |
| High | 7.6 | 0.956 (0.922–0.986) | <0.001 * | 0.956 (0.921–0.969) | <0.001 * | 0.913 (0.889–0.953) | <0.001 * | |
| Overweight BMI 25.0–29.9 | Low | 9.4 | 1 | 1 | 1 | |||
| Medium | 8.6 | 0.839 (0.806–0.869) | <0.001 * | 0.959 (0.931–0.985) | <0.001 * | 0.945 (0.925–0.976) | <0.001 * | |
| High | 10.9 | 1.080 (0.894–1.230) | 0.090 | 0.978 (0.964–1.009) | 0.212 | 0.980 (0.964–0.991) | <0.001 * | |
| Obese BMI ≥ 30.0 | Low | 9.3 | 1 | 1 | 1 | |||
| Medium | 7.5 | 1.112 (0.810–1.094) | 0.893 | 1.001 (0.953–1.059) | 0.981 | 0.997 (0.943–1.129) | 0.846 | |
| High | 10.8 | 1.125 (0.911–1.235) | 0.104 | 1.041 (0.995–1.086) | 0.112 | 1.011 (0.976–1.063) | 0.095 | |
| PA | Incidence (%) | Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|---|---|
| ARR (95% CI) | p | ARR (95% CI) | p | ARR (95% CI) | p | |||
| Normal BMI 18.5–24.9 | Low | 17.6 | 1 | 1 | 1 | |||
| Medium | 17.9 | 0.995 (0.964–1.021) | 0.125 | 0.986 (0.961–1.003) | 0.159 | 0.985 (0.963–0.997) | <0.001 * | |
| High | 24.6 | 1.085 (0.992–1.287) | 0.098 | 0.993 (0.972–1.016) | 0.451 | 0.991 (0.967–1.029) | 0.234 | |
| Overweight BMI 25.0–29.9 | Low | 40.1 | 1 | 1 | 1 | |||
| Medium | 36.5 | 0.900 (0.847–0.931) | <0.001 * | 0.946 (0.929–0.977) | <0.001 * | 0.943 (0.928–0.961) | <0.001 * | |
| High | 44.7 | 0.993 (0.942–1.059) | 0.094 | 1.001 (0.988–1.030) | 0.270 | 0.999 (0.988–1.019) | 0.129 | |
| Obese BMI ≥ 30.0 | Low | 48.7 | 1 | 1 | 1 | |||
| Medium | 44.9 | 0.902 (0.821–0.969) | <0.001 * | 0.941 (0.921–0.966) | <0.001 * | 0.933 (0.920–0.955) | <0.001 * | |
| High | 55.8 | 1.053 (0.927–1.199) | 0.198 | 0.985 (0.974–0.995) | 0.002 * | 0.981 (0.971–0.997) | <0.001 * | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, N.; Kim, Y.; Won, Y. Association of Primary Hypertension and Risk of Cerebrovascular Diseases with Overweight and Physical Activity in Korean Women: A Longitudinal Study. Healthcare 2021, 9, 1093. https://doi.org/10.3390/healthcare9091093
Su N, Kim Y, Won Y. Association of Primary Hypertension and Risk of Cerebrovascular Diseases with Overweight and Physical Activity in Korean Women: A Longitudinal Study. Healthcare. 2021; 9(9):1093. https://doi.org/10.3390/healthcare9091093
Chicago/Turabian StyleSu, Nan, Yonghwan Kim, and Youngin Won. 2021. "Association of Primary Hypertension and Risk of Cerebrovascular Diseases with Overweight and Physical Activity in Korean Women: A Longitudinal Study" Healthcare 9, no. 9: 1093. https://doi.org/10.3390/healthcare9091093
APA StyleSu, N., Kim, Y., & Won, Y. (2021). Association of Primary Hypertension and Risk of Cerebrovascular Diseases with Overweight and Physical Activity in Korean Women: A Longitudinal Study. Healthcare, 9(9), 1093. https://doi.org/10.3390/healthcare9091093







