Approaches to Inducing β-Cell Regeneration
Abstract
:1. Introduction
2. β-Cell Replication
3. β-Cell Neogenesis from Ducts
3.1. Partial Pancreatectomy
3.2. Pancreatic Duct Ligation
3.3. Inductive Factors
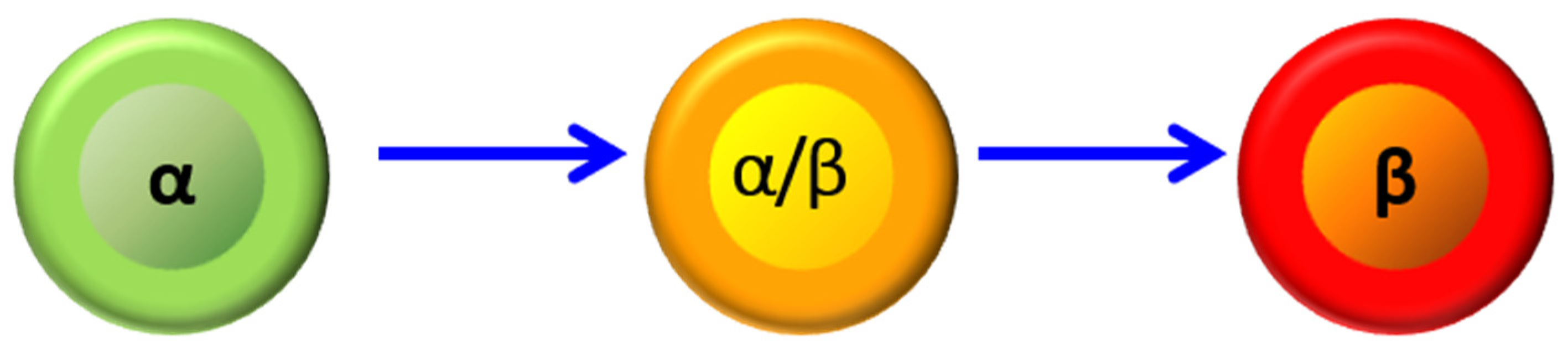
4. Dedifferentiation/Redifferentiation
5. β-Cell Neogenesis by Transdifferentiation from Other Islet Cells
6. Conclusions
Funding
Conflicts of Interest
References
- Chen, C.; Cohrs, C.M.; Stertmann, J.; Bozsak, R.; Speier, S. Human beta cell mass and function in diabetes: Recent advances in knowledge and technologies to understand disease pathogenesis. Mol. Metab. 2017, 6, 943–957. [Google Scholar] [CrossRef] [PubMed]
- Meier, J.; Kohler, C.; Alkhatib, B.; Sergi, C.; Junker, T.; Klein, H.; Schmidt, W.; Fritsch, H. Beta-cell development and turnover during prenatal life in humans. Eur. J. Endocrinol. 2009, 162, 559–568. [Google Scholar] [CrossRef] [Green Version]
- Cnop, M.; Hughes, S.J.; Igoillo-Esteve, M.; Hoppa, M.B.; Sayyed, F.; van de Laar, L.; Gunter, J.H.; de Koning, E.J.; Walls, G.V.; Gray, D.W.; et al. The long lifespan and low turnover of human islet beta cells estimated by mathematical modelling of lipofuscin accumulation. Diabetologia 2010, 53, 321–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.H.; Itkin-Ansari, P.; Levine, F. CENP-A, a protein required for chromosome segregation in mitosis, declines with age in islet but not exocrine cells. Aging 2010, 2, 785–790. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Tata, V. Age-related impairment of pancreatic Beta-cell function: Pathophysiological and cellular mechanisms. Front. Endocrinol. 2014, 5, 138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, K.; Suebsuwong, C.; Wang, P.; Garcia-Ocana, A.; Stewart, A.F.; DeVita, R.J. DYRK1A Inhibitors as Potential Therapeutics for beta-Cell Regeneration for Diabetes. J. Med. Chem. 2021, 64, 2901–2922. [Google Scholar] [CrossRef]
- Lee, S.H.; Hao, E.; Levine, F.; Itkin-Ansari, P. Id3 upregulates BrdU incorporation associated with a DNA damage response, not replication, in human pancreatic beta-cells. Islets 2011, 3, 358–366. [Google Scholar] [CrossRef] [Green Version]
- Taupin, P. BrdU immunohistochemistry for studying adult neurogenesis: Paradigms, pitfalls, limitations, and validation. Brain Res. Rev. 2007, 53, 198–214. [Google Scholar] [CrossRef]
- Sun, X.; Kaufman, P.D. Ki-67: More than a proliferation marker. Chromosoma 2018, 127, 175–186. [Google Scholar] [CrossRef]
- Oliver-Krasinski, J.M.; Stoffers, D.A. On the origin of the beta cell. Genes Dev. 2008, 22, 1998–2021. [Google Scholar] [CrossRef] [Green Version]
- Bonner-Weir, S.; Baxter, L.A.; Schuppin, G.T.; Smith, F.E. A second pathway for regeneration of adult exocrine and endocrine pancreas. A possible recapitulation of embryonic development. Diabetes 1993, 42, 1715–1720. [Google Scholar] [CrossRef]
- Goldman, J.A.; Poss, K.D. Gene regulatory programmes of tissue regeneration. Nat. Rev. 2020, 21, 511–525. [Google Scholar] [CrossRef]
- Chung, C.H.; Hao, E.; Piran, R.; Keinan, E.; Levine, F. Pancreatic beta-cell neogenesis by direct conversion from mature alpha-cells. Stem Cells 2010, 28, 1630–1638. [Google Scholar] [CrossRef]
- Hao, E.; Tyrberg, B.; Itkin-Ansari, P.; Lakey, J.R.; Geron, I.; Monosov, E.Z.; Barcova, M.; Mercola, M.; Levine, F. Beta-cell differentiation from nonendocrine epithelial cells of the adult human pancreas. Nat. Med. 2006, 12, 310–316. [Google Scholar] [CrossRef]
- Dirice, E.; De Jesus, D.F.; Kahraman, S.; Basile, G.; Ng, R.W.; El Ouaamari, A.; Teo, A.K.K.; Bhatt, S.; Hu, J.; Kulkarni, R.N. Human duct cells contribute to beta cell compensation in insulin resistance. JCI Insight 2019, 4, e99576. [Google Scholar] [CrossRef] [Green Version]
- Gu, D.; Sarvetnick, N. Epithelial cell proliferation and islet neogenesis in IFN-g transgenic mice. Development 1993, 18, 33–46. [Google Scholar] [CrossRef]
- Bonner-Weir, S.; Inada, A.; Yatoh, S.; Li, W.C.; Aye, T.; Toschi, E.; Sharma, A. Transdifferentiation of pancreatic ductal cells to endocrine beta-cells. Biochem. Soc. Trans. 2008, 36, 353–356. [Google Scholar] [CrossRef]
- Lee, S.H.; Hao, E.; Levine, F. beta-Cell replication and islet neogenesis following partial pancreatectomy. Islets 2011, 3, 188–195. [Google Scholar] [CrossRef] [Green Version]
- Menge, B.A.; Tannapfel, A.; Belyaev, O.; Drescher, R.; Muller, C.; Uhl, W.; Schmidt, W.E.; Meier, J.J. Partial pancreatectomy in adult humans does not provoke beta-cell regeneration. Diabetes 2008, 57, 142–149. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.S.; De Leon, D.D.; Kaestner, K.H.; Stoffers, D.A. Regeneration of pancreatic islets after partial pancreatectomy in mice does not involve the reactivation of neurogenin-3. Diabetes 2006, 55, 269–272. [Google Scholar] [CrossRef]
- Van de Casteele, M.; Leuckx, G.; Cai, Y.; Yuchi, Y.; Coppens, V.; De Groef, S.; Van Gassen, N.; Baeyens, L.; Heremans, Y.; Wright, C.V.; et al. Partial duct ligation: Beta-cell proliferation and beyond. Diabetes 2014, 63, 2567–2577. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inada, A.; Nienaber, C.; Katsuta, H.; Fujitani, Y.; Levine, J.; Morita, R.; Sharma, A.; Bonner-Weir, S. Carbonic anhydrase II-positive pancreatic cells are progenitors for both endocrine and exocrine pancreas after birth. Proc. Natl. Acad. Sci. USA 2008, 105, 19915–19919. [Google Scholar] [CrossRef] [Green Version]
- Solar, M.; Cardalda, C.; Houbracken, I.; Martin, M.; Maestro, M.A.; De Medts, N.; Xu, X.; Grau, V.; Heimberg, H.; Bouwens, L.; et al. Pancreatic exocrine duct cells give rise to insulin-producing beta cells during embryogenesis but not after birth. Dev. Cell 2009, 17, 849–860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, X.; D’Hoker, J.; Stange, G.; Bonne, S.; De Leu, N.; Xiao, X.; Van de Casteele, M.; Mellitzer, G.; Ling, Z.; Pipeleers, D.; et al. Beta cells can be generated from endogenous progenitors in injured adult mouse pancreas. Cell 2008, 132, 197–207. [Google Scholar] [CrossRef] [Green Version]
- Cavelti-Weder, C.; Shtessel, M.; Reuss, J.E.; Jermendy, A.; Yamada, T.; Caballero, F.; Bonner-Weir, S.; Weir, G.C. Pancreatic duct ligation after almost complete beta-cell loss: Exocrine regeneration but no evidence of beta-cell regeneration. Endocrinology 2013, 154, 4493–4502. [Google Scholar] [CrossRef] [PubMed]
- Rankin, M.M.; Wilbur, C.J.; Rak, K.; Shields, E.J.; Granger, A.; Kushner, J.A. Beta Cells Are Not Generated in Pancreatic Duct Ligation Induced Injury in Adult Mice. Diabetes 2013, 62, 1634–1645. [Google Scholar] [CrossRef] [Green Version]
- Gribben, C.; Lambert, C.; Messal, H.A.; Hubber, E.L.; Rackham, C.; Evans, I.; Heimberg, H.; Jones, P.; Sancho, R.; Behrens, A. Ductal Ngn3-expressing progenitors contribute to adult beta cell neogenesis in the pancreas. Cell Stem. Cell 2021, 28, 2000–2008.e4. [Google Scholar] [CrossRef]
- Cras-Meneur, C.; Elghazi, L.; Czernichow, P.; Scharfmann, R. Epidermal growth factor increases undifferentiated pancreatic embryonic cells in vitro: A balance between proliferation and differentiation. Diabetes 2001, 50, 1571–1579. [Google Scholar] [CrossRef]
- Rooman, I.; Bouwens, L. Combined gastrin and epidermal growth factor treatment induces islet regeneration and restores normoglycaemia in C57Bl6/J mice treated with alloxan. Diabetologia 2004, 47, 259–265. [Google Scholar] [CrossRef] [Green Version]
- Hayek, A.; Beattie, G.M.; Cirulli, V.; Lopez, A.D.; Ricordi, C.; Rubin, J.S. Growth factor/matrix-induced proliferation of human adult beta-cells. Diabetes 1995, 44, 1458–1460. [Google Scholar] [CrossRef] [Green Version]
- Lefebvre, V.H.; Otonkoski, T.; Ustinov, J.; Huotari, M.A.; Pipeleers, D.G.; Bouwens, L. Culture of adult human islet preparations with hepatocyte growth factor and 804G matrix is mitogenic for duct cells but not for beta-cells. Diabetes 1998, 47, 134–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brelje, T.C.; Parsons, J.A.; Sorenson, R.L. Regulation of islet beta-cell proliferation by prolactin in rat islets. Diabetes 1994, 43, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Butler, A.E.; Cao-Minh, L.; Galasso, R.; Rizza, R.A.; Corradin, A.; Cobelli, C.; Butler, P.C. Adaptive changes in pancreatic beta cell fractional area and beta cell turnover in human pregnancy. Diabetologia 2010, 53, 2167–2176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Unno, M.; Itoh, T.; Watanabe, T.; Miyashita, H.; Moriizumi, S.; Teraoka, H.; Yonekura, H.; Okamoto, H. Islet beta-cell regeneration and reg genes. Adv. Exp. Med. Biol. 1992, 321, 61–66, discussion 67–69. [Google Scholar] [CrossRef]
- Rafaeloff, R.; Pittenger, G.L.; Barlow, S.W.; Qin, X.F.; Yan, B.; Rosenberg, L.; Duguid, W.P.; Vinik, A.I. Cloning and sequencing of the pancreatic islet neogenesis associated protein (INGAP) gene and its expression in islet neogenesis in hamsters. J. Clin. Invest. 1997, 99, 2100–2109. [Google Scholar] [CrossRef] [Green Version]
- Ratner, R.E. Double-Blind, Placebo-Controlled Trial of Islet Neogenesis Gene Associated Protein (INGAP) in Type 1 Diabetes (T1DM) Subjects. In Proceedings of the American Diabetes Association 65th Scientific Sessions, London, UK, 9–13 June 2006. [Google Scholar]
- Bensellam, M.; Jonas, J.C.; Laybutt, D.R. Mechanisms of beta-cell dedifferentiation in diabetes: Recent findings and future research directions. J. Endocrinol. 2018, 236, R109–R143. [Google Scholar] [CrossRef] [Green Version]
- Talchai, C.; Xuan, S.; Lin, H.V.; Sussel, L.; Accili, D. Pancreatic beta cell dedifferentiation as a mechanism of diabetic beta cell failure. Cell 2012, 150, 1223–1234. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.H.; Demeterco, C.; Geron, I.; Abrahamsson, A.; Levine, F.; Itkin-Ansari, P. Islet specific Wnt activation in human type II diabetes. Exp. Diabetes Res. 2008, 2008, 728763. [Google Scholar] [CrossRef] [Green Version]
- Cinti, F.; Bouchi, R.; Kim-Muller, J.Y.; Ohmura, Y.; Sandoval, P.R.; Masini, M.; Marselli, L.; Suleiman, M.; Ratner, L.E.; Marchetti, P.; et al. Evidence of beta-Cell Dedifferentiation in Human Type 2 Diabetes. J. Clin. Endocrinol. Metab. 2016, 101, 1044–1054. [Google Scholar] [CrossRef] [Green Version]
- Hallberg, S.J.; Gershuni, V.M.; Hazbun, T.L.; Athinarayanan, S.J. Reversing Type 2 Diabetes: A Narrative Review of the Evidence. Nutrients 2019, 11, 766. [Google Scholar] [CrossRef] [Green Version]
- Rigby, M.R.; Ehlers, M.R. Targeted immune interventions for type 1 diabetes: Not as easy as it looks! Curr. Opin. Endocrinol. Diabetes Obes. 2014, 21, 271–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piran, R.; Lee, S.H.; Li, C.R.; Charbono, A.; Bradley, L.M.; Levine, F. Pharmacological induction of pancreatic islet cell transdifferentiation: Relevance to type I diabetes. Cell Death Dis. 2014, 5, e1357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arrojo, E.D.R.; Ali, Y.; Diez, J.; Srinivasan, D.K.; Berggren, P.O.; Boehm, B.O. New insights into the architecture of the islet of Langerhans: A focused cross-species assessment. Diabetologia 2015, 58, 2218–2228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lam, C.J.; Chatterjee, A.; Shen, E.; Cox, A.R.; Kushner, J.A. Low-Level Insulin Content Within Abundant Non-beta Islet Endocrine Cells in Long-standing Type 1 Diabetes. Diabetes 2019, 68, 598–608. [Google Scholar] [CrossRef] [Green Version]
- Hull, R.L.; Westermark, G.T.; Westermark, P.; Kahn, S.E. Islet amyloid: A critical entity in the pathogenesis of type 2 diabetes. J. Clin. Endocrinol. Metab. 2004, 89, 3629–3643. [Google Scholar] [CrossRef] [Green Version]
- Kilimnik, G.; Zhao, B.; Jo, J.; Periwal, V.; Witkowski, P.; Misawa, R.; Hara, M. Altered islet composition and disproportionate loss of large islets in patients with type 2 diabetes. PLoS ONE 2011, 6, e27445. [Google Scholar] [CrossRef]
- Fernandes, A.; King, L.C.; Guz, Y.; Stein, R.; Wright, C.V.; Teitelman, G. Differentiation of new insulin-producing cells is induced by injury in adult pancreatic islets. Endocrinology 1997, 138, 1750–1762. [Google Scholar] [CrossRef]
- Thorel, F.; Nepote, V.; Avril, I.; Kohno, K.; Desgraz, R.; Chera, S.; Herrera, P.L. Conversion of adult pancreatic alpha-cells to beta-cells after extreme beta-cell loss. Nature 2010, 464, 1149–1154. [Google Scholar] [CrossRef] [Green Version]
- Piran, R.; Lee, S.H.; Kuss, P.; Hao, E.; Newlin, R.; Millan, J.L.; Levine, F. PAR2 regulates regeneration, transdifferentiation, and death. Cell Death Dis. 2016, 7, e2452. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.H.; Hao, E.; Scharp, D.; Levine, F. Insulin acts as a repressive factor to inhibit the ability of PAR2 to induce islet cell transdifferentiation. Islets 2018, 10, 201–212. [Google Scholar] [CrossRef] [Green Version]
- Moin, A.S.M.; Butler, A.E. Alterations in Beta Cell Identity in Type 1 and Type 2 Diabetes. Curr. Diabetes Rep. 2019, 19, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warshauer, J.T.; Bluestone, J.A.; Anderson, M.S. New Frontiers in the Treatment of Type 1 Diabetes. Cell Metab 2020, 31, 46–61. [Google Scholar] [CrossRef] [PubMed]
- Taran, S.; Adhikari, N.K.J.; Fan, E. Falsifiability in medicine: What clinicians can learn from Karl Popper. Intensive Care Med. 2021, 47, 1054–1056. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Levine, F. Approaches to Inducing β-Cell Regeneration. Biomedicines 2022, 10, 571. https://doi.org/10.3390/biomedicines10030571
Levine F. Approaches to Inducing β-Cell Regeneration. Biomedicines. 2022; 10(3):571. https://doi.org/10.3390/biomedicines10030571
Chicago/Turabian StyleLevine, Fred. 2022. "Approaches to Inducing β-Cell Regeneration" Biomedicines 10, no. 3: 571. https://doi.org/10.3390/biomedicines10030571
APA StyleLevine, F. (2022). Approaches to Inducing β-Cell Regeneration. Biomedicines, 10(3), 571. https://doi.org/10.3390/biomedicines10030571





