Meleagrin Isolated from the Red Sea Fungus Penicillium chrysogenum Protects against Bleomycin-Induced Pulmonary Fibrosis in Mice
Abstract
:1. Introduction
2. Materials and Methods
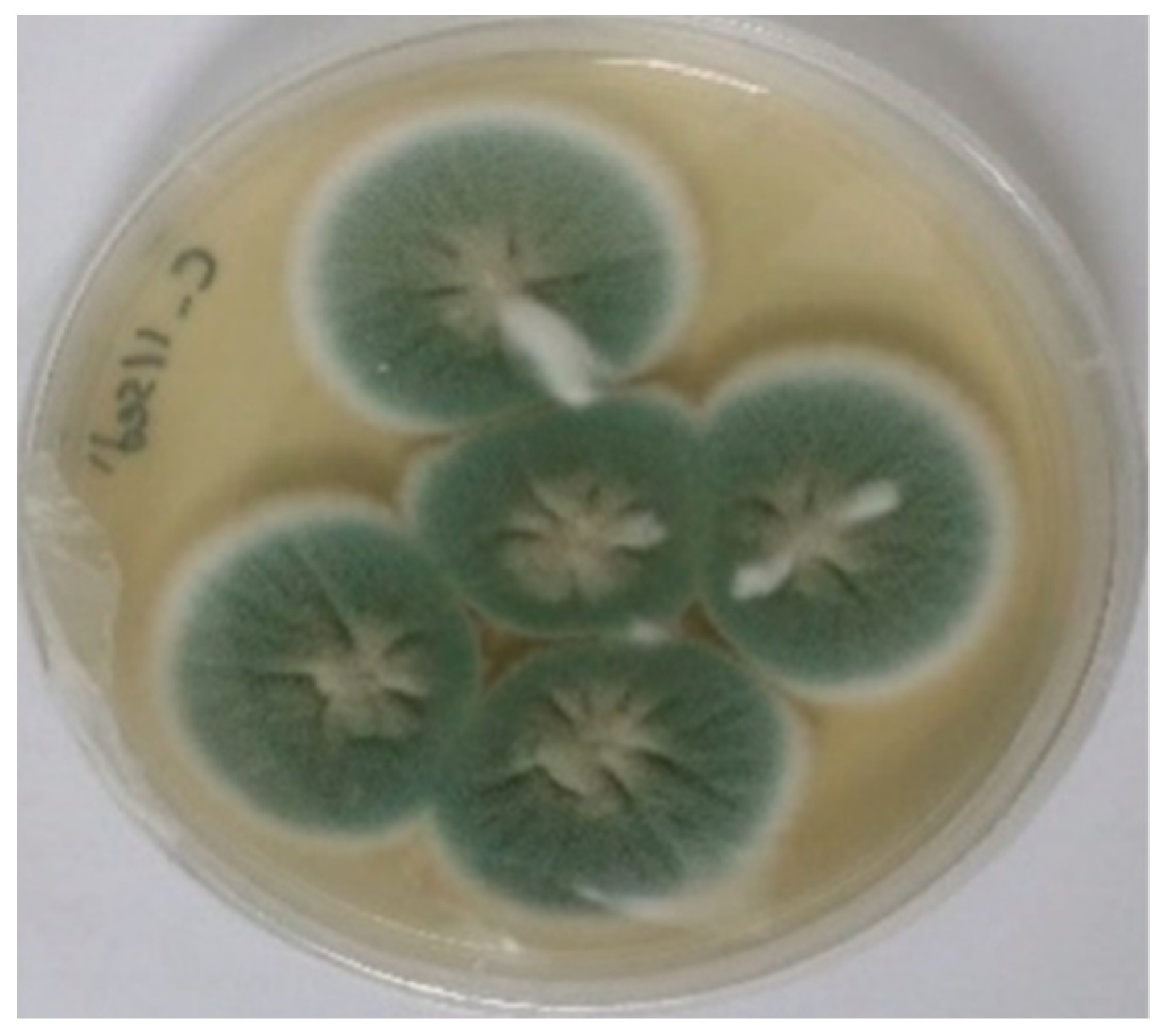
2.1. Collection and Isolation of Marine P. chrysogenum
2.2. Fermentation Method and Extraction Process
2.3. Isolation and Purification of Pure Meleagrin
2.4. Investigation of Meleagrin’s Bilogical Action in a Mouce Model of Bleomycin-Induced Lung Fibrosis
2.4.1. Drugs and Treatment Preparation
2.4.2. Experimental Design
2.4.3. Determination of Oxidative Stress Biomarkers
2.4.4. Quantitative RT-PCR Analysis for Determination of Inflammatory and Fibrotic Biomarkers
2.4.5. Measurement of Protein Levels of Inflammatory, Fibrotic and Apoptotic Biomarkers in Lung Homogenate
2.4.6. Immunohistochemical Examination
2.4.7. Histopathological Examination
2.4.8. Statistical Analysis
3. Results
3.1. Identification of Meleagrin
3.2. In Vivo Investigation of the Effects of Meleagrin in a Model of Bleomycin-Induced Lung Fibrosis in Experimental Mice
3.2.1. Effect of Meleagrin on Markers of Oxidative Stress and Inflammation in the Lung Tissue
3.2.2. Effect of Meleagrin on the Expression of Markers of Apoptosis in the Lung Tissue
3.2.3. Effect of Meleagrin on the Expression of Fibrotic Markers in the Lung Tissue:
3.2.4. Histopathological Examination of the Lung Tissue in the Experimental Mice
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tsukioka, T.; Takemura, S.; Minamiyama, Y.; Mizuguchi, S.; Toda, M.; Okada, S. Attenuation of Bleomycin-induced pulmonary fibrosis in rats with S-Allyl cysteine. Molecules 2017, 22, 543. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.L.; Pu, S.B.; Qi, Y.; Wu, B.F.; Shang, J.H.; Liu, Y.P.; Hu, D.; Luo, X.D. Pharmacological effects of indole alkaloids from Alstonia scholaris (L.) R. Br. on pulmonary fibrosis in vivo. J. Ethnopharmacol. 2021, 267, 113506. [Google Scholar] [CrossRef] [PubMed]
- Kalayarasan, S.; Sriram, N.; Sudhandiran, G. Diallyl sulfide attenuates bleomycin-induced pulmonary fibrosis: Critical role of iNOS, NF-κB, TNF-α and IL-1β. Life Sci. 2008, 82, 1142–1153. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Jiang, M.; He, R.; Lv, X.; Liao, X.; He, Y.; Zhang, F.; Long, L.; Jiang, G.; Peng, Z. Mefunidone Ameliorates Bleomycin-Induced Pulmonary Fibrosis in Mice. Front. Pharmacol. 2021, 12, 713572. [Google Scholar] [CrossRef]
- Huai, B.; Ding, J. Atractylenolide III attenuates bleomycin-induced experimental pulmonary fibrosis and oxidative stress in rat model via Nrf2/NQO1/HO-1 pathway activation. Immunopharmacol. Immunotoxicol. 2020, 42, 436–444. [Google Scholar] [CrossRef]
- Amend, A.; Burgaud, G.; Cunliffe, M.; Edgcomb, V.P.; Ettinger, C.L.; Gutiérrez, M.H.; Heitman, J.; Hom, E.F.Y.; Ianiri, G.; Jones, A.C.; et al. Fungi in the marine environment: Open questions and unsolved problems. mBio 2019, 10, e01189-18. [Google Scholar] [CrossRef] [Green Version]
- Nair, D.G.; Weiskirchen, R.; Al-Musharafi, S.K. Compounds as potential hepatoprotective agents. Acta Pharmacol. Sin. 2015, 36, 158–170. [Google Scholar] [CrossRef] [Green Version]
- Mady, M.S.; Mohyeldin, M.M.; Ebrahim, H.Y.; Elsayed, H.E.; Houssen, W.E.; Haggag, E.G.; Soliman, R.F.; El Sayed, K.A. The indole alkaloid meleagrin, from the olive tree endophytic fungus Penicillium chrysogenum, as a novel lead for the control of c-Met-dependent breast cancer proliferation, migration, and invasion. Bioorg. Med. Chem. 2016, 24, 113–122. [Google Scholar] [CrossRef] [Green Version]
- Youssef, F.S.; Ashour, M.L.; Singab, A.N.B.; Wink, M. A comprehensive review of bioactive peptides from marine fungi and their biological significance. Mar. Drugs 2019, 17, 559. [Google Scholar] [CrossRef] [Green Version]
- Gou, X.; Tian, D.; Wei, J.; Ma, Y.; Zhang, Y.; Chen, M.; Ding, W.; Wu, B.; Tang, J. New drimane sesquiterpenes and polyketides from marine-derived fungus Penicillium sp. TW58-16 and their anti-inflammatory and α-glucosidase inhibitory effects. Mar. Drugs 2021, 19, 416. [Google Scholar] [CrossRef]
- García-Estrada, C.; Ullán, R.V.; Albillos, S.M.; Fernández-Bodega, M.Á.; Durek, P.; von Döhren, H.; Martín, J.F. A single cluster of coregulated genes encodes the biosynthesis of the mycotoxins roquefortine C and meleagrin in Penicillium chrysogenum. Chem. Biol. 2011, 18, 1499–1512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, X.; Wang, Y.; Sun, K.; Liu, P.; Yin, X.; Zhu, W. Cerebrosides and 2-pyridone alkaloids from the halotolerant fungus Penicillium chrysogenum grown in a hypersaline medium. J. Nat. Prod. 2011, 74, 1298–1302. [Google Scholar] [CrossRef] [PubMed]
- Alshehri, S.O.; Malatani, R.T.; Bogari, H.A.; Noor, A.O.; Ibrahim, A.K.; Elhady, S.S.; Abdelhameed, R. LAMA-1: A cerebroside isolated from the deep-sea-derived fungus Penicillium chrysogenum. Metabolites 2020, 10, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, I.-S.; ElSohly, H.N.; Croom, E.M.; Hufford, C.D. Microbial metabolism studies of the antimalarial sesquiterpene artemisinin. J. Nat. Prod. 1989, 52, 337–341. [Google Scholar] [CrossRef]
- Gao, Q.; Leet, J.E.; Thomas, S.T.; Matson, J.A.; Bancroft, D.P. Crystal Structure of Trichodimerol. J. Nat. Prod. 1995, 58, 1817–1821. [Google Scholar] [CrossRef]
- Stierle, D.B.; Stierle, A.A.; Hobbs, J.D.; Stokken, J.; Clardy, J. Berkeleydione and berkeleytrione, new bioactive metabolites from an acid mine organism. Org. Lett. 2004, 6, 1049–1052. [Google Scholar] [CrossRef]
- Bringmann, G.; Lang, G.; Gulder, T.A.M.; Tsuruta, H.; Mühlbacher, J.; Maksimenka, K.; Steffens, S.; Schaumann, K.; Stöhr, R.; Wiese, J.; et al. The first sorbicillinoid alkaloids, the antileukemic sorbicillactones A and B, from a sponge derived Penicillium chrysogenum strain. Tetrahedron 2005, 61, 7252–7265. [Google Scholar] [CrossRef]
- Kim, H.J.; Lee, I.S. Microbial metabolism of the prenylated chalcone xanthohumol. J. Nat. Prod. 2006, 69, 1522–1524. [Google Scholar] [CrossRef]
- De la Campa, R.; Seifert, K.; Miller, J.D. Toxins from strains of Penicillium chrysogenum isolated from buildings and other sources. Mycopathologia 2007, 163, 161–168. [Google Scholar] [CrossRef]
- Murshid, S.S.A.; Badr, J.M.; Youssef, D.T.A. Penicillosides A and B: New cerebrosides from the marine-derived fungus Penicillium species. Rev. Bras. Farmacogn. 2016, 26, 29–33. [Google Scholar] [CrossRef] [Green Version]
- Zheng, C.J.; Sohn, M.J.; Lee, S.; Kim, W.G. Meleagrin, a new FabI inhibitor from Penicillium chryosogenum with at least one additional mode of action. PLoS ONE 2013, 8, e78922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asfour, H.Z.; Awan, Z.A.; Bagalagel, A.A.; Elfaky, M.A.; Abdelhameed, R.F.A.; Elhady, S.S. Large-scale production of bioactive terrein by Aspergillus terreus Strain S020 isolated from the Saudi Coast of the Red Sea. Biomolecules 2019, 9, 480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cortijo, J.; Cerda-Nicolas, M.; Serrano, A.; Bioque, G.; Estrela, J.; Santangelo, F.; Esteras, A.; Llombart-Bosch, A.; Morcillo, E. Attenuation by oral N-acetylcysteine of bleomycin-induced lung injury in rats. Eur. Respir. J. 2001, 17, 1228–1235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Redente, E.F.; Jacobsen, K.M.; Solomon, J.J.; Lara, A.R.; Faubel, S.; Keith, R.C.; Henson, P.M.; Downey, G.P.; Riches, D.W. Age and sex dimorphisms contribute to the severity of bleomycin-induced lung injury and fibrosis. Am. J. Physiol. Lung Cell. Mol. Physiol. 2011, 301, L510–L518. [Google Scholar] [CrossRef]
- Schmittgen, T.D.; Livak, K.J. Analyzing real-time PCR data by the comparative CT method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef]
- De Langhe, E.; Vande Velde, G.; Hostens, J.; Himmelreich, U.; Nemery, B.; Luyten, F.P.; Vanoirbeek, J.; Lories, R.J. Quantification of lung fibrosis and emphysema in mice using automated micro-computed tomography. PLoS ONE 2012, 7, e43123. [Google Scholar] [CrossRef] [Green Version]
- Kawai, K.; Nozawa, K.; Nakajima, S.; Iitaka, Y. Studies on fungal products. VII. The structures of meleagrin and 9-O-p-bromobenzoylmeleagrin. Chem. Pharm. Bull. 1984, 32, 94–98. [Google Scholar] [CrossRef] [Green Version]
- Li, L.-C.; Xu, L.; Hu, Y.; Cui, W.-J.; Cui, W.-H.; Zhou, W.-C.; Kan, L.-D. Astragaloside IV improves bleomycin-induced pulmonary fibrosis in rats by attenuating extracellular matrix deposition. Front. Pharmacol. 2017, 8, 513. [Google Scholar] [CrossRef] [Green Version]
- Chen, L.; Zhao, W. Apigenin protects against bleomycin-induced lung fibrosis in rats. Exp. Ther. Med. 2016, 11, 230–234. [Google Scholar] [CrossRef] [Green Version]
- Kinnula, V.L.; Fattman, C.L.; Tan, R.J.; Oury, T.D. Oxidative stress in pulmonary fibrosis: A possible role for redox modulatory therapy. Am. J. Respir. Crit. Care Med. 2005, 172, 417–422. [Google Scholar] [CrossRef] [Green Version]
- Turgut, N.H.; Kara, H.; Elagoz, S.; Deveci, K.; Gungor, H.; Arslanbas, E. The protective effect of naringin against bleomycin-induced pulmonary fibrosis in Wistar rats. Pulm. Med. 2016, 2016, 7601393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, L.; Wang, X.; Chang, Q.; Xu, J.; Huang, Y.; Guo, Q.; Zhang, S.; Wang, W.; Chen, X.; Wang, J. Neferine, a bisbenzylisoquinline alkaloid attenuates bleomycin-induced pulmonary fibrosis. Eur. J. Pharmacol. 2010, 627, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Luo, S.; Gong, J.; Cao, X.; Liu, S. Ligustilide modulates oxidative stress, apoptosis, and immunity to avoid pathological damages in bleomycin induced pulmonary fibrosis rats via inactivating TLR4/MyD88/NF-KB P65. Ann. Transl. Med. 2020, 8, 931. [Google Scholar] [CrossRef] [PubMed]
- Mansour, H.H.; Omran, M.M.; Hasan, H.F.; El Kiki, S.M. Modulation of bleomycin-induced oxidative stress and pulmonary fibrosis by N-acetylcysteine in rats via AMPK/SIRT1/NF-κβ. Clin. Exp. Pharmacol. Physiol. 2020, 47, 1943–1952. [Google Scholar] [CrossRef]
- Gao, W.; Guo, L.; Yang, Y.; Wang, Y.; Xia, S.; Gong, H.; Zhang, B.K.; Yan, M. Dissecting the Crosstalk Between Nrf2 and NF-kappaB Response Pathways in Drug-Induced Toxicity. Front. Cell Dev. Biol. 2021, 9, 809952. [Google Scholar] [CrossRef]
- Ahmad, A.; Alkharfy, K.M.; Jan, B.L.; Ahad, A.; Ansari, M.A.; Al-Jenoobi, F.I.; Raish, M. Thymoquinone treatment modulates the Nrf2/HO-1 signaling pathway and abrogates the inflammatory response in an animal model of lung fibrosis. Exp. Lung Res. 2020, 46, 53–63. [Google Scholar] [CrossRef]
- Zhao, H.; Li, C.; Li, L.; Liu, J.; Gao, Y.; Mu, K.; Chen, D.; Lu, A.; Ren, Y.; Li, Z. Baicalin alleviates bleomycin-induced pulmonary fibrosis and fibroblast proliferation in rats via the PI3K/AKT signaling pathway. Mol. Med. Rep. 2020, 21, 2321–2334. [Google Scholar] [CrossRef] [Green Version]
- Kendall, R.T.; Feghali-Bostwick, C.A. Fibroblasts in fibrosis: Novel roles and mediators. Front. Pharmacol. 2014, 5, 123. [Google Scholar] [CrossRef] [Green Version]
- Kuang, P.-P.; Zhang, X.-H.; Rich, C.B.; Foster, J.A.; Subramanian, M.; Goldstein, R.H. Activation of elastin transcription by transforming growth factor-β in human lung fibroblasts. Am. J. Physiol. Lung Cell Mol. Physiol. 2007, 292, L944–L952. [Google Scholar] [CrossRef]
- Yang, L.; Chen, P.P.; Luo, M.; Shi, W.L.; Hou, D.S.; Gao, Y.; Xu, S.F.; Deng, J. Inhibitory effects of total ginsenoside on bleomycin-induced pulmonary fibrosis in mice. Biomed. Pharmacother. 2019, 114, 108851. [Google Scholar] [CrossRef]
- Zhou, X.L.; Xu, P.; Chen, H.H.; Zhao, Y.; Shen, J.; Jiang, C.; Jiang, S.; Ni, S.Z.; Xu, B.; Li, L. Thalidomide Inhibits TGF-beta1-induced Epithelial to Mesenchymal Transition in Alveolar Epithelial Cells via Smad-Dependent and Smad-Independent Signaling Pathways. Sci. Rep. 2017, 7, 14727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, R.S.; Xu, G.H.; Cao, J.; Liu, B.; Xie, H.F.; Ishii, Y.; Zhang, C.F. Alpha-mangostin ameliorates bleomycin-induced pulmonary fibrosis in mice partly through activating adenosine 5′-monophosphate-activated protein kinase. Front. Pharmacol. 2019, 10, 1305. [Google Scholar] [CrossRef] [PubMed]
- Qin, R.; Zhao, Q.; Han, B.; Zhu, H.-P.; Peng, C.; Zhan, G.; Huang, W. Indole-Based Small Molecules as Potential Therapeutic Agents for the Treatment of Fibrosis. Front. Pharmacol. 2022, 13, 845892. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.O.; Choi, Y.H. Indole-6-Carboxaldehyde Isolated from Sargassum thunbergii (Mertens) Kuntze Prevents Oxidative Stress-Induced Cellular Damage in V79-4 Chinese Hamster Lung Fibroblasts through the Activation of the Nrf2/HO-1 Signaling Pathway. Cell. Physiol. Biochem. 2020, 54, 959–974. [Google Scholar] [CrossRef]
- Zhao, Y.L.; Yang, Z.F.; Wu, B.F.; Shang, J.H.; Liu, Y.P.; Wang, X.H.; Luo, X.D. Indole alkaloids from leaves of Alstonia scholaris (L.) R. Br. protect against emphysema in mice. J. Ethnopharmacol. 2020, 259, 112949. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.H.; Miao, R.X.; Zhang, Q. Hypaphorine exerts anti-inflammatory effects in sepsis induced acute lung injury via modulating DUSP1/p38/JNK pathway. Kaohsiung J. Med. Sci. 2021, 37, 883–893. [Google Scholar] [CrossRef]
- Li, W.Q.; Li, X.-H.; Du, J.; Zhang, W.; Li, D.; Xiong, X.M.; Li, Y.J. Rutaecarpine attenuates hypoxia-induced right ventricular remodeling in rats. Naunyn Schmiedebergs Arch. Pharmacol. 2016, 389, 757–767. [Google Scholar] [CrossRef]
- Wang, Q.; Yu, J.; Hu, Y.; Chen, X.; Zhang, L.; Pan, T.; Miao, K.; Mou, Y.; Xu, Y.; Xiong, W. Indirubin alleviates bleomycin-induced pulmonary fibrosis in mice by suppressing fibroblast to myofibroblast differentiation. Biomed. Pharmacother. 2020, 131, 110715. [Google Scholar] [CrossRef]
- Ruiz Castro, P.A.; Kogel, U.; Lo Sasso, G.; Phillips, B.W.; Sewer, A.; Titz, B.; Garcia, L.; Kondylis, A.; Guedj, E.; Peric, D. Anatabine ameliorates intestinal inflammation and reduces the production of pro-inflammatory factors in a dextran sulfate sodium mouse model of colitis. J. Inflamm. 2020, 17, 29. [Google Scholar] [CrossRef]

















| GenBank Accession No. | Gene | Primers | Annealing Temperature |
|---|---|---|---|
| NM_009045.5 | NF-κB | Forward: 5′-CAATGGCTACACAGGACCA-3′ | 52 °C |
| Reverse: 5′-CACTGTCACCTGGAACCAGA-3′ | |||
| NM_013693.3 | TNF-α | Forward: 5′-TCTACTGAACTTCGGGGTGATCG-3′ | 56 °C |
| Reverse: 5′-TGATCTGAGTGTGAGGGTCTGGG-3′ | |||
| NM_010902.4 | Nrf-2 | Forward: 5′-CTCTCTGGAGACGGCCATGACT-3′ | 58 °C |
| Reverse: 5′-CTGGGCTGGGGACAGTGGTAGT-3′ | |||
| NM_007742.4 | Collagen-1 | Forward: 5′-GTCCCTGAAGTCAGCTGCATA-3′ | 53 °C |
| Reverse: 5′-TGGGACAGTCCAGTTCTTCAT-3′ | |||
| NM_011577.2 | TGF-β1 | Forward: 5′-CAGTGGCTGAACCAAGGAGAC-3′ | 53 °C |
| Reverse: 5′-ATCCCGTTGATTTCCACGTG-3′ | |||
| NM_007392.3 | α-SMA | Forward: 5′-ACTGCCGAGCGTGAGATTGT-3′ | 52 °C |
| Reverse: 5′-TGATGCTGTTATAGGTGGTTTCG-3′ | |||
| NM_010754.5 | Smad-2 | Forward: 5′-TAGGTGGGGAAGTGTTTGA-3′ | 50ᴼC |
| Reverse: 5′-TGACAGACTGAGCCAGAAGAGC-3′ | |||
| NM_004994.3 | MMP-9 | Forward: 5′-TCGAAGGCGACCTCAAGTG-3′ | 53 °C |
| Reverse: 5′-TTCGGTGTAGCTTTGGATCCA-3′ | |||
| NM_021297.3 | TLR-4 | Forward: 5′-TTTATTCAGAGCCGTTGGTG-3′ | 50 °C |
| Reverse: 5′- CAGAGGATTGTCCTCCCATT-3′ | |||
| NM_007393.5 | β-actin | Forward: 5′-ACGGCCAGGTCATCACTATTG-3′ | 52 °C |
| Reverse: 5′-CAAGAAGGAAGGCTGGAAAAGA-3′ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elhady, S.S.; Goda, M.S.; Mehanna, E.T.; Elfaky, M.A.; Koshak, A.E.; Noor, A.O.; Bogari, H.A.; Malatani, R.T.; Abdelhameed, R.F.A.; Wahba, A.S. Meleagrin Isolated from the Red Sea Fungus Penicillium chrysogenum Protects against Bleomycin-Induced Pulmonary Fibrosis in Mice. Biomedicines 2022, 10, 1164. https://doi.org/10.3390/biomedicines10051164
Elhady SS, Goda MS, Mehanna ET, Elfaky MA, Koshak AE, Noor AO, Bogari HA, Malatani RT, Abdelhameed RFA, Wahba AS. Meleagrin Isolated from the Red Sea Fungus Penicillium chrysogenum Protects against Bleomycin-Induced Pulmonary Fibrosis in Mice. Biomedicines. 2022; 10(5):1164. https://doi.org/10.3390/biomedicines10051164
Chicago/Turabian StyleElhady, Sameh S., Marwa S. Goda, Eman T. Mehanna, Mahmoud A. Elfaky, Abdulrahman E. Koshak, Ahmad O. Noor, Hanin A. Bogari, Rania T. Malatani, Reda F. A. Abdelhameed, and Alaa S. Wahba. 2022. "Meleagrin Isolated from the Red Sea Fungus Penicillium chrysogenum Protects against Bleomycin-Induced Pulmonary Fibrosis in Mice" Biomedicines 10, no. 5: 1164. https://doi.org/10.3390/biomedicines10051164
APA StyleElhady, S. S., Goda, M. S., Mehanna, E. T., Elfaky, M. A., Koshak, A. E., Noor, A. O., Bogari, H. A., Malatani, R. T., Abdelhameed, R. F. A., & Wahba, A. S. (2022). Meleagrin Isolated from the Red Sea Fungus Penicillium chrysogenum Protects against Bleomycin-Induced Pulmonary Fibrosis in Mice. Biomedicines, 10(5), 1164. https://doi.org/10.3390/biomedicines10051164








