Effect of Hyperthyroidism Treatments on Heart Rate Variability: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
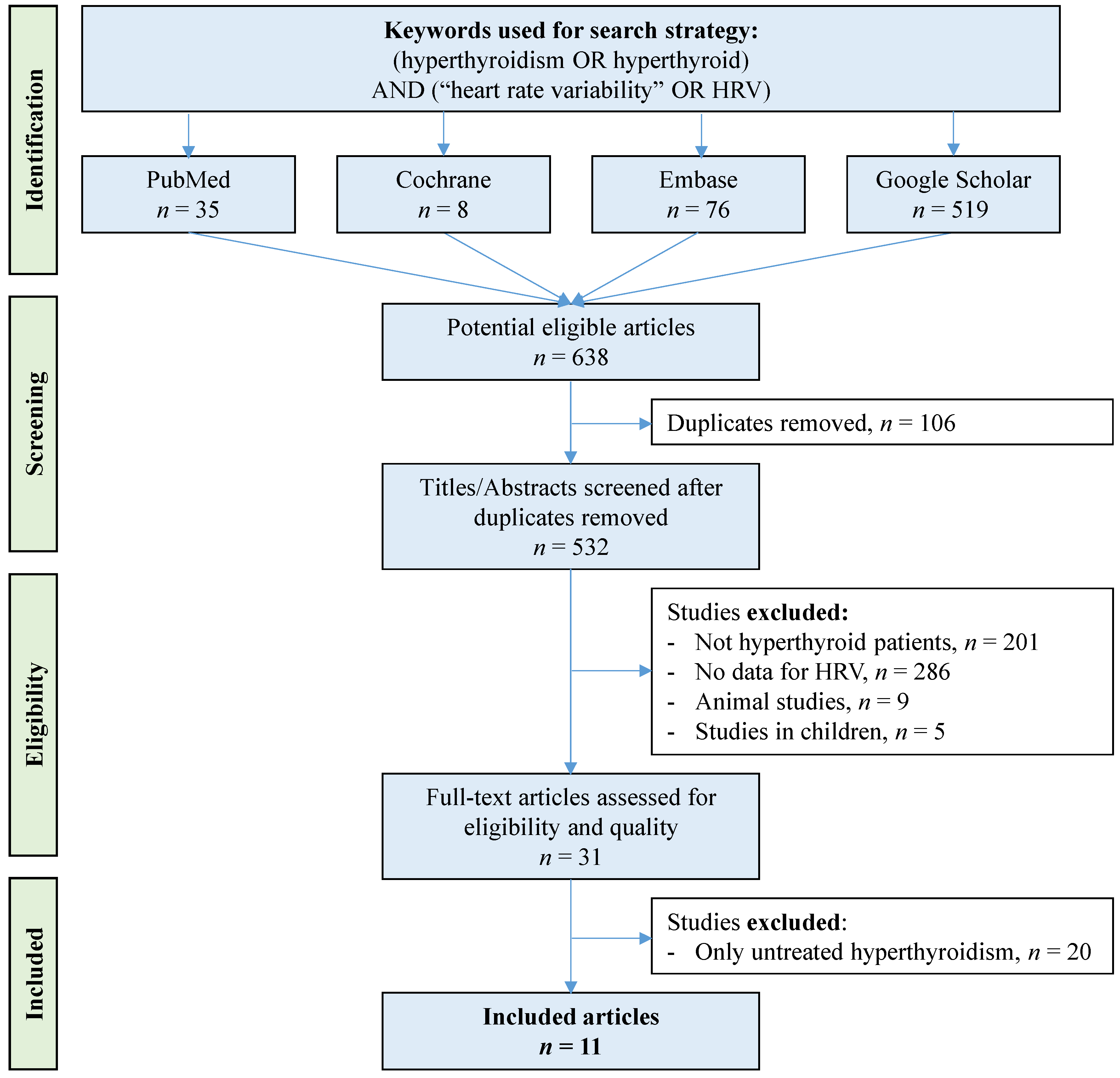
2. Methods
2.1. Literature Search
2.2. Data Extraction
2.3. Quality of Assessment
2.4. Statistical Considerations
3. Results
3.1. Meta-Analysis on the Effect of Antithyroid Treatment on HRV in Hyperthyroid Patients
3.2. Meta-Analysis Stratified by Subclinical or Overt Status
3.3. Meta-Analysis of Treated Patients Compared with Healthy Controls
3.4. Metaregressions and Sensitivity Analyses
4. Discussion
4.1. Effects of Antithyroid Treatment on HRV Parameters in Hyperthyroidism
4.2. Clinical and Therapeutic Implications
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Demers, L.; Spencer, C. Pathophysiology and thyroid function testing. In Tietz Textbook of Clinical Chemistry and Molecular Diagnostics; Burtis, C.A., Ashwood, E.R., Bruns, D.E., Eds.; W.B Saunders: Washington, DC, USA, 2006; pp. 2053–2096. [Google Scholar]
- Delemer, B. Hyperthyroïdie: Signes cliniques et diagnostic étiologique. In Traité d’Endocrinologie, 2nd ed.; Lavoisier Médecine Sciences; Lavoisier: Paris, France, 2019; pp. 187–192. [Google Scholar]
- Sawin, C.T.; Geller, A.; Wolf, P.A.; Belanger, A.J.; Baker, E.; Bacharach, P.; Wilson, P.; Benjamin, E.J.; D’Agostino, R.B. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N. Engl. J. Med. 1994, 331, 1249–1252. [Google Scholar] [CrossRef]
- Clerc, J. Traitement de l’hyperthyroïdie et des goitres par l’iode radioactif. In Traité d’Endocrinologie, 2nd ed.; Lavoisier Médecine Sciences; Lavoisier: Paris, France, 2019; pp. 251–261. [Google Scholar]
- Collet, T.-H.; Gussekloo, J.; Bauer, D.C.; Den Elzen, P.J.; Cappola, A.R.; Balmer, P.; Iervasi, G.; Åsvold, B.O.; Sgarbi, J.A.; Völzke, H.; et al. Subclinical Hyperthyroidism and the Risk of Coronary Heart Disease and Mortality. Arch. Intern. Med. 2012, 172, 799–809. [Google Scholar] [CrossRef]
- Parle, J.V.; Maisonneuve, P.; Sheppard, M.C.; Boyle, P.; A Franklyn, J. Prediction of all-cause and cardiovascular mortality in elderly people from one low serum thyrotropin result: A 10-year cohort study. Lancet 2001, 358, 861–865. [Google Scholar] [CrossRef]
- Tseng, F.-Y.; Lin, W.-Y.; Lin, C.-C.; Lee, L.-T.; Li, T.-C.; Sung, P.-K.; Huang, K.-C. Subclinical Hypothyroidism Is Associated with Increased Risk for All-Cause and Cardiovascular Mortality in Adults. J. Am. Coll. Cardiol. 2012, 60, 730–737. [Google Scholar] [CrossRef]
- Marek, M. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Task Force of The European Society of Cardiology and The North American Society of Pacing and Electrophysiology. Eur. Heart J. 1996, 17, 28. [Google Scholar]
- Brusseau, V.; Tauveron, I.; Bagheri, R.; Ugbolue, U.C.; Magnon, V.; Bouillon-Minois, J.-B.; Navel, V.; Dutheil, F. Heart rate variability in hyperthyroidism: A systematic review and meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 3606. [Google Scholar] [CrossRef] [PubMed]
- La Rovere, M.T.; Bigger, J.T., Jr.; Marcus, F.I.; Mortara, A.; Schwartz, P.J. Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. Lancet 1998, 351, 478–484. [Google Scholar] [CrossRef]
- Dekker, J.M.; Crow, R.S.; Folsom, A.R.; Hannan, P.J.; Liao, D.; Swenne, C.A.; Schouten, E.G. Low heart rate variability in a 2-minute rhythm strip predicts risk of coronary heart disease and mortality from several causes: The ARIC Study. Circulation 2000, 102, 1239–1244. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, R.; Subramanian, M.; Ramasamy, N.; Thangaraj, P.; Murugaiyan, J.; Selvaraj, V. Comparative study on Spectral analysis of heart rate variability in hyperthyroid patients and euthyroids. Natl. J. Physiol. Pharm. Pharmacol. 2015, 5, 93. [Google Scholar] [CrossRef]
- Biondi, B.; Fazio, S.; Carella, C.; Sabatini, D.; Amato, G.; Cittadini, A.; Bellastella, A.; Lombardi, G.; Saccà, L. Control of adrenergic overactivity by beta-blockade improves the quality of life in patients receiving long term suppressive therapy with levothyroxine. J. Clin. Endocrinol. Metab. 1994, 78, 1028–1033. [Google Scholar]
- Biondi, B.; Palmieri, E.A.; Fazio, S.; Cosco, C.; Nocera, M.; Saccà, L.; Filetti, S.; Lombardi, G.; Perticone, F. Endogenous Subclinical Hyperthyroidism Affects Quality of Life and Cardiac Morphology and Function in Young and Middle-Aged Patients. J. Clin. Endocrinol. Metab. 2000, 85, 4701–4705. [Google Scholar] [CrossRef] [PubMed]
- Mercuro, G.; Panzuto, M.G.; Bina, A.; Leo, M.; Cabula, R.; Petrini, L.; Pigliaru, F.; Mariotti, S. Cardiac function, physical exercise capacity, and quality of life during long-term thyrotropin- suppressive therapy with levothyroxine: Effect of individual dose tailoring. J. Clin. Endocrinol. Metab. 2000, 85, 6. [Google Scholar] [CrossRef]
- Falcone, C.; Matrone, B.; Bozzini, S.; Guasti, L.; Falcone, R.; Benzi, A.; Colonna, A.; Savulescu, I.; Vailati, A.; Pelissero, G. Time-Domain Heart Rate Variability in Coronary Artery Disease Patients Affected by Thyroid Dysfunction. Int. Heart J. 2014, 55, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Cooper, D.S. Antithyroid Drugs. N. Engl. J. Med. 2005, 13, 905–917. [Google Scholar] [CrossRef]
- Zhang, J. Effect of Age and Sex on Heart Rate Variability in Healthy Subjects. J. Manip. Physiol. Ther. 2007, 30, 374–379. [Google Scholar] [CrossRef]
- Saleem, S.; Hussain, M.M.; Majeed, S.M.I.; Khan, M.A. Gender differences of heart rate variability in healthy volunteers. J. Pak. Med. Assoc. 2012, 62, 4. [Google Scholar]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar]
- Kuusela, T. Methodological Aspects of Heart Rate Variability Analysis. In Heart Rate Variability (HRV) Signal Analysis Clinical Applications; Kamath, M.V., Watanabe, M., Upton, A., Eds.; CRC Press: Boca Raton, FL, USA, 2012; pp. 9–42. [Google Scholar]
- Umetani, K.; Singer, D.H.; McCraty, R.; Atkinson, M. Twenty-Four Hour Time Domain Heart Rate Variability and Heart Rate: Relations to Age and Gender Over Nine Decades. J. Am. Coll. Cardiol. 1998, 31, 593–601. [Google Scholar] [CrossRef]
- Shaffer, F.; McCraty, R.; Zerr, C.L. A healthy heart is not a metronome: An integrative review of the heart’s anatomy and heart rate variability. Front. Psychol. 2014, 5, 1040. [Google Scholar] [CrossRef]
- Taylor, J.A.; Carr, D.L.; Myers, C.W.; Eckberg, D.L. Mechanisms underlying very-low-frequency RR-interval oscillations in humans. Circulation 1998, 98, 547–555. [Google Scholar] [CrossRef]
- Kleiger, R.E.; Stein, P.K.; Bigger, J.T. Heart rate variability: Measurement and clinical utility. Ann. Noninvasive Electrocardiol. 2005, 10, 88–101. [Google Scholar] [CrossRef]
- Harbour, R.; Miller, J. A new system for grading recommendations in evidence based guidelines. BMJ 2001, 323, 334–336. [Google Scholar] [CrossRef]
- Elm E von Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gotzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Douglas, G.A. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c869. [Google Scholar] [CrossRef]
- Benoist d’Azy, C.; Pereira, B.; Chiambaretta, F.; Dutheil, F. Oxidative and anti-oxidative stress markers in chronic glaucoma: A systematic review and meta-analysis. PLoS ONE 2016, 11, e0166915. [Google Scholar] [CrossRef]
- Benoist d’Azy, C.; Pereira, B.; Naughton, G.; Chiambaretta, F.; Dutheil, F. Antibioprophylaxis in prevention of endophthalmitis in intravitreal injection: A systematic review and meta-analysis. PLoS ONE 2016, 11, e0156431. [Google Scholar] [CrossRef]
- Lanhers, C.; Pereira, B.; Naughton, G.; Trousselard, M.; Lesage, F.-X.; Dutheil, F. Creatine Supplementation and Lower Limb Strength Performance: A Systematic Review and Meta-Analyses. Sports Med. 2015, 45, 1285–1294. [Google Scholar] [CrossRef]
- Lanhers, C.; Pereira, B.; Naughton, G.; Trousselard, M.; Lesage, F.-X.; Dutheil, F. Creatine Supplementation and Upper Limb Strength Performance: A Systematic Review and Meta-Analysis. Sports Med. 2017, 47, 163–173. [Google Scholar] [CrossRef]
- Ollier, M.; Chamoux, A.; Naughton, G.; Pereira, B.; Dutheil, F. Chest CT scan screening for lung cancer in asbestos occupational exposure. Chest 2014, 145, 1339–1346. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Citrome, L. An effect size interpretation is required STAT!: Visualising effect size and an interview with Kristoffer Magnusson. Int. J. Clin. Pract. 2014, 68, 533–534. [Google Scholar] [CrossRef] [PubMed]
- Burggraaf, J.; Tulen, J.H.M.; Lalezari, S.; Schoemaker, R.C.; De Meyer, P.H.E.M.; Meinders, A.E.; Cohen, A.F.; Pijl, H. Sympathovagal imbalance in hyperthyroidism. Am. J. Physiol. Endocrinol. Metab. 2001, 281, 190–195. [Google Scholar] [CrossRef]
- Cacciatori, V.; Bellavere, F.; Pezzarossa, A.; Dellera, A.; Gemma, M.L.; Thomaseth, K.; Castelló, R.; Moghetti, P.; Muggeo, M. Power spectral analysis of heart rate in hyperthyroidism. J. Clin. Endocrinol. Metab. 1996, 81, 2828–2835. [Google Scholar] [PubMed]
- Cai, Z.; Dai, M.; Zhang, Y.; Zhong, H.; Tan, T.; Bao, M. Imbalance of cardiac autonomic nervous activity and increase of ventricular repolarization dynamicity induced by thyroid hormones in hyperthyroidism. Auton. Neurosci. 2018, 213, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.-L.; Chiu, H.-W.; Tseng, Y.-J.; Chu, W.-C. Hyperthyroidism is characterized by both increased sympathetic and decreased vagal modulation of heart rate: Evidence from spectral analysis of heart rate variability. Clin. Endocrinol. 2006, 64, 611–616. [Google Scholar] [CrossRef]
- Eustatia-Rutten, C.F.A.; Corssmit, E.P.M.; Heemstra, K.A.; Smit, J.W.A.; Schoemaker, R.C.; Romijn, J.A.; Burggraaf, J. Autonomic Nervous System Function in Chronic Exogenous Subclinical Thyrotoxicosis and the Effect of Restoring Euthyroidism. J. Clin. Endocrinol. Metab. 2008, 93, 2835–2841. [Google Scholar] [CrossRef]
- Kabir, R.; Begum, N.; Ferdousi, S.; Begum, S.; Ali, T. Heart Rate Variability in Hyperthyroidism. J. Bangladesh Soc. Physiol. 2009, 4, 51–57. [Google Scholar] [CrossRef]
- Osman, F.; Franklyn, J.A.; Daykin, J.; Chowdhary, S.; Holder, R.L.; Sheppard, M.C.; Gammage, M.D. Heart rate variability and turbulence in hyperthyroidism before, during, and after treatment. Am. J. Cardiol. 2004, 94, 465–469. [Google Scholar] [CrossRef]
- Kaminski, G.; Makowski, K.; Michałkiewicz, D.; Kowal, J.; Ruchala, M.; Szczepanek, E.; Gielerak, G. The influence of subclinical hyperthyroidism on blood pressure, heart rate variability, and prevalence of arrhythmias. Thyroid 2012, 22, 454–460. [Google Scholar] [CrossRef]
- Wustmann, K.; Kucera, J.P.; Zanchi, A.; Burow, A.; Stuber, T.; Chappuis, B.; Diem, P.; Delacrétaz, E. Activation of Electrical Triggers of Atrial Fibrillation in Hyperthyroidism. J. Clin. Endocrinol. Metab. 2008, 93, 2104–2108. [Google Scholar] [CrossRef]
- Dökmetas, Y.; Erselcan, A. Is antithyroid treatment really relevant for young patients with subclinical hyperthyroidism. Endocr. J. 2002, 49, 307–314. [Google Scholar]
- Liggett, S.B.; Shah, S.D.; Cryer, P.E. Increased fat and skeletal muscle B-adrenergic receptors but unaltered metabolic and hemodynamic sensitivity to epinephrine in vivo in experimental human thyrotoxicosis. J. Clin. Investig. 1989, 83, 803–809. [Google Scholar] [CrossRef] [PubMed]
- Levey, G.S.; Klein, I. Catecholamine-thyroid hormone interactions and the cardiovascular manifestations of hyperthyroidism. Am. J. Med. 1990, 88, 642–646. [Google Scholar] [CrossRef]
- Coulombe, P.; Dussault, J.H.; Letarte, J.; Simard, S.J. Catecholamines Metabolism in Thyroid Diseases. I. Epinephrine Secretion Rate in Hyperthyroidism and Hypothyroidism. J. Clin. Endocrinol. Metab. 1976, 42, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Maciel, B.C.; Gallo, L.; Neto, J.A.M.; Maciel, L.M.Z.; Alves, M.L.D.; Paccola, G.M.F.; Iazigi, N. The role of the autonomic nervous system in the resting tachycardia of human hyperthyroidism. Clin. Sci. 1987, 72, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.; Taha, W.; Kundumadam, S.; Khan, M. Atrial fibrillation and hyperthyroidism: A literature review. Indian Heart J. 2017, 69, 545–550. [Google Scholar] [CrossRef]
- Insel, P. Adrenergic receptors. Evolving concepts on structure and function. Am. J. Hypertens. 1989, 3 Pt. 2, 112–118. [Google Scholar] [CrossRef]
- Straznicky, N.E.; Eikelis, N.; Lambert, E.A.; Esler, M.D. Mediators of sympathetic activation in metabolic syndrome obesity. Curr. Hypertens. Rep. 2008, 10, 440–447. [Google Scholar] [CrossRef]
- Malliani, A.; Pagani, M.; Lombardi, F.; Cerutti, S. Cardiovascular neural regulation explored in the frequency domain. Circulation 1991, 84, 482–492. [Google Scholar] [CrossRef]
- Maor, E.; Kivity, S.; Kopel, E.; Segev, S.; Sidi, Y.; Goldenberg, I.; Olchovsky, D. Differences in Heart Rate Profile During Exercise Among Subjects with Subclinical Thyroid Disease. Thyroid 2013, 23, 1226–1232. [Google Scholar] [CrossRef]
- Rodondi, N.; Bauer, D.C.; Cappola, A.R.; Cornuz, J.; Robbins, J.; Fried, L.P.; Ladeson, P.M.; Vittinghoff, E.; Gottdiener, J.S.; Newman, A.B. Subclinical thyroid dysfunction, cardiac function, and the risk of heart failure. J. Am. Coll. Cardiol. 2008, 52, 1152–1159. [Google Scholar] [CrossRef] [PubMed]
- Rodondi, N.; den Elzen, W.P.J.; Bauer, D.C.; Cappola, A.R.; Razvi, S.; Walsh, J.P.; Asvold, B.O.; Iervasi, G.; Imaizumi, M.; Collet, T.-H.; et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA 2010, 304, 1365. [Google Scholar] [CrossRef] [PubMed]
- Sawin, C.T. Subclinical Hyperthyroidism and Atrial Fibrillation. Thyroid 2002, 12, 501–503. [Google Scholar] [CrossRef] [PubMed]
- Garmendia Madariaga, A.; Santos Palacios, S.; Guillén-Grima, F.; Galofré, J.C. The incidence and prevalence of thyroid dysfunction in Europe: A meta-analysis. J. Clin. Endocrinol. Metab. 2014, 99, 923–931. [Google Scholar] [CrossRef] [PubMed]
- Boelaert, K.; Torlinska, B.; Holder, R.L.; Franklyn, J.A. Older Subjects with Hyperthyroidism Present with a Paucity of Symptoms and Signs: A Large Cross-Sectional Study. J. Clin. Endocrinol. Metab. 2010, 95, 2715–2726. [Google Scholar] [CrossRef] [PubMed]
- Auer, J.; Scheibner, P.; Mische, T.; Langsteger, W.; Eber, O.; Eber, B. Subclinical hyperthyroidism as a risk factor for atrial fibrillation. Am. Heart J. 2001, 142, 838–842. [Google Scholar] [CrossRef]
- Cappola, A.R.; Fried, L.P.; Arnold, A.M.; Kuller, L.H.; Burke, G.L.; Tracy, R.P.; Ladenson, P.V. Thyroid status, cardiovascular risk, and mortality in older adults: The cardiovascular health study. JAMA 2006, 295, 1033–1041. [Google Scholar] [CrossRef]
- Biondi, B.; Fazio, S.; Coltorti, F.; Palmieri, E.A.; Carella, C.; Lombardi, G.; Sacca, L. Reentrant Atrioventricular Nodal Tachycardia Induced by Levothyroxine. J. Clin. Endocrinol. Metab. 1998, 83, 2643–2645. [Google Scholar] [CrossRef]
- Lombardi, F.; Tarricone, D.; Tundo, F.; Colombo, F.; Belletti, S.; Fiorentini, C. Autonomic nervous system and paroxysmal atrial fibrillation: A study based on the analysis of RR interval changes before, during and after paroxysmal atrial fibrillation. Eur. Heart J. 2004, 25, 1242–1248. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.; Graham, R.R. Clinical Hyperthyroidism Associated with a Normal Basal Metabolic Rate. Can. Med. Assoc. J. 1935, 32, 162–165. [Google Scholar] [PubMed]
- Staffurth, J.S.; Gibberd, M.C.; Fui, S.N. Arterial embolism in thyrotoxicosis with atrial fibrillation. BMJ 1977, 2, 688–690. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, P.J.; La Revere, V. Autonomic nervous system and sudden cardiac death. Experimental basis and clinical observations for post-myocardial infarction risk stratification. Circulation 1992, 85, 177–199. [Google Scholar]
- Levy, M.N. Sympathetic-parasympathetic interactions in the heart. Circ. Res. 1971, 29, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Benichou, T.; Pereira, B.; Mermillod, M.; Tauveron, I.; Pfabigan, D.; Maqdasy, S.; Dutheil, F. Heart rate variability in type 2 diabetes mellitus: A systematic review and meta–analysis. PLoS ONE 2018, 13, e0195166. [Google Scholar] [CrossRef] [PubMed]
- La Rovere, M.T.; Pinna, G.D.; Maestri, R.; Mortara, A.; Capomolla, S.; Febo, O.; Ferrari, R.; Franchini, M.; Gnemmi, M.; Opasich, C.; et al. Short-term heart rate variability strongly predicts sudden cardiac death in chronic heart failure patients. Circulation 2003, 107, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Bigger, J.T.; Fleiss, J.L.; Steinman, R.C.; Rolnitzky, L.M.; Kleiger, R.E.; Rottman, J.N. Frequency domain measures of heart period variability and mortality after myocardial infarction. Circulation 1992, 85, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Hufnagel, C.; Chambres, P.; Bertrand, P.R.; Dutheil, F. The Need for Objective Measures of Stress in Autism. Front. Psychol. 2017, 8, 64. [Google Scholar] [CrossRef] [PubMed]
- Tankeu, A.T.; Azabji-Kenfack, M.; Nganou, C.-N.; Ngassam, E.; Kuate-Mfeukeu, L.; Mba, C.; Dehayem, M.Y.; Mbanya, J.-C.; Sobngwi, E. Effect of propranolol on heart rate variability in hyperthyroidism. BMC Res. Notes 2018, 11, 1–4. [Google Scholar] [CrossRef]
- Pal, G.; Pal, P.; Nanda, N. Integrated Regulation of Cardiovascular Functions. Jaypee Brothers Medical Publishers: New Delhi, India, 2017; Volume 42, pp. 654–657. [Google Scholar]
- LeLorier, J.; Grégoire, G.; Benhaddad, A.; Lapierre, J.; Derderian, F. Discrepancies between meta-analyses and subsequent Large Randomized, Controlled Trials. N. Engl. J. Med. 1997, 337, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Egger, D.S.; Schneider, M. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Lee, Y.H. An overview of meta-analysis for clinicians. Korean J. Intern. Med. 2018, 33, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Sterne, E. Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. J. Clin. Epidemiol. 2001, 54, 1046–1055. [Google Scholar] [CrossRef]
- Copas, S. Meta-analysis, funnel plots and sensitivity analysis. Biostatistic 2000, 1, 247–262. [Google Scholar] [CrossRef] [PubMed]
- Ernst, G. Heart-rate variability—More than heart beats. Front. Public Health 2017, 5, 240. [Google Scholar] [CrossRef]
- Piskorski, J.; Guzik, P. Filtering Poincaré plots. Computational methods in science and technology. ICHB PAS Pozn. Supercomput. Netw. Cent. 2005, 11, 39–48. [Google Scholar]
- Goichot, B. Dysthyroïdies infracliniques. In Traité d’Endocrinologie, 2nd ed.; Lavoisier Médecine Sciences; Lavoisier: Paris, France, 2019; pp. 218–224. [Google Scholar]
- Donangelo, I.; Suh, S.Y. Subclinical Hyperthyroidism: When to Consider Treatment. Am. Fam. Physician 2017, 95, 710–716. [Google Scholar] [PubMed]




| HRV Parameters | ||
|---|---|---|
| Acronym (Unit) | Full Name | Signification |
| Time domain | ||
| RR (ms) | RR-intervals (or normal-to-normal intervals—NN) (i.e., beat-by-beat variations of heart rate) | Overall autonomic activity |
| SDNN (ms) | Standard deviation of RR intervals | Correlated with LF power |
| RMSSD (ms) | Root mean square of successive RR-interval differences | Associated with HF power and hence parasympathetic activity |
| pNN50 (%) | Percentage of adjacent NN intervals varying by more than 50 milliseconds | Associated with HF power and hence parasympathetic activity |
| Frequency domain | ||
| TP (ms2) | Total power i.e., power of all spectral bands | Overall autonomic activity |
| VLF (ms2) | Very low frequency (0.003 to 0.04 Hz) | Thermoregulation, renin-angiotensin system |
| LF (ms2) | Power of the high-frequency band (0.04–0.15 Hz) | Index of both sympathetic and parasympathetic activity, with a predominance of sympathetic |
| HF (ms2) | Power of the high-frequency band (0.15–0.4 Hz) | Represents the most efferent vagal (parasympathetic) activity to the sinus node |
| LF/HF | LF/HF ratio | Sympathovagal balance |
| Study | Country | Design | Subgroup | Intervention | Duration * | Healthy Controls | Age, Years | Sex (% men) | Before Treatment | After Treatment | ECG, min | HRV Parameters | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | fT4, pmol/L | TSH, mIU/L | n | fT4, pmol/L | TSH, mIU/L | |||||||||||
| Burggraaf 2001 | The Netherlands | Prospective | 1 group: Overt | Obtaining 1 month of euthyroidism after antithyroid treatment (ATD **, thiamazole) | 5 ± 3.5 | Yes | 38.9 ± 9.7 | 7.1% | 14 | 64.8 ± 18.9 | 0.2 ± 0.3 | 14 | 16.5 ± 3.6 | 1.4 ± 1.9 | 20 | RR, SDNN, TP, LF, HF, LF/HF |
| Cacciatori 1996 | Italy | Prospective | 1 group: Overt | Treatment by ATD (methimazole) for 12–18 months | 15 ± 3 | Yes | - | - | 8 | 38.0 ± 4.0 | <0.01 | 8 | 10.4 ± 1.4 | 1.8 ± 0.6 | 10 | RR, TP, LF, HF, LF/HF |
| Cai 2018 | China | Prospective | 1 group: Overt | Antithyroid treatment by ATD (carbimazole, PTU ***) ± RT **** | 3.7 ± 0.7 | Yes | 35.0 ± 13.0 | 38.6% | 57 | 122 ± 104 | <0.01 | 50 | 21.9 ± 7.7 | 4.0 ± 2.1 | 1440 | RR, SDNN, RMSSD, pNN50, LF, HF, VLF, LF/HF |
| Chen 2006 | Taiwan | Prospective | 1 group: Overt | Antithyroid treatment by ATD | 6.0 ± 3.0 | Yes | 31.0 ± 2.0 | 9.4% | 32 | 72.9 ± 3.1 | <0.01 | 28 | 15.2 ± 1.0 | 1.9 ± 0.5 | 30 | RR, TP, LF, HF, VLF, LF/HF |
| Eustatia-Rutten 2008 | The Netherlands | Randomised trial | 1 group: Subclinical | Stop TSH-suppression treatment with restauration of euthyroidism at 6 months | 6.0 ± 0.0 | Yes | 51.0 ± 10.5 | 33.3% | 12 | 22.6 ± 3.9 | 0.1 ± 0.1 | 12 | 18.5 ± 4.1 | 3.0 ± 2.3 | 16 | RR, SDNN |
| Falcone 2014 | Italy | Cross-sectional | 2 groups: | No intervention—Two different groups | Yes | 1440 | RR, SDNN, RMSSD, pNN50 | |||||||||
| Untreated subclinical | - | 67.0 ± 14.1 | 17.9% | 28 | 15.4 ± 7.3 | 0.2 ± 0.1 | - | - | - | |||||||
| Treated subclinical by ATD (tapazole) | Unspecified | 66.3 ± 11.0 | 35% | - | - | - | 20 | 14.5 ± 2.8 | 1.7 ± 0.7 | |||||||
| Kabir 2009 | Bangladesh | Cross-sectional | 2 groups: | No intervention—Two different groups (untreated vs treated) | Yes | 5 | RR, SDNN, RMSSD | |||||||||
| Untreated overt | - | 38.9 ± 2.4 | - | 30 | 51.4 ± 7.6 | 0.02 ± 0.01 | - | - | - | |||||||
| Treated overt by ATD | 2.0 ± 0.5 | 40.8 ± 4.8 | - | - | - | - | 30 | 30.4 ± 4.2 | 0.02 ± 0.0 | |||||||
| Kaminski 2012 | Poland | Prospective | 1 group: Subclinical | Obtaining 6 months of euthyroidism after antithyroid treatment (RT) | 6.0 ± 0.0 | No | 45.9 ± 11.0 | 15.9% | 44 | 14.2 ± 2.4 | 0.2 ± 0.1 | 44 | 13.1 ± 1.8 | 1.3 ± 0.8 | 1440 | RMSSD |
| Osman 2004 | United Kingdom | Prospective | 1 group: Overt | Antithyroid treatment by ATD or RT | 6.4 ± 1.2 | Yes | 49.0 ± 12.5 | 23.2% | 224 | 35.8 ± 12.0 | - | 219 | 12.8 ± 2.0 | - | 1440 | RR, SDNN, RMSSD, pNN50 |
| Wustmann 2008 | Switzerland | Prospective | 1 group: Overt | Antithyroid treatment by ATD (carbimazole, PTU) | 16.0 ± 6.0 | No | 43.0 ± 11.0 | 10.7% | 28 | 27.1 ± 14.1 | <0.01 | 28 | 13.1 ± 3.9 | 2.2 ± 1.6 | 1440 | RR, SDNN, RMSSD, pNN50, LF, HF, VLF, LF/HF |
| Yönem 2002 | Turkey | Randomised controls trial | 1 group: Subclinical | Antithyroid treatment by ATD (PTU) and RT | 6.0 ± 0.9 | Yes | 38.7 ± 1.4 | 10% | 10 | 16.4 ± 0.1 | 0.2 ± 0.03 | 10 | 12.7 ± 1.4 | 0.8 ± 0.2 | 1440 | SDNN, RMSSD |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brusseau, V.; Tauveron, I.; Bagheri, R.; Ugbolue, U.C.; Magnon, V.; Bouillon-Minois, J.-B.; Navel, V.; Dutheil, F. Effect of Hyperthyroidism Treatments on Heart Rate Variability: A Systematic Review and Meta-Analysis. Biomedicines 2022, 10, 1982. https://doi.org/10.3390/biomedicines10081982
Brusseau V, Tauveron I, Bagheri R, Ugbolue UC, Magnon V, Bouillon-Minois J-B, Navel V, Dutheil F. Effect of Hyperthyroidism Treatments on Heart Rate Variability: A Systematic Review and Meta-Analysis. Biomedicines. 2022; 10(8):1982. https://doi.org/10.3390/biomedicines10081982
Chicago/Turabian StyleBrusseau, Valentin, Igor Tauveron, Reza Bagheri, Ukadike Chris Ugbolue, Valentin Magnon, Jean-Baptiste Bouillon-Minois, Valentin Navel, and Frederic Dutheil. 2022. "Effect of Hyperthyroidism Treatments on Heart Rate Variability: A Systematic Review and Meta-Analysis" Biomedicines 10, no. 8: 1982. https://doi.org/10.3390/biomedicines10081982








