Navigating the Complexities of Traumatic Encephalopathy Syndrome (TES): Current State and Future Challenges
Abstract
:1. Background
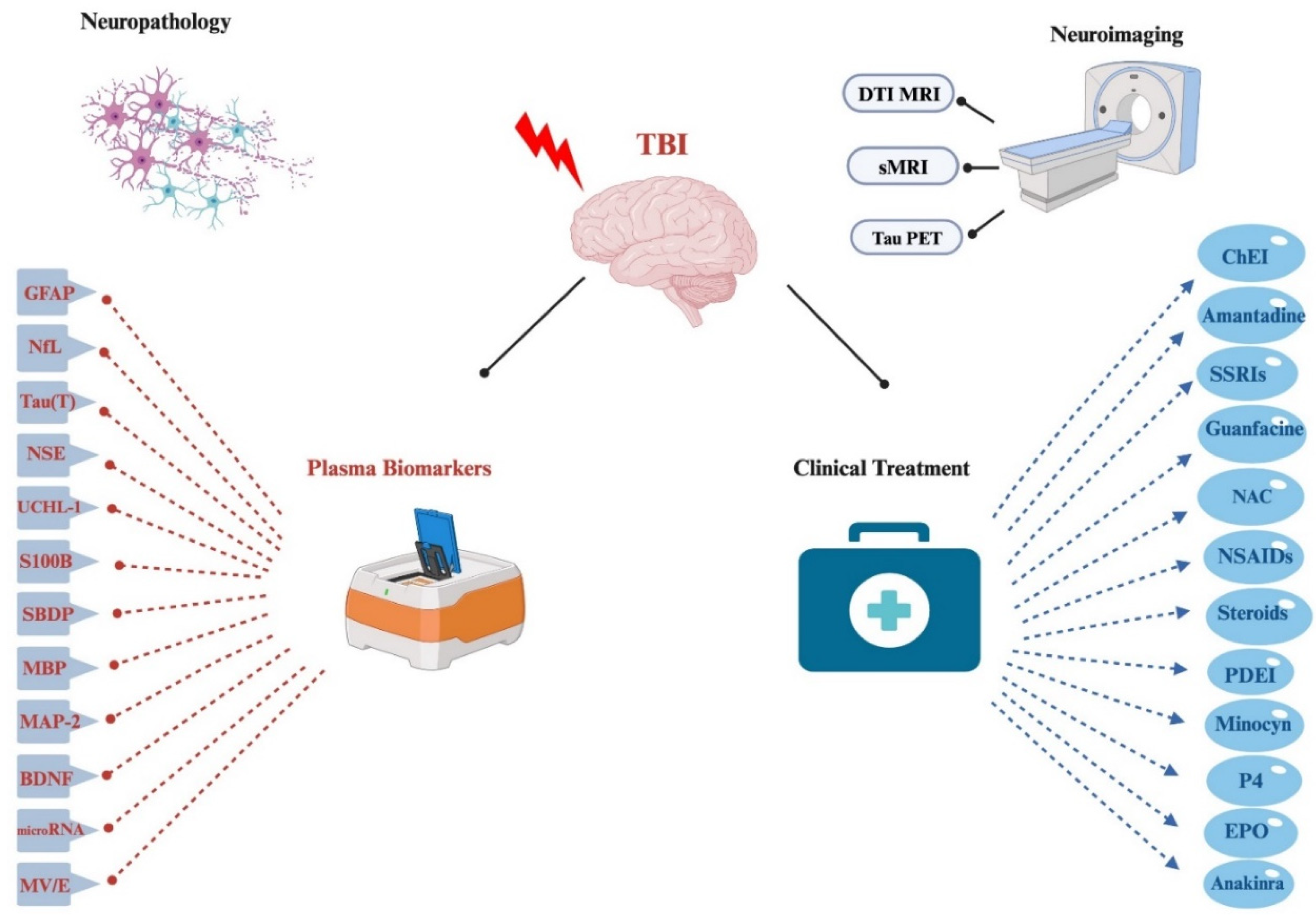
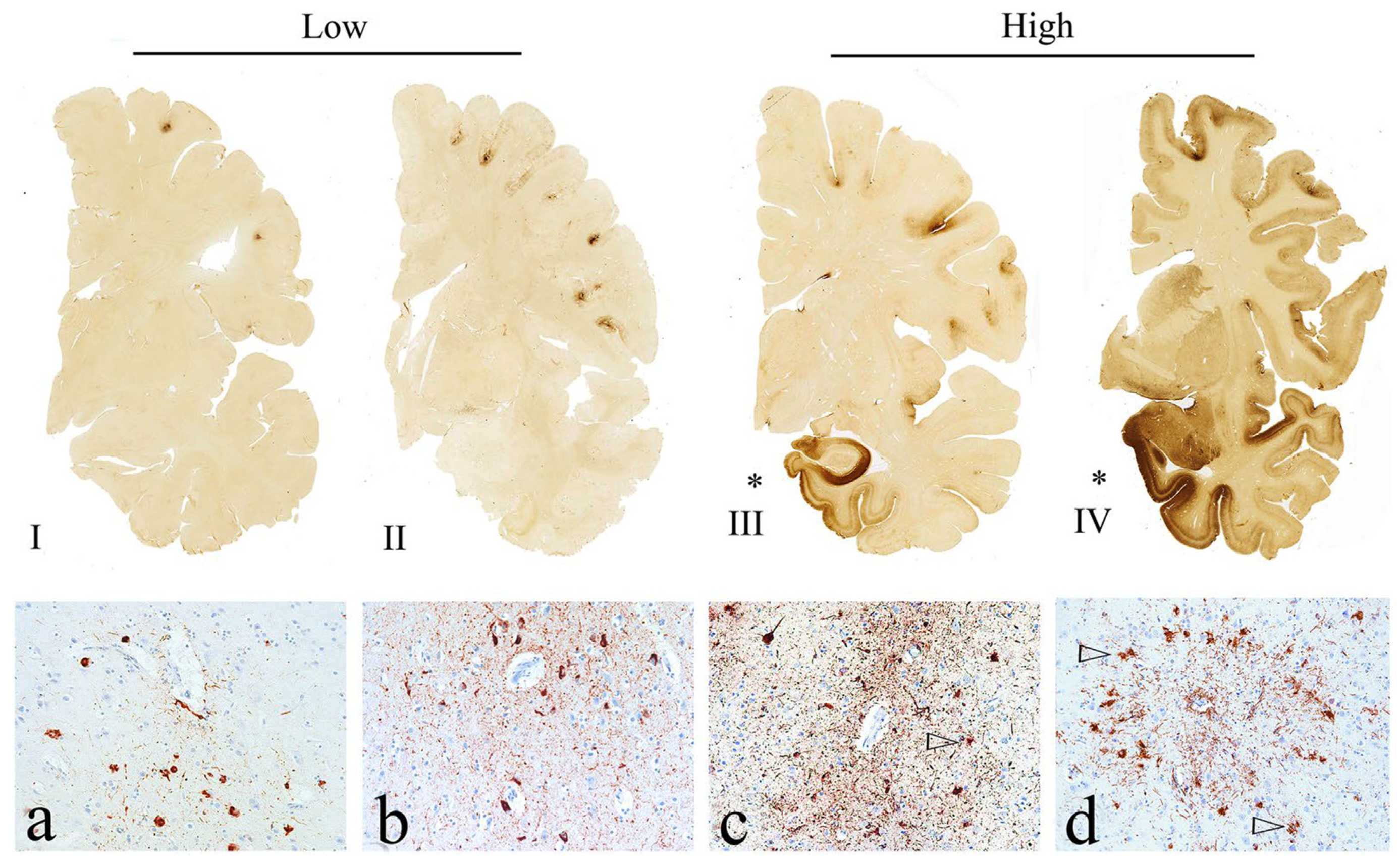
2. Neuropathology
3. Potential TES Biomarkers
3.1. Neuroimaging
3.2. CSF
3.3. Plasma
4. Treatment
4.1. Non-Pharmacological Management
4.2. Clinical Pharmacological Management
4.3. Clinical Use of Nutraceutical Regimen
4.4. Preclinical Investigational Pharmacological Intervention
4.5. Targeting Tau Acetylation
4.6. Targeting Tau Phosphorylation
4.7. Targeting Inflammation
4.8. Immunotherapy
4.9. Potential Dietary Targets
5. Future Directions
Funding
Conflicts of Interest
References
- McKee, A.C.; the TBI/CTE group; Cairns, N.J.; Dickson, D.W.; Folkerth, R.D.; Keene, C.D.; Litvan, I.; Perl, D.P.; Stein, T.D.; Vonsattel, J.-P.; et al. The first NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. Acta Neuropathol. 2016, 131, 75–86. [Google Scholar] [CrossRef]
- Martland, H.S. Punch drunk. J. Am. Med. Assoc. 1928, 91, 1103–1107. [Google Scholar] [CrossRef]
- Castellani, R.J.; Perry, G. Dementia pugilistica revisited. J. Alzheimer’s Dis. 2017, 60, 1209–1221. [Google Scholar] [CrossRef] [PubMed]
- Asken, B.M.; Sullan, M.J.; DeKosky, S.T.; Jaffee, M.S.; Bauer, R.M. Research gaps and controversies in chronic traumatic encephalopathy: A review. JAMA Neurol. 2017, 74, 1255–1262. [Google Scholar] [CrossRef] [PubMed]
- Omalu, B.I.; DeKosky, S.T.; Minster, R.L.; Kamboh, M.I.; Hamilton, R.L.; Wecht, C.H. Chronic traumatic encephalopathy in a National Football League player. Neurosurgery 2005, 57, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Omalu, B.I.; DeKosky, S.T.; Hamilton, R.L.; Minster, R.L.; Kamboh, M.I.; Shakir, A.M.; Wecht, C.H. Chronic traumatic encephalopathy in a national football league player: Part II. Neurosurgery 2006, 59, 1086–1092. [Google Scholar] [CrossRef] [PubMed]
- Omalu, B.I.; Bailes, J.; Hammers, J.L.; Fitzsimmons, R.P. Chronic traumatic encephalopathy, suicides and parasuicides in professional American athletes: The role of the forensic pathologist. Am. J. Forensic Med. Pathol. 2010, 31, 130–132. [Google Scholar] [CrossRef]
- Montenigro, P.H.; Baugh, C.M.; Daneshvar, D.H.; Mez, J.; Budson, A.E.; Au, R.; Katz, D.I.; Cantu, R.C.; Stern, R.A. Clinical subtypes of chronic traumatic encephalopathy: Literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimer’s Res. Ther. 2014, 6, 68. [Google Scholar] [CrossRef]
- Mez, J.; Alosco, M.L.; Daneshvar, D.H.; Saltiel, N.; Baucom, Z.; Abdolmohammadi, B.; Uretsky, M.; Nicks, R.; Martin, B.M.; Palmisano, J.N.; et al. Validity of the 2014 traumatic encephalopathy syndrome criteria for CTE pathology. Alzheimer’s Dement. 2021, 17, 1709–1724. [Google Scholar] [CrossRef]
- Kelly, J.P.; Priemer, D.S.; Perl, D.P.; Filley, C.M. Sports concussion and chronic traumatic encephalopathy: Finding a path forward. Ann. Neurol. 2023, 93, 222–225. [Google Scholar] [CrossRef]
- Corsellis, J.; Bruton, C.; Freeman-Browne, D. The aftermath of boxing1. Psychol. Med. 1973, 3, 270–303. [Google Scholar] [CrossRef] [PubMed]
- McKee, A.C.; Stein, T.D.; Nowinski, C.J.; Stern, R.A.; Daneshvar, D.H.; Alvarez, V.E.; Lee, H.-S.; Hall, G.; Wojtowicz, S.M.; Baugh, C.M.; et al. The spectrum of disease in chronic traumatic encephalopathy. Brain 2013, 136, 43–64. [Google Scholar] [CrossRef] [PubMed]
- Alosco, M.L.; Mariani, M.L.; Adler, C.H.; Balcer, L.J.; Bernick, C.; Au, R.; Banks, S.J.; Barr, W.B.; Bouix, S.; Cantu, R.C.; et al. Developing methods to detect and diagnose chronic traumatic encephalopathy during life: Rationale, design, and methodology for the DIAGNOSE CTE Research Project. Alzheimer’s Res. Ther. 2021, 13, 136. [Google Scholar] [CrossRef] [PubMed]
- Falcon, B.; Zivanov, J.; Zhang, W.; Murzin, A.G.; Garringer, H.J.; Vidal, R.; Crowther, R.A.; Newell, K.L.; Ghetti, B.; Goedert, M.; et al. Novel tau filament fold in chronic traumatic encephalopathy encloses hydrophobic molecules. Nature 2019, 568, 420–423. [Google Scholar] [CrossRef] [PubMed]
- McKee, A.C.; Stein, T.D.; Kiernan, P.T.; Alvarez, V.E. The neuropathology of chronic traumatic encephalopathy. Brain Pathol. 2015, 25, 350–364. [Google Scholar] [CrossRef] [PubMed]
- Gardner, A.; Iverson, G.L.; McCrory, P. Chronic traumatic encephalopathy in sport: A systematic review. Br. J. Sports Med. 2014, 48, 84–90. [Google Scholar] [CrossRef]
- McKee, A.C.; Stein, T.D.; Huber, B.R.; Crary, J.F.; Bieniek, K.; Dickson, D.; Alvarez, V.E.; Cherry, J.D.; Farrell, K.; Butler, M.; et al. Chronic traumatic encephalopathy (CTE): Criteria for neuropathological diagnosis and relationship to repetitive head impacts. Acta Neuropathol. 2023, 145, 371–394. [Google Scholar] [CrossRef] [PubMed]
- Bieniek, K.F.; Blessing, M.M.; Heckman, M.G.; Diehl, N.N.; Serie, A.M.; Paolini, M.A.; Boeve, B.F.; Savica, R.; Reichard, R.R.; Dickson, D.W. Association between contact sports participation and chronic traumatic encephalopathy: A retrospective cohort study. Brain Pathol. 2020, 30, 63–74. [Google Scholar] [CrossRef]
- Stern, R.A.; Daneshvar, D.H.; Baugh, C.M.; Seichepine, D.R.; Montenigro, P.H.; Riley, D.O.; Fritts, N.G.; Stamm, J.M.; Robbins, C.A.; McHale, L.; et al. Clinical presentation of chronic traumatic encephalopathy. Neurology 2013, 81, 1122–1129. [Google Scholar] [CrossRef]
- Wang, K.K.; Yang, Z.; Zhu, T.; Shi, Y.; Rubenstein, R.; Tyndall, J.A.; Manley, G.T. An update on diagnostic and prognostic biomarkers for traumatic brain injury. Expert Rev. Mol. Diagn. 2018, 18, 165–180. [Google Scholar] [CrossRef]
- Asken, B.M.; Elahi, F.M.; La Joie, R.; Strom, A.; Staffaroni, A.M.; Lindbergh, C.A.; Apple, A.C.; You, M.; Weiner-Light, S.; Brathaban, N.; et al. Plasma glial fibrillary acidic protein levels differ along the spectra of amyloid burden and clinical disease stage. J. Alzheimer’s Dis. 2020, 78, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Schulte, S.; Podlog, L.W.; Hamson-Utley, J.J.; Strathmann, F.G.; Strüder, H.K. A systematic review of the biomarker S100B: Implications for sport-related concussion management. J. Athl. Train. 2014, 49, 830–850. [Google Scholar] [CrossRef] [PubMed]
- Stein, D.M.; Kufera, J.A.; Lindell, A.; Murdock, K.R.; Menaker, J.; Bochicchio, G.V.; Aarabi, B.; Scalea, T.M. Association of CSF biomarkers and secondary insults following severe traumatic brain injury. Neurocrit. Care 2011, 14, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.P.; Pierce, M.C.; Wisniewski, S.R.; Adelson, P.D.; Clark, R.S.B.; Ruppel, R.A.; Kochanek, P.M. Neuron-specific enolase and S100B in cerebrospinal fluid after severe traumatic brain injury in infants and children. Pediatrics 2002, 109, e31. [Google Scholar] [CrossRef]
- Abdel Baki, S.G.; Schwab, B.; Haber, M.; Fenton, A.A.; Bergold, P.J. Minocycline synergizes with N-acetylcysteine and improves cognition and memory following traumatic brain injury in rats. PLoS ONE 2010, 5, e12490. [Google Scholar] [CrossRef]
- Filippidis, A.S.; Papadopoulos, D.C.; Kapsalaki, E.Z.; Fountas, K.N. Role of the S100B serum biomarker in the treatment of children suffering from mild traumatic brain injury. Neurosurg. Focus 2010, 29, E2. [Google Scholar] [CrossRef] [PubMed]
- Kiechle, K.; Bazarian, J.J.; Merchant-Borna, K.; Stoecklein, V.; Rozen, E.; Blyth, B.; Huang, J.H.; Dayawansa, S.; Kanz, K.; Biberthaler, P. Subject-specific increases in serum S-100B distinguish sports-related concussion from sports-related exertion. PLoS ONE 2014, 9, e84977. [Google Scholar] [CrossRef] [PubMed]
- Mondello, S.; Robicsek, S.A.; Gabrielli, A.; Brophy, G.M.; Papa, L.; TepasIII, J.; Robertson, C.; Buki, A.; Scharf, D.; Jixiang, M.; et al. αII-spectrin breakdown products (SBDPs): Diagnosis and outcome in severe traumatic brain injury patients. J. Neurotrauma 2010, 27, 1203–1213. [Google Scholar] [CrossRef]
- Korley, F.K.; Diaz-Arrastia, R.; Wu, A.H.B.; Yue, J.K.; Manley, G.T.; Sair, H.I.; Van Eyk, J.E.; Everett, A.D.; Okonkwo, D.O.; Valadka, A.B.; et al. Circulating brain-derived neurotrophic factor has diagnostic and prognostic value in traumatic brain injury. J. Neurotrauma 2016, 33, 215–225. [Google Scholar] [CrossRef]
- Diaz-Arrastia, R.; Papa, L.; Sorani, M.D.; Yue, J.K.; Puccio, A.M.; McMahon, P.J.; Inoue, T.; Yuh, E.L.; Lingsma, H.F.; Valadka, A.B.; et al. Acute biomarkers of traumatic brain injury: Relationship between plasma levels of ubiquitin C-terminal hydrolase-L1 and glial fibrillary acidic protein. J. Neurotrauma 2014, 31, 19–25. [Google Scholar] [CrossRef]
- Papa, L.; Robicsek, S.A.; Brophy, G.M.; Wang, K.K.; Hannay, H.J.; Heaton, S.; Schmalfuss, I.; Gabrielli, A.; Hayes, R.L.; Robertson, C.S. Temporal profile of microtubule-associated protein 2: A novel indicator of diffuse brain injury severity and early mortality after brain trauma. J. Neurotrauma 2018, 35, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Brophy, G.M.; Mondello, S.; Papa, L.; Robicsek, S.A.; Gabrielli, A.; Tepas, J.; Buki, A.; Robertson, C.; Tortella, F.C.; Hayes, R.L.; et al. Biokinetic analysis of ubiquitin C-terminal hydrolase-L1 (UCH-L1) in severe traumatic brain injury patient biofluids. J. Neurotrauma 2011, 28, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Balakathiresan, N.; Bhomia, M.; Chandran, R.; Chavko, M.; McCarron, R.M.; Maheshwari, R.K.; Papa, L.; Slobounov, S.M.; Breiter, H.C.; Walter, A.; et al. MicroRNA let-7i is a promising serum biomarker for blast-induced traumatic brain injury. J. Neurotrauma 2012, 29, 1379–1387. [Google Scholar] [CrossRef] [PubMed]
- Mitra, B.; Rau, T.F.; Surendran, N.; Brennan, J.H.; Thaveenthiran, P.; Sorich, E.; Fitzgerald, M.C.; Rosenfeld, J.V.; Patel, S.A. Plasma micro-RNA biomarkers for diagnosis and prognosis after traumatic brain injury: A pilot study. J. Clin. Neurosci. 2017, 38, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Stern, R.A.; Tripodis, Y.; Baugh, C.M.; Fritts, N.G.; Martin, B.M.; Chaisson, C.; Cantu, R.C.; Joyce, J.A.; Shah, S.; Ikezu, T.; et al. Preliminary study of plasma exosomal tau as a potential biomarker for chronic traumatic encephalopathy. J. Alzheimer’s Dis. 2016, 51, 1099–1109. [Google Scholar] [CrossRef] [PubMed]
- Shi, K.; Zhang, J.; Dong, J.-F.; Shi, F.-D. Dissemination of brain inflammation in traumatic brain injury. Cell. Mol. Immunol. 2019, 16, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Asken, B.M.; Tanner, J.A.; VandeVrede, L.; Casaletto, K.B.; Staffaroni, A.M.; Mundada, N.; Iaccarino, L.; La Joie, R.; Tsuei, T.; Mladinov, M.; et al. Multi-Modal Biomarkers of Repetitive Head Impacts and Traumatic Encephalopathy Syndrome: A Clinicopathological Case Series. J. Neurotrauma 2022, 39, 1195–1213. [Google Scholar] [CrossRef]
- Strain, J.; Didehbani, N.; Cullum, C.M.; Mansinghani, S.; Conover, H.; Kraut, M.A.; Hart, J.; Womack, K.B. Depressive symptoms and white matter dysfunction in retired NFL players with concussion history. Neurology 2013, 81, 25–32. [Google Scholar] [CrossRef]
- Turk, K.W.; Budson, A.E. Chronic traumatic encephalopathy. Contin. Lifelong Learn. Neurol. 2019, 25, 187–207. [Google Scholar] [CrossRef]
- Stern, R.A.; Adler, C.H.; Chen, K.; Navitsky, M.; Luo, J.; Dodick, D.W.; Alosco, M.L.; Tripodis, Y.; Goradia, D.D.; Martin, B.; et al. Tau positron-emission tomography in former national football league players. N. Engl. J. Med. 2019, 380, 1716–1725. [Google Scholar] [CrossRef]
- Grashow, R.; Weisskopf, M.G.; Baggish, A.; Speizer, F.E.; Whittington, A.J.; Nadler, L.; Connor, A.; Keske, R.; Taylor, H.; Zafonte, R.; et al. Premortem chronic traumatic encephalopathy diagnoses in professional football. Ann. Neurol. 2020, 88, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Alosco, M.L.; Tripodis, Y.; Fritts, N.G.; Heslegrave, A.; Baugh, C.M.; Conneely, S.; Mariani, M.; Martin, B.M.; Frank, S.; Mez, J.; et al. Cerebrospinal fluid tau, Aβ, and sTREM2 in Former National Football League Players: Modeling the relationship between repetitive head impacts, microglial activation, and neurodegeneration. Alzheimer’s Dement. 2018, 14, 1159–1170. [Google Scholar] [CrossRef] [PubMed]
- Benedet, A.L.; Hu, Y.; Cummings, J.; Mattke, S.; Iwatsubo, T.; Nakamura, A.; Vellas, B.; O’Bryant, S.; Shaw, L.M.; Cho, M.; et al. Differences between plasma and cerebrospinal fluid glial fibrillary acidic protein levels across the Alzheimer disease continuum. JAMA Neurol. 2021, 78, 1471–1483. [Google Scholar] [CrossRef]
- Pereira, J.B.; Janelidze, S.; Smith, R.; Mattsson-Carlgren, N.; Palmqvist, S.; E Teunissen, C.; Zetterberg, H.; Stomrud, E.; Ashton, N.J.; Blennow, K.; et al. Plasma GFAP is an early marker of amyloid-β but not tau pathology in Alzheimer’s disease. Brain 2021, 144, 3505–3516. [Google Scholar] [CrossRef] [PubMed]
- Böhmer, A.E.; Oses, J.P.; Schmidt, A.P.; Perón, C.S.; Krebs, C.L.; Oppitz, P.P.; D’Avila, T.T.; Souza, D.O.; Portela, L.V.; Stefani, M.A.; et al. Neuron-specific enolase, S100B, and glial fibrillary acidic protein levels as outcome predictors in patients with severe traumatic brain injury. Neurosurgery 2011, 68, 1624–1631. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Zhang, C.; Liu, W.; Luo, P.; Zhang, L.; Wang, Y.; Wang, Z.; Fei, Z. A novel rat model of blast-induced traumatic brain injury simulating different damage degree: Implications for morphological, neurological, and biomarker changes. Front. Cell. Neurosci. 2015, 9, 168. [Google Scholar] [CrossRef] [PubMed]
- Topolovec-Vranic, J.; Pollmann-Mudryj, M.-A.; Ouchterlony, D.; Klein, D.; Spence, J.; Romaschin, A.; Rhind, S.; Tien, H.C.; Baker, A.J. The value of serum biomarkers in prediction models of outcome after mild traumatic brain injury. J. Trauma Acute Care Surg. 2011, 71, S478–S486. [Google Scholar] [CrossRef] [PubMed]
- Buonora, J.E.; Yarnell, A.M.; Lazarus, R.C.; Mousseau, M.; Latour, L.L.; Rizoli, S.B.; Baker, A.J.; Rhind, S.; Diaz-Arrastia, R.; Mueller, G.P. Multivariate analysis of traumatic brain injury: Development of an assessment score. Front. Neurol. 2015, 6, 68. [Google Scholar] [CrossRef]
- Verfaillie, C.J.; Delanghe, J.R. Hemolysis correction factor in the measurement of serum neuron-specific enolase. Clin. Chem. Lab. Med. 2010, 48, 891–892. [Google Scholar] [CrossRef]
- Kobeissy, F.H.; Ottens, A.K.; Zhang, Z.; Liu, M.C.; Denslow, N.D.; Dave, J.R.; Tortella, F.C.; Hayes, R.L.; Wang, K.K. Novel differential neuroproteomics analysis of traumatic brain injury in rats. Mol. Cell. Proteom. 2006, 5, 1887–1898. [Google Scholar] [CrossRef]
- Mondello, S.; Linnet, A.; Buki, A.; Robicsek, S.; Gabrielli, A.; Tepas, J.; Papa, L.; Brophy, G.M.; Tortella, F.; Hayes, R.L.; et al. Clinical utility of serum levels of ubiquitin C-terminal hydrolase as a biomarker for severe traumatic brain injury. Neurosurgery 2012, 70, 666. [Google Scholar] [PubMed]
- Blyth, B.J.; Farhavar, A.; Gee, C.; Hawthorn, B.; He, H.; Nayak, A.; Stöcklein, V.; Bazarian, J.J. Validation of serum markers for blood-brain barrier disruption in traumatic brain injury. J. Neurotrauma 2009, 26, 1497–1507. [Google Scholar] [CrossRef] [PubMed]
- Papa, L.; Akinyi, L.; Liu, M.C.; Pineda, J.A.; Tepas, J.J., 3rd; Oli, M.W.; Zheng, W.; Robinson, G.; Robicsek, S.A.; Gabrielli, A.; et al. Ubiquitin C-terminal hydrolase is a novel biomarker in humans for severe traumatic brain injury. Crit. Care Med. 2010, 38, 138. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.-Y.; Zhang, L.-X.; Dong, X.-Q.; Yu, W.-H.; Du, Q.; Yang, D.-B.; Shen, Y.-F.; Wang, H.; Zhu, Q.; Che, Z.-H.; et al. Comparison of the performances of copeptin and multiple biomarkers in long-term prognosis of severe traumatic brain injury. Peptides 2014, 60, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Papa, L.; Lewis, L.M.; Falk, J.L.; Zhang, Z.; Silvestri, S.; Giordano, P.; Brophy, G.M.; Demery, J.A.; Dixit, N.K.; Ferguson, I.; et al. Elevated levels of serum glial fibrillary acidic protein breakdown products in mild and moderate traumatic brain injury are associated with intracranial lesions and neurosurgical intervention. Ann. Emerg. Med. 2012, 59, 471–483. [Google Scholar] [CrossRef] [PubMed]
- Bazarian, J.J.; Biberthaler, P.; Welch, R.D.; Lewis, L.M.; Barzo, P.; Bogner-Flatz, V.; Brolinson, P.G.; Büki, A.; Chen, J.Y.; Christenson, R.H.; et al. Serum GFAP and UCH-L1 for prediction of absence of intracranial injuries on head CT (ALERT-TBI): A multicentre observational study. Lancet Neurol. 2018, 17, 782–789. [Google Scholar] [CrossRef] [PubMed]
- Korley, F.K.; Datwyler, S.A.; Jain, S.; Sun, X.; Beligere, G.; Chandran, R.; Marino, J.A.; McQuiston, B.; Zhang, H.; Caudle, K.L.; et al. Comparison of GFAP and UCH-L1 measurements from two prototype assays: The Abbott i-STAT and ARCHITECT assays. Neurotrauma Rep. 2021, 2, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Cervellin, G.; Benatti, M.; Carbucicchio, A.; Mattei, L.; Cerasti, D.; Aloe, R.; Lippi, G. Serum levels of protein S100B predict intracranial lesions in mild head injury. Clin. Biochem. 2012, 45, 408–411. [Google Scholar] [CrossRef]
- Papa, L.; Benatti, M.; Carbucicchio, A.; Mattei, L.; Cerasti, D.; Aloe, R.; Lippi, G. GFAP out-performs S100β in detecting traumatic intracranial lesions on computed tomography in trauma patients with mild traumatic brain injury and those with extracranial lesions. J. Neurotrauma 2014, 31, 1815–1822. [Google Scholar] [CrossRef]
- Metting, Z.; Wilczak, N.; Rodiger, L.; Schaaf, J.; Van Der Naalt, J. GFAP and S100B in the acute phase of mild traumatic brain injury. Neurology 2012, 78, 1428–1433. [Google Scholar] [CrossRef]
- Barbosa, R.R.; Jawa, R.; Watters, J.M.; Knight, J.C.; Kerwin, A.J.; Winston, E.S.; Barraco, R.D.; Tucker, B.; Bardes, J.M.; Rowell, S.E.; et al. Evaluation and management of mild traumatic brain injury: An Eastern Association for the Surgery of Trauma practice management guideline. J. Trauma Acute Care Surg. 2012, 73, S307–S314. [Google Scholar] [CrossRef] [PubMed]
- Zongo, D.; Ribéreau-Gayon, R.; Masson, F.; Laborey, M.; Contrand, B.; Salmi, L.R.; Montaudon, D.; Beaudeux, J.L.; Meurin, A.; Dousset, V.; et al. S100-B protein as a screening tool for the early assessment of minor head injury. Ann. Emerg. Med. 2012, 59, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Pike, B.R.; Flint, J.; Dave, J.R.; Lu, X.C.M.; Wang, K.K.; Tortella, F.C.; Hayes, R.L. Accumulation of calpain and caspase-3 proteolytic fragments of brain-derived αII-spectrin in cerebral spinal fluid after middle cerebral artery occlusion in rats. J. Cereb. Blood Flow Metab. 2004, 24, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Vartanian, M.G.; Cordon, J.J.; Kupina, N.C.; Schielke, G.P.; Posner, A.; Raser, K.J.; Wang, K.K.W.; Taylor, C.P. Phenytoin pretreatment prevents hypoxic-ischemic brain damage in neonatal rats. Dev. Brain Res. 1996, 95, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.P.; Houle, J.; Hayes, R.L.; Wang, K.K.; Mondello, S.; Bell, M.J. Translating biomarkers research to clinical care: Applications and issues for rehabilomics. PM&R 2011, 3, S31–S38. [Google Scholar]
- Pike, B.R.; Flint, J.; Dutta, S.; Johnson, E.; Wang, K.K.; Hayes, R.L. Accumulation of non-erythroid αII-spectrin and calpain-cleaved αII-spectrin breakdown products in cerebrospinal fluid after traumatic brain injury in rats. J. Neurochem. 2001, 78, 1297–1306. [Google Scholar] [CrossRef] [PubMed]
- Yokobori, S.; Zhang, Z.; Moghieb, A.; Mondello, S.; Gajavelli, S.; Dietrich, W.D.; Bramlett, H.; Hayes, R.L.; Wang, M.; Wang, K.K.W.; et al. Acute diagnostic biomarkers for spinal cord injury: Review of the literature and preliminary research report. World Neurosurg. 2015, 83, 867–878. [Google Scholar] [CrossRef]
- Massaro, A.N.; Jeromin, A.; Kadom, N.; Vezina, G.; Hayes, R.L.; Wang, K.K.; Streeter, J.; Johnston, M.V. Serum biomarkers of MRI brain injury in neonatal hypoxic ischemic encephalopathy treated with whole-body hypothermia: A pilot study. Pediatr. Crit. Care Med. 2013, 14, 310. [Google Scholar] [CrossRef]
- Siman, R.; Giovannone, N.; Hanten, G.; Wilde, E.A.; McCauley, S.R.; Hunter, J.V.; Li, X.; Levin, H.S.; Smith, D.H. Evidence that the blood biomarker SNTF predicts brain imaging changes and persistent cognitive dysfunction in mild TBI patients. Front. Neurol. 2013, 4, 190. [Google Scholar] [CrossRef]
- Ringger, N.C.; O’steen, B.E.; Brabham, J.G.; Silver, X.; Pineda, J.; Wang, K.K.W.; Hayes, R.L.; Papa, L. A novel marker for traumatic brain injury: CSF αII-spectrin breakdown product levels. J. Neurotrauma 2004, 21, 1443–1456. [Google Scholar] [CrossRef]
- Yang, J.; Korley, F.K.; Dai, M.; Everett, A.D. Serum neurogranin measurement as a biomarker of acute traumatic brain injury. Clin. Biochem. 2015, 48, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Bhomia, M.; Balakathiresan, N.S.; Wang, K.K.; Papa, L.; Maheshwari, R.K. A panel of serum MiRNA biomarkers for the diagnosis of severe to mild traumatic brain injury in humans. Sci. Rep. 2016, 6, 28148. [Google Scholar] [CrossRef]
- Agoston, D.V.; Shutes-David, A.; Peskind, E.R. Biofluid biomarkers of traumatic brain injury. Brain Inj. 2017, 31, 1195–1203. [Google Scholar] [CrossRef] [PubMed]
- Moyron, R.B.; Gonda, A.; Selleck, M.J.; Luo-Owen, X.; Catalano, R.D.; O’Callahan, T.; Garberoglio, C.; Turay, D.; Wall, N.R. Differential protein expression in exosomal samples taken from trauma patients. Proteom. Clin. Appl. 2017, 11, 1700061. [Google Scholar] [CrossRef] [PubMed]
- Manek, R.; Moghieb, A.; Yang, Z.; Kumar, D.; Kobessiy, F.; Sarkis, G.A.; Raghavan, V.; Wang, K.K.W. Protein biomarkers and neuroproteomics characterization of microvesicles/exosomes from human cerebrospinal fluid following traumatic brain injury. Mol. Neurobiol. 2018, 55, 6112–6128. [Google Scholar] [CrossRef] [PubMed]
- Rodney, T.; Osier, N.; Gill, J. Pro-and anti-inflammatory biomarkers and traumatic brain injury outcomes: A review. Cytokine 2018, 110, 248–256. [Google Scholar] [CrossRef]
- Visser, K.; Koggel, M.; Blaauw, J.; van der Horn, H.J.; Jacobs, B.; van der Naalt, J. Blood-based biomarkers of inflammation in mild traumatic brain injury: A systematic review. Neurosci. Biobehav. Rev. 2022, 132, 154–168. [Google Scholar] [CrossRef]
- Ooi, S.Z.Y.; Spencer, R.J.; Hodgson, M.; Mehta, S.; Phillips, N.L.; Preest, G.; Manivannan, S.; Wise, M.P.; Galea, J.; Zaben, M. Interleukin-6 as a prognostic biomarker of clinical outcomes after traumatic brain injury: A systematic review. Neurosurg. Rev. 2022, 45, 3035–3054. [Google Scholar] [CrossRef]
- Xu, L.B.; Yue, J.K.; Korley, F.; Puccio, A.M.; Yuh, E.L.; Sun, X.; Rabinowitz, M.; Vassar, M.J.; Taylor, S.R.; Winkler, E.A.; et al. High-sensitivity C-reactive protein is a prognostic biomarker of six-month disability after traumatic brain injury: Results from the TRACK-TBI study. J. Neurotrauma 2021, 38, 918–927. [Google Scholar] [CrossRef]
- Monsour, M.; Ebedes, D.; Borlongan, C.V. A review of the pathology and treatment of TBI and PTSD. Exp. Neurol. 2022, 351, 114009. [Google Scholar] [CrossRef]
- Katrinli, S.; Oliveira, N.C.; Felger, J.C.; Michopoulos, V.; Smith, A.K. The role of the immune system in posttraumatic stress disorder. Transl. Psychiatry 2022, 12, 313. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, N.D.; Panenka, W.J. Antidepressants for depression after concussion and traumatic brain injury are still best practice. BMC Psychiatry 2019, 19, 100. [Google Scholar] [CrossRef] [PubMed]
- Osimo, E.F.; Baxter, L.J.; Lewis, G.; Jones, P.B.; Khandaker, G.M. Prevalence of low-grade inflammation in depression: A systematic review and meta-analysis of CRP levels. Psychol. Med. 2019, 49, 1958–1970. [Google Scholar] [CrossRef]
- Pierre, K.; Dyson, K.; Dagra, A.; Williams, E.; Porche, K.; Lucke-Wold, B. Chronic traumatic encephalopathy: Update on current clinical diagnosis and management. Biomedicines 2021, 9, 415. [Google Scholar] [CrossRef]
- Mohamed, M.S.; El Sayed, I.; Zaki, A.; Abdelmonem, S. Assessment of the effect of amantadine in patients with traumatic brain injury: A meta-analysis. J. Trauma Acute Care Surg. 2022, 92, 605–614. [Google Scholar] [CrossRef]
- McAllister, T.W.; McDonald, B.C.; Flashman, L.A.; Ferrell, R.B.; Tosteson, T.D.; Yanofsky, N.N.; Grove, M.R.; Saykin, A.J. Alpha-2 adrenergic challenge with guanfacine one month after mild traumatic brain injury: Altered working memory and BOLD response. Int. J. Psychophysiol. 2011, 82, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Fesharaki-Zadeh, A. Oxidative Stress in Traumatic Brain Injury. Int. J. Mol. Sci. 2022, 23, 13000. [Google Scholar] [CrossRef]
- Di Pietro, V.; Yakoub, K.M.; Caruso, G.; Lazzarino, G.; Signoretti, S.; Barbey, A.K.; Tavazzi, B.; Lazzarino, G.; Belli, A.; Amorini, A.M. Antioxidant Therapies in Traumatic Brain Injury. Antioxidants 2020, 9, 260. [Google Scholar] [CrossRef]
- Xiong, Y.; Mahmood, A.; Chopp, M. Animal models of traumatic brain injury. Nat. Rev. Neurosci. 2013, 14, 128–142. [Google Scholar] [CrossRef]
- Tang, S.J.; Fesharaki-Zadeh, A.; Takahashi, H.; Nies, S.H.; Smith, L.M.; Luo, A.; Chyung, A.; Chiasseu, M.; Strittmatter, S.M. Fyn kinase inhibition reduces protein aggregation, increases synapse density and improves memory in transgenic and traumatic Tauopathy. Acta Neuropathol. Commun. 2020, 8, 96. [Google Scholar] [CrossRef]
- Ojo, J.O.; Mouzon, B.; Greenberg, M.B.; Bachmeier, C.; Mullan, M.; Crawford, F. Repetitive mild traumatic brain injury augments tau pathology and glial activation in aged hTau mice. J. Neuropathol. Exp. Neurol. 2013, 72, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Weber, J.T. Experimental models of repetitive brain injuries. Prog. Brain Res. 2007, 161, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Mouzon, B.; Crynen, G.; Bachmeier, C.; Stewart, J.; Mullan, M.; Stewart, W.; Crawford, F.; Briggs, D.I.; Angoa-Pérez, M.; Kuhn, D.M.; et al. Repetitive mild traumatic brain injury in a mouse model produces learning and memory deficits accompanied by histological changes. J. Neurotrauma 2012, 29, 2761–2773. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Coats, J.S.; Mohd-Yusof, A.; Yin, Y.; Assaad, S.; Muellner, M.J.; Kamper, J.E.; Hartman, R.E.; Dulcich, M.; Donovan, V.M.; et al. Tissue vulnerability is increased following repetitive mild traumatic brain injury in the rat. Brain Res. 2013, 1499, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Petraglia, A.L.; Plog, B.A.; Dayawansa, S.; Chen, M.; Dashnaw, M.L.; Czerniecka, K.; Walker, C.T.; Viterise, T.; Hyrien, O.; Iliff, J.J.; et al. The spectrum of neurobehavioral sequelae after repetitive mild traumatic brain injury: A novel mouse model of chronic traumatic encephalopathy. J. Neurotrauma 2014, 31, 1211–1224. [Google Scholar] [CrossRef]
- Lucke-Wold, B.; Seidel, K.; Udo, R.; Omalu, B.; Ornstein, M.; Nolan, R.; Rosen, C.; Ross, J. Role of Tau Acetylation in Alzheimer’s Disease and Chronic Traumatic Encephalopathy: The Way Forward for Successful Treatment. J. Neurol. Neurosurg. 2017, 4, 140. [Google Scholar] [PubMed]
- Rubenstein, R.; Sharma, D.R.; Chang, B.; Oumata, N.; Cam, M.; Vaucelle, L.; Lindberg, M.F.; Chiu, A.; Wisniewski, T.; Wang, K.K.W.; et al. Novel mouse tauopathy model for repetitive mild traumatic brain injury: Evaluation of long-term effects on cognition and biomarker levels after therapeutic inhibition of tau phosphorylation. Front. Neurol. 2019, 10, 124. [Google Scholar] [CrossRef] [PubMed]
- Min, S.W.; Chen, X.; Tracy, T.E.; Li, Y.; Zhou, Y.; Wang, C.; Shirakawa, K.; Minami, S.S.; Defensor, E.; Mok, S.-A.; et al. Critical role of acetylation in tau-mediated neurodegeneration and cognitive deficits. Nat. Med. 2015, 21, 1154–1162. [Google Scholar] [CrossRef]
- Lagraoui, M.; Sukumar, G.; Latoche, J.R.; Maynard, S.K.; Dalgard, C.L.; Schaefer, B.C. Salsalate treatment following traumatic brain injury reduces inflammation and promotes a neuroprotective and neurogenic transcriptional response with concomitant functional recovery. Brain Behav. Immun. 2017, 61, 96–109. [Google Scholar] [CrossRef]
- Shirakawa, K.; Wang, L.; Man, N.; Maksimoska, J.; Sorum, A.W.; Lim, H.W.; Lee, I.S.; Shimazu, T.; Newman, J.C.; Schröder, S.; et al. Salicylate, diflunisal and their metabolites inhibit CBP/p300 and exhibit anticancer activity. eLife 2016, 5, e11156. [Google Scholar] [CrossRef]
- Tucker, D.; Lu, Y.; Zhang, Q. From Mitochondrial Function to Neuroprotection-an Emerging Role for Methylene Blue. Mol. Neurobiol. 2018, 55, 5137–5153. [Google Scholar] [CrossRef] [PubMed]
- Vekaria, H.J.; Talley Watts, L.; Lin, A.L.; Sullivan, P.G. Targeting mitochondrial dysfunction in CNS injury using Methylene Blue; still a magic bullet? Neurochem. Int. 2017, 109, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Talley Watts, L.; Long, J.A.; Chemello, J.; Van Koughnet, S.; Fernandez, A.; Huang, S.; Shen, Q.; Duong, T.Q.; Zhang, Y.; Chopp, M.; et al. Methylene blue is neuroprotective against mild traumatic brain injury. J. Neurotrauma 2014, 31, 1063–1071. [Google Scholar] [CrossRef] [PubMed]
- Cohen, T.J.; Guo, J.L.; Hurtado, D.E.; Kwong, L.K.; Mills, I.P.; Trojanowski, J.Q.; Lee, V.M.Y. The acetylation of tau inhibits its function and promotes pathological tau aggregation. Nat. Commun. 2011, 2, 252. [Google Scholar] [CrossRef] [PubMed]
- Rojo, A.I.; de Sagarra, M.R.; Cuadrado, A. GSK-3β down-regulates the transcription factor Nrf2 after oxidant damage: Relevance to exposure of neuronal cells to oxidative stress. J. Neurochem. 2008, 105, 192–202. [Google Scholar] [CrossRef]
- Rankin, C.A.; Sun, Q.; Gamblin, T.C. Tau phosphorylation by GSK-3β promotes tangle-like filament morphology. Mol. Neurodegener. 2007, 2, 12. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, F.; Lucas, J.J.; Avila, J. GSK3 and tau: Two convergence points in Alzheimer’s disease. J. Alzheimer’s Dis. 2013, 33, S141–S144. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.; Wang, Z.; Tchantchou, F.; Chiu, C.-T.; Zhang, Y.; Chuang, D.-M.; Guley, N.H.; Rogers, J.T.; Del Mar, N.A.; Deng, Y.; et al. Lithium ameliorates neurodegeneration, suppresses neuroinflammation, and improves behavioral performance in a mouse model of traumatic brain injury. J. Neurotrauma 2012, 29, 362–374. [Google Scholar] [CrossRef]
- Dash, P.K.; Johnson, D.; Clark, J.; Orsi, S.A.; Zhang, M.; Zhao, J.; Grill, R.J.; Moore, A.N.; Pati, S. Involvement of the glycogen synthase kinase-3 signaling pathway in TBI pathology and neurocognitive outcome. PLoS ONE 2011, 6, e24648. [Google Scholar] [CrossRef]
- Shapira, M.; Licht, A.; Milman, A.; Pick, C.G.; Shohami, E.; Eldar-Finkelman, H. Role of glycogen synthase kinase-3β in early depressive behavior induced by mild traumatic brain injury. Mol. Cell. Neurosci. 2007, 34, 571–577. [Google Scholar] [CrossRef]
- Zhu, Z.-F.; Wang, Q.-G.; Han, B.-J.; William, C.P. Neuroprotective effect and cognitive outcome of chronic lithium on traumatic brain injury in mice. Brain Res. Bull. 2010, 83, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Leeds, P.R.; Yu, F.; Wang, Z.; Chiu, C.-T.; Zhang, Y.; Leng, Y.; Linares, G.R.; Chuang, D.-M. A new avenue for lithium: Intervention in traumatic brain injury. ACS Chem. Neurosci. 2014, 5, 422–433. [Google Scholar] [CrossRef] [PubMed]
- De Rivero Vaccari, J.P.; Dietrich, W.D.; Keane, R.W. Activation and regulation of cellular inflammasomes: Gaps in our knowledge for central nervous system injury. J. Cereb. Blood Flow Metab. 2014, 34, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Bergold, P.J. Treatment of traumatic brain injury with anti-inflammatory drugs. Exp. Neurol. 2016, 275, 367–380. [Google Scholar] [CrossRef] [PubMed]
- LKelso, M.; Gendelman, H.E. Bridge between neuroimmunity and traumatic brain injury. Curr. Pharm. Des. 2014, 20, 4284–4298. [Google Scholar]
- Panikashvili, D.; Shein, N.A.; Mechoulam, R.; Trembovler, V.; Kohen, R.; Alexandrovich, A.; Shohami, E. The endocannabinoid 2-AG protects the blood–brain barrier after closed head injury and inhibits mRNA expression of proinflammatory cytokines. Neurobiol. Dis. 2006, 22, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Alderson, P.; Roberts, I. Corticosteroids for acute traumatic brain injury. Cochrane Database Syst. Rev. 2005, CD000196. [Google Scholar] [CrossRef]
- Lozano, D.; Gonzales-Portillo, G.S.; Acosta, S.; de la Pena, I.; Tajiri, N.; Kaneko, Y.; Borlongan, C.V. Neuroinflammatory responses to traumatic brain injury: Etiology, clinical consequences, and therapeutic opportunities. Neuropsychiatr. Dis. Treat. 2015, 11, 97–106. [Google Scholar]
- Woodcock, T.; Morganti-Kossmann, M.C. The role of markers of inflammation in traumatic brain injury. Front. Neurol. 2013, 4, 18. [Google Scholar] [CrossRef]
- Wu, H.; Zheng, J.; Xu, S.; Fang, Y.; Wu, Y.; Zeng, J.; Shao, A.; Shi, L.; Lu, J.; Mei, S.; et al. Mer regulates microglial/macrophage M1/M2 polarization and alleviates neuroinflammation following traumatic brain injury. J. Neuroinflamm. 2021, 18, 2. [Google Scholar] [CrossRef]
- Rodriguez-Rodriguez, A.; Jose Egea-Guerrero, J.; Murillo-Cabezas, F.; Carrillo-Vico, A. Oxidative stress in traumatic brain injury. Curr. Med. Chem. 2014, 21, 1201–1211. [Google Scholar] [CrossRef] [PubMed]
- Gensel, J.C.; Zhang, B. Macrophage activation and its role in repair and pathology after spinal cord injury. Brain Res. 2015, 1619, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Loane, D.J.; Stoica, B.A.; Faden, A.I. Neuroprotection for traumatic brain injury. Handb. Clin. Neurol. 2015, 127, 343–366. [Google Scholar] [PubMed]
- Pozdnyakov, D.I.; Miroshnichenko, K.A.; Voronkov, A.V.; Kovaleva, T.G. The administration of the new pyrimidine derivative—4-{2-[2-(3, 4-Dimethoxyphenyl)-Vinyl]-6-Ethyl-4-Oxo-5-Phenyl-4H-pyrimidine-1-Il} benzsulfamide restores the activity of brain cells in experimental chronic traumatic encephalopathy by maintaining mitochondrial function. Medicina 2019, 55, 386. [Google Scholar] [PubMed]
- Logsdon, A.F.; Lucke-Wold, B.P.; Nguyen, L.; Matsumoto, R.R.; Turner, R.C.; Rosen, C.L.; Huber, J.D. Salubrinal reduces oxidative stress, neuroinflammation and impulsive-like behavior in a rodent model of traumatic brain injury. Brain Res. 2016, 1643, 140–151. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, Y.; Nham, A.; Sherbaf, A.; Quach, D.; Yahya, E.; Ranburger, D.; Bi, X.; Baudry, M. Calpain-2 as a therapeutic target in repeated concussion–induced neuropathy and behavioral impairment. Sci. Adv. 2020, 6, eaba5547. [Google Scholar] [CrossRef]
- Roberts, I.; Yates, D.; Sandercock, P.; Farrell, B.; Wasserberg, J.; Lomas, G.; Cottingham, R.; Svoboda, P.; Brayley, N.; Mazairac, G.; et al. Effect of intravenous corticosteroids on death within 14 days in 10,008 adults with clinically significant head injury (MRC CRASH trial): Randomised placebo-controlled trial. Lancet 2004, 364, 1321–1328. [Google Scholar] [CrossRef]
- Hein, A.M.; O’Banion, M.K. Neuroinflammation and memory: The role of prostaglandins. Mol. Neurobiol. 2009, 40, 15–32. [Google Scholar] [CrossRef]
- Shohami, E.; Gallily, R.; Mechoulam, R.; Bass, R.; Ben-Hur, T. Cytokine production in the brain following closed head injury: Dexanabinol (HU-211) is a novel TNF-α inhibitor and an effective neuroprotectant. J. Neuroimmunol. 1997, 72, 169–177. [Google Scholar] [CrossRef]
- Chio, C.-C.; Chang, C.H.; Wang, C.C.; Cheong, C.U.; Chao, C.M.; Cheng, B.C.; Yang, C.-Z.; Chang, C.-P. Etanercept attenuates traumatic brain injury in rats by reducing early microglial expression of tumor necrosis factor-α. BMC Neurosci. 2013, 14, 33. [Google Scholar] [CrossRef]
- Finnie, J. Neuroinflammation: Beneficial and detrimental effects after traumatic brain injury. Inflammopharmacology 2013, 21, 309–320. [Google Scholar] [CrossRef] [PubMed]
- Anderson, G.D.; Peterson, T.C.; Haar, C.V.; Kantor, E.D.; Farin, F.M.; Bammler, T.K.; MacDonald, J.W.; Hoane, M.R. Comparison of the effects of erythropoietin and anakinra on functional recovery and gene expression in a traumatic brain injury model. Front. Pharmacol. 2013, 4, 129. [Google Scholar] [CrossRef] [PubMed]
- Atkins, C.; Kang, Y.; Furones, C.; Truettner, J.; Alonso, O.; Dietrich, W. Postinjury treatment with rolipram increases hemorrhage after traumatic brain injury. J. Neurosci. Res. 2012, 90, 1861–1871. [Google Scholar] [CrossRef] [PubMed]
- Garrido-Mesa, N.; Zarzuelo, A.; Galvez, J. What is behind the non-antibiotic properties of minocycline? Pharmacol. Res. 2013, 67, 18–30. [Google Scholar] [CrossRef]
- Adembri, C.; Selmi, V.; Vitali, L.; Tani, A.; Margheri, M.; Loriga, B.; Carlucci, M.; Nosi, D.; Formigli, L.; De Gaudio, A.R. Minocycline but not tigecycline is neuroprotective and reduces the neuroinflammatory response induced by the superimposition of sepsis upon traumatic brain injury. Crit. Care Med. 2014, 42, e570–e582. [Google Scholar] [CrossRef]
- Haber, M.; Baki, S.G.A.; Grin’Kina, N.M.; Irizarry, R.; Ershova, A.; Orsi, S.; Grill, R.J.; Dash, P.; Bergold, P.J. Minocycline plus N-acetylcysteine synergize to modulate inflammation and prevent cognitive and memory deficits in a rat model of mild traumatic brain injury. Exp. Neurol. 2013, 249, 169–177. [Google Scholar] [CrossRef]
- Homsi, S.; Piaggio, T.; Croci, N.; Noble, F.; Plotkine, M.; Marchand-Leroux, C.; Jafarian-Tehrani, M. Blockade of acute microglial activation by minocycline promotes neuroprotection and reduces locomotor hyperactivity after closed head injury in mice: A twelve-week follow-up study. J. Neurotrauma 2010, 27, 911–921. [Google Scholar] [CrossRef]
- Wright, D.W.; Yeatts, S.D.; Silbergleit, R.; Palesch, Y.Y.; Hertzberg, V.S.; Frankel, M.; Goldstein, F.C.; Caveney, A.F.; Howlett-Smith, H.; Bengelink, E.M.; et al. Very early administration of progesterone for acute traumatic brain injury. N. Engl. J. Med. 2014, 371, 2457–2466. [Google Scholar] [CrossRef]
- Radosevich, J.J.; Patanwala, A.E.; Erstad, B.L. Emerging pharmacological agents to improve survival from traumatic brain injury. Brain Inj. 2013, 27, 1492–1499. [Google Scholar] [CrossRef]
- Bian, X.-X.; Yuan, X.-S.; Qi, C.-P. Effect of recombinant human erythropoietin on serum S100B protein and interleukin-6 levels after traumatic brain injury in the rat. Neurol. Med. Chir. 2010, 50, 361–366. [Google Scholar] [CrossRef]
- Hellewell, S.C.; Yan, E.B.; Alwis, D.S.; Bye, N.; Morganti-Kossmann, M.C. Erythropoietin improves motor and cognitive deficit, axonal pathology, and neuroinflammation in a combined model of diffuse traumatic brain injury and hypoxia, in association with upregulation of the erythropoietin receptor. J. Neuroinflamm. 2013, 10, 926. [Google Scholar] [CrossRef] [PubMed]
- Robertson, C.S.; Hannay, H.J.; Yamal, J.-M.; Gopinath, S.; Goodman, J.C.; Tilley, B.C.; Baldwin, A.; Lara, L.R.; Saucedo-Crespo, H.; Ahmed, O.; et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: A randomized clinical trial. JAMA 2014, 312, 36–47. [Google Scholar] [CrossRef] [PubMed]
- Talving, P.; Lustenberger, T.; Inaba, K.; Lam, L.; Mohseni, S.; Chan, L.; Demetriades, D. Erythropoiesis-stimulating agent administration and survival after severe traumatic brain injury: A prospective study. Arch. Surg. 2012, 147, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Helmy, A.; Guilfoyle, M.R.; Carpenter, K.L.; Pickard, J.D.; Menon, D.K.; Hutchinson, P.J. Recombinant human interleukin-1 receptor antagonist in severe traumatic brain injury: A phase II randomized control trial. J. Cereb. Blood Flow Metab. 2014, 34, 845–851. [Google Scholar] [CrossRef]
- Schneider, E.B.; Efron, D.T.; MacKenzie, E.J.; Rivara, F.P.; Nathens, A.B.; Jurkovich, G.J. Premorbid statin use is associated with improved survival and functional outcomes in older head-injured individuals. J. Trauma 2011, 71, 815–819. [Google Scholar] [CrossRef]
- Sacramento, C.B.; Sondhi, D.; Rosenberg, J.B.; Chen, A.; Giordano, S.; Pey, E.; Lee, V.; Stiles, K.M.; Havlicek, D.F.; Leopold, P.L.; et al. Anti-phospho-tau gene therapy for chronic traumatic encephalopathy. Hum. Gene Ther. 2020, 31, 57–69. [Google Scholar] [CrossRef]
- Nobuhara, C.K.; DeVos, S.L.; Commins, C.; Wegmann, S.; Moore, B.D.; Roe, A.D.; Costantino, I.; Frosch, M.P.; Pitstick, R.; Carlson, G.A.; et al. Tau antibody targeting pathological species blocks neuronal uptake and interneuron propagation of tau in vitro. Am. J. Pathol. 2017, 187, 1399–1412. [Google Scholar] [CrossRef]
- Kondo, A.; Shahpasand, K.; Mannix, R.; Qiu, J.; Moncaster, J.; Chen, C.-H.; Yao, Y.; Lin, Y.-M.; Driver, J.A.; Sun, Y.; et al. Antibody against early driver of neurodegeneration cis P-tau blocks brain injury and tauopathy. Nature 2015, 523, 431–436. [Google Scholar] [CrossRef]
- Lu, K.P.; Kondo, A.; Albayram, O.; Herbert, M.K.; Liu, H.; Zhou, X.Z. Potential of the antibody against cis–phosphorylated tau in the early diagnosis, treatment, and prevention of Alzheimer disease and brain injury. JAMA Neurol. 2016, 73, 1356–1362. [Google Scholar] [CrossRef]
- Houck, A.; Kondo, A.; Lu, K.P. Cis p-tau directly links traumatic brain injury with chronic traumatic encephalopathy and Alzheimer’s disease, but can be blocked by antibody (P5. 221). AAN Enterp. 2017, 88. [Google Scholar]
- Willis, E.F.; MacDonald, K.P.; Nguyen, Q.H.; Garrido, A.L.; Gillespie, E.R.; Harley, S.B.; Bartlett, P.F.; Schroder, W.A.; Yates, A.G.; Anthony, D.C.; et al. Repopulating microglia promote brain repair in an IL-6-dependent manner. Cell 2020, 180, 833–846.e16. [Google Scholar] [CrossRef] [PubMed]
- Shaito, A.; Hasan, H.; Habashy, K.J.; Fakih, W.; Abdelhady, S.; Ahmad, F.; Zibara, K.; Eid, A.H.; El-Yazbi, A.F.; Kobeissy, F.H. Western diet aggravates neuronal insult in post-traumatic brain injury: Proposed pathways for interplay. EBioMedicine 2020, 57, 102829. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, J.C.; Killcross, A.S.; Jenkins, T.A. Obesity and cognitive decline: Role of inflammation and vascular changes. Front. Neurosci. 2014, 8, 375. [Google Scholar] [CrossRef] [PubMed]
- Posey, K.A.; Hasan, H.; Habashy, K.J.; Fakih, W.; Abdelhady, S.; Ahmad, F.; Zibara, K.; Eid, A.H.; El-Yazbi, A.F.; Kobeissy, F.H. Hypothalamic proinflammatory lipid accumulation, inflammation, and insulin resistance in rats fed a high-fat diet. Am. J. Physiol. Endocrinol. Metab. 2009, 296, E1003–E1012. [Google Scholar] [CrossRef]
- Gemma, C.; Bickford, P.C. Interleukin-1ß and Caspase-1: Players in the regulation of age-related cognitive dysfunction. Rev. Neurosci. 2007, 18, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Sherman, M.; Liu, M.-M.; Birnbaum, S.; Wolf, S.E.; Minei, J.P.; Gatson, J.W. Adult obese mice suffer from chronic secondary brain injury after mild TBI. J. Neuroinflamm. 2016, 13, 171. [Google Scholar] [CrossRef]
- Avena, N.M.; Gold, M.S. Food and addiction–sugars, fats and hedonic overeating. Addiction 2011, 106, 1214–1215. [Google Scholar] [CrossRef]
- Zilberter, T.; Zilberter, Y. Ketogenic ratio determines metabolic effects of macronutrients and prevents interpretive bias. Front. Nutr. 2018, 5, 75. [Google Scholar] [CrossRef]
- Gasior, M.; Rogawski, M.A.; Hartman, A.L. Neuroprotective and disease-modifying effects of the ketogenic diet. Behav. Pharmacol. 2006, 17, 431. [Google Scholar] [CrossRef]
- Murphy, P.; Likhodii, S.; Nylen, K.; Burnham, W. The antidepressant properties of the ketogenic diet. Biol. Psychiatry 2004, 56, 981–983. [Google Scholar] [CrossRef]
- Krikorian, R.; Shidler, M.D.; Dangelo, K.; Couch, S.C.; Benoit, S.C.; Clegg, D.J. Dietary ketosis enhances memory in mild cognitive impairment. Neurobiol. Aging 2012, 33, 425.e19–425.e27. [Google Scholar] [CrossRef] [PubMed]
- White, H.; Venkatesh, B. Clinical review: Ketones and brain injury. Critical Care 2011, 15, 219. [Google Scholar] [CrossRef] [PubMed]
- Anastasiou, C.A.; Yannakoulia, M.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Arampatzi, X.; Bougea, A.; Labropoulos, I.; Scarmeas, N. Mediterranean diet and cognitive health: Initial results from the Hellenic Longitudinal Investigation of Ageing and Diet. PLoS ONE 2017, 12, e0182048. [Google Scholar] [CrossRef] [PubMed]
- McGrattan, A.M.; McGuinness, B.; McKinley, M.C.; Kee, F.; Passmore, P.; Woodside, J.V.; McEvoy, C.T. Diet and inflammation in cognitive ageing and Alzheimer’s disease. Curr. Nutr. Rep. 2019, 8, 53–65. [Google Scholar] [CrossRef] [PubMed]
- Ritter, A.; Shan, G.; Montes, A.; Randall, R.; Bernick, C. Traumatic encephalopathy syndrome: Application of new criteria to a cohort exposed to repetitive head impacts. Br. J. Sports Med. 2023, 57, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Ruprecht, R.; Scheurer, E.; Lenz, C. Systematic review on the characterization of chronic traumatic encephalopathy by MRI and MRS. J. Magn. Reson. Imaging 2019, 49, 212–228. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, L.E.; McKee, A.C.; Stanton, P.K. Considerations for animal models of blast-related traumatic brain injury and chronic traumatic encephalopathy. Alzheimer’s Res. Ther. 2014, 6, 64. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, N.D.; Cammack, K.M. Chronic Traumatic Encephalopathy: A Review of Clinical Diagnosis, Animal Models, Sex Differences, and A Revised Return-to-Play Protocol. Impulse 2017, 1–16. [Google Scholar]
- Risling, M.; Smith, D.; Stein, T.D.; Thelin, E.P.; Zanier, E.R.; Ankarcrona, M.; Nilsson, P. Modelling human pathology of traumatic brain injury in animal models. J. Intern. Med. 2019, 285, 594–607. [Google Scholar] [CrossRef]
- Fesharaki-Zadeh, A.; Miyauchi, J.T.; St Laurent-Arriot, K.; Tsirka, S.E.; Bergold, P.J. Increased Behavioral Deficits and Inflammation in a Mouse Model of Co-Morbid Traumatic Brain Injury and Post-Traumatic Stress Disorder. ASN Neuro 2020, 12, 1759091420979567. [Google Scholar] [CrossRef]
- Breen, P.W.; Krishnan, V. Recent preclinical insights into the treatment of chronic traumatic encephalopathy. Front. Neurosci. 2020, 14, 616. [Google Scholar] [CrossRef] [PubMed]
- Lindsley, C.W. Chronic traumatic encephalopathy (CTE): A brief historical overview and recent focus on NFL players. ACS Chem. Neurosci. 2017, 8, 1629–1631. [Google Scholar] [CrossRef] [PubMed]
- Fesharaki-Zadeh, A. Chronic traumatic encephalopathy: A brief overview. Front. Neurol. 2019, 10, 713. [Google Scholar] [CrossRef] [PubMed]
- Nylen, K.; Öst, M.; Csajbok, L.; Nilsson, I.; Blennow, K.; Nellgård, B.; Rosengren, L. Increased serum-GFAP in patients with severe traumatic brain injury is related to outcome. J. Neurol. Sci. 2006, 240, 85–91. [Google Scholar] [CrossRef]
- Shahim, P.; Gren, M.; Liman, V.; Andreasson, U.; Norgren, N.; Tegner, Y.; Mattsson, N.; Andreasen, N.; Öst, M.; Zetterberg, H.; et al. Serum neurofilament light protein predicts clinical outcome in traumatic brain injury. Sci. Rep. 2016, 6, 36791. [Google Scholar] [CrossRef]
- Abbasi, M.; Sajjadi, M.; Fathi, M.; Maghsoudi, M. Serum S100B protein as an outcome prediction tool in emergency department patients with traumatic brain injury. Turk. J. Emerg. Med. 2014, 14, 147–152. [Google Scholar] [CrossRef]
- Bazarian, J.J.; Zemlan, F.P.; Mookerjee, S.; Stigbrand, T. Serum S-100B and cleaved-tau are poor predictors of long-term outcome after mild traumatic brain injury. Brain Inj. 2006, 20, 759–765. [Google Scholar] [CrossRef]
- Skolnick, B.E.; Maas, A.I.; Narayan, R.K.; van der Hoop, R.G.; MacAllister, T.; Ward, J.D.; Nelson, N.R.; Stocchetti, N. A clinical trial of progesterone for severe traumatic brain injury. N. Engl. J. Med. 2014, 371, 2467–2476. [Google Scholar] [CrossRef]

| Serum Biomarker | TBI Outcomes |
|---|---|
| GFAP | Clinical TBI studies have reported longitudinal elevation in GFAP levels [21]. GFAP was also recently approved by the FDA as a TBI outcome clinical measure [22]. |
| NfL | Clinical TBI studies have reported elevated NfL serum levels both acutely and longitudinally [21]. |
| Tau (total) | Total tau elevation has been reported both acutely and chronically in TBI populations [21]. |
| NSE | NSE elevated levels have been reported in both mild and more severe TBI populations [23,24]. |
| UCHL-1 | UCHL-1 has been shown to be robustly elevated in both mTBI and more severe TBI patients [25]. UCHL-1 was recently FDA-approved as a TBI outcome clinical measure [22]. |
| S100B | S100B has been reported to be more acutely elevated in various TBI severity cases [26,27]. |
| SBDP | SBDPs are products of calpain and caspase-3 post-TBI and have been reported to be elevated in both preclinical and clinical studies [28,29]. |
| MBP | MBP is an oligodendrocyte protein and a product of proteases, including calpain, and is reported to be elevated in severe TBI patients [30,31]. |
| MAP-2 | An emerging biomarker for TBI patients [32]. |
| BDNF | Mainly reported in the preclinical TBI studies, with potential application to the clinical TBI population [33]. |
| microRNA | A class of small endogenous RNA molecules that have been reported to be elevated in biofluid (CSF, serum, or plasma) in several rodent models of TBI of various severities [34]. |
| MV/E | Lipid-bilayered, encapsulated particles (10–100 nm in diameter) that are released from cells into the CSF and blood during TBI [35]. Reported elevated MV/E released into CSF in TBI patients [36]. |
| Pro-inflammatory cytokines (IL-6, IL-1, IL-8, IL-10, TNFα, CRP) | Pro-inflammatory markers, especially Il-6 and CRP, have been shown to have robust diagnostic and prognostic value [20]. |
| TBI Pharmacological Regimen | Proposed Mechanism |
|---|---|
| Cholinesterase Inhibitors | Cholinesterase inhibitors, including galantamine, donepezil, and rivastigmine, have been repurposed for TBI patients [84]. |
| NMDA receptor antagonists | NMDA receptor antagonist, amantadine, has been shown to improve cognition in moderate to severe TBI patients [85]. |
| SSRIs | Selective serotonin reuptake inhibitors (SSRIs) like sertraline and escitalopram have been utilized to mange behavioral symptoms in TBI patients [82]. |
| Guanfacine | Guanfacine has been reported to improve working memory deficits in mild TBI patients [86]. |
| Nutraceuticals | A number of nutraceuticals have been utilized in the treatment of TBI in preclinical and clinical studies, including N-acetylcysteine (NAC), flavonoids, resveratrol, alpha-tocopherol (vitamin E), coenzyme Q10 [87]. |
| NSAIDs | COX-2 selective drugs like carprofen, celecoxib, meloxicam, nimesulide, and rofecoxib have undergone testing in various preclinical TBI models with no significant degree of established efficacy [114]. |
| Glucocorticoids | Despite several promising preclinical studies, clinical trials have resulted in limited success, likely due to a narrow therapeutic window [127]. |
| Phosphodiesterase Inhibitors | Phophodiesterase inhibitors have been utilized mostly in preclinical studies and have not been systematically studied in a clinical trial setting [133]. |
| Minocycline | In prior preclinical studies, minocycline given between 5 min and 1 h after injury improved performance on a variety of neurobehavioral tests [136]. |
| Progesterone | A large, multi-center Phase III PROtect III trial, as well as a second larger-scale trial (SYNAPSE), examined progesterone and did not establish clinical efficacy [178]. |
| Erythropoietin | Despite preclinical studies’ success, the evidence for the use of erythropoietin has not reached the threshold for its use in a phase III trial [126]. |
| Anakinra | A small phase II randomized controlled clinical trial reported anti-inflammatory benefits in an Anakinra-treated group; the study size was too small to establish efficacy but provided an intriguing potential future approach [144]. |
| Tau phosphorylation targets | The studies focusing on tau-phosphorylation targets have been mostly preclinical, with possible future clinical applications [90]. |
| Tau acetylation targets | Tau acetylation inhibitors, including salsalate and methylene blue, as well as histone deacetylase 6 and sirtuins, have largely been examined in the preclinical setting [104]. |
| Immunotherapy | Specific antibodies targeting the pathogenic cis-P-tau post-TBI have been reported to lead to improved structural and functional outcomes [148] but have yet to be examined in larger clinical trial settings. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fesharaki-Zadeh, A. Navigating the Complexities of Traumatic Encephalopathy Syndrome (TES): Current State and Future Challenges. Biomedicines 2023, 11, 3158. https://doi.org/10.3390/biomedicines11123158
Fesharaki-Zadeh A. Navigating the Complexities of Traumatic Encephalopathy Syndrome (TES): Current State and Future Challenges. Biomedicines. 2023; 11(12):3158. https://doi.org/10.3390/biomedicines11123158
Chicago/Turabian StyleFesharaki-Zadeh, Arman. 2023. "Navigating the Complexities of Traumatic Encephalopathy Syndrome (TES): Current State and Future Challenges" Biomedicines 11, no. 12: 3158. https://doi.org/10.3390/biomedicines11123158
APA StyleFesharaki-Zadeh, A. (2023). Navigating the Complexities of Traumatic Encephalopathy Syndrome (TES): Current State and Future Challenges. Biomedicines, 11(12), 3158. https://doi.org/10.3390/biomedicines11123158






