Biomechanical Behaviors and Degradation Properties of Multilayered Polymer Scaffolds: The Phase Space Method for Bile Duct Design and Bioengineering
Abstract
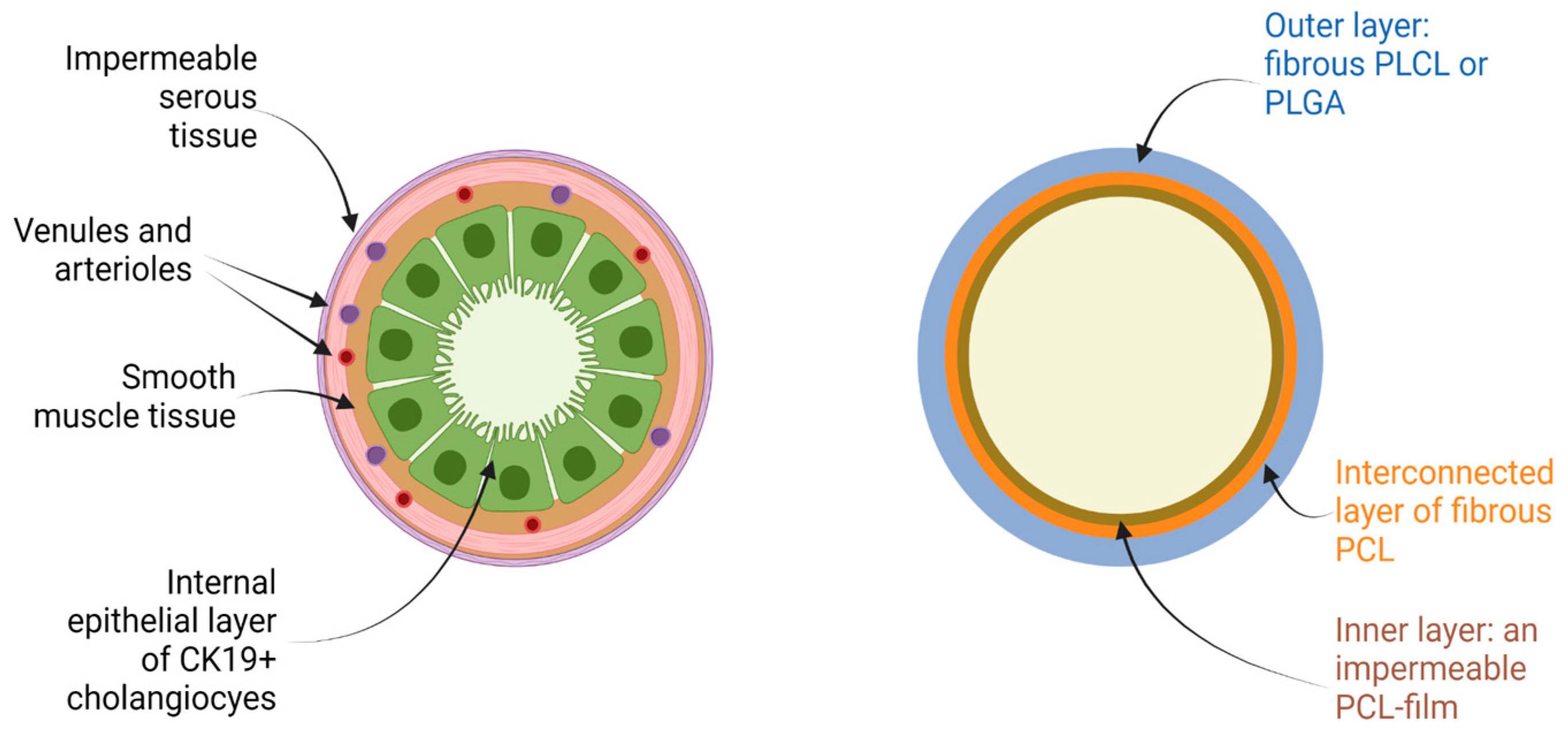
:1. Introduction
2. Materials and Methods
2.1. Polymeric Materials
2.2. Fabrication of Flat Scaffold Samples
2.3. Electrospinning of Tubular Multi-Layered Scaffolds
2.4. Degradation of Flat Polymeric Scaffolds
2.5. Decellularization of a Native Bile Duct
2.6. Mechanical Properties of Native and Decellularized Bile Duct and Synthetic Tubular Scaffolds
2.7. Scanning Electron Microscopy of Flat Polymeric Scaffolds
2.8. Differential Scanning Calorimetry
2.9. Cytocompatibility Evaluation
2.10. Statistics
3. Results
3.1. Mechanical Properties of Native and Decellularized Bile Duct
3.2. Mass Loss of Flat Polymeric Scaffolds during Degradation
3.3. Changes in Fibrous Morphology of Flat Scaffolds during Degradation
3.4. Variation of Molecular Mass Characteristics of Flat Polymeric Scaffolds
3.5. Changes in the Mechanical Properties of Flat Scaffolds during Degradation
3.6. Cytocompatibility Evaluation
3.7. Biomechanical Behavior of Tubular Synthetic Scaffolds
4. Discussion
5. Challenges and Perspectives
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, X.; Yu, W.L.; Fu, X.H.; Zhu, B.; Zhao, T.; Zhang, Y.J. Early versus delayed surgical repair and referral for patients with bile duct injury: A systematic review and meta-analysis. Ann. Surg. 2020, 271, 449–459. [Google Scholar] [CrossRef]
- Fletcher, R.; Cortina, C.S.; Kornfield, H.; Varelas, A.; Li, R.; Veenstra, B.; Bonomo, S. Bile duct injuries: A contemporary survey of surgeon attitudes and experiences. Surg. Endosc. 2020, 34, 3079–3084. [Google Scholar] [CrossRef]
- Sun, Q.; Shen, Z.; Liang, X.; He, Y.; Kong, D.; Midgley, A.C.; Wang, K. Progress and Current Limitations of Materials for Artificial Bile Duct Engineering. Materials 2021, 14, 7468. [Google Scholar] [CrossRef]
- Sandru, V.; Stan-Ilie, M.; Plotogea, O.-M.; Vladut, C.; Ungureanu, B.S.; Balan, G.G.; Gheonea, D.I.; Constantinescu, G. Endoscopic Management of Biliary Strictures after Orthotopic Liver Transplantation: A Single Center Experience Study. Diagnostics 2022, 12, 1221. [Google Scholar] [CrossRef] [PubMed]
- Sandha, J.; van Zanten, S.V.; Sandha, G. The safety and efficacy of single-operator cholangioscopy in the treatment of difficult common bile duct stones after failed conventional ERCP. J. Can. Assoc. Gastroenterol. 2018, 1, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Lyundup, A.V.; Demchenko, A.G.; Tenchurin, T.H.; Krasheninnikov, M.E.; Klabukov, I.D.; Shepelev, A.D.; Mamagulashvili, V.G.; Oganesyan, R.V.; Orehov, A.S.; Chvalun, S.N.; et al. Improving the seeding effectiveness of stromal and epithelial cell cultures in biodegradable matrixes by dynamic cultivation. Genes Cells 2016, 11, 102–107. [Google Scholar]
- Gil, C.J.; Li, L.; Hwang, B.; Cadena, M.; Theus, A.S.; Finamore, T.A.; Bauser-Heaton, H.; Mahmoudi, M.; Roeder, R.K.; Serpooshan, V. Tissue engineered drug delivery vehicles: Methods to monitor and regulate the release behavior. J. Control. Release 2022, 349, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Schröder, H.C.; Wang, X.; Neufurth, M.; Wang, S.; Tan, R.; Müller, W.E. Inorganic Polymeric Materials for Injured Tissue Repair: Biocatalytic Formation and Exploitation. Biomedicines 2022, 10, 658. [Google Scholar] [CrossRef]
- Singh, G.; Chanda, A. Mechanical properties of whole-body soft human tissues: A review. Biomed. Mater. 2021, 16, 062004. [Google Scholar] [CrossRef]
- Kim, Y.; Son, K.H.; Lee, J.W. Auxetic structures for tissue engineering scaffolds and biomedical devices. Materials 2021, 14, 6821. [Google Scholar] [CrossRef] [PubMed]
- Girard, E.; Chagnon, G.; Gremen, E.; Calvez, M.; Masri, C.; Boutonnat, J.; Trilling, B.; Nottelet, B. Biomechanical behaviour of human bile duct wall and impact of cadaveric preservation processes. J. Mech. Behav. Biomed. Mater. 2019, 98, 291–300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grolich, T.; Crha, M.; Novotný, L.; Kala, Z.; Hep, A.; Nečas, A.; Hlavsa, J.; Mitáš, L.; Misík, J. Self-expandable biodegradable biliary stents in porcine model. J. Surg. Res. 2015, 193, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Miyazawa, M.; Aikawa, M.; Okada, K.; Toshimitsu, Y.; Okamoto, K.; Koyama, I.; Ikada, Y. Regeneration of extrahepatic bile ducts by tissue engineering with a bioabsorbable polymer. J. Artif. Organs 2012, 15, 26–31. [Google Scholar] [CrossRef]
- Laukkarinen, J.M.; Sand, J.A.; Chow, P.; Juuti, H.; Kellomäki, M.; Kärkkäinen, P.; Isola, J.; Yu, S.; Somanesan, S.; Kee, I.; et al. A novel biodegradable biliary stent in the normal duct hepaticojejunal anastomosis: An 18-month follow-up in a large animal model. J. Gastrointest. Surg. 2007, 11, 750–757. [Google Scholar] [CrossRef]
- Yamamoto, K.; Yoshioka, T.; Furuichi, K.; Sakaguchi, H.; Anai, H.; Tanaka, T.; Morimoto, K.; Uchida, H.; Kichikawa, K. Experimental study of poly-L-lactic acid biodegradable stents in normal canine bile ducts. Cardiovasc. Interv. Radiol. 2011, 34, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Zong, C.; Wang, M.; Yang, F.; Chen, G.; Chen, J.; Tang, Z.; Liu, Q.; Gao, C.; Ma, L.; Wang, J. A novel therapy strategy for bile duct repair using tissue engineering technique: PCL/PLGA bilayered scaffold with hMSCs. J. Tissue Eng. Regen. Med. 2017, 11, 966–976. [Google Scholar] [CrossRef]
- Kahaleh, M.; Brijbassie, A.; Sethi, A.; Degaetani, M.; Poneros, J.M.; Loren, D.E.; Kowalski, T.E.; Sejpal, D.V.; Patel, S.; Rosenkranz, L.; et al. Multicenter trial evaluating the use of covered self-expanding metal stents in benign biliary strictures: Time to revisit our therapeutic options? J. Clin. Gastroenterol. 2013, 47, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Saxena, P.; Diehl, D.L.; Kumbhari, V.; Shieh, F.; Buscaglia, J.M.; Sze, W.; Kapoor, S.; Komanduri, S.; Nasr, J.; Shin, E.J.; et al. A US Multicenter Study of Safety and Efficacy of Fully Covered Self-Expandable Metallic Stents in Benign Extrahepatic Biliary Strictures. Dig. Dis. Sci. 2015, 60, 3442–3448. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, A.; Pickartz, T.; Lerch, M.M.; Fanelli, F.; Fiocca, F.; Lucatelli, P.; Cereatti, F.; Hoffmeister, A.; van Steenbergen, W.; Kraft, M.; et al. Effective treatment of benign biliary strictures with a removable, fully covered, self-expandable metal stent: A prospective, multicenter European study. United Eur. Gastroenterol. J. 2017, 5, 398–407. [Google Scholar] [CrossRef]
- Apalakis, A. An experimental evaluation of the types of material used for bile duct drainage tubes. Br. J. Surg. 1976, 63, 440–445. [Google Scholar] [CrossRef]
- Schanaider, A.; Pannain, V.L.N.; Müller, L.C.C.M.; Maya, M.C.A. Expanded polytetrafluoroethylene in canine bile duct injury: A critical analysis. Acta Cir. Bras. 2011, 26, 247–252. [Google Scholar] [CrossRef] [Green Version]
- Yan, J.; Liu, X.; Liu, J.; Zhang, X.; Zheng, Q.; Nan, J.; Lin, M.; Pan, H.; Wang, Y.; Cai, X.; et al. A dual-layer cell-laden tubular scaffold for bile duct regeneration. Mater. Des. 2021, 212, 110229. [Google Scholar] [CrossRef]
- Malikmammadov, E.; Tanir, T.E.; Kiziltay, A.; Hasirci, V.; Hasirci, N. PCL and PCL-based materials in biomedical applications. J. Biomater. Sci. Polym. Ed. 2018, 29, 863–893. [Google Scholar] [CrossRef] [PubMed]
- Doyle, S.E.; Henry, L.; McGennisken, E.; Onofrillo, C.; Bella, C.D.; Duchi, S.; O’Connell, C.D.; Pirogova, E. Characterization of Polycaprolactone Nanohydroxyapatite Composites with Tunable Degradability Suitable for Indirect Printing. Polymers 2021, 13, 295. [Google Scholar] [CrossRef]
- Siddiqui, N.; Asawa, S.; Birru, B.; Baadhe, R.; Rao, S. PCL-based composite scaffold matrices for tissue engineering applications. Mol. Biotechnol. 2018, 60, 506–532. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Du, Y.; Yang, G.; Hu, X.; Wang, L.; Liu, B.; Wang, J.; Zhang, S. Delivering proangiogenic factors from 3D-printed polycaprolactone scaffolds for vascularized bone regeneration. Adv. Healthc. Mater. 2020, 9, 2000727. [Google Scholar] [CrossRef]
- Kundu, J.; Shim, J.H.; Jang, J.; Kim, S.W.; Cho, D.W. An additive manufacturing-based PCL–alginate–chondrocyte bioprinted scaffold for cartilage tissue engineering. J. Tissue Eng. Regen. Med. 2015, 9, 1286–1297. [Google Scholar] [CrossRef] [PubMed]
- Mousavi Nejad, Z.; Zamanian, A.; Saeidifar, M.; Vanaei, H.R.; Salar Amoli, M. 3D bioprinting of polycaprolactone-based scaffolds for pulp-dentin regeneration: Investigation of physicochemical and biological behavior. Polymers 2021, 13, 4442. [Google Scholar] [CrossRef]
- Levengood, S.L.; Erickson, A.E.; Chang, F.C.; Zhang, M. Chitosan–poly (caprolactone) nanofibers for skin repair. J. Mater. Chem. B 2017, 5, 1822–1833. [Google Scholar] [CrossRef] [Green Version]
- Jana, S.; Bhagia, A.; Lerman, A. Optimization of polycaprolactone fibrous scaffold for heart valve tissue engineering. Biomed. Mater. 2019, 14, 065014. [Google Scholar] [CrossRef]
- Yari, A.; Teimourian, S.; Amidi, F.; Bakhtiyari, M.; Heidari, F.; Sajedi, N.; Veijouye, S.J.; Dodel, M.; Nobakht, M. The role of biodegradable engineered random polycaprolactone nanofiber scaffolds seeded with nestin-positive hair follicle stem cells for tissue engineering. Adv. Biomed. Res. 2016, 5, 22. [Google Scholar] [CrossRef]
- Li, J.; Tao, R.; Wu, W.; Cao, H.; Xin, J.; Li, J.; Guo, J.; Jiang, L.; Gao, C.; Demetriou, A.A.; et al. 3D PLGA scaffolds improve differentiation and function of bone marrow mesenchymal stem cell–derived hepatocytes. Stem Cells Dev. 2010, 19, 1427–1436. [Google Scholar] [CrossRef] [PubMed]
- Patrick Jr, C.W.; Chauvin, P.B.; Hobley, J.; Reece, G.P. Preadipocyte seeded PLGA scaffolds for adipose tissue engineering. Tissue Eng. 1999, 5, 139–151. [Google Scholar] [CrossRef]
- Xiong, Y.; Zeng, Y.S.; Zeng, C.G.; Du, B.L.; He, L.M.; Quan, D.P.; Zhang, W.; Wang, J.M.; Wu, J.L.; Li, Y.; et al. Synaptic transmission of neural stem cells seeded in 3-dimensional PLGA scaffolds. Biomaterials 2009, 30, 3711–3722. [Google Scholar] [CrossRef] [PubMed]
- Bar, J.K.; Kowalczyk, T.; Grelewski, P.G.; Stamnitz, S.; Paprocka, M.; Lis, J.; Lis-Nawara, A.; An, S.; Klimczak, A. Characterization of Biological Properties of Dental Pulp Stem Cells Grown on an Electrospun Poly (l-lactide-co-caprolactone) Scaffold. Materials 2022, 15, 1900. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.Y.; Hollister, S.J.; Krebsbach, P.H.; Nosrat, C. Poly (ϵ-Caprolactone) and Poly (L-Lactic-Co-Glycolic Acid) Degradable Polymer Sponges Attenuate Astrocyte Response and Lesion Growth in Acute Traumatic Brain Injury. Tissue Eng. 2007, 13, 2515–2523. [Google Scholar] [CrossRef] [Green Version]
- Duffy, P.; McMahon, S.; Wang, X.; Keaveney, S.; O’Cearbhaill, E.D.; Quintana, I.; Rodríguez, F.J.; Wang, W. Synthetic bioresorbable poly-α-hydroxyesters as peripheral nerve guidance conduits; a review of material properties, design strategies and their efficacy to date. Biomater. Sci. 2019, 7, 4912–4943. [Google Scholar] [CrossRef]
- Gundu, S.; Varshney, N.; Sahi, A.K.; Mahto, S.K. Recent developments of biomaterial scaffolds and regenerative approaches for craniomaxillofacial bone tissue engineering. J. Polym. Res. 2022, 29, 73. [Google Scholar] [CrossRef]
- Goonoo, N. Tunable biomaterials for myocardial tissue regeneration: Promising new strategies for advanced biointerface control and improved therapeutic outcomes. Biomater. Sci. 2022, 10, 1626–1646. [Google Scholar] [CrossRef]
- Yi, B.; Xu, Q.; Liu, W. An overview of substrate stiffness guided cellular response and its applications in tissue regeneration. Bioact. Mater. 2021, 15, 82–102. [Google Scholar] [CrossRef]
- Baranovskii, D.S.; Klabukov, I.D.; Arguchinskaya, N.V.; Yakimova, A.O.; Kisel, A.A.; Yatsenko, E.M.; Ivanov, S.A.; Shegay, P.V.; Kaprin, A.D. Adverse events, side effects and complications in mesenchymal stromal cell-based therapies. Stem Cell Investig. 2022, 9, 7. [Google Scholar] [CrossRef]
- Yoo, C.; Vines, J.B.; Alexander, G.; Murdock, K.; Hwang, P.; Jun, H.W. Adult stem cells and tissue engineering strategies for salivary gland regeneration: A review. Biomater. Res. 2014, 18, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebata, H.; Kidoaki, S. Avoiding tensional equilibrium in cells migrating on a matrix with cell-scale stiffness-heterogeneity. Biomaterials 2021, 274, 120860. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Sakai, Y.; Hara, T.; Katsuda, T.; Ochiya, T.; Gu, W.L.; Miyamoto, D.; Hamada, T.; Hidaka, M.; Kanetaka, K.; et al. Bioengineering of a CLiP-derived tubular biliary-duct-like structure for bile transport in vitro. Biotechnol. Bioeng. 2021, 118, 2572–2584. [Google Scholar] [CrossRef]
- Wang, Z.; Faria, J.; Penning, L.C.; Masereeuw, R.; Spee, B. Tissue-Engineered Bile Ducts for Disease Modeling and Therapy. Tissue Eng. Part C Methods 2021, 27, 59–76. [Google Scholar] [CrossRef]
- Wang, W.; Chen, D.; Wang, J.; Wen, L. Cellular Homeostasis and Repair in the Biliary Tree. Semin. Liver Dis. 2022, 42, 271–282. [Google Scholar] [CrossRef] [PubMed]
- Justin, A.W.; Saeb-Parsy, K.; Markaki, A.E.; Vallier, L.; Sampaziotis, F. Advances in the generation of bioengineered bile ducts. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2018, 1864, 1532–1538. [Google Scholar] [CrossRef]
- Emmert, M.Y.; Schmitt, B.A.; Loerakker, S.; Sanders, B.; Spriestersbach, H.; Fioretta, E.S.; Bruder, L.; Brakmann, K.; Motta, S.E.; Lintas, V.; et al. Computational modeling guides tissue-engineered heart valve design for long-term in vivo performance in a translational sheep model. Sci. Transl. Med. 2018, 10, eaan4587. [Google Scholar] [CrossRef] [Green Version]
- Perez, J.J.; Perez, R.A.; Perez, A. Computational modeling as a tool to investigate PPI: From drug design to tissue engineering. Front. Mol. Biosci. 2021, 8, 681617. [Google Scholar] [CrossRef]
- Behrens, M.R.; Ruder, W.C. Biopolymers in Regenerative Medicine: Overview, Current Advances, and Future Trends. In Biopolymers for Biomedical and Biotechnological Applications; Rehm, B.H.A., Moradali, M.F., Eds.; Wiley-VCH Verlag GmbH: Weinheim, Germany, 2021; pp. 357–380. [Google Scholar] [CrossRef]
- Qi, Y.; Wang, C.; Wang, Q.; Zhou, F.; Li, T.; Wang, B.; Su, W.; Shang, D.; Wu, S. A simple, quick, and cost-effective strategy to fabricate polycaprolactone/silk fibroin nanofiber yarns for biotextile-based tissue scaffold application. Eur. Polym. J. 2023, 186, 111863. [Google Scholar] [CrossRef]
- Li, M.; Qiu, W.; Wang, Q.; Li, N.; Liu, L.; Wang, X.; Yu, J.; Li, X.; Li, F.; Wu, D. Nitric oxide-releasing tryptophan-based poly (ester urea) s electrospun composite nanofiber mats with antibacterial and antibiofilm activities for infected wound healing. ACS Appl. Mater. Interfaces 2022, 14, 15911–15926. [Google Scholar] [CrossRef] [PubMed]
- Tenchurin, T.H.; Lyundup, A.V.; Demchenko, A.G.; Krasheninnikov, M.E.; Balyasin, M.V.; Klabukov, I.D.; Shepelev, A.D.; Mamagulashvili, V.G.; Orehov, A.S.; Chvalun, S.N.; et al. Modification of biodegradable fibrous scaffolds with Epidermal Growth Factor by emulsion electrospinning for promotion of epithelial cells proliferation. Genes Cells 2017, 12, 47–52. [Google Scholar] [CrossRef] [Green Version]
- Legon’kova, O.A.; Grigor’ev, M.M.; Vinokurova, T.I.; Marinova, L.A.; Zhao, A.V.; Lavrent’ev, S.Y.; Chentsov, A.V.; Solov’ev, N.G.; Lisovenko, D.S. The Behavior of Linear Polyesters in Model Conditions of Bile Ducts. Polym. Sci. Ser. D 2021, 14, 106–111. [Google Scholar] [CrossRef]
- Bazgir, M.; Zhang, W.; Zhang, X.; Elies, J.; Saeinasab, M.; Coates, P.; Youseffi, M.; Sefat, F. Fabrication and Characterization of PCL/PLGA Coaxial and Bilayer Fibrous Scaffolds for Tissue Engineering. Materials 2021, 14, 6295. [Google Scholar] [CrossRef] [PubMed]
- Dyuzheva, T.G.; Lyundup, A.V.; Klabukov, I.D.; Chvalun, S.N.; Grigorev, T.E.; Shepelev, A.D.; Tenchurin, T.H.; Krasheninnikov, M.E.; Oganesyan, R.V. Prospects for tissue engineered bile duct. Genes Cells 2016, 11, 43–47. [Google Scholar]
- Magazzini, L.; Grilli, S.; Fenni, S.E.; Donetti, A.; Cavallo, D.; Monticelli, O. The Blending of Poly (glycolic acid) with Polycaprolactone and Poly (l-lactide): Promising Combinations. Polymers 2021, 13, 2780. [Google Scholar] [CrossRef]
- Chouzouri, G.; Xanthos, M. Degradation of Aliphatic Polyesters in the Presence of Inorganic Fillers. J. Plast. Film Sheeting 2007, 23, 19–36. [Google Scholar] [CrossRef]
- Dulnik, J.; Denis, P.; Sajkiewicz, P.; Kołbuk, D.; Choińska, E. Biodegradation of bicomponent PCL/gelatin and PCL/collagen nanofibers electrospun from alternative solvent system. Polym. Degrad. Stab. 2016, 130, 10–21. [Google Scholar] [CrossRef]
- Seyednejad, H.; Ji, W.; Schuurman, W.; Dhert, W.J.A.; Malda, J.; Yang, F.; Jansen, J.A.; van Nostrum, C.; Vermonden, T.; Hennink, W.E. An Electrospun Degradable Scaffold Based on a Novel Hydrophilic Polyester for Tissue-Engineering Applications. Macromol. Biosci. 2011, 11, 1684–1692. [Google Scholar] [CrossRef]
- Sefat, F.; McKean, R.; Deshpande, P.; Ramachandran, C.; Hill, C.J.; Sangwan, V.S.; Ryan, A.J.; MacNeil, S. Production, Sterilisation and Storage of Biodegradable Electrospun PLGA Membranes for Delivery of Limbal Stem Cells to the Cornea. Procedia Eng. 2013, 59, 101–116. [Google Scholar] [CrossRef]
- Qi, X.; Ren, Y.; Wang, X. New advances in the biodegradation of Poly (lactic) acid. Int. Biodeterior. Biodegrad. 2017, 117, 215–223. [Google Scholar] [CrossRef]
- Pan, J. (Ed.) Modelling Degradation of Bioresorbable Polymeric Medical Devices, 1st ed.; Woodhead Publishing: Sawston, UK, 2014. [Google Scholar]
- Rodriguez, E.J.; Marcos, B.; Huneault, M.A. Hydrolysis of polylactide in aqueous media. J. Appl. Polym. Sci. 2016, 133. [Google Scholar] [CrossRef]
- Rosario, D.J.; Reilly, G.C.; Salah, E.A.; Glover, M.; Bullock, A.J.; Macneil, S. Decellularization and sterilization of porcine urinary bladder matrix for tissue engineering in the lower urinary tract. Regen. Med. 2008, 3, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Chin, A.L.; Wang, X.; Tong, R. Aliphatic Polyester-Based Materials for Enhanced Cancer Immunotherapy. Macromol. Biosci. 2021, 21, 2100087. [Google Scholar] [CrossRef] [PubMed]
- Pappalardo, D.; Mathisen, T.; Finne-Wistrand, A. Biocompatibility of resorbable polymers: A historical perspective and framework for the future. Biomacromolecules 2019, 20, 1465–1477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosworth, L.A.; Downes, S. Physicochemical characterisation of degrading polycaprolactone scaffolds. Polym. Degrad. Stab. 2010, 95, 2269–2276. [Google Scholar] [CrossRef]
- Lam, C.X.F.; Hutmacher, D.W.; Schantz, J.-T.; Woodruff, M.A.; Teoh, S.H. Evaluation of polycaprolactone scaffold degradation for 6 months in vitro and in vivo. J. Biomed. Mater. Res. Part A 2009, 90A, 906–919. [Google Scholar] [CrossRef]
- Iablonskii, P.; Cebotari, S.; Tudorache, I.; Granados, M.; Morticelli, L.; Goecke, T.; Klein, N.; Korossis, S.; Hilfiker, A.; Haverich, A. Tissue-engineered mitral valve: Morphology and biomechanics. Interact. Cardiovasc. Thorac. Surg. 2015, 20, 712–719; discussion 719. [Google Scholar] [CrossRef] [Green Version]
- Grabow, N.; Schmohl, K.; Khosravi, A.; Philipp, M.; Scharfschwerdt, M.; Graf, B.; Stamm, C.; Haubold, A.; Schmitz, K.-P.; Steinhoff, G. Mechanical and structural properties of a novel hybrid heart valve scaffold for tissue engineering. Artif. Organs 2004, 28, 971–979. [Google Scholar] [CrossRef]
- Ye, J.; Xie, C.; Wang, C.; Huang, J.; Yin, Z.; Heng, B.C.; Chen, X.; Shen, W. Promoting musculoskeletal system soft tissue regeneration by biomaterial-mediated modulation of macrophage polarization. Bioact. Mater. 2021, 6, 4096–4109. [Google Scholar] [CrossRef]
- Iqbal, N.; Khan, A.S.; Asif, A.; Yar, M.; Haycock, J.W.; Rehman, I.U. Recent concepts in biodegradable polymers for tissue engineering paradigms: A critical review. Int. Mater. Rev. 2019, 64, 91–126. [Google Scholar] [CrossRef] [Green Version]
- Fathi-Karkan, S.; Banimohamad-Shotorbani, B.; Saghati, S.; Rahbarghazi, R.; Davaran, S. A critical review of fibrous polyurethane-based vascular tissue engineering scaffolds. J. Biol. Eng. 2022, 16, 6. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kang, S.K. Principles for controlling the shape recovery and degradation behavior of biodegradable shape-memory polymers in biomedical applications. Micromachines 2021, 12, 757. [Google Scholar] [CrossRef] [PubMed]
- Tan, R.; Feng, Q.; She, Z.; Wang, M.; Jin, H.; Li, J.; Yu, X. In vitro and in vivo degradation of an injectable bone repair composite. Polym. Degrad. Stab. 2010, 95, 1736–1742. [Google Scholar] [CrossRef]
- Gordienko, M.; Karakatenko, E.; Menshutina, N.; Koroleva, M.; Gilmutdinova, I.; Eremin, P. Composites Composed of Hydrophilic and Hydrophobic Polymers, and Hydroxyapatite Nanoparticles: Synthesis, Characterization, and Study of Their Biocompatible Properties. J. Funct. Biomater. 2021, 12, 55. [Google Scholar] [CrossRef] [PubMed]
- Pitt, C.G.; Gratzl, M.M.; Kimmel, G.L.; Surles, J.; Schindler, A. Aliphatic polyesters II. The degradation of poly (DL-lactide), poly (epsilon-caprolactone), and their copolymers in vivo. Biomaterials 1981, 2, 215–220. [Google Scholar] [CrossRef]
- Akhtar, R.; Sherratt, M.J.; Cruickshank, J.K.; Derby, B. Characterizing the elastic properties of tissues. Mater. Today 2011, 14, 96–105. [Google Scholar] [CrossRef]
- Maccabi, A.; Shin, A.; Namiri, N.; Bajwa, N.; John, M.S.; Taylor, Z.D.; Grundfest, W.; Saddik, G.N. Quantitative characterization of viscoelastic behavior in tissue-mimicking phantoms and ex vivo animal tissues. PLoS ONE 2018, 13, e0191919. [Google Scholar] [CrossRef] [Green Version]
- Yan, J.; Qiang, L.; Gao, Y.; Cui, X.; Zhou, H.; Zhong, S.; Wang, Q.; Wang, H. Effect of fiber alignment in electrospun scaffolds on keratocytes and corneal epithelial cells behavior. J. Biomed. Mater. Res. Part A 2012, 100A, 527–535. [Google Scholar] [CrossRef]
- Whited, B.M.; Rylander, M.N. The influence of electrospun scaffold topography on endothelial cell morphology, alignment, and adhesion in response to fluid flow. Biotechnol. Bioeng. 2014, 111, 184–195. [Google Scholar] [CrossRef] [Green Version]
- Jung, J.H.; Ree, M.; Kim, H. Acid-and base-catalyzed hydrolyses of aliphatic polycarbonates and polyesters. Catal. Today 2006, 115, 283–287. [Google Scholar] [CrossRef]
- Lyu, S.; Schley, J.; Loy, B.; Lind, D.; Hobot, C.; Sparer, R.; Untereker, D. Kinetics and time− temperature equivalence of polymer degradation. Biomacromolecules 2007, 8, 2301–2310. [Google Scholar] [CrossRef]
- Burkersroda, F.; Schedl, L.; Göpferich, A. Why degradable polymers undergo surface erosion or bulk erosion. Biomaterials 2002, 23, 4221–4231. [Google Scholar] [CrossRef]
- Lim, C.Y.; Owens, N.A.; Wampler, R.D.; Ying, Y.; Granger, J.H.; Porter, M.D.; Takahashi, M.; Shimazu, K. Succinimidyl Ester Surface Chemistry: Implications of the Competition between Aminolysis and Hydrolysis on Covalent Protein Immobilization. Langmuir 2014, 30, 12868–12878. [Google Scholar] [CrossRef] [PubMed]
- Palm, K.; Luthman, K.; Ros, J.; Gråsjö, J.; Artursson, P. Effect of Molecular Charge on Intestinal Epithelial Drug Transport: pH-Dependent Transport of Cationic Drugs. J. Pharmacol. Exp. Ther. 1999, 291, 435–443. [Google Scholar]
- Bhattarai, N.; Li, Z.; Gunn, J.; Leung, M.; Cooper, A.; Edmondson, D.; Veiseh, O.; Chen, M.-H.; Zhang, Y.; Ellenbogen, R.G.; et al. Natural-Synthetic Polyblend Nanofibers for Biomedical Applications. Adv. Mater. 2009, 21, 2792–2797. [Google Scholar] [CrossRef]
- Maldonado-Valderrama, J.; Wilde, P.; Macierzanka, A.; Mackie, A. The role of bile salts in digestion. Adv. Colloid Interface Sci. 2011, 165, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Shamsah, A.H.; Cartmell, S.H.; Richardson, S.M.; Bosworth, L.A. Material characterization of PCL: PLLA electrospun fibers following six months degradation in vitro. Polymers 2020, 12, 700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, D.F.; Zhong, S.P. Biodeterioration/Biodegradation of Polymeric Medical Devices In Situ. Int. Biodeterior. Biodegrad. 1994, 34, 95–130. [Google Scholar] [CrossRef]
- Cao, P.; de Leon, A.; Rong, L.; Yin, K.; Abenojar, E.C.; Su, Z.; Tiu, B.D.; Exner, A.A.; Baer, E.; Advincula, R.C. Polymer Nanosheet Containing Star-like Copolymers: A Novel Scalable Controlled Release System. Small 2018, 14, 1800115. [Google Scholar] [CrossRef]
- Morokov, E.S.; Demina, V.A.; Sedush, N.G.; Kalinin, K.T.; Khramtsova, E.A.; Dmitryakov, P.V.; Bakirov, A.V.; Grigoriev, T.E.; Levin, V.M.; Chvalun, S.N. Noninvasive high-frequency acoustic microscopy for 3D visualization of microstructure and estimation of elastic properties during hydrolytic degradation of lactide and ε-caprolactone polymers. Acta Biomater. 2020, 109, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Walejewska, E.; Idaszek, J.; Heljak, M.; Chlanda, A.; Choinska, E.; Hasirci, V.; Swieszkowski, W. The effect of introduction of filament shift on degradation behaviour of PLGA-and PLCL-based scaffolds fabricated via additive manufacturing. Polym. Degrad. Stab. 2020, 171, 109030. [Google Scholar] [CrossRef]
- San Miguel, V.; Peinado, C.; Catalina, F.; Abrusci, C. Bioremediation of naphthalene in water by Sphingomonas paucimobilis using new biodegradable surfactants based on poly (ɛ-caprolactone). Int. Biodeterior. Biodegrad. 2009, 63, 217–223. [Google Scholar] [CrossRef] [Green Version]
- Rediguieri, C.F.; Sassonia, R.C.; Dua, K.; Kikuchi, I.S.; de Jesus Andreoli Pinto, T. Impact of sterilization methods on electrospun scaffolds for tissue engineering. Eur. Polym. J. 2016, 82, 181–195. [Google Scholar] [CrossRef]
- Natu, M.V.; de Sousa, H.C.; Gil, M.H. Influence of polymer processing technique on long term degradation of poly (ε-caprolactone) constructs. Polym. Degrad. Stab. 2013, 98, 44–51. [Google Scholar] [CrossRef] [Green Version]
- Park, S.J.; Lee, B.K.; Na, M.H.; Kim, D.S. Melt-spun shaped fibers with enhanced surface effects: Fiber fabrication, characterization and application to woven scaffolds. Acta Biomater. 2013, 9, 7719–7726. [Google Scholar] [CrossRef] [PubMed]
- Lyu, S.; Untereker, D. Degradability of polymers for implantable biomedical devices. Int. J. Mol. Sci. 2009, 10, 4033–4065. [Google Scholar] [CrossRef] [Green Version]
- Laycock, B.; Nikolić, M.; Colwell, J.M.; Gauthier, E.; Halley, P.; Bottle, S.; George, G. Lifetime prediction of biodegradable polymers. Prog. Polym. Sci. 2017, 71, 144–189. [Google Scholar] [CrossRef] [Green Version]
- Pena, J.; Corrales, T.; Izquierdo-Barba, I.; Serrano, M.C.; Portolés, M.T.; Pagani, R.; Vallet-Regí, M. Alkaline-treated poly (ϵ-caprolactone) films: Degradation in the presence or absence of fibroblasts. J. Biomed. Mater. Res. Part A 2006, 76, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Ahola, N.; Veiranto, M.; Rich, J.; Efimov, A.; Hannula, M.; Seppälä, J.; Kellomäki, M. Hydrolytic degradation of composites of poly (L-lactide-co-ɛ-caprolactone) 70/30 and β-tricalcium phosphate. J. Biomater. Appl. 2013, 28, 529–543. [Google Scholar] [CrossRef]
- Fernández, J.; Larrañaga, A.; Etxeberría, A.; Sarasua, J.R. Effects of chain microstructures and derived crystallization capability on hydrolytic degradation of poly (L-lactide/ε-caprolactone) copolymers. Polym. Degrad. Stab. 2013, 98, 481–489. [Google Scholar] [CrossRef]
- Brito, J.; Andrianov, A.K.; Sukhishvili, S.A. Factors Controlling Degradation of Biologically Relevant Synthetic Polymers in Solution and Solid State. ACS Appl. Bio Mater. 2022, 5, 5057–5076. [Google Scholar] [CrossRef] [PubMed]
- Darie-Niță, R.N.; Râpă, M.; Frąckowiak, S. Special Features of Polyester-Based Materials for Medical Applications. Polymers 2022, 14, 951. [Google Scholar] [CrossRef] [PubMed]
- Woodruff, M.A.; Hutmacher, D.W. The return of a forgotten polymer—Polycaprolactone in the 21st century. Prog. Polym. Sci. 2010, 35, 1217–1256. [Google Scholar] [CrossRef] [Green Version]
- Trofimchuk, E.S.; Moskvina, M.A.; Nikonorova, N.I.; Efimov, A.V.; Garina, E.S.; Grokhovskaya, T.E.; Ivanova, O.A.; Bakirov, A.V.; Sedush, N.G.; Chvalun, S.N. Hydrolytic degradation of polylactide films deformed by the environmental crazing mechanism. Eur. Polym. J. 2020, 139, 110000. [Google Scholar] [CrossRef]
- Barral, V.; Dropsit, S.; Cayla, A.; Campagne, C.; Devaux, É. Study of the influence of PCL on the in vitro degradation of extruded pla monofilaments and melt-spun filaments. Polymers 2021, 13, 171. [Google Scholar] [CrossRef]
- Moya-Lopez, C.; González-Fuentes, J.; Bravo, I.; Chapron, D.; Bourson, P.; Alonso-Moreno, C.; Hermida-Merino, D. Polylactide Perspectives in Biomedicine: From Novel Synthesis to the Application Performance. Pharmaceutics 2022, 14, 1673. [Google Scholar] [CrossRef]
- Visan, A.I.; Popescu-Pelin, G.; Socol, G. Degradation behavior of polymers used as coating materials for drug delivery—A basic review. Polymers 2021, 13, 1272. [Google Scholar] [CrossRef]
- Bhattarai, D.P.; Aguilar, L.E.; Park, C.H.; Kim, C.S. A review on properties of natural and synthetic based electrospun fibrous materials for bone tissue engineering. Membranes 2018, 8, 62. [Google Scholar] [CrossRef] [Green Version]
- Reddy, M.S.B.; Ponnamma, D.; Choudhary, R.; Sadasivuni, K.K. A comparative review of natural and synthetic biopolymer composite scaffolds. Polymers 2021, 13, 1105. [Google Scholar] [CrossRef]
- Li, Q.; Wang, P.; Liu, C.; Liu, F.; Zhao, H.; Guo, Y.; Zhao, G. Preparation and mechanical behavior of the acellular porcine common bile duct and its immunogenicity in vivo. J. Mech. Behav. Biomed. Mater. 2022, 136, 105494. [Google Scholar] [CrossRef]
- Wu, J.; Hu, C.; Tang, Z.; Yu, Q.; Liu, X.; Chen, H. Tissue-engineered vascular grafts: Balance of the four major requirements. Colloid Interface Sci. Commun. 2018, 23, 34–44. [Google Scholar] [CrossRef]
- Harrell, D.B. Basic science of regenerative biology and application to regenerative medicine: Past, present, and future. Tech. Reg. Anesth. Pain Manag. 2015, 19, 3–9. [Google Scholar] [CrossRef]
- Caddeo, S.; Boffito, M.; Sartori, S. Tissue Engineering Approaches in the Design of Healthy and Pathological In Vitro Tissue Models. Front. Bioeng. Biotechnol. 2017, 5, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Savina, I.N.; Zoughaib, M.; Yergeshov, A.A. Design and assessment of biodegradable macroporous cryogels as advanced tissue engineering and drug carrying materials. Gels 2021, 7, 79. [Google Scholar] [CrossRef] [PubMed]
- Bermejillo Barrera, M.D.; Franco-Martínez, F.; Díaz Lantada, A. Artificial intelligence aided design of tissue engineering scaffolds employing virtual tomography and 3D Convolutional Neural Networks. Materials 2021, 14, 5278. [Google Scholar] [CrossRef] [PubMed]
- Miyazawa, M.; Aikawa, M.; Takashima, J.; Kobayashi, H.; Ohnishi, S.; Ikada, Y. Pitfalls and promises of bile duct alternatives: A narrative review. World J. Gastroenterol. 2022, 28, 5707–5722. [Google Scholar] [CrossRef]
- Klabukov, I.; Balyasin, M.; Krasilnikova, O.; Tenchurin, T.; Titov, A.; Krasheninnikov, M.; Mudryak, D.; Sulina, Y.; Shepelev, A.; Chvalun, S.; et al. Angiogenic Modification of Microfibrous Polycaprolactone by pCMV-VEGF 165 Plasmid Promotes Local Vascular Growth after Implantation in Rats. Int. J. Mol. Sci. 2023, 24, 1399. [Google Scholar] [CrossRef] [PubMed]
- Pond, K.W.; Doubrovinski, K.; Thorne, C.A. Wnt/β-catenin Signaling in Tissue Self-Organization. Genes 2020, 11, 939. [Google Scholar] [CrossRef]
- Klabukov, I.D.; Krasilnikova, O.A.; Baranovskii, D.S. Quantitative human physiology: An introduction guide for advanced tissue engineering. Biotechnol. J. 2022, 17, 2100481. [Google Scholar] [CrossRef]







| No. | Polymer | Concentration (wt.%) | Volumetric Flow Rate of Solution, mL/h | Applied Voltage, kV | Inter-Electrode Gap, cm |
|---|---|---|---|---|---|
| 1 | PCL | 7 | 8 | 14 | 25 |
| 2 | PLCL | 12 | 30 | 14 | 25 |
| 3 | PLGA | 14 | 30 | 14 | 20 |
| Sample | Test Direction | N | σ, MPa | ε, % | E, MPa |
|---|---|---|---|---|---|
| Native | radial | 3 | 0.75 ± 0.15 | 135 ± 14 | 1.2 ± 0.20 |
| axial | 3 | 4.1 ± 0.25 | 32 ± 5 | 22.1 ± 1.3 | |
| Decellularized | radial | 3 | 1.3 ± 0.20 | 145 ± 11 | 2.4 ± 0.20 |
| axial | 3 | 6.3 ± 0.25 | 35 ± 5 | 29.6 ± 1.5 |
| Polymer | PCL | PLGA | PLCL | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Form-factor | Rod | Film | Fibrous material | Rod | Film | Fibrous material | Rod | Film | Fibrous material |
| Dimensions | ⌀ 1.7 mm | Thickness 0.1 mm | ⌀ 0.0016 mm | ⌀ 2.3 mm | Thickness 0.1 mm | ⌀ 0.0049 mm | ⌀ 2.5 mm | Thickness 0.2 mm | ⌀ 0.0036 mm |
| Specific surface area, m2/g | 0.002 | 0.016 | 2.1 | 0.0013 | 0.016 | 0.62 | 0.0012 | 0.008 | 0.88 |
| Original Mn, kDa | 96 | 50 | 111 | 63 | 58 | 69 | 91 | 36.6 | 54 |
| Crystallinity, % | 64 | 58 | 35 | 75:25 | 75:25 | 70:30 | 70:30 | 74:26 | 70:30 |
| Mn decreasing after 140 days in PBS at 37 °C, % | 0 | 11 | 36 | 52 | 38 | 15 | 40 | 52 | 14 |
| Mn decreasing after 140 days in DMEM at 37 °C, % | - | 25 | 86 | 94 | 86 | 68 | 89 | - | 62 |
| Reference | [69] | [101] | - | [101] | [102] | - | [102] | [103] | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klabukov, I.; Tenchurin, T.; Shepelev, A.; Baranovskii, D.; Mamagulashvili, V.; Dyuzheva, T.; Krasilnikova, O.; Balyasin, M.; Lyundup, A.; Krasheninnikov, M.; et al. Biomechanical Behaviors and Degradation Properties of Multilayered Polymer Scaffolds: The Phase Space Method for Bile Duct Design and Bioengineering. Biomedicines 2023, 11, 745. https://doi.org/10.3390/biomedicines11030745
Klabukov I, Tenchurin T, Shepelev A, Baranovskii D, Mamagulashvili V, Dyuzheva T, Krasilnikova O, Balyasin M, Lyundup A, Krasheninnikov M, et al. Biomechanical Behaviors and Degradation Properties of Multilayered Polymer Scaffolds: The Phase Space Method for Bile Duct Design and Bioengineering. Biomedicines. 2023; 11(3):745. https://doi.org/10.3390/biomedicines11030745
Chicago/Turabian StyleKlabukov, Ilya, Timur Tenchurin, Alexey Shepelev, Denis Baranovskii, Vissarion Mamagulashvili, Tatiana Dyuzheva, Olga Krasilnikova, Maksim Balyasin, Alexey Lyundup, Mikhail Krasheninnikov, and et al. 2023. "Biomechanical Behaviors and Degradation Properties of Multilayered Polymer Scaffolds: The Phase Space Method for Bile Duct Design and Bioengineering" Biomedicines 11, no. 3: 745. https://doi.org/10.3390/biomedicines11030745







