Differentiating Lumbar Spinal Etiology from Peripheral Plexopathies
Abstract
:1. Introduction
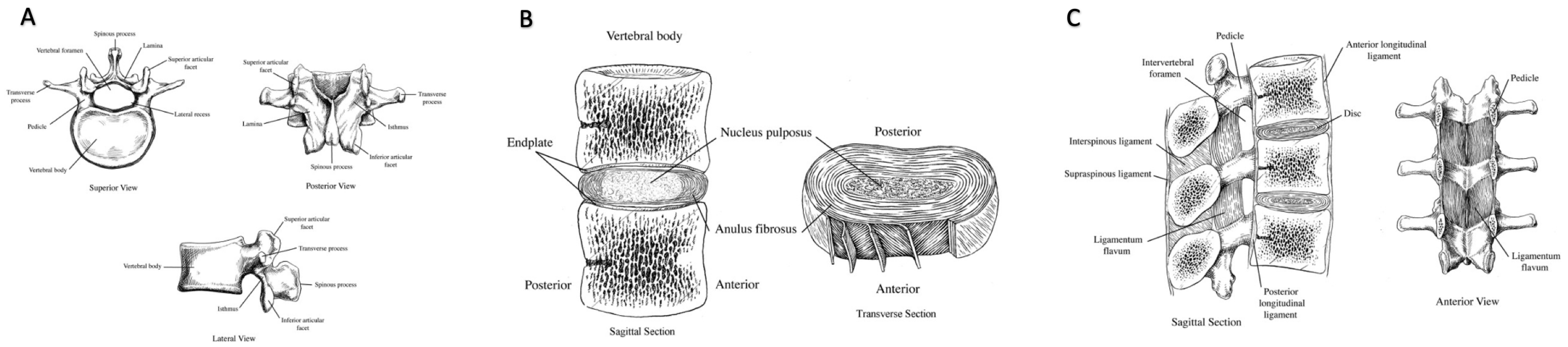
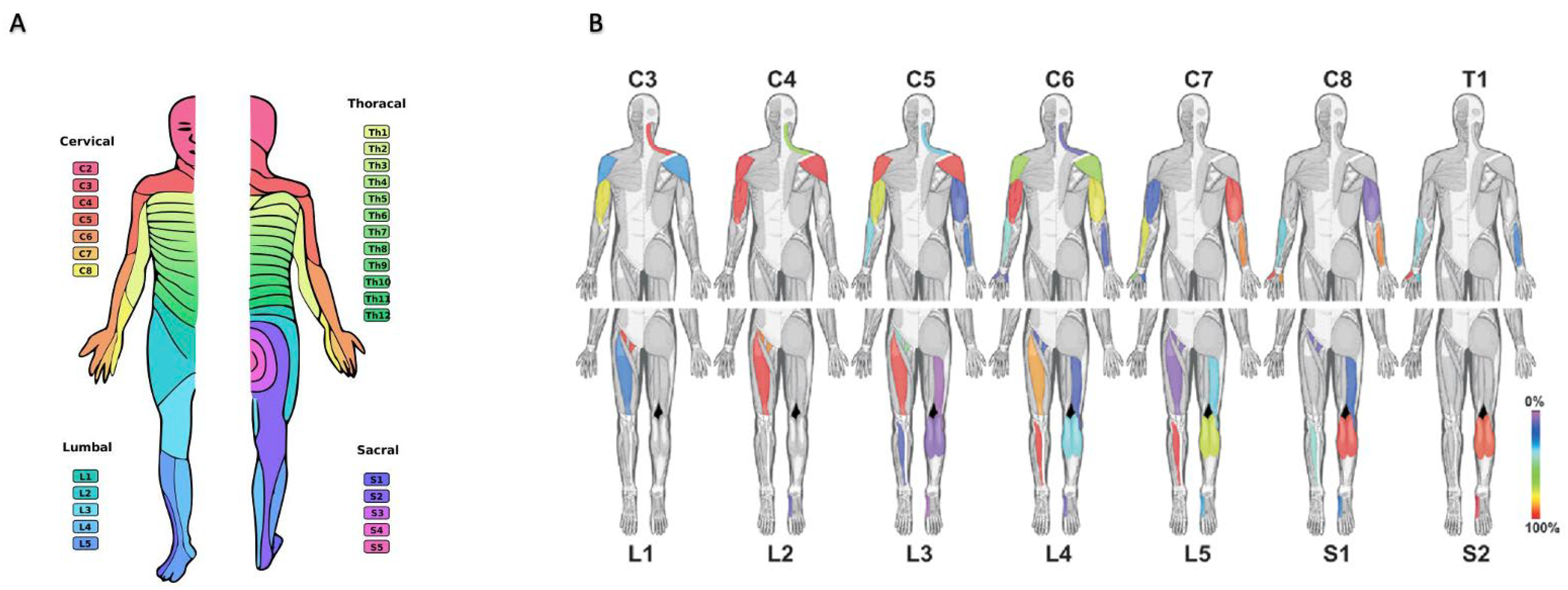
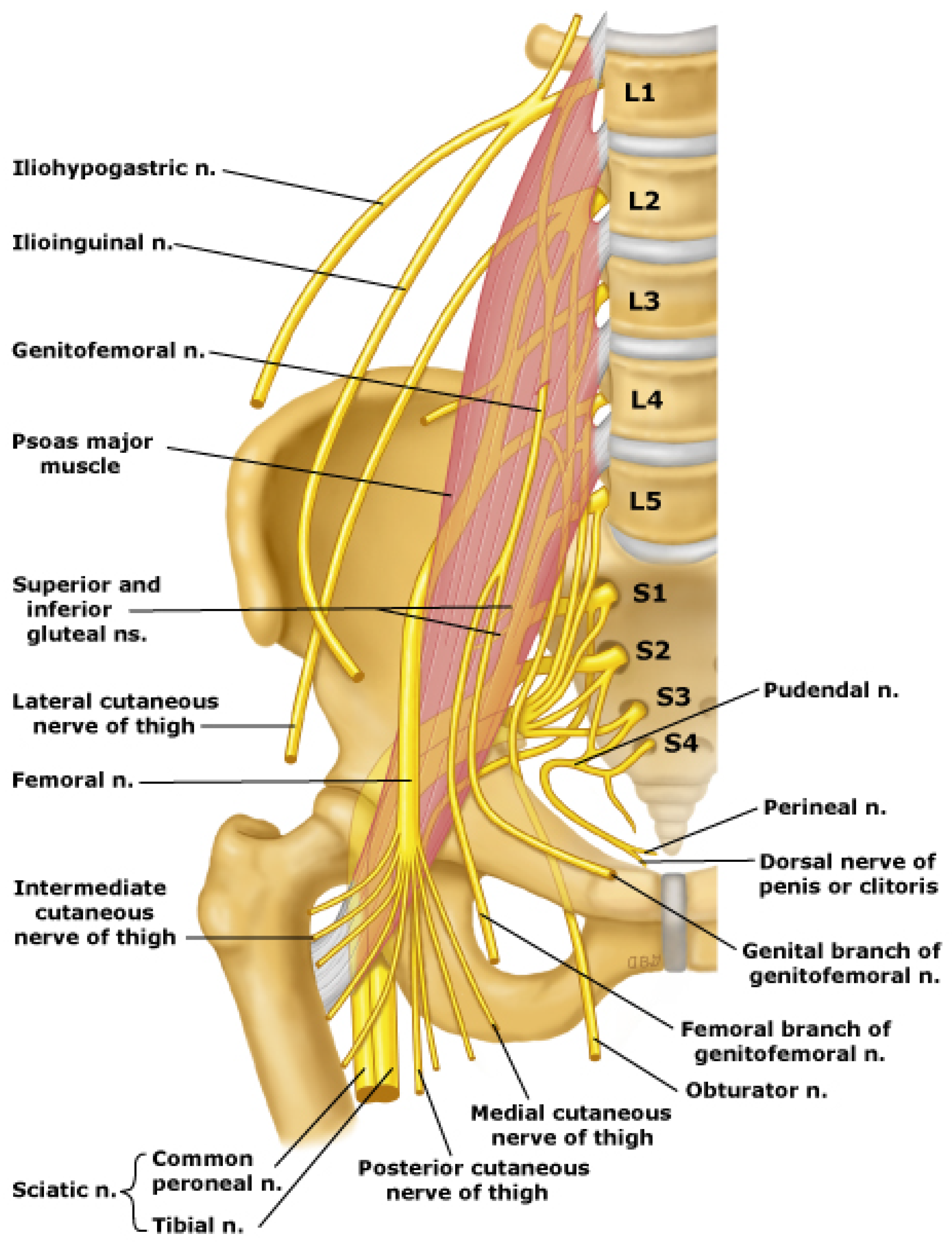
2. Anatomy of the Lumbar Spine and Lumbosacral Plexus
3. Etiology
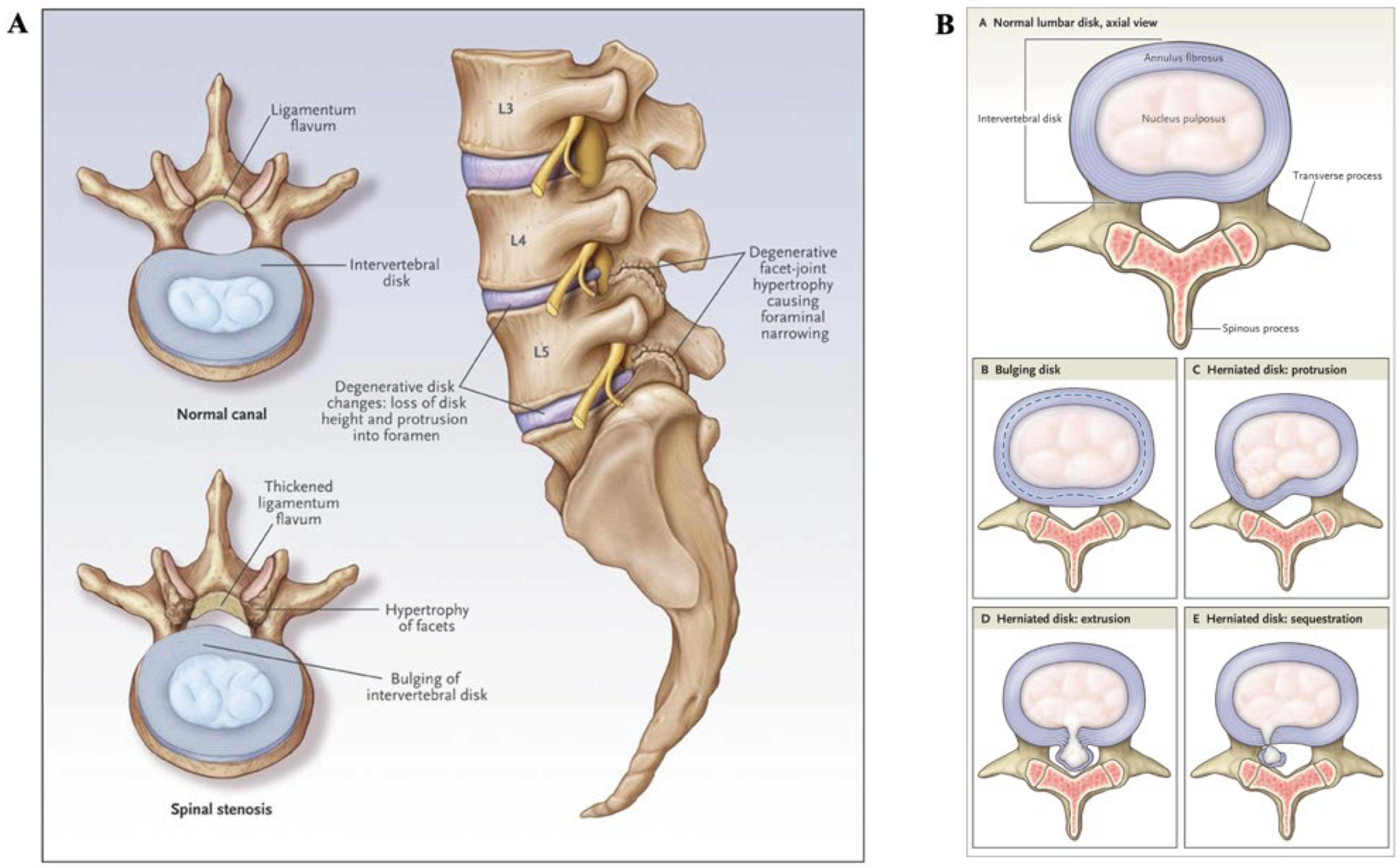
3.1. Lumbar Spine Pathology
3.1.1. Herniated Nucleus Pulposus
3.1.2. Osteoarthritis
3.1.3. Ligamentum Flavum Thickening
3.1.4. Other Causes
3.2. Lumbosacral Plexopathy
3.2.1. Trauma
3.2.2. Metabolic and Inflammatory Causes
3.2.3. Neoplastic
3.2.4. Other Causes
4. Neurologic Consultation
4.1. Clinical Presentationand Physical Examination
4.1.1. Distinctions in Symptomatic Presentation
4.1.2. Physical Examination
4.2. Diagnostic Evaluation
4.2.1. Radiological Imaging
4.2.2. Electroneurography and Electromyography Studies
5. Treatment and Management
5.1. Conservative Approaches
5.2. Surgical Approaches
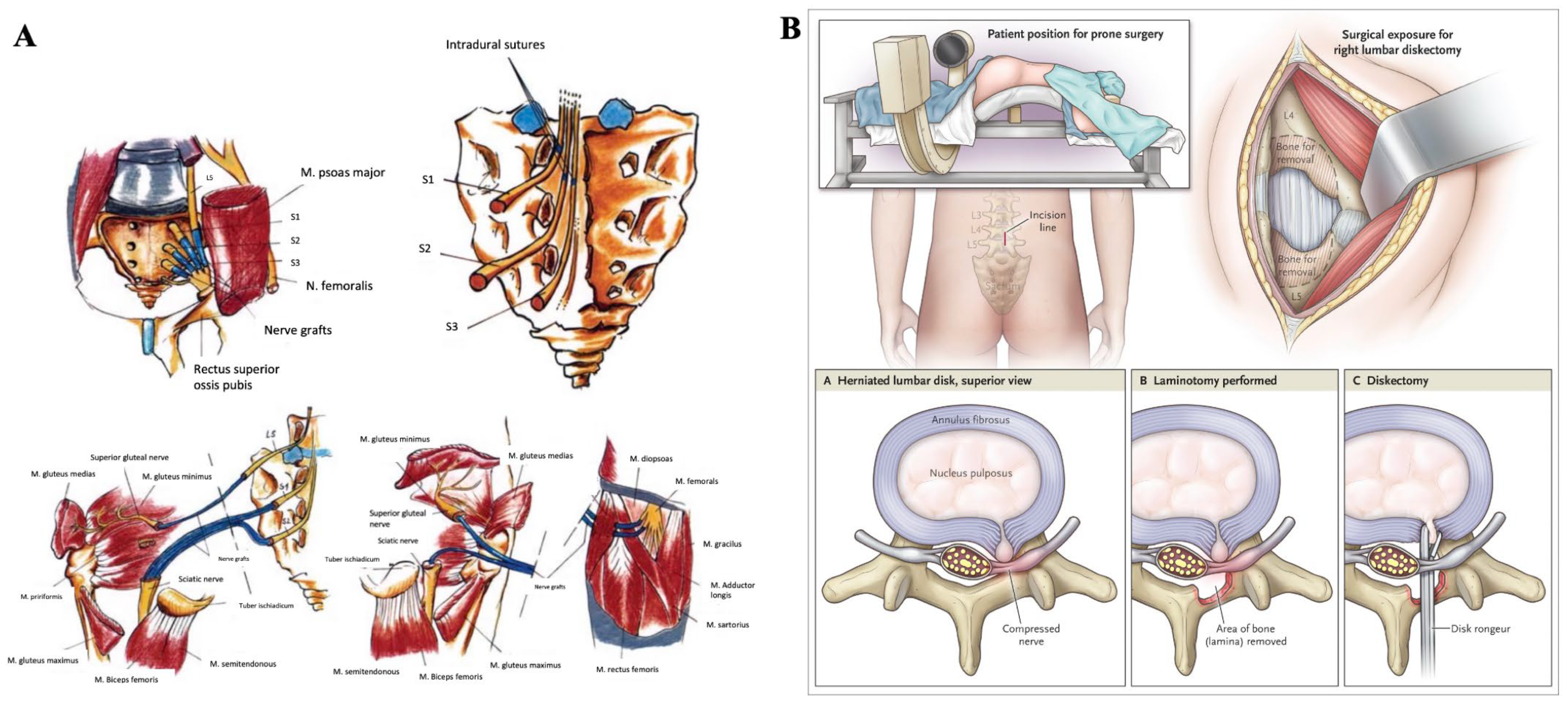
5.2.1. Laminectomy for Lumbar Spinal Stenosis
5.2.2. Discectomy for Lumbar Herniated Nucleus Pulposus
5.2.3. Surgical Intervention Strategies for Lumbosacral Plexopathy
6. Emerging Treatment Options
6.1. Novel Conservative and Surgical Techniques
6.1.1. Approaches for Common Lumbar Spinal Pathologies
6.1.2. Approaches for Lumbosacral Plexopathies
6.2. Nerve Regeneration Strategies
7. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mattiuzzi, C.; Lippi, G.; Bovo, C. Current Epidemiology of Low Back Pain. J. Hosp. Manag. Health Policy 2020, 4, 15. [Google Scholar] [CrossRef]
- Koes, B.W.; van Tulder, M.W.; Thomas, S. Diagnosis and Treatment of Low Back Pain. BMJ 2006, 332, 1430–1434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frymoyer, J.W. Lumbar Disk Disease: Epidemiology. Instr. Course Lect. 1992, 41, 217–223. [Google Scholar]
- Koes, B.W.; van Tulder, M.W.; Peul, W.C. Diagnosis and Treatment of Sciatica. BMJ 2007, 334, 1313–1317. [Google Scholar] [CrossRef] [Green Version]
- Dydyk, A.M.; Hameed, S. Lumbosacral Plexopathy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Wilbourn, A.J. Plexopathies. Neurol. Clin. 2007, 25, 139–171. [Google Scholar] [CrossRef]
- Van Alfen, N.; Malessy, M.J.A. Chapter 18—Diagnosis of Brachial and Lumbosacral Plexus Lesions. In Handbook of Clinical Neurology; Said, G., Krarup, C., Eds.; Peripheral Nerve Disorders; Elsevier: Amsterdam, The Netherlands, 2013; Volume 115, pp. 293–310. [Google Scholar] [CrossRef]
- Brejt, N.; Berry, J.; Nisbet, A.; Bloomfield, D.; Burkill, G. Pelvic Radiculopathies, Lumbosacral Plexopathies, and Neuropathies in Oncologic Disease: A Multidisciplinary Approach to a Diagnostic Challenge. Cancer Imaging 2013, 13, 591–601. [Google Scholar] [CrossRef] [Green Version]
- Ebraheim, N.A.; Hassan, A.; Lee, M.; Xu, R. Functional Anatomy of the Lumbar Spine. Semin. Pain Med. 2004, 2, 131–137. [Google Scholar] [CrossRef]
- Intervertebral Foramina—An Overview. ScienceDirect Topics. Available online: https://www.sciencedirect.com/topics/veterinary-science-and-veterinary-medicine/intervertebral-foramina (accessed on 9 January 2023).
- Waxenbaum, J.A.; Reddy, V.; Williams, C.; Futterman, B. Anatomy, Back, Lumbar Vertebrae. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Walter, B.A.; Torre, O.M.; Laudier, D.; Naidich, T.P.; Hecht, A.C.; Iatridis, J.C. Form and Function of the Intervertebral Disc in Health and Disease: A Morphological and Stain Comparison Study. J. Anat. 2015, 227, 707–716. [Google Scholar] [CrossRef] [Green Version]
- Lundon, K.; Bolton, K. Structure and Function of the Lumbar Intervertebral Disk in Health, Aging, and Pathologic Conditions. J. Orthop. Sports Phys. Ther. 2001, 31, 291–303; discussion 304–306. [Google Scholar] [CrossRef] [Green Version]
- Cleveland Clinic. Lumbar Spine: What It Is, Anatomy & Disorders. Available online: https://my.clevelandclinic.org/health/articles/22396-lumbar-spine (accessed on 8 January 2023).
- Whitman, P.A.; Adigun, O.O. Anatomy, Skin, Dermatomes. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Schirmer, C.M.; Shils, J.L.; Arle, J.E.; Cosgrove, G.R.; Dempsey, P.K.; Tarlov, E.; Kim, S.; Martin, C.J.; Feltz, C.; Moul, M.; et al. Heuristic Map of Myotomal Innervation in Humans Using Direct Intraoperative Nerve Root Stimulation: Clinical Article. J. Neurosurg. Spine 2011, 15, 64–70. [Google Scholar] [CrossRef]
- Edgar, M.A.; Ghadially, J.A. Innervation of the Lumbar Spine. Clin. Orthop. Relat. Res. 1976, 115, 35. [Google Scholar] [CrossRef]
- Thaisetthawatkul, P.; Dyck, P.J.B. Chapter 9—Cervical and Lumbosacral Radiculoplexus Neuropathies. In Dysimmune Neuropathies; Rajabally, Y.A., Ed.; Academic Press: Cambridge, MA, USA, 2020; pp. 199–223. [Google Scholar] [CrossRef]
- Lumbosacral Plexus—UpToDate. Available online: https://sso.uptodate.com/contents/image/print?imageKey=NEURO%2F75983&source=graphics_gallery&topicKey=5278 (accessed on 15 January 2023).
- Rubin, D.I. Brachial and Lumbosacral Plexopathies: A Review. Clin. Neurophysiol. Pract. 2020, 5, 173–193. [Google Scholar] [CrossRef] [PubMed]
- Kawaji, Y.; Uchiyama, S.; Yagi, E. Three-Dimensional Evaluation of Lumbar Disc Hernia and Prediction of Absorption by Enhanced MRI. J. Orthop. Sci. 2001, 6, 498–502. [Google Scholar] [CrossRef] [PubMed]
- Asch, H.L.; Lewis, P.J.; Moreland, D.B.; Egnatchik, J.G.; Yu, Y.J.; Clabeaux, D.E.; Hyland, A.H. Prospective Multiple Outcomes Study of Outpatient Lumbar Microdiscectomy: Should 75 to 80% Success Rates Be the Norm? J. Neurosurg. 2002, 96 (Suppl. S1), 34–44. [Google Scholar] [CrossRef] [PubMed]
- Fisher, C.; Noonan, V.; Bishop, P.; Boyd, M.; Fairholm, D.; Wing, P.; Dvorak, M. Outcome Evaluation of the Operative Management of Lumbar Disc Herniation Causing Sciatica. J. Neurosurg. 2004, 100 (Suppl. S4), 317–324. [Google Scholar] [CrossRef] [Green Version]
- Bush, K.; Cowan, N.; Katz, D.E.; Gishen, P. The Natural History of Sciatica Associated with Disc Pathology. A Prospective Study with Clinical and Independent Radiologic Follow-Up. Spine 1992, 17, 1205–1212. [Google Scholar] [CrossRef]
- Strayer, A. Lumbar Spine: Common Pathology and Interventions. J. Neurosci. Nurs. 2005, 37, 181–193. [Google Scholar] [CrossRef]
- Sarzi-Puttini, P.; Atzeni, F.; Fumagalli, M.; Capsoni, F.; Carrabba, M. Osteoarthritis of the Spine. Semin. Arthritis Rheum. 2005, 34 (Suppl. S2), 38–43. [Google Scholar]
- Goode, A.P.; Carey, T.S.; Jordan, J.M. Low Back Pain and Lumbar Spine Osteoarthritis: How Are They Related? Curr. Rheumatol. Rep. 2013, 15, 305. [Google Scholar] [CrossRef] [Green Version]
- Laplante, B.L.; DePalma, M.J. Spine Osteoarthritis. PM R 2012, 4 (Suppl. S5), S28–S36. [Google Scholar] [CrossRef]
- Goode, A.P.; Nelson, A.E.; Kraus, V.B.; Renner, J.B.; Jordan, J.M. Biomarkers Reflect Differences in Osteoarthritis Phenotypes of the Lumbar Spine: The Johnston County Osteoarthritis Project. Osteoarthr. Cartil. 2017, 25, 1672–1679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gellhorn, A.C.; Katz, J.N.; Suri, P. Osteoarthritis of the Spine: The Facet Joints. Nat. Rev. Rheumatol. 2013, 9, 216–224. [Google Scholar] [CrossRef] [Green Version]
- Lindsey, T.; Dydyk, A.M. Spinal Osteoarthritis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Gandhi, R.; Woo, K.M.; Zywiel, M.G.; Rampersaud, Y.R. Metabolic Syndrome Increases the Prevalence of Spine Osteoarthritis. Orthop. Surg. 2014, 6, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Naylor, A. Factors in the Development of the Spinal Stenosis Syndrome. J. Bone Jt. Surg. Br. 1979, 61-B, 306–309. [Google Scholar] [CrossRef]
- Hansson, T.; Suzuki, N.; Hebelka, H.; Gaulitz, A. The Narrowing of the Lumbar Spinal Canal during Loaded MRI: The Effects of the Disc and Ligamentum Flavum. Eur. Spine J. 2009, 18, 679–686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altinkaya, N.; Yildirim, T.; Demir, S.; Alkan, O.; Sarica, F.B. Factors Associated with the Thickness of the Ligamentum Flavum: Is Ligamentum Flavum Thickening Due to Hypertrophy or Buckling? Spine 2011, 36, E1093–E1097. [Google Scholar] [CrossRef] [PubMed]
- Sairyo, K.; Biyani, A.; Goel, V.; Leaman, D.; Booth, R.; Thomas, J.; Gehling, D.; Vishnubhotla, L.; Long, R.; Ebraheim, N. Pathomechanism of Ligamentum Flavum Hypertrophy: A Multidisciplinary Investigation Based on Clinical, Biomechanical, Histologic, and Biologic Assessments. Spine 2005, 30, 2649–2656. [Google Scholar] [CrossRef]
- Sakamaki, T.; Sairyo, K.; Sakai, T.; Tamura, T.; Okada, Y.; Mikami, H. Measurements of Ligamentum Flavum Thickening at Lumbar Spine Using MRI. Arch. Orthop. Trauma Surg. 2009, 129, 1415–1419. [Google Scholar] [CrossRef]
- Sudhir, G.; Vignesh Jayabalan, S.; Gadde, S.; Venkatesh Kumar, G.; Karthik Kailash, K. Analysis of Factors Influencing Ligamentum Flavum Thickness in Lumbar Spine—A Radiological Study of 1070 Disc Levels in 214 Patients. Clin. Neurol. Neurosurg. 2019, 182, 19–24. [Google Scholar] [CrossRef]
- Yoshiiwa, T.; Miyazaki, M.; Kawano, M.; Ikeda, S.; Tsumura, H. Analysis of the Relationship between Hypertrophy of the Ligamentum Flavum and Lumbar Segmental Motion with Aging Process. Asian Spine J. 2016, 10, 528–535. Available online: https://pubmed.ncbi.nlm.nih.gov/27340534 (accessed on 22 January 2023). [CrossRef] [Green Version]
- Ito, M.; Abumi, K.; Takeda, N.; Satoh, S.; Hasegawa, K.; Kaneda, K. Pathologic Features of Spinal Disorders in Patients Treated with Long-Term Hemodialysis. Spine 1998, 23, 2127–2133. [Google Scholar] [CrossRef] [PubMed]
- Inatomi, K.; Matsumoto, T.; Tomonaga, T.; Eto, M.; Shindo, H.; Hayashi, T.; Konishi, H. Histological Analysis of the Ligamentum Flavum of Patients with Dialysis-Related Spondyloarthropathy. J. Orthop. Sci. 2004, 9, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Dunn, B. Lumbar spondylolysis and spondylolisthesis. J. Am. Acad. Physician Assist. 2019, 32, 50–51. Available online: https://journals.lww.com/jaapa/Fulltext/2019/12000/Lumbar_spondylolysis_and_spondylolisthesis.11.aspx (accessed on 22 January 2023). [CrossRef] [PubMed]
- Nickerson, E.K.; Sinha, R. Vertebral osteomyelitis in adults: An update. Br. Med. Bull. 2016, 117, 121–138. Available online: https://academic.oup.com/bmb/article/117/1/121/1744712 (accessed on 22 January 2023). [CrossRef] [PubMed]
- Katz, J.N.; Harris, M.B. Lumbar Spinal Stenosis. N. Engl. J. Med. 2008, 358, 818–825. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Mirza, S.K. Herniated Lumbar Intervertebral Disk. N. Engl. J. Med. 2016, 374, 1763–1772. [Google Scholar] [CrossRef]
- Chiou-Tan, F.Y.; Kemp, K., Jr.; Elfenbaum, M.; Chan, K.T.; Song, J. Lumbosacral plexopathy in gunshot wounds and motor vehicle accidents: Comparison of electrophysiologic findings. Am. J. Phys. Med. Rehabil. 2001, 80, 280–285. Available online: https://pubmed.ncbi.nlm.nih.gov/11277135 (accessed on 22 January 2023). [CrossRef]
- Kutsy, R.L.; Robinson, L.R.; Routt, M.L., Jr. Lumbosacral plexopathy in pelvic trauma. Muscle Nerve 2000, 23, 1757–1760. Available online: https://pubmed.ncbi.nlm.nih.gov/11054756 (accessed on 22 January 2023). [CrossRef]
- Laughlin, R.S.; Dyck, P.J.B. Diabetic Radiculoplexus Neuropathies. Handb. Clin. Neurol. 2014, 126, 45–52. [Google Scholar] [CrossRef]
- Ng, P.S.; Dyck, P.J.; Laughlin, R.S.; Thapa, P.; Pinto, M.V.; Dyck, P.J.B. Lumbosacral Radiculoplexus Neuropathy: Incidence and the Association with Diabetes Mellitus. Neurology 2019, 92, e1188–e1194. [Google Scholar] [CrossRef]
- Ladha, S.S.; Dyck, P.J.B.; Spinner, R.J.; Perez, D.G.; Zeldenrust, S.R.; Amrami, K.K.; Solomon, A.; Klein, C.J. Isolated amyloidosis presenting with lumbosacral radiculoplexopathy: Description of two cases and pathogenic review. J. Peripher. Nerv. Syst. 2006, 11, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Jaeckle, K.A.; Young, D.F.; Foley, K.M. The Natural History of Lumbosacral Plexopathy in Cancer. Neurology 1985, 35, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Song, E.J.; Park, J.S.; Ryu, K.N.; Park, S.Y.; Jin, W. Perineural Spread Along Spinal and Obturator Nerves in Primary Vaginal Carcinoma: A Case Report. World Neurosurg. 2018, 115, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Ladha, S.S.; Spinner, R.J.; Suarez, G.A.; Amrami, K.K.; Dyck, P.J.B. Neoplastic lumbosacral radiculoplexopathy in prostate cancer by direct perineural spread: An unusual entity. Muscle Nerve 2006, 34, 659–665. Available online: https://pubmed.ncbi.nlm.nih.gov/16810682 (accessed on 22 January 2023). [CrossRef]
- Thomas, J.E.; Cascino, T.L.; Earle, J.D. Differential Diagnosis between Radiation and Tumor Plexopathy of the Pelvis. Neurology 1985, 35, 1–7. [Google Scholar] [CrossRef]
- Wu, L.; Cruz, R. Lumbar Spinal Stenosis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Davis, D.; Maini, K.; Vasudevan, A. Sciatica. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Donnally, C.J., III; Butler, A.J.; Varacallo, M. Lumbosacral Disc Injuries. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Hall, S.; Bartleson, J.D.; Onofrio, B.M.; Baker, H.L.; Okazaki, H.; O’Duffy, J.D. Lumbar Spinal Stenosis. Clinical Features, Diagnostic Procedures, and Results of Surgical Treatment in 68 Patients. Ann. Intern. Med. 1985, 103, 271–275. [Google Scholar] [CrossRef]
- Dyck, P.J.B.; Thaisetthawatkul, P. Lumbosacral Plexopathy. Contin. Lifelong Learn. Neurol. 2014, 20, 1343. [Google Scholar] [CrossRef]
- Lang, E.M.; Borges, J.; Carlstedt, T. Surgical Treatment of Lumbosacral Plexus Injuries. J. Neurosurg. Spine 2004, 1, 64–71. [Google Scholar] [CrossRef]
- Yabuki, S.; Fukumori, N.; Takegami, M.; Onishi, Y.; Otani, K.; Sekiguchi, M.; Wakita, T.; Kikuchi, S.; Fukuhara, S.; Konno, S. Prevalence of Lumbar Spinal Stenosis, Using the Diagnostic Support Tool, and Correlated Factors in Japan: A Population-Based Study. J. Orthop. Sci. 2013, 18, 893–900. [Google Scholar] [CrossRef] [Green Version]
- Schmid, R.; Reinhold, M.; Blauth, M. Lumbosacral Dislocation: A Review of the Literature and Current Aspects of Management. Injury 2010, 41, 321–328. [Google Scholar] [CrossRef]
- Falkson, S.R.; Hinson, J.W. Westphal Sign. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Kurt, S.; Kaplan, Y.; Karaer, H.; Erkorkmaz, U. Femoral Nerve Involvement in Diabetics. Eur. J. Neurol. 2009, 16, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Solheim, L.F.; Hagen, R. Femoral and Sciatic Neuropathies After Total Hip Arthroplasty. Acta Orthop. Scand. 1980, 51, 531–534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poage, C.; Roth, C.; Scott, B. Peroneal Nerve Palsy: Evaluation and Management. JAAOS J. Am. Acad. Orthop. Surg. 2016, 24, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Fleischman, A.N.; Rothman, R.H.; Parvizi, J. Femoral Nerve Palsy Following Total Hip Arthroplasty: Incidence and Course of Recovery. J. Arthroplast. 2018, 33, 1194–1199. [Google Scholar] [CrossRef]
- Distad, B.J.; Weiss, M.D. Clinical and Electrodiagnostic Features of Sciatic Neuropathies. Phys. Med. Rehabil. Clin. N. Am. 2013, 24, 107–120. [Google Scholar] [CrossRef]
- Maravilla, K.R.; Bowen, B.C. Imaging of the Peripheral Nervous System: Evaluation of Peripheral Neuropathy and Plexopathy. AJNR Am. J. Neuroradiol. 1998, 19, 1011–1023. [Google Scholar]
- Stynes, S.; Konstantinou, K.; Ogollah, R.; Hay, E.M.; Dunn, K.M. Clinical Diagnostic Model for Sciatica Developed in Primary Care Patients with Low Back-Related Leg Pain. PLoS ONE 2018, 13, e0191852. [Google Scholar] [CrossRef]
- Ro, T.H.; Edmonds, L. Diagnosis and Management of Piriformis Syndrome: A Rare Anatomic Variant Analyzed by Magnetic Resonance Imaging. J. Clin. Imaging Sci. 2018, 8, 6. [Google Scholar] [CrossRef] [Green Version]
- Moore, K.R.; Tsuruda, J.S.; Dailey, A.T. The Value of MR Neurography for Evaluating Extraspinal Neuropathic Leg Pain: A Pictorial Essay. AJNR Am. J. Neuroradiol. 2001, 22, 786–794. [Google Scholar]
- Gupta, L.; Yadav, M.; Thulkar, S. ‘Trident Sign’ in Pelvis: Sinister Sign with Poor Prognosis. BMJ Case Rep. 2017, 2017, bcr2017220460. [Google Scholar] [CrossRef]
- Laughlin, R.S.; Dyck, P.J.B. Electrodiagnostic Testing in Lumbosacral Plexopathies. Phys. Med. Rehabil. Clin. N. Am. 2013, 24, 93–105. [Google Scholar] [CrossRef] [PubMed]
- Ehler, E.; Vyšata, O.; Včelák, R.; Pazdera, L. Painful Lumbosacral Plexopathy. Medicine 2015, 94, e766. [Google Scholar] [CrossRef] [PubMed]
- Bastron, J.A.; Thomas, J.E. Diabetic Polyradiculopathy: Clinical and Electromyographic Findings in 105 Patients. Mayo Clin. Proc. 1981, 56, 725–732. [Google Scholar] [PubMed]
- Haig, A.J.; Tong, H.C.; Yamakawa, K.S.J.; Quint, D.J.; Hoff, J.T.; Chiodo, A.; Miner, J.A.; Choksi, V.R.; Geisser, M.E. The Sensitivity and Specificity of Electrodiagnostic Testing for the Clinical Syndrome of Lumbar Spinal Stenosis. Spine 2005, 30, 2667–2676. [Google Scholar] [CrossRef]
- Jacobs, W.C.H.; van Tulder, M.; Arts, M.; Rubinstein, S.M.; van Middelkoop, M.; Ostelo, R.; Verhagen, A.; Koes, B.; Peul, W.C. Surgery versus Conservative Management of Sciatica Due to a Lumbar Herniated Disc: A Systematic Review. Eur. Spine J. 2011, 20, 513–522. [Google Scholar] [CrossRef] [Green Version]
- Garozzo, D.; Zollino, G.; Ferraresi, S. In Lumbosacral Plexus Injuries Can We Identify Indicators That Predict Spontaneous Recovery or the Need for Surgical Treatment? Results from a Clinical Study on 72 Patients. J. Brachial Plex. Peripher. Nerve Inj. 2014, 9, 1. [Google Scholar] [CrossRef]
- Lurie, J.; Tomkins-Lane, C. Management of Lumbar Spinal Stenosis. BMJ 2016, 352, h6234. [Google Scholar] [CrossRef]
- Ammendolia, C.; Stuber, K.; de Bruin, L.K.; Furlan, A.D.; Kennedy, C.A.; Rampersaud, Y.R.; Steenstra, I.A.; Pennick, V. Nonoperative Treatment of Lumbar Spinal Stenosis with Neurogenic Claudication: A Systematic Review. Spine 2012, 37, E609–E616. [Google Scholar] [CrossRef]
- Shabat, S.; Folman, Y.; Leitner, Y.; Fredman, B.; Gepstein, R. Failure of Conservative Treatment for Lumbar Spinal Stenosis in Elderly Patients. Arch. Gerontol. Geriatr. 2007, 44, 235–241. [Google Scholar] [CrossRef]
- Whitman, J.M.; Flynn, T.W.; Fritz, J.M. Nonsurgical Management of Patients with Lumbar Spinal Stenosis: A Literature Review and a Case Series of Three Patients Managed with Physical Therapy. Phys. Med. Rehabil. Clin. N. Am. 2003, 14, 77–101. [Google Scholar] [CrossRef]
- Macedo, L.G.; Hum, A.; Kuleba, L.; Mo, J.; Truong, L.; Yeung, M.; Battié, M.C. Physical Therapy Interventions for Degenerative Lumbar Spinal Stenosis: A Systematic Review. Phys. Ther. 2013, 93, 1646–1660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aalto, T.J.; Leinonen, V.; Herno, A.; Alen, M.; Kröger, H.; Turunen, V.; Savolainen, S.; Saari, T.; Airaksinen, O. Postoperative Rehabilitation Does Not Improve Functional Outcome in Lumbar Spinal Stenosis: A Prospective Study with 2-Year Postoperative Follow-Up. Eur. Spine J. 2011, 20, 1331–1340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Messiah, S.; Tharian, A.R.; Candido, K.D.; Knezevic, N.N. Neurogenic Claudication: A Review of Current Understanding and Treatment Options. Curr. Pain Headache Rep. 2019, 23, 32. [Google Scholar] [CrossRef] [PubMed]
- Dowell, D.; Haegerich, T.M.; Chou, R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA 2016, 315, 1624–1645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rutkove, S.B.; Sax, T.W. Lumbosacral Plexopathies. In Neuromuscular Disorders in Clinical Practice; Katirji, B., Kaminski, H.J., Ruff, R.L., Eds.; Springer: New York, NY, USA, 2014; pp. 1063–1071. [Google Scholar] [CrossRef]
- Song, S.H.; Ryu, G.H.; Park, J.W.; Lee, H.J.; Nam, K.Y.; Kim, H.; Kim, S.Y.; Kwon, B.S. The Effect and Safety of Steroid Injection in Lumbar Spinal Stenosis: With or Without Local Anesthetics. Ann. Rehabil. Med. 2016, 40, 14–20. [Google Scholar] [CrossRef] [Green Version]
- Deyo, R.A.; Mirza, S.K.; Martin, B.I.; Kreuter, W.; Goodman, D.C.; Jarvik, J.G. Trends, Major Medical Complications, and Charges Associated with Surgery for Lumbar Spinal Stenosis in Older Adults. JAMA J. Am. Med. Assoc. 2010, 303, 1259–1265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kovacs, F.M.; Urrútia, G.; Alarcón, J.D. Surgery Versus Conservative Treatment for Symptomatic Lumbar Spinal Stenosis: A Systematic Review of Randomized Controlled Trials. Spine 2011, 36, E1335. [Google Scholar] [CrossRef] [Green Version]
- Silvers, H.R.; Lewis, P.J.; Asch, H.L. Decompressive Lumbar Laminectomy for Spinal Stenosis. J. Neurosurg. 1993, 78, 695–701. [Google Scholar] [CrossRef]
- Estefan, M.; Munakomi, S.; Camino Willhuber, G.O. Laminectomy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Bydon, M.; Macki, M.; Abt, N.B.; Sciubba, D.M.; Wolinsky, J.-P.; Witham, T.F.; Gokaslan, Z.L.; Bydon, A. Clinical and Surgical Outcomes after Lumbar Laminectomy: An Analysis of 500 Patients. Surg. Neurol. Int. 2015, 6 (Suppl. S4), S190–S193. [Google Scholar] [CrossRef]
- Guha, D.; Heary, R.F.; Shamji, M.F. Iatrogenic Spondylolisthesis Following Laminectomy for Degenerative Lumbar Stenosis: Systematic Review and Current Concepts. Neurosurg. Focus 2015, 39, E9. [Google Scholar] [CrossRef] [Green Version]
- Ghogawala, Z.; Dziura, J.; Butler, W.E.; Dai, F.; Terrin, N.; Magge, S.N.; Coumans, J.-V.C.E.; Harrington, J.F.; Amin-Hanjani, S.; Schwartz, J.S.; et al. Laminectomy plus Fusion versus Laminectomy Alone for Lumbar Spondylolisthesis. N. Engl. J. Med. 2016, 374, 1424–1434. [Google Scholar] [CrossRef] [PubMed]
- Sharif, S.; Shaikh, Y.; Bajamal, A.H.; Costa, F.; Zileli, M. Fusion Surgery for Lumbar Spinal Stenosis: WFNS Spine Committee Recommendations. World Neurosurg. X 2020, 7, 100077. [Google Scholar] [CrossRef] [PubMed]
- De Cicco, F.L.; Camino Willhuber, G.O. Nucleus Pulposus Herniation. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Blamoutier, A. Surgical Discectomy for Lumbar Disc Herniation: Surgical Techniques. Orthop. Traumatol. Surg. Res. 2013, 99 (Suppl. S1), S187–S196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lurie, J.D.; Faucett, S.C.; Hanscom, B.; Tosteson, T.D.; Ball, P.A.; Abdu, W.A.; Frymoyer, J.W.; Weinstein, J.N. Lumbar Discectomy Outcomes Vary by Herniation Level in the Spine Patient Outcomes Research Trial. J. Bone Jt. Surg. Am. 2008, 90, 1811–1819. [Google Scholar] [CrossRef] [Green Version]
- Loupasis, G.A.; Stamos, K.; Katonis, P.G.; Sapkas, G.; Korres, D.S.; Hartofilakidis, G. Seven- to 20-Year Outcome of Lumbar Discectomy. Spine 1999, 24, 2313–2317. [Google Scholar] [CrossRef]
- Alexandre, A.; Corò, L.; Azuelos, A. Microsurgical Treatment of Lumbosacral Plexus Injuries. Acta Neurochir. Suppl. 2005, 92, 53–59. [Google Scholar] [CrossRef]
- Nichols, D.S.; Fenton, J.; Cox, E.; Dang, J.; Garbuzov, A.; McCall-Wright, P.; Chim, H. Surgical Interventions for Lumbosacral Plexus Injuries: A Systematic Review. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4436. [Google Scholar] [CrossRef]
- Safavi-Abbasi, S.; Feiz-Erfan, I.; Shetter, A.G. Neurolysis. In Encyclopedia of the Neurological Sciences, 2nd ed.; Aminoff, M.J., Daroff, R.B., Eds.; Academic Press: Oxford, UK, 2014; pp. 406–407. [Google Scholar] [CrossRef]
- Lipinski, L.J.; Spinner, R.J. Neurolysis, Neurectomy, and Nerve Repair/Reconstruction for Chronic Pain. Neurosurg. Clin. N. Am. 2014, 25, 777–787. [Google Scholar] [CrossRef]
- Kim, D.H.; Murovic, J.A.; Tiel, R.L.; Kline, D.G. Intrapelvic and Thigh-Level Femoral Nerve Lesions: Management and Outcomes in 119 Surgically Treated Cases. J. Neurosurg. 2004, 100, 989–996. [Google Scholar] [CrossRef]
- Kitagawa, R.; Kim, D.; Reid, N.; Kline, D. Surgical Management of Obturator Nerve Lesions. Neurosurgery 2009, 65 (Suppl. S4), A24–A28. [Google Scholar] [CrossRef]
- Dahlin, L.B. Techniques of Peripheral Nerve Repair. Scand. J. Surg. 2008, 97, 310–316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kornfeld, T.; Vogt, P.M.; Radtke, C. Nerve Grafting for Peripheral Nerve Injuries with Extended Defect Sizes. Wien. Med. Wochenschr. 2019, 169, 240–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osgaard, O.; Husby, J. Femoral Nerve Repair with Nerve Autografts. Report of Two Cases. J. Neurosurg. 1977, 47, 751–754. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Li, Y.; Zhang, Y.; Li, S.; Jiang, J.; Gu, Y.; Xu, L. Different Surgical Reconstructions for Femoral Nerve Injury: A Clinical Study on 9 Cases. Ann. Plast. Surg. 2020, 84 (Suppl. S3), S171–S177. [Google Scholar] [CrossRef] [PubMed]
- Shacklock, M.; Rade, M.; Poznic, S.; Marčinko, A.; Fredericson, M.; Kröger, H.; Kankaanpää, M.; Airaksinen, O. Treatment of Sciatica and Lumbar Radiculopathy with an Intervertebral Foramen Opening Protocol: Pilot Study in a Hospital Emergency and In-Patient Setting. Physiother. Theory Pract. 2022, 1–11. [Google Scholar] [CrossRef]
- Metz, L.N.; Deviren, V. Low-Grade Spondylolisthesis. Neurosurg. Clin. N. Am. 2007, 18, 237–248. [Google Scholar] [CrossRef]
- Abdu, W.A.; Sacks, O.A.; Tosteson, A.N.A.; Zhao, W.; Tosteson, T.D.; Morgan, T.S.; Pearson, A.; Weinstein, J.N.; Lurie, J.D. Long-Term Results of Surgery Compared With Nonoperative Treatment for Lumbar Degenerative Spondylolisthesis in the Spine Patient Outcomes Research Trial (SPORT). Spine 2018, 43, 1619–1630. [Google Scholar] [CrossRef]
- Hennemann, S.; de Abreu, M.R. Degenerative Lumbar Spinal Stenosis. Rev. Bras. Ortop. 2021, 56, 9–17. [Google Scholar] [CrossRef]
- Bae, J.; Lee, S.-H.; Wagner, R.; Shen, J.; Telfeian, A.E. Full Endoscopic Surgery for Thoracic Pathology: Next Step after Mastering Lumbar and Cervical Endoscopic Spine Surgery? BioMed Res. Int. 2022, 2022, 8345736. [Google Scholar] [CrossRef]
- Kim, H.S.; Raorane, H.D.; Wu, P.H.; Heo, D.H.; Sharma, S.B.; Jang, I.-T. Incidental Durotomy During Endoscopic Stenosis Lumbar Decompression: Incidence, Classification, and Proposed Management Strategies. World Neurosurg. 2020, 139, e13–e22. [Google Scholar] [CrossRef]
- Liang, J.; Lian, L.; Liang, S.; Zhao, H.; Shu, G.; Chao, J.; Yuan, C.; Zhai, M. Efficacy and Complications of Unilateral Biportal Endoscopic Spinal Surgery for Lumbar Spinal Stenosis: A Meta-Analysis and Systematic Review. World Neurosurg. 2022, 159, e91–e102. [Google Scholar] [CrossRef]
- Häckel, S.; Christen, S.; Vögelin, E.; Keel, M.J.B. Exposure of the Lumbosacral Plexus by Using the Pararectus Approach: A Technical Note. Oper. Neurosurg. 2023, 24, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Kurze, C.; Keel, M.J.B.; Kollár, A.; Siebenrock, K.A.; Klenke, F.M. The Pararectus Approach—A Versatile Option in Pelvic Musculoskeletal Tumor Surgery. J. Orthop. Surg. 2019, 14, 232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, G.; Chen, J.; Liang, C.; Zhang, C.; Li, X.; Hu, Y. The Pararectus Approach in Acetabular Fractures Treatment: Functional and Radiologcial Results. BMC Musculoskelet. Disord. 2022, 23, 370. [Google Scholar] [CrossRef] [PubMed]
- Sanuki, N.; Kodama, S.; Seta, H.; Sakai, M.; Watanabe, H. Radiation Therapy for Malignant Lumbosacral Plexopathy: A Case Series. Cureus 2022, 14, e20939. [Google Scholar] [CrossRef]
- Cao, X.; Gao, X.-S.; Li, W.; Liu, P.; Qin, S.-B.; Dou, Y.-B.; Li, H.-Z.; Shang, S.; Gu, X.-B.; Ma, M.-W.; et al. Contouring Lumbosacral Plexus Nerves with MR Neurography and MR/CT Deformable Registration Technique. Front. Oncol. 2022, 12, 818953. [Google Scholar] [CrossRef]
- Chen, A.M.; Hall, W.H.; Li, J.; Beckett, L.; Farwell, D.G.; Lau, D.H.; Purdy, J.A. Brachial Plexus-Associated Neuropathy After High-Dose Radiation Therapy for Head-and-Neck Cancer. Int. J. Radiat. Oncol. 2012, 84, 165–169. [Google Scholar] [CrossRef]
- Kong, Y.; Kuss, M.; Shi, Y.; Fang, F.; Xue, W.; Shi, W.; Liu, Y.; Zhang, C.; Zhong, P.; Duan, B. Exercise Facilitates Regeneration after Severe Nerve Transection and Further Modulates Neural Plasticity. Brain Behav. Immun. Health 2022, 26, 100556. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Li, Y.-T.; Chen, Y.C.; Li, Z.-Y.; Hung, C.-H. Exercise Training Attenuates Neuropathic Pain and Cytokine Expression after Chronic Constriction Injury of Rat Sciatic Nerve. Anesth. Analg. 2012, 114, 1330–1337. [Google Scholar] [CrossRef]
- Kami, K.; Tajima, F.; Senba, E. Exercise-Induced Hypoalgesia: Potential Mechanisms in Animal Models of Neuropathic Pain. Anat. Sci. Int. 2017, 92, 79–90. [Google Scholar] [CrossRef]
- de Freria, C.M.; Van Niekerk, E.; Blesch, A.; Lu, P. Neural Stem Cells: Promoting Axonal Regeneration and Spinal Cord Connectivity. Cells 2021, 10, 3296. [Google Scholar] [CrossRef]
- Kadoya, K.; Lu, P.; Nguyen, K.; Lee-Kubli, C.; Kumamaru, H.; Yao, L.; Knackert, J.; Poplawski, G.; Dulin, J.N.; Strobl, H.; et al. Spinal Cord Reconstitution with Homologous Neural Grafts Enables Robust Corticospinal Regeneration. Nat. Med. 2016, 22, 479–487. [Google Scholar] [CrossRef] [Green Version]
- Dulin, J.N.; Adler, A.F.; Kumamaru, H.; Poplawski, G.H.D.; Lee-Kubli, C.; Strobl, H.; Gibbs, D.; Kadoya, K.; Fawcett, J.W.; Lu, P.; et al. Injured Adult Motor and Sensory Axons Regenerate into Appropriate Organotypic Domains of Neural Progenitor Grafts. Nat. Commun. 2018, 9, 84. [Google Scholar] [CrossRef] [Green Version]
- Cofano, F.; Boido, M.; Monticelli, M.; Zenga, F.; Ducati, A.; Vercelli, A.; Garbossa, D. Mesenchymal Stem Cells for Spinal Cord Injury: Current Options, Limitations, and Future of Cell Therapy. Int. J. Mol. Sci. 2019, 20, 2698. [Google Scholar] [CrossRef] [Green Version]
- Qu, J.; Zhang, H. Roles of Mesenchymal Stem Cells in Spinal Cord Injury. Stem Cells Int. 2017, 2017, 5251313. [Google Scholar] [CrossRef] [Green Version]
- Zachar, L.; Bačenková, D.; Rosocha, J. Activation, Homing, and Role of the Mesenchymal Stem Cells in the Inflammatory Environment. J. Inflamm. Res. 2016, 9, 231–240. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.-C.; Huang, Y.-Y. Biomaterials and Strategies for Nerve Regeneration. Artif. Organs 2006, 30, 514–522. [Google Scholar] [CrossRef]
- George, P.M.; Lyckman, A.W.; LaVan, D.A.; Hegde, A.; Leung, Y.; Avasare, R.; Testa, C.; Alexander, P.M.; Langer, R.; Sur, M. Fabrication and Biocompatibility of Polypyrrole Implants Suitable for Neural Prosthetics. Biomaterials 2005, 26, 3511–3519. [Google Scholar] [CrossRef]
- Lladó, J.; Haenggeli, C.; Maragakis, N.J.; Snyder, E.Y.; Rothstein, J.D. Neural Stem Cells Protect against Glutamate-Induced Excitotoxicity and Promote Survival of Injured Motor Neurons through the Secretion of Neurotrophic Factors. Mol. Cell. Neurosci. 2004, 27, 322–331. [Google Scholar] [CrossRef]
- Huang, E.J.; Reichardt, L.F. Trk Receptors: Roles in Neuronal Signal Transduction. Annu. Rev. Biochem. 2003, 72, 609–642. [Google Scholar] [CrossRef] [Green Version]
- Song, S.; McConnell, K.W.; Amores, D.; Levinson, A.; Vogel, H.; Quarta, M.; Rando, T.A.; George, P.M. Electrical Stimulation of Human Neural Stem Cells via Conductive Polymer Nerve Guides Enhances Peripheral Nerve Recovery. Biomaterials 2021, 275, 120982. [Google Scholar] [CrossRef] [PubMed]
| Nerve | Muscles | Sensory Distribution | |
|---|---|---|---|
| Lumbar Plexus | Iliohypogastric (L1-2) | - | Inferior abdominal wall |
| Ilioinguinal (L1-2) | - | Medial Groin | |
| Genitofemoral (L1-2) | - | - | |
| Lateral femoral cutaneous (L3-4) | - | Anterolateral thigh | |
| Obturator (L2,3,4) | Adductor long Adductor magnus Gracilis | - | |
| Femoral (L2,3,4) Saphenous (L2,3,4) | Quadriceps - | - Medial leg and foot | |
| Sacral Plexus | Sup. Gluteal (L4-5) | Gluteus medius Tensor fascia lata | - |
| Inf. Gluteal (L4-S1) | Gluteus maximus | - | |
| Sciatic (L4-S2) | Anterior tibialis Peroneus longus Gastrocnemius Soleus Foot muscles | Foot Lateral leg | |
| Pudendal (S2,3,4) | External anal sphincter | Perineal |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foreman, M.; Maddy, K.; Patel, A.; Reddy, A.; Costello, M.; Lucke-Wold, B. Differentiating Lumbar Spinal Etiology from Peripheral Plexopathies. Biomedicines 2023, 11, 756. https://doi.org/10.3390/biomedicines11030756
Foreman M, Maddy K, Patel A, Reddy A, Costello M, Lucke-Wold B. Differentiating Lumbar Spinal Etiology from Peripheral Plexopathies. Biomedicines. 2023; 11(3):756. https://doi.org/10.3390/biomedicines11030756
Chicago/Turabian StyleForeman, Marco, Krisna Maddy, Aashay Patel, Akshay Reddy, Meredith Costello, and Brandon Lucke-Wold. 2023. "Differentiating Lumbar Spinal Etiology from Peripheral Plexopathies" Biomedicines 11, no. 3: 756. https://doi.org/10.3390/biomedicines11030756
APA StyleForeman, M., Maddy, K., Patel, A., Reddy, A., Costello, M., & Lucke-Wold, B. (2023). Differentiating Lumbar Spinal Etiology from Peripheral Plexopathies. Biomedicines, 11(3), 756. https://doi.org/10.3390/biomedicines11030756






