The Relationship between Type 1 Diabetes Mellitus, TNF-α, and IL-10 Gene Expression
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Ethics
2.3. Participants and Eligibility
2.4. Groups
- Group 1: patients with T1DM during an episode of ketoacidosis, admitted to the emergency service up to 72 h after the event;
- Group 2: T1DM patients with HbA1c ≥ 8%;
- Group 3: T1DM patients with HbA1c < 8%;
- Group 4: a control group with healthy participants (without TDM1).
2.5. Measurements
2.6. RNA Extraction
2.7. Diabetes Definitions Criteria
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Negrato, C.A.; Lauris, J.R.P.; Saggioro, I.B.; Corradini, M.C.M.; Borges, P.R.; Cres, M.C.; Junior, A.L.; Guedes, M.F.S.; Gomes, M.B. Increasing incidence of type 1 diabetes between 1986 and 2015 in Bauru, Brazil. Diabetes Res. Clin. Pr. 2017, 127, 198–204. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2019. Diabetes Care 2019, 42, S13–S28. [Google Scholar] [CrossRef] [Green Version]
- Tenenbaum Weiss, Y.; Friger, M.; Haim, A.; Hershkovitz, E. Patterns in Body Mass Index Changes in Children after Type 1 Diabetes Mellitus Diagnosis. Isr. Med. Assoc. J. IMAJ 2023, 25, 137–142. [Google Scholar] [PubMed]
- Wang, Z.; Xie, Z.; Lu, Q.; Chang, C.; Zhou, Z. Beyond Genetics: What Causes Type 1 Diabetes. Clin. Rev. Allergy Immunol. 2017, 52, 273–286. [Google Scholar] [CrossRef]
- DCCT Research Group. Effects of age, duration and treatment of insulin-dependent diabetes mellitus on residual beta-cell function: Observations during eligibility testing for the Diabetes Control and Complications Trial (DCCT). The DCCT Research Group. J. Clin. Endocrinol. Metab. 1987, 65, 30–36. [Google Scholar] [CrossRef]
- Katsarou, A.; Gudbjornsdottir, S.; Rawshani, A.; Dabelea, D.; Bonifacio, E.; Anderson, B.J.; Jacobsen, L.M.; Schatz, D.A.; Lernmark, A. Type 1 diabetes mellitus. Nat. Rev. Dis. Primers 2017, 3, 17016. [Google Scholar] [CrossRef] [PubMed]
- Peakman, M. Immunological pathways to β-cell damage in Type 1 diabetes. Diabet. Med. 2013, 30, 147–154. [Google Scholar] [CrossRef]
- Buckner, T.; Johnson, R.K.; Vanderlinden, L.A.; Carry, P.M.; Romero, A.; Onengut-Gumuscu, S.; Chen, W.M.; Fiehn, O.; Frohnert, B.I.; Crume, T.; et al. An Oxylipin-Related Nutrient Pattern and Risk of Type 1 Diabetes in the Diabetes Autoimmunity Study in the Young (DAISY). Nutrients 2023, 15, 945. [Google Scholar] [CrossRef]
- Ouyang, W.; O'Garra, A. IL-10 Family Cytokines IL-10 and IL-22: From Basic Science to Clinical Translation. Immunity 2019, 50, 871–891. [Google Scholar] [CrossRef]
- Pierson, W.; Liston, A. A new role for interleukin-10 in immune regulation. Immunol. Cell Biol. 2010, 88, 769–770. [Google Scholar] [CrossRef]
- Trifunovic, J.; Miller, L.; Debeljak, Z.; Horvat, V. Pathologic patterns of interleukin 10 expression--a review. Biochem. Med. 2015, 25, 36–48. [Google Scholar] [CrossRef] [PubMed]
- Rutz, S.; Ouyang, W. Regulation of Interleukin-10 Expression. Adv. Exp. Med. Biol. 2016, 941, 89–116. [Google Scholar] [CrossRef]
- Obasanmi, G.; Lois, N.; Armstrong, D.; Hombrebueno, J.M.R.; Lynch, A.; Chen, M.; Xu, H. Peripheral Blood Mononuclear Cells from Patients with Type 1 Diabetes and Diabetic Retinopathy Produce Higher Levels of IL-17A, IL-10 and IL-6 and Lower Levels of IFN-γ-A Pilot Study. Cells 2023, 12, 467. [Google Scholar] [CrossRef]
- Russell, M.A.; Morgan, N.G. The impact of anti-inflammatory cytokines on the pancreatic β-cell. Islets 2014, 6, e950547. [Google Scholar] [CrossRef] [Green Version]
- Nouar, M.; Miliani, M.; Belhassena, I.; Fatmi, A.; Aribi, M. Sodium selenite modulates global activation of proinflammatory M1-like macrophages, necroinflammation and M1-like/M2-like dichotomy at the onset of human type 1 diabetes. Endocr. Metab. Immune Disord. Drug Targets 2023. Ahead of Print. [Google Scholar] [CrossRef]
- Jang, D.I.; Lee, A.H.; Shin, H.Y.; Song, H.R.; Park, J.H.; Kang, T.B.; Lee, S.R.; Yang, S.H. The Role of Tumor Necrosis Factor Alpha (TNF-α) in Autoimmune Disease and Current TNF-α Inhibitors in Therapeutics. Int. J. Mol. Sci. 2021, 22, 2719. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Y.C.; Chen, Y.L.; Pan, Y.H.; Tian, F.; Xu, Y.; Zhang, X.X.; Zhao, H.L. The change of serum tumor necrosis factor alpha in patients with type 1 diabetes mellitus: A systematic review and meta-analysis. PLoS One 2017, 12, e0176157. [Google Scholar] [CrossRef] [Green Version]
- Wang, K.; Li, F.; Cui, Y.; Cui, C.; Cao, Z.; Xu, K.; Han, S.; Zhu, P.; Sun, Y. The Association between Depression and Type 1 Diabetes Mellitus: Inflammatory Cytokines as Ferrymen in between? Mediat. Inflamm. 2019, 2019, 2987901. [Google Scholar] [CrossRef]
- Ozgur, B.A.; Cinar, S.A.; Coskunpinar, E.; Yilmaz, A.; Altunkanat, D.; Deniz, G.; Gurol, A.O.; Yilmaz, M.T. The role of cytokines and T-bet, GATA3, ROR-γt, and FOXP3 transcription factors of T cell subsets in the natural clinical progression of Type 1 Diabetes. Immunol. Res. 2023. [Google Scholar] [CrossRef]
- Alkaabi, J.; Sharma, C.; Yasin, J.; Afandi, B.; Beshyah, S.A.; Almazrouei, R.; Alkaabi, A.; Al Hamad, S.; Ahmed, L.A.; Beiram, R.; et al. Relationship between lipid profile, inflammatory and endothelial dysfunction biomarkers, and type 1 diabetes mellitus: A case-control study. Am. J. Transl. Res. 2022, 14, 4838–4847. [Google Scholar]
- Lechleitner, M.; Koch, T.; Herold, M.; Dzien, A.; Hoppichler, F. Tumour necrosis factor-alpha plasma level in patients with type 1 diabetes mellitus and its association with glycaemic control and cardiovascular risk factors. J. Intern. Med. 2000, 248, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Arnold, S.V.; de Lemos, J.A.; Zheng, L.; Rosenson, R.S.; Ballantyne, C.M.; Alam, S.; Bhatt, D.L.; Cannon, C.P.; Kosiborod, M. Use of optimal medical therapy in patients with diabetes and atherosclerotic cardiovascular disease: Insights from a prospective longitudinal cohort study. Diabetes Obes. Metab. 2023. [Google Scholar] [CrossRef] [PubMed]
- Dallavalasa, S.; Tulimilli, S.V.; Prakash, J.; Ramachandra, R.; Madhunapantula, S.V.; Veeranna, R.P. COVID-19: Diabetes Perspective—Pathophysiology and Management. Pathogens 2023, 12, 184. [Google Scholar]
- Conlon, K.C.; Miljkovic, M.D.; Waldmann, T.A. Cytokines in the Treatment of Cancer. J. Interferon Cytokine Res. 2019, 39, 6–21. [Google Scholar] [CrossRef] [Green Version]
- Starosz, A.; Jamiołkowska-Sztabkowska, M.; Głowińska-Olszewska, B.; Moniuszko, M.; Bossowski, A.; Grubczak, K. Immunological balance between Treg and Th17 lymphocytes as a key element of type 1 diabetes progression in children. Front. Immunol. 2022, 13, 958430. [Google Scholar] [CrossRef]
- Besser, R.E.J.; Bell, K.J.; Couper, J.J.; Ziegler, A.-G.; Wherrett, D.K.; Knip, M.; Speake, C.; Casteels, K.; Driscoll, K.A.; Jacobsen, L.; et al. ISPAD Clinical Practice Consensus Guidelines 2022: Stages of type 1 diabetes in children and adolescents. Pediatr. Diabetes 2022, 23, 1175–1187. [Google Scholar] [CrossRef]
- Chiang, J.L.; Maahs, D.M.; Garvey, K.C.; Hood, K.K.; Laffel, L.M.; Weinzimer, S.A.; Wolfsdorf, J.I.; Schatz, D. Type 1 Diabetes in Children and Adolescents: A Position Statement by the American Diabetes Association. Diabetes Care 2018, 41, 2026–2044. [Google Scholar] [CrossRef] [Green Version]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Wolfsdorf, J.I.; Glaser, N.; Agus, M.; Fritsch, M.; Hanas, R.; Rewers, A.; Sperling, M.A.; Codner, E. ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Pediatr. Diabetes 2018, 19, 155–177. [Google Scholar] [CrossRef]
- DiMeglio, L.A.; Acerini, C.L.; Codner, E.; Craig, M.E.; Hofer, S.E.; Pillay, K.; Maahs, D.M. ISPAD Clinical Practice Consensus Guidelines 2018: Glycemic control targets and glucose monitoring for children, adolescents, and young adults with diabetes. Pediatr. Diabetes 2018, 19, 105–114. [Google Scholar] [CrossRef] [Green Version]
- Nunes, R. Citocinas de resposta Th1 e Th2 e diabetes mellitus tipo 1. Th1 Th2 Response Cytokins Type 1 Diabetes Mellit. 2017, 49, 359–364. [Google Scholar] [CrossRef]
- Ding, J.T.; Yang, K.P.; Lin, K.L.; Cao, Y.K.; Zou, F. Mechanisms and therapeutic strategies of immune checkpoint molecules and regulators in type 1 diabetes. Front. Endocrinol. 2022, 13, 1090842. [Google Scholar] [CrossRef] [PubMed]
- Ghoneum, M.H.; Gimzewski, J.K.; Ghoneum, A.D.; Agrawal, S. Potential role of MRN-100, an iron-based compound, in upregulating production of cytokine IL-10 in human dendritic cells to promote an anti-inflammatory response in vitro. Int. J. Immunopathol. Pharmacol. 2019, 33, 2058738419844932. [Google Scholar] [CrossRef] [PubMed]
- Seyfarth, J.; Fortsch, K.; Ahlert, H.; Laws, H.J.; Karges, B.; Deenen, R.; Kohrer, K.; Mayatepek, E.; Meissner, T.; Jacobsen, M. Dominant TNFalpha and impaired IL-2 cytokine profiles of CD4(+) T cells from children with type-1 diabetes. Immunol. Cell Biol. 2017, 95, 630–639. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Zhong, T.; Yan, X.; Xie, Y.T.; He, B.B.; Li, X.; Zhou, Z.G. The relation between residual β-cell function and autoimmune status in long-term type 1 diabetes patients. Zhonghua Yi Xue Za Zhi 2022, 102, 1209–1215. [Google Scholar] [CrossRef] [PubMed]
- Boks, M.A.; Kager-Groenland, J.R.; Mousset, C.M.; van Ham, S.M.; ten Brinke, A. Inhibition of TNF receptor signaling by anti-TNFalpha biologicals primes naive CD4(+) T cells towards IL-10(+) T cells with a regulatory phenotype and function. Clin. Immunol. 2014, 151, 136–145. [Google Scholar] [CrossRef]
- Boks, M.A.; Kager-Groenland, J.R.; van Ham, S.M.; ten Brinke, A. IL-10/IFNgamma co-expressing CD4(+) T cells induced by IL-10 DC display a regulatory gene profile and downmodulate T cell responses. Clin. Immunol. 2016, 162, 91–99. [Google Scholar] [CrossRef]
- Kyriacou, A.; Melson, E.; Chen, W.; Kempegowda, P. Is immune checkpoint inhibitor-associated diabetes the same as fulminant type 1 diabetes mellitus? Clin. Med. 2020, 20, 417–423. [Google Scholar] [CrossRef]
- Cnop, M.; Welsh, N.; Jonas, J.C.; Jörns, A.; Lenzen, S.; Eizirik, D.L. Mechanisms of pancreatic beta-cell death in type 1 and type 2 diabetes: Many differences, few similarities. Diabetes 2005, 54, S97–S107. [Google Scholar] [CrossRef] [Green Version]
- Lu, J.; Liu, J.; Li, L.; Lan, Y.; Liang, Y. Cytokines in type 1 diabetes: Mechanisms of action and immunotherapeutic targets. Clin. Transl. Immunol. 2020, 9, e1122. [Google Scholar] [CrossRef]
- Rickels, M.R.; Evans-Molina, C.; Bahnson, H.T.; Ylescupidez, A.; Nadeau, K.J.; Hao, W.; Clements, M.A.; Sherr, J.L.; Pratley, R.E.; Hannon, T.S.; et al. High residual C-peptide likely contributes to glycemic control in type 1 diabetes. J. Clin. Invest. 2020, 130, 1850–1862. [Google Scholar] [CrossRef] [Green Version]
- Robert, S.; Gysemans, C.; Takiishi, T.; Korf, H.; Spagnuolo, I.; Sebastiani, G.; Van Huynegem, K.; Steidler, L.; Caluwaerts, S.; Demetter, P.; et al. Oral delivery of glutamic acid decarboxylase (GAD)-65 and IL10 by Lactococcus lactis reverses diabetes in recent-onset NOD mice. Diabetes 2014, 63, 2876–2887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, C.; Zhang, L.; Chen, Y.; Lin, X.; Li, T. Protective role of adenovirus vector-mediated interleukin-10 gene therapy on endogenous islet β-cells in recent-onset type 1 diabetes in NOD mice. Exp. Ther. Med. 2016, 11, 1625–1632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, J.; Tan, Q.; Tai, N.; Pearson, J.A.; Li, Y.; Chao, C.; Zhang, L.; Peng, J.; Xing, Y.; Zhang, L.; et al. IL-10 Deficiency Accelerates Type 1 Diabetes Development via Modulation of Innate and Adaptive Immune Cells and Gut Microbiota in BDC2.5 NOD Mice. Front. Immunol. 2021, 12, 702955. [Google Scholar] [CrossRef]
- Rapoport, M.J.; Mor, A.; Vardi, P.; Ramot, Y.; Winker, R.; Hindi, A.; Bistritzer, T. Decreased secretion of Th2 cytokines precedes Up-regulated and delayed secretion of Th1 cytokines in activated peripheral blood mononuclear cells from patients with insulin-dependent diabetes mellitus. J. Autoimmun. 1998, 11, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Kleffel, S.; Vergani, A.; Tezza, S.; Ben Nasr, M.; Niewczas, M.A.; Wong, S.; Bassi, R.; D'Addio, F.; Schatton, T.; Abdi, R.; et al. Interleukin-10+ regulatory B cells arise within antigen-experienced CD40+ B cells to maintain tolerance to islet autoantigens. Diabetes 2015, 64, 158–171. [Google Scholar] [CrossRef] [Green Version]
- Wogensen, L.; Lee, M.S.; Sarvetnick, N. Production of interleukin 10 by islet cells accelerates immune-mediated destruction of beta cells in nonobese diabetic mice. J. Exp. Med. 1994, 179, 1379–1384. [Google Scholar] [CrossRef] [Green Version]
- Moritani, M.; Yoshimoto, K.; Tashiro, F.; Hashimoto, C.; Miyazaki, J.; Ii, S.; Kudo, E.; Iwahana, H.; Hayashi, Y.; Sano, T.; et al. Transgenic expression of IL-10 in pancreatic islet A cells accelerates autoimmune insulitis and diabetes in non-obese diabetic mice. Int. Immunol. 1994, 6, 1927–1936. [Google Scholar] [CrossRef]
- Rabinovitch, A.; Suarez-Pinzon, W.L. Roles of cytokines in the pathogenesis and therapy of type 1 diabetes. Cell Biochem. Biophys. 2007, 48, 159–163. [Google Scholar] [CrossRef]
- Nikolic, T.; Suwandi, J.S.; Wesselius, J.; Laban, S.; Joosten, A.M.; Sonneveld, P.; Mul, D.; Aanstoot, H.J.; Kaddis, J.S.; Zwaginga, J.J.; et al. Tolerogenic dendritic cells pulsed with islet antigen induce long-term reduction in T-cell autoreactivity in type 1 diabetes patients. Front. Immunol. 2022, 13, 1054968. [Google Scholar] [CrossRef]
- Iglesias, M.; Arun, A.; Chicco, M.; Lam, B.; Talbot, C.C., Jr.; Ivanova, V.; Lee, W.P.A.; Brandacher, G.; Raimondi, G. Type-I Interferons Inhibit Interleukin-10 Signaling and Favor Type 1 Diabetes Development in Nonobese Diabetic Mice. Front. Immunol. 2018, 9, 1565. [Google Scholar] [CrossRef]
- Germini, D.E.; Franco, M.I.F.; Fonseca, F.L.A.; de Sousa Gehrke, F.; da Costa Aguiar Alves Reis, B.; Cardili, L.; Oshima, C.T.F.; Theodoro, T.R.; Waisberg, J. Association of expression of inflammatory response genes and DNA repair genes in colorectal carcinoma. Tumour Biol. 2019, 42, 1010428319843042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quiros, M.; Nishio, H.; Neumann, P.A.; Siuda, D.; Brazil, J.C.; Azcutia, V.; Hilgarth, R.; O'Leary, M.N.; Garcia-Hernandez, V.; Leoni, G.; et al. Macrophage-derived IL-10 mediates mucosal repair by epithelial WISP-1 signaling. J. Clin. Investig. 2017, 127, 3510–3520. [Google Scholar] [CrossRef] [Green Version]
- Ramalho, T.; Filgueiras, L.; Silva-Jr, I.A.; Pessoa, A.F.M.; Jancar, S. Impaired wound healing in type 1 diabetes is dependent on 5-lipoxygenase products. Sci. Rep. 2018, 8, 14164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Green, E.A.; Flavell, R.A. The temporal importance of TNFalpha expression in the development of diabetes. Immunity 2000, 12, 459–469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, J.; Haskins, K. Pathogenicity of T helper 2 T-cell clones from T-cell receptor transgenic non-obese diabetic mice is determined by tumour necrosis factor-alpha. Immunology 2008, 123, 108–117. [Google Scholar] [CrossRef]
- Koulmanda, M.; Bhasin, M.; Awdeh, Z.; Qipo, A.; Fan, Z.; Hanidziar, D.; Putheti, P.; Shi, H.; Csizuadia, E.; Libermann, T.A.; et al. The role of TNF-alpha in mice with type 1- and 2- diabetes. PLoS One 2012, 7, e33254. [Google Scholar] [CrossRef] [Green Version]
- Lee, L.F.; Xu, B.; Michie, S.A.; Beilhack, G.F.; Warganich, T.; Turley, S.; McDevitt, H.O. The role of TNF-alpha in the pathogenesis of type 1 diabetes in the nonobese diabetic mouse: Analysis of dendritic cell maturation. Proc. Natl. Acad. Sci. USA 2005, 102, 15995–16000. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christen, U.; Wolfe, T.; Möhrle, U.; Hughes, A.C.; Rodrigo, E.; Green, E.A.; Flavell, R.A.; von Herrath, M.G. A dual role for TNF-alpha in type 1 diabetes: Islet-specific expression abrogates the ongoing autoimmune process when induced late but not early during pathogenesis. J. Immunol. 2001, 166, 7023–7032. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.D.; Tisch, R.; Singer, S.M.; Cao, Z.A.; Liblau, R.S.; Schreiber, R.D.; McDevitt, H.O. Effect of tumor necrosis factor alpha on insulin-dependent diabetes mellitus in NOD mice. I. The early development of autoimmunity and the diabetogenic process. J. Exp. Med. 1994, 180, 995–1004. [Google Scholar] [CrossRef] [Green Version]
- Wang, G.; Yan, Y.; Xu, N.; Yin, D.; Hui, Y. Treatment of type 1 diabetes by regulatory T-cell infusion via regulating the expression of inflammatory cytokines. J. Cell. Biochem. 2019, 120, 19338–19344. [Google Scholar] [CrossRef] [PubMed]
- Hamouda, L.; Miliani, M.; Hadjidj, Z.; Messali, R.; Aribi, M. Rituximab Treatment Modulates the Release of Hydrogen Peroxide and the Production of Pro-inflammatory Cytokines by Monocyte at the Onset of Type 1 Diabetes. Endocr. Metab. Immune Disord. Drug Targets 2019, 19, 643–655. [Google Scholar] [CrossRef] [PubMed]
- Dib, S.A. Heterogeneity of type 1 diabetes mellitus. Arq. Bras. de Endocrinol. Metabol. 2008, 52, 205–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Couper, J.J.; Haller, M.J.; Greenbaum, C.J.; Ziegler, A.G.; Wherrett, D.K.; Knip, M.; Craig, M.E. ISPAD Clinical Practice Consensus Guidelines 2018: Stages of type 1 diabetes in children and adolescents. Pediatr. Diabetes 2018, 19, 20–27. [Google Scholar] [CrossRef]
- Bergamin, C.S.; Dib, S.A. Enterovirus and type 1 diabetes: What is the matter? World J. Diabetes 2015, 6, 828–839. [Google Scholar] [CrossRef]
| Parameters | T1DM n = 77 | Controls n = 30 | p-Value |
|---|---|---|---|
| Age (years) | 13.0 (3.8) | 12.6 (3.8) | 0.600 |
| Female, n (%) | 33 (42.9) | 17 (56.7) | 0.200 |
| z-Height | 0.15 (1.0) | 0.57 (1.1) | 0.060 |
| z-BMI (kg/m2) | 0.49 (0.9) | 0.85 (1.1) | 0.900 |
| FPG (ng/dL) | 210 (134) | 83.9 (5.7) | <0.001 |
| HbA1c (%) | 9.0 (2.3) | 4.9 (0.3) | <0.001 |
| C-peptide (nmol/L) | 0.32 (0.5) | 2.34 (0.8) | <0.001 |
| Group 1 (TDM1) n = 15 | Group 2 n = 32 | Group 3 n = 30 | Controls n = 30 | p-Value | |
|---|---|---|---|---|---|
| Age (years) | 10.1 (4.0) a | 13.5 (2.9) b | 13.8 (4.0) b | 12.6 (3.8) | 0.0100 * |
| Female, n (%) | 7 (46.7) | 17 (53.1) | 9 (30.0) | 17 (56.7) | 0.850 |
| z-Height | 0.13 (1.3) | 0.09 (1.0) | 0.22 (0.9) | 0.58 (1.1) | 0.290 |
| z-BMI (Kg/m2) | 0.11 (1.29) | 0.53 (0.9) | 0.59 (0.94) | 0.85 (1.14) | 0.160 |
| Age of diagnosis of TDM1 (months) | 94.6 (41.10) | 98.7 (38) | 97.3 (41.9) | 0.940 | |
| TDM1 diagnostic time (months) | 27.0 (39.5) a | 65.9 (38.1) b | 67.0 (61.9) b | 0.005 † | |
| FPG (ng/dL) | 389.2 (127.5) a | 190.8 (111.5) b | 141.4 (65.5) b | 83.9 (5.7) c | <0.001 † |
| Basal HbA1c (%) | 11.8 (2.1) a | 9.7 (1.5) b | 6.8 (0.8) c | 4.9 (0.4) d | <0.001 † |
| Mean HbA1c (%) | 10.3 (2.3) a | 9.3 (1.3) a | 7.1 (1.2) b | <0.001 † | |
| C-Peptide (nmol/L) | 0.31 (0.2) a | 0.15 (0.2) b | 0.45 (0.7) b | 2.23 (0.8) c | < 0.001 † |
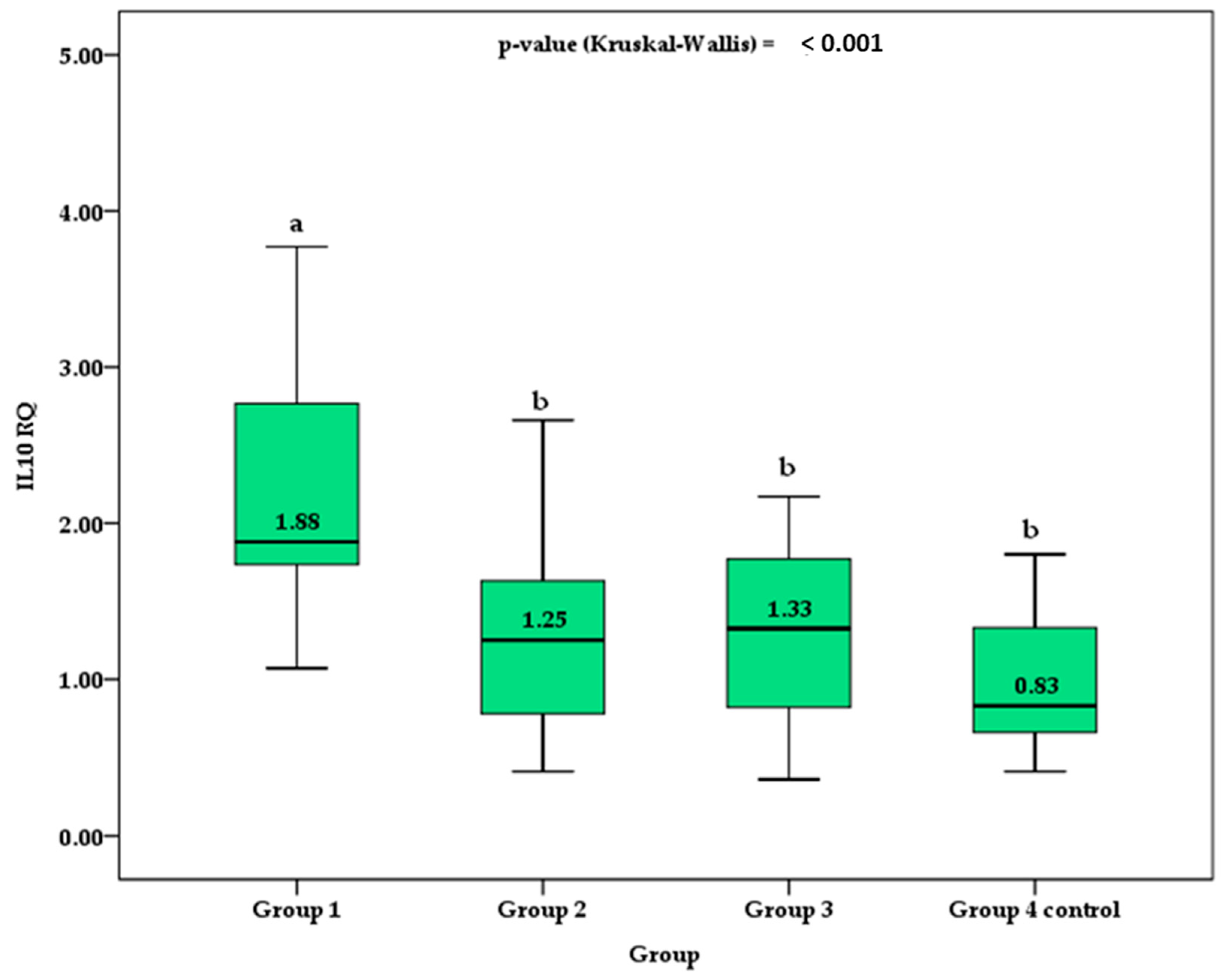
| IL10 RQ | 2.63 (1.62) a | 1.3 (0.62) b | 1.30 (0.53) b | 1.05 (0.67) b | <0.001 † |
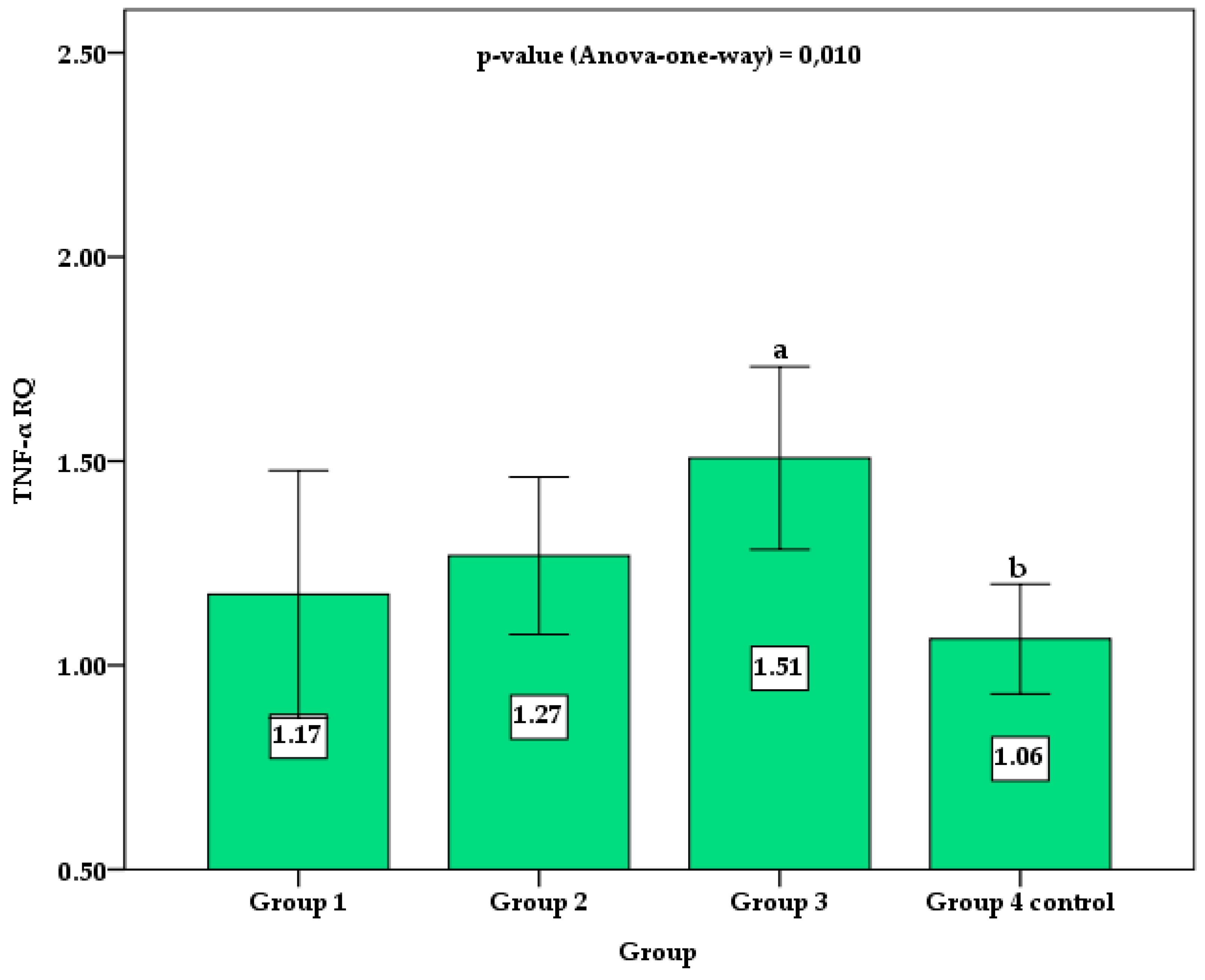
| TNF-α RQ | 1.17 (0.55) | 1.27 (0.53) | 1.50 (0.53) a | 1.06 (0.36) b | 0.010 * |
| IL10 RQ | TNF RQ | |||
|---|---|---|---|---|
| r | p-Value | r | p-Value | |
| Age (years) | −0.248 | 0.029 * | 0.29 | 0.010 * |
| Diagnostic time (months) | −0.238 | 0.036 * | 0.158 | 0.170 |
| z-BMI kg/m2 | −0.094 | 0.421 | −0.002 | 0.986 |
| Fasting blood glucose (mg/dL) | 0.272 | 0.016 * | −0.152 | 0.186 |
| % HbA1c | 0.226 | 0.048 * | −0.174 | 0.129 |
| C-Peptide | 0.247 | 0.069 | 0.063 | 0.648 |
| Gender (1 = male; 2 = female) | −0.089 | 0.441 | −0.096 | 0.405 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
dos Santos Haber, J.F.; Barbalho, S.M.; Sgarbi, J.A.; de Argollo Haber, R.S.; de Labio, R.W.; Laurindo, L.F.; Chagas, E.F.B.; Payão, S.L.M. The Relationship between Type 1 Diabetes Mellitus, TNF-α, and IL-10 Gene Expression. Biomedicines 2023, 11, 1120. https://doi.org/10.3390/biomedicines11041120
dos Santos Haber JF, Barbalho SM, Sgarbi JA, de Argollo Haber RS, de Labio RW, Laurindo LF, Chagas EFB, Payão SLM. The Relationship between Type 1 Diabetes Mellitus, TNF-α, and IL-10 Gene Expression. Biomedicines. 2023; 11(4):1120. https://doi.org/10.3390/biomedicines11041120
Chicago/Turabian Styledos Santos Haber, Jesselina Francisco, Sandra Maria Barbalho, Jose Augusto Sgarbi, Rafael Santos de Argollo Haber, Roger William de Labio, Lucas Fornari Laurindo, Eduardo Federighi Baisi Chagas, and Spencer Luiz Marques Payão. 2023. "The Relationship between Type 1 Diabetes Mellitus, TNF-α, and IL-10 Gene Expression" Biomedicines 11, no. 4: 1120. https://doi.org/10.3390/biomedicines11041120
APA Styledos Santos Haber, J. F., Barbalho, S. M., Sgarbi, J. A., de Argollo Haber, R. S., de Labio, R. W., Laurindo, L. F., Chagas, E. F. B., & Payão, S. L. M. (2023). The Relationship between Type 1 Diabetes Mellitus, TNF-α, and IL-10 Gene Expression. Biomedicines, 11(4), 1120. https://doi.org/10.3390/biomedicines11041120







