Correlation of Shear Bond Strength and Degree of Conversion in Conventional and Self-Adhesive Systems Used in Orthodontic Bonding Procedures
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Size
2.2. Sample Preparation
2.3. Tooth Mounting
2.4. Bonding Procedure
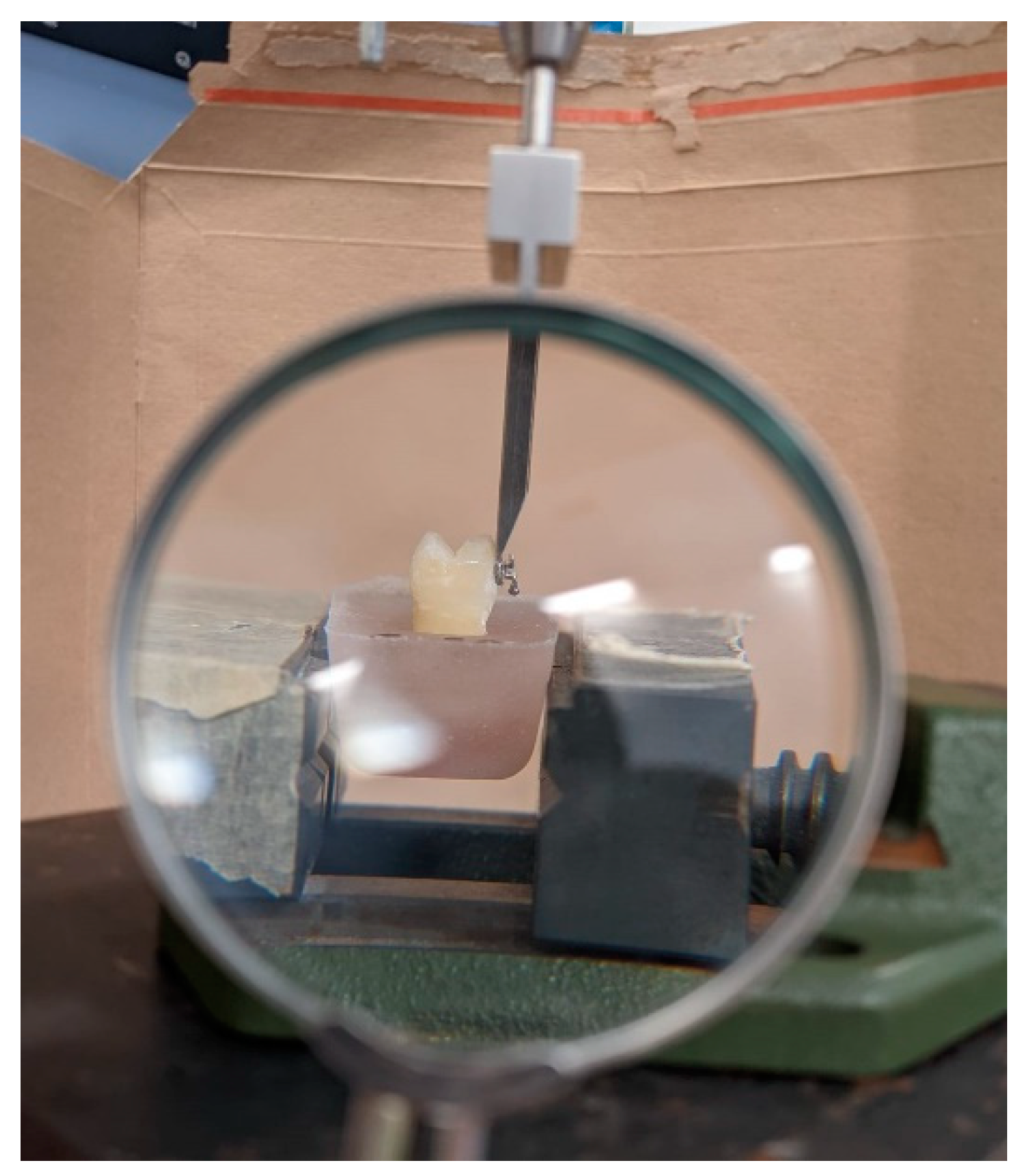
2.5. Shear Bond Strength Testing (SBS)
2.6. Adhesive Remnant Index (ARI)
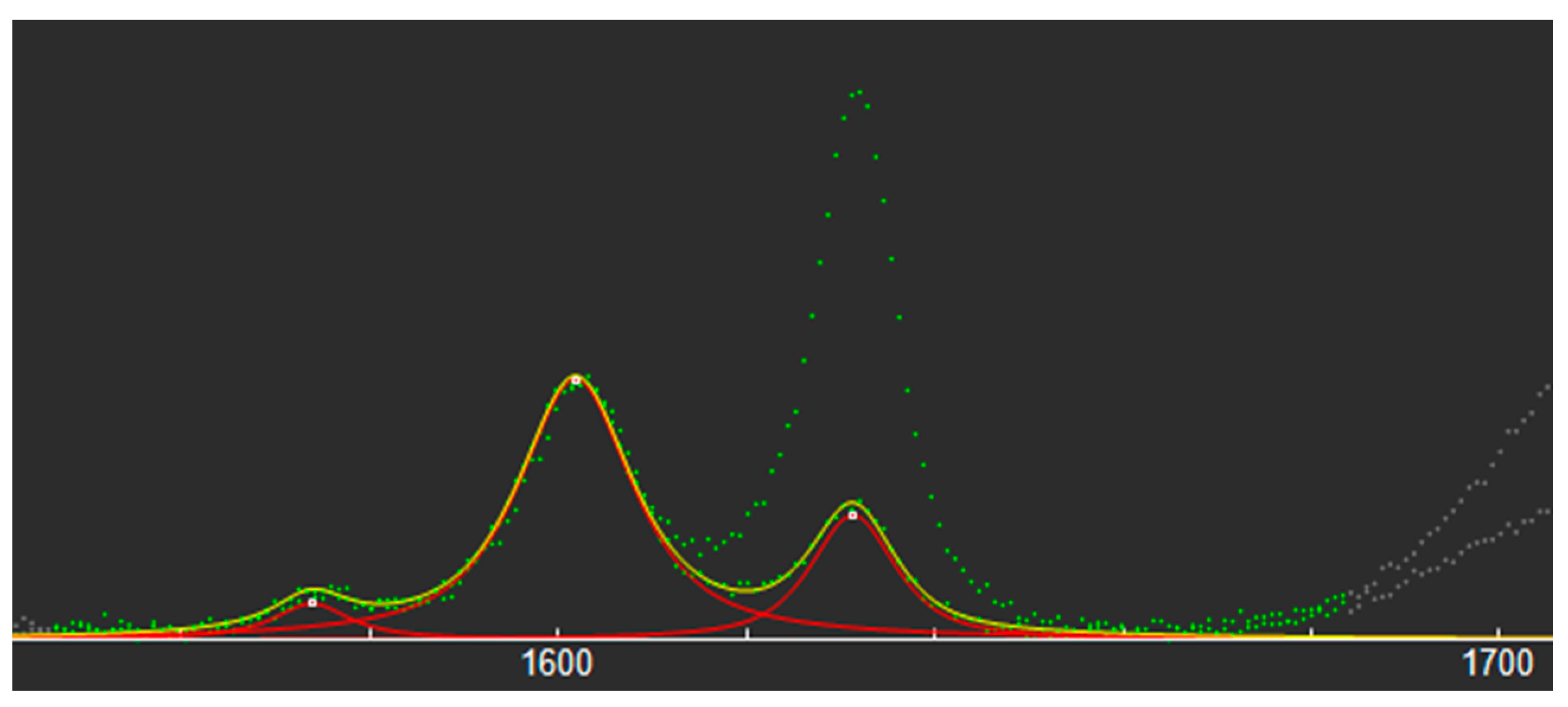
2.7. Degree of Conversion (DC)
2.8. Data Analyses
3. Results
3.1. SBS
3.2. ARI Scores
3.3. DC
3.4. Correalation
3.5. DC in Three Points
4. Discussion
5. Conclusions
- No difference was found in SBS values between the conventional and self-adhesive systems used in orthodontics. The self-adhesive systems can be used as a good alternative as they reduce clinical steps.
- The self-adhesive system demonstrated a higher DC compared to the conventional system.
- No significant difference was found in the adhesive remnant index score between the two materials.
- There is an overall very weak or moderate correlation between the DC and SBS values in the self-adhesive system. The DC has minimal effect on the SBS.
- The polymerization was equally effective both in the points closer to and further from the light-curing unit.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aguirre, M.J.; King, G.J.; Waldron, J.M. Assessment of bracket placement and bond strength when comparing direct bonding to indirect bonding techniques. Am. J. Orthod. 1982, 82, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Thiyagarajah, S.; Spary, D.J.; Rock, W.P. A clinical comparison of bracket bond failures in association with direct and indirect bonding. J. Orthod. 2006, 33, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Read, M.J.F.; O’Brien, K.D. A clinical trial of an indirect bonding technique with a visible light-cured adhesive. Am. J. Orthod. Dentofac. Orthop. 1990, 98, 259–262. [Google Scholar] [CrossRef] [PubMed]
- Newman George V Epoxy adhesives for orthodontic attachments: Progress report. Am. J. Orthod. 1965, 51, 901–912. [CrossRef] [PubMed]
- Costa, A.R.; Correr, A.B.; Puppin-Rontani, R.M.; Vedovello, S.A.; Valdrighi, H.C.; Correr-Sobrinho, L.; Vedovello Filho, M. Effect of bonding material, etching time and silane on the bond strength of metallic orthodontic brackets to ceramic. Braz. Dent. J. 2012, 23, 223–227. [Google Scholar] [CrossRef]
- Bishara, S.E.; Vonwald, L.; Olsen, M.E. Effect of time on the shear bond strength of glass ionomer and. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 616–620. [Google Scholar] [CrossRef]
- Tavas, M.A.; Watts, D.C. Bonding of orthodontic brackets by transillumination of a light activated composite: An in vitro study. Br. J. Orthod. 1979, 6, 207–208. [Google Scholar] [CrossRef]
- Aljubouri, Y.D.; Millett, D.T.; Gilmour, W.H. Six and 12 months’ evaluation of a self-etching primer versus two-stage etch and prime for orthodontic bonding: A randomized clinical trial. Eur. J. Orthod. 2004, 26, 565–571. [Google Scholar] [CrossRef]
- Banks, P.; Thiruvenkatachari, B. Long-term clinical evaluation of bracket failure with a self-etching primer: A randomized controlled trial. J. Orthod. 2007, 34, 243–251. [Google Scholar] [CrossRef]
- Elekdag-Turk, S.; Isci, D.; Turk, T.; Cakmak, F. Six-month bracket failure rate evaluation of a self-etching primer. Eur. J. Orthod. 2008, 30, 211–216. [Google Scholar] [CrossRef]
- Al-Saleh, M.; El-Mowafy, O. Bond strength of orthodontic brackets with new self-adhesive resin cements. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 528–533. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.H.; Ou, K.L.; Dong, D.R.; Huang, H.M.; Tsai, H.H.; Wang, W.N. Orthodontic bonding with self-etching primer and self-adhesive systems. Eur. J. Orthod. 2011, 33, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, I.R.; von Fraunhofer, J.A. Direct Bonding of Orthodontic Brackets—A comparative study of adhesives. Br. J. Orthod. 1976, 3, 143–146. [Google Scholar] [CrossRef]
- Al-Hity, R.; Gustin, M.P.; Bridel, N.; Morgon, L.; Grosgogeat, B. In vitro orthodontic bracket bonding to porcelain. Eur. J. Orthod. 2012, 34, 505–511. [Google Scholar] [CrossRef]
- Rahiotis, C. Degree of cure and monomer leaching from orthodontic adhesive resins: In vitro and in vivo evidence. Semin. Orthod. 2010, 16, 266–273. [Google Scholar] [CrossRef]
- Wichai, W.; Nimcharoensuk, K.; Anuwongnukroh, N.; Dechkunakorn, S.; Roongrujimek, P. Degree of conversion of three light-cured orthodontic adhesives. Key Eng. Mater. 2018, 777, 577–581. [Google Scholar] [CrossRef]
- Çörekçi, B.; Malkoç, S.; Öztürk, B.; Gündüz, B.; Toy, E. Polymerization capacity of orthodontic composites analyzed by Fourier transform infrared spectroscopy. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 299–304. [Google Scholar] [CrossRef]
- Anne Rathbun, M.; Craig, R.G.; Hanks, C.T.; Filisko, F.E. Cytotoxicity of a BIS-GMA dental composite before and after leaching in organic solvents. J. Biomed. Mater. Res. 1991, 25, 443–457. [Google Scholar] [CrossRef]
- Thompson, L.R.; Miller, E.G.; Bowles, W.H. Materials Science: Leaching of Unpolymerized Materials from Orthodontic Bonding Resin. J. Dent. Res. 1982, 61, 989–992. [Google Scholar] [CrossRef]
- Henbest, N. Orthodontic Bracket Bond Strength and Resin Composite Adhesive; University of Missouri: Kansas City, MI, USA, 2013. [Google Scholar]
- Ponikvar, M.J. Effect of Delayed Polymerization Time and Bracket Manipulation on Orthodontic Bracket Bonding. ProQuest Diss. Master Thesis, University of Missouri-Kansas City, Kansas City, MO, USA, 2014; 63p. [Google Scholar]
- Årtun, J.; Bergland, S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am. J. Orthod. 1984, 85, 333–340. [Google Scholar] [CrossRef]
- Jia, L.; Stawarczyk, B.; Schmidlin, P.R.; Attin, T.; Wiegand, A. Effect of caries infiltrant application on shear bond strength of different adhesive systems to sound and demineralized enamel. J. Adhes. Dent. 2012, 14, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Mews, L.; Kern, M.; Ciesielski, R.; Fischer-Brandies, H.; Koos, B. Shear bond strength of orthodontic brackets to enamel after application of a caries infiltrant. Angle Orthod. 2015, 85, 645–650. [Google Scholar] [CrossRef] [PubMed]
- Gaur, A.; Maheshwari, S.; Verma, S.; Tariq, M. Effects of adhesion promoter on orthodontic bonding in fluorosed teeth: A scanning electron microscopy study. J. Orthod. Sci. 2016, 5, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, K.; Miyazaki, M.; Takamizawa, T.; Tsubota, K.; Rikuta, A. Influence of crosshead speed on micro-tensile bond strength of two-step adhesive systems. Dent. Mater. 2006, 22, 420–425. [Google Scholar] [CrossRef]
- Finnema, K.J.; Özcan, M.; Post, W.J.; Ren, Y.; Dijkstra, P.U. In-vitro orthodontic bond strength testing: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Asiri, A.A.; Khan, R.; Alzahrani, S.S.; Haider, S.; Khan, S.U. Comparative Analysis of the Shear Bond Strength of Flowable. Coatings 2021, 11, 273. [Google Scholar] [CrossRef]
- Bhattacharjee, D.; Sharma, K.; Sahu, R.; Neha, K.; Kumari, A.; Rai, A. Comparative Evaluation of Shear Bond Strength of Brackets Bonded with self Etch Primer/Adhesive and Conventional Etch/Primer and Adhesive System. J. Pharm. Bioallied Sci. 2021, 13, S1168–S1173. [Google Scholar] [CrossRef]
- Brauchli, L.; Steineck, M. Siloranes–suitability of a novel adhesive for orthodontic bracket bonding. Dent. J. 2021, 9, 135. [Google Scholar] [CrossRef]
- Naidu, E.; Stawarczyk, B.; Tawakoli, P.N.; Attin, R.; Attin, T.; Wiegand, A. Shear bond strength of orthodontic resins after caries infiltrant preconditioning. Angle Orthod. 2013, 83, 306–312. [Google Scholar] [CrossRef]
- Ekizer, A.; Zorba, Y.O.; Uysal, T.; Ayrikcil, S. Effects of demineralizaton-inhibition procedures on the bond strength of brackets bonded to demineralized enamel surface. Korean J. Orthod. 2012, 42, 17–22. [Google Scholar] [CrossRef]
- Costenoble, A.; Vennat, E.; Attal, J.P.; Dursun, E. Bond strength and interfacial morphology of orthodontic brackets bonded to eroded enamel treated with calcium silicate-sodium phosphate salts or resin infiltration. Angle Orthod. 2016, 86, 909–916. [Google Scholar] [CrossRef] [PubMed]
- VelI, I.; Akin, M.; Baka, Z.M.; Uysal, T. Effects of different pre-treatment methods on the shear bond strength of orthodontic brackets to demineralized enamel. Acta Odontol. Scand. 2015, 74, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Anicic, M.S.; Goracci, C.; Juloski, J.; Miletic, I.; Mestrovic, S. The influence of resin infiltration pretreatment on orthodontic bonding to demineralized human enamel. Appl. Sci. 2020, 10, 3619. [Google Scholar] [CrossRef]
- Khalil, A.S.; Tamish, N.M.; Elkalza, A.R. Assessment of chemical, ultrasonic, diode laser, and Er:YAG laser application on debonding of ceramic brackets. BMC Oral Health 2022, 22, 79. [Google Scholar] [CrossRef]
- Iglesias, A.; Flores, T.; Moyano, J.; Artés, M.; Gil, F.J.; Puigdollers, A. In vitro study of shear bond strength in direct and indirect bonding with three types of adhesive systems. Materials 2020, 13, 2644. [Google Scholar] [CrossRef]
- O’Brien, K.D.; Watts, D.C.; Read, M.J.F. Residual debris and bond strength-Is there a relationship? Am. J. Orthod. Dentofac. Orthop. 1988, 94, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Bishara, S.E.; VonWald, L.; Laffoon, J.F.; Warren, J.J. Effect of a self-etch primer/adhesive on the shear bond strength of orthodontic brackets. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 621–624. [Google Scholar] [CrossRef]
- Flores, T.; Mayoral, J.R.; Giner, L.; Puigdollers, A. Comparison of enamel-bracket bond strength using direct- and indirect-bonding techniques with a self-etching ion releasing S-PRG filler. Dent. Mater. J. 2015, 34, 41–47. [Google Scholar] [CrossRef]
- Bishara, S.E.; VonWald, L.; Laffoon, J.F.; Jakobsen, J.R. Effect of altering the type of enamel conditioner on the shear bond strength of a resin-reinforced glass ionomer adhesive. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 288–294. [Google Scholar] [CrossRef]
- Pianelli, C.; Devaux, J.; Bebelman, S.; Leloup, G. The micro-Raman spectroscopy, a useful tool to determine the degree of conversion of light-activated composite resins. J. Biomed. Mater. Res. 1999, 48, 675–681. [Google Scholar] [CrossRef]
- Gilchrist, F.; Santini, A.; Harley, K.; Deery, C. The use of micro-Raman spectroscopy to differentiate between sound and eroded primary enamel. Int. J. Paediatr. Dent. 2007, 17, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Imazato, S.; McCabe, J.F.; Tarumi, H.; Ehara, A.; Ebisu, S. Degree of conversion of composites measured by DTA and FTIR. Dent. Mater. 2001, 17, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Iliadi, A.; Baumgartner, S.; Athanasiou, A.E.; Eliades, T.; Eliades, G. Effect of intraoral aging on the setting status of resin composite and glass ionomer orthodontic adhesives. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 425–433. [Google Scholar] [CrossRef] [PubMed]
- de Sena, L.M.F.; Barbosa, H.A.M.; Caldas, S.G.F.R.; Ozcan, M.; Souza, R.O.d.A.E. Effect of different bonding protocols on degree of monomer conversion and bond strength between orthodontic brackets and enamel. Braz. Oral Res. 2018, 32, e58. [Google Scholar] [CrossRef]
- de Araujo, L.O.F.; Barreto, O.; de Mendonça, A.A.M.; França, R. Assessment of the degree of conversion in light-curing orthodontic resins with various viscosities. Appl. Adhes. Sci. 2015, 3, 3–9. [Google Scholar] [CrossRef]
- Ferracane, J.L.; Greener, E.H. The effect of resin formulation on the degree of conversion and mechanical properties of dental restorative resins. J. Biomed. Mater. Res. 1986, 20, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, B.; Bakkal, M.; Zengin Kurt, B. Structural and mechanical analysis of three orthodontic adhesive composites cured with different light units. J. Appl. Biomater. Funct. Mater. 2020, 18, 2280800020901716. [Google Scholar] [CrossRef] [PubMed]
| Name | Composition | Manufacturer |
|---|---|---|
| Transbond XT primer | Bis-GMA, TEGDMA, dimethylamono-bezenethanol, DL-camphorquinone, hydrochinone | 3M Unitek, Monrovia, CA, USA |
| Transbond XT Light Cure Adhesive | Silane-treated quartz, Bis-GMA, Bis-EMA, silane-treated silica, diphenyliodonium hexa-fluorophosphate | 3M Unitek, Monrovia, CA, USA |
| GC Ortho Connect | 7.7.9-trimethyl-4.13-dioxo-3.14-dioxa-5.12-diazahexadecane-1.16-diyl bismethacrylate | GC America, Alsip, Illinois, USA |
| Group | Number | SBS | ||||
|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Minimum | Maximum | Significance t-Test | ||
| I | 16 | 14.82 | 2.12 | 10.17 | 18.94 | p = 0.308 |
| II | 16 | 13.71 | 3.71 | 7.85 | 19.34 | |
| Group | Total Number of Cases | ARI | Significance Mann Whitney U Test | |||
|---|---|---|---|---|---|---|
| Score 0 (Number of Cases) | Score 1 (Number of Cases) | Score 2 (Number of Cases) | Score 3 (Number of Cases) | |||
| I | 16 | 0 | 15 | 1 | 0 | p = 0.968 |
| II | 16 | 2 | 11 | 2 | 1 | |
| Group | Number | SBS | ||||
|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Minimum | Maximum | Significance t-Test | ||
| I | 16 | 62.94 | 3.46 | 58.18 | 71.06 | p = 0.0000113 p < 0.01 |
| II | 16 | 73.68 | 7.08 | 52.54 | 83.32 | |
| Group I | Mean | Minimum | Maximum | SD | R |
|---|---|---|---|---|---|
| DC “Center” | 62.95 | 57.02 | 72.36 | 0.04 | 0.01 |
| DC “Near” | 65.30 | 55.85 | 96.65 | 0.09 | 0.1 |
| DC “Far” | 62.27 | 52.65 | 70.81 | 0.05 | 0.02 |
| Group II | Mean | Minimum | Maximum | SD | R |
|---|---|---|---|---|---|
| DC “Center” | 74.50 | 54.78 | 85.54 | 0.07 | 0.21 |
| DC “Near” | 70.71 | 51.84 | 82.38 | 0.08 | 0.41 |
| DC “Far” | 71.55 | 14.24 | 80.82 | 0.15 | 0.34 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perković, V.; Šimunović Aničić, M.; Lughi, V.; Pozzan, L.; Meštrović, S.; Turco, G. Correlation of Shear Bond Strength and Degree of Conversion in Conventional and Self-Adhesive Systems Used in Orthodontic Bonding Procedures. Biomedicines 2023, 11, 1252. https://doi.org/10.3390/biomedicines11051252
Perković V, Šimunović Aničić M, Lughi V, Pozzan L, Meštrović S, Turco G. Correlation of Shear Bond Strength and Degree of Conversion in Conventional and Self-Adhesive Systems Used in Orthodontic Bonding Procedures. Biomedicines. 2023; 11(5):1252. https://doi.org/10.3390/biomedicines11051252
Chicago/Turabian StylePerković, Vjera, Marina Šimunović Aničić, Vanni Lughi, Lucia Pozzan, Senka Meštrović, and Gianluca Turco. 2023. "Correlation of Shear Bond Strength and Degree of Conversion in Conventional and Self-Adhesive Systems Used in Orthodontic Bonding Procedures" Biomedicines 11, no. 5: 1252. https://doi.org/10.3390/biomedicines11051252
APA StylePerković, V., Šimunović Aničić, M., Lughi, V., Pozzan, L., Meštrović, S., & Turco, G. (2023). Correlation of Shear Bond Strength and Degree of Conversion in Conventional and Self-Adhesive Systems Used in Orthodontic Bonding Procedures. Biomedicines, 11(5), 1252. https://doi.org/10.3390/biomedicines11051252






