Brain-Derived Neurotrophic Factor (BDNF) in Mechanisms of Autistic-like Behavior in BTBR Mice: Crosstalk with the Dopaminergic Brain System
Abstract
1. Introduction
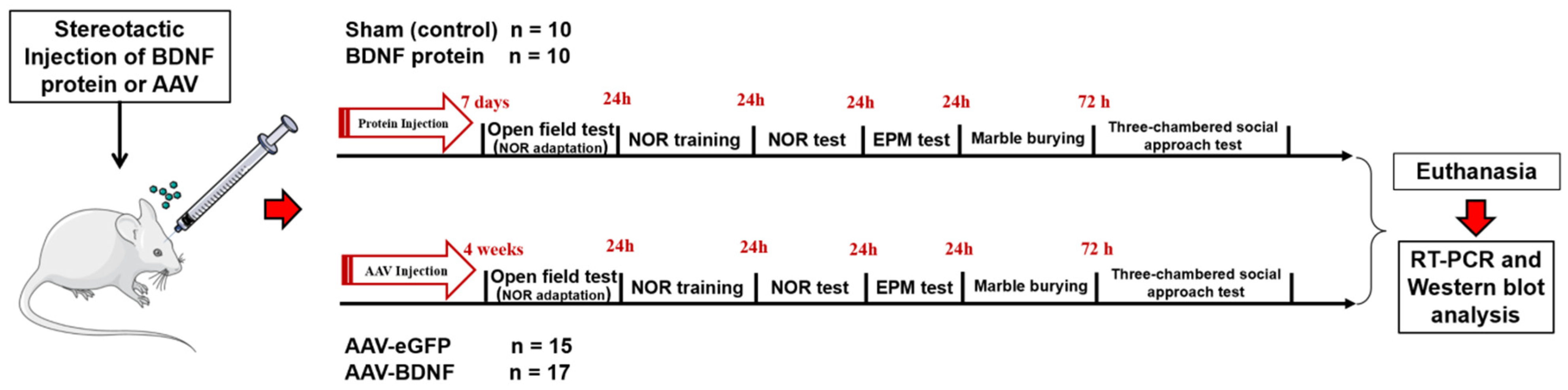
2. Materials and Methods
2.1. Animals
2.2. BDNF i.c.v Injection
2.3. A Cell Line
2.4. Production of rAAV Vectors
2.5. Stereotaxic Microinjections
2.6. Behavioral Testing
2.7. Excision of the Brain Structures
2.8. Reverse-Transcription Quantitative PCR
2.9. Western Blot
2.10. Fluorescence Microscopy of Mouse Brain Sections
2.11. Statistics
3. Results
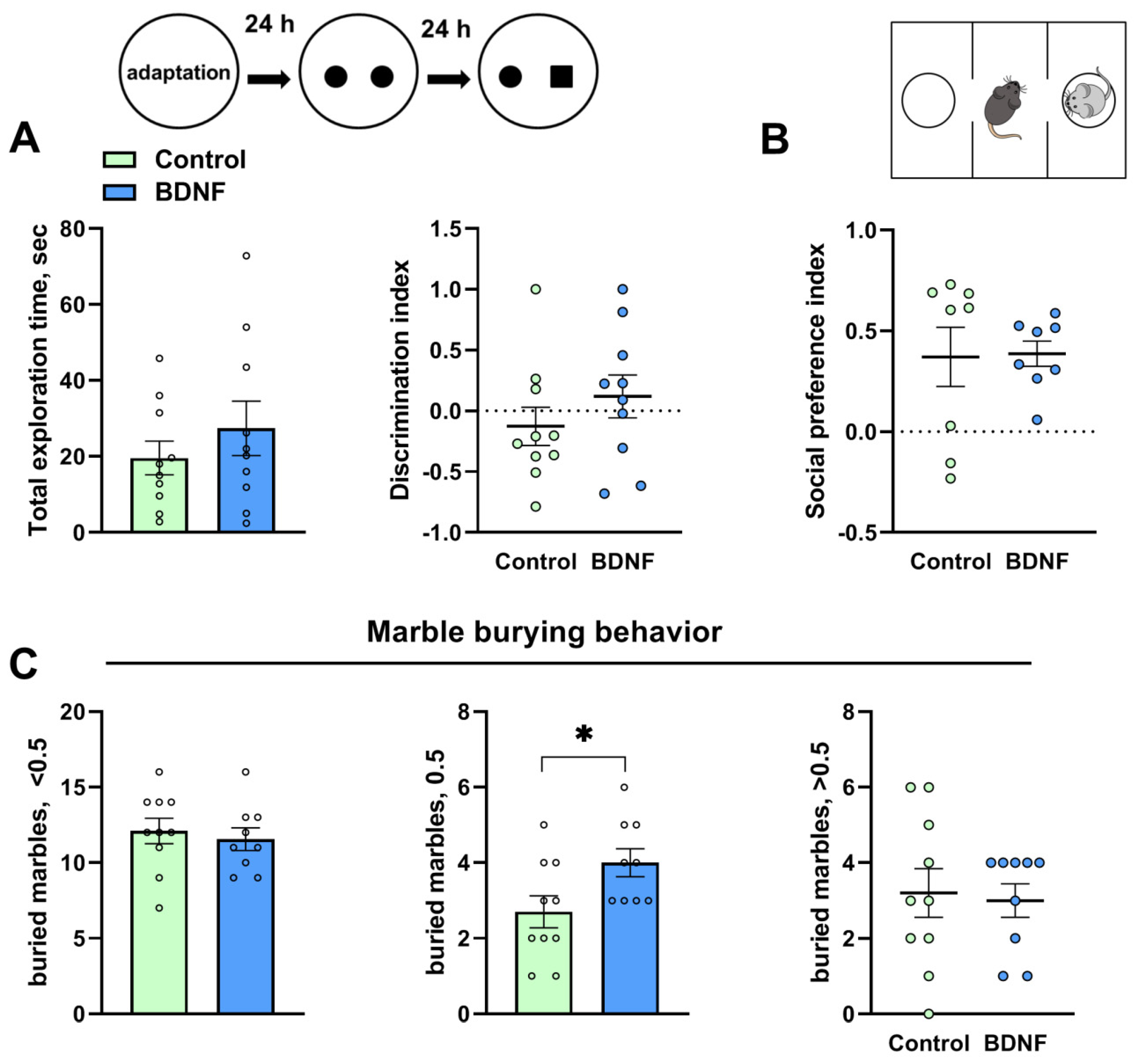
3.1. The i.c.v. Injection of BDNF Failed to Affect Behavior in BTBR Mice
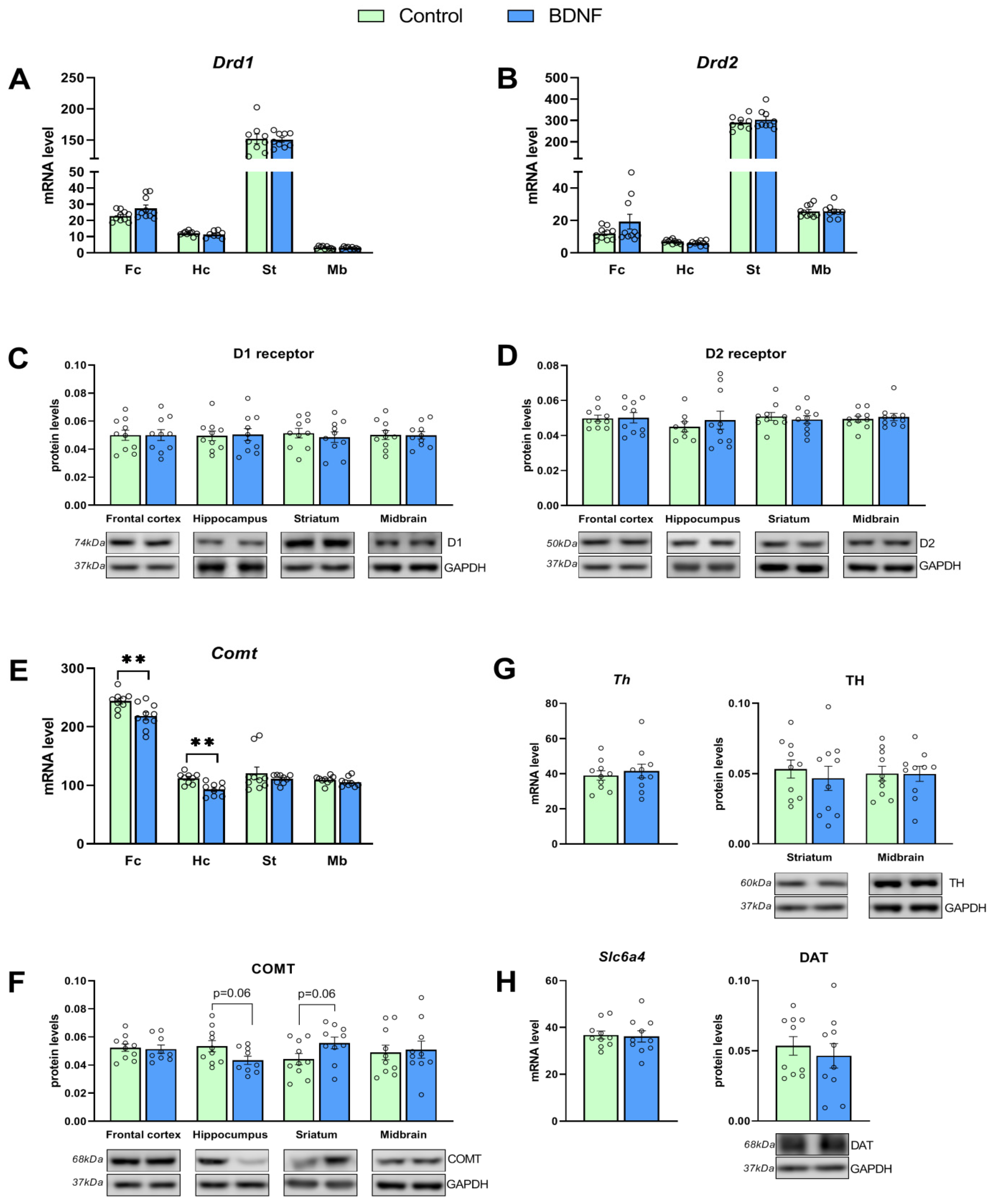
3.2. mRNA and Protein Levels of Key Genes of the DA System Are Changed by the i.c.v. Injection of BDNF
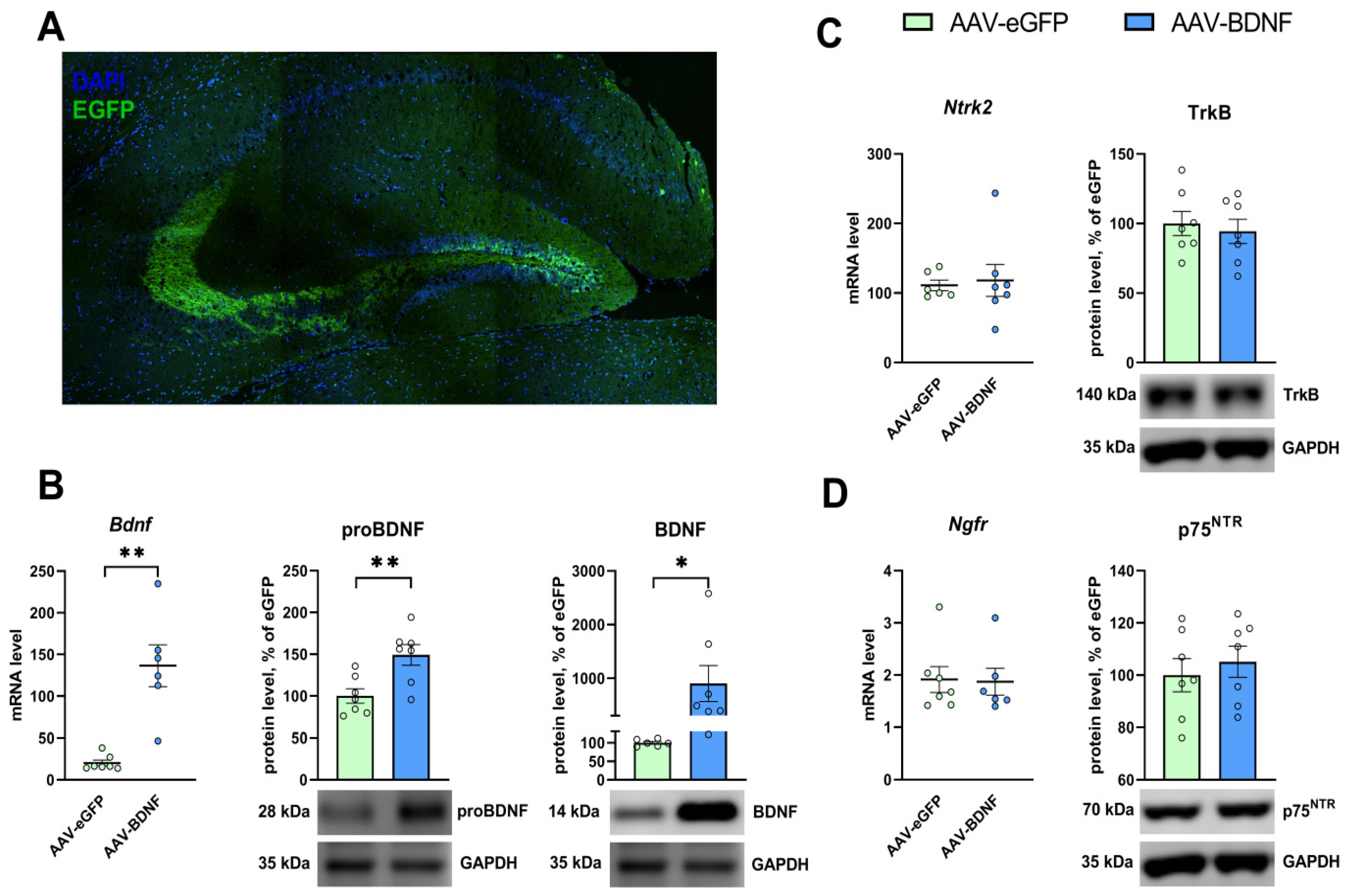
3.3. rAAV-Mediated Bdnf Gene Delivery Effectively Overexpresses BDNF in the Hippocampus of BTBR Mice
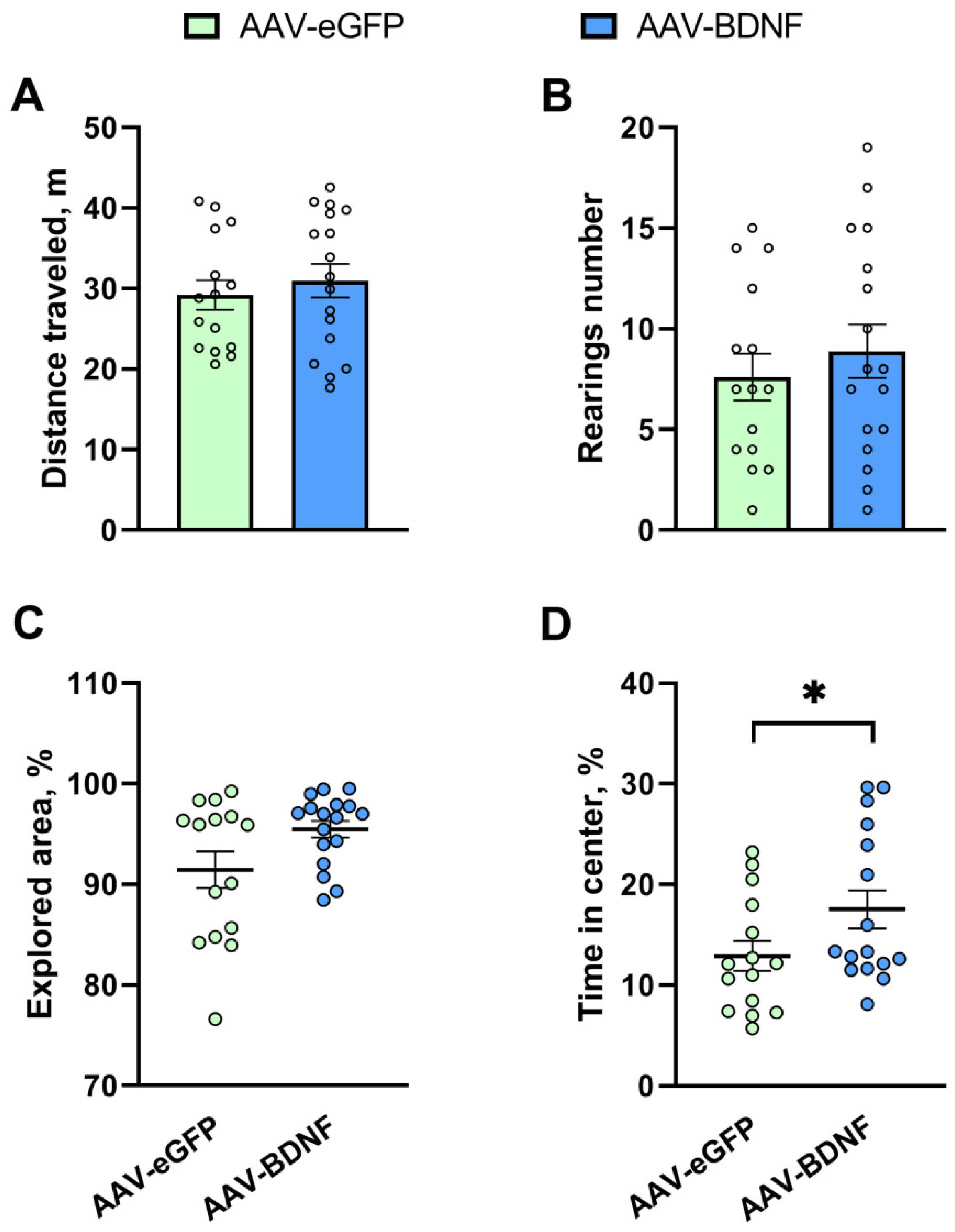
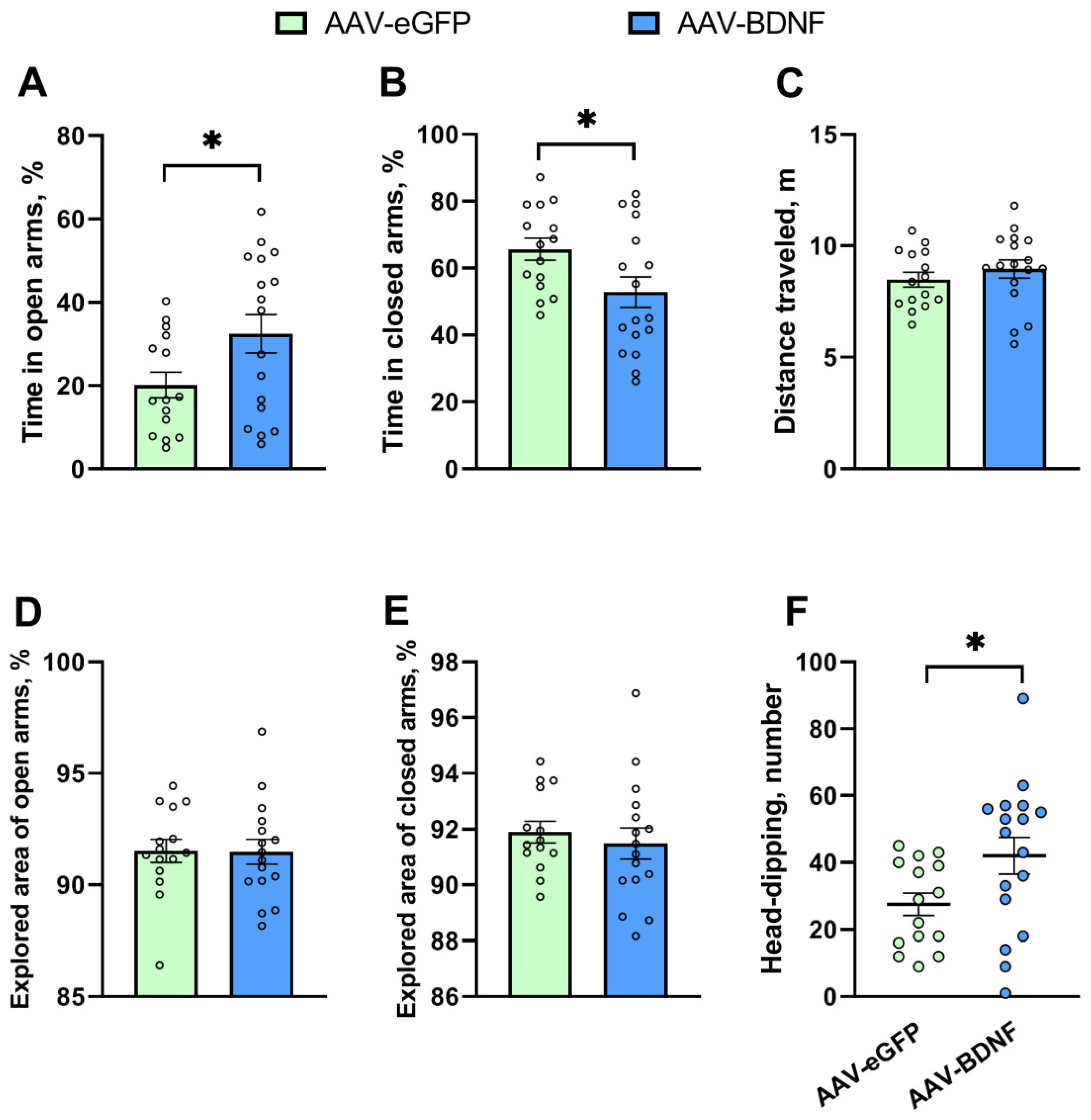
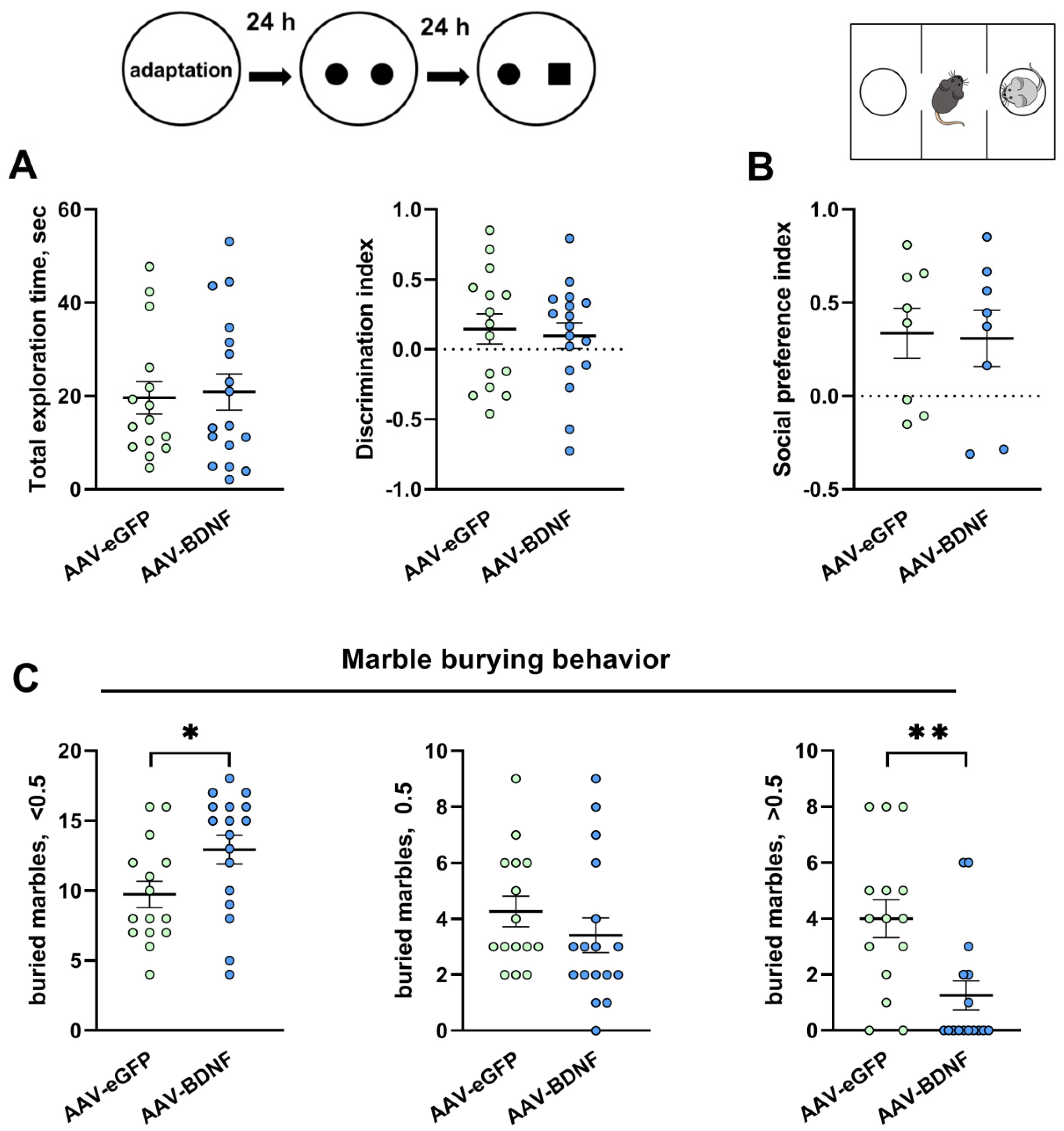
3.4. Hippocampal BDNF Overexpression Reduces Anxiety and Stereotypy in BTBR Mice
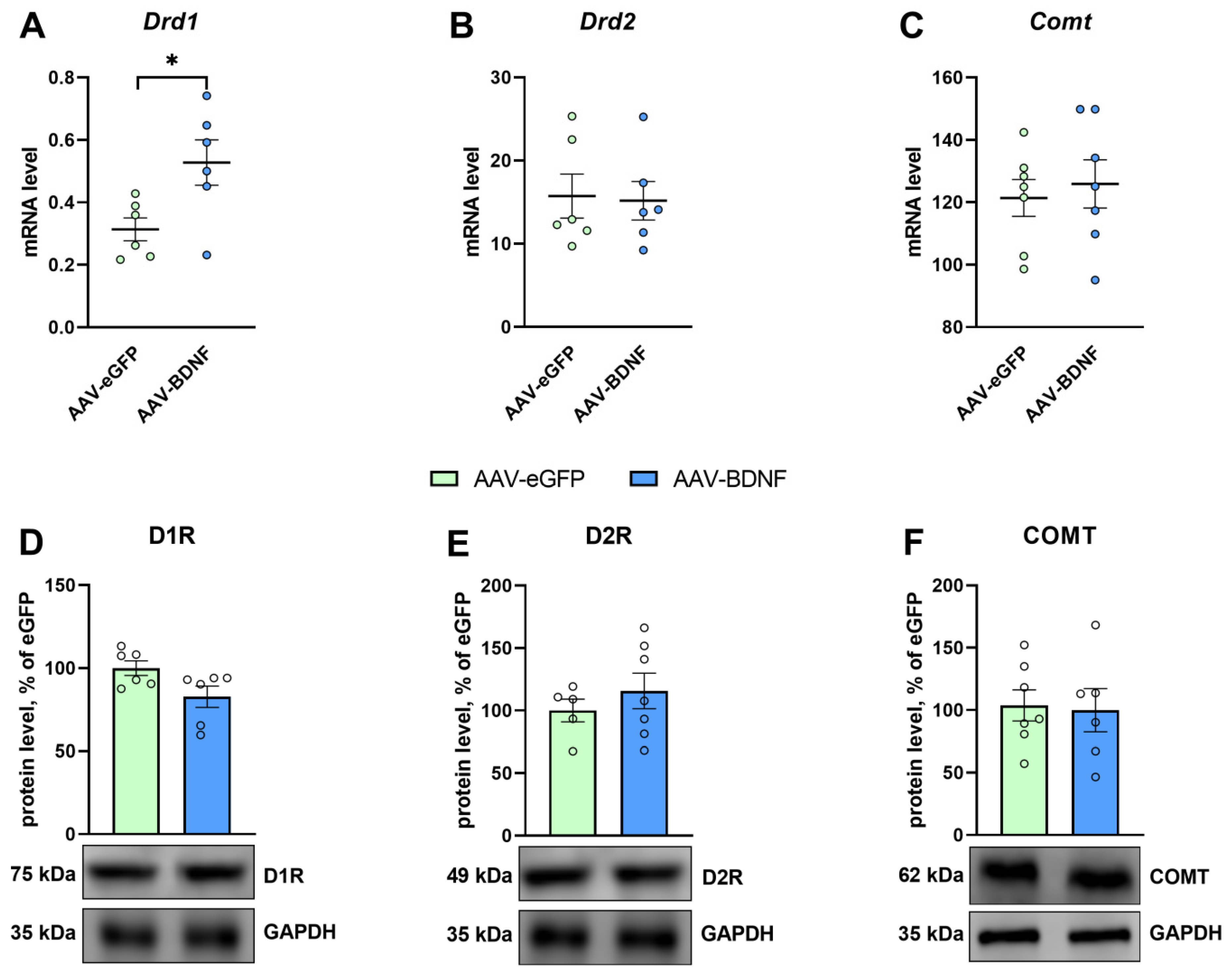
3.5. mRNA and Protein Levels in the Hippocampus after the AAV-BDNF Injection
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Target Gene | Primer Sequences | Annealing Temperature, °C | Amplicon Length, bp |
|---|---|---|---|
| rPol2 | F 5′-TGTGACAACTCCATACAATGC-3′ R 5′-CTCTCTTAGTGAATTTGCGTACT-3′ | 60 | 188 |
| Bdnf | F 5′-TGAAGCCACCTCTCTCAGTC-3′ R 5′-AGCAGTACTCTCAGGGCTAGG-3′ | 59 | 126 |
| Ngfr | F 5′-CTTGCTTCTGACCACCCTTCTC-3′ R 5′-GCTCCCTTCTCCTAGTGTCAAAC-3′ | 61 | 145 |
| Ntrk2 | F 5′-GTCGCTTTCTCTCCCTTTGG-3′ R 5′-GCATTGTTAGTTGTGGTGGGC-3′ | 60 | 277 |
| Drd1 | F 5′-GGAAACCCTGTCGAATGCTCTC-3′ R 5′-CCAGCCAAACCACACAAATACATCG-3′ | 64 | 222 |
| Drd2 | F 5′-TCCGCCACTTCTTGACATACATTG-3′ R 5′-CCCATCCACAGCCTCCTCTAAG-3′ | 65 | 203 |
| Th | F 5′-CCGTACACCCTGGCCATTGATG-3′ R 5′-ATGAAGGCCAGGAGGAATGCAGG-3′ | 64 | 320 |
| Slc6a3 | F 5′-TTCACTGTCATCCTCATCTCTTTC-3′ R 5′-TCAAAATACTCAGCAGCGGGTG-3′ | 63 | 224 |
| Comt |
F 5′-GACTTCCTGGCGTATGTGAG-3′ R 5′-AGAGTGAGTGTGTGTCATCG-3′ | 60 | 199 |
| Maoa |
F 5′-AATGAGGATGTTAAATGGGTAGATGTTGGT-3′ R 5′-CTTGACATATTCAACTAGACGCTC-3′ | 61 | 138 |
References
- Chiarotti, F.; Venerosi, A. Epidemiology of Autism Spectrum Disorders: A Review of Worldwide Prevalence Estimates Since 2014. Brain Sci. 2020, 10, 274. [Google Scholar] [CrossRef] [PubMed]
- Guang, S.; Pang, N.; Deng, X.; Yang, L.; He, F.; Wu, L.; Chen, C.; Yin, F.; Peng, J. Synaptopathology Involved in Autism Spectrum Disorder. Front. Cell. Neurosci. 2018, 12, 470. [Google Scholar] [CrossRef] [PubMed]
- Courchesne, E.; Gazestani, V.H.; Lewis, N.E. Prenatal Origins of ASD: The When, What, and How of ASD Development. Trends Neurosci. 2020, 43, 326–342. [Google Scholar] [CrossRef] [PubMed]
- Takumi, T.; Tamada, K.; Hatanaka, F.; Nakai, N.; Bolton, P.F. Behavioral Neuroscience of Autism. Neurosci. Biobehav. Rev. 2020, 110, 60–76. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Mao, X.; Zhu, C.; Zou, X.; Peng, F.; Yang, W.; Li, B.; Li, G.; Ge, T.; Cui, R. GABAergic System Dysfunction in Autism Spectrum Disorders. Front. Cell Dev. Biol. 2021, 9, 781327. [Google Scholar] [CrossRef]
- Montanari, M.; Martella, G.; Bonsi, P.; Meringolo, M. Autism Spectrum Disorder: Focus on Glutamatergic Neurotransmission. Int. J. Mol. Sci. 2022, 23, 3861. [Google Scholar] [CrossRef]
- Dawson, G.; Webb, S.J.; McPartland, J. Understanding the Nature of Face Processing Impairment in Autism: Insights from Behavioral and Electrophysiological Studies. Dev. Neuropsychol. 2005, 27, 403–424. [Google Scholar] [CrossRef]
- Schultz, R.T. Developmental Deficits in Social Perception in Autism: The Role of the Amygdala and Fusiform Face Area. Int. J. Dev. Neurosci. Off. J. Int. Soc. Dev. Neurosci. 2005, 23, 125–141. [Google Scholar] [CrossRef]
- Zalla, T.; Labruyère, N.; Clément, A.; Georgieff, N. Predicting Ensuing Actions in Children and Adolescents with Autism Spectrum Disorders. Exp. Brain Res. 2010, 201, 809–819. [Google Scholar] [CrossRef]
- Solomon, M.; Smith, A.C.; Frank, M.J.; Ly, S.; Carter, C.S. Probabilistic Reinforcement Learning in Adults with Autism Spectrum Disorders. Autism Res. Off. J. Int. Soc. Autism Res. 2011, 4, 109–120. [Google Scholar] [CrossRef]
- Scott-Van Zeeland, A.A.; Dapretto, M.; Ghahremani, D.G.; Poldrack, R.A.; Bookheimer, S.Y. Reward Processing in Autism. Autism Res. Off. J. Int. Soc. Autism Res. 2010, 3, 53–67. [Google Scholar] [CrossRef] [PubMed]
- Dichter, G.S. Functional Magnetic Resonance Imaging of Autism Spectrum Disorders. Dialogues Clin. Neurosci. 2012, 14, 319–351. [Google Scholar] [CrossRef] [PubMed]
- Kohls, G.; Schulte-Rüther, M.; Nehrkorn, B.; Müller, K.; Fink, G.R.; Kamp-Becker, I.; Herpertz-Dahlmann, B.; Schultz, R.T.; Konrad, K. Reward System Dysfunction in Autism Spectrum Disorders. Soc. Cogn. Affect. Neurosci. 2013, 8, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Zürcher, N.R.; Walsh, E.C.; Phillips, R.D.; Cernasov, P.M.; Tseng, C.-E.J.; Dharanikota, A.; Smith, E.; Li, Z.; Kinard, J.L.; Bizzell, J.C.; et al. A Simultaneous [(11)C]Raclopride Positron Emission Tomography and Functional Magnetic Resonance Imaging Investigation of Striatal Dopamine Binding in Autism. Transl. Psychiatry 2021, 11, 33. [Google Scholar] [CrossRef]
- De Krom, M.; Staal, W.G.; Ophoff, R.A.; Hendriks, J.; Buitelaar, J.; Franke, B.; de Jonge, M.V.; Bolton, P.; Collier, D.; Curran, S.; et al. A Common Variant in DRD3 Receptor Is Associated with Autism Spectrum Disorder. Biol. Psychiatry 2009, 65, 625–630. [Google Scholar] [CrossRef]
- Reiersen, A.M.; Todorov, A.A. Association between DRD4 Genotype and Autistic Symptoms in DSM-IV ADHD. J. Can. Acad. Child Adolesc. Psychiatry = J. L’academie Can. Psychiatr. L’enfant L’adolescent 2011, 20, 15–21. [Google Scholar]
- Hettinger, J.A.; Liu, X.; Hudson, M.L.; Lee, A.; Cohen, I.L.; Michaelis, R.C.; Schwartz, C.E.; Lewis, S.M.E.; Holden, J.J.A. DRD2 and PPP1R1B (DARPP-32) Polymorphisms Independently Confer Increased Risk for Autism Spectrum Disorders and Additively Predict Affected Status in Male-Only Affected Sib-Pair Families. Behav. Brain Funct. 2012, 8, 19. [Google Scholar] [CrossRef]
- Hamilton, P.J.; Campbell, N.G.; Sharma, S.; Erreger, K.; Herborg Hansen, F.; Saunders, C.; Belovich, A.N.; Sahai, M.A.; Cook, E.H.; Gether, U.; et al. De Novo Mutation in the Dopamine Transporter Gene Associates Dopamine Dysfunction with Autism Spectrum Disorder. Mol. Psychiatry 2013, 18, 1315–1323. [Google Scholar] [CrossRef]
- Bowton, E.; Saunders, C.; Reddy, I.A.; Campbell, N.G.; Hamilton, P.J.; Henry, L.K.; Coon, H.; Sakrikar, D.; Veenstra-VanderWeele, J.M.; Blakely, R.D.; et al. SLC6A3 Coding Variant Ala559Val Found in Two Autism Probands Alters Dopamine Transporter Function and Trafficking. Transl. Psychiatry 2014, 4, e464. [Google Scholar] [CrossRef]
- Campbell, N.G.; Shekar, A.; Aguilar, J.I.; Peng, D.; Navratna, V.; Yang, D.; Morley, A.N.; Duran, A.M.; Galli, G.; O’Grady, B.; et al. Structural, Functional, and Behavioral Insights of Dopamine Dysfunction Revealed by a Deletion in SLC6A3. Proc. Natl. Acad. Sci. USA 2019, 116, 3853–3862. [Google Scholar] [CrossRef]
- Toma, C.; Hervás, A.; Balmaña, N.; Salgado, M.; Maristany, M.; Vilella, E.; Aguilera, F.; Orejuela, C.; Cuscó, I.; Gallastegui, F.; et al. Neurotransmitter Systems and Neurotrophic Factors in Autism: Association Study of 37 Genes Suggests Involvement of DDC. World J. Biol. Psychiatry 2013, 14, 516–527. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.; Roth, A.; Kyzar, E.J.; Poudel, M.K.; Wong, K.; Stewart, A.M.; Kalueff, A.V. Decoding the Contribution of Dopaminergic Genes and Pathways to Autism Spectrum Disorder (ASD). Neurochem. Int. 2014, 66, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.T.N.; Kato, H.; Masuda, K.; Yamaza, H.; Hirofuji, Y.; Sato, H.; Pham, T.T.M.; Takayama, F.; Sakai, Y.; Ohga, S.; et al. Impaired Neurite Development Associated with Mitochondrial Dysfunction in Dopaminergic Neurons Differentiated from Exfoliated Deciduous Tooth-Derived Pulp Stem Cells of Children with Autism Spectrum Disorder. Biochem. Biophys. Rep. 2018, 16, 24–31. [Google Scholar] [CrossRef]
- Pavǎl, D. A Dopamine Hypothesis of Autism Spectrum Disorder. Dev. Neurosci. 2017, 39, 355–360. [Google Scholar] [CrossRef]
- Pavǎl, D.; Miclutia, I.V. The Dopamine Hypothesis of Autism Spectrum Disorder Revisited: Current Status and Future Prospects. Dev. Neurosci. 2021, 43, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Galvez-Contreras, A.Y.; Campos-Ordonez, T.; Lopez-Virgen, V.; Gomez-Plascencia, J.; Ramos-Zuniga, R.; Gonzalez-Perez, O. Growth Factors as Clinical Biomarkers of Prognosis and Diagnosis in Psychiatric Disorders. Cytokine Growth Factor Rev. 2016, 32, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Tsybko, A.S.; Ilchibaeva, T.V.; Popova, N.K. Role of Glial Cell Line-Derived Neurotrophic Factor in the Pathogenesis and Treatment of Mood Disorders. Rev. Neurosci. 2017, 28, 219–233. [Google Scholar] [CrossRef]
- Popova, N.K.; Naumenko, V.S. Neuronal and Behavioral Plasticity: The Role of Serotonin and BDNF Systems Tandem. Expert Opin. Ther. Targets 2019, 23, 227–239. [Google Scholar] [CrossRef]
- Autry, A.E.; Monteggia, L.M. Brain-Derived Neurotrophic Factor and Neuropsychiatric Disorders. Pharmacol. Rev. 2012, 64, 238–258. [Google Scholar] [CrossRef]
- Björkholm, C.; Monteggia, L.M. BDNF—A Key Transducer of Antidepressant Effects. Neuropharmacology 2016, 102, 72–79. [Google Scholar] [CrossRef]
- Castrén, E.; Antila, H. Neuronal Plasticity and Neurotrophic Factors in Drug Responses. Mol. Psychiatry 2017, 22, 1085–1095. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.-Y.; Feng, J.-C.; Cao, C.; Wu, H.-T.; Loh, Y.P.; Cheng, Y. Association of Peripheral Blood Levels of Brain-Derived Neurotrophic Factor With Autism Spectrum Disorder in Children: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2016, 170, 1079–1086. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Zhang, L.; Zhu, T.; Huang, J.; Qu, Y.; Mu, D. Peripheral Brain-Derived Neurotrophic Factor in Autism Spectrum Disorder: A Systematic Review and Meta-Analysis. Sci. Rep. 2016, 6, 31241. [Google Scholar] [CrossRef] [PubMed]
- Armeanu, R.; Mokkonen, M.; Crespi, B. Meta-Analysis of BDNF Levels in Autism. Cell. Mol. Neurobiol. 2017, 37, 949–954. [Google Scholar] [CrossRef] [PubMed]
- Saghazadeh, A.; Rezaei, N. Brain-Derived Neurotrophic Factor Levels in Autism: A Systematic Review and Meta-Analysis. J. Autism Dev. Disord. 2017, 47, 1018–1029. [Google Scholar] [CrossRef]
- Liu, S.H.; Shi, X.J.; Fan, F.C.; Cheng, Y. Peripheral Blood Neurotrophic Factor Levels in Children with Autism Spectrum Disorder: A Meta-Analysis. Sci. Rep. 2021, 11, 15. [Google Scholar] [CrossRef]
- Hashimoto, K.; Iwata, Y.; Nakamura, K.; Tsujii, M.; Tsuchiya, K.J.; Sekine, Y.; Suzuki, K.; Minabe, Y.; Takei, N.; Iyo, M.; et al. Reduced Serum Levels of Brain-Derived Neurotrophic Factor in Adult Male Patients with Autism. Prog. Neuropsychopharmacol. Biol. Psychiatry 2006, 30, 1529–1531. [Google Scholar] [CrossRef]
- Katoh-Semba, R.; Wakako, R.; Komori, T.; Shigemi, H.; Miyazaki, N.; Ito, H.; Kumagai, T.; Tsuzuki, M.; Shigemi, K.; Yoshida, F.; et al. Age-Related Changes in BDNF Protein Levels in Human Serum: Differences between Autism Cases and Normal Controls. Int. J. Dev. Neurosci. 2007, 25, 367–372. [Google Scholar] [CrossRef]
- Kasarpalkar, N.J.; Kothari, S.T.; Dave, U.P. Brain-Derived Neurotrophic Factor in Children with Autism Spectrum Disorder. Ann. Neurosci. 2014, 21, 129–133. [Google Scholar] [CrossRef]
- Taurines, R.; Segura, M.; Schecklmann, M.; Albantakis, L.; Grünblatt, E.; Walitza, S.; Jans, T.; Lyttwin, B.; Haberhausen, M.; Theisen, F.M.; et al. Altered Peripheral BDNF MRNA Expression and BDNF Protein Concentrations in Blood of Children and Adolescents with Autism Spectrum Disorder. J. Neural Transm. 2014, 121, 1117–1128. [Google Scholar] [CrossRef]
- Francis, K.; Dougali, A.; Sideri, K.; Kroupis, C.; Vasdekis, V.; Dima, K.; Douzenis, A. Brain-Derived Neurotrophic Factor (BDNF) in Children with ASD and Their Parents: A 3-Year Follow-Up. Acta Psychiatr. Scand. 2018, 137, 433–441. [Google Scholar] [CrossRef]
- Skogstrand, K.; Hagen, C.M.; Borbye-Lorenzen, N.; Christiansen, M.; Bybjerg-Grauholm, J.; Bækvad-Hansen, M.; Werge, T.; Børglum, A.; Mors, O.; Nordentoft, M.; et al. Reduced Neonatal Brain-Derived Neurotrophic Factor Is Associated with Autism Spectrum Disorders. Transl. Psychiatry 2019, 9, 252. [Google Scholar] [CrossRef]
- Garcia, K.L.P.; Yu, G.; Nicolini, C.; Michalski, B.; Garzon, D.J.; Chiu, V.S.; Tongiorgi, E.; Szatmari, P.; Fahnestock, M. Altered Balance of Proteolytic Isoforms of Pro-Brain-Derived Neurotrophic Factor in Autism. J. Neuropathol. Exp. Neurol. 2012, 71, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Hansen, S.L.; Lorentzen, J.; Pedersen, L.T.; Hendrich, F.L.; Jorsal, M.; Pingel, J.; Nielsen, J.B.; Kiens, B. Suboptimal Nutrition and Low Physical Activity Are Observed Together with Reduced Plasma Brain-Derived Neurotrophic Factor (BDNF) Concentration in Children with Severe Cerebral Palsy (CP). Nutrients 2019, 11, 620. [Google Scholar] [CrossRef] [PubMed]
- Liang, F.Q.; Allen, G.; Earnest, D. Role of Brain-Derived Neurotrophic Factor in the Circadian Regulation of the Suprachiasmatic Pacemaker by Light. J. Neurosci. Off. J. Soc. Neurosci. 2000, 20, 2978–2987. [Google Scholar] [CrossRef] [PubMed]
- Begliuomini, S.; Lenzi, E.; Ninni, F.; Casarosa, E.; Merlini, S.; Pluchino, N.; Valentino, V.; Luisi, S.; Luisi, M.; Genazzani, A.R. Plasma Brain-Derived Neurotrophic Factor Daily Variations in Men: Correlation with Cortisol Circadian Rhythm. J. Endocrinol. 2008, 197, 429. [Google Scholar] [CrossRef]
- Bercik, P.; Denou, E.; Collins, J.; Jackson, W.; Lu, J.; Jury, J.; Deng, Y.; Blennerhassett, P.; MacRi, J.; McCoy, K.D.; et al. The Intestinal Microbiota Affect Central Levels of Brain-Derived Neurotropic Factor and Behavior in Mice. Gastroenterology 2011, 141, 599–609. [Google Scholar] [CrossRef]
- Hyman, C.; Hofer, M.; Barde, Y.A.; Juhasz, M.; Yancopoulos, G.D.; Squinto, S.P.; Lindsay, R.M. BDNF Is a Neurotrophic Factor for Dopaminergic Neurons of the Substantia Nigra. Nature 1991, 350, 230–232. [Google Scholar] [CrossRef]
- Blöchl, A.; Sirrenberg, C. Neurotrophins Stimulate the Release of Dopamine from Rat Mesencephalic Neurons via Trk and P75(Lntr) Receptors. J. Biol. Chem. 1996, 271, 21100–21107. [Google Scholar] [CrossRef]
- Zhou, J.; Bradford, H.F.; Stern, G.M. Influence of BDNF on the Expression of the Dopaminergic Phenotype of Tissue Used for Brain Transplants. Brain Res. Dev. Brain Res. 1997, 100, 43–51. [Google Scholar] [CrossRef]
- Saylor, A.J.; Meredith, G.E.; Vercillo, M.S.; Zahm, D.S.; McGinty, J.F. BDNF Heterozygous Mice Demonstrate Age-Related Changes in Striatal and Nigral Gene Expression. Exp. Neurol. 2006, 199, 362–372. [Google Scholar] [CrossRef]
- Porritt, M.J.; Batchelor, P.E.; Howells, D.W. Inhibiting BDNF Expression by Antisense Oligonucleotide Infusion Causes Loss of Nigral Dopaminergic Neurons. Exp. Neurol. 2005, 192, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Venero, J.L.; Vizuete, M.L.; Revuelta, M.; Vargas, C.; Cano, J.; Machado, A. Upregulation of BDNF MRNA and TrkB MRNA in the Nigrostriatal System and in the Lesion Site Following Unilateral Transection of the Medial Forebrain Bundle. Exp. Neurol. 2000, 161, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Bower, K.A.; Ma, C.; Fang, S.; Thiele, C.J.; Luo, J. Glycogen Synthase Kinase 3beta (GSK3beta) Mediates 6-Hydroxydopamine-Induced Neuronal Death. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2004, 18, 1162–1164. [Google Scholar] [CrossRef]
- Canudas, A.M.; Pezzi, S.; Canals, J.M.; Pallàs, M.; Alberch, J. Endogenous Brain-Derived Neurotrophic Factor Protects Dopaminergic Nigral Neurons against Transneuronal Degeneration Induced by Striatal Excitotoxic Injury. Brain Res. Mol. Brain Res. 2005, 134, 147–154. [Google Scholar] [CrossRef]
- Kang, S.S.; Zhang, Z.; Liu, X.; Manfredsson, F.P.; Benskey, M.J.; Cao, X.; Xu, J.; Sun, Y.E.; Ye, K. TrkB Neurotrophic Activities Are Blocked by α-Synuclein, Triggering Dopaminergic Cell Death in Parkinson’s Disease. Proc. Natl. Acad. Sci. USA 2017, 114, 10773–10778. [Google Scholar] [CrossRef]
- Ding, Y.-X.; Xia, Y.; Jiao, X.-Y.; Duan, L.; Yu, J.; Wang, X.; Chen, L.-W. The TrkB-Positive Dopaminergic Neurons Are Less Sensitive to MPTP Insult in the Substantia Nigra of Adult C57/BL Mice. Neurochem. Res. 2011, 36, 1759–1766. [Google Scholar] [CrossRef]
- Park, H.-J.; Lim, S.; Joo, W.-S.; Yin, C.-S.; Lee, H.-S.; Lee, H.-J.; Seo, J.C.; Leem, K.; Son, Y.-S.; Kim, Y.-J.; et al. Acupuncture Prevents 6-Hydroxydopamine-Induced Neuronal Death in the Nigrostriatal Dopaminergic System in the Rat Parkinson’s Disease Model. Exp. Neurol. 2003, 180, 93–98. [Google Scholar] [CrossRef]
- Sagi, Y.; Mandel, S.; Amit, T.; Youdim, M.B.H. Activation of Tyrosine Kinase Receptor Signaling Pathway by Rasagiline Facilitates Neurorescue and Restoration of Nigrostriatal Dopamine Neurons in Post-MPTP-Induced Parkinsonism. Neurobiol. Dis. 2007, 25, 35–44. [Google Scholar] [CrossRef]
- Katsuki, H.; Kurimoto, E.; Takemori, S.; Kurauchi, Y.; Hisatsune, A.; Isohama, Y.; Izumi, Y.; Kume, T.; Shudo, K.; Akaike, A. Retinoic Acid Receptor Stimulation Protects Midbrain Dopaminergic Neurons from Inflammatory Degeneration via BDNF-Mediated Signaling. J. Neurochem. 2009, 110, 707–718. [Google Scholar] [CrossRef]
- Galpern, W.R.; Frim, D.M.; Tatter, S.B.; Altar, C.A.; Beal, M.F.; Isacson, O. Cell-Mediated Delivery of Brain-Derived Neurotrophic Factor Enhances Dopamine Levels in an MPP+ Rat Model of Substantia Nigra Degeneration. Cell Transplant. 1996, 5, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Erickson, J.T.; Brosenitsch, T.A.; Katz, D.M. Brain-Derived Neurotrophic Factor and Glial Cell Line-Derived Neurotrophic Factor Are Required Simultaneously for Survival of Dopaminergic Primary Sensory Neurons in vivo. J. Neurosci. Off. J. Soc. Neurosci. 2001, 21, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Somoza, R.; Juri, C.; Baes, M.; Wyneken, U.; Rubio, F.J. Intranigral Transplantation of Epigenetically Induced BDNF-Secreting Human Mesenchymal Stem Cells: Implications for Cell-Based Therapies in Parkinson’s Disease. Biol. Blood Marrow Transplant. 2010, 16, 1530–1540. [Google Scholar] [CrossRef] [PubMed]
- Collo, G.; Cavalleri, L.; Spano, P.F. Structural Plasticity in Mesencephalic Dopaminergic Neurons Produced by Drugs of Abuse: Critical Role of BDNF and Dopamine. Front. Pharmacol. 2014, 5, 259. [Google Scholar] [CrossRef] [PubMed]
- Douma, E.H.; de Kloet, E.R. Stress-Induced Plasticity and Functioning of Ventral Tegmental Dopamine Neurons. Neurosci. Biobehav. Rev. 2020, 108, 48–77. [Google Scholar] [CrossRef]
- Article, O.; Lee, Y.; Han, P. Early-Life Stress in D2 Heterozygous Mice Promotes Autistic-like Behaviors through the Downregulation of the BDNF-TrkB Pathway in the Dorsal Striatum. Exp. Neurobiol. 2019, 28, 337–351. [Google Scholar]
- Meyza, K.Z.; Defensor, E.B.; Jensen, A.L.; Corley, M.J.; Pearson, B.L.; Pobbe, R.L.H.; Bolivar, V.J.; Blanchard, D.C.; Blanchard, R.J. The BTBR T+ Tf/J Mouse Model for Autism Spectrum Disorders-in Search of Biomarkers. Behav. Brain Res. 2013, 251, 25–34. [Google Scholar] [CrossRef]
- Meyza, K.Z.; Blanchard, D.C. The BTBR Mouse Model of Idiopathic Autism—Current View on Mechanisms. Neurosci. Biobehav. Rev. 2017, 76, 99–110. [Google Scholar] [CrossRef]
- McFarlane, H.G.; Kusek, G.K.; Yang, M.; Phoenix, J.L.; Bolivar, V.J.; Crawley, J.N. Autism-like Behavioral Phenotypes in BTBR T+tf/J Mice. Genes Brain. Behav. 2008, 7, 152–163. [Google Scholar] [CrossRef]
- Ellegood, J.; Crawley, J.N. Behavioral and Neuroanatomical Phenotypes in Mouse Models of Autism. Neurother. J. Am. Soc. Exp. Neurother. 2015, 12, 521–533. [Google Scholar] [CrossRef]
- Squillace, M.; Dodero, L.; Federici, M.; Migliarini, S.; Errico, F.; Napolitano, F.; Krashia, P.; Di Maio, A.; Galbusera, A.; Bifone, A.; et al. Dysfunctional Dopaminergic Neurotransmission in Asocial BTBR Mice. Transl. Psychiatry 2014, 4, e427. [Google Scholar] [CrossRef] [PubMed]
- Chao, O.Y.; Pathak, S.S.; Zhang, H.; Dunaway, N.; Li, J.S.; Mattern, C.; Nikolaus, S.; Huston, J.P.; Yang, Y.M. Altered Dopaminergic Pathways and Therapeutic Effects of Intranasal Dopamine in Two Distinct Mouse Models of Autism. Mol. Brain 2020, 13, 1–16. [Google Scholar] [CrossRef]
- Stephenson, D.T.; O’Neill, S.M.; Narayan, S.; Tiwari, A.; Arnold, E.; Samaroo, H.D.; Du, F.; Ring, R.H.; Campbell, B.; Pletcher, M.; et al. Histopathologic Characterization of the BTBR Mouse Model of Autistic-like Behavior Reveals Selective Changes in Neurodevelopmental Proteins and Adult Hippocampal Neurogenesis. Mol. Autism 2011, 2, 7. [Google Scholar] [CrossRef]
- Daimon, C.M.; Jasien, J.M.; Wood, W.H.; Zhang, Y.; Becker, K.G.; Silverman, J.L.; Crawley, J.N.; Martin, B.; Maudsley, S. Hippocampal Transcriptomic and Proteomic Alterations in the BTBR Mouse Model of Autism Spectrum Disorder. Front. Physiol. 2015, 6, 324. [Google Scholar] [CrossRef]
- Scattoni, M.L.; Martire, A.; Cartocci, G.; Ferrante, A.; Ricceri, L. Reduced Social Interaction, Behavioural Flexibility and BDNF Signalling in the BTBR T+tf/J Strain, a Mouse Model of Autism. Behav. Brain Res. 2013, 251, 35–40. [Google Scholar] [CrossRef]
- Jasien, J.M.; Daimon, C.M.; Wang, R.; Shapiro, B.K.; Martin, B.; Maudsley, S. The Effects of Aging on the BTBR Mouse Model of Autism Spectrum Disorder. Front. Aging Neurosci. 2014, 6, 225. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.R.; Kim, C.Y.; Shin, K.M.; Jo, J.H.; Kim, H.A.; Heo, Y. Altered Expression Levels of Neurodevelopmental Proteins in Fetal Brains of BTBR T+tf/J Mice with Autism-like Behavioral Characteristics. J. Toxicol. Environ. Health Part A Curr. Issues 2015, 78, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Queen, N.J.; Boardman, A.A.; Patel, R.S.; Siu, J.J.; Mo, X.; Cao, L. Environmental Enrichment Improves Metabolic and Behavioral Health in the BTBR Mouse Model of Autism. Psychoneuroendocrinology 2020, 111, 104476. [Google Scholar] [CrossRef]
- De Simone, R.; Butera, A.; Armida, M.; Pezzola, A.; Boirivant, M.; Potenza, R.L.; Ricceri, L. Beneficial Effects of Fingolimod on Social Interaction, CNS and Peripheral Immune Response in the BTBR Mouse Model of Autism. Neuroscience 2020, 435, 22–32. [Google Scholar] [CrossRef]
- Cristiano, C.; Pirozzi, C.; Coretti, L.; Cavaliere, G.; Lama, A.; Russo, R.; Lembo, F.; Mollica, M.P.; Meli, R.; Calignano, A.; et al. Palmitoylethanolamide Counteracts Autistic-like Behaviours in BTBR T+tf/J Mice: Contribution of Central and Peripheral Mechanisms. Brain. Behav. Immun. 2018, 74, 166–175. [Google Scholar] [CrossRef]
- Avraham, Y.; Berry, E.M.; Donskoy, M.; Ahmad, W.A.; Vorobiev, L.; Albeck, A.; Mankuta, D. Beta-Carotene as a Novel Therapy for the Treatment of “Autistic like Behavior” in Animal Models of Autism. Behav. Brain Res. 2019, 364, 469–479. [Google Scholar] [CrossRef] [PubMed]
- Segal-Gavish, H.; Karvat, G.; Barak, N.; Barzilay, R.; Ganz, J.; Edry, L.; Aharony, I.; Offen, D.; Kimchi, T. Mesenchymal Stem Cell Transplantation Promotes Neurogenesis and Ameliorates Autism Related Behaviors in BTBR Mice. Autism Res. 2016, 9, 17–32. [Google Scholar] [CrossRef]
- Zhang, R.; Cai, Y.; Xiao, R.; Zhong, H.; Li, X.; Guo, L.; Xu, H.; Fan, X. Human Amniotic Epithelial Cell Transplantation Promotes Neurogenesis and Ameliorates Social Deficits in BTBR Mice. Stem Cell Res. Ther. 2019, 10, 153. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Zhuang, M.; Wu, R. Secretion of Nerve Growth Factor, Brain-Derived Neurotrophic Factor, and Glial Cell-Line Derived Neurotrophic Factor in Co-Culture of Four Cell Types in Cerebrospinal Fluid-Containing Medium. Neural Regen. Res. 2012, 7, 2907–2914. [Google Scholar] [CrossRef] [PubMed]
- Rota, C.; Imberti, B.; Pozzobon, M.; Piccoli, M.; De Coppi, P.; Atala, A.; Gagliardini, E.; Xinaris, C.; Benedetti, V.; Fabricio, A.S.C.; et al. Human Amniotic Fluid Stem Cell Preconditioning Improves Their Regenerative Potential. Stem Cells Dev. 2012, 21, 1911–1923. [Google Scholar] [CrossRef] [PubMed]
- Crigler, L.; Robey, R.C.; Asawachaicharn, A.; Gaupp, D.; Phinney, D.G. Human Mesenchymal Stem Cell Subpopulations Express a Variety of Neuro-Regulatory Molecules and Promote Neuronal Cell Survival and Neuritogenesis. Exp. Neurol. 2006, 198, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Beopoulos, A.; Géa, M.; Fasano, A.; Iris, F. Autism Spectrum Disorders Pathogenesis: Toward a Comprehensive Model Based on Neuroanatomic and Neurodevelopment Considerations. Front. Neurosci. 2022, 16, 988735. [Google Scholar] [CrossRef]
- Dodero, L.; Damiano, M.; Galbusera, A.; Bifone, A.; Tsaftsaris, S.A.; Scattoni, M.L.; Gozzi, A. Neuroimaging Evidence of Major Morpho-Anatomical and Functional Abnormalities in the BTBR T+TF/J Mouse Model of Autism. PLoS ONE 2013, 8, e76655. [Google Scholar] [CrossRef]
- Ellegood, J.; Babineau, B.A.; Henkelman, R.M.; Lerch, J.P.; Crawley, J.N. Neuroanatomical Analysis of the BTBR Mouse Model of Autism Using Magnetic Resonance Imaging and Diffusion Tensor Imaging. Neuroimage 2013, 70, 288–300. [Google Scholar] [CrossRef]
- Pagani, M.; Damiano, M.; Galbusera, A.; Tsaftaris, S.A.; Gozzi, A. Semi-Automated Registration-Based Anatomical Labelling, Voxel Based Morphometry and Cortical Thickness Mapping of the Mouse Brain. J. Neurosci. Methods 2016, 267, 62–73. [Google Scholar] [CrossRef]
- Sforazzini, F.; Bertero, A.; Dodero, L.; David, G.; Galbusera, A.; Scattoni, M.L.; Pasqualetti, M.; Gozzi, A. Altered Functional Connectivity Networks in Acallosal and Socially Impaired BTBR Mice. Brain Struct. Funct. 2016, 221, 941–954. [Google Scholar] [CrossRef] [PubMed]
- Faraji, J.; Karimi, M.; Lawrence, C.; Mohajerani, M.H.; Metz, G.A.S. Non-Diagnostic Symptoms in a Mouse Model of Autism in Relation to Neuroanatomy: The BTBR Strain Reinvestigated. Transl. Psychiatry 2018, 8, 234. [Google Scholar] [CrossRef] [PubMed]
- Reshetnikov, V.V.; Ayriyants, K.A.; Ryabushkina, Y.A.; Sozonov, N.G.; Bondar, N.P. Sex-Specific Behavioral and Structural Alterations Caused by Early-Life Stress in C57BL/6 and BTBR Mice. Behav. Brain Res. 2021, 414, 113489. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.A.; Hsu, F.-W.; Herd, B.; Gregg, M.; Sample, H.; Kaplan, J. Executive Functions in Agenesis of the Corpus Callosum: Working Memory and Sustained Attention in the BTBR Inbred Mouse Strain. Brain Behav. 2021, 11, e01933. [Google Scholar] [CrossRef] [PubMed]
- Paul, L.K.; Corsello, C.; Kennedy, D.P.; Adolphs, R. Agenesis of the Corpus Callosum and Autism: A Comprehensive Comparison. Brain 2014, 137, 1813–1829. [Google Scholar] [CrossRef]
- Grimm, D.; Kay, M.A.; Kleinschmidt, J.A. Helper Virus-Free, Optically Controllable, and Two-Plasmid-Based Production of Adeno-Associated Virus Vectors of Serotypes 1 to 6. Mol. Ther. 2003, 7, 839–850. [Google Scholar] [CrossRef]
- Kulikov, A.V.; Tikhonova, M.A.; Kulikov, V.A. Automated Measurement of Spatial Preference in the Open Field Test with Transmitted Lighting. J. Neurosci. Methods 2008, 170, 345–351. [Google Scholar] [CrossRef]
- Khotskin, N.V.; Plyusnina, A.V.; Kulikova, E.A.; Bazhenova, E.Y.; Fursenko, D.V.; Sorokin, I.E.; Kolotygin, I.; Mormede, P.; Terenina, E.E.; Shevelev, O.B.; et al. On Association of the Lethal Yellow (A(Y)) Mutation in the Agouti Gene with the Alterations in Mouse Brain and Behavior. Behav. Brain Res. 2019, 359, 446–456. [Google Scholar] [CrossRef]
- Njung’e, K.; Handley, S.L. Evaluation of Marble-Burying Behavior as a Model of Anxiety. Pharmacol. Biochem. Behav. 1991, 38, 63–67. [Google Scholar] [CrossRef]
- Deacon, R.M.J. Digging and Marble Burying in Mice: Simple Methods for in Vivo Identification of Biological Impacts. Nat. Protoc. 2006, 1, 122–124. [Google Scholar] [CrossRef]
- Yang, M.; Abrams, D.N.; Zhang, J.Y.; Weber, M.D.; Katz, A.M.; Clarke, A.M.; Silverman, J.L.; Crawley, J.N. Low Sociability in BTBR T+tf/J Mice Is Independent of Partner Strain. Physiol. Behav. 2012, 107, 649–662. [Google Scholar] [CrossRef] [PubMed]
- Rein, B.; Ma, K.; Yan, Z. A Standardized Social Preference Protocol for Measuring Social Deficits in Mouse Models of Autism. Nat. Protoc. 2020, 15, 3464–3477. [Google Scholar] [CrossRef] [PubMed]
- Lueptow, L.M. Novel Object Recognition Test for the Investigation of Learning and Memory in Mice. J. Vis. Exp. 2017, 2017, e55718. [Google Scholar] [CrossRef]
- Kulikov, A.V.; Naumenko, V.S.; Voronova, I.P.; Tikhonova, M.A.; Popova, N.K. Quantitative RT-PCR Assay of 5-HT1A and 5-HT2A Serotonin Receptor MRNAs Using Genomic DNA as an External Standard. J. Neurosci. Methods 2005, 141, 97–101. [Google Scholar] [CrossRef]
- Naumenko, V.S.; Kulikov, A.V. Quantitative assay of 5-HT(1A) serotonin receptor gene expression in the brain. Mol. Biol. 2006, 40, 37–44. [Google Scholar] [CrossRef]
- Naumenko, V.S.; Osipova, D.V.; Kostina, E.V.; Kulikov, A.V. Utilization of a Two-Standard System in Real-Time PCR for Quantification of Gene Expression in the Brain. J. Neurosci. Methods 2008, 170, 197–203. [Google Scholar] [CrossRef]
- Naumenko, V.S.; Kondaurova, E.M.; Bazovkina, D.V.; Tsybko, A.S.; Tikhonova, M.A.; Kulikov, A.V.; Popova, N.K. Effect of Brain-Derived Neurotrophic Factor on Behavior and Key Members of the Brain Serotonin System in Genetically Predisposed to Behavioral Disorders Mouse Strains. Neuroscience 2012, 214, 59–67. [Google Scholar] [CrossRef]
- Popova, N.K.; Morozova, M.V.; Naumenko, V.S. Ameliorative Effect of BDNF on Prenatal Ethanol and Stress Exposure-Induced Behavioral Disorders. Neurosci. Lett. 2011, 505, 82–86. [Google Scholar] [CrossRef]
- Naumenko, V.S.; Bazovkina, D.V.; Morozova, M.V.; Popova, N.K. Effects of Brain-Derived and Glial Cell Line-Derived Neurotrophic Factors on Startle Response and Disrupted Prepulse Inhibition in Mice of DBA/2J Inbred Strain. Neurosci. Lett. 2013, 550, 115–118. [Google Scholar] [CrossRef]
- Zarneshan, S.N.; Fakhri, S.; Khan, H. Targeting Akt/CREB/BDNF Signaling Pathway by Ginsenosides in Neurodegenerative Diseases: A Mechanistic Approach. Pharmacol. Res. 2022, 177, 106099. [Google Scholar] [CrossRef]
- Belokopytova, I.I.; Kondaurova, E.M.; Kulikova, E.A.; Ilchibaeva, T.V.; Naumenko, V.S.; Popova, N.K. Effects of the Cc2d1a/Freud-1 Knockdown in the Hippocampus of BTBR Mice on the Autistic-Like Behavior, Expression of Serotonin 5-HT(1A) and D2 Dopamine Receptors, and CREB and NF-KB Intracellular Signaling. Biochemistry 2022, 87, 1206–1218. [Google Scholar] [CrossRef]
- Kondaurova, E.M.; Plyusnina, A.V.; Ilchibaeva, T.V.; Eremin, D.V.; Rodnyy, A.Y.; Grygoreva, Y.D.; Naumenko, V.S. Effects of a Cc2d1a/Freud-1 Knockdown in the Hippocampus on Behavior, the Serotonin System, and BDNF. Int. J. Mol. Sci. 2021, 22, 13319. [Google Scholar] [CrossRef] [PubMed]
- Shillingsburg, M.A.; Hansen, B.; Wright, M. Rapport Building and Instructional Fading Prior to Discrete Trial Instruction: Moving From Child-Led Play to Intensive Teaching. Behav. Modif. 2019, 43, 288–306. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.-H.; Chen, K.-L.; Li, H.-J.; Chen, K.-H.; Hsu, C.-W.; Lu, C.-H.; Hsieh, K.-Y.; Huang, C.-Y. The Symptoms of Autism Including Social Communication Deficits and Repetitive and Restricted Behaviors Are Associated with Different Emotional and Behavioral Problems. Sci. Rep. 2020, 10, 20509. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.-B.; Liu, H.-X.; Shi, W.; Ding, T.; Hu, H.-Q.; Guo, H.-W.; Jin, S.; Wang, X.-L.; Zhang, T.; Lu, Y.-C.; et al. Various BDNF Administrations Attenuate SPS-Induced Anxiety-like Behaviors. Neurosci. Lett. 2022, 788, 136851. [Google Scholar] [CrossRef] [PubMed]
- Pietropaolo, S.; Paterna, J.-C.; Büeler, H.; Feldon, J.; Yee, B.K. Bidirectional Changes in Water-Maze Learning Following Recombinant Adenovirus-Associated Viral Vector (RAAV)-Mediated Brain-Derived Neurotrophic Factor Expression in the Rat Hippocampus. Behav. Pharmacol. 2007, 18, 533–547. [Google Scholar] [CrossRef] [PubMed]
- Diniz, D.M.; Calabrese, F.; Brivio, P.; Riva, M.A.; Grandjean, J.; Homberg, J.R. BDNF Overexpression in the Ventral Hippocampus Promotes Antidepressant- and Anxiolytic-Like Activity in Serotonin Transporter Knockout Rats. Int. J. Mol. Sci. 2021, 22, 5040. [Google Scholar] [CrossRef]
- Bahi, A. Hippocampal BDNF Overexpression or MicroR124a Silencing Reduces Anxiety- and Autism-like Behaviors in Rats. Behav. Brain Res. 2017, 326, 281–290. [Google Scholar] [CrossRef]
- Weidner, K.L.; Buenaventura, D.F.; Chadman, K.K. Mice Over-Expressing BDNF in Forebrain Neurons Develop an Altered Behavioral Phenotype with Age. Behav. Brain Res. 2014, 268, 222–228. [Google Scholar] [CrossRef]
- Palasz, E.; Wysocka, A.; Gasiorowska, A.; Chalimoniuk, M.; Niewiadomski, W.; Niewiadomska, G. BDNF as a Promising Therapeutic Agent in Parkinson’s Disease. Int. J. Mol. Sci. 2020, 21, 1170. [Google Scholar] [CrossRef]
- Neal, M.; Cunningham, J.; Lever, I.; Pezet, S.; Malcangio, M. Mechanism by Which Brain-Derived Neurotrophic Factor Increases Dopamine Release from the Rabbit Retina. Investig. Ophthalmol. Vis. Sci. 2003, 44, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Bazovkina, D.; Naumenko, V.; Bazhenova, E.; Kondaurova, E. Effect of Central Administration of Brain-Derived Neurotrophic Factor (BDNF) on Behavior and Brain Monoamine Metabolism in New Recombinant Mouse Lines Differing by 5-HT(1A) Receptor Functionality. Int. J. Mol. Sci. 2021, 22, 11987. [Google Scholar] [CrossRef] [PubMed]
- Berton, O.; McClung, C.A.; Dileone, R.J.; Krishnan, V.; Renthal, W.; Russo, S.J.; Graham, D.; Tsankova, N.M.; Bolanos, C.A.; Rios, M.; et al. Essential Role of BDNF in the Mesolimbic Dopamine Pathway in Social Defeat Stress. Science 2006, 311, 864–868. [Google Scholar] [CrossRef]
- Larson, E.B.; Wang, L.; Bowen, J.D.; McCormick, W.C.; Teri, L.; Crane, P.; Kukull, W. Exercise Is Associated with Reduced Risk for Incident Dementia among Persons 65 Years of Age and Older. Ann. Intern. Med. 2006, 144, 73–81. [Google Scholar] [CrossRef]
- Verburgh, K. Nutrigerontology: Why We Need a New Scientific Discipline to Develop Diets and Guidelines to Reduce the Risk of Aging-Related Diseases. Aging Cell 2015, 14, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.S.; Scherr, P.A.; Schneider, J.A.; Tang, Y.; Bennett, D.A. Relation of Cognitive Activity to Risk of Developing Alzheimer Disease. Neurology 2007, 69, 1911–1920. [Google Scholar] [CrossRef]

| Target Protein | Primary Antibody | Secondary Antibody: Dilution, Manufacturer Code | |
|---|---|---|---|
| Antibody Dilution | Manufacturer Code | ||
| BDNF | 1:1000 | Ab108319 (Abcam, UK) | Anti-rabbit 1:10,000, G-21234 (Invitrogen, USA) |
| TrkB | 1:400 | Ab32096 (Abcam, UK) | |
| P75NTR | 1:500 | Ab38335 (Abcam, UK) | |
| TH | 1:500 | Ab112 (Abcam, UK) | |
| DAT | 1:500 | Ab184451 (Abcam, UK) | |
| COMT | 1:200 | Sc-137253 (Santa Cruz, USA) | |
| D1R | 1:250 | Ab20066 (Abcam, UK) | |
| D2R | 1:500 | Sc-9113 (Santa Cruz, USA) | |
| proBDNF | 1:2500 | Sc-65513 (Santa Cruz, USA) | Anti-mouse 1:30,000, #31430 (Invitrogen, Waltham, MA, USA) |
| GAPDH | 1:7000 | Ab8245 (Abcam, UK) | Anti-mouse 1:30,000, ab6728 (Abcam, Cambridge, UK) |
| Parameter | Control | BDNF | p Values |
|---|---|---|---|
| Time in the center of arena, % | 15.88 ± 1.83 | 15.49 ± 1.54 | p = 0.87 |
| Explored area of the arena, % | 94.35 ± 2.00 | 95.82 ± 1.21 | p = 0.79 |
| Distance traveled, m | 34.70 ± 3.61 | 35.74 ± 2.54 | p = 0.81 |
| Rearings, number | 16.30 ± 2.64 | 17.80 ± 3.08 | p = 0.71 |
| Parameter | Control | BDNF | p Values |
|---|---|---|---|
| Time in open arms, % | 19.26 ± 4.46 | 23.11 ± 4.41 | p = 0.55 |
| Explored area of open arms, % | 62.04 ± 9.83 | 67.93 ± 8.88 | p = 0.63 |
| Time in closed arms, % | 67.16 ± 5.16 | 61.61 ± 4.91 | p = 0.45 |
| Explored area of closed arms, % | 91.24 ± 0.49 | 91.16 ± 0.39 | p = 0.97 |
| Distance traveled, m | 8.36 ± 0.52 | 8.98 ± 0.43 | p = 0.37 |
| Head-dips, number | 20.40 ± 4.08 | 24.70 ± 3.86 | p = 0.45 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ilchibaeva, T.; Tsybko, A.; Lipnitskaya, M.; Eremin, D.; Milutinovich, K.; Naumenko, V.; Popova, N. Brain-Derived Neurotrophic Factor (BDNF) in Mechanisms of Autistic-like Behavior in BTBR Mice: Crosstalk with the Dopaminergic Brain System. Biomedicines 2023, 11, 1482. https://doi.org/10.3390/biomedicines11051482
Ilchibaeva T, Tsybko A, Lipnitskaya M, Eremin D, Milutinovich K, Naumenko V, Popova N. Brain-Derived Neurotrophic Factor (BDNF) in Mechanisms of Autistic-like Behavior in BTBR Mice: Crosstalk with the Dopaminergic Brain System. Biomedicines. 2023; 11(5):1482. https://doi.org/10.3390/biomedicines11051482
Chicago/Turabian StyleIlchibaeva, Tatiana, Anton Tsybko, Marina Lipnitskaya, Dmitry Eremin, Kseniya Milutinovich, Vladimir Naumenko, and Nina Popova. 2023. "Brain-Derived Neurotrophic Factor (BDNF) in Mechanisms of Autistic-like Behavior in BTBR Mice: Crosstalk with the Dopaminergic Brain System" Biomedicines 11, no. 5: 1482. https://doi.org/10.3390/biomedicines11051482
APA StyleIlchibaeva, T., Tsybko, A., Lipnitskaya, M., Eremin, D., Milutinovich, K., Naumenko, V., & Popova, N. (2023). Brain-Derived Neurotrophic Factor (BDNF) in Mechanisms of Autistic-like Behavior in BTBR Mice: Crosstalk with the Dopaminergic Brain System. Biomedicines, 11(5), 1482. https://doi.org/10.3390/biomedicines11051482






