Pathology and Treatment of Psoriasis Using Nanoformulations
Abstract
1. Introduction
2. Pathology and Pathogenesis of Psoriasis
- Plaque PSO:
- Flexural PSO:
- −
- Also recognized as inverse PSO.
- −
- It can be observed in the armpits, groin, breasts, and various skin crevices surrounding the genitals and buttocks.
- −
- PSO affects approximately 20% of the population.
- −
- CAUSE: Yeast proliferation, extreme hypersensitivity to abrasion or perspiration [24].
- Guttate PSO:
- −
- Typically provoked by a microbial infestation.
- −
- Microscopic drop lesions appear on the torso, limbs and scalp.
- −
- CAUSE: Streptococcal infection, microbial infections, skin injuries, such as cuts, blisters, or insect bites, medications, Sun damage, psychological tension, and alcohol intake [25].
- Nail PSO:
- −
- Irregular nail development and discoloration can occur in fingernails and toenails. Color changes, small pits, lines across the nails, a white area on the plate, thickening of the skin under, and loosening of the nails are all symptoms.
- −
- CAUSE: A confluence of inherited, ecological, and immunological factors [26].
- Psoriatic arthritis:
- −
- An inflammatory condition that affects the joints of children and adults with PSO.
- −
- Red, swollen, tender, warm, and stiff joints, stroke, atherosclerosis, myocardial infarction.
- −
- CAUSE: Trauma or injury on the skin, like cuts or burns, medicines, alcohol, skin irritants, and smoking [27].
- Erythrodermic PSO:
- −
- Defined by recurring, intense erythema of the epidermis and the accumulation of scales in layers instead of tiny flakes.
- −
- Increased cardiac pace, changing body temperature, skin reddening.
- −
- CAUSE: Corticosteroid usage, burns, psychological pain, drinking, illnesses, and allergies [28].
- Pustular PSO:
- −
- Dermal reddening, accompanied by pustule development and scaling. Discomfort or light sensitivities.
- −
- CAUSE: Excessive UV radiation, pregnancies, steroids, diseases, extreme trauma, and abrupt discontinuation of systemic medicines or powerful external stimulants [29].
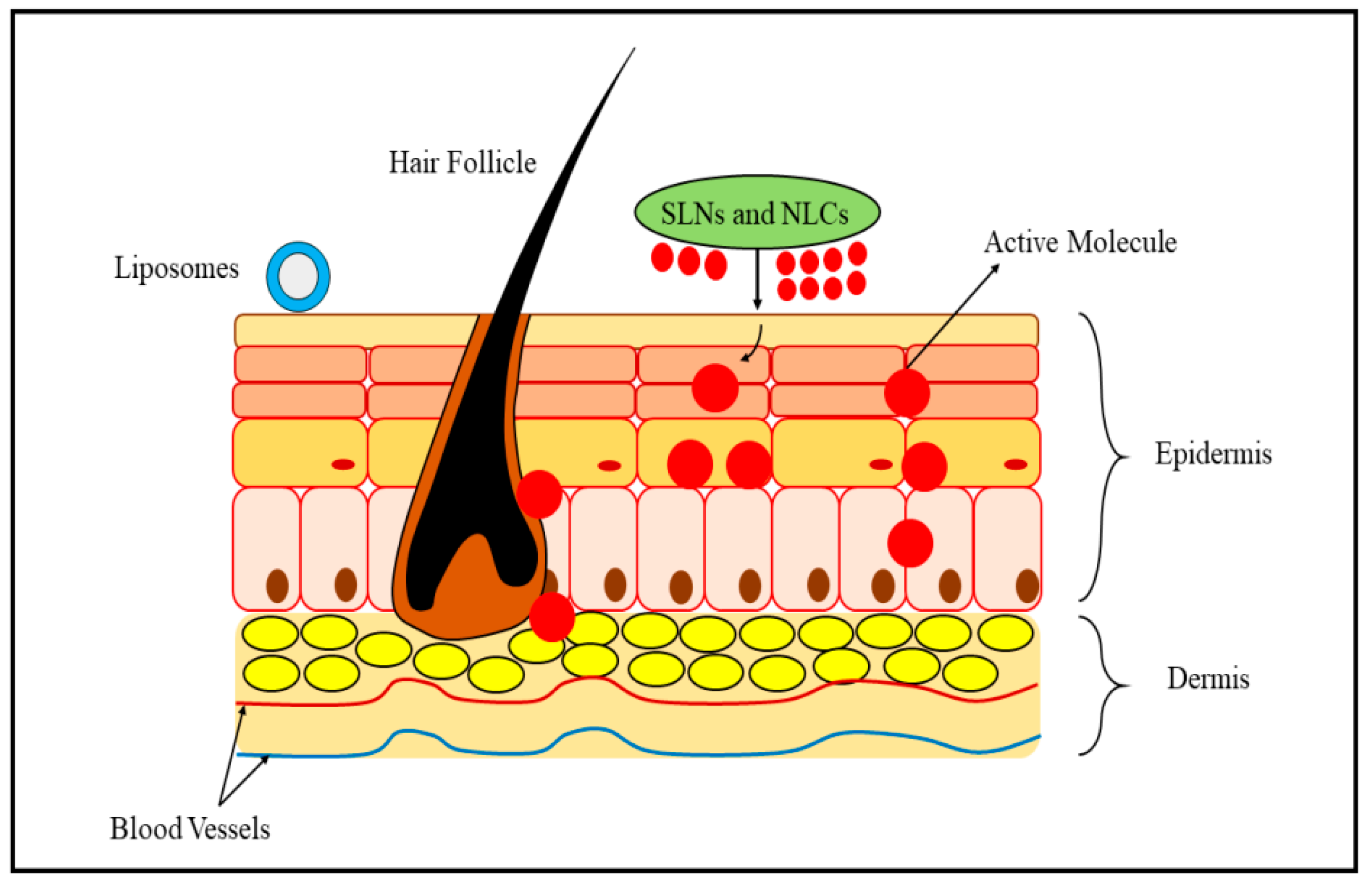
3. Mechanism of Percutaneous Absorption and Treatment
4. Drug Delivery Systems for the Treatment of PSO
4.1. Nanoparticles
4.2. Lipid Nanoparticles
4.3. Metallic Nanoparticles
4.4. Phytocompounds
5. Current Therapies
5.1. Topical Therapy
5.2. Photo-Based Therapy
5.3. Systemic Therapy
6. Applications
- Development of novel gene loci linked to PSO: Genome-wide association studies (GWAS) have revealed many distinct genomic loci linked to PSO, showing knowledge of the disorder’s etiology.
- Monitoring technologies that have been upgraded: Imaging tools like optical coherence tomography (OCT) and confocal microscopy have made it easier to identify and track PSO [101].
- Innovative medicinal strategies: Biologic medicines that address certain immunological system elements are now conventional PSO therapies. Further, new medicines are invented, such as small molecules, genetic treatments, and stem cell therapeutics [102].
- The skin microbiome’s dysbiosis has been linked to the emergence of psoriasis, according to research. As a result, various studies are concentrating on designing PSO-specific microbiome-based therapeutics.
- Artificial intelligence and neural networks: There is growing curiosity about employing artificial intelligence and machine learning to create improved psoriatic evaluations and therapy methodologies [103].
7. Biosafety
8. Future Perspectives and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PSO | Psoriasis |
| NPs | Nanoparticles |
| ITNPs | Intrinsically therapeutic nanoparticles |
| FDA | Food and Drug Administration |
| API | Active pharmaceutical ingredients |
| SLNPs | Solid lipid nanoparticles |
| NLCs | Nanostructured lipid carriers |
| HaCaT | Human keratinocyte |
| ROS | Reactive oxygen species |
| PDT | Photo-based therapy |
| TEWL | Trans epidermal water loss |
| NB-UVB | Narrowband UVB |
| PUVA | Psoralen plus UVA |
| CPT | Calcipotriol |
| EPS | Exopolysaccharides |
| ECM | Extracellular matrix |
| SC | Stratum corneum |
| IL | Interleukins |
| IFN | Interferons |
| AuNPs | Gold nanoparticles |
| MTX | Methotrexate |
| AgNPs | Silver nanoparticles |
| Cur | Curcumin |
| CSNPs | Chitosan nanoparticles |
| NFs | Nano formulations |
References
- Grän, F.; Kerstan, A.; Serfling, E.; Goebeler, M.; Muhammad, K. Current Developments in the Immunology of Psoriasis. Yale J. Biol. Med. 2020, 93, 97–110. [Google Scholar] [PubMed]
- Parisi, R.; Iskandar, I.Y.K.; Kontopantelis, E.; Augustin, M.; Griffiths, C.E.M.; Ashcroft, D.M.; Global Psoriasis Atlas. National, regional, and worldwide epidemiology of psoriasis: Systematic analysis and modelling study. BMJ 2020, 369, m1590. [Google Scholar] [CrossRef] [PubMed]
- Bs, S.E.L.; Cohen, J.M.; Ho, R.S. Psoriasis and suicidality: A review of the literature. Dermatol. Ther. 2019, 32, e12771. [Google Scholar]
- Armstrong, A.W.; Puig, L.; Joshi, A.; Skup, M.; Williams, D.; Li, J.; Betts, K.A.; Augustin, M. Comparison of biologics and oral treatments for plaque psoriasis: A meta-analysis. JAMA Dermatol. 2020, 156, 258–269. [Google Scholar] [CrossRef]
- Menter, A.; Strober, B.E.; Kaplan, D.H.; Kivelevitch, D.; Prater, E.F.; Stoff, B.; Armstrong, A.W.; Connor, C.; Cordoro, K.M.; Davis, D.M.R.; et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J. Am. Acad. Dermatol. 2019, 80, 1029–1072. [Google Scholar] [CrossRef]
- Kumari, S.; Goyal, A.; Garg, M.; Antonescu, A.; Sindhu, R.K. Lyotropic Liquid Crystal System for Drug Delivery of Astaxanthin: Physical Characterization and Enhanced Antioxidant Potential. Crystals 2023, 13, 142. [Google Scholar] [CrossRef]
- Gaspar-Pintiliescu, A.; Stanciuc, A.-M.; Craciunescu, O. Natural composite dressings based on collagen, gelatin and plant bioactive compounds for wound healing: A review. Int. J. Biol. Macromol. 2019, 138, 854–865. [Google Scholar] [CrossRef]
- Shrivastav, S.; Sindhu, R.; Kumar, S.; Kumar, P. Anti-psoriatic and phyto chemical evaluation of Thespesia populnea bark extracts. Int. J. Pharm. Pharm. Sci. 2009, 1, 176–185. [Google Scholar]
- Hawkes, J.E.; Chan, T.C.; Krueger, J.G. Psoriasis pathogenesis and the development of novel targeted immune therapies. J. Allergy Clin. Immunol. 2017, 140, 645–653. [Google Scholar] [CrossRef]
- Woo, Y.R.; Cho, D.H.; Park, H.J. Molecular mechanisms and management of a cutaneous inflammatory disorder: Psoriasis. Int. J. Mol. Sci. 2017, 18, 2684. [Google Scholar] [CrossRef]
- Sindhu, R.K.; Gupta, R.; Wadhera, G.; Kumar, P. Modern Herbal Nanogels: Formulation, Delivery Methods, and Applications. Gels 2022, 8, 97. [Google Scholar] [CrossRef]
- Pradhan, M.; Alexander, A.; Singh, M.R.; Singh, D.; Saraf, S.; Saraf, S. Understanding the prospective of nano-formulations towards the treatment of psoriasis. Biomed. Pharmacother. 2018, 107, 447–463. [Google Scholar] [CrossRef]
- Lorthois, I.; Simard, M.; Morin, S.; Pouliot, R. Infiltration of T Cells into a Three-Dimensional Psoriatic Skin Model Mimics Pathological Key Features. Int. J. Mol. Sci. 2019, 20, 1670. [Google Scholar] [CrossRef]
- Rizwan, S.B.; Boyd, B.J.; Rades, T.; Hook, S. Bicontinuous cubic liquid crystals as sustained delivery systems for peptides and proteins. Expert Opin. Drug Deliv. 2010, 7, 1133–1144. [Google Scholar] [CrossRef]
- Pezzolo, E.; Cazzaniga, S.; Colombo, P.; Chatenoud, L.; Naldi, L. Psoriasis incidence and lifetime prevalence: Suggestion for a higher mortality rate in older age-classes among psoriatic patients compared to the general population in Italy. Acta Derm. Venereol. 2019, 99, 400–403. [Google Scholar] [CrossRef]
- Finsterbusch, M.; Schrottmaier, W.C.; Kral-Pointner, J.B.; Salzmann, M.; Assinger, A. Measuring and interpreting platelet-leukocyte aggregates. Platelets 2018, 29, 677–685. [Google Scholar] [CrossRef]
- Luo, Y.; Hara, T.; Kawashima, A.; Ishido, Y.; Suzuki, S.; Ishii, N.; Kambara, T.; Suzuki, K. Pathological role of excessive DNA as a trigger of keratinocyte proliferation in psoriasis. Clin. Exp. Immunol. 2020, 202, 1–10. [Google Scholar] [CrossRef]
- Armstrong, A.W.; Read, C. Pathophysiology, clinical presentation, and treatment of psoriasis: A review. JAMA 2020, 323, 1945–1960. [Google Scholar] [CrossRef]
- Santalices, I.; Gonella, A.; Torres, D.; Alonso, M.J. Advances on the formulation of proteins using nanotechnologies. J. Drug Deliv. Sci. Technol. 2017, 42, 155–180. [Google Scholar] [CrossRef]
- Li, D.; Wang, W.; Wu, Y.; Ma, X.; Zhou, W.; Lai, Y. Lipopeptide 78 from Staphylococcus epidermidis activates beta-catenin to inhibit skin inflammation. J. Immunol. 2019, 202, 1219–1228. [Google Scholar] [CrossRef]
- Hawkes, J.E.; Yan, B.Y.; Chan, T.C.; Krueger, J.G. Discovery of the IL-23/IL-17 Signaling Pathway and the Treatment of Psoriasis. J. Immunol. 2018, 201, 1605. [Google Scholar] [CrossRef] [PubMed]
- Galimova, E.S.; Akhmetova, V.L.; Khusnutdinova, E.K. Molecular genetic basis of susceptibility to psoriasis. Russ. J. Genet. 2008, 44, 513–522. [Google Scholar] [CrossRef] [PubMed]
- Luba, K.M.; Stulberg, D.L. Chronic plaque psoriasis. S. Afr. Fam. Pract. 2006, 48, 20–29. [Google Scholar] [CrossRef]
- Syed, Z.U.; Khachemoune, A. Inverse psoriasis. Am. J. Clin. Dermatol. 2011, 12, 143–146. [Google Scholar] [CrossRef]
- Chalmers, R.J.G.; O’sullivan, T.; Owen, C.M.; Griffiths, C.E.M. A systematic review of treatments for guttate psoriasis. Br. J. Dermatol. 2001, 145, 891–894. [Google Scholar] [CrossRef]
- Farber, E.M.; Nall, L. Nail psoriasis. Cutis 1992, 50, 174–178. [Google Scholar]
- Ritchlin, C.T.; Colbert, R.A.; Gladman, D.D. Psoriatic arthritis. N. Engl. J. Med. 2017, 376, 957–970. [Google Scholar] [CrossRef]
- Liao, W.; Singh, R.K.; Lee, K.M.; Ucmak, D.; Brodsky, M.; Atanelov, Z.; Farahnik, B.; Abrouk, M.; Nakamura, M.; Zhu, T.H. Erythrodermic psoriasis: Pathophysiology and current treatment perspectives. Psoriasis Targets Ther. 2016, ume 6, 93–104. [Google Scholar] [CrossRef]
- Gooderham, M.J.; Van Voorhees, A.S.; Lebwohl, M.G. An update on generalized pustular psoriasis. Expert Rev. Clin. Immunol. 2019, 15, 907–919. [Google Scholar] [CrossRef]
- Florek, A.G.; Wang, C.J.; Armstrong, A.W. Treatment preferences and treatment satisfaction among psoriasis patients: A systematic review. Arch. Dermatol. Res. 2018, 310, 271–319. [Google Scholar] [CrossRef]
- Wollina, U.; Tirant, M.; Vojvodic, A.; Lotti, T. Treatment of Psoriasis: Novel Approaches to Topical Delivery. Open Access Maced. J. Med. Sci. 2019, 7, 3018–3025. [Google Scholar] [CrossRef]
- Bouwstra, J.A.; Honeywell-Nguyen, P.L. Skin structure and mode of action of vesicles. Adv. Drug Deliv. Rev. 2002, 54 (Suppl. S1), S41–S55. [Google Scholar] [CrossRef]
- Schatzlein, A.; Cevc, G. Non-uniform cellular packing of the stratum corneum and permeability barrier function of intact skin: A high-resolution confocal laser scanning microscopy study using highly deformable vesicles (Transfersomes). Br. J. Derm. 1998, 138, 583–592. [Google Scholar] [CrossRef]
- Cheng, C.-Y.; Lin, Y.-K.; Yang, S.-C.; Alalaiwe, A.; Lin, C.-J.; Fang, J.-Y.; Lin, C.-F. Percutaneous absorption of resveratrol and its oligomers to relieve psoriasiform lesions: In silico, in vitro and in vivo evaluations. Int. J. Pharm. 2020, 585, 119507. [Google Scholar] [CrossRef]
- Chen, H.F.; Wang, Z.Y.; Chen, J.J.; Fan, X.P.; Qian, G.D. Preparation and aging behaviour of nano SiO2 modified PEA coating by in-situ polymerization. Rare Metal Mat. Eng. 2004, 33, 9–12. [Google Scholar]
- Khameneh, B.; Halimi, V.; Jaafari, M.R.; Golmohammadzadeh, S. Safranal-loaded solid lipid nanoparticles: Evaluation of sunscreen and moisturizing potential for topical applications. Iran J. Basic Med. Sci. 2015, 18, 58–63. [Google Scholar]
- Troccaz, M.; Gaïa, N.; Beccucci, S.; Schrenzel, J.; Cayeux, I.; Starkenmann, C.; Lazarevic, V. Mapping axillary microbiota responsible for body odours using a culture-independent approach. Microbiome 2015, 3, 3. [Google Scholar] [CrossRef]
- Carter, P.; Narasimhan, B.; Wang, Q. Biocompatible nanoparticles and vesicular systems in transdermal drug delivery for various skin diseases. Int. J. Pharm. 2019, 555, 49–62. [Google Scholar] [CrossRef]
- Hossain, K.M.Z.; Patel, U.; Ahmed, I. Development of microspheres for biomedical applications: A review. Prog. Biomater. 2015, 4, 1–19. [Google Scholar] [CrossRef]
- Fratoddi, I.; Benassi, L.; Botti, E.; Vaschieri, C.; Venditti, I.; Bessar, H.; Samir, M.A.; Azzoni, P.; Magnoni, C.; Costanzo, A.; et al. Effects of topical methotrexate loaded gold nanoparticle in cutaneous inflammatory mouse model. Nanomed. Nanotechnol. Biol. Med. 2019, 17, 276–286. [Google Scholar] [CrossRef]
- Badhe, K.P.; Saudagar, R. A Review on Microsponge a Novel Drug Delivery System. Asian J. Pharm. Res. 2016, 6, 51. [Google Scholar] [CrossRef]
- Goebel, A.S.; Neubert, R.H.; Wohlrab, J. Dermal targeting of tacrolimus using colloidal carrier systems. Int. J. Pharm. 2011, 404, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Erdal, M.S.; Özhan, G.; Mat, M.C.; Özsoy, Y.; Güngör, S. Colloidal nanocarriers for the enhanced cutaneous delivery of naftifine: Characterization studies and in vitro and in vivo evaluations. Int. J. Nanomed. 2016, 11, 1027–1037. [Google Scholar] [CrossRef] [PubMed]
- Gungor, S.; Rezigue, M. Nanocarriers mediated topical drug delivery for psoriasis treatment. Curr. Drug Metabol. 2017, 18, 454–468. [Google Scholar] [CrossRef]
- Cho, H.; Lai, T.C.; Tomoda, K.; Kwon, G.S. Polymeric micelles for multi-drug delivery in cancer. AAPS PharmSciTech. 2015, 16, 10–20. [Google Scholar] [CrossRef]
- Mahant, S.; Kumar, S.; Nanda, S.; Rao, R. Microsponges for dermatological applications: Perspectives and challenges. Asian J. Pharm. Sci. 2020, 15, 273–291. [Google Scholar] [CrossRef]
- Lee, J.H.; Jung, Y.S.; Kim, G.M.; Bae, J.M. A hyaluronic acid-based microneedle patch to treat psoriatic plaques: A pilot open trial. Br. J. Dermatol. 2018, 178, e24–e25. [Google Scholar] [CrossRef]
- Waghule, T.; Singhvi, G.; Dubey, S.K.; Pandey, M.M.; Gupta, G.; Singh, M.; Dua, K. Microneedles: A smart approach and increasing potential for transdermal drug delivery system. Biomed. Pharmacother. 2019, 109, 1249–1258. [Google Scholar] [CrossRef]
- Bulbake, U.; Doppalapudi, S.; Kommineni, N.; Khan, W. Liposomal Formulations in Clinical Use: An Updated Review. Pharmaceutics 2017, 9, 12. [Google Scholar] [CrossRef]
- Sathe, P.; Saka, R.; Kommineni, N.; Raza, K.; Khan, W. Dithranol-loaded nanostructured lipid carrier-based gel ameliorate psoriasis in imiquimod-induced mice psoriatic plaque model. Drug Dev. Ind. Pharm. 2019, 45, 826–838. [Google Scholar] [CrossRef]
- Schwarz, J.C.; Baisaeng, N.; Hoppel, M.; Löw, M.; Keck, C.M.; Valenta, C. Ultra-small NLC for improved dermal delivery of coenyzme Q10. Int. J. Pharm. 2013, 447, 213–217. [Google Scholar] [CrossRef]
- Beloqui, A.; Solinís, M.A.; Rodríguez-Gasón, A.; Almeida, A.J.; Préat, V. Nanostructured lipid carriers: Promising drug delivery systems for future clinics, Nanomed. Nanotechnol. Biol. Med. 2016, 12, 143–161. [Google Scholar] [CrossRef]
- Prasad, V.; Chaurasia, S. Performance evaluation of non-ionic surfactant based tazarotene encapsulated proniosomal gel for the treatment of psoriasis. Mater. Sci. Eng. C 2017, 79, 168–176. [Google Scholar] [CrossRef]
- Pradhan, M. Solid lipid nanoparticles: A potential carrier for transdermal drug delivery. Hum. J. Rev. Artic. 2016, 7, 627–641. [Google Scholar]
- Kumari, S.; Goyal, A.; Sönmez Gürer, E.; Algın Yapar, E.; Garg, M.; Sood, M.; Sindhu, R.K. Bioactive Loaded Novel Nano-Formulations for Targeted Drug Delivery and Their Therapeutic Potential. Pharmaceutics 2022, 14, 1091. [Google Scholar] [CrossRef]
- Lauterbach, A.; Müller-Goymann, C.C. Applications and limitations of lipid nanoparticles in dermal and transdermal drug delivery via the follicular route. Eur. J. Pharm. Biopharm. 2015, 97, 152–163. [Google Scholar] [CrossRef]
- Pradhan, M.; Singh, D.; Singh, M.R. Novel colloidal carriers for psoriasis: Current issues, mechanistic insight and novel delivery approaches. J. Control. Release 2013, 170, 380–395. [Google Scholar] [CrossRef]
- Gupta, M.; Agrawal, U.; Vyas, S.P. Nanocarrier-based topical drug delivery for the treatment of skin diseases. Expert Opin. Drug Deliv. 2012, 9, 783–804. [Google Scholar] [CrossRef]
- Pabreja, S.; Garg, T.; Rath, G.; Goyal, A.K. Mucosal vaccination against tuberculosis using Ag85A-loaded immunostimulating complexes. Artif. Cells Nanomed. Biotechnol. 2016, 44, 532–539. [Google Scholar] [CrossRef]
- Rohilla, R.; Garg, T.; Bariwal, J.; Goyal, A.K.; Rath, G. Development, optimization and characterization of glycyrrhetinic acid–chitosan nanoparticles of atorvastatin for liver targeting. Drug Deliv. 2016, 23, 2290–2297. [Google Scholar] [CrossRef]
- Rajan, R.; Jose, S.; Mukund, V.B.; Vasudevan, D.T. Transferosomes—A vesicular transdermal delivery system for enhanced drug permeation. J. Adv. Pharm. Technol. Res. 2011, 2, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Garg, T.; Rath, G.; Goyal, A.K. Nanotechnological approaches for the effective management of psoriasis. Artif. Cells Nanomed. Biotechnol. 2016, 44, 1374–1382. [Google Scholar] [CrossRef] [PubMed]
- Tekade, R.K.; Kumar, P.V.; Jain, N.K. Dendrimers in Oncology: An Expanding Horizon. Chem. Rev. 2009, 109, 49–87. [Google Scholar] [CrossRef] [PubMed]
- Shaif, M.; Kushwaha, P.; Usmani, S.; Pandey, S. Exploring the potential of nanocarriers in antipsoriatic therapeutics. J. Dermatolog. Treat. 2022, 33, 2919–2930. [Google Scholar] [CrossRef]
- Morin, A.; Simard, M.; Rioux, G.; Grenier, A.; Morin, S.; Pouliot, R. Application of an In Vitro Psoriatic Skin Model to Study Cutaneous Metabolization of Tazarotene. Processes 2019, 7, 871. [Google Scholar] [CrossRef]
- Benezeder, T.; Painsi, C.; Patra, V.; Dey, S.; Holcmann, M.; Lange-Asschenfeldt, B.; Sibilia, M.; Wolf, P. Dithranol targets keratinocytes, their crosstalk with neutrophils and inhibits the IL-36 inflammatory loop in psoriasis. eLife 2020, 9, e56991. [Google Scholar] [CrossRef]
- Van de Kerkhof, P.C.M.; de Gruijl, F.R. Phototherapy in the perspective of the chronicity of psoriasis. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 926–931. [Google Scholar] [CrossRef]
- Elmets, C.A.; Lim, H.W.; Stoff, B.; Connor, C.; Cordoro, K.M.; Lebwohl, M.; Armstrong, A.W.; Davis, D.M.R.; Elewski, B.E.; Gelfand, J.M.; et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis with phototherapy. J. Am. Acad. Dermatol. 2019, 81, 775–804. [Google Scholar] [CrossRef]
- Hyde, K.; Cardwell, L.A.; Stotts, R.; Feldman, S.R. Psoriasis Treatment Cost Comparison: Biologics Versus Home Phototherapy. Am. J. Pharm. Benefits 2018, 10, 18–21. [Google Scholar]
- Liebmann, J.; Born, M.; Kolb-Bachofen, V. Blue-light irradiation regulates proliferation and differentiation in human skin cells. J. Investig. Dermatol. 2010, 130, 259–269. [Google Scholar] [CrossRef]
- Jin, Y.; Zhang, X.; Zhang, B.; Kang, H.; Du, L.; Li, M. Nanostructures of an amphiphilic zinc phthalocyanine polymer conjugate for photodynamic therapy of psoriasis. Colloids Surf. B Biointerfaces 2015, 128, 405–409. [Google Scholar] [CrossRef]
- Wang, X.L.; Wang, H.W.; Yuan, K.H.; Li, F.L.; Huang, Z. Combination of photodynamic therapy and immunomodulation for skin diseases—Update of clinical aspects. Photochem. Photobiol. Sci. 2011, 10, 704–711. [Google Scholar] [CrossRef]
- Larisch, P.; Verwanger, T.; Linecker, M.; Krammer, B. The interrelation between a pro-inflammatory milieu and fluorescence diagnosis or photodynamic therapy of human skin cell lines. Photodiagn. Photodyn. Ther. 2014, 11, 91–103. [Google Scholar] [CrossRef]
- Yiu, Z.Z.; Warren, R.B. Efficacy and safety of emerging immunotherapies in psoriasis. Immunotherapy 2015, 7, 119–133. [Google Scholar] [CrossRef]
- Jadhav, K.R.; Shaikh, I.M.; Ambade, K.W.; Kadam, V.J. Applications of microemulsion based drug delivery system. Curr. Drug Deliv. 2006, 3, 267–273. [Google Scholar] [CrossRef]
- Wine-Lee, L.; Keller, S.C.; Wilck, M.B.; Gluckman, S.J.; Van Voorhees, A.S. From the Medical Board of the National Psoriasis Foundation: Vaccination in adult patients on systemic therapy for psoriasis. J. Am. Acad. Dermatol. 2013, 69, 1003–1013. [Google Scholar] [CrossRef]
- Juhaščik, M.; Kováčik, A.; Huerta-Ángeles, G. Recent Advances of Hyaluronan for Skin Delivery: From Structure to Fabrication Strategies and Applications. Polymers 2022, 14, 4833. [Google Scholar] [CrossRef]
- Frieder, J.; Kivelevitch, D.; Menter, A. Calcipotriene betamethasone dipropionate aerosol foam in the treatment of plaque psoriasis: A review of the literature. Ther. Deliv. 2017, 8, 737–746. [Google Scholar] [CrossRef]
- Najafi-Taher, R.; Ghaemi, B.; Amani, A. Delivery of adapalene using a novel topical gel based on tea tree oil nano-emulsion: Permeation, antibacterial and safety assessments. Eur. J. Pharm. Sci. 2018, 120, 142. [Google Scholar] [CrossRef]
- Song, B.; Song, R.; Cheng, M.; Chu, H.; Yan, F.; Wang, Y. Preparation of Calcipotriol Emulsion Using Bacterial Exopolysaccharides as Emulsifier for Percutaneous Treatment of Psoriasis Vulgaris. Int. J. Mol. Sci. 2020, 21, 77. [Google Scholar] [CrossRef]
- Kornhauser, A. Applications of hydroxy acids: Classification, mechanisms, and photoactivity. Clin. Cosmet. Investig. Dermatol. 2010, 3, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.M.; Ascenso, A.; Ribeiro, H.M.; Marto, J. Current and Future Therapies for Psoriasis with a Focus on Serotonergic Drugs. Mol. Neurobiol. 2020, 57, 2391–2419. [Google Scholar] [CrossRef] [PubMed]
- Singhvi, G.; Hejmady, S.; Rapalli, V.K.; Dubey, S.K.; Dubey, S. Nanocarriers for topical delivery in psoriasis. Deliv. Drugs 2020, 2, 75–96. [Google Scholar]
- Mitsutake, H.; Ribeiro, L.N.M.; da Silva, G.H.R.; Castro, S.R.; de Paula, E.; Poppi, R.J.; Breitkreitz, M.C. Evaluation of miscibility and polymorphism of synthetic and natural lipids for nanostructured lipid carrier (NLC) formulations by Raman mapping and multivariate curve resolution (MCR). Eur. J. Pharm. Sci. 2019, 135, 51–59. [Google Scholar] [CrossRef]
- Crisan, D.; Scharffetter-Kochanek, K.; Crisan, M.; Schatz, S.; Hainzl, A.; Olenic, L.; Filip, A.; Schneider, L.A.; Sindrilaru, A. Topical silver and gold nanoparticles complexed with Cornus mas suppress inflammation in human psoriasis plaques by inhibiting NF-κB activity. Exp. Dermatol. 2018, 27, 1166–1169. [Google Scholar] [CrossRef]
- Nair, R.S.; Morris, A.; Billa, N.; Leong, C.-O. An Evaluation of Curcumin-Encapsulated Chitosan Nanoparticles for Transdermal Delivery. AAPS PharmSciTech 2019, 20, 69. [Google Scholar] [CrossRef]
- Abdel-Hafez, S.M.; Hathout, R.M.; Sammour, O.A. Tracking the transdermal penetration pathways of optimized curcumin-loaded chitosan nanoparticles via confocal laser scanning microscopy. Int. J. Biol. Macromol. 2018, 108, 753–764. [Google Scholar] [CrossRef]
- Shende, P.; Gupta, H. Formulation and comparative characterization of nanoparticles of curcumin using natural, synthetic and semi-synthetic polymers for wound healing. Life Sci. 2020, 253, 117588. [Google Scholar] [CrossRef]
- Li, F.; Shi, Y.; Liang, J.; Zhao, L. Curcumin-loaded chitosan nanoparticles promote diabetic wound healing via attenuating inflammation in a diabetic rat model. J. Biomater. Appl. 2019, 34, 476–486. [Google Scholar] [CrossRef]
- Saheb, M.; Fereydouni, N.; Nemati, S.; Barreto, G.E.; Johnston, T.P.; Sahebkar, A. Chitosan-based delivery systems for curcumin: A review of pharmacodynamic and pharmacokinetic aspects. J. Cell Physiol. 2019, 234, 12325–12340. [Google Scholar] [CrossRef]
- Ali, A.; Ahmed, S. A review on chitosan and its nanocomposites in drug delivery. Int. J. Biol. Macromol. 2018, 109, 273–286. [Google Scholar] [CrossRef]
- Muangnoi, C.; Jithavech, P.; Ratnatilaka Na Bhuket, P.; Supasena, W.; Wichitnithad, W.; Towiwat, P.; Niwattisaiwong, N.; Haworth, I.S.; Rojsitthisak, P. A curcumin-diglutaric acid conjugated prodrug with improved water solubility and antinociceptive properties compared to curcumin. Biosci. Biotechnol. Biochem. 2018, 82, 1301–1308. [Google Scholar] [CrossRef]
- Luckanagul, J.A.; Pitakchatwong, C.; Ratnatilaka Na Bhuket, P.; Muangnoi, C.; Rojsitthisak, P.; Chirachanchai, S.; Wang, Q.; Rojsitthisak, P. Chitosan-based polymer hybrids for thermo-responsive nanogel delivery of curcumin. Carbohydr. Polym. 2018, 181, 1119–1127. [Google Scholar] [CrossRef]
- Aljuffali, I.A.; Lin, C.H.; Yang, S.C.; Alalaiwe, A.; Fang, J.Y. Nanoencapsulation of tea catechins for enhancing skin absorption and therapeutic efficacy. AAPS PharmSciTech 2022, 23, 187. [Google Scholar] [CrossRef]
- Gentilini, R.; Bozzini, S.; Munarin, F.; Petrini, P.; Visai, L.; Tanzi, M.C. Pectins from aloe vera: Extraction and production of gels for regenerative medicine. J. Appl. Polym. Sci. 2014, 131, 39760. [Google Scholar] [CrossRef]
- Varma, S.R.; Sivaprakasam, T.O.; Mishra, A.; Prabhu, S.; Rafiq, M.; Rangesh, P. Imiquimod-induced psoriasis-like inflammation in differentiated human keratinocytes: Its evaluation using curcumin. Eur. J. Pharmacol. 2017, 813, 33–41. [Google Scholar] [CrossRef]
- Li, Y.L.; Du, Z.Y.; Li, P.H.; Yan, L.; Zhou, W.; Tang, Y.D.; Liu, G.R.; Fang, Y.X.; Zhang, K.; Dong, C.Z.; et al. Aromatic-turmerone ameliorates imiquimod-induced psoriasis-like inflammation of BALB/c mice. Int. Immunopharmacol. 2018, 64, 319–325. [Google Scholar] [CrossRef]
- Zhou, W.; Liu, W.; Zou, L.; Liu, W.; Liu, C.; Liang, R.; Chen, J. Storage stability and skin permeation of vitamin C liposomes improved by pectin coating. Colloids Surf. B Biointerfaces 2014, 117, 330–337. [Google Scholar] [CrossRef]
- Nesseem, D. Formulation of sunscreens with enhancement sun protection factor response based on solid lipid nanoparticles. Int. J. Cosmet. Sci. 2011, 33, 70–79. [Google Scholar] [CrossRef]
- Soeur, J.; Eilstein, J.; Lereaux, G.; Jones, C.; Marrot, L. Skin resistance to oxidative stress induced by resveratrol: From Nrf2 activation to GSH biosynthesis. Free Radic Biol. Med. 2015, 78, 213–223. [Google Scholar] [CrossRef]
- Farris, P. Idebenone, green tea, and coffeeberry extract: New and innovative antioxidants. Dermatol. Ther. 2007, 20, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Parveen, S.; Ahmed, M.; Baboota, S.; Ali, J. An Innovative Approach in Nanotechnology-based Delivery System for the Effective Management of Psoriasis. Curr. Pharm. Des. 2022, 28, 1082–1102. [Google Scholar] [PubMed]
- Patil, T.S.; Gujarathi, N.A.; Aher, A.A.; Pachpande, H.E.; Sharma, C.; Ojha, S.; Goyal, S.N.; Agrawal, Y.O. Recent Advancements in Topical Anti-Psoriatic Nanostructured Lipid Carrier-Based Drug Delivery. Int. J. Mol. Sci. 2023, 24, 2978. [Google Scholar] [CrossRef] [PubMed]
- Yadav, N.; Aggarwal, R.; Targhotra, M.; Sahoo, P.K.; Chauhan, M.K. Natural and Nanotechnology Based Treatment: An Alternative Approach to Psoriasis. Curr. Nanomed. 2021, 11, 21–39. [Google Scholar] [CrossRef]
- Burak, C.; Brüll, V.; Langguth, P.; Zimmermann, B.F.; Stoffel-Wagner, B.; Sausen, U.; Stehle, P.; Wolffram, S.; Egert, S. Higher plasma quercetin levels following oral administration of an onion skin extract compared with pure quercetin dihydrate in humans. Eur. J. Nutr. 2015, 18, 600–615. [Google Scholar] [CrossRef]
- Lopes, L.B.; VanDeWall, H.; Li, H.T.; Venugopal, V.; Li, H.K.; Naydin, S.; Hosmer, J.; Levendusky, M.; Zheng, H.; Bentley, M.V.L.; et al. Topical Delivery of Lycopene using Microemulsions: Enhanced Skin Penetration and Tissue Antioxidant Activity. J. Pharm. Sci. 2010, 99, 1346–1357. [Google Scholar] [CrossRef]
- Kang, N.W.; Kim, M.H.; Sohn, S.Y.; Kim, K.T.; Park, J.H.; Lee, S.Y.; Lee, J.Y.; Kim, D.D. Curcumin-loaded lipid-hybridized cellulose nanofiber film ameliorates imiquimod-induced psoriasis-like dermatitis in mice. Biomaterials 2018, 182, 245–258. [Google Scholar] [CrossRef]
- Nwabudike, L.C.; Tatu, A.L. Response to—Chronic exposure to tetracyclines and subsequent diagnosis for non-melanoma skin cancer in a large Mid-Western US population. J. Eur. Acad. Dermatol. Venereol. 2018, 32, e159. [Google Scholar] [CrossRef]
- Brănișteanu, D.E.; Ianoşi, S.L.; Dimitriu, A.; Stoleriu, G.; Oanţǎ, A.; Brănișteanu, D.C. Drug-induced Rowell syndrome, a rare and difficult to manage disease: A case report. Exp. Ther. Med. 2018, 15, 785–788. [Google Scholar] [CrossRef]
- Martinez-Lopez, A.; Blasco-Morente, G.; Perez-Lopez, I.; Tercedor-Sanchez, J.; Arias-Santiago, S. Studying the effect of systemic and biological drugs on intima-media thickness in patients suffering from moderate and severe psoriasis. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 1492–1498. [Google Scholar] [CrossRef]



| S.No | Bioactive Products | Functions | Reference |
|---|---|---|---|
| 1. | Nano anti-aging agents | cause collagen to lose physical appearance | [35] |
| 2. | Nano moisturizers | generate a thin film/moisture-avoiding shield on the body’s external layer | [36] |
| 3. | Nano skin cleansers | encourage the clearance of epidermal layer germs, resulting in less odor formation | [37] |
| 4. | Nano sunscreens | avoid extensive UV ray exposure and discomfort. | [38] |
| Phytoconstituents | Characteristics | Functions | Reference |
|---|---|---|---|
| Aloe vera | Antiseptic, anti-inflammatory, wound-healing, and anti-diabetic properties. | Enhances the synthesis of collagen and elastin fibers. | [75] |
| Curcumin | Anti-inflammatory, anticarcinogenic, antioxidant, antimicrobial and wound-healing. | Inhibits the inflammation and that of keratinocyte abnormal proliferation resides on nuclear factor-κB (NF-κB) suppression, TNF-α, IL-1β and IL-6 downregulation. | [76,77] |
| Nanovitamin C | Enhanced stability and higher antioxidant activity. | Enhances the carrier of the vitamin against apoptotic effects. | [78] |
| Nanovitamin E | Antiwrinkle, enhanced skin moisturizing, and prevention of skin disease. | Prepared using solid lipid nanoparticle delivery systems with a size equivalent to 292 nm and enhanced skin protection activity. | [79] |
| Nanoresveratrol | Functional foods for skincare and health. | Enhanced resveratrol bioavailability to the skin to protect against UV radiation. | [80] |
| Nanogreen tea | Skincare roles such as anti-aging and prevention of UV-induced photoaging. | Techniques enhance the bioavailability of these compounds in cosmeceutical products. | [81] |
| Nanoquercetin | Efficiency in skin and beauty care through antioxidant activities | Enhanced beauty due to its abundance of OH groups. | [82] |
| Nanolycopene | Skincare, including anti-aging and antioxidant activity. | Enhanced bioavailability to the skin with potential antioxidant activity. It enhances the penetration of lycopene to the inner cell and nucleus, which could be useful in skin protection and care. | [83,84] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thirumal, D.; Sindhu, R.K.; Goyal, S.; Sehgal, A.; Kumar, A.; Babu, M.A.; Kumar, P. Pathology and Treatment of Psoriasis Using Nanoformulations. Biomedicines 2023, 11, 1589. https://doi.org/10.3390/biomedicines11061589
Thirumal D, Sindhu RK, Goyal S, Sehgal A, Kumar A, Babu MA, Kumar P. Pathology and Treatment of Psoriasis Using Nanoformulations. Biomedicines. 2023; 11(6):1589. https://doi.org/10.3390/biomedicines11061589
Chicago/Turabian StyleThirumal, Divya, Rakesh K. Sindhu, Shuchi Goyal, Aayush Sehgal, Ashok Kumar, Marianesan Arockia Babu, and Pradeep Kumar. 2023. "Pathology and Treatment of Psoriasis Using Nanoformulations" Biomedicines 11, no. 6: 1589. https://doi.org/10.3390/biomedicines11061589
APA StyleThirumal, D., Sindhu, R. K., Goyal, S., Sehgal, A., Kumar, A., Babu, M. A., & Kumar, P. (2023). Pathology and Treatment of Psoriasis Using Nanoformulations. Biomedicines, 11(6), 1589. https://doi.org/10.3390/biomedicines11061589







