The Use of Small-Molecule Compounds for Cell Adhesion and Migration in Regenerative Medicine
Abstract
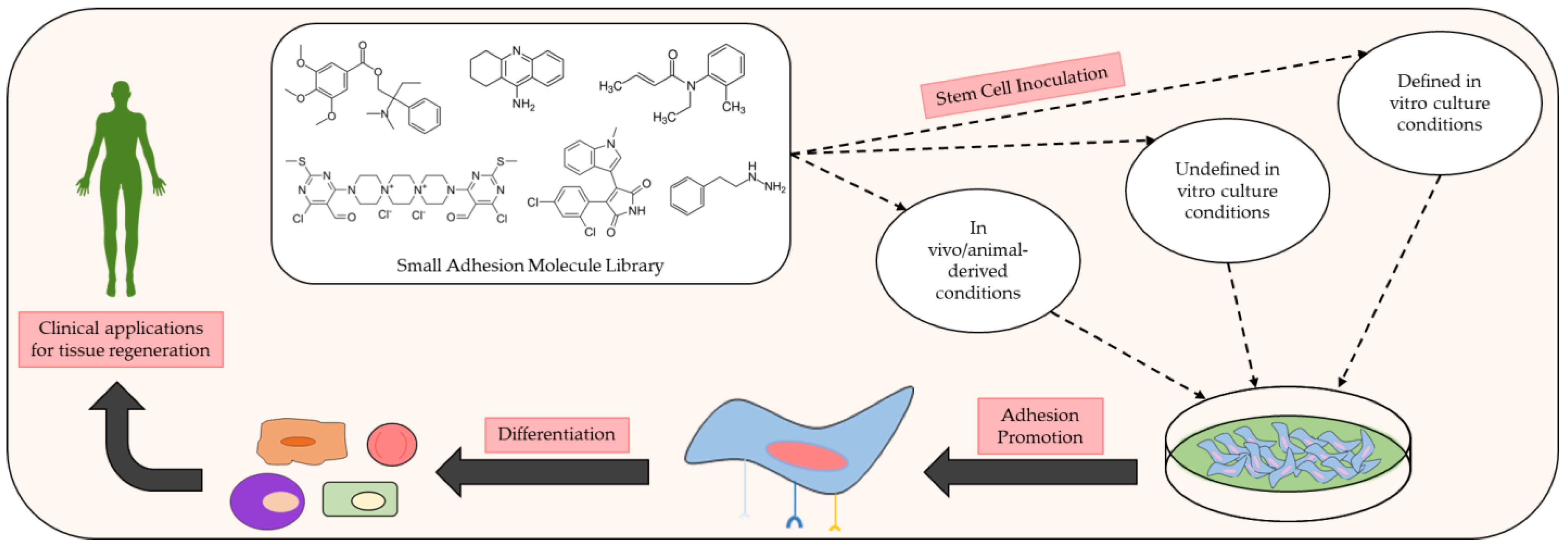
:1. Introduction
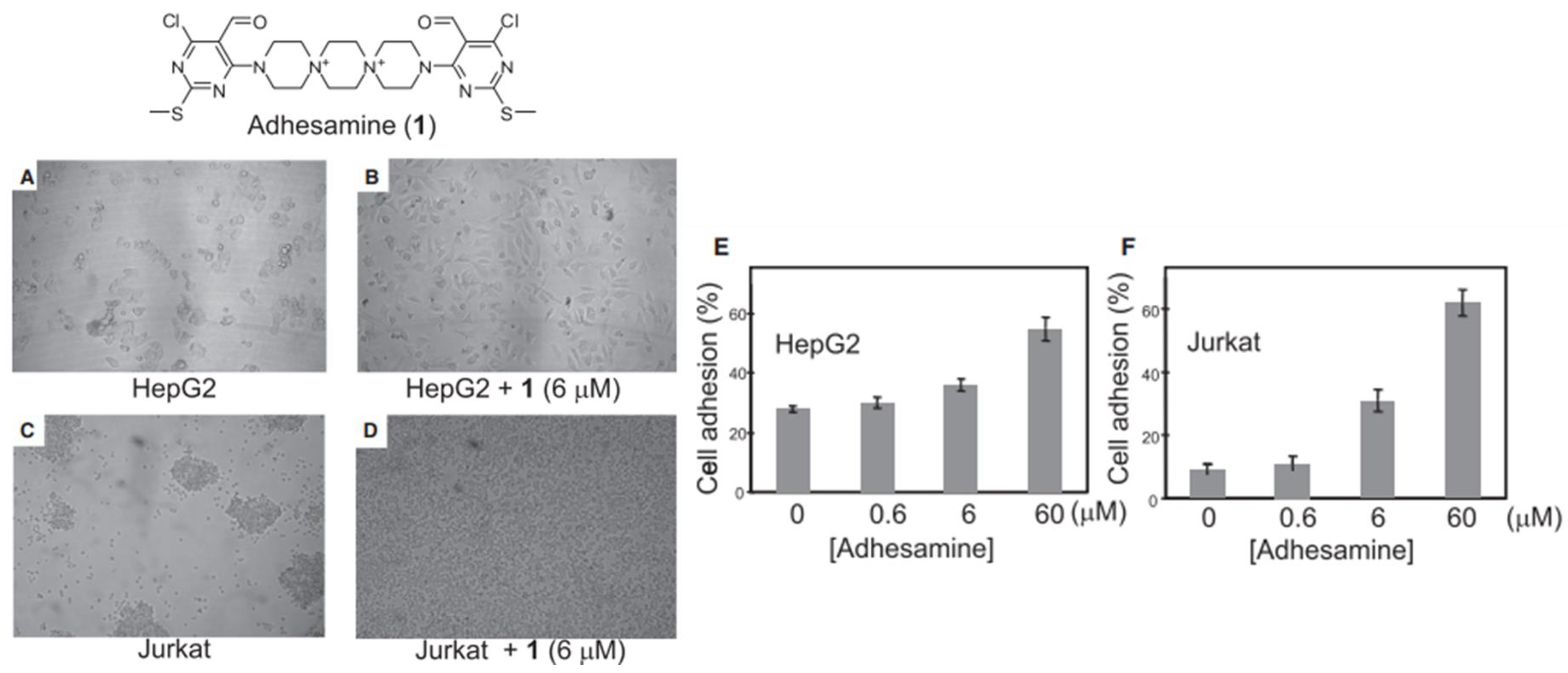
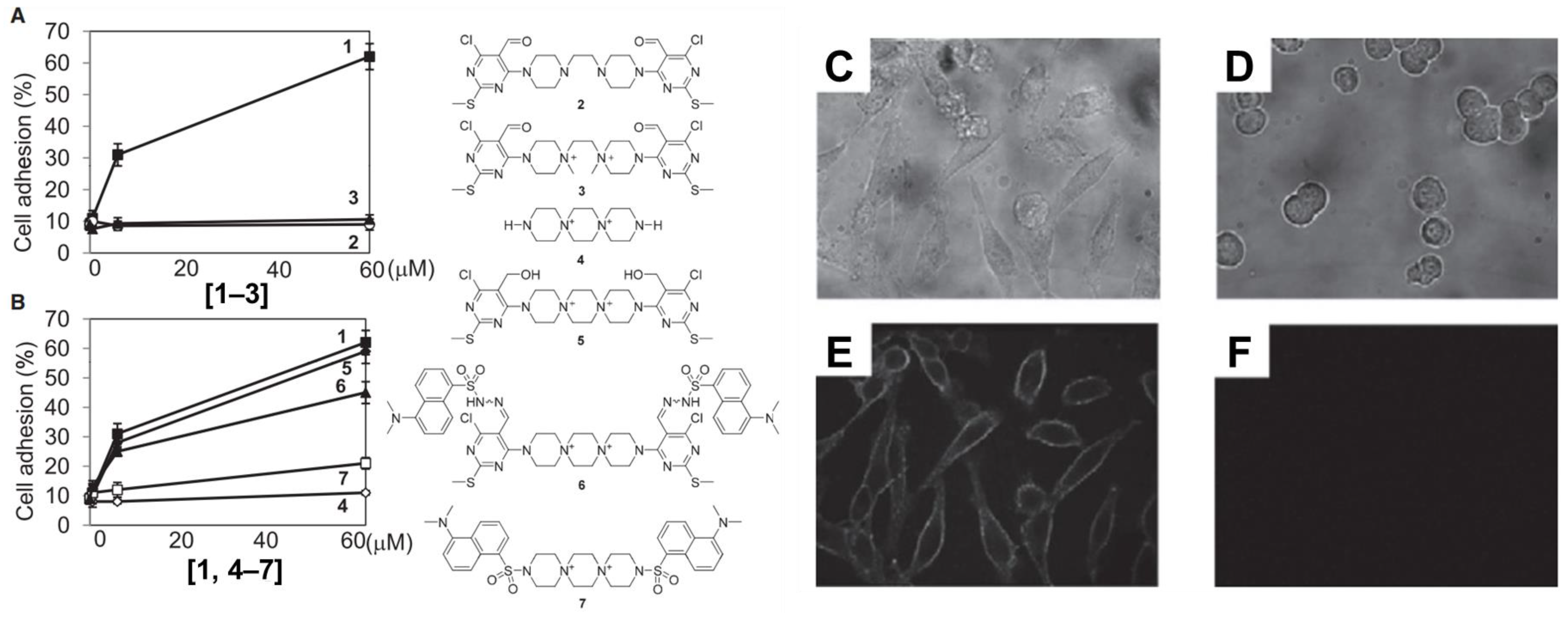
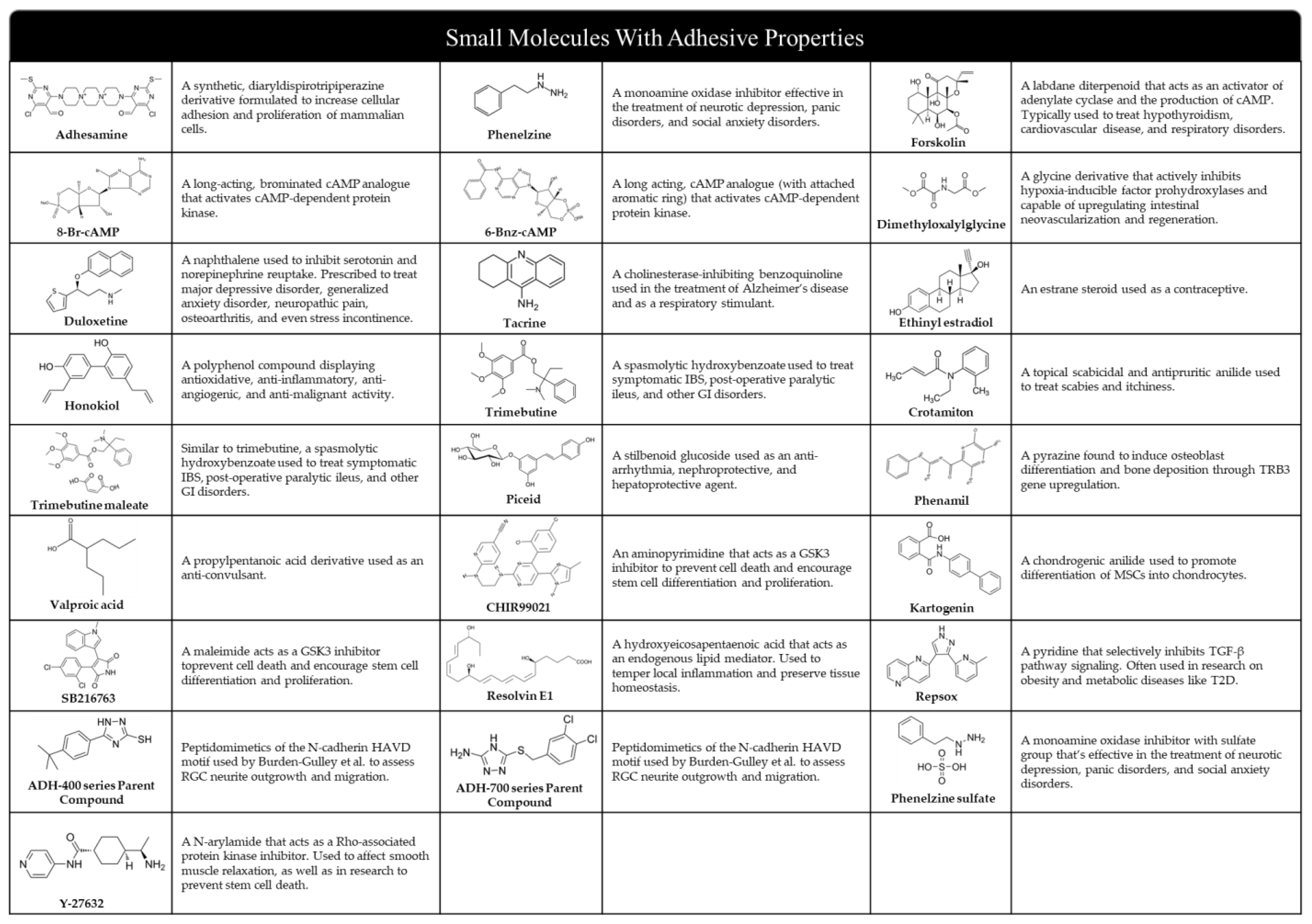
2. Adhesamine
3. L1CAM and L1 Agonists or Mimetics
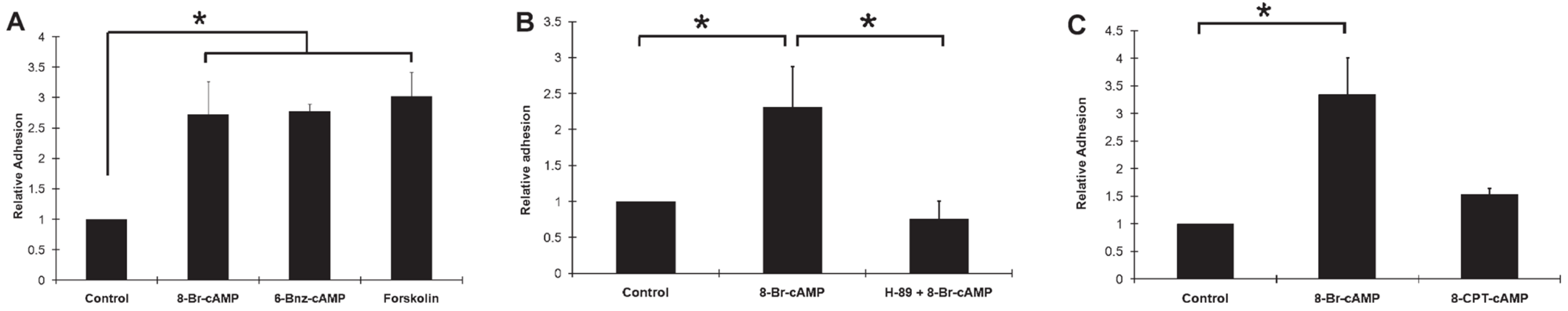
4. cAMP-Mediated Adhesion Utilizing Small Molecules
5. Other Identified Adhesive Small Molecules and Small Molecule-Incorporated Scaffolds or Gels
6. Concluding Remarks and Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Janiszewska, M.; Primi, M.C.; Izard, T. Cell adhesion in cancer: Beyond the migration of single cells. Perspect. Surg. 2020, 295, 2495–2505. [Google Scholar] [CrossRef]
- Wu, S.; Du, W.; Duan, Y.; Zhang, D.; Liu, Y.; Wu, B.; Gao, C. Regulating the migration of smooth muscle cells by a vertically distributed poly(2-hydroxyethyl methacrylate) gradient on polymer brushes covalently immobilized with RGD peptides. Acta Biomater. 2018, 75, 75–92. [Google Scholar] [CrossRef]
- Bolívar-Monsalve, E.J.; Alvarez, M.M.; Hosseini, S.; Espinosa-Hernandez, M.A.; Ceballos-González, C.F.; Sanchez-Dominguez, M.; Shin, S.R.; Cecen, B.; Hassan, S.; Di Maio, E.; et al. Engineering bioactive synthetic polymers for biomedical applications: A review with emphasis on tissue engineering and controlled release. Mater. Adv. 2021, 2, 4447–4478. [Google Scholar] [CrossRef]
- Khalili, A.A.; Ahmad, M.R. A Review of Cell Adhesion Studies for Biomedical and Biological Applications. Int. J. Mol. Sci. 2015, 16, 18149–18184. [Google Scholar] [CrossRef]
- Yang, W.; Sun, L.; Cai, S.; Chen, Y.; Liang, W.; Zhou, P.; Liu, L. Dynamically directing cell organization via micro-hump structure patterned cell-adhered interfaces. Lab Chip 2020, 20, 2447–2452. [Google Scholar] [CrossRef]
- Kukumberg, M.; Yao, Y.; Goh, S.H.; Neo, D.J.H.; Yao, J.Y.; Yim, E.K.F. Evaluation of the Topographical Influence on the Cellular Behavior of Human Umbilical Vein Endothelial Cells. Adv. Biosyst. 2018, 2, 1700217. [Google Scholar] [CrossRef]
- Chen, S.; Lewallen, M.; Xie, T. Adhesion in the stem cell niche: Biological roles and regulation. Development 2013, 140, 255–265. [Google Scholar] [CrossRef]
- Anselme, K. Osteoblast adhesion on biomaterials. Biomaterials 2000, 21, 667–681. [Google Scholar] [CrossRef]
- Rao, S.S.; Winter, J.O. Adhesion molecule-modified biomaterials for neural tissue engineering. Front. Neuroeng. 2009, 2, 6. [Google Scholar] [CrossRef]
- Özkaya, A.B.; Geyik, C. From viability to cell death: Claims with insufficient evidence in high-impact cell culture studies. PLoS ONE 2022, 17, e0250754. [Google Scholar] [CrossRef]
- Kim, H.S.; Kumbar, S.G.; Nukavarapu, S.P. Biomaterial-directed cell behavior for tissue engineering. Curr. Opin. Biomed. Eng. 2021, 17, 100260. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Jacob, R.S.; Patel, K.; Singh, N.; Maji, S.K. Amyloid Fibrils: Versatile Biomaterials for Cell Adhesion and Tissue Engineering Applications. Biomacromolecules 2018, 19, 1826–1839. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Hu, S.; Christy, J.; Chou, F.; Ramli, T.C.; Chen, H. Biointerface Coatings With Structural and Biochemical Properties Modifications of Biomaterials. Adv. Mater. Interfaces 2023, 10, 2202286. [Google Scholar] [CrossRef]
- Neděla, O.; Slepička, P.; Švorčík, V. Surface Modification of Polymer Substrates for Biomedical Applications. Materials 2017, 10, 1115. [Google Scholar] [CrossRef]
- Pang, X.; He, X.; Qiu, Z.; Zhang, H.; Xie, R.; Liu, Z.; Cui, Y. Targeting integrin pathways: Mechanisms and advances in therapy. Signal Transduct. Target. Ther. 2023, 8, 1. [Google Scholar] [CrossRef]
- Järveläinen, H.; Sainio, A.; Koulu, M.; Wight, T.N.; Penttinen, R. Extracellular matrix molecules: Potential targets in pharmacotherapy. Pharmacol. Rev. 2009, 61, 198–223. [Google Scholar] [CrossRef]
- Nicolas, J.; Magli, S.; Rabbachin, L.; Sampaolesi, S.; Nicotra, F.; Russo, L. 3D Extracellular Matrix Mimics: Fundamental Concepts and Role of Materials Chemistry to Influence Stem Cell Fate. Biomacromolecules 2020, 21, 1968–1994. [Google Scholar] [CrossRef]
- Tallawi, M.; Rosellini, E.; Barbani, N.; Cascone, M.G.; Rai, R.; Saint-Pierre, G.; Boccaccini, A.R. Strategies for the chemical and biological functionalization of scaffolds for cardiac tissue engineering: A review. J. R. Soc. Interface 2015, 12, 20150254. [Google Scholar] [CrossRef]
- Parisi, L.; Toffoli, A.; Ghezzi, B.; Mozzoni, B.; Lumetti, S.; Macaluso, G.M. A glance on the role of fibronectin in controlling cell response at biomaterial interface. Jpn. Dent. Sci. Rev. 2020, 56, 50–55. [Google Scholar] [CrossRef]
- Xing, H.; Lee, H.; Luo, L.; Kyriakides, T.R. Extracellular matrix-derived biomaterials in engineering cell function. Biotechnol. Adv. 2020, 42, 107421. [Google Scholar] [CrossRef]
- Hassan, M.E.; Yang, Q.; Xiao, Z.; Liu, L.; Wang, N.; Cui, X.; Yang, L. Impact of immobilization technology in industrial and pharmaceutical applications. 3 Biotech 2019, 9, 440. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, Z.; Lu, W.W.; Zhen, W.; Yang, D.; Peng, S. Novel biomaterial strategies for controlled growth factor delivery for biomedical applications. NPG Asia Mater. 2017, 9, e435. [Google Scholar] [CrossRef]
- Kasravi, M.; Ahmadi, A.; Babajani, A.; Mazloomnejad, R.; Hatamnejad, M.R.; Shariatzadeh, S.; Niknejad, H. Immunogenicity of decellularized extracellular matrix scaffolds: A bottleneck in tissue engineering and regenerative medicine. Biomater. Res. 2023, 27, 10. [Google Scholar] [CrossRef]
- Yamada, Y.; Onda, T.; Wada, Y.; Hamada, K.; Kikkawa, Y.; Nomizu, M. Structure–Activity Relationships of RGD-Containing Peptides in Integrin αvβ5-Mediated Cell Adhesion. ACS Omega 2023, 8, 4687–4693. [Google Scholar] [CrossRef] [PubMed]
- Haggag, Y.A. Peptides as Drug Candidates: Limitations and Recent Development Perspectives. Biomed. J. Sci. Tech. Res. 2018, 8, 6659–6662. [Google Scholar] [CrossRef]
- Klimek, K.; Ginalska, G.G. Proteins and Peptides as Important Modifiers of the Polymer Scaffolds for Tissue Engineering Applications—A Review. Polymers 2020, 12, 844. [Google Scholar] [CrossRef] [PubMed]
- Ren, X.; Zhao, M.; Lash, B.; Martino, M.M.; Julier, Z. Growth Factor Engineering Strategies for Regenerative Medicine Applications. Front. Bioeng. Biotechnol. 2020, 7, 469. [Google Scholar] [CrossRef]
- Wang, H.-J.; Di, L.; Ren, Q.-S.; Wang, J.-Y. Applications and Degradation of Proteins Used as Tissue Engineering Materials. Materials 2009, 2, 613–635. [Google Scholar] [CrossRef]
- Wang, L.; Wang, N.; Zhang, W.; Cheng, X.; Yan, Z.; Shao, G.; Fu, C. Therapeutic peptides: Current applications and future directions. Signal Transduct. Target. Ther. 2022, 7, 48. [Google Scholar] [CrossRef]
- Barker, T.H. The role of ECM proteins and protein fragments in guiding cell behavior in regenerative medicine. Biomaterials 2011, 32, 4211–4214. [Google Scholar] [CrossRef]
- Carson, A.E.; Barker, T.H. Emerging concepts in engineering extracellular matrix variants for directing cell phenotype. Regen. Med. 2009, 4, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Zhou, H.; Gerhard, E.M.; Zhang, S.; Rodríguez, F.I.P.; Pan, T. Smart bioadhesives for wound healing and closure. Bioact. Mater. 2023, 19, 360–375. [Google Scholar] [CrossRef] [PubMed]
- Tarafder, S.; Park, G.Y.; Felix, J.; Lee, C.H. Bioadhesives for musculoskeletal tissue regeneration. Acta Biomater. 2020, 117, 77–92. [Google Scholar] [CrossRef]
- Tzagiollari, A.; McCarthy, H.O.; Levingstone, T.J.; Dunne, N.J. Biodegradable and Biocompatible Adhesives for the Effective Stabilisation, Repair and Regeneration of Bone. Bioengineering 2022, 9, 250. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.; Lo, K.W.H. Small molecule-mediated regenerative engineering for craniofacial and dentoalveolar bone. Front. Bioeng. Biotechnol. 2022, 10, 1003936. [Google Scholar] [CrossRef] [PubMed]
- Lo, K.W.-H.; Ashe, K.M.; Kan, H.M.; Laurencin, C.T. The role of small molecules in musculoskeletal regeneration. Regen. Med. 2012, 7, 535–549. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Tang, X.; Gohil, S.V.; Laurencin, C.T. Biomaterials for Bone Regenerative Engineering. Adv. Healthc. Mater. 2015, 4, 1268–1285. [Google Scholar] [CrossRef]
- Allsopp, T.E.; Bunnage, M.E.; Fish, P.V. Small molecule modulation of stem cells in regenerative medicine: Recent applications and future direction. MedChemComm 2010, 1, 16. [Google Scholar] [CrossRef]
- Lu, B.; Atala, A. Small molecules and small molecule drugs in regenerative medicine. Drug Discov. Today 2014, 19, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Segar, C.E.; Ogle, M.E.; Botchwey, E.A. Regulation of Angiogenesis and Bone Regeneration with Natural and Synthetic Small Molecules. Curr. Pharm. Des. 2013, 19, 3403–3419. [Google Scholar] [CrossRef]
- Laurencin, C.T.; Ashe, K.M.; Henry, N.; Kan, H.M.; Lo, K.W.-H. Delivery of small molecules for bone regenerative engineering: Preclinical studies and potential clinical applications. Drug Discov. Today 2014, 19, 794–800. [Google Scholar] [CrossRef] [PubMed]
- Tat, S.K.; Pelletier, J.-P.; Mineau, F.; Caron, J.; Martel-Pelletier, J. Strontium ranelate inhibits key factors affecting bone remodeling in human osteoarthritic subchondral bone osteoblasts. Bone 2011, 49, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; Jiang, S.; Qi, X.; Bai, R.; Ye, X.; Xie, T. Races of small molecule clinical trials for the treatment of COVID-19: An up-to-date comprehensive review. Drug Dev. Res. 2022, 83, 16–54. [Google Scholar] [CrossRef] [PubMed]
- Awale, G.M.; Barajaa, M.A.; Kan, H.-M.; Seyedsalehi, A.; Nam, G.H.; Hosseini, F.S.; Laurencin, C.T. Regenerative engineering of long bones using the small molecule forskolin. Proc. Nat. Acad. Sci. USA 2023, 120, e2219756120. [Google Scholar] [CrossRef]
- Jiang, T.; Carbone, E.J.; Lo, K.W.-H.; Laurencin, C.T. Electrospinning of polymer nanofibers for tissue regeneration. Prog. Polym. Sci. 2015, 46, 1–24. [Google Scholar] [CrossRef]
- Goonoo, N.; Bhaw-Luximon, A. Mimicking growth factors: Role of small molecule scaffold additives in promoting tissue regeneration and repair. RSC Adv. 2019, 9, 18124–18146. [Google Scholar] [CrossRef]
- Moore, A.N.; Hartgerink, J.D. Self-Assembling Multidomain Peptide Nanofibers for Delivery of Bioactive Molecules and Tissue Regeneration. Accounts Chem. Res. 2017, 50, 714–722. [Google Scholar] [CrossRef]
- Liu, C.; Yu, Q.; Yuan, Z.; Guo, Q.; Liao, X.; Han, F.; Feng, T.; Liu, G.; Zhao, R.; Zhu, Z.; et al. Engineering the viscoelasticity of gelatin methacryloyl (GelMA) hydrogels via small “dynamic bridges” to regulate BMSC behaviors for osteochondral regeneration. Bioact. Mater. 2022, 25, 445–459. [Google Scholar] [CrossRef]
- Jeon, O.H.; Elisseeff, J. Orthopedic tissue regeneration: Cells, scaffolds, and small molecules. Drug Deliv. Transl. Res. 2016, 6, 105–120. [Google Scholar] [CrossRef]
- Carbone, E.J.; Jiang, T.; Nelson, C.; Henry, N.; Lo, K.W.-H. Small molecule delivery through nanofibrous scaffolds for musculoskeletal regenerative engineering. Nanomed. Nanotechnol. Biol. Med. 2014, 10, 1691–1699. [Google Scholar] [CrossRef]
- Hoshino, M.; Tsujimoto, T.; Yamazoe, S.; Uesugi, M.; Terada, S. Adhesamine, a new synthetic molecule, accelerates differentiation and prolongs survival of primary cultured mouse hippocampal neurons. Biochem. J. 2010, 427, 297–304. [Google Scholar] [CrossRef]
- Yamazoe, S.; Shimogawa, H.; Sato, S.-I.; Esko, J.D.; Uesugi, M. A Dumbbell-Shaped Small Molecule that Promotes Cell Adhesion and Growth. Chem. Biol. 2009, 16, 773–782. [Google Scholar] [CrossRef] [PubMed]
- Braicu, C.; Buse, M.; Busuioc, C.; Drula, R.; Gulei, D.; Raduly, L.; Berindan-Neagoe, I. A Comprehensive Review on MAPK: A Promising Therapeutic Target in Cancer. Cancers 2019, 11, 1618. [Google Scholar] [CrossRef]
- Cau, F.; Fanni, D.; Manchia, M.; Gerosa, C.; Piras, M.; Murru, R.; Faa, G. Expression of L1 Cell Adhesion Molecule (L1CAM) in extracellular vesicles in the human spinal cord during development. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 6273–6282. [Google Scholar] [CrossRef] [PubMed]
- Giger, R.J.; Hollis, E.R., 2nd; Tuszynski, M.H. Guidance Molecules in Axon Regeneration. Cold Spring Harb. Perspect. Biol. 2010, 2, a001867. [Google Scholar] [CrossRef]
- Kataria, H.; Lutz, D.; Chaudhary, H.; Schachner, M.; Loers, G. Small Molecule Agonists of Cell Adhesion Molecule L1 Mimic L1 Functions In Vivo. Mol. Neurobiol. 2016, 53, 4461–4483. [Google Scholar] [CrossRef]
- Nagaraj, V.; Kim, R.; Martianou, T.; Kurian, S.; Nayak, A.; Patel, M.; Schachner, M.; Theis, T. Effects of L1 adhesion molecule agonistic mimetics on signal transduction in neuronal functions. Biochem. Biophys. Res. Commun. 2023, 642, 27–34. [Google Scholar] [CrossRef]
- Xu, J.; Hu, C.; Jiang, Q.; Pan, H.; Shen, H.; Schachner, M. Trimebutine, a small molecule mimetic agonist of adhesion molecule L1, contributes to functional recovery after spinal cord injury in mice. Dis. Models Mech. 2017, 10, 1117–1128. [Google Scholar] [CrossRef]
- Li, R.; Sahu, S.; Schachner, M. Phenelzine, a cell adhesion molecule L1 mimetic small organic compound, promotes functional recovery and axonal regrowth in spinal cord-injured zebrafish. Pharmacol. Biochem. Behav. 2018, 171, 30–38. [Google Scholar] [CrossRef]
- Joseph, T.P.; Jagadeesan, N.; Sai, L.Y.; Lin, S.L.; Sahu, S.; Schachner, M. Adhesion Molecule L1 Agonist Mimetics Protect Against the Pesticide Paraquat-Induced Locomotor Deficits and Biochemical Alterations in Zebrafish. Front. Neurosci. 2020, 14, 458. [Google Scholar] [CrossRef]
- Li, R.; Sahu, S.; Schachner, M. Phenelzine, a small organic compound mimicking the functions of cell adhesion molecule L1, promotes functional recovery after mouse spinal cord injury. Restor. Neurol. Neurosci. 2018, 36, 469–483. [Google Scholar] [CrossRef] [PubMed]
- Berdeaux, R.; Stewart, R. cAMP signaling in skeletal muscle adaptation: Hypertrophy, metabolism, and regeneration. Am. J. Physiol.-Endocrinol. Metab. 2012, 303, E1–E17. [Google Scholar] [CrossRef] [PubMed]
- Lo, K.W.-H.; Ashe, K.M.; Kan, H.M.; Lee, D.A.; Laurencin, C.T. Activation of cyclic amp/protein kinase: A signaling pathway enhances osteoblast cell adhesion on biomaterials for regenerative engineering. J. Orthop. Res. 2011, 29, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Lo, K.W.-H.; Kan, H.M.; Gagnon, K.A.; Laurencin, C.T. One-day treatment of small molecule 8-bromo-cyclic AMP analogue induces cell-based VEGF production forin vitroangiogenesis and osteoblastic differentiation: CAMP analogue promotes cell-based VEGF production forin vitroangiogenesis and osteogenic differentiation. J. Tissue Eng. Regen. Med. 2016, 10, 867–875. [Google Scholar] [CrossRef]
- Ifegwu, O.C.; Awale, G.; Kan, H.M.; Rajpura, K.; O’neill, E.; Kuo, C.-L.; Lo, K.W.-H. Bone Regenerative Engineering Using a Protein Kinase A-Specific Cyclic AMP Analogue Administered for Short Term. Regen. Eng. Transl. Med. 2018, 4, 206–215. [Google Scholar] [CrossRef]
- Lo, K.W.-H.; Kan, H.M.; Ashe, K.M.; Laurencin, C.T. The small molecule PKA-specific cyclic AMP analogue as an inducer of osteoblast-like cells differentiation and mineralization. J. Tissue Eng. Regen. Med. 2011, 6, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.O.; Ryu, J.M.; Na Suh, H.; Park, S.H.; Oh, Y.-M.; Lee, S.H.; Han, H.J. CAMP Promotes Cell Migration Through Cell Junctional Complex Dynamics and Actin Cytoskeleton Remodeling: Implications in Skin Wound Healing. Stem Cells Dev. 2015, 24, 2513–2524. [Google Scholar] [CrossRef]
- Costa, M.H.G.; Serra, J.; McDevitt, T.C.; Cabral, J.M.S.; da Silva, C.L.; Ferreira, F.C. Dimethyloxalylglycine, a small molecule, synergistically increases the homing and angiogenic properties of human mesenchymal stromal cells when cultured as 3D spheroids. Biotechnol. J. 2021, 16, 2000389. [Google Scholar] [CrossRef]
- Yuan, J.; Hou, Q.; Zhong, L.; Dai, X.; Lu, Q.; Li, M.; Fu, X. Sustained release of inhibitor from bionic scaffolds for wound healing and functional regeneration. Biomater. Sci. 2020, 8, 5647–5655. [Google Scholar] [CrossRef]
- Quiros, M.; Feier, D.; Birkl, D.; Agarwal, R.; Zhou, D.W.; García, A.J.; Parkos, C.A.; Nusrat, A. Resolvin E1 is a pro-repair molecule that promotes intestinal epithelial wound healing. Proc. Natl. Acad. Sci. USA 2020, 117, 9477–9482. [Google Scholar] [CrossRef]
- Spakova, T.; Plsikova, J.; Harvanova, D.; Lacko, M.; Stolfa, S.; Rosocha, J. Influence of Kartogenin on Chondrogenic Differentiation of Human Bone Marrow-Derived MSCs in 2D Culture and in Co-Cultivation with OA Osteochondral Explant. Molecules 2018, 23, 181. [Google Scholar] [CrossRef] [PubMed]
- Yi, B.; Ding, T.; Jiang, S.; Gong, T.; Chopra, H.; Sha, O.; Dissanayaka, W.L.; Ge, S.; Zhang, C. Conversion of stem cells from apical papilla into endothelial cells by small molecules and growth factors. Stem Cell Res. Ther. 2021, 12, 266. [Google Scholar] [CrossRef]
- Burden-Gulley, S.M.; Gates, T.J.; Craig, S.E.; Gupta, M.; Brady-Kalnay, S.M. Stimulation of N-cadherin-dependent neurite outgrowth by small molecule peptide mimetic agonists of the N-cadherin HAV motif. Peptides 2010, 31, 842–849. [Google Scholar] [CrossRef]
- Lo, K.W.-H.; Ulery, B.D.; Kan, H.M.; Ashe, K.M.; Laurencin, C.T. Evaluating the feasibility of utilizing the small molecule phenamil as a novel biofactor for bone regenerative engineering: Small molecule phenamil for bone regenerative engineering. J. Tissue Eng. Regen. Med. 2012, 8, 728–736. [Google Scholar] [CrossRef] [PubMed]
- Lo, K.W.-H.; Kan, H.M.; Laurencin, C.T. Short-term administration of small molecule phenamil induced a protracted osteogenic effect on osteoblast-like MC3T3-E1 cells. J. Tissue Eng. Regen. Med. 2013, 10, 518–526. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhao, X.; Zhang, R.; Huang, Y.; Li, Y.; Shan, M.; Zhong, X.; Xing, Y.; Wang, M.; Zhang, Y.; et al. Cartilage Extracellular Matrix Scaffold With Kartogenin-Encapsulated PLGA Microspheres for Cartilage Regeneration. Front. Bioeng. Biotechnol. 2020, 8, 600103. [Google Scholar] [CrossRef] [PubMed]
- Lo, K.W.-H. Effects on bone regeneration of single-dose treatment with osteogenic small molecules. Drug Discov. Today 2022, 27, 1538–1544. [Google Scholar] [CrossRef]
- Jurgens, W.J.; Kroeze, R.J.; Bank, R.A.; Ritt, M.J.P.F.; Helder, M.N. Rapid attachment of adipose stromal cells on resorbable polymeric scaffolds facilitates the one-step surgical procedure for cartilage and bone tissue engineering purposes: Adipose stromal cells allow one-step procedure. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2011, 29, 853–860. [Google Scholar] [CrossRef]


| Molecule Type | Advantages | Disadvantages | References |
|---|---|---|---|
| Proteins | Tissue specificity | Large size; easily cleared from the body; immunogenic; unstable; difficult to fabricate; expensive; can have off- target effects | [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34] |
| Short Peptides | Small size; stable; easy to manufacture; chain length can be altered for different applications | Tendency to aggregate; unstable; relatively low affinity to target tissue | [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34] |
| Small molecules (<1000 Da) | Inexpensive; non-immunogenic; stable; ability to conjugate easily at high densities; high oral bioavailability; many are FDA-approved for other therapies | No distinguishable deficits detetermined thus far | [35,36,37,38,39,40,41,42,43] |
| Molecule | Classification | Molecular Weight | Working Concentrations | Cell Lineage/Surgical Model | Delivery Methods | Adhesive Properties | References |
|---|---|---|---|---|---|---|---|
| Adhesamine | Diaryldispirotripiperazine derivatives | 670.5 g/mol | 0.6–60 µM | HepG2 cells; Jurkat cells | Inoculation in culture plates treated with adhesamine | Enhanced adhesion of HepG2 and Jurkat cells to culture plate by up to 2 fold; adhesive effect is dose dependent | [52] |
| Phenelzine sulfate | Monoamine oxidase inhibitors (MAOIs) | 234.3 g/mol | 0.1–100 µM | Cerebellar neurons and Schwann cells isolated from mice | Incubated in well plates treated with phenelzine sulfate | Increased surface and nuclear expression of L1 in cerebellar neurons; enhanced cerebellar neuron and Schwan cell migration | [56] |
| Forskolin | Labdane diterpenoids | 410.5 g/mol | 0.1 mM | Osteoblast-like MC3T3-E1 cells | Inoculation in culture plates treated with growth media containing Forskolin | Induced cAMP-mediated cell adhesion of MC3T3-E1 cells to PLAGA thin films | [63] |
| 8-Br-cAMP | cAMP analogues | 408.1 g/mol | 100 µM | Osteoblast-like MC3T3-E1 cells | Inoculation in culture plates treated with 8-Br-cAMP | Promoted integrin-dependent cell adhesion of MC3T3-E1 cells | [64,71] |
| 0.02 mM, 0.1 mM, and 0.5 mM | Osteoblast-like MC3T3-E1 cells | Increasing dosages of 8-Br-cAMP introduced to trypsinized MC3T3-E1 cells suspensed in basal medium | Promoted integrin-dependent cell adhesion of MC3T3-E1 cells to PLAGA thin films | [63] | |||
| 10 µM | mESCs | Incubated in laminin-coated well plates treated with 8-Br-cAMP | Evoked substantial migration of cells into the denuded areas; induced the translocation of junctional proteins from the plasma membrane to the cytosol; | [67] | |||
| 6-Bnz-cAMP | cAMP analogues | 455.3 g/mol | 100 µM | Osteoblast-like MC3T3-E1 cells | Inoculation in culture plates treated with growth media containing 6-Bnz-cAMP | Promoted integrin-dependent cell adhesion of MC3T3-E1 cells | [64,65,66] |
| 0.1 mM | Osteoblast-like MC3T3-E1 cells | Introduced to trypsinized MC3T3-E1 cells suspensed in basal medium | Promoted integrin-dependent cell adhesion of MC3T3-E1 cells to PLAGA thin films | [63] | |||
| Dimethyloxalylglycine | Glycine derivatives | 175.1 g/mol | 500 µM | MSC spheroids | Incubated in fibronectin-coated well plates with DMOG medium | 69 ± 7% MSC spheroids pre-exposed to DMOG adhered to fibronectin in the well plates, an increase from the 49 ± 6% MSC spheroids pre-exposed to hypoxic or normal atmospheric conditions | [68] |
| Duloxetine | Naphthalenes | 297.4 g/mol | 0.1–100 µM | Cerebellar neurons and Schwann cells isolated from mice | Incubated in well plates treated with duloxetine | Increased surface and nuclear expression of L1 in cerebellar neurons; enhanced cerebellar neuron and Schwan cell migration | [56,57] |
| Tacrine | Benzoquinolines | 198.3 g/mol | 0.1–100 µM | Cerebellar neurons and Schwann cells isolated from mice | Incubated in well plates treated with tacrine | Increased surface and nuclear expression of L1 in cerebellar neurons; enhanced cerebellar neuron migration | [56,57] |
| Ethinyl estradiol | Estrane steroids | 296.4 g/mol | 0.1–100 µM | Cerebellar neurons and Schwann cells isolated from mice | Incubated in well plates treated with ethinyl estradiol | Increased surface and nuclear expression of L1 in cerebellar neurons; enhanced cerebellar neuron and Schwan cell migration | [56,57] |
| Crotamiton | Anilides | 203.3 g/mol | 0.1–100 µM | Cerebellar neurons and Schwann cells isolated from mice | Incubated in well plates treated with crotamiton | Increased surface and nuclear expression of L1 in cerebellar neurons; enhanced cerebellar neuron migration | [56,57] |
| Honokiol | Phenols | 266.3 g/mol | 0.1–100 µM | Cerebellar neurons and Schwann cells isolated from mice | Incubated in well plates treated with honokiol | Increased surface and nuclear expression of L1 in cerebellar neurons; enhanced cerebellar neuron and Schwan cell migration | [56] |
| 50 nM, 100 nM, 200 nM | Cerebellar granule cells isolated from mice at postnatal day 7 | Inoculation in culture plates treated with honokiol | Induced L1-mediated intracellular pathway at 50 or 100 nM | [57,58] | |||
| Trimebutine | Hydroxybenzoates | 387.5 g/mol | 5 nM, 10 nM, 20 nM | Cerebellar granule cells isolated from mice at postnatal day 7 | Inoculation in culture plates treated with trimebutine | Induced L1-mediated intracellular pathway at 5 nM | [57,58] |
| Trimebutine maleate | Hydroxybenzoates | 503.5 g/mol | 0.1–100 µM | Cerebellar neurons and Schwann cells isolated from mice | Incubated in well plates treated with trimebutine maleate | Increased surface and nuclear expression of L1 in cerebellar neurons; enhanced cerebellar neuron and Schwan cell migration | [56,57] |
| Piceid | Stilbenoid glucosides | 390.4 g/mol | 0.1–100 µM | Cerebellar neurons and Schwann cells isolated from mice | Incubated in well plates treated with piceid | Increased surface and nuclear expression of L1 in cerebellar neurons; enhanced cerebellar neuron and Schwan cell migration | [56] |
| 0.01–1000 nM | Cerebellar granule neurons | - | Promoted neurite outgrowth; enhanced cerebellar neuron migration | [57] | |||
| Phenamil | Pyrazines | 305.7 g/mol | 10 µM | Osteoblast-like MC3T3-E1 cells | Solubilized and loaded into PLAGA scaffolds and introduced to well plates with MC3T3-E1 cells | Promoted a greater than two-fold increase in initial cell adhesion | [74] |
| 10 µM | Osteoblast-like MC3T3-E1 cells | Solubilized and loaded into PLAGA scaffolds and introduced to well plates with MC3T3-E1 cells | Upregulated phosphorylated (pCREB) and p125FAK proteins; promoted integrin-dependent cell adhesion of MC3T3-E1 cells to PLAGA thin films | [75] | |||
| SB216763 | Maleimides | 371.2 g/mol | 1–50 ppm | HDF cells | Solubilized and loaded into CSNF-SB bionic composite scaffolds and introduced to well plates with HDF cells | Stimulated HDF adhesion to well plates | [69] |
| Chemical cocktail * | Assortment (see footnote) | Assortment (see footnote) | Assortment (see footnote) | SCAP-ECs | Incubated on well plates containing culture medium treated chemical cocktail | Stimulated differentiation of SCAPs to SCAP-ECs and helped facilitate migration; upregulated expression of VE-Cadherin | [72] |
| ADH-400 series † ADH-700 series † | Peptidomimetics of the N-cadherin HAVD motif | 400 series parent: 233.3 g/mol 700 series parent: 275.16 g/mol | 50 µM, 100 µM, 200 µM | RGCs | Retinal explants cultured with peptidomimetics of both ADH parent compounds suspended in DMSO | All peptidomimetics enhanced RGC neurite outgrowth (129–161% control); five peptidomimetics prompted RGC migration on a N-cadherin substrate (ADH-200408, ADH200433, ADH-200439, ADH-200786, ADH-201707) | [73] |
| Resolvin E1 | Hydroxyeicosapentaenoic acids | 350.4 g/mol | 10–500 nM | hIECs (line SKOC15) | Incubated on fibronectin-coated well glass coverslips treated with RvE1 | Significantly increased cell adhesion strength to ECM when compared to untreated control (111.1 ± 1.83 control vs. 126.9 ± 4.70 RvE1) | [70] |
| Kartogenin | Anilides | 317.3 g/mol | 10 µM | hBMSCs | Co-cultured on osteochondral explants treated with kartogenin | Higher density of adhered hBMSCs on cartilage surface of osteochondral explants when compared to control; enhanced staining of hBMSCs on cartilaginous edge in kartogenin treatment group | [71] |
| Not reported | BMSCs | Kartogenin-encapsulated PLAGA microspheres on CECM scaffold | Amplified adhesion of BMSCs to composite scaffold surface | [76] |
| Molecule | Classification | Molecular Weight | Working Concentrations | Cell Lineage/Surgical Model | Delivery Methods | Adhesive Properties | References |
|---|---|---|---|---|---|---|---|
| Honokiol | Phenols | 266.3 g/mol | 1 mg/kg | 3 month old female mice with SCI | Injection through the tail vein of anesthetized mice | Elevated neuronal levels of L1, pCK2α and mTOR expression and phosphorylation | [58] |
| Trimebutine | Hydroxybenzoates | 387.5 g/mol | 1 mg/kg | 3 month old female mice with SCI | Injection through the tail vein of anesthetized mice | No substantial change in neuronal L1 expression | [58] |
| Phenelzine | Monoamine oxidase inhibitors (MAOIs) | 136.2 g/mol | 500 nM | Zebrafish larvae with SCI | Inoculated in well plates with E3 medium conatining phenelzine | Stimulated L1.1 protein levels for axonal regrowth in zebrafish larvae | [59] |
| 6 and 12 mg/kg | 4–5 month old female mice with SCI | Intraperitoneal injection once daily starting immediately following trauma until 6 weeks after SCI | Stimulated L1.1 protein levels for axonal regrowth in young mice | [61] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitchell, J.; Lo, K.W.-H. The Use of Small-Molecule Compounds for Cell Adhesion and Migration in Regenerative Medicine. Biomedicines 2023, 11, 2507. https://doi.org/10.3390/biomedicines11092507
Mitchell J, Lo KW-H. The Use of Small-Molecule Compounds for Cell Adhesion and Migration in Regenerative Medicine. Biomedicines. 2023; 11(9):2507. https://doi.org/10.3390/biomedicines11092507
Chicago/Turabian StyleMitchell, Juan, and Kevin W.-H. Lo. 2023. "The Use of Small-Molecule Compounds for Cell Adhesion and Migration in Regenerative Medicine" Biomedicines 11, no. 9: 2507. https://doi.org/10.3390/biomedicines11092507
APA StyleMitchell, J., & Lo, K. W.-H. (2023). The Use of Small-Molecule Compounds for Cell Adhesion and Migration in Regenerative Medicine. Biomedicines, 11(9), 2507. https://doi.org/10.3390/biomedicines11092507





