Safety and Effectiveness of Meatal Mobilization (MEMO) Technique for Glandular, Coronal, and Subcoronal Hypospadias Repair in Children: A 5-Year Single-Center Study with 105 Hypospadias
Abstract
1. Introduction
2. Methodology
2.1. Patients
2.2. Ethical Aspects
2.3. Outcomes of the Study
2.4. Data Collection and Study Design
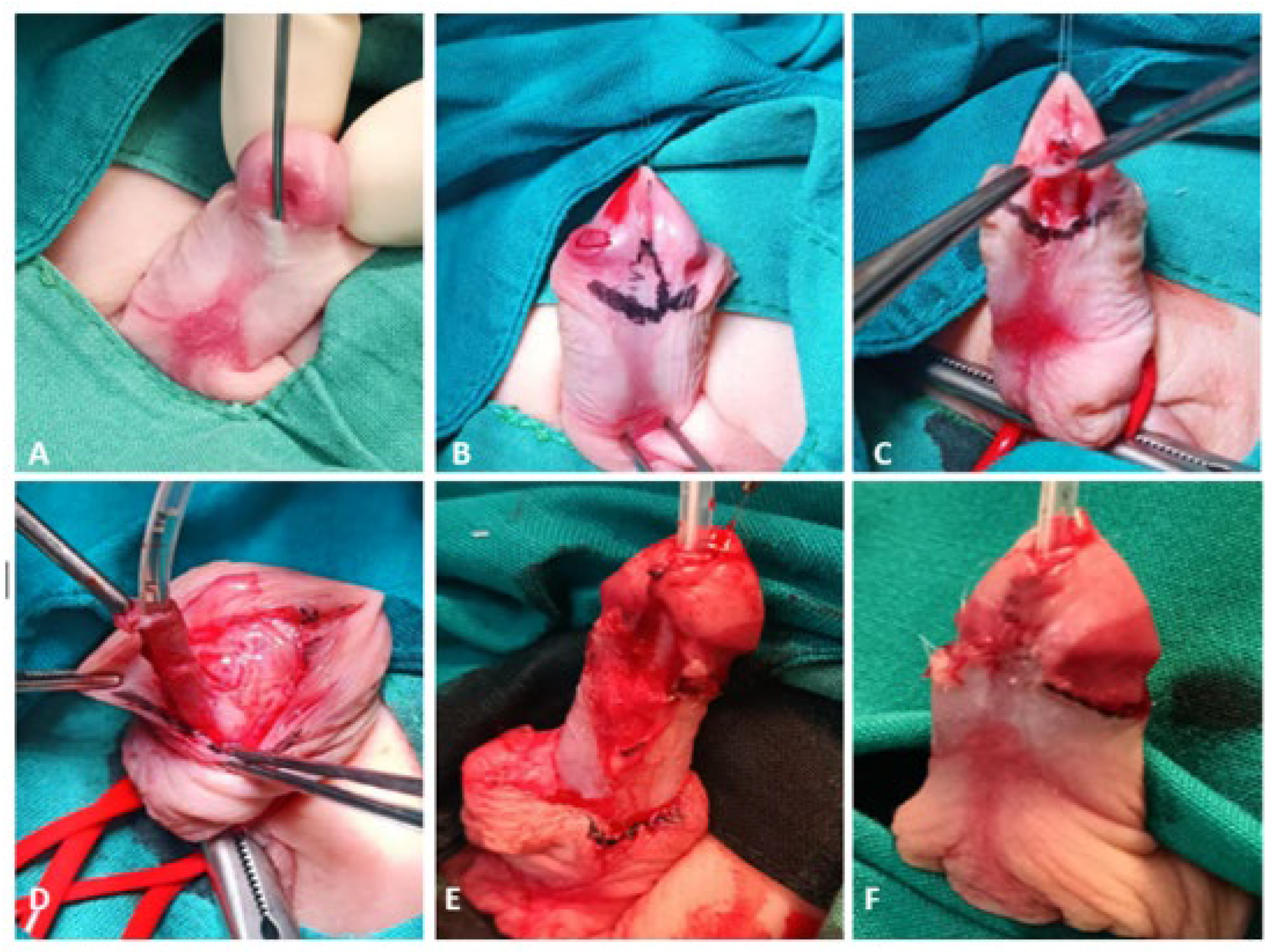
2.5. Suturgical Techniques
2.5.1. MEMO Technique
2.5.2. Snodgrass Technique
2.6. Postoperative Protocol and Follow-Up
2.7. Statistical Analysis
3. Results
3.1. Demographic and Clinical Data of the Patients
3.2. Comparison of Surgical Techniques in Relation to Study Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Van der Horst, H.J.; de Wall, L.L. Hypospadias, all there is to know. Eur. J. Pediatr. 2017, 176, 435–441. [Google Scholar] [CrossRef]
- Kaefer, M. Hypospadias. Semin. Pediatr. Surg. 2021, 30, 151080. [Google Scholar] [CrossRef]
- Pogorelić, Z. Surgical approach to the treatment of urinary tract anomalies. Liječ Vjesn. 2022, 144 (Suppl. 1), 185–190. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, Q.; Liu, Z.; Wang, C.; Chen, H.; Luo, X.; Shen, L.; Long, C.; Wei, G.; Liu, X. Rab25 is involved in hypospadias via the β1 integrin/EGFR pathway. Exp. Cell Res. 2024, 436, 113980. [Google Scholar] [CrossRef]
- Arboleda, V.A.; Sandberg, D.E.; Vilain, E. DSDs: Genetics, underlying pathologies and psychosexual differentiation. Nat. Rev. Endocrinol. 2014, 10, 603–615. [Google Scholar] [CrossRef]
- Catti, M.; Demède, D.; Valmalle, A.F.; Mure, P.Y.; Hameury, F.; Mouriquand, P. Management of severe hypospadias. Indian. J. Urol. 2008, 24, 233–240. [Google Scholar] [CrossRef]
- Society for Maternal-Fetal Medicine (SMFM); Sparks, T.N. Hypospadias. Am. J. Obstet. Gynecol. 2021, 225, B18–B20. [Google Scholar] [CrossRef]
- Nordenskjöld, A.; Lagerstedt-Robinson, K.; Anderlid, B.M.; Lundin, J. Tissue specific trisomy 15 mosaicism associated with urogenital malformations. Eur. J. Med. Genet. 2023, 66, 104824. [Google Scholar] [CrossRef]
- Joodi, M.; Amerizadeh, F.; Hassanian, S.M.; Erfani, M.; Ghayour-Mobarhan, M.; Ferns, G.A.; Khazaei, M.; Avan, A. The genetic factors contributing to hypospadias and their clinical utility in its diagnosis. J. Cell Physiol. 2019, 234, 5519–5523. [Google Scholar] [CrossRef]
- Subramaniam, R.; Spinoit, A.F.; Hoebeke, P. Hypospadias repair: An overview of the actual techniques. Semin. Plast. Surg. 2011, 25, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Askarpour, S.; Peyvasteh, M.; Mohamadi, A.; Khoshkhabar, M. Comparative study of modifying meatal advancement glandular with release chordi versus Snodgrass surgical methods regarding the repair of distal hypospadias. World J. Plast. Surg. 2021, 10, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Asad, S.; Khan, F.A.; Ali, S.; Khan, H.; Rafaqat, H.; Din Khattak, I.U. Snodgrass hypospadias repair at Ayub teaching hospital: An audit of complications and outcomes. J. Ayub Med. Coll. Abbottabad. 2023, 35, 259–264. [Google Scholar] [CrossRef]
- Arshadi, H.; Sabetkish, S.; Kajbafzadeh, A.M. Modified tubularized incised plate urethroplasty reduces the risk of fistula and meatal stenosis for proximal hypospadias: A report of 63 cases. Int. Urol. Nephrol. 2017, 49, 2099–2104. [Google Scholar] [CrossRef] [PubMed]
- Moradi, M.; Kazemzadeh, B.; Hood, B.; Rezaee, H.; Kaseb, K. Meatal mobilization and glanuloplasty: A viable option for coronal and glanular hypospadias repair. Urology 2016, 94, 204–207. [Google Scholar] [CrossRef]
- Seibold, J.; Boehmer, A.; Verger, A.; Merseburger, A.S.; Stenzl, A.; Sievert, K.D. The meatal mobilization technique for coronal/subcoronal hypospadias repair. BJU Int. 2007, 100, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Seibold, J.; Werther, M.; Alloussi, S.; Gakis, G.; Schilling, D.; Colleselli, D.; Stenzl, A.; Schwentner, C. Objective long-term evaluation after distal hypospadias repair using the meatal mobilization technique. Scand. J. Urol. Nephrol. 2010, 44, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Jukić, M.; Antišić, J.; Pogorelić, Z. Incidence and causes of 30-day readmission rate from discharge as an indicator of quality care in pediatric surgery. Acta Chir. Belg. 2023, 123, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Jukić, M.; Biuk, I.; Pogorelić, Z. The incidence and causes of unplanned reoperations as a quality indicator in pediatric surgery. Children 2022, 9, 106. [Google Scholar] [CrossRef]
- Snodgrass, W.T. Snodgrass technique for hypospadias repair. BJU Int. 2005, 95, 683–693. [Google Scholar] [CrossRef]
- Gozar, H.; Bara, Z.; Dicu, E.; Derzsi, Z. Current perspectives in hypospadias research: A scoping review of articles published in 2021 (Review). Exp. Ther. Med. 2023, 25, 211. [Google Scholar] [CrossRef]
- Zhang, Y.; Shen, Z.; Zhou, X.; Chi, Z.; Hong, X.; Huang, Y.; Huang, H.; Chen, S.; Lan, K.; Lin, J.; et al. Comparison of meatal-based flap (Mathieu) and tubularized incised-plate (TIP) urethroplasties for primary distal hypospadias: A systematic review and meta-analysis. J. Pediatr. Surg. 2020, 55, 2718–2727. [Google Scholar] [CrossRef]
- Winberg, H.; Arnbjörnsson, E.; Anderberg, M.; Stenström, P. Postoperative outcomes in distal hypospadias: A meta-analysis of the Mathieu and tubularized incised plate repair methods for development of urethrocutaneous fistula and urethral stricture. Pediatr. Surg. Int. 2019, 35, 1301–1308. [Google Scholar] [CrossRef] [PubMed]
- El-Helaly, H.A.; Youssof, H.A.; Ibrahim, H.M.; Aldaqadossi, H.A.; Abdalla, O.M.; Dogha, M.M. Distal hypospadias repair: Comparative study between Snodgrass and transverse preputial onlay flap. J. Pediatr. Urol. 2022, 18, 610.e1–610.e6. [Google Scholar] [CrossRef]
- Snodgrass, W.; Bush, N. Primary hypospadias repair techniques: A review of the evidence. Urol. Ann. 2016, 8, 403–408. [Google Scholar] [CrossRef]
- Soave, A.; Riechardt, S.; Engel, O.; Rink, M.; Fisch, M. Complications of hypospadias repairs. Urologe A 2014, 53, 1001–1005. [Google Scholar] [CrossRef] [PubMed]
- Buisson, P.; Ricard, J.; Hamzy, M.; Pouzac, M.; Canarelli, J.P. Evaluation of the results of the Snodgrass procedure in hypospadias surgery. Prog. Urol. 2004, 14, 385–389. [Google Scholar]
- Pfistermuller, K.L.; McArdle, A.J.; Cuckow, P.M. Meta-analysis of complication rates of the tubularized incised plate (TIP) repair. J. Pediatr. Urol. 2015, 11, 54–59. [Google Scholar] [CrossRef]
- Snodgrass, W.; Bush, N.C. Re-operative urethroplasty after failed hypospadias repair: How prior surgery impacts risk for additional complications. J. Pediatr. Urol. 2017, 13, 289.e1–289.e6. [Google Scholar] [CrossRef]
- Chukwubuike, K.E.; Obianyo, N.E.N.; Ekenze, S.O.; Ezomike, U.O. Assessment of the effect of urethral plate width on outcome of hypospadias repair. J. Pediatr. Urol. 2019, 15, 627.e1–627.e6. [Google Scholar] [CrossRef]
- Galal, M.; Taha, D.E.; Elabden, K.Z.; Nabeeh, H.; Abdelbaky, T. The effect of pre-incision urethral plate width and glanular width on the outcome of tubularized incised urethral plate repair surgery in distal penile hypospadias, a prospective study. Urol. J. 2021, 19, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Bush, N.C.; Snodgrass, W. Pre-incision urethral plate width does not impact short-term Tubularized Incised Plate urethroplasty outcomes. J. Pediatr. Urol. 2017, 13, 625.e1–625.e6. [Google Scholar] [CrossRef] [PubMed]
- Akova, F.; Aydın, E.; Salabas, E.; Bilgili, Z. Glans Diameter and Meatus localization are the sole predictors of primary distal hypospadias surgery complications: A multivariate analysis of single surgeon series. Cureus 2022, 14, e30306. [Google Scholar] [CrossRef] [PubMed]
- Bush, N.C.; Villanueva, C.; Snodgrass, W. Glans size is an independent risk factor for urethroplasty complications after hypospadias repair. J. Pediatr. Urol. 2015, 11, 355.e1–355.e3555. [Google Scholar] [CrossRef] [PubMed]
- Güler, Y. TIPU outcomes for hypospadias treatment and predictive factors causing urethrocutaneous fistula and external urethral meatus stenosis in TIPU: Clinical study. Andrologia 2020, 52, e13668. [Google Scholar] [CrossRef]
- Neheman, A.; Schwarztuch Gildor, O.; Shumaker, A.; Beberashvili, I.; Bar-Yosef, Y.; Arnon, S.; Zisman, A.; Stav, K. Use of validated questionnaires to predict cosmetic outcomes of hypospadias repair. Children 2024, 11, 189. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Ram Dhayal, I. A Comparative Study on the Outcomes of hypospadias surgery following early versus late bladder catheter removal. Cureus 2022, 14, e26104. [Google Scholar] [CrossRef] [PubMed]
- Xu, N.; Xue, X.Y.; Wei, Y.; Li, X.D.; Zheng, Q.S.; Jiang, T.; Huang, J.B. Outcome analysis of tubularized incised plate repair in hypospadias: Is a catheter necessary? Urol. Int. 2013, 90, 354–357. [Google Scholar] [CrossRef] [PubMed]
- Borkar, N.; Tiwari, C.; Mohanty, D.; Baruah, T.D.; Mohanty, M.; Sinha, C.K. Post-urethroplasty complications in hypospadias repair: A systematic review and meta-analysis comparing polydioxanone and polyglactin sutures. World J. Pediatr. Surg. 2024, 7, e000659. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Stričević, L.; Elezović Baloević, S.; Todorić, J.; Budimir, D. Safety and effectiveness of triclosan-coated polydioxanone (PDS Plus) versus uncoated polydioxanone (PDS II) sutures for prevention of surgical site infection after hypospadias repair in children: A 10-year single center experience with 550 hypospadias. Biomedicines 2024, 12, 583. [Google Scholar] [CrossRef]



| Variables | Group I (n = 49) | Group II (n = 56) | p |
|---|---|---|---|
| MEMO | SNODGRASS | ||
| Demographic characteristics of patients; median (IQR) or n (%) | |||
| Age (months) | 17 (12, 35.5) | 17 (13, 29) | 0.342 * |
| Height (cm) | 90 (82, 104) | 90 (84, 98) | 0.818 * |
| Weight (kg) | 13 (11, 15.2) | 12 (10, 14) | 0.173 * |
| BMI (kg/m2) | 16.2 (14.7, 17.5) | 15.6 (14.1, 17) | 0.190 * |
| Associated anomalies | 6 (12.2) | 7 (12.5) | 0.940 † |
| Type of hypospadias; n (%) | |||
| Glandular | 6 (12.2) | 8 (14.3) | 0.881 † |
| Subglandular | 8 (16.3) | 9 (16.1) | |
| Coronal | 21 (42.9) | 20 (35.7) | |
| Subcoronal | 14 (28.6) | 19 (33.9) | |
| Preoperative urinary difficulties; n (%) | |||
| Meatal stenosis | 1 (2) | 1 (1.8) | >0.999 ‡ |
| Dripping | 0 (0) | 1 (1.8) | >0.999 ‡ |
| Straining | 1 (2) | 0 (0) | >0.999 ‡ |
| Variables | Group I (n = 49) | Group II (n = 56) | p |
|---|---|---|---|
| MEMO | SNODGRASS | ||
| Complications; n (%) | |||
| Total number of complications | 4 (8.2) | 14 (25) | 0.037 * |
| Urethrocutaneous fistula | 1 (2) | 8 (14.3) | 0.034 * |
| Wound infection | 2 (4.1) | 3 (4.4) | >0.999 * |
| Meatal stenosis | 1 (2) | 3 (4.4) | 0.621 * |
| Intraoperative/postoperative outcomes; median (IQR) | |||
| Duration of surgery (min) | 41 (38, 47) | 51 (45.5, 61) | <0.001 † |
| Length of hospital stay (days) | 1 (1, 2) | 3 (2, 6) | <0.001 † |
| Catheter removal (days) | 3 (2.5, 5) | 6 (6, 8) | <0.001 † |
| ReAd/uROR/redo surgery; n (%) | |||
| ReAd | 0 (0) | 1 (1.8) | >0.999 * |
| uROR | 0 (0) | 0 (0) | - |
| Redo surgery | 3 (6.1) | 11 (19.6) | 0.048 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pogorelić, Z.; Milovac, B.; Čohadžić, T.; Todorić, J. Safety and Effectiveness of Meatal Mobilization (MEMO) Technique for Glandular, Coronal, and Subcoronal Hypospadias Repair in Children: A 5-Year Single-Center Study with 105 Hypospadias. Biomedicines 2024, 12, 831. https://doi.org/10.3390/biomedicines12040831
Pogorelić Z, Milovac B, Čohadžić T, Todorić J. Safety and Effectiveness of Meatal Mobilization (MEMO) Technique for Glandular, Coronal, and Subcoronal Hypospadias Repair in Children: A 5-Year Single-Center Study with 105 Hypospadias. Biomedicines. 2024; 12(4):831. https://doi.org/10.3390/biomedicines12040831
Chicago/Turabian StylePogorelić, Zenon, Boris Milovac, Tin Čohadžić, and Jakov Todorić. 2024. "Safety and Effectiveness of Meatal Mobilization (MEMO) Technique for Glandular, Coronal, and Subcoronal Hypospadias Repair in Children: A 5-Year Single-Center Study with 105 Hypospadias" Biomedicines 12, no. 4: 831. https://doi.org/10.3390/biomedicines12040831
APA StylePogorelić, Z., Milovac, B., Čohadžić, T., & Todorić, J. (2024). Safety and Effectiveness of Meatal Mobilization (MEMO) Technique for Glandular, Coronal, and Subcoronal Hypospadias Repair in Children: A 5-Year Single-Center Study with 105 Hypospadias. Biomedicines, 12(4), 831. https://doi.org/10.3390/biomedicines12040831







