Fibrinaloid Microclots and Atrial Fibrillation
Abstract
:1. Introduction
- Irregular R-R intervals (when atrioventricular conduction is not impaired),
- Absence of distinct repeating P waves, and
- Irregular atrial activations.” [11]
2. “Risk Factors”, Covariates, Confounders, Biases, and Coherence
3. What Are Fibrinaloid Microclots?
4. Risk Factors for AF That Are Not to Be Seen as Disease Comorbidities
5. Risk Factors for AF Based on Lifestyle Factors
6. Risk Factors That Are Recognised as Known Disease Comorbidities
7. Examples in Which We Know That Infection Can Lead to Atrial Fibrillation
8. Infection and Stroke
9. Some Biochemical Changes Accompanying AF
10. Virchow’s Triad: Coagulopathies and Thrombogenic Potential as Predictors of AF
11. Clinical Risk Scores, e.g., CHA2DS2-VASc
12. Machine Learning in AF
13. Final Discussion and Conclusions, and a Forward Look
Funding
Conflicts of Interest
References
- Chugh, S.S.; Havmoeller, R.; Narayanan, K.; Singh, D.; Rienstra, M.; Benjamin, E.J.; Gillum, R.F.; Kim, Y.H.; McAnulty, J.H., Jr.; Zheng, Z.J.; et al. Worldwide epidemiology of atrial fibrillation: A Global Burden of Disease 2010 Study. Circulation 2014, 129, 837–847. [Google Scholar] [CrossRef] [PubMed]
- Zulkifly, H.; Lip, G.Y.H.; Lane, D.A. Epidemiology of atrial fibrillation. Int. J. Clin. Pract. 2018, 72, e13070. [Google Scholar] [CrossRef] [PubMed]
- Corica, B.; Bonini, N.; Imberti, J.F.; Romiti, G.F.; Vitolo, M.; Attanasio, L.; Basili, S.; Freedman, B.; Potpara, T.S.; Boriani, G.; et al. Yield of diagnosis and risk of stroke with screening strategies for atrial fibrillation: A comprehensive review of current evidence. Eur. Heart J. Open 2023, 3, oead031. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Wolf, P.A.; D’Agostino, R.B.; Silbershatz, H.; Kannel, W.B.; Levy, D. Impact of atrial fibrillation on the risk of death: The Framingham Heart Study. Circulation 1998, 98, 946–952. [Google Scholar] [CrossRef] [PubMed]
- Staerk, L.; Sherer, J.A.; Ko, D.; Benjamin, E.J.; Helm, R.H. Atrial Fibrillation: Epidemiology, Pathophysiology, and Clinical Outcomes. Circ. Res. 2017, 120, 1501–1517. [Google Scholar] [CrossRef] [PubMed]
- Dai, H.; Zhang, Q.; Much, A.A.; Maor, E.; Segev, A.; Beinart, R.; Adawi, S.; Lu, Y.; Bragazzi, N.L.; Wu, J. Global, regional, and national prevalence, incidence, mortality, and risk factors for atrial fibrillation, 1990–2017: Results from the Global Burden of Disease Study 2017. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 7, 574–582. [Google Scholar] [CrossRef] [PubMed]
- Okafor, C.; Byrnes, J.; Stewart, S.; Scuffham, P.; Afoakwah, C. Cost Effectiveness of Strategies to Manage Atrial Fibrillation in Middle- and High-Income Countries: A Systematic Review. Pharmacoeconomics 2023, 41, 913–943. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Ye, M.; Lei, F.; Qin, J.J.; Liu, Y.M.; Chen, Z.; Chen, M.M.; Yang, C.; Zhang, P.; Ji, Y.X.; et al. Prevalence and trend of atrial fibrillation and its associated risk factors among the population from nationwide health check-up centers in China, 2012–2017. Front. Cardiovasc. Med. 2023, 10, 1151575. [Google Scholar] [CrossRef]
- Camacho, E.M.; Lip, G.Y.H. Estimating the impact of implementing an integrated care management approach with Atrial fibrillation Better Care (ABC) pathway for patients with atrial fibrillation in England from 2020–2040. Eur. Heart J.-Qual. Care Clin. Outcomes 2023, qcad055. [Google Scholar] [CrossRef]
- Joseph, P.G.; Healey, J.S.; Raina, P.; Connolly, S.J.; Ibrahim, Q.; Gupta, R.; Avezum, A.; Dans, A.L.; Lopez-Jaramillo, P.; Yeates, K.; et al. Global variations in the prevalence, treatment, and impact of atrial fibrillation in a multi-national cohort of 153,152 middle-aged individuals. Cardiovasc. Res. 2021, 117, 1523–1531. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomstrom-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Genaidy, A.; Tran, G.; Marroquin, P.; Estes, C.; Sloop, S. Improving Stroke Risk Prediction in the General Population: A Comparative Assessment of Common Clinical Rules, a New Multimorbid Index, and Machine-Learning-Based Algorithms. Thromb. Haemost. 2022, 122, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Li, S.; Liu, X.; Lip, G.Y.H.; Guo, L.; Zhu, W. Effect of Oral Anticoagulants in Atrial Fibrillation Patients with Polypharmacy: A Meta-analysis. Thromb. Haemost. 2023. [Google Scholar] [CrossRef] [PubMed]
- Treewaree, S.; Lip, G.Y.H.; Krittayaphong, R. Non-vitamin K Antagonist Oral Anticoagulant, Warfarin, and ABC Pathway Adherence on Hierarchical Outcomes: Win Ratio Analysis of the COOL-AF Registry. Thromb. Haemost. 2024, 124, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Romiti, G.F.; Proietti, M.; Bonini, N.; Ding, W.Y.; Boriani, G.; Huisman, M.V.; Lip, G.Y.H.; Investigators, G.-A. Clinical Complexity Domains, Anticoagulation, and Outcomes in Patients with Atrial Fibrillation: A Report from the GLORIA-AF Registry Phase II and III. Thromb. Haemost. 2022, 122, 2030–2041. [Google Scholar] [CrossRef]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association. Circulation 2023, 147, e93–e621. [Google Scholar] [CrossRef] [PubMed]
- Alshehri, A.M. Stroke in atrial fibrillation: Review of risk stratification and preventive therapy. J. Fam. Community Med. 2019, 26, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Son, M.K.; Lim, N.K.; Kim, H.W.; Park, H.Y. Risk of ischemic stroke after atrial fibrillation diagnosis: A national sample cohort. PLoS ONE 2017, 12, e0179687. [Google Scholar] [CrossRef]
- Wolf, P.A.; Abbott, R.D.; Kannel, W.B. Atrial fibrillation as an independent risk factor for stroke: The Framingham Study. Stroke 1991, 22, 983–988. [Google Scholar] [CrossRef]
- Marini, C.; De Santis, F.; Sacco, S.; Russo, T.; Olivieri, L.; Totaro, R.; Carolei, A. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: Results from a population-based study. Stroke 2005, 36, 1115–1119. [Google Scholar] [CrossRef]
- Schnabel, R.B.; Haeusler, K.G.; Healey, J.S.; Freedman, B.; Boriani, G.; Brachmann, J.; Brandes, A.; Bustamante, A.; Casadei, B.; Crijns, H.; et al. Searching for Atrial Fibrillation Poststroke: A White Paper of the AF-SCREEN International Collaboration. Circulation 2019, 140, 1834–1850. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.H.; Lane, D.A.; Lenarczyk, R.; Boriani, G.; Doehner, W.; Benjamin, L.A.; Fisher, M.; Lowe, D.; Sacco, R.L.; Schnabel, R.; et al. Integrated care for optimizing the management of stroke and associated heart disease: A position paper of the European Society of Cardiology Council on Stroke. Eur. Heart J. 2022, 43, 2442–2460. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, A.; Lip, G.Y.H.; Nordsletten, D.A.; Williams, S.E.; Aslanidi, O.; de Vecchi, A. Imaging and biophysical modelling of thrombogenic mechanisms in atrial fibrillation and stroke. Front. Cardiovasc. Med. 2022, 9, 1074562. [Google Scholar] [CrossRef]
- Ozdemir, H.; Sagris, D.; Lip, G.Y.H.; Abdul-Rahim, A.H. Stroke in Atrial Fibrillation and Other Atrial Dysrhythmias. Curr. Cardiol. Rep. 2023, 25, 357–369. [Google Scholar] [CrossRef]
- Kannel, W.B.; Abbott, R.D.; Savage, D.D.; McNamara, P.M. Coronary heart disease and atrial fibrillation: The Framingham Study. Am. Heart J. 1983, 106, 389–396. [Google Scholar] [CrossRef]
- Emdin, C.A.; Wong, C.X.; Hsiao, A.J.; Altman, D.G.; Peters, S.A.E.; Woodward, M.; Odutayo, A.A. Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: Systematic review and meta-analysis of cohort studies. BMJ 2016, 532, h7013. [Google Scholar] [CrossRef]
- Odutayo, A.; Wong, C.X.; Hsiao, A.J.; Hopewell, S.; Altman, D.G.; Emdin, C.A. Atrial fibrillation and risks of cardiovascular disease, renal disease, and death: Systematic review and meta-analysis. BMJ 2016, 354, i4482. [Google Scholar] [CrossRef] [PubMed]
- Ruddox, V.; Sandven, I.; Munkhaugen, J.; Skattebu, J.; Edvardsen, T.; Otterstad, J.E. Atrial fibrillation and the risk for myocardial infarction, all-cause mortality and heart failure: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2017, 24, 1555–1566. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Lenarczyk, R.; Pastori, D.; Ntaios, G.; Doehner, W.; Schnabel, R.B. Poststroke Cardiovascular Management: Current Concepts, Integrated Care, and Future Developments. Curr. Probl. Cardiol. 2023, 48, 101738. [Google Scholar] [CrossRef] [PubMed]
- Sposato, L.A.; Cipriano, L.E.; Saposnik, G.; Ruiz Vargas, E.; Riccio, P.M.; Hachinski, V. Diagnosis of atrial fibrillation after stroke and transient ischaemic attack: A systematic review and meta-analysis. Lancet Neurol. 2015, 14, 377–387. [Google Scholar] [CrossRef]
- Yang, X.M.; Rao, Z.Z.; Gu, H.Q.; Zhao, X.Q.; Wang, C.J.; Liu, L.P.; Liu, C.; Wang, Y.L.; Li, Z.X.; Xiao, R.P.; et al. Atrial Fibrillation Known before or Detected after Stroke Share Similar Risk of Ischemic Stroke Recurrence and Death. Stroke 2019, 50, 1124–1129. [Google Scholar] [CrossRef] [PubMed]
- Thakur, M.; Alsinbili, A.; Chattopadhyay, R.; Warburton, E.A.; Khadjooi, K.; Induruwa, I. Identifying the optimal time period for detection of atrial fibrillation after ischaemic stroke and TIA: An updated systematic review and meta-analysis of randomized control trials. Int. J. Stroke 2023, 30, 17474930231215277. [Google Scholar] [CrossRef] [PubMed]
- Kalarus, Z.; Mairesse, G.H.; Sokal, A.; Boriani, G.; Sredniawa, B.; Casado-Arroyo, R.; Wachter, R.; Frommeyer, G.; Traykov, V.; Dagres, N.; et al. Searching for atrial fibrillation: Looking harder, looking longer, and in increasingly sophisticated ways. An EHRA position paper. Europace 2023, 25, 185–198. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Mbotwe, S.; Bester, J.; Robinson, C.J.; Kell, D.B. Acute induction of anomalous and amyloidogenic blood clotting by molecular amplification of highly substoichiometric levels of bacterial lipopolysaccharide. J. R. Soc. Interface 2016, 123, 20160539. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Vlok, M.; Venter, C.; Bezuidenhout, J.A.; Laubscher, G.J.; Steenkamp, J.; Kell, D.B. Persistent clotting protein pathology in Long COVID/Post-Acute Sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc. Diabetol. 2021, 20, 172. [Google Scholar] [CrossRef] [PubMed]
- Kruger, A.; Vlok, M.; Turner, S.; Venter, C.; Laubscher, G.J.; Kell, D.B.; Pretorius, E. Proteomics of fibrin amyloid microclots in Long COVID/Post-Acute Sequelae of COVID-19 (PASC) shows many entrapped pro-inflammatory molecules that may also contribute to a failed fibrinolytic system. Cardiovasc. Diabetol. 2022, 21, 190. [Google Scholar] [CrossRef] [PubMed]
- Kell, D.B.; Pretorius, E. Proteins behaving badly. Substoichiometric molecular control and amplification of the initiation and nature of amyloid fibril formation: Lessons from and for blood clotting. Prog. Biophys. Mol. Biol. 2017, 123, 16–41. [Google Scholar] [CrossRef] [PubMed]
- Kell, D.B.; Pretorius, E. Are fibrinaloid microclots a cause of autoimmunity in Long Covid and other post-infection diseases? Biochem. J. 2023, 480, 1217–1240. [Google Scholar] [CrossRef] [PubMed]
- de Waal, G.M.; Engelbrecht, L.; Davis, T.; de Villiers, W.J.S.; Kell, D.B.; Pretorius, E. Correlative Light-Electron Microscopy detects lipopolysaccharide and its association with fibrin fibres in Parkinson’s Disease, Alzheimer’s Disease and Type 2 Diabetes Mellitus. Sci. Rep. 2018, 8, 16798. [Google Scholar] [CrossRef]
- Pretorius, E.; Page, M.J.; Mbotwe, S.; Kell, D.B. Lipopolysaccharide-binding protein (LBP) can reverse the amyloid state of fibrin seen or induced in Parkinson’s disease. PLoS ONE 2018, 13, e0192121. [Google Scholar] [CrossRef]
- Pretorius, E.; Page, M.J.; Hendricks, L.; Nkosi, N.B.; Benson, S.R.; Kell, D.B. Both lipopolysaccharide and lipoteichoic acids potently induce anomalous fibrin amyloid formation: Assessment with novel Amytracker™ stains. J. R. Soc. Interface 2018, 15, 20170941. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Bester, J.; Page, M.J.; Kell, D.B. The potential of LPS-binding protein to reverse amyloid formation in plasma fibrin of individuals with Alzheimer-type dementia. Front. Aging Neurosci. 2018, 10, 257. [Google Scholar] [CrossRef] [PubMed]
- Grobbelaar, L.M.; Venter, C.; Vlok, M.; Ngoepe, M.; Laubscher, G.J.; Lourens, P.J.; Steenkamp, J.; Kell, D.B.; Pretorius, E. SARS-CoV-2 spike protein S1 induces fibrin(ogen) resistant to fibrinolysis: Implications for microclot formation in COVID-19. Biosci. Rep. 2021, 41, BSR20210611. [Google Scholar] [CrossRef] [PubMed]
- Grobbelaar, L.M.; Kruger, A.; Venter, C.; Burger, E.M.; Laubscher, G.J.; Maponga, T.G.; Kotze, M.J.; Kwaan, H.C.; Miller, J.B.; Fulkerson, D.; et al. Relative hypercoagulopathy of the SARS-CoV-2 Beta and Delta variants when compared to the less severe Omicron variants is related to TEG parameters, the extent of fibrin amyloid microclots, and the severity of clinical illness. Semin. Thromb. Haemost. 2022, 48, 858–868. [Google Scholar] [CrossRef] [PubMed]
- Alon, U. An Introduction to Systems Biology: Design Principles of Biological Circuits; Chapman and Hall/CRC: London, UK, 2006. [Google Scholar]
- Kell, D.B.; Knowles, J.D. The role of modeling in systems biology. In System Modeling in Cellular Biology: From Concepts to Nuts and Bolts; Szallasi, Z., Stelling, J., Periwal, V., Eds.; MIT Press: Cambridge, UK, 2006; pp. 3–18. [Google Scholar]
- Palsson, B.Ø. Systems Biology: Properties of Reconstructed Networks; Cambridge University Press: Cambridge, UK, 2006. [Google Scholar]
- Klipp, E.; Herwig, R.; Kowald, A.; Wierling, C.; Lehrach, H. Systems Biology in Practice: Concepts, Implementation and Clinical Application; Wiley/VCH: Berlin, Germany, 2005. [Google Scholar]
- Buzan, T. How to Mind Map; Thorsons: London, UK, 2002. [Google Scholar]
- Hull, D.; Pettifer, S.R.; Kell, D.B. Defrosting the digital library: Bibliographic tools for the next generation web. PLoS Comput. Biol. 2008, 4, e1000204. [Google Scholar] [CrossRef] [PubMed]
- Kell, D.B.; Kenny, L.C. A dormant microbial component in the development of pre-eclampsia. Front. Med. Obs. Gynecol. 2016, 3, 60. [Google Scholar] [CrossRef]
- Kenny, L.C.; Kell, D.B. Immunological tolerance, pregnancy and pre-eclampsia: The roles of semen microbes and the father. Front. Med. Obs. Gynecol. 2018, 4, 239. [Google Scholar] [CrossRef]
- Bilano, V.L.; Ota, E.; Ganchimeg, T.; Mori, R.; Souza, J.P. Risk factors of pre-eclampsia/eclampsia and its adverse outcomes in low- and middle-income countries: A WHO secondary analysis. PLoS ONE 2014, 9, e91198. [Google Scholar] [CrossRef] [PubMed]
- Bartsch, E.; Medcalf, K.E.; Park, A.L.; Ray, J.G.; High Risk of Pre-eclampsia Identification, G. Clinical risk factors for pre-eclampsia determined in early pregnancy: Systematic review and meta-analysis of large cohort studies. BMJ 2016, 353, i1753. [Google Scholar] [CrossRef]
- Giannakou, K.; Evangelou, E.; Papatheodorou, S.I. Genetic and non-genetic risk factors for pre-eclampsia: Umbrella review of systematic reviews and meta-analyses of observational studies. Ultrasound Obstet. Gynecol. 2018, 51, 720–730. [Google Scholar] [CrossRef]
- Allotey, J.; Snell, K.I.E.; Smuk, M.; Hooper, R.; Chan, C.L.; Ahmed, A.; Chappell, L.C.; von Dadelszen, P.; Dodds, J.; Green, M.; et al. Validation and development of models using clinical, biochemical and ultrasound markers for predicting pre-eclampsia: An individual participant data meta-analysis. Health Technol. Assess. 2020, 24, 72. [Google Scholar] [CrossRef] [PubMed]
- Machano, M.M.; Joho, A.A. Prevalence and risk factors associated with severe pre-eclampsia among postpartum women in Zanzibar: A cross-sectional study. BMC Public Health 2020, 20, 1347. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Brayboy, L.; Tripathi, A. Pre-eclampsia: A Scoping Review of Risk Factors and Suggestions for Future Research Direction. Regen. Eng. Transl. Med. 2022, 8, 394–406. [Google Scholar] [CrossRef] [PubMed]
- Xue, Y.; Yang, N.; Gu, X.; Wang, Y.; Zhang, H.; Jia, K. Risk Prediction Model of Early-Onset Preeclampsia Based on Risk Factors and Routine Laboratory Indicators. Life 2023, 13, 1648. [Google Scholar] [CrossRef] [PubMed]
- Elawad, T.; Scott, G.; Bone, J.N.; Elwell, H.; Lopez, C.E.; Filippi, V.; Green, M.; Khalil, A.; Kinshella, M.W.; Mistry, H.D.; et al. Risk factors for pre-eclampsia in clinical practice guidelines: Comparison with the evidence. BJOG 2024, 131, 46–62. [Google Scholar] [CrossRef] [PubMed]
- Todros, T.; Verdiglione, P.; Oggè, G.; Paladini, D.; Vergani, P.; Cardaropoli, S. Low incidence of hypertensive disorders of pregnancy in women treated with spiramycin for toxoplasma infection. Br. J. Clin. Pharmacol. 2006, 61, 336–340. [Google Scholar] [CrossRef]
- Todros, T.; Vasario, E.; Cardaropoli, S. Preeclampsia as an infectious disease. Exp. Rev. Obs. Gynecol. 2007, 2, 735–741. [Google Scholar] [CrossRef]
- Thagard, P. How Scientists Explain Disease; Princeton University Press: Princeton, NJ, USA, 1999. [Google Scholar]
- Thagard, P. Coherence, truth, and the development of scientific knowledge. Philos. Sci. 2007, 74, 28–47. [Google Scholar] [CrossRef]
- Thagard, P. (Ed.) The Cognitive Science of Science: Explanation, Discovery, and Conceptual Change; MIT Press: Cambridge, MA, USA, 2012. [Google Scholar]
- Petsko, G.A. Guilt by association. Genome Biol. 2009, 10, 104. [Google Scholar] [CrossRef]
- Oliver, S.G. Guilt-by-association goes global. Nature 2000, 403, 601–603. [Google Scholar] [CrossRef]
- Voy, B.H.; Scharff, J.A.; Perkins, A.D.; Saxton, A.M.; Borate, B.; Chesler, E.J.; Branstetter, L.K.; Langston, M.A. Extracting gene networks for low-dose radiation using graph theoretical algorithms. PLoS Comput. Biol. 2006, 2, e89. [Google Scholar] [CrossRef] [PubMed]
- Tian, W.; Zhang, L.V.; Tasan, M.; Gibbons, F.D.; King, O.D.; Park, J.; Wunderlich, Z.; Cherry, J.M.; Roth, F.P. Combining guilt-by-association and guilt-by-profiling to predict Saccharomyces cerevisiae gene function. Genome Biol. 2008, 9 (Suppl. S1), S7. [Google Scholar] [CrossRef] [PubMed]
- Gillis, J.; Pavlidis, P. “Guilt by association” is the exception rather than the rule in gene networks. PLoS Comput. Biol. 2012, 8, e1002444. [Google Scholar] [CrossRef] [PubMed]
- Baker, M. Genomics: The search for association. Nature 2010, 467, 1135–1138. [Google Scholar] [CrossRef] [PubMed]
- Lappalainen, T.; Scott, A.J.; Brandt, M.; Hall, I.M. Genomic Analysis in the Age of Human Genome Sequencing. Cell 2019, 177, 70–84. [Google Scholar] [CrossRef] [PubMed]
- Alsheikh, A.J.; Wollenhaupt, S.; King, E.A.; Reeb, J.; Ghosh, S.; Stolzenburg, L.R.; Tamim, S.; Lazar, J.; Davis, J.W.; Jacob, H.J. The landscape of GWAS validation; systematic review identifying 309 validated non-coding variants across 130 human diseases. BMC Med. Genom. 2022, 15, 74. [Google Scholar] [CrossRef] [PubMed]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate—A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. B Met. 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Broadhurst, D.; Kell, D.B. Statistical strategies for avoiding false discoveries in metabolomics and related experiments. Metabolomics 2006, 2, 171–196. [Google Scholar] [CrossRef]
- van den Oord, E.J. Controlling false discoveries in genetic studies. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2008, 147B, 637–644. [Google Scholar] [CrossRef]
- Gunning, M.; Pavlidis, P. “Guilt by association” is not competitive with genetic association for identifying autism risk genes. Sci. Rep. 2021, 11, 15950. [Google Scholar] [CrossRef]
- Al-Falahi, Z.; Williamson, J.; Dimitri, H. Atrial Fibrillation and Sleep Apnoea: Guilt by Association? Heart Lung Circ. 2017, 26, 902–910. [Google Scholar] [CrossRef]
- Bommasani, R.; Hudson, D.A.; Adeli, E.; Altman, R.; Arora, S.; Arx, S.v.; Bernstein, M.S.; Bohg, J.; Bosselut, A.; Brunskill, E.; et al. On the Opportunities and Risks of Foundation Models. arXiv 2021, arXiv:2108.07258. [Google Scholar]
- Vaswani, A.; Shazeer, N.; Parmar, N.; Uszkoreit, J.; Jones, L.; Gomez, A.N.; Kaiser, L.; Polosukhin, I. Attention Is All You Need. arXiv 2017, arXiv:1706.03762. [Google Scholar]
- Kollman, J.M.; Pandi, L.; Sawaya, M.R.; Riley, M.; Doolittle, R.F. Crystal Structure of Human Fibrinogen. Biochemistry 2009, 48, 3877–3886. [Google Scholar] [CrossRef] [PubMed]
- Weisel, J.W. Fibrinogen and fibrin. Adv. Protein Chem. 2005, 70, 247–299. [Google Scholar] [CrossRef]
- Weisel, J.W.; Litvinov, R.I. Fibrin Formation, Structure and Properties. Subcell. Biochem. 2017, 82, 405–456. [Google Scholar] [CrossRef]
- Collet, J.P.; Park, D.; Lesty, C.; Soria, J.; Soria, C.; Montalescot, G.; Weisel, J.W. Influence of fibrin network conformation and fibrin fiber diameter on fibrinolysis speed: Dynamic and structural approaches by confocal microscopy. Arterioscler. Thromb. Vasc. Biol. 2000, 20, 1354–1361. [Google Scholar] [CrossRef] [PubMed]
- Ferri, S.; Kojima, K.; Sode, K. Review of glucose oxidases and glucose dehydrogenases: A bird’s eye view of glucose sensing enzymes. J. Diabetes Sci. Technol. 2011, 5, 1068–1076. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Sigley, J.; Pieters, M.; Helms, C.C.; Nagaswami, C.; Weisel, J.W.; Guthold, M. Fibrin Fiber Stiffness Is Strongly Affected by Fiber Diameter, but Not by Fibrinogen Glycation. Biophys. J. 2016, 110, 1400–1410. [Google Scholar] [CrossRef] [PubMed]
- Belcher, H.A.; Guthold, M.; Hudson, N.E. What is the diameter of a fibrin fiber? Res. Pract. Thromb. Haemost. 2023, 7, 100285. [Google Scholar] [CrossRef]
- Guthold, M.; Liu, W.; Stephens, B.; Lord, S.T.; Hantgan, R.R.; Erie, D.A.; Taylor, R.M., Jr.; Superfine, R. Visualization and mechanical manipulations of individual fibrin fibers suggest that fiber cross section has fractal dimension 1.3. Biophys. J. 2004, 87, 4226–4236. [Google Scholar] [CrossRef] [PubMed]
- Kell, D.B.; Laubscher, G.J.; Pretorius, E. A central role for amyloid fibrin microclots in long COVID/PASC: Origins and therapeutic implications. Biochem. J. 2022, 479, 537–559. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Bronkhorst, P.; Briedenhann, S.; Smit, E.; Franz, R.C. Comparisons of the fibrin networks during pregnancy, nonpregnancy and pregnancy during dysfibrinogenaemia using the scanning electron microscope. Blood Coagul. Fibrinolysis 2009, 20, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Oberholzer, H.M.; van der Spuy, W.J.; Meiring, J.H. The changed ultrastructure of fibrin networks during use of oral contraception and hormone replacement. J. Thromb. Thrombolysis 2010, 30, 502–506. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Swanepoel, A.C.; Oberholzer, H.M.; van der Spuy, W.J.; Duim, W.; Wessels, P.F. A descriptive investigation of the ultrastructure of fibrin networks in thrombo-embolic ischemic stroke. J. Thromb. Thrombolysis 2011, 31, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Steyn, H.; Engelbrecht, M.; Swanepoel, A.C.; Oberholzer, H.M. Differences in fibrin fiber diameters in healthy individuals and thromboembolic ischemic stroke patients. Blood Coagul. Fibrinolysis 2011, 22, 696–700. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E. The use of a desktop scanning electron microscope as a diagnostic tool in studying fibrin networks of thrombo-embolic ischemic stroke. Ultrastruct. Pathol. 2011, 35, 245–250. [Google Scholar] [CrossRef]
- Pretorius, E.; Oberholzer, H.M.; van der Spuy, W.J.; Swanepoel, A.C.; Soma, P. Qualitative scanning electron microscopy analysis of fibrin networks and platelet abnormalities in diabetes. Blood Coagul. Fibrinolysis 2011, 22, 463–467. [Google Scholar] [CrossRef] [PubMed]
- Lipinski, B.; Pretorius, E. Novel pathway of iron-induced blood coagulation: Implications for diabetes mellitus and its complications. Pol. Arch. Med. Wewn. 2012, 122, 115–122. [Google Scholar] [CrossRef]
- Kell, D.B.; Pretorius, E. The simultaneous occurrence of both hypercoagulability and hypofibrinolysis in blood and serum during systemic inflammation, and the roles of iron and fibrin(ogen). Integr. Biol. 2015, 7, 24–52. [Google Scholar] [CrossRef]
- Pretorius, E.; Vermeulen, N.; Bester, J.; Lipinski, B.; Kell, D.B. A novel method for assessing the role of iron and its functional chelation in fibrin fibril formation: The use of scanning electron microscopy. Toxicol. Mech. Methods 2013, 23, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Kell, D.B. Diagnostic morphology: Biophysical indicators for iron-driven inflammatory diseases. Integr. Biol. 2014, 6, 486–510. [Google Scholar] [CrossRef]
- Pretorius, E.; Bester, J.; Kell, D.B. A bacterial component to Alzheimer-type dementia seen via a systems biology approach that links iron dysregulation and inflammagen shedding to disease. J. Alzheimers Dis. 2016, 53, 1237–1256. [Google Scholar] [CrossRef] [PubMed]
- Kell, D.B.; Pretorius, E. No effects without causes. The Iron Dysregulation and Dormant Microbes hypothesis for chronic, inflammatory diseases. Biol. Rev. 2018, 93, 1518–1557. [Google Scholar] [CrossRef] [PubMed]
- Kell, D.B.; Heyden, E.L.; Pretorius, E. The biology of lactoferrin, an iron-binding protein that can help defend against viruses and bacteria. Front. Immunol. 2020, 11, 1221. [Google Scholar] [CrossRef]
- Lipinski, B.; Pretorius, E.; Oberholzer, H.M.; van der Spuy, W.J. Interaction of fibrin with red blood cells: The role of iron. Ultrastruct. Pathol. 2012, 36, 79–84. [Google Scholar] [CrossRef]
- Crystal, A.S.; Giasson, B.I.; Crowe, A.; Kung, M.P.; Zhuang, Z.P.; Trojanowski, J.Q.; Lee, V.M. A comparison of amyloid fibrillogenesis using the novel fluorescent compound K114. J. Neurochem. 2003, 86, 1359–1368. [Google Scholar] [CrossRef]
- Palladini, G.; Merlini, G. Systemic amyloidoses: What an internist should know. Eur. J. Intern. Med. 2013, 24, 729–739. [Google Scholar] [CrossRef]
- Martinez-Naharro, A.; Hawkins, P.N.; Fontana, M. Cardiac amyloidosis. Clin. Med. 2018, 18, s30–s35. [Google Scholar] [CrossRef]
- Fagihi, M.H.A.; Bhattacharjee, S. Amyloid Fibrillation of Insulin: Amelioration Strategies and Implications for Translation. ACS Pharmacol. Transl. Sci. 2022, 5, 1050–1061. [Google Scholar] [CrossRef]
- Kuo, C.T.; Chen, Y.L.; Hsu, W.T.; How, S.C.; Cheng, Y.H.; Hsueh, S.S.; Liu, H.S.; Lin, T.H.; Wu, J.W.; Wang, S.S. Investigating the effects of erythrosine B on amyloid fibril formation derived from lysozyme. Int. J. Biol. Macromol. 2017, 98, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Aguzzi, A.; Lakkaraju, A.K.K. Cell Biology of Prions and Prionoids: A Status Report. Trends Cell Biol. 2016, 26, 40–51. [Google Scholar] [CrossRef] [PubMed]
- Aguzzi, A.; De Cecco, E. Shifts and drifts in prion science. Science 2020, 370, 32–34. [Google Scholar] [CrossRef] [PubMed]
- Frontzek, K.; Bardelli, M.; Senatore, A.; Henzi, A.; Reimann, R.R.; Bedir, S.; Marino, M.; Hussain, R.; Jurt, S.; Meisl, G.; et al. A conformational switch controlling the toxicity of the prion protein. Nat. Struct. Mol. Biol. 2022, 29, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Mbotwe, S.; Kell, D.B. Lipopolysaccharide-binding protein (LBP) reverses the amyloid state of fibrin seen in plasma of type 2 diabetics with cardiovascular comorbidities. Sci. Rep. 2017, 7, 9680. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Page, M.J.; Engelbrecht, L.; Ellis, G.C.; Kell, D.B. Substantial fibrin amyloidogenesis in type 2 diabetes assessed using amyloid-selective fluorescent stains. Cardiovasc. Diabetol. 2017, 16, 141. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Bester, J.; Page, M.J.; Kell, D.B. Reversal of amyloid formation in the plasma fibrin of individuals with Alzheimer-type dementia using LPS-binding protein. J. Alzheimers Dis. 2018. [Google Scholar]
- Pretorius, E.; Venter, C.; Laubscher, G.J.; Lourens, P.J.; Steenkamp, J.; Kell, D.B. Prevalence of readily detected amyloid blood clots in ‘unclotted’ Type 2 Diabetes Mellitus and COVID-19 plasma: A preliminary report. Cardiovasc. Diabetol. 2020, 19, 193. [Google Scholar] [CrossRef]
- Pretorius, E.; Venter, C.; Laubscher, G.J.; Kotze, M.J.; Oladejo, S.; Watson, L.R.; Rajaratnam, K.; Watson, B.W.; Kell, D.B. Prevalence of symptoms, comorbidities, fibrin amyloid microclots and platelet pathology in individuals with Long COVID/Post-Acute Sequelae of COVID-19 (PASC). Cardiovasc. Diabetol. 2022, 21, 148. [Google Scholar] [CrossRef]
- Turner, S.; Laubscher, G.J.; Khan, M.A.; Kell, D.B.; Pretorius, E. Accelerating discovery: A novel flow cytometric method for detecting fibrin(ogen) amyloid microclots using long COVID as a model. Heliyon 2023, 9, e19605. [Google Scholar] [CrossRef]
- Laubscher, G.J.; Lourens, P.J.; Venter, C.; Kell, D.B.; Pretorius, E. TEG®, Microclot and Platelet Mapping for Guiding Early Management of Severe COVID-19 Coagulopathy. J. Clin. Med. 2021, 10, 5381. [Google Scholar] [CrossRef] [PubMed]
- Zamolodchikov, D.; Strickland, S. Abeta delays fibrin clot lysis by altering fibrin structure and attenuating plasminogen binding to fibrin. Blood 2012, 119, 3342–3351. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Gianoulis, T.A.; Yip, K.Y.; Gerstein, M.; Snyder, M. Extensive in vivo metabolite-protein interactions revealed by large-scale systematic analyses. Cell 2010, 143, 639–650. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Snyder, M. Metabolites as global regulators: A new view of protein regulation: Systematic investigation of metabolite-protein interactions may help bridge the gap between genome-wide association studies and small molecule screening studies. Bioessays 2011, 33, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Kell, D.B. Metabolites do social networking. Nat. Chem. Biol. 2011, 7, 7–8. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, A.C.; Lindeque, B.G.; Swart, P.J.; Abdool, Z.; Pretorius, E. Estrogen causes ultrastructural changes of fibrin networks during the menstrual cycle: A qualitative investigation. Microsc. Res. Technol. 2014, 77, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, A.C.; Visagie, A.; de Lange, Z.; Emmerson, O.; Nielsen, V.G.; Pretorius, E. The clinical relevance of altered fibrinogen packaging in the presence of 17beta-estradiol and progesterone. Thromb. Res. 2016, 146, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Undas, A. Fibrin clot properties and their modulation in thrombotic disorders. Thromb. Haemost. 2014, 112, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Carr, M.E., Jr.; Alving, B.M. Effect of fibrin structure on plasmin-mediated dissolution of plasma clots. Blood Coagul. Fibrinolysis 1995, 6, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Bryk, A.H.; Natorska, J.; Zabczyk, M.; Zettl, K.; Wiśniewski, J.R.; Undas, A. Plasma fibrin clot proteomics in patients with acute pulmonary embolism: Association with clot properties. J. Proteom. 2020, 229, 103946. [Google Scholar] [CrossRef]
- Kell, D.B.; Pretorius, E. The potential role of ischaemia-reperfusion injury in chronic, relapsing diseases such as rheumatoid arthritis, long COVID and ME/CFS: Evidence, mechanisms, and therapeutic implications. Biochem. J. 2022, 479, 1653–1708. [Google Scholar] [PubMed]
- Appelman, B.; Charlton, B.T.; Goulding, R.P.; Kerkhoff, T.J.; Breedveld, E.A.; Noort, W.; Offringa, C.; Bloemers, F.W.; van Weeghel, M.; Schomakers, B.V.; et al. Muscle abnormalities worsen after postexertional malaise in long COVID. Nat. Commun. 2024, 15, 17. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Johnsen, S.P.; Guo, Y.; Lip, G.Y.H. Epidemiology of Atrial Fibrillation: Geographic/Ecological Risk Factors, Age, Sex, Genetics. Card. Electrophysiol. Clin. 2021, 13, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Essien, U.R.; Chiswell, K.; Kaltenbach, L.A.; Wang, T.Y.; Fonarow, G.C.; Thomas, K.L.; Turakhia, M.P.; Benjamin, E.J.; Rodriguez, F.; Fang, M.C.; et al. Association of Race and Ethnicity with Oral Anticoagulation and Associated Outcomes in Patients with Atrial Fibrillation: Findings from the Get with the Guidelines-Atrial Fibrillation Registry. JAMA Cardiol. 2022, 7, 1207–1217. [Google Scholar] [CrossRef] [PubMed]
- Marinigh, R.; Lip, G.Y.; Fiotti, N.; Giansante, C.; Lane, D.A. Age as a risk factor for stroke in atrial fibrillation patients: Implications for thromboprophylaxis. J. Am. Coll. Cardiol. 2010, 56, 827–837. [Google Scholar] [CrossRef] [PubMed]
- Lowres, N.; Olivier, J.; Chao, T.F.; Chen, S.A.; Chen, Y.; Diederichsen, A.; Fitzmaurice, D.A.; Gomez-Doblas, J.J.; Harbison, J.; Healey, J.S.; et al. Estimated stroke risk, yield, and number needed to screen for atrial fibrillation detected through single time screening: A multicountry patient-level meta-analysis of 141,220 screened individuals. PLoS Med. 2019, 16, e1002903. [Google Scholar] [CrossRef]
- Ayinde, H.; Schweizer, M.L.; Crabb, V.; Ayinde, A.; Abugroun, A.; Hopson, J. Age modifies the risk of atrial fibrillation among athletes: A systematic literature review and meta-analysis. Int. J. Cardiol. Heart Vasc. 2018, 18, 25–29. [Google Scholar] [CrossRef]
- Goudis, C.A.; Ntalas, I.V.; Ketikoglou, D.G. Atrial Fibrillation in Athletes. Cardiol. Rev. 2015, 23, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Isaac, E.; Cooper, S.M.; Jones, S.A.; Loubani, M. Do age-associated changes of voltage-gated sodium channel isoforms expressed in the mammalian heart predispose the elderly to atrial fibrillation? World J. Cardiol. 2020, 12, 123–135. [Google Scholar] [CrossRef]
- Wang, T.J.; Parise, H.; Levy, D.; D’Agostino, R.B., Sr.; Wolf, P.A.; Vasan, R.S.; Benjamin, E.J. Obesity and the risk of new-onset atrial fibrillation. JAMA 2004, 292, 2471–2477. [Google Scholar] [CrossRef]
- Wanahita, N.; Messerli, F.H.; Bangalore, S.; Gami, A.S.; Somers, V.K.; Steinberg, J.S. Atrial fibrillation and obesity--results of a meta-analysis. Am. Heart J. 2008, 155, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Overvad, T.F.; Rasmussen, L.H.; Skjøth, F.; Overvad, K.; Lip, G.Y.H.; Larsen, T.B. Body mass index and adverse events in patients with incident atrial fibrillation. Am. J. Med. 2013, 126, 640.e9–640.e17. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, R.K.; Ezekowitz, J.; Andersson, U.; Alexander, J.H.; Granger, C.B.; Halvorsen, S.; Hanna, M.; Hijazi, Z.; Jansky, P.; Lopes, R.D.; et al. The ‘obesity paradox’ in atrial fibrillation: Observations from the ARISTOTLE (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation) trial. Eur. Heart J. 2016, 37, 2869–2878. [Google Scholar] [CrossRef]
- Zhu, W.; Wan, R.; Liu, F.; Hu, J.; Huang, L.; Li, J.; Hong, K. Relation of Body Mass Index with Adverse Outcomes among Patients with Atrial Fibrillation: A Meta-Analysis and Systematic Review. J. Am. Heart Assoc. 2016, 5, e004006. [Google Scholar] [CrossRef] [PubMed]
- Proietti, M.; Guiducci, E.; Cheli, P.; Lip, G.Y. Is There an Obesity Paradox for Outcomes in Atrial Fibrillation? A Systematic Review and Meta-Analysis of Non-Vitamin K Antagonist Oral Anticoagulant Trials. Stroke 2017, 48, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, R.K.; Ezekowitz, J.A.; Hijazi, Z.; Westerbergh, J.; Aulin, J.; Alexander, J.H.; Granger, C.B.; Halvorsen, S.; Hanna, M.S.; Lopes, R.D.; et al. Obesity paradox on outcome in atrial fibrillation maintained even considering the prognostic influence of biomarkers: Insights from the ARISTOTLE trial. Open Heart 2018, 5, e000908. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Guo, L.; Xiao, K.; Zhu, W.; Liu, M.; Wan, R.; Hong, K. The obesity paradox for outcomes in atrial fibrillation: Evidence from an exposure-effect analysis of prospective studies. Obes. Rev. 2020, 21, e12970. [Google Scholar] [CrossRef] [PubMed]
- Panchal, G.; Mahmood, M.; Lip, G.Y.H. Revisiting the risks of incident atrial fibrillation: A narrative review. Part 2. Kardiol. Pol. 2019, 77, 515–524. [Google Scholar] [CrossRef]
- Proietti, M.; Boriani, G. Obesity Paradox in Atrial Fibrillation: Implications for Outcomes and Relationship with Oral Anticoagulant Drugs. Am. J. Cardiovasc. Drugs 2020, 20, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Reyes, H.; Lara-Vaca, S.; Ochoa-Guzmán, A.; Chiquete, E.; Registro Mexicano de Fibrilación Auricular Study Group. Obesity Paradox and 12 Month Outcome in Patients with Atrial Fibrillation. Arch. Med. Res. 2021, 52, 233–239. [Google Scholar] [CrossRef]
- Li, Y.G.; Xie, P.X.; Alsheikh-Ali, A.A.; AlMahmeed, W.; Sulaiman, K.; Asaad, N.; Liu, S.W.; Zubaid, M.; Lip, G.Y.H. The “obesity paradox” in patients with atrial fibrillation: Insights from the Gulf SAFE registry. Front. Cardiovasc. Med. 2022, 9, 1032633. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Huang, N.; Chen, X.; Jiang, S.; Zhang, W.; Hu, W.; Su, J.; Dai, H.; Gu, P.; Huang, X.; et al. Association between Body Mass Index and Clinical Outcomes in Patients with Non-valvular Atrial Fibrillation Receiving Direct Oral Anticoagulants: A New Piece of Evidence on the Obesity Paradox from China. Cardiovasc. Drugs Ther. 2023, 37, 715–727. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.U.; Duran, C.A.; Rahman, H.; Lekkala, M.; Saleem, M.A.; Kaluski, E. A meta-analysis of continuous positive airway pressure therapy in prevention of cardiovascular events in patients with obstructive sleep apnoea. Eur. Heart J. 2018, 39, 2291–2297. [Google Scholar] [CrossRef] [PubMed]
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pepin, J.L.; et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Ye, K.; Xiaokereti, J.; Ma, M.; Guo, Y.; Zhou, X.; Tang, B. Histopathological substrate of the atrial myocardium in the progression of obstructive sleep apnoea-related atrial fibrillation. Sleep Breath. 2021, 25, 807–818. [Google Scholar] [CrossRef] [PubMed]
- Feghaly, J.; Zakka, P.; London, B.; MacRae, C.A.; Refaat, M.M. Genetics of Atrial Fibrillation. J. Am. Heart Assoc. 2018, 7, e009884. [Google Scholar] [CrossRef]
- Christophersen, I.E.; Ravn, L.S.; Budtz-Jørgensen, E.; Skytthe, A.; Haunsø, S.; Svendsen, J.H.; Christensen, K. Familial aggregation of atrial fibrillation: A study in Danish twins. Circ. Arrhythm. Electrophysiol. 2009, 2, 378–383. [Google Scholar] [CrossRef]
- Christophersen, I.E.; Budtz-Jorgensen, E.; Olesen, M.S.; Haunso, S.; Christensen, K.; Svendsen, J.H. Familial atrial fibrillation predicts increased risk of mortality: A study in Danish twins. Circ. Arrhythm. Electrophysiol. 2013, 6, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Weng, L.C.; Choi, S.H.; Klarin, D.; Smith, J.G.; Loh, P.R.; Chaffin, M.; Roselli, C.; Hulme, O.L.; Lunetta, K.L.; Dupuis, J.; et al. Heritability of Atrial Fibrillation. Circ. Cardiovasc. Genet. 2017, 10, e001838. [Google Scholar] [CrossRef]
- Roselli, C.; Chaffin, M.D.; Weng, L.C.; Aeschbacher, S.; Ahlberg, G.; Albert, C.M.; Almgren, P.; Alonso, A.; Anderson, C.D.; Aragam, K.G.; et al. Multi-ethnic genome-wide association study for atrial fibrillation. Nat. Genet. 2018, 50, 1225–1233. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J.G.M. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest 2010, 137, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Friberg, L.; Rosenqvist, M.; Lip, G.Y.H. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: The Swedish Atrial Fibrillation cohort study. Eur. Heart J. 2012, 33, 1500–1510. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Q.; Proietti, M.; Senoo, K.; Lip, G.Y.H. Asymptomatic versus symptomatic atrial fibrillation: A systematic review of age/gender differences and cardiovascular outcomes. Int. J. Cardiol. 2015, 191, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.G.; Miyazawa, K.; Wolff, A.; Zubaid, M.; Alsheikh-Ali, A.A.; Sulaiman, K.; Lip, G.Y.H. One-year risks of stroke and mortality in patients with atrial fibrillation from different clinical settings: The Gulf SAFE registry and Darlington AF registry. Int. J. Cardiol. 2019, 274, 158–162. [Google Scholar] [CrossRef]
- Djoussé, L.; Levy, D.; Benjamin, E.J.; Blease, S.J.; Russ, A.; Larson, M.G.; Massaro, J.M.; D’Agostino, R.B.; Wolf, P.A.; Ellison, R.C. Long-term alcohol consumption and the risk of atrial fibrillation in the Framingham Study. Am. J. Cardiol. 2004, 93, 710–713. [Google Scholar] [CrossRef] [PubMed]
- Mukamal, K.J.; Tolstrup, J.S.; Friberg, J.; Jensen, G.; Gronbaek, M. Alcohol consumption and risk of atrial fibrillation in men and women: The Copenhagen City Heart Study. Circulation 2005, 112, 1736–1742. [Google Scholar] [CrossRef] [PubMed]
- Powers, S.K.; Deminice, R.; Ozdemir, M.; Yoshihara, T.; Bomkamp, M.P.; Hyatt, H. Exercise-induced oxidative stress: Friend or foe? J. Sport. Health Sci. 2020, 9, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Thirupathi, A.; Pinho, R.A.; Ugbolue, U.C.; He, Y.; Meng, Y.; Gu, Y. Effect of Running Exercise on Oxidative Stress Biomarkers: A Systematic Review. Front. Physiol. 2020, 11, 610112. [Google Scholar] [CrossRef]
- Cerqueira, E.; Marinho, D.A.; Neiva, H.P.; Lourenco, O. Inflammatory Effects of High and Moderate Intensity Exercise-A Systematic Review. Front. Physiol. 2019, 10, 1550. [Google Scholar] [CrossRef]
- da Rocha, A.L.; Pinto, A.P.; Kohama, E.B.; Pauli, J.R.; de Moura, L.P.; Cintra, D.E.; Ropelle, E.R.; da Silva, A.S.R. The proinflammatory effects of chronic excessive exercise. Cytokine 2019, 119, 57–61. [Google Scholar] [CrossRef]
- Durand, F.; Raberin, A. Exercise-Induced Hypoxemia in Endurance Athletes: Consequences for Altitude Exposure. Front. Sports Act. Living 2021, 3, 663674. [Google Scholar] [CrossRef] [PubMed]
- Aizer, A.; Gaziano, J.M.; Cook, N.R.; Manson, J.E.; Buring, J.E.; Albert, C.M. Relation of vigorous exercise to risk of atrial fibrillation. Am. J. Cardiol. 2009, 103, 1572–1577. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, W.T.; Alirhayim, Z.; Blaha, M.J.; Juraschek, S.P.; Keteyian, S.J.; Brawner, C.A.; Al-Mallah, M.H. Cardiorespiratory Fitness and Risk of Incident Atrial Fibrillation: Results from the Henry Ford Exercise Testing (FIT) Project. Circulation 2015, 131, 1827–1834. [Google Scholar] [CrossRef]
- Blaszczyk, R.T.; Gorlo, A.; Dukacz, M.; Konopka, A.; Glowniak, A. Association between exposure to air pollution and incidence of atrial fibrillation. Ann. Agric. Environ. Med. 2023, 30, 15–21. [Google Scholar] [CrossRef]
- Mandaglio-Collados, D.; López-Gálvez, R.; Ruiz-Alcaraz, A.J.; López-García, C.; Roldán, V.; Lip, G.Y.H.; Marín, F.; Rivera-Caravaca, J.M. Impact of particulate matter on the incidence of atrial fibrillation and the risk of adverse clinical outcomes: A review. Sci. Total Environ. 2023, 880, 163352. [Google Scholar] [CrossRef]
- Link, M.S.; Luttmann-Gibson, H.; Schwartz, J.; Mittleman, M.A.; Wessler, B.; Gold, D.R.; Dockery, D.W.; Laden, F. Acute exposure to air pollution triggers atrial fibrillation. J. Am. Coll. Cardiol. 2013, 62, 816–825. [Google Scholar] [CrossRef]
- Zhang, J.; Chen, G.; Xia, H.; Wang, X.; Wang, C.; Cai, M.; Gao, Y.; Lip, G.Y.H.; Lin, H. Associations of Life’s Essential 8 and fine particulate matter pollution with the incidence of atrial fibrillation. J. Hazard. Mater. 2023, 459, 132114. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Su, B.; Li, D.; Cui, F.; Tang, L.; Wang, J.; Tian, Y.; Zheng, X. Air pollution, genetic susceptibility, and the risk of atrial fibrillation: A large prospective cohort study. Proc. Natl. Acad. Sci. USA 2023, 120, e2302708120. [Google Scholar] [CrossRef]
- Wang, F.; Ahat, X.; Liang, Q.; Ma, Y.; Sun, M.; Lin, L.; Li, T.; Duan, J.; Sun, Z. The relationship between exposure to PM2.5 and atrial fibrillation in older adults: A systematic review and meta-analysis. Sci. Total Environ. 2021, 784, 147106. [Google Scholar] [CrossRef]
- Shao, Q.; Liu, T.; Korantzopoulos, P.; Zhang, Z.; Zhao, J.; Li, G. Association between air pollution and development of atrial fibrillation: A meta-analysis of observational studies. Heart Lung 2016, 45, 557–562. [Google Scholar] [CrossRef]
- Yue, C.; Yang, F.; Li, F.; Chen, Y. Association between air pollutants and atrial fibrillation in general population: A systematic review and meta-analysis. Ecotoxicol. Environ. Saf. 2021, 208, 111508. [Google Scholar] [CrossRef] [PubMed]
- Calderón-Garcidueñas, L.; Solt, A.C.; Henriquez-Roldán, C.; Torres-Jardon, R.; Nuse, B.; Herritt, L.; Villarreal-Calderón, R.; Osnaya, N.; Stone, I.; Garcia, R.; et al. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid beta-42 and alpha-synuclein in children and young adults. Toxicol. Pathol. 2008, 36, 289–310. [Google Scholar] [CrossRef] [PubMed]
- Iaccarino, L.; La Joie, R.; Lesman-Segev, O.H.; Lee, E.; Hanna, L.; Allen, I.E.; Hillner, B.E.; Siegel, B.A.; Whitmer, R.A.; Carrillo, M.C.; et al. Association between Ambient Air Pollution and Amyloid Positron Emission Tomography Positivity in Older Adults with Cognitive Impairment. JAMA Neurol. 2021, 78, 197–207. [Google Scholar] [CrossRef]
- Jang, S.; Kim, E.W.; Zhang, Y.; Lee, J.; Cho, S.Y.; Ha, J.; Kim, H.; Kim, E. Particulate matter increases beta-amyloid and activated glial cells in hippocampal tissues of transgenic Alzheimer’s mouse: Involvement of PARP-1. Biochem. Biophys. Res. Commun. 2018, 500, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Sahu, B.; Mackos, A.R.; Floden, A.M.; Wold, L.E.; Combs, C.K. Particulate Matter Exposure Exacerbates Amyloid-beta Plaque Deposition and Gliosis in APP/PS1 Mice. J. Alzheimers Dis. 2021, 80, 761–774. [Google Scholar] [CrossRef]
- Marfella, R.; Prattichizzo, F.; Sardu, C.; Fulgenzi, G.; Graciotti, L.; Spadoni, T.; D’Onofrio, N.; Scisciola, L.; La Grotta, R.; Frigé, C.; et al. Microplastics and nanoplastics in atheromas and cardiovascular events. N. Engl. J. Med. 2024, 390, 900–910. [Google Scholar] [CrossRef] [PubMed]
- Eaker, E.D.; Sullivan, L.M.; Kelly-Hayes, M.; D’Agostino, R.B., Sr.; Benjamin, E.J. Anger and hostility predict the development of atrial fibrillation in men in the Framingham Offspring Study. Circulation 2004, 109, 1267–1271. [Google Scholar] [CrossRef] [PubMed]
- Panchal, G.; Mahmood, M.; Lip, G.Y.H. Revisiting the risks of incident atrial fibrillation: A narrative review. Part 1. Kardiol. Pol. 2019, 77, 430–436. [Google Scholar] [CrossRef]
- Kell, D.B. Iron behaving badly: Inappropriate iron chelation as a major contributor to the aetiology of vascular and other progressive inflammatory and degenerative diseases. BMC Med. Genom. 2009, 2, 2. [Google Scholar]
- Kell, D.B. Towards a unifying, systems biology understanding of large-scale cellular death and destruction caused by poorly liganded iron: Parkinson’s, Huntington’s, Alzheimer’s, prions, bactericides, chemical toxicology and others as examples. Arch. Toxicol. 2010, 577, 825–889. [Google Scholar]
- Kell, D.B.; Pretorius, E. Serum ferritin is an important disease marker, and is mainly a leakage product from damaged cells. Metallomics 2014, 6, 748–773. [Google Scholar] [CrossRef]
- Kell, D.B.; Heyden, E.L.; Pretorius, E. The biology of lactoferrin, an iron-binding protein that defends against viruses and bacteria. OSF Prepr. 2020. Available online: https://osf.io/fxudj/ (accessed on 1 March 2024). [CrossRef] [PubMed]
- Itzhaki, R.F.; Cosby, S.L.; Wozniak, M.A. Herpes simplex virus type 1 and Alzheimer’s disease: The autophagy connection. J. Neurovirol. 2008, 14, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Itzhaki, R.F.; Lathe, R.; Balin, B.J.; Ball, M.J.; Braak, H.; Bearer, E.L.; Bullido, M.J.; Carter, C.; Clerici, M.; Cosby, S.L.; et al. Microbes and Alzheimer’s Disease. J. Alzheimers Dis. 2016, 51, 979–984. [Google Scholar] [CrossRef] [PubMed]
- Itzhaki, R.F.; Lathe, R. Herpes Viruses and Senile Dementia: First Population Evidence for a Causal Link. J. Alzheimers Dis. 2018, 64, 363–366. [Google Scholar] [CrossRef] [PubMed]
- Itzhaki, R.F. Corroboration of a Major Role for Herpes Simplex Virus Type 1 in Alzheimer’s Disease. Front. Aging Neurosci. 2018, 10, 324. [Google Scholar] [CrossRef] [PubMed]
- Grobler, C.; van Tongeren, M.; Gettemans, J.; Kell, D.; Pretorius, E. Alzheimer-type dementia: A systems view provides a unifying explanation of its development. J. Alzheimer’s Dis. 2023, 91, 43–70. [Google Scholar] [CrossRef] [PubMed]
- Jean-Baptiste, V.S.E.; Xia, C.Q.; Clare-Salzler, M.J.; Horwitz, M.S. Type 1 Diabetes and Type 1 Interferonopathies: Localization of a Type 1 Common Thread of Virus Infection in the Pancreas. EBioMedicine 2017, 22, 10–17. [Google Scholar] [CrossRef]
- Gundersen, E. Is Diabetes of Infectious Origin? J. Infect. Dis. 1927, 41, 197–202. [Google Scholar] [CrossRef]
- Craighead, J.E. The role of viruses in the pathogenesis of pancreatic disease and diabetes mellitus. Prog. Med. Virol. 1975, 19, 161–214. [Google Scholar]
- Notkins, A.L. Virus-induced diabetes mellitus. Arch. Virol. 1977, 54, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.W.; Notkins, A.L. Virus-induced diabetes in mice. Metabolism 1983, 32, 37–40. [Google Scholar] [CrossRef]
- Rajsfus, B.F.; Mohana-Borges, R.; Allonso, D. Diabetogenic viruses: Linking viruses to diabetes mellitus. Heliyon 2023, 9, e15021. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Bester, J.; Vermeulen, N.; Alummoottil, S.; Soma, P.; Buys, A.V.; Kell, D.B. Poorly controlled type 2 diabetes is accompanied by significant morphological and ultrastructural changes in both erythrocytes and in thrombin-generated fibrin: Implications for diagnostics. Cardiovasc. Diabetol. 2015, 13, 30. [Google Scholar] [CrossRef] [PubMed]
- Soma, P.; Pretorius, E. Interplay between ultrastructural findings and atherothrombotic complications in type 2 diabetes mellitus. Cardiovasc. Diabetol. 2015, 14, 96. [Google Scholar] [CrossRef] [PubMed]
- Jayakrishnan, B. Historical aspects and current understanding of the connections and implications of viruses and diabetes: A narrative review. Clin. Epidemiol. Glob. Health 2022, 16, 101110. [Google Scholar] [CrossRef]
- Sohail, M.U.; Mashood, F.; Oberbach, A.; Chennakkandathil, S.; Schmidt, F. The role of pathogens in diabetes pathogenesis and the potential of immunoproteomics as a diagnostic and prognostic tool. Front. Microbiol. 2022, 13, 1042362. [Google Scholar] [CrossRef] [PubMed]
- Nobs, S.P.; Kolodziejczyk, A.A.; Adler, L.; Horesh, N.; Botscharnikow, C.; Herzog, E.; Mohapatra, G.; Hejndorf, S.; Hodgetts, R.J.; Spivak, I.; et al. Lung dendritic-cell metabolism underlies susceptibility to viral infection in diabetes. Nature 2023, 624, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Naveed, Z.; Velasquez Garcia, H.A.; Wong, S.; Wilton, J.; McKee, G.; Mahmood, B.; Binka, M.; Rasali, D.; Janjua, N.Z. Association of COVID-19 Infection with Incident Diabetes. JAMA Netw. Open. 2023, 6, e238866. [Google Scholar] [CrossRef]
- Wekerle, H. Epstein-Barr virus sparks brain autoimmunity in multiple sclerosis. Nature 2022, 603, 230–232. [Google Scholar] [CrossRef]
- Schönrich, G.; Abdelaziz, M.O.; Raftery, M.J. Epstein-Barr virus, interleukin-10 and multiple sclerosis: A ménage à trois. Front. Immunol. 2022, 13, 1028972. [Google Scholar] [CrossRef]
- Rousseau, B.A.; Bhaduri-McIntosh, S. Inflammation and Epstein-Barr Virus at the Crossroads of Multiple Sclerosis and Post-Acute Sequelae of COVID-19 Infection. Viruses 2023, 15, 949. [Google Scholar] [CrossRef]
- Nunes, J.M.; Kell, D.B.; Pretorius, E. Cardiovascular and haematological pathology in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): A role for Viruses. Blood Rev. 2023, 60, 101075. [Google Scholar] [CrossRef]
- Nunes, J.M.; Kruger, A.; Proal, A.; Kell, D.B.; Pretorius, E. The Occurrence of Hyperactivated Platelets and Fibrinaloid Microclots in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). Pharmaceuticals 2022, 15, 931. [Google Scholar] [CrossRef]
- Cannon, T.; Gruenheid, S. Microbes and Parkinson’s disease: From associations to mechanisms. Trends Microbiol. 2022, 30, 749–760. [Google Scholar] [CrossRef]
- Leta, V.; Urso, D.; Batzu, L.; Lau, Y.H.; Mathew, D.; Boura, I.; Raeder, V.; Falup-Pecurariu, C.; van Wamelen, D.; Ray Chaudhuri, K. Viruses, parkinsonism and Parkinson’s disease: The past, present and future. J. Neural Transm. 2022, 129, 1119–1132. [Google Scholar] [CrossRef]
- Limphaibool, N.; Iwanowski, P.; Holstad, M.J.V.; Kobylarek, D.; Kozubski, W. Infectious Etiologies of Parkinsonism: Pathomechanisms and Clinical Implications. Front. Neurol. 2019, 10, 652. [Google Scholar] [CrossRef]
- Caggiu, E.; Arru, G.; Hosseini, S.; Niegowska, M.; Sechi, G.; Zarbo, I.R.; Sechi, L.A. Inflammation, Infectious Triggers, and Parkinson’s Disease. Front. Neurol. 2019, 10. [Google Scholar] [CrossRef]
- Ebringer, A.; Rashid, T. Rheumatoid arthritis is caused by Proteus: The molecular mimicry theory and Karl Popper. Front. Biosci. 2009, 1, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Ebringer, A.; Rashid, T.; Wilson, C. Rheumatoid arthritis, Proteus, anti-CCP antibodies and Karl Popper. Autoimmun. Rev. 2010, 9, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Ebringer, A. Rheumatoid Arthritis and Proteus; Springer: London, UK, 2012. [Google Scholar]
- Ebringer, A.; Rashid, T. Rheumatoid arthritis is caused by a Proteus urinary tract infection. APMIS 2014, 122, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Bezuidenhout, J.; Venter, C.; Roberts, T.; Tarr, G.; Kell, D.; Pretorius, E. Detection of citrullinated fibrin in plasma clots of RA patients and its relation to altered structural clot properties, disease-related inflammation and prothrombotic tendency. Front. Immunol. 2020, 11, 577523. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Oberholzer, H.M.; van der Spuy, W.J.; Swanepoel, A.C.; Soma, P. Scanning electron microscopy of fibrin networks in rheumatoid arthritis: A qualitative analysis. Rheumatol. Int. 2012, 32, 1611–1615. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Akeredolu, O.-O.; Soma, P.; Kell, D.B. Major involvement of bacterial components in rheumatoid arthritis and its accompanying oxidative stress, systemic inflammation and hypercoagulability. Exp. Biol. Med. 2017, 242, 355–373. [Google Scholar] [CrossRef] [PubMed]
- Goudis, C.A.; Ketikoglou, D.G. Obstructive sleep and atrial fibrillation: Pathophysiological mechanisms and therapeutic implications. Int. J. Cardiol. 2017, 230, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.A.; Cappuccio, F.P. A systematic review of COVID-19 and obstructive sleep apnoea. Sleep Med. Rev. 2021, 55, 101382. [Google Scholar] [CrossRef]
- Mandel, H.L.; Colleen, G.; Abedian, S.; Ammar, N.; Charles Bailey, L.; Bennett, T.D.; Daniel Brannock, M.; Brosnahan, S.B.; Chen, Y.; Chute, C.G.; et al. Risk of post-acute sequelae of SARS-CoV-2 infection associated with pre-coronavirus disease obstructive sleep apnea diagnoses: An electronic health record-based analysis from the RECOVER initiative. Sleep 2023, 46, zsad126. [Google Scholar] [CrossRef] [PubMed]
- Su, V.Y.; Liu, C.J.; Wang, H.K.; Wu, L.A.; Chang, S.C.; Perng, D.W.; Su, W.J.; Chen, Y.M.; Lin, E.Y.; Chen, T.J.; et al. Sleep apnea and risk of pneumonia: A nationwide population-based study. CMAJ 2014, 186, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Chiner, E.; Llombart, M.; Valls, J.; Pastor, E.; Sancho-Chust, J.N.; Andreu, A.L.; Sanchez-de-la-Torre, M.; Barbe, F. Association between Obstructive Sleep Apnea and Community-Acquired Pneumonia. PLoS ONE 2016, 11, e0152749. [Google Scholar] [CrossRef] [PubMed]
- Hariyanto, T.I.; Kurniawan, A. Obstructive sleep apnea (OSA) and outcomes from coronavirus disease 2019 (COVID-19) pneumonia: A systematic review and meta-analysis. Sleep Med. 2021, 82, 47–53. [Google Scholar] [CrossRef]
- Ihara, M.; Washida, K. Linking Atrial Fibrillation with Alzheimer’s Disease: Epidemiological, Pathological, and Mechanistic Evidence. J. Alzheimers Dis. 2018, 62, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Benenati, S.; Canale, C.; De Marzo, V.; Della Bona, R.; Rosa, G.M.; Porto, I. Atrial fibrillation and Alzheimer’s disease: A conundrum. Eur. J. Clin. Investig. 2021, 51, e13451. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Wang, Y.; Wang, Y. Investigation of Causal Effect of Atrial Fibrillation on Alzheimer Disease: A Mendelian Randomization Study. J. Am. Heart Assoc. 2020, 9, e014889. [Google Scholar] [CrossRef] [PubMed]
- Proietti, R.; AlTurki, A.; Vio, R.; Licchelli, L.; Rivezzi, F.; Marafi, M.; Russo, V.; Potpara, T.S.; Kalman, J.M.; de Villers-Sidani, E.; et al. The association between atrial fibrillation and Alzheimer’s disease: Fact or fallacy? A systematic review and meta-analysis. J. Cardiovasc. Med. 2020, 21, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Papanastasiou, C.A.; Theochari, C.A.; Zareifopoulos, N.; Arfaras-Melainis, A.; Giannakoulas, G.; Karamitsos, T.D.; Palaiodimos, L.; Ntaios, G.; Avgerinos, K.I.; Kapogiannis, D.; et al. Atrial Fibrillation Is Associated with Cognitive Impairment, All-Cause Dementia, Vascular Dementia, and Alzheimer’s Disease: A Systematic Review and Meta-Analysis. J. Gen. Intern. Med. 2021, 36, 3122–3135. [Google Scholar] [CrossRef] [PubMed]
- Manemann, S.M.; Chamberlain, A.M.; Bielinski, S.J.; Jiang, R.; Weston, S.A.; Roger, V.L. Predicting Alzheimer’s Disease and Related Dementias in Heart Failure and Atrial Fibrillation. Am. J. Med. 2023, 136, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Nakase, T.; Tatewaki, Y.; Thyreau, B.; Odagiri, H.; Tomita, N.; Yamamoto, S.; Takano, Y.; Muranaka, M.; Taki, Y. Impact of atrial fibrillation on the cognitive decline in Alzheimer’s disease. Alzheimers Res. Ther. 2023, 15, 15. [Google Scholar] [CrossRef] [PubMed]
- Falsetti, L.; Viticchi, G.; Buratti, L.; Grigioni, F.; Capucci, A.; Silvestrini, M. Interactions between Atrial Fibrillation, Cardiovascular Risk Factors, and ApoE Genotype in Promoting Cognitive Decline in Patients with Alzheimer’s Disease: A Prospective Cohort Study. J. Alzheimers Dis. 2018, 62, 713–725. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Z.; Liu, T.; Tse, G.; Gong, M.; Gladding, P.A.; Smaill, B.H.; Stiles, M.K.; Gillis, A.M.; Zhao, J. A Machine Learning Aided Systematic Review and Meta-Analysis of the Relative Risk of Atrial Fibrillation in Patients with Diabetes Mellitus. Front. Physiol. 2018, 9, 835. [Google Scholar] [CrossRef]
- Wang, A.; Green, J.B.; Halperin, J.L.; Piccini, J.P., Sr. Atrial Fibrillation and Diabetes Mellitus: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2019, 74, 1107–1115. [Google Scholar] [CrossRef]
- Domek, M.; Li, Y.G.; Gumprecht, J.; Asaad, N.; Rashed, W.; Alsheikh-Ali, A.; Nabrdalik, K.; Gumprecht, J.; Zubaid, M.; Lip, G.Y.H. One-year all-cause mortality risk among atrial fibrillation patients in Middle East with and without diabetes: The Gulf SAFE registry. Int. J. Cardiol. 2020, 302, 47–52. [Google Scholar] [CrossRef]
- Alijla, F.; Buttia, C.; Reichlin, T.; Razvi, S.; Minder, B.; Wilhelm, M.; Muka, T.; Franco, O.H.; Bano, A. Association of diabetes with atrial fibrillation types: A systematic review and meta-analysis. Cardiovasc. Diabetol. 2021, 20, 230. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Lee, S.R.; Choi, E.K.; Lee, H.; Han, M.; Ahn, H.J.; Kwon, S.; Lee, S.W.; Han, K.D.; Oh, S.; et al. Accumulated hypertension burden on atrial fibrillation risk in diabetes mellitus: A nationwide population study. Cardiovasc. Diabetol. 2023, 22, 12. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.; Lee, S.R.; Choi, E.K.; Ahn, H.J.; Lee, S.W.; Jung, J.H.; Han, K.D.; Oh, S.; Lip, G.Y.H. Association between Atrial Fibrillation and Diabetes-Related Complications: A Nationwide Cohort Study. Diabetes Care 2023, 46, 2240–2248. [Google Scholar] [CrossRef] [PubMed]
- Ding, W.Y.; Kotalczyk, A.; Boriani, G.; Marin, F.; Blomström-Lundqvist, C.; Potpara, T.S.; Fauchier, L.; Lip, G.Y.H.; ESC-EHRA EORP-AF Long-Term General Registry Investigators. Impact of diabetes on the management and outcomes in atrial fibrillation: An analysis from the ESC-EHRA EORP-AF Long-Term General Registry. Eur. J. Intern. Med. 2022, 103, 41–49. [Google Scholar] [CrossRef]
- Lorenzo-Almorós, A.; Casado Cerrada, J.; Álvarez-Sala Walther, L.A.; Méndez Bailón, M.; Lorenzo González, Ó. Atrial Fibrillation and Diabetes Mellitus: Dangerous Liaisons or Innocent Bystanders? J. Clin. Med. 2023, 12, 2868. [Google Scholar] [CrossRef] [PubMed]
- Bohne, L.J.; Johnson, D.; Rose, R.A.; Wilton, S.B.; Gillis, A.M. The Association between Diabetes Mellitus and Atrial Fibrillation: Clinical and Mechanistic Insights. Front. Physiol. 2019, 10, 135. [Google Scholar] [CrossRef] [PubMed]
- Hong, C.T.; Chan, L.; Wu, D.; Chen, W.T.; Chien, L.N. Association between Parkinson’s Disease and Atrial Fibrillation: A Population-Based Study. Front. Neurol. 2019, 10, 22. [Google Scholar] [CrossRef] [PubMed]
- Alves, M.; Abrantes, A.M.; Portugal, G.; Cruz, M.M.; Reimao, S.; Caldeira, D.; Ferro, J.M.; Ferreira, J.J. Does Parkinson’s Disease Increase the Risk of Atrial Fibrillation? Insights from Electrocardiogram and Risk Scores from a Case-Control Study. Front. Neurol. 2021, 12, 633900. [Google Scholar] [CrossRef]
- Han, S.; Moon, I.; Choi, E.K.; Han, K.D.; Cho, H.C.; Lee, S.Y.; Yang, S.; Kwon, S.; Choi, Y.J.; Lee, H.J.; et al. Increased atrial fibrillation risk in Parkinson’s disease: A nationwide population-based study. Ann. Clin. Transl. Neurol. 2021, 8, 238–246. [Google Scholar] [CrossRef]
- Cereja, F.; Alves, M.; Ferreira, J.J.; Caldeira, D. Atrial fibrillation risk on Parkinson’s disease—A systematic review and meta-analysis. J. Thromb. Thrombolysis 2023, 55, 747–750. [Google Scholar] [CrossRef] [PubMed]
- Rong, J.C.; Chen, X.D.; Jin, N.K.; Hong, J. Exploring the causal association of rheumatoid arthritis with atrial fibrillation: A Mendelian randomization study. Clin. Rheumatol. 2023, 43, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.W.; Han, M.; Jung, I.; Ahn, S.S. New-onset atrial fibrillation in seropositive rheumatoid arthritis: Association with disease-modifying anti-rheumatic drugs treatment. Rheumatology 2023, 63, 630–638. [Google Scholar] [CrossRef] [PubMed]
- Kerola, A.M.; Rollefstad, S.; Semb, A.G. Atherosclerotic Cardiovascular Disease in Rheumatoid Arthritis: Impact of Inflammation and Antirheumatic Treatment. Eur. Cardiol. 2021, 16, e18. [Google Scholar] [CrossRef] [PubMed]
- Semb, A.G.; Rollefstad, S.; Sexton, J.; Ikdahl, E.; Crowson, C.S.; van Riel, P.; Kitas, G.; Graham, I.; Kerola, A.M.; Surf-RA. Oral anticoagulant treatment in rheumatoid arthritis patients with atrial fibrillation results of an international audit. Int. J. Cardiol. Heart Vasc. 2022, 42, 101117. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Haththotuwa, R.; Kwok, C.S.; Babu, A.; Kotronias, R.A.; Rushton, C.; Zaman, A.; Fryer, A.A.; Kadam, U.; Chew-Graham, C.A.; et al. Preeclampsia and Future Cardiovascular Health: A Systematic Review and Meta-Analysis. Circ. Cardiovasc. Qual. Outcomes 2017, 10, e003497. [Google Scholar] [CrossRef] [PubMed]
- Thilaganathan, B.; Kalafat, E. Cardiovascular System in Preeclampsia and Beyond. Hypertension 2019, 73, 522–531. [Google Scholar] [CrossRef]
- Corica, B.; Tartaglia, F.; Oliva, A.; Raparelli, V.; Cangemi, R.; Basili, S.; Lip, G.Y.H.; Proietti, M.; Romiti, G.F. Prevalence of new-onset atrial fibrillation in hospitalized patients with community-acquired pneumonia: A systematic review and meta-analysis. Intern. Emerg. Med. 2023, 18, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Bhatla, A.; Mayer, M.M.; Adusumalli, S.; Hyman, M.C.; Oh, E.; Tierney, A.; Moss, J.; Chahal, A.A.; Anesi, G.; Denduluri, S.; et al. COVID-19 and cardiac arrhythmias. Heart Rhythm. 2020, 17, 1439–1444. [Google Scholar] [CrossRef]
- García-Granja, P.E.; Veras, C.; Aparisi, Á.; Amat-Santos, I.J.; Catalá, P.; Marcos, M.; Cabezón, G.; Candela, J.; Gil, J.F.; Uribarri, A.; et al. Atrial fibrillation in patients with SARS-CoV-2 infection. Med. Clin. 2021, 157, 58–63. [Google Scholar] [CrossRef]
- Al-Abbas, O.; Alshaikhli, A.; Amran, H.A. New-Onset Atrial Fibrillation and Multiple Systemic Emboli in a COVID-19 Patient. Cureus 2021, 13, e12917. [Google Scholar] [CrossRef] [PubMed]
- Bagnato, G.; Imbalzano, E.; Aragona, C.O.; Ioppolo, C.; Di Micco, P.; La Rosa, D.; Costa, F.; Micari, A.; Tomeo, S.; Zirilli, N.; et al. New-Onset Atrial Fibrillation and Early Mortality Rate in COVID-19 Patients: Association with IL-6 Serum Levels and Respiratory Distress. Medicina 2022, 58, 530. [Google Scholar] [CrossRef]
- Kanuri, S.H.; Jayesh Sirrkay, P.; Ulucay, A.S. COVID-19 HEART unveiling as atrial fibrillation: Pathophysiology, management and future directions for research. Egypt. Heart J. 2023, 75, 36. [Google Scholar] [CrossRef] [PubMed]
- Duckheim, M.; Schreieck, J. COVID-19 and Cardiac Arrhythmias. Hamostaseologie 2021, 41, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Rav-Acha, M.; Orlev, A.; Itzhaki, I.; Zimmerman, S.F.; Fteiha, B.; Bohm, D.; Kurd, R.; Samuel, T.Y.; Asher, E.; Helviz, Y.; et al. Cardiac arrhythmias amongst hospitalised Coronavirus 2019 (COVID-19) patients: Prevalence, characterisation, and clinical algorithm to classify arrhythmic risk. Int. J. Clin. Pract. 2021, 75, e13788. [Google Scholar] [CrossRef] [PubMed]
- Mouram, S.; Pannone, L.; Gauthey, A.; Sorgente, A.; Vergara, P.; Bisignani, A.; Monaco, C.; Mojica, J.; Al Housari, M.; Miraglia, V.; et al. Incidence and Predictors of Cardiac Arrhythmias in Patients with COVID-19. Front. Cardiovasc. Med. 2022, 9, 908177. [Google Scholar] [CrossRef] [PubMed]
- Niehues, P.; Wegner, F.K.; Wolfes, J.; Willy, K.; Ellermann, C.; Vollenberg, R.; Reinecke, H.; Rosenow, F.; Lepper, J.; Sackarnd, J.; et al. Incidence and predictors of cardiac arrhythmias in patients with COVID-19 induced ARDS. J. Cardiol. 2022, 80, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Jiang, Z.; Meulendijks, E.R.; Baylan, U.; Waas, I.S.E.; Bugiani, M.; Tuinman, P.R.; Fronczek, J.; Heunks, L.M.A.; de Groot, J.R.; et al. Atrial inflammation and microvascular thrombogenicity are increased in deceased COVID-19 patients. Cardiovasc. Pathol. 2023, 64, 107524. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, J. The COVID Heart-One Year after SARS-CoV-2 Infection, Patients Have an Array of Increased Cardiovascular Risks. JAMA 2022, 327, 1113–1114. [Google Scholar] [CrossRef]
- Berman, A.; Iglesias, M.; Khanna, R.; Beaulieu, T. The association between COVID-19 infection and incident atrial fibrillation: Results from a retrospective cohort study using a large US commercial insurance database. Open Heart 2023, 10, e002399. [Google Scholar] [CrossRef]
- Azaña Gómez, J.; Pérez-Belmonte, L.M.; Rubio-Rivas, M.; Bascuñana, J.; Quirós-López, R.; Martínez, M.L.T.; Hernandez, E.M.; Roque-Rojas, F.; Méndez-Bailón, M.; Gómez-Huelgas, R.; et al. Mortality risk factors in patients with SARS-CoV-2 infection and atrial fibrillation: Data from the SEMI-COVID-19 registry. Med. Clin. 2022, 159, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Rubini-Costa, R.; Bermúdez-Jiménez, F.; Rivera-López, R.; Sola-García, E.; Nagib-Raya, H.; Moreno-Escobar, E.; López-Zúñiga, M.Á.; Briones-Través, A.; Sanz-Herrera, F.; Sequí-Sabater, J.M.; et al. Prevalence of bleeding secondary to anticoagulation and mortality in patients with atrial fibrillation admitted with SARS-CoV-2 infection. Med. Clin. 2022, 158, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Zuin, M.; Rigatelli, G.; Bilato, C.; Zanon, F.; Zuliani, G.; Roncon, L. Pre-existing atrial fibrillation is associated with increased mortality in COVID-19 Patients. J. Interv. Card. Electrophysiol. 2021, 62, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Musikantow, D.R.; Turagam, M.K.; Sartori, S.; Chu, E.; Kawamura, I.; Shivamurthy, P.; Bokhari, M.; Oates, C.; Zhang, C.; Pumill, C.; et al. Atrial Fibrillation in Patients Hospitalized with COVID-19: Incidence, Predictors, Outcomes, and Comparison to Influenza. JACC Clin. Electrophysiol. 2021, 7, 1120–1130. [Google Scholar] [CrossRef] [PubMed]
- Pardo Sanz, A.; Salido Tahoces, L.; Ortega Pérez, R.; González Ferrer, E.; Sánchez Recalde, Á.; Zamorano Gómez, J.L. New-onset atrial fibrillation during COVID-19 infection predicts poor prognosis. Cardiol. J. 2021, 28, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Guo, B.; Zhao, C.; He, M.Z.; Senter, C.; Zhou, Z.; Peng, J.; Li, S.; Fitzpatrick, A.L.; Lindstrom, S.; Stebbins, R.C.; et al. Identifying patterns of reported findings on long-term cardiac complications of COVID-19: A systematic review and meta-analysis. BMC Med. 2023, 21, 468. [Google Scholar] [CrossRef] [PubMed]
- Huseynov, A.; Akin, I.; Duerschmied, D.; Scharf, R.E. Cardiac Arrhythmias in Post-COVID Syndrome: Prevalence, Pathology, Diagnosis, and Treatment. Viruses 2023, 15, 389. [Google Scholar] [CrossRef]
- Pari, B.; Babbili, A.; Kattubadi, A.; Thakre, A.; Thotamgari, S.; Gopinathannair, R.; Olshansky, B.; Dominic, P. COVID-19 Vaccination and Cardiac Arrhythmias: A Review. Curr. Cardiol. Rep. 2023, 25, 925–940. [Google Scholar] [CrossRef] [PubMed]
- Walkey, A.J.; Greiner, M.A.; Heckbert, S.R.; Jensen, P.N.; Piccini, J.P.; Sinner, M.F.; Curtis, L.H.; Benjamin, E.J. Atrial fibrillation among Medicare beneficiaries hospitalized with sepsis: Incidence and risk factors. Am. Heart J. 2013, 165, 949–955.e943. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, S.; Klein Klouwenberg, P.M.C.; Cremer, O.L. Incidence, risk factors and outcomes of new-onset atrial fibrillation in patients with sepsis: A systematic review. Crit. Care 2014, 18, 688. [Google Scholar] [CrossRef]
- Klein Klouwenberg, P.M.C.; Frencken, J.F.; Kuipers, S.; Ong, D.S.Y.; Peelen, L.M.; van Vught, L.A.; Schultz, M.J.; van der Poll, T.; Bonten, M.J.; Cremer, O.L.; et al. Incidence, Predictors, and Outcomes of New-Onset Atrial Fibrillation in Critically Ill Patients with Sepsis. A Cohort Study. Am. J. Respir. Crit. Care Med. 2017, 195, 205–211. [Google Scholar] [CrossRef]
- Bosch, N.A.; Cohen, D.M.; Walkey, A.J. Risk Factors for New-Onset Atrial Fibrillation in Patients with Sepsis: A Systematic Review and Meta-Analysis. Crit. Care Med. 2019, 47, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Bashar, S.K.; Hossain, M.B.; Ding, E.; Walkey, A.J.; McManus, D.D.; Chon, K.H. Atrial Fibrillation Detection During Sepsis: Study on MIMIC III ICU Data. IEEE J. Biomed. Health Inform. 2020, 24, 3124–3135. [Google Scholar] [CrossRef]
- Aibar, J.; Schulman, S. New-Onset Atrial Fibrillation in Sepsis: A Narrative Review. Semin. Thromb. Hemost. 2021, 47, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Proietti, M.; Romiti, G.F. Management of Ventricular Heart Rate in Atrial Fibrillation Patients with Sepsis. Chest 2021, 159, 1315–1316. [Google Scholar] [CrossRef]
- Xiao, F.P.; Chen, M.Y.; Wang, L.; He, H.; Jia, Z.Q.; Kuai, L.; Zhou, H.B.; Liu, M.; Hong, M. Outcomes of new-onset atrial fibrillation in patients with sepsis: A systematic review and meta-analysis of 225,841 patients. Am. J. Emerg. Med. 2021, 42, 23–30. [Google Scholar] [CrossRef]
- Induruwa, I.; Hennebry, E.; Hennebry, J.; Thakur, M.; Warburton, E.A.; Khadjooi, K. Sepsis-driven atrial fibrillation and ischaemic stroke. Is there enough evidence to recommend anticoagulation? Eur. J. Intern. Med. 2022, 98, 32–36. [Google Scholar] [CrossRef]
- Corica, B.; Romiti, G.F.; Basili, S.; Proietti, M. Prevalence of New-Onset Atrial Fibrillation and Associated Outcomes in Patients with Sepsis: A Systematic Review and Meta-Analysis. J. Pers. Med. 2022, 12, 547. [Google Scholar] [CrossRef] [PubMed]
- Honorato, M.O.; Sousa Filho, J.T.; Honorato Junior, L.F.B.; Watanabe, N.; Goulart, G.M.; Prado, R.R.D. Atrial Fibrillation and Sepsis in Elderly Patients and Their Associaton with In-Hospital Mortality. Arq. Bras. Cardiol. 2023, 120, e20220295. [Google Scholar] [CrossRef]
- Downes, M.; Welters, I.D.; Johnston, B.W. Study protocol: A systematic review and meta-analysis regarding the influence of coagulopathy and immune activation on new onset atrial fibrillation in patients with sepsis. PLoS ONE 2023, 18, e0290963. [Google Scholar] [CrossRef]
- Cano-Gamez, E.; Burnham, K.L.; Goh, C.; Allcock, A.; Malick, Z.H.; Overend, L.; Kwok, A.; Smith, D.A.; Peters-Sengers, H.; Antcliffe, D.; et al. An immune dysfunction score for stratification of patients with acute infection based on whole-blood gene expression. Sci. Transl. Med. 2022, 14, eabq4433. [Google Scholar] [CrossRef]
- van Amstel, R.B.E.; Kennedy, J.N.; Scicluna, B.P.; Bos, L.D.J.; Peters-Sengers, H.; Butler, J.M.; Cano-Gamez, E.; Knight, J.C.; Vlaar, A.P.J.; Cremer, O.L.; et al. Uncovering heterogeneity in sepsis: A comparative analysis of subphenotypes. Intensive Care Med. 2023, 49, 1360–1369. [Google Scholar] [CrossRef] [PubMed]
- Kell, D.B.; Pretorius, E. To what extent are the terminal stages of sepsis, septic shock, SIRS, and multiple organ dysfunction syndrome actually driven by a toxic prion/amyloid form of fibrin? Semin. Thromb. Hemost. 2018, 44, 224–238. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Mbotwe, S.; Bester, J.; Robinson, C.; Kell, D.B. Acute induction of anomalous blood clotting by highly substoichiometric levels of bacterial lipopolysaccharide (LPS). bioRxiv version. bioRxiv 2016, 2016-053538v053531. [Google Scholar] [CrossRef]
- Pretorius, E.; Kell, D.B. A perspective on how microscopy imaging of fibrinaloid microclots and platelet pathology may be applied in clinical investigations. Semin. Thromb. Haemost. 2023. [Google Scholar] [CrossRef]
- Levi, M.; van der Poll, T.; ten Cate, H.; van Deventer, S.J. The cytokine-mediated imbalance between coagulant and anticoagulant mechanisms in sepsis and endotoxaemia. Eur. J. Clin. Investig. 1997, 27, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Gando, S. Microvascular thrombosis and multiple organ dysfunction syndrome. Crit. Care Med. 2010, 38, S35–S42. [Google Scholar] [CrossRef]
- Levi, M. The coagulant response in sepsis and inflammation. Hamostaseologie 2010, 30, 10–16. [Google Scholar] [CrossRef]
- Iba, T.; Nagaoka, I.; Boulat, M. The anticoagulant therapy for sepsis-associated disseminated intravascular coagulation. Thromb. Res. 2013, 131, 383–389. [Google Scholar] [CrossRef]
- Allen, K.S.; Sawheny, E.; Kinasewitz, G.T. Anticoagulant modulation of inflammation in severe sepsis. World J. Crit. Care Med. 2015, 4, 105–115. [Google Scholar] [CrossRef]
- Li, X.; Ma, X. The role of heparin in sepsis: Much more than just an anticoagulant. Br. J. Haematol. 2017, 179, 389–398. [Google Scholar] [CrossRef]
- Murao, S.; Yamakawa, K. A Systematic Summary of Systematic Reviews on Anticoagulant Therapy in Sepsis. J. Clin. Med. 2019, 8, 1869. [Google Scholar] [CrossRef]
- Yu, S.; Ma, X.; Li, X. Phenotype-oriented anticoagulant therapy for sepsis: Still a work in progress. Int. J. Hematol. 2022, 116, 48–54. [Google Scholar] [CrossRef]
- Meziani, F.; Gando, S.; Vincent, J.L. Should all patients with sepsis receive anticoagulation? Yes. Intensive Care Med. 2017, 43, 452–454. [Google Scholar] [CrossRef]
- Scarlatescu, E.; Tomescu, D.; Arama, S.S. Anticoagulant Therapy in Sepsis. The Importance of Timing. J. Crit. Care Med. 2017, 3, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Umemura, Y.; Yamakawa, K. Optimal patient selection for anticoagulant therapy in sepsis: An evidence-based proposal from Japan. J. Thromb. Haemost. 2018, 16, 462–464. [Google Scholar] [CrossRef]
- Qi, W.; Liu, J.; Li, A. Effect of Anticoagulant versus Non-Anticoagulant Therapy on Mortality of Sepsis-Induced Disseminated Intravascular Coagulation: A Systematic Review and Meta-Analysis. Clin. Appl. Thromb. Hemost. 2023, 29, 10760296231157766. [Google Scholar] [CrossRef] [PubMed]
- Umemura, Y.; Nishida, T.; Yamakawa, K.; Ogura, H.; Oda, J.; Fujimi, S. Anticoagulant therapies against sepsis-induced disseminated intravascular coagulation. Acute Med. Surg. 2023, 10, e884. [Google Scholar] [CrossRef] [PubMed]
- Bustamante, A.; Garcia-Berrocoso, T.; Penalba, A.; Giralt, D.; Simats, A.; Muchada, M.; Zapata, E.; Rubiera, M.; Montaner, J. Sepsis biomarkers reprofiling to predict stroke-associated infections. J. Neuroimmunol. 2017, 312, 19–23. [Google Scholar] [CrossRef]
- Kishore, A.K.; Vail, A.; Jeans, A.R.; Chamorro, A.; Di Napoli, M.; Kalra, L.; Langhorne, P.; Roffe, C.; Westendorp, W.; Nederkoorn, P.J.; et al. Microbiological Etiologies of Pneumonia Complicating Stroke: A Systematic Review. Stroke 2018, 49, 1602–1609. [Google Scholar] [CrossRef]
- Shim, R.; Wong, C.H.Y. Ischemia, Immunosuppression and Infection--Tackling the Predicaments of Post-Stroke Complications. Int. J. Mol. Sci. 2016, 17, 64. [Google Scholar] [CrossRef]
- Westendorp, W.F.; Vermeij, J.D.; Hilkens, N.A.; Brouwer, M.C.; Algra, A.; van der Worp, H.B.; Dippel, D.W.J.; van de Beek, D.; Nederkoorn, P.J.; PASS-Investigators. Development and internal validation of a prediction rule for post-stroke infection and post-stroke pneumonia in acute stroke patients. Eur. Stroke J. 2018, 3, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, S.; Pourgholaminejad, A.; Saberi, A. Stroke Associated with SARS-CoV-2 Infection and its Pathogenesis: A Systematic Review. Basic. Clin. Neurosci. 2021, 12, 569–586. [Google Scholar] [CrossRef] [PubMed]
- Vermeij, F.H.; Scholte op Reimer, W.J.; de Man, P.; van Oostenbrugge, R.J.; Franke, C.L.; de Jong, G.; de Kort, P.L.; Dippel, D.W.; Netherlands Stroke Survey, I. Stroke-associated infection is an independent risk factor for poor outcome after acute ischemic stroke: Data from the Netherlands Stroke Survey. Cerebrovasc. Dis. 2009, 27, 465–471. [Google Scholar] [CrossRef]
- Westendorp, W.F.; Nederkoorn, P.J.; Vermeij, J.D.; Dijkgraaf, M.G.; van de Beek, D. Post-stroke infection: A systematic review and meta-analysis. BMC Neurol. 2011, 11, 110. [Google Scholar] [CrossRef] [PubMed]
- Mélé, N.; Turc, G. Stroke Associated With Recent Mycoplasma pneumoniae Infection: A Systematic Review of Clinical Features and Presumed Pathophysiological Mechanisms. Front. Neurol. 2018, 9, 1109. [Google Scholar] [CrossRef]
- Haak, B.W.; Westendorp, W.F.; van Engelen, T.S.R.; Brands, X.; Brouwer, M.C.; Vermeij, J.D.; Hugenholtz, F.; Verhoeven, A.; Derks, R.J.; Giera, M.; et al. Disruptions of Anaerobic Gut Bacteria Are Associated with Stroke and Post-stroke Infection: A Prospective Case-Control Study. Transl. Stroke Res. 2021, 12, 581–592. [Google Scholar] [CrossRef]
- Westendorp, W.F.; Vermeij, J.D.; Zock, E.; Hooijenga, I.J.; Kruyt, N.D.; Bosboom, H.J.L.W.; Kwa, V.I.; Weisfelt, M.; Remmers, M.J.M.; ten Houten, R.; et al. The Preventive Antibiotics in Stroke Study (PASS): A pragmatic randomised open-label masked endpoint clinical trial. Lancet 2015, 385, 1519–1526. [Google Scholar] [CrossRef] [PubMed]
- Kalra, L.; Irshad, S.; Hodsoll, J.; Simpson, M.; Gulliford, M.; Smithard, D.; Patel, A.; Rebollo-Mesa, I.; Investigators, S.-I. Prophylactic antibiotics after acute stroke for reducing pneumonia in patients with dysphagia (STROKE-INF): A prospective, cluster-randomised, open-label, masked endpoint, controlled clinical trial. Lancet 2015, 386, 1835–1844. [Google Scholar] [CrossRef]
- Vermeij, J.D.; Westendorp, W.F.; Dippel, D.W.J.; van de Beek, D.; Nederkoorn, P.J. Antibiotic therapy for preventing infections in people with acute stroke. Cochrane Database Syst. Rev. 2018, 1, CD008530. [Google Scholar] [CrossRef]
- Westendorp, W.F.; Vermeij, J.D.; Smith, C.J.; Kishore, A.K.; Hodsoll, J.; Kalra, L.; Meisel, A.; Chamorro, A.; Chang, J.J.; Rezaei, Y.; et al. Preventive antibiotic therapy in acute stroke patients: A systematic review and meta-analysis of individual patient data of randomized controlled trials. Eur. Stroke J. 2021, 6, 385–394. [Google Scholar] [CrossRef]
- Badve, M.S.; Zhou, Z.; Anderson, C.S.; Hackett, M.L. Effectiveness and Safety of Antibiotics for Preventing Pneumonia and Improving Outcome after Acute Stroke: Systematic Review and Meta-analysis. J. Stroke Cerebrovasc. Dis. 2018, 27, 3137–3147. [Google Scholar] [CrossRef]
- Badve, M.S.; Zhou, Z.; van de Beek, D.; Anderson, C.S.; Hackett, M.L. Frequency of post-stroke pneumonia: Systematic review and meta-analysis of observational studies. Int. J. Stroke 2019, 14, 125–136. [Google Scholar] [CrossRef]
- Sluis, W.M.; Westendorp, W.F.; van de Beek, D.; Nederkoorn, P.J.; van der Worp, H.B. Preventive ceftriaxone in patients at high risk of stroke-associated pneumonia. A post-hoc analysis of the PASS trial. PLoS ONE 2022, 17, e0279700. [Google Scholar] [CrossRef]
- Jackson, J.J.; Kropp, H. beta-Lactam antibiotic-induced release of free endotoxin: In vitro comparison of penicillin-binding protein (PBP) 2-specific imipenem and PBP 3-specific ceftazidime. J. Infect. Dis. 1992, 165, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Opal, S.M.; Horn, D.L.; Palardy, J.E.; Parejo, N.; Jhung, J.; Bhattacharjee, A.; Young, L.D. The in vivo significance of antibiotic-induced endotoxin release in experimental Gram-negative sepsis. J. Endotox Res. 1996, 3, 245–252. [Google Scholar] [CrossRef]
- van Langevelde, P.; Kwappenberg, K.M.; Groeneveld, P.H.; Mattie, H.; van Dissel, J.T. Antibiotic-induced lipopolysaccharide (LPS) release from Salmonella typhi: Delay between killing by ceftazidime and imipenem and release of LPS. Antimicrob. Agents Chemother. 1998, 42, 739–743. [Google Scholar] [CrossRef] [PubMed]
- Mickiewicz, K.M.; Kawai, Y.; Drage, L.; Gomes, M.C.; Davison, F.; Pickard, R.; Hall, J.; Mostowy, S.; Aldridge, P.D.; Errington, J. Possible role of L-form switching in recurrent urinary tract infection. Nat. Commun. 2019, 10, 4379. [Google Scholar] [CrossRef]
- Huang, H.K.; Wang, J.H.; Lei, W.Y.; Chen, C.L.; Chang, C.Y.; Liou, L.S. Helicobacter pylori infection is associated with an increased risk of Parkinson’s disease: A population-based retrospective cohort study. Park. Relat. Disord. 2018, 47, 26–31. [Google Scholar] [CrossRef]
- Dardiotis, E.; Tsouris, Z.; Mentis, A.A.; Siokas, V.; Michalopoulou, A.; Sokratous, M.; Dastamani, M.; Bogdanos, D.P.; Deretzi, G.; Kountouras, J. H. pylori and Parkinson’s disease: Meta-analyses including clinical severity. Clin. Neurol. Neurosurg. 2018, 175, 16–24. [Google Scholar] [CrossRef]
- Meng, L.; Shen, L.; Ji, H.F. Impact of infection on risk of Parkinson’s disease: A quantitative assessment of case-control and cohort studies. J. Neurovirol. 2019, 25, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, X.; Tan, C.; Zhou, W.; Jiang, J.; Peng, W.; Zhou, X.; Mo, L.; Chen, L. Bacterial, viral, and fungal infection-related risk of Parkinson’s disease: Meta-analysis of cohort and case-control studies. Brain Behav. 2020, 10, e01549. [Google Scholar] [CrossRef]
- Smeyne, R.J.; Noyce, A.J.; Byrne, M.; Savica, R.; Marras, C. Infection and Risk of Parkinson’s Disease. J. Park. Dis. 2021, 11, 31–43. [Google Scholar] [CrossRef]
- Mikkelsen, L.F.; Nordestgaard, B.G.; Schnohr, P.; Ellervik, C. Increased Ferritin Concentration and Risk of Atrial Fibrillation and Heart Failure in Men and Women: Three Studies of the Danish General Population Including 35,799 Individuals. Clin. Chem. 2019, 65, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Altieri, C.; Pisano, C.; Vincenzo, L.; Ferrante, M.S.; Pellerito, V.; Nardi, P.; Bassano, C.; Buioni, D.; Greco, E.; Ruvolo, G.; et al. Circulating Levels of Ferritin, RDW, PTLs as Predictive Biomarkers of Postoperative Atrial Fibrillation Risk after Cardiac Surgery in Extracorporeal Circulation. Int. J. Mol. Sci. 2022, 23, 14800. [Google Scholar] [CrossRef] [PubMed]
- Farrell, D.H. gamma’ Fibrinogen as a novel marker of thrombotic disease. Clin. Chem. Lab. Med. 2012, 50, 1903–1909. [Google Scholar] [CrossRef] [PubMed]
- Luyendyk, J.P.; Schoenecker, J.G.; Flick, M.J. The multifaceted role of fibrinogen in tissue injury and inflammation. Blood 2019, 133, 511–520. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Lowe, G.D.; Rumley, A.; Dunn, F.G. Increased markers of thrombogenesis in chronic atrial fibrillation: Effects of warfarin treatment. Br. Heart J. 1995, 73, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.H.; Lowe, G.D.; Rumley, A.; Dunn, F.G. Fibrinogen and fibrin D-dimer levels in paroxysmal atrial fibrillation: Evidence for intermediate elevated levels of intravascular thrombogenesis. Am. Heart J. 1996, 131, 724–730. [Google Scholar] [CrossRef]
- Li-Saw-Hee, F.L.; Blann, A.D.; Gurney, D.; Lip, G.Y. Plasma von Willebrand factor, fibrinogen and soluble P-selectin levels in paroxysmal, persistent and permanent atrial fibrillation. Effects of cardioversion and return of left atrial function. Eur. Heart J. 2001, 22, 1741–1747. [Google Scholar] [CrossRef]
- Di Lecce, V.N.; Loffredo, L.; Fimognari, F.L.; Cangemi, R.; Violi, F. Fibrinogen as predictor of ischemic stroke in patients with non-valvular atrial fibrillation. J. Thromb. Haemost. 2003, 1, 2453–2455. [Google Scholar] [CrossRef] [PubMed]
- Mukamal, K.J.; Tolstrup, J.S.; Friberg, J.; Gronbaek, M.; Jensen, G. Fibrinogen and albumin levels and risk of atrial fibrillation in men and women (the Copenhagen City Heart Study). Am. J. Cardiol. 2006, 98, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Weymann, A.; Sabashnikov, A.; Ali-Hasan-Al-Saegh, S.; Popov, A.F.; Jalil Mirhosseini, S.; Baker, W.L.; Lotfaliani, M.; Liu, T.; Dehghan, H.; Yavuz, S.; et al. Predictive Role of Coagulation, Fibrinolytic, and Endothelial Markers in Patients with Atrial Fibrillation, Stroke, and Thromboembolism: A Meta-Analysis, Meta-Regression, and Systematic Review. Med. Sci. Monit. Basic. Res. 2017, 23, 97–140. [Google Scholar] [PubMed]
- Semczuk-Kaczmarek, K.; Platek, A.E.; Rys, A.; Adamowicz, J.; Legosz, P.; Kotkowski, M.; Dudzik-Plocica, A.; Gorko, D.; Szymanski, F.M.; Filipiak, K.J. CHA2DS2-VASc score and fibrinogen concentration in patients with atrial fibrillation. Adv. Clin. Exp. Med. 2019, 28, 1451–1457. [Google Scholar] [CrossRef]
- Rafaqat, S.; Afzal, S.; Khurshid, H.; Safdar, S.; Rafaqat, S.; Rafaqat, S. The Role of Major Inflammatory Biomarkers in the Pathogenesis of Atrial Fibrillation. J. Innov. Card. Rhythm. Manag. 2022, 13, 5265–5277. [Google Scholar] [CrossRef] [PubMed]
- Bao, J.; Gao, Z.; Hu, Y.; Liu, W.; Ye, L.; Wang, L. Serum fibrinogen-to-albumin ratio predicts new-onset atrial fibrillation risk during hospitalization in patients with acute myocardial infarction after percutaneous coronary intervention: A retrospective study. BMC Cardiovasc. Disord. 2023, 23, 432. [Google Scholar] [CrossRef] [PubMed]
- Tilly, M.J.; Geurts, S.; Pezzullo, A.M.; Bramer, W.M.; de Groot, N.M.S.; Kavousi, M.; de Maat, M.P.M. The association of coagulation and atrial fibrillation: A systematic review and meta-analysis. Europace 2023, 25, 28–39. [Google Scholar] [CrossRef] [PubMed]
- Drabik, L.; Wolkow, P.; Undas, A. Fibrin Clot Permeability as a Predictor of Stroke and Bleeding in Anticoagulated Patients with Atrial Fibrillation. Stroke 2017, 48, 2716–2722. [Google Scholar] [CrossRef] [PubMed]
- Drabik, L.; Konieczynska, M.; Undas, A. Clot Lysis Time Predicts Stroke during Anticoagulant Therapy in Patients with Atrial Fibrillation. Can. J. Cardiol. 2020, 36, 119–126. [Google Scholar] [CrossRef]
- Paquissi, F.C. The Predictive Role of Inflammatory Biomarkers in Atrial Fibrillation as Seen through Neutrophil-Lymphocyte Ratio Mirror. J. Biomark. 2016, 2016, 8160393. [Google Scholar] [CrossRef]
- Korantzopoulos, P.; Letsas, K.P.; Tse, G.; Fragakis, N.; Goudis, C.A.; Liu, T. Inflammation and atrial fibrillation: A comprehensive review. J. Arrhythm. 2018, 34, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Marín, F.; Roldan, V.; Monmeneu, J.V.; Bodí, V.; Fernández, C.; Garía de Burgos, F.; Marco, P.; Sogorb, F. Prothrombotic state and elevated levels of plasminogen activator inhibitor-1 in mitral stenosis with and without atrial fibrillation. Am. J. Cardiol. 1999, 84, 862–864. [Google Scholar] [CrossRef]
- Pretorius, M.; Donahue, B.S.; Yu, C.; Greelish, J.P.; Roden, D.M.; Brown, N.J. Plasminogen activator inhibitor-1 as a predictor of postoperative atrial fibrillation after cardiopulmonary bypass. Circulation 2007, 116, I1–I7. [Google Scholar] [CrossRef]
- Li, Q.; Lai, Y.; Gao, X.; Li, X.; Deng, C.Y.; Guo, H.; Zhao, J.; Yang, H.; Xu, Y.; Wu, S.; et al. Involvement of plasminogen activator inhibitor-1 and its related molecules in atrial fibrosis in patients with atrial fibrillation. PeerJ 2021, 9, e11488. [Google Scholar] [CrossRef]
- Yamauchi, K.; Furui, H.; Taniguchi, N.; Sotobata, I. Plasma beta-thromboglobulin and platelet factor 4 concentrations in patients with atrial fibrillation. Jpn. Heart J. 1986, 27, 481–487. [Google Scholar] [CrossRef]
- Sohara, H.; Amitani, S.; Kurose, M.; Miyahara, K. Atrial fibrillation activates platelets and coagulation in a time-dependent manner: A study in patients with paroxysmal atrial fibrillation. J. Am. Coll. Cardiol. 1997, 29, 106–112. [Google Scholar] [CrossRef]
- Drabik, L.; Wolkow, P.; Undas, A. Denser plasma clot formation and impaired fibrinolysis in paroxysmal and persistent atrial fibrillation while on sinus rhythm: Association with thrombin generation, endothelial injury and platelet activation. Thromb. Res. 2015, 136, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.H.; Lip, P.L.; Zarifis, J.; Watson, R.D.S.; Bareford, D.; Lowe, G.D.O.; Beevers, D.G. Fibrin D-dimer and beta-thromboglobulin as markers of thrombogenesis and platelet activation in atrial fibrillation. Effects of introducing ultra-low-dose warfarin and aspirin. Circulation 1996, 94, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Kamath, S.; Blann, A.D.; Chin, B.S.; Lanza, F.; Aleil, B.; Cazenave, J.P.; Lip, G.Y.H. A study of platelet activation in atrial fibrillation and the effects of antithrombotic therapy. Eur. Heart J. 2002, 23, 1788–1795. [Google Scholar] [CrossRef]
- Kaura, A.; Arnold, A.D.; Panoulas, V.; Glampson, B.; Davies, J.; Mulla, A.; Woods, K.; Omigie, J.; Shah, A.D.; Channon, K.M.; et al. Prognostic significance of troponin level in 3121 patients presenting with atrial fibrillation (The NIHR Health Informatics Collaborative TROP-AF study). J. Am. Heart Assoc. 2020, 9, e013684. [Google Scholar] [CrossRef]
- Costabel, J.P.; Burgos, L.M.; Trivi, M. The Significance of Troponin Elevation in Atrial Fibrillation. J. Atr. Fibrillation 2017, 9, 1530. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Guo, S.D.; Liu, Y.; Ma, C.S.; Lip, G.Y.H. Relationship of troponin to incident atrial fibrillation occurrence, recurrence after radiofrequency ablation and prognosis: A systematic review, meta-analysis and meta-regression. Biomarkers 2018, 23, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Sepehri Shamloo, A.; Arya, A.; Darma, A.; Nedios, S.; Doring, M.; Bollmann, A.; Dagres, N.; Hindricks, G. Atrial fibrillation: Is there a role for cardiac troponin? Diagnosis 2021, 8, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Lucrecia Maria, B.; Marcelo, T.; Andreina, G.R.; Juan Pablo, C. Prognostic Value of Troponin in Patients with Atrial Fibrillation Admitted to an Emergency Department: Review and Meta-Analysis. J. Atr. Fibrillation 2020, 13, 2346. [Google Scholar] [CrossRef] [PubMed]
- Cortés, M.; Arbucci, R.; Lambardi, F.; Furmento, J.; Muñoz, F.; Viruel, M.; Alexander, B.; Baranchuk, A.; Costabel, J.P. High-Sensitivity Troponin T for The Risk Assessment of Patients with Acute Atrial Fibrillation. Curr. Probl. Cardiol. 2022, 47, 101079. [Google Scholar] [CrossRef] [PubMed]
- Grobler, C.; Maphumulo, S.C.; Grobbelaar, L.M.; Bredenkamp, J.; Laubscher, J.; Lourens, P.J.; Steenkamp, J.; Kell, D.B.; Pretorius, E. COVID-19: The Rollercoaster of Fibrin(ogen), D-dimer, von Willebrand Factor, P-selectin and Their Interactions with Endothelial Cells, Platelets and Erythrocytes. Int. J. Mol. Sci. 2020, 21, 5168. [Google Scholar] [CrossRef] [PubMed]
- Freestone, B.; Gustafsson, F.; Chong, A.Y.; Corell, P.; Kistorp, C.; Hildebrandt, P.; Lip, G.Y.H. Influence of atrial fibrillation on plasma von willebrand factor, soluble E-selectin, and N-terminal pro B-type natriuretic peptide levels in systolic heart failure. Chest 2008, 133, 1203–1208. [Google Scholar] [CrossRef]
- Zhong, C.; Xin, M.; He, L.; Sun, G.; Shen, F. Prognostic value of von Willebrand factor in patients with atrial fibrillation: A meta-analysis. Medicine 2018, 97, e11269. [Google Scholar] [CrossRef]
- Marín, F.; Roldan, V.; Lip, G.Y.H. Fibrinolytic function and atrial fibrillation. Thromb. Res. 2003, 109, 233–240. [Google Scholar] [CrossRef]
- Danese, E.; Montagnana, M.; Cervellin, G.; Lippi, G. Hypercoagulability, D-dimer and atrial fibrillation: An overview of biological and clinical evidence. Ann. Med. 2014, 46, 364–371. [Google Scholar] [CrossRef]
- Ding, W.Y.; Gupta, D.; Lip, G.Y.H. Atrial fibrillation and the prothrombotic state: Revisiting Virchow’s triad in 2020. Heart 2020, 106, 1463–1468. [Google Scholar] [CrossRef] [PubMed]
- Ding, W.Y.; Protty, M.B.; Davies, I.G.; Lip, G.Y.H. Relationship between lipoproteins, thrombosis, and atrial fibrillation. Cardiovasc. Res. 2022, 118, 716–731. [Google Scholar] [CrossRef]
- Bagot, C.N.; Arya, R. Virchow and his triad: A question of attribution. Br. J. Haematol. 2008, 143, 180–190. [Google Scholar] [CrossRef] [PubMed]
- Watson, T.; Shantsila, E.; Lip, G.Y.H. Mechanisms of thrombogenesis in atrial fibrillation: Virchow’s triad revisited. Lancet 2009, 373, 155–166. [Google Scholar] [CrossRef]
- Darlington, A.; McCauley, M.D. Atrial Cardiomyopathy: An Unexplored Limb of Virchow’s Triad for AF Stroke Prophylaxis. Front. Cardiovasc. Med. 2020, 7, 11. [Google Scholar] [CrossRef]
- Yamashita, T. Virchow triad and beyond in atrial fibrillation. Heart Rhythm. 2016, 13, 2377–2378. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Saadat, V.; Co, M.L.; Contractor, T.; Mandapati, R.; Parwani, P. Permanent left atrial thrombi after multiple atrial fibrillation ablations: Acquired Virchow’s triad? HeartRhythm Case Rep. 2022, 8, 715–718. [Google Scholar] [CrossRef]
- Arvanitis, P.; Johansson, A.K.; Frick, M.; Malmborg, H.; Gerovasileiou, S.; Larsson, E.M.; Blomström-Lundqvist, C. Recent-onset atrial fibrillation: A study exploring the elements of Virchow’s triad after cardioversion. J. Interv. Card. Electrophysiol. 2022, 64, 49–58. [Google Scholar] [CrossRef]
- Freestone, B.; Lip, G.Y.H. The endothelium and atrial fibrillation. The prothrombotic state revisited. Hamostaseologie 2008, 28, 207–212. [Google Scholar] [CrossRef]
- Freestone, B.; Chong, A.Y.; Nuttall, S.; Lip, G.Y. Impaired flow mediated dilatation as evidence of endothelial dysfunction in chronic atrial fibrillation: Relationship to plasma von Willebrand factor and soluble E-selectin levels. Thromb. Res. 2008, 122, 85–90. [Google Scholar] [CrossRef]
- Chung, I.; Lip, G.Y.H. Virchow’s triad revisited: Blood constituents. Pathophysiol. Haemost. Thromb. 2003, 33, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Lip, G.Y.H. The prothrombotic state in atrial fibrillation: Pathophysiological and management implications. Cardiovasc. Res. 2019, 115, 31–45. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Zimba, O.; Gasparyan, A.Y. Thrombosis in Coronavirus disease 2019 (COVID-19) through the prism of Virchow’s triad. Clin. Rheumatol. 2020, 39, 2529–2543. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Stergiopoulos, K.; Wang, L.; Chen, L.; Cao, J. COVID-19 Presenting as Major Thromboembolic Events: Virchow’s Triad Revisited and Clinical Considerations of Therapeutic Anticoagulation. Cureus 2020, 12, e10137. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Gonzalez, F.J.; Ziccardi, M.R.; McCauley, M.D. Virchow’s Triad and the Role of Thrombosis in COVID-Related Stroke. Front. Physiol. 2021, 12, 769254. [Google Scholar] [CrossRef] [PubMed]
- Carbillon, L.; Fermaut, M.; Benbara, A.; Boujenah, J. COVID-19, Virchow’s triad and thromboembolic risk in obese pregnant women. Clin. Cardiol. 2021, 44, 593–594. [Google Scholar] [CrossRef] [PubMed]
- Mehta, J.L.; Calcaterra, G.; Bassareo, P.P. COVID-19, thromboembolic risk, and Virchow’s triad: Lesson from the past. Clin. Cardiol. 2020, 43, 1362–1367. [Google Scholar] [CrossRef] [PubMed]
- Flaumenhaft, R.; Enjyoji, K.; Schmaier, A.A. Vasculopathy in COVID-19. Blood 2022, 140, 222–235. [Google Scholar] [CrossRef]
- Conway, E.M.; Mackman, N.; Warren, R.Q.; Wolberg, A.S.; Mosnier, L.O.; Campbell, R.A.; Gralinski, L.E.; Rondina, M.T.; van de Veerdonk, F.L.; Hoffmeister, K.M.; et al. Understanding COVID-19-associated coagulopathy. Nat. Rev. Immunol. 2022, 22, 639–649. [Google Scholar] [CrossRef]
- Wadowski, P.P.; Panzer, B.; Jozkowicz, A.; Kopp, C.W.; Gremmel, T.; Panzer, S.; Koppensteiner, R. Microvascular Thrombosis as a Critical Factor in Severe COVID-19. Int. J. Mol. Sci. 2023, 24, 2492. [Google Scholar] [CrossRef]
- Invernizzi, A.; Schiuma, M.; Parrulli, S.; Torre, A.; Zicarelli, F.; Colombo, V.; Marini, S.; Villella, E.; Bertoni, A.; Antinori, S.; et al. Retinal vessels modifications in acute and post-COVID-19. Sci. Rep. 2021, 11, 19373. [Google Scholar] [CrossRef] [PubMed]
- Jing, H.; Wu, X.; Xiang, M.; Liu, L.; Novakovic, V.A.; Shi, J. Pathophysiological mechanisms of thrombosis in acute and long COVID-19. Front. Immunol. 2022, 13, 992384. [Google Scholar] [CrossRef] [PubMed]
- Zanini, G.; Selleri, V.; Roncati, L.; Coppi, F.; Nasi, M.; Farinetti, A.; Manenti, A.; Pinti, M.; Mattioli, A.V. Vascular “Long COVID”: A New Vessel Disease? Angiology 2024, 75, 8–14. [Google Scholar] [CrossRef]
- Writing Committee Members; Joglar, J.A.; Chung, M.K.; Armbruster, A.L.; Benjamin, E.J.; Chyou, J.Y.; Cronin, E.M.; Deswal, A.; Eckhardt, L.L.; Goldberger, Z.D.; et al. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2024, 83, 109–279. [Google Scholar] [CrossRef]
- Chao, T.F.; Joung, B.; Takahashi, Y.; Lim, T.W.; Choi, E.K.; Chan, Y.H.; Guo, Y.; Sriratanasathavorn, C.; Oh, S.; Okumura, K.; et al. 2021 Focused Update Consensus Guidelines of the Asia Pacific Heart Rhythm Society on Stroke Prevention in Atrial Fibrillation: Executive Summary. Thromb. Haemost. 2022, 122, 20–47. [Google Scholar] [CrossRef]
- Chi, E.Y.; Frey, S.L.; Winans, A.; Lam, K.L.; Kjaer, K.; Majewski, J.; Lee, K.Y. Amyloid-beta fibrillogenesis seeded by interface-induced peptide misfolding and self-assembly. Biophys. J. 2010, 98, 2299–2308. [Google Scholar] [CrossRef]
- Michaels, T.C.T.; Liu, L.X.; Meisl, G.; Knowles, T.P.J. Physical principles of filamentous protein self-assembly kinetics. J. Phys. Condens. Matter 2017, 29, 153002. [Google Scholar] [CrossRef] [PubMed]
- Michaels, T.C.T.; Qian, D.; Šarić, A.; Vendruscolo, M.; Linse, S.; Knowles, T.P.J. Amyloid formation as a protein phase transition. Nat. Rev. Phys. 2023, 5, 379–397. [Google Scholar] [CrossRef]
- Seuma, M.; Faure, A.J.; Badia, M.; Lehner, B.; Bolognesi, B. The genetic landscape for amyloid beta fibril nucleation accurately discriminates familial Alzheimer’s disease mutations. eLife 2021, 10, e63364. [Google Scholar] [CrossRef]
- Seuma, M.; Lehner, B.; Bolognesi, B. An atlas of amyloid aggregation: The impact of substitutions, insertions, deletions and truncations on amyloid beta fibril nucleation. Nat. Commun. 2022, 13, 7084. [Google Scholar] [CrossRef]
- De, S.; Klenerman, D. Imaging individual protein aggregates to follow aggregation and determine the role of aggregates in neurodegenerative disease. Biochim. Biophys. Acta Proteins Proteom. 2019, 1867, 870–878. [Google Scholar] [CrossRef] [PubMed]
- Camino, J.D.; Gracia, P.; Cremades, N. The role of water in the primary nucleation of protein amyloid aggregation. Biophys. Chem. 2021, 269, 106520. [Google Scholar] [CrossRef] [PubMed]
- Cawood, E.E.; Karamanos, T.K.; Wilson, A.J.; Radford, S.E. Visualizing and trapping transient oligomers in amyloid assembly pathways. Biophys. Chem. 2021, 268, 106505. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.G.; Meisl, G.; Horrocks, M.H.; Zetterberg, H.; Knowles, T.P.J.; Klenerman, D. Extrinsic Amyloid-Binding Dyes for Detection of Individual Protein Aggregates in Solution. Anal. Chem. 2018, 90, 10385–10393. [Google Scholar] [CrossRef] [PubMed]
- Pepe, S.; Delbridge, L.M. Pacemaker cell and atrial function: Unravelling how calcium initiates and regulates the heart beat and how ionic dysfunction, ‘channelopathies’ and other membrane remodelling contribute to atrial fibrillation. Heart Lung Circ. 2007, 16, 331–334. [Google Scholar] [CrossRef] [PubMed]
- Thejus, J.; Francis, J. Atrial fibrillation in cardiac channelopathies. Indian Pacing Electrophysiol. J. 2009, 9, 342–350. [Google Scholar] [PubMed]
- Enriquez, A.; Antzelevitch, C.; Bismah, V.; Baranchuk, A. Atrial fibrillation in inherited cardiac channelopathies: From mechanisms to management. Heart Rhythm. 2016, 13, 1878–1884. [Google Scholar] [CrossRef]
- El-Battrawy, I.; Lang, S.; Zhou, X.; Borggrefe, M.; Akin, I. The link between atrial fibrillation and hereditary channelopathies. Europace 2018, 20, 1872. [Google Scholar] [CrossRef] [PubMed]
- Al-Azaam, B.; Darbar, D. Atrial Fibrillation in Inherited Channelopathies. Card. Electrophysiol. Clin. 2021, 13, 155–163. [Google Scholar] [CrossRef]
- Laubscher, G.J.; Khan, M.A.; Venter, C.; Pretorius, J.H.; Kell, D.B.; Pretorius, E. Treatment of Long COVID Symptoms with Triple Anticoagulant Therapy. 2023. Available online: https://www.researchsquare.com/article/rs-2697680/v2697681 (accessed on 1 March 2024).
- Kell, D.B.; Oliver, S.G. Here is the evidence, now what is the hypothesis? The complementary roles of inductive and hypothesis-driven science in the post-genomic era. Bioessays 2004, 26, 99–105. [Google Scholar] [CrossRef]
- Sekelj, S.; Sandler, B.; Johnston, E.; Pollock, K.G.; Hill, N.R.; Gordon, J.; Tsang, C.; Khan, S.; Ng, F.S.; Farooqui, U. Detecting undiagnosed atrial fibrillation in UK primary care: Validation of a machine learning prediction algorithm in a retrospective cohort study. Eur. J. Prev. Cardiol. 2021, 28, 598–605. [Google Scholar] [CrossRef]
- Tseng, A.S.; Noseworthy, P.A. Prediction of Atrial Fibrillation Using Machine Learning: A Review. Front. Physiol. 2021, 12, 752317. [Google Scholar] [CrossRef]
- Siontis, K.C.; Yao, X.; Pirruccello, J.P.; Philippakis, A.A.; Noseworthy, P.A. How Will Machine Learning Inform the Clinical Care of Atrial Fibrillation? Circ. Res. 2020, 127, 155–169. [Google Scholar] [CrossRef]
- Rizwan, A.; Zoha, A.; Mabrouk, I.B.; Sabbour, H.M.; Al-Sumaiti, A.S.; Alomainy, A.; Imran, M.A.; Abbasi, Q.H. A Review on the State of the Art in Atrial Fibrillation Detection Enabled by Machine Learning. IEEE Rev. Biomed. Eng. 2021, 14, 219–239. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Genaidy, A.; Tran, G.; Marroquin, P.; Estes, C. Incident atrial fibrillation and its risk prediction in patients developing COVID-19: A machine learning based algorithm approach. Eur. J. Intern. Med. 2021, 91, 53–58. [Google Scholar] [CrossRef]
- Pollock, K.G.; Sekelj, S.; Johnston, E.; Sandler, B.; Hill, N.R.; Ng, F.S.; Khan, S.; Nassar, A.; Farooqui, U. Application of a machine learning algorithm for detection of atrial fibrillation in secondary care. Int. J. Cardiol. Heart Vasc. 2020, 31, 100674. [Google Scholar] [CrossRef]
- Szymanski, T.; Ashton, R.; Sekelj, S.; Petrungaro, B.; Pollock, K.G.; Sandler, B.; Lister, S.; Hill, N.R.; Farooqui, U. Budget impact analysis of a machine learning algorithm to predict high risk of atrial fibrillation among primary care patients. Europace 2022, 24, 1240–1247. [Google Scholar] [CrossRef]
- Grant, P.J. Diabetes mellitus as a prothrombotic condition. J. Intern. Med. 2007, 262, 157–172. [Google Scholar] [CrossRef]
- Konieczynska, M.; Fil, K.; Bazanek, M.; Undas, A. Prolonged duration of type 2 diabetes is associated with increased thrombin generation, prothrombotic fibrin clot phenotype and impaired fibrinolysis. Thromb. Haemost. 2014, 111, 685–693. [Google Scholar] [CrossRef]
- Karaban, K.; Slupik, D.; Reda, A.; Gajewska, M.; Rolek, B.; Borovac, J.A.; Papakonstantinou, P.E.; Bongiovanni, D.; Ehrlinder, H.; Parker, W.A.E.; et al. Coagulation Disorders and Thrombotic Complications in Heart Failure with Preserved Ejection Fraction. Curr. Probl. Cardiol. 2024, 49, 102127. [Google Scholar] [CrossRef]
- Antoniak, S.; Boltzen, U.; Riad, A.; Kallwellis-Opara, A.; Rohde, M.; Dorner, A.; Tschope, C.; Noutsias, M.; Pauschinger, M.; Schultheiss, H.P.; et al. Viral myocarditis and coagulopathy: Increased tissue factor expression and plasma thrombogenicity. J. Mol. Cell. Cardiol. 2008, 45, 118–126. [Google Scholar] [CrossRef]
- Bennett, P.C.; Silverman, S.H.; Gill, P.S.; Lip, G.Y.H. Peripheral arterial disease and Virchow’s triad. Thromb. Haemost. 2009, 101, 1032–1040. [Google Scholar] [CrossRef]
- Staff, A.C.; Redman, C.W.; Williams, D.; Leeson, P.; Moe, K.; Thilaganathan, B.; Magnus, P.; Steegers, E.A.; Tsigas, E.Z.; Ness, R.B.; et al. Pregnancy and Long-Term Maternal Cardiovascular Health: Progress through Harmonization of Research Cohorts and Biobanks. Hypertension 2016, 67, 251–260. [Google Scholar] [CrossRef]
- Roy, M.; Nath, A.K.; Pal, I.; Dey, S.G. Second Sphere Interactions in Amyloidogenic Diseases. Chem. Rev. 2022, 122, 12132–12206. [Google Scholar] [CrossRef]
- Martinez-Naharro, A.; Gonzalez-Lopez, E.; Corovic, A.; Mirelis, J.G.; Baksi, A.J.; Moon, J.C.; Garcia-Pavia, P.; Gillmore, J.D.; Hawkins, P.N.; Fontana, M. High Prevalence of Intracardiac Thrombi in Cardiac Amyloidosis. J. Am. Coll. Cardiol. 2019, 73, 1733–1734. [Google Scholar] [CrossRef]
- Martinez-Naharro, A.; Baksi, A.J.; Hawkins, P.N.; Fontana, M. Diagnostic imaging of cardiac amyloidosis. Nat. Rev. Cardiol. 2020, 17, 413–426. [Google Scholar] [CrossRef]
- Romiti, G.F.; Guo, Y.; Corica, B.; Proietti, M.; Zhang, H.; Lip, G.Y.H.; mAF-App II Trial Investigators. Mobile Health-Technology-Integrated Care for Atrial Fibrillation: A Win Ratio Analysis from the mAFA-II Randomized Clinical Trial. Thromb. Haemost. 2023, 123, 1042–1048. [Google Scholar] [CrossRef]
- Romiti, G.F.; Pastori, D.; Rivera-Caravaca, J.M.; Ding, W.Y.; Gue, Y.X.; Menichelli, D.; Gumprecht, J.; Koziel, M.; Yang, P.S.; Guo, Y.; et al. Adherence to the ‘Atrial Fibrillation Better Care’ Pathway in Patients with Atrial Fibrillation: Impact on Clinical Outcomes-A Systematic Review and Meta-Analysis of 285,000 Patients. Thromb. Haemost. 2022, 122, 406–414. [Google Scholar] [CrossRef]
- Shantsila, E.; Choi, E.K.; Lane, D.A.; Joung, B.; Lip, G.Y.H. Atrial fibrillation: Comorbidities, lifestyle, and patient factors. Lancet Reg. Health Eur. 2024, 37, 100784. [Google Scholar] [CrossRef]
- Schofield, J.; Abrams, S.T.; Jenkins, R.; Lane, S.; Wang, G.; Toh, C.H. Amyloid-fibrinogen aggregates (“microclots”) predict risks of Disseminated Intravascular Coagulation and mortality. Blood Adv. 2024, in press. [CrossRef]
- Dalton, C.F.; de Oliveira, M.I.R.; Stafford, P.; Peake, N.; Kane, B.; Higham, A.; Singh, D.; Jackson, N.; Davies, H.; Price, D.; et al. Increased fibrinaloid microclot counts in platelet-poor plasma are associated with Long COVID. medRxiv 2024. [Google Scholar] [CrossRef]
- Grixti, J.M.; Theron, C.W.; Salcedo-Sora, J.E.; Pretorius, E.; Kell, D.B. Automated microscopic measurement of fibrinaloid microclots and their degradation by nattokinase, the main natto protease. bioRxiv 2024. [Google Scholar] [CrossRef]
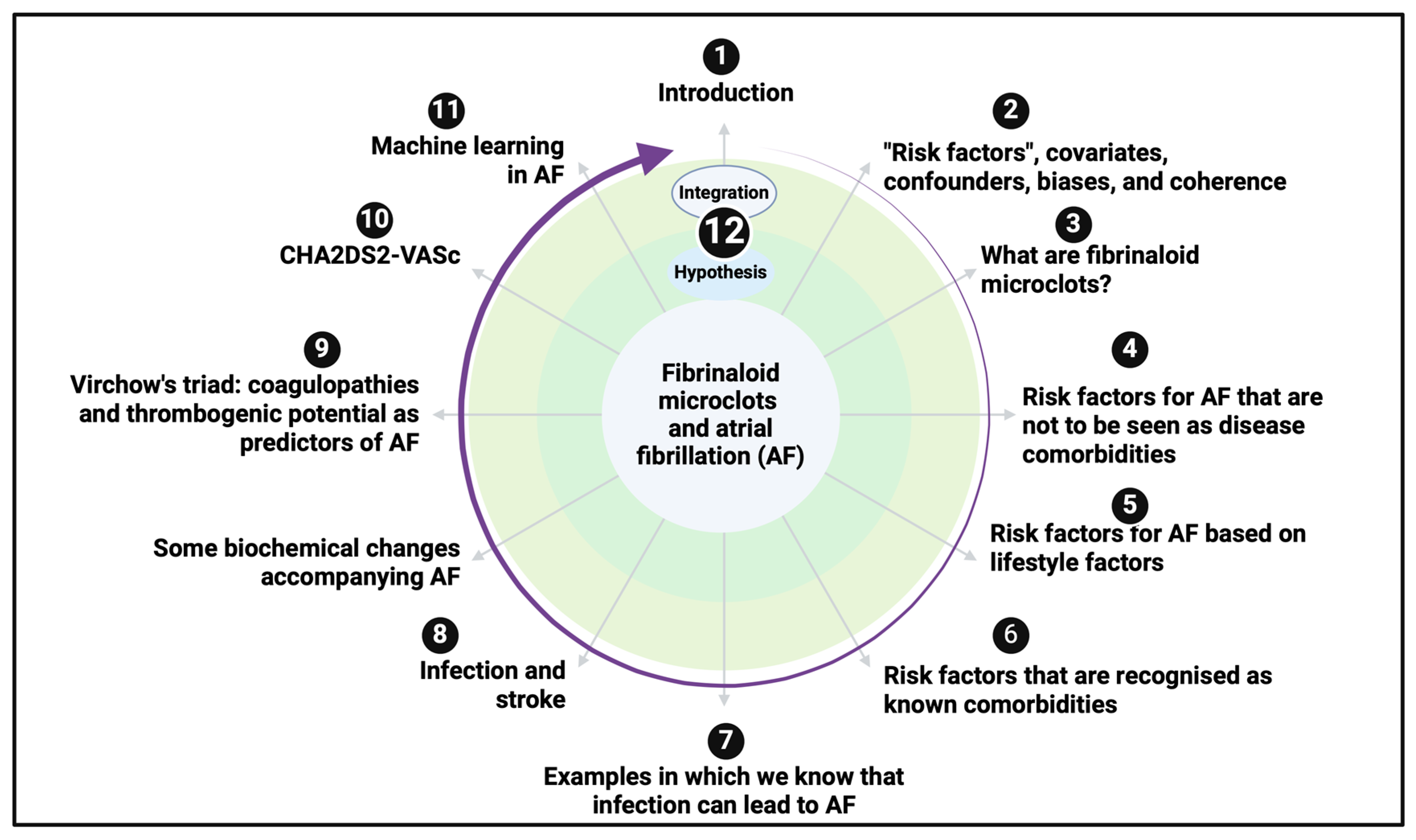




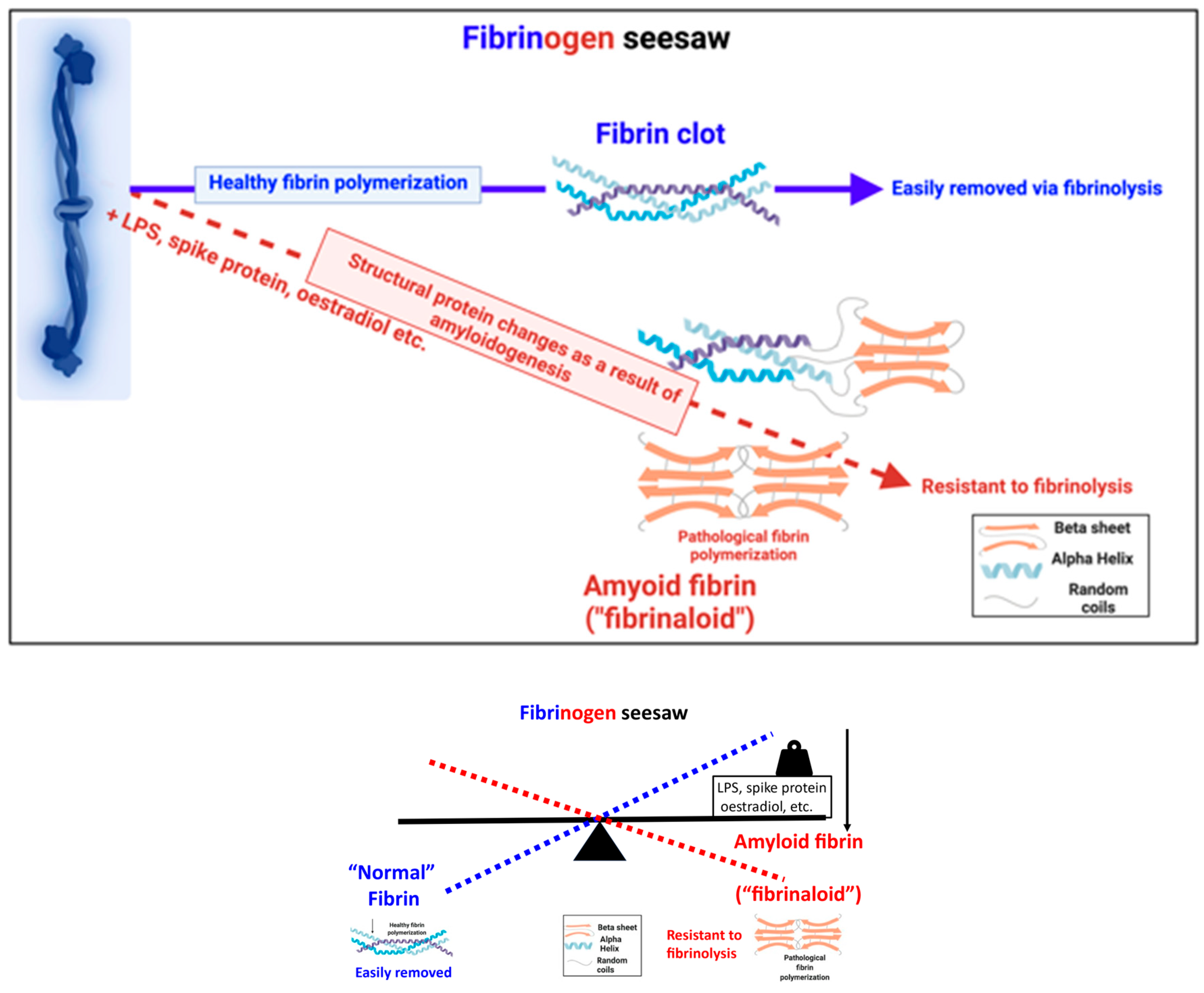

| Risk Factor | Comments | Selected References |
|---|---|---|
| Age | Normally a significant increase in AF with age. | [11,130,132,133] |
| In some cases the opposite can be true for athletes. | [134,135] | |
| May involve age-dependent Na+ channel expression. | [136] | |
| BMI | Obesity is sometimes a clear risk factor [4] (as for many metabolic diseases), but there are also (and more commonly) a variety of so-called ‘obesity paradoxes’, where the hazard ratios for acquiring or manifesting AF, and, in particular, suffering disease sequelae therefrom, are actually significantly greater for those with a lower BMI. | [137,138,139,140,141,142,143,144,145,146,147,148,149] |
| Obesity may induce sleep apnoea, which is a known risk factor for AF. | [78,150,151,152] | |
| Ethnicity | More prevalent among Caucasians; not entirely clear how much is genetics, culture/lifestyle, or GxE, and as with genetics, no studies really seek to deconvolve these factors. | [130] |
| Familial associations/Genetics | Mostly less significant than lifestyle factors and co-morbidities, apart from some particular and relatively uncommon ion channelopathies. | [153]; |
| Monozygotic/dizygotic ratio does predict a role for genetics, so not purely cultural associations. | [154,155] | |
| Highly polygenic, with genes involved in developmental, contractile, and electrophysiological functions. Necessarily convolved with GxE association that cannot be interpreted from GWAS studies alone. | [149,156,157] | |
| Gender | More prevalent in males, though outcomes can be worse for females (so being female contributes to the CHA2DS2-VASc score [158,159]). Less important than age for asymptomatic AF. | [130,160,161] |
| Risk Factor | Comments | Selected References |
|---|---|---|
| Alcohol consumption | Some increase in AF risk as a function of alcohol intake; greater in men; studies mainly not controlled for BMI. Not a huge effect for moderate levels of consumption. | [145,162,163] |
| Exercise | As with BMI, the relationship is nonlinear, with moderate exercise and general cardio-respiratory fitness being beneficial, but excess exercise (which could cause oxidative stress [164,165], inflammation [166,167], hypoxaemia [168], etc.) having negative effects. | [145,169,170] |
| Particulate matter exposure | New-onset AF can follow exposure to particulate matter. | [171,172,173,174] |
| This can be an acute occurrence | [175] | |
| Increases with known genetic risk factors. | ||
| Meta-analyses. | [176,177,178] | |
| Particulate matter is also amyloidogenic. | [179,180,181,182] | |
| Particulate matter can cause other cardiac problems. | [183] | |
| Psychosocial Stress | As estimated by surrogates reflecting anger and hostility, it can be a minor risk factor in men but not women, even after controlling for hypertension. | [145,184] |
| Smoking | Although important to other cardiovascular diseases, for AF seemingly a marginal risk, and probably dwarfed by other risks of smoking such as lung cancer. | [185] |
| Disease or Syndrome | Comments | References Regarding an Infectious Origin | References Illustrating Anomalous Clotting/Microclots |
|---|---|---|---|
| Alzheimer’s | Many references, not least from Ruth Itzhaki focusing on HSV, imply this strongly. Other organisms have also been implicated. | [190,191,192,193,194] | [39,42,100] |
| Diabetes, type 2 | Originally asked by Gundersen in 1927. Even greater evidence for type 1 [195], not covered here. | [196,197,198,199,200] | [39,95,113,115,116,201,202] |
| Many reviews (also those with T2D are more susceptible to infections; this direction is not discussed here). | [203,204,205] | ||
| Increased diabetes prevalence following COVID-19 infection. | [206] | ||
| Multiple sclerosis | Now recognised as being caused by Epstein–Barr virus. | [207,208,209] | Not yet studied |
| Myalgic encephalitis/chronic fatigue syndrome (ME/CFS) | Clear infectious origin, likely viral, and most likely a herpes virus. | [210] | [210,211] |
| Parkinson’s | Induction of disease progression by bacterial LPS and by viruses. | [212,213] | [39] |
| Reviews | [214,215] | ||
| Rheumatoid arthritis | Absolutely clear evidence for Proteus spp. as the infectious agent. | [216,217,218,219] | [128,220,221,222] |
| Sleep apnoea | Obstructive sleep apnoea is a strong risk factor or comorbidity of AF, also associated with obesity [5,78,152,223] and both acute [224] and long COVID [225]. | [226,227,228] | Not yet studied |
| Disease | Comments | Selected References |
|---|---|---|
| Alzheimer’s | AF is of course related to age, as is AD. Stroke is also related to vascular dementia. Strong comorbidities between cardiovascular disease and AD. | [229] [230] |
| Some indications that AF is associated with an exacerbation of the onset of AD and related dementias, but not causally. | [231,232,233,234,235,236] | |
| Diabetes, type 2 | Very strong association of AF with diabetic complications, and of diabetes increasing the risk of AF. | [237,238,239,240,241,242,243,244,245] |
| Parkinson’s | Some evidence of an association of AF with early PD, much less so if PD is diagnosed later (i.e., evidence either way is relatively weak). | [246,247,248,249] |
| Rheumatoid arthritis | Small, significant association, but confounded with use of small molecule drugs. Also associated with greater risk of cardiovascular disease. | [250] [251] [252,253] |
| Biochemical Marker | Comments | Selected References |
|---|---|---|
| Ferritin | Serum ferritin is a marker of cell death [188], whose accompanying release of free iron can cause microclots and may itself be induced by them or other traumas. It is significantly raised in AF. | [332,333] |
| Fibrinogen | Fibrinogen (including γ′ [334]) levels are commonly raised in inflammatory diseases [335]. Fibrinogen levels are higher in individuals with AF (and in those having a higher CHA2DS2-VASc score and likelihood of stroke), consistent with a role of microclots in the onset of AF. | [336,337,338,339,340,341,342,343,344,345] |
| Fibrin clot properties also relate to stroke likelihood/severity in AF, though no amyloid measurements have yet been made. | [346,347] | |
| Inflammation | Occurs (by definition) in all kinds of chronic, inflammatory disease [101], but is certainly associated with AF. An accompaniment to all syndromes involving microclots. | [343,348,349] |
| Plasminogen Activator Inhibitor-1 (PAI-1) | Significantly raised in AF, potentially reducing the rate at which fibrinaloid microclots might be removed. | [350,351,352] |
| Platelet Factor-4 and platelet activation | Platelet activation is another key feature of chronic, inflammatory diseases accompanied by microclots. | [353,354,355] |
| β-Thromboglobulin | Raised in AF. | [353,356,357] |
| Troponin (cardiac isoforms) | Probably more a metric of severity of cardiac events, but as a measure of cell death (like ferritin), it may have predictive value. | [358,359,360,361,362,363] |
| Von Willebrand Factor | It should be noted that it is unlikely to be a simple function, as too much or too little can be bad in terms of causing hyper- or hypo-coagulation, respectively [364]. | [341,365,366] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kell, D.B.; Lip, G.Y.H.; Pretorius, E. Fibrinaloid Microclots and Atrial Fibrillation. Biomedicines 2024, 12, 891. https://doi.org/10.3390/biomedicines12040891
Kell DB, Lip GYH, Pretorius E. Fibrinaloid Microclots and Atrial Fibrillation. Biomedicines. 2024; 12(4):891. https://doi.org/10.3390/biomedicines12040891
Chicago/Turabian StyleKell, Douglas B., Gregory Y. H. Lip, and Etheresia Pretorius. 2024. "Fibrinaloid Microclots and Atrial Fibrillation" Biomedicines 12, no. 4: 891. https://doi.org/10.3390/biomedicines12040891
APA StyleKell, D. B., Lip, G. Y. H., & Pretorius, E. (2024). Fibrinaloid Microclots and Atrial Fibrillation. Biomedicines, 12(4), 891. https://doi.org/10.3390/biomedicines12040891





