Improved Ultrasound-Guided Balloon-Assisted Maturation Angioplasty Using Drug-Eluting Balloons in the First Autogenous Arteriovenous Fistula Procedure: Early Experience
Abstract
1. Introduction
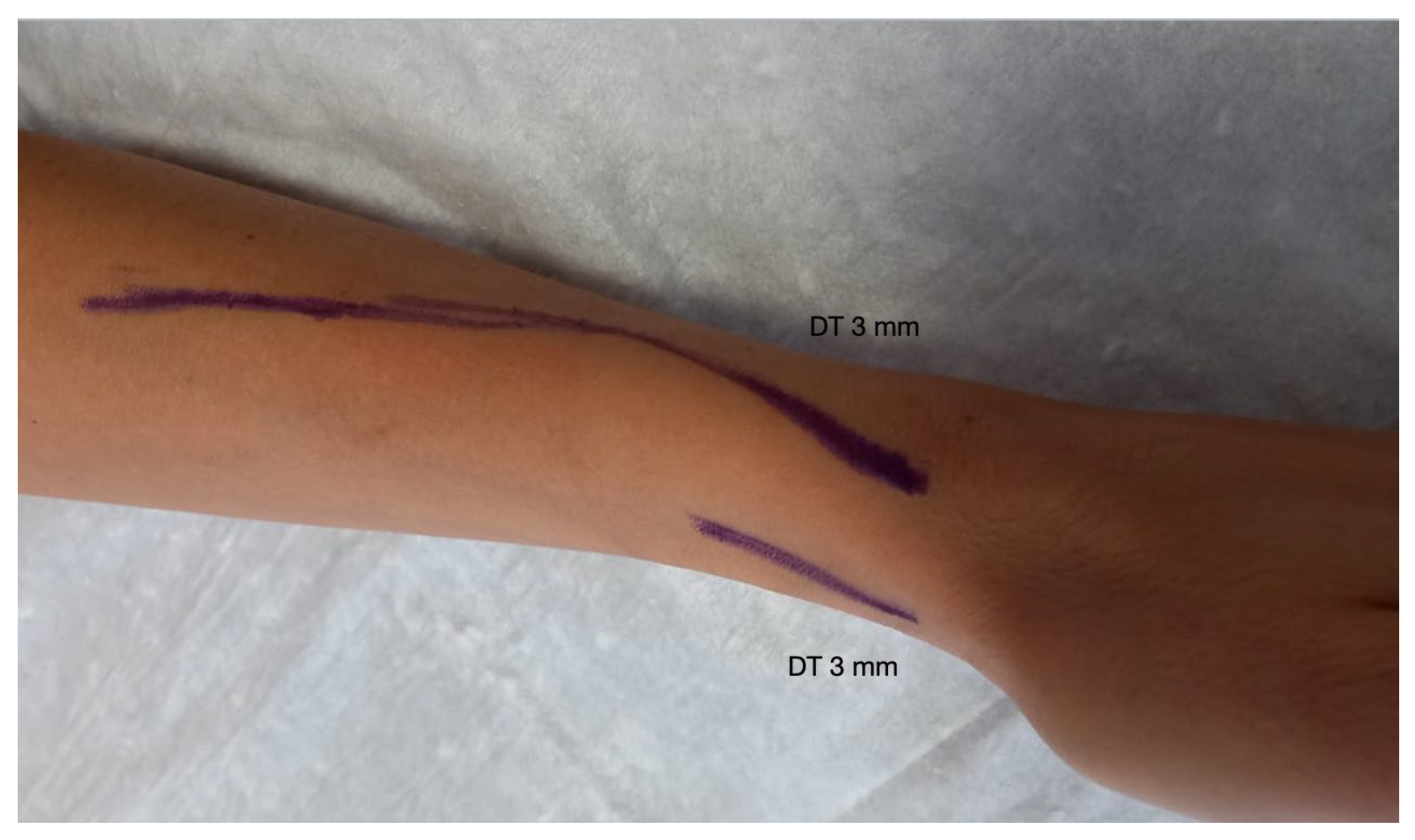
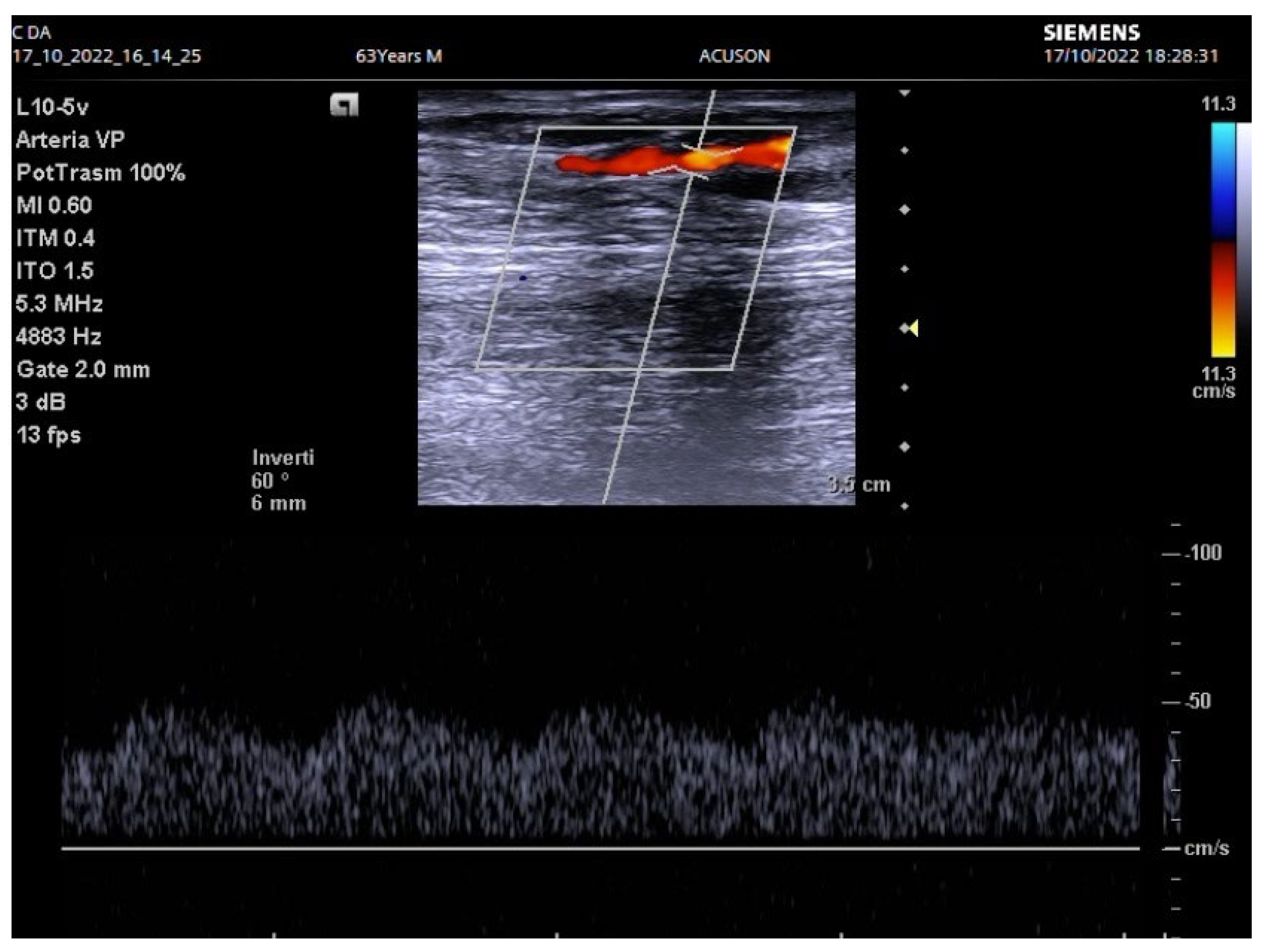
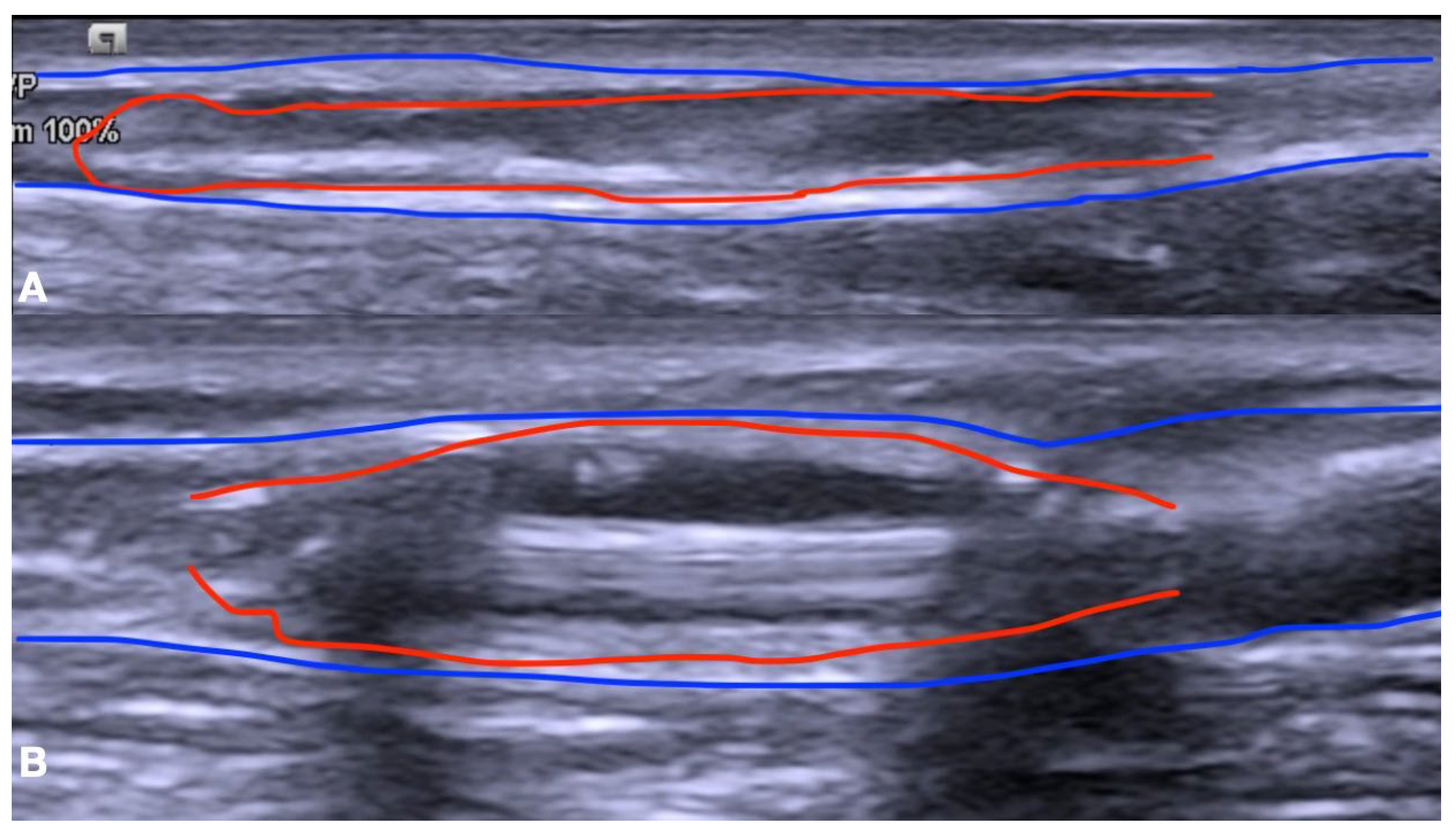
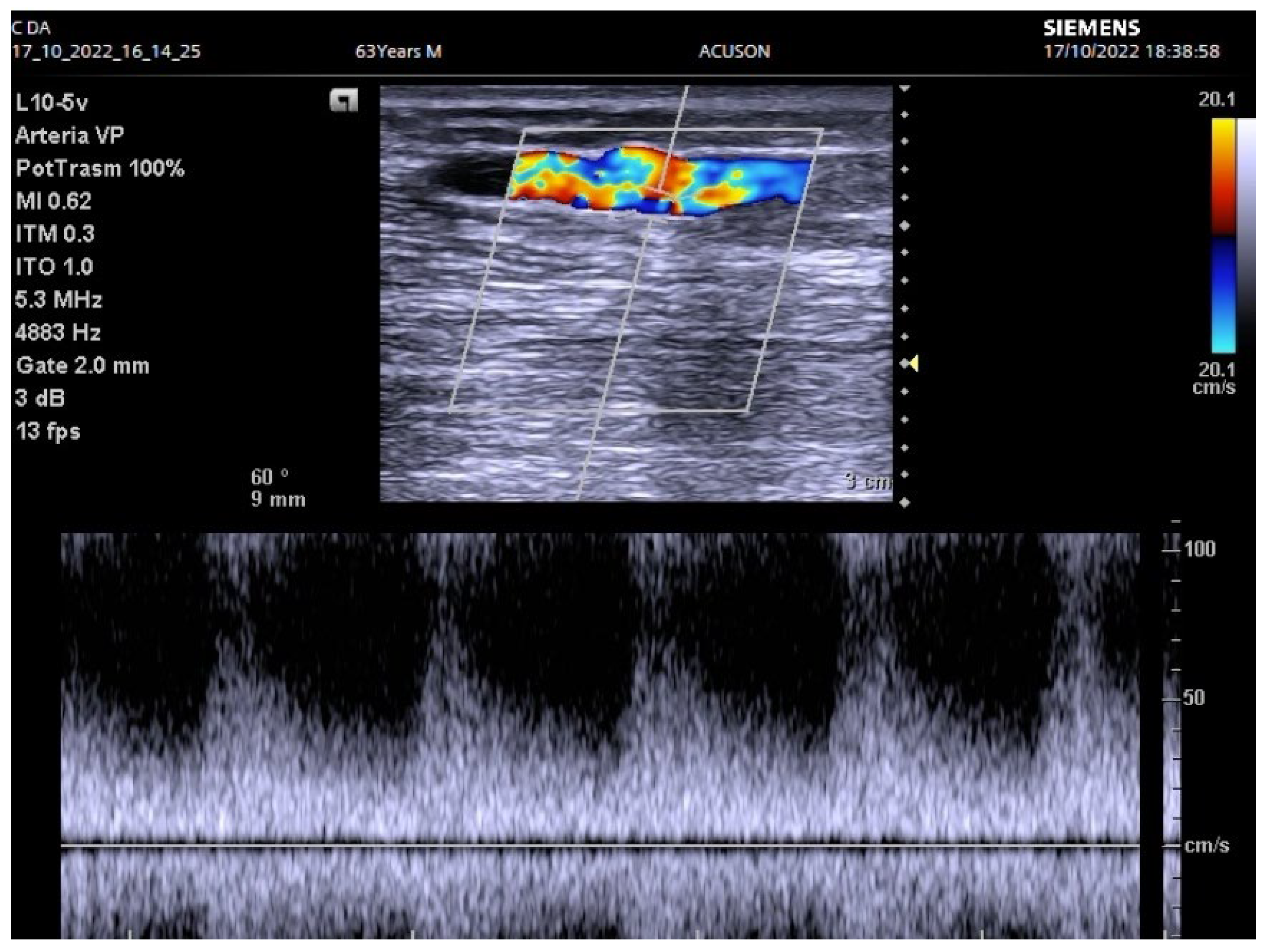
2. Materials and Methods
3. Results
4. Discussion
| References | N Patients Treated | PTA with DEB | % of Technical Success |
|---|---|---|---|
| Li et al. [10] | 148 | No | 78% |
| Lookstein et al. [35] | 330 | Yes (170) | 82% |
| No (160) | 59% | ||
| Wang et al. [41] | 254 | No | 100% |
| Voto et al. [42] | 662 | No | 100% |
| Irani et al. [44] | 119 | Yes (59) | 81% |
| No (60) | 61% | ||
| Huang et al. [48] | 290 | No | 94% |
| De Marco Garcia et al. [50] | 62 | No | 85% |
| Kao et al. [54] | 38 | No | 95% |
| Kohiyama et al. [55] | 205 | No | 100% |
| Kanchanasuttirak et al. [56] | 1427 | No | 97% |
| Kim et al. [57] | 92 | No | 90% |
| Elkassaby et al. [58] | 153 | No | 78% |
| Rizvi et al. [59] | 54 | No | 55% |
| Gallagher et al. [60] | 45 | No | 99% |
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sahasrabudhe, P.; Bindu, A. Nuances of Arteriovenous Fistula Creation for Vascular Access in Hemodialysis. Indian J. Plast. Surg. 2021, 54, 257–263. [Google Scholar] [CrossRef]
- Panagrosso, M.; Bracale, U.M.; Del Guercio, L.; Viscardi, A.; Peluso, A.; Dinoto, E. Case report of a large cephalic vein aneurysm inducing heart failure in a renal transplant patient with radio-cephalic fistula for haemodialysis. Int. J. Surg. Case Rep. 2020, 77, S162–S165. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dixon, B.S. Why don’t fistulas mature? Kidney Int. 2006, 70, 1413–1422. [Google Scholar] [CrossRef] [PubMed]
- Wolford, H.Y.; Hsu, J.; Rhodes, J.M.; Shortell, C.K.; Davies, M.G.; Bakhru, A.; Illig, K.A. Outcome after autogenous brachial-basilic upper arm transpositions in the post-National Kidney Foundation Dialysis Outcomes Quality Initiative era. J. Vasc. Surg. 2005, 42, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Falk, A. Maintenance and salvage of arteriovenous fistulas. J. Vasc. Interv. Radiol. 2006, 17, 807–813. [Google Scholar] [CrossRef] [PubMed]
- van Vliet, L.V.; Zonnebeld, N.; Tordoir, J.H.; Huberts, W.; Bouwman, L.H.; Cuypers, P.W.; Heinen, S.G.; Huisman, L.C.; Lemson, S.; Mees, B.M.; et al. Guideline recommendations on minimal blood vessel diameters and arteriovenous fistula outcomes. J. Vasc. Access 2023, 11297298231180627. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, G.; Talassi, E.; Baraldi, C.; Baruffaldi, M.; Tarchini, R.; Galli, F.; Arienzo, A.; Pacchioni, R. Un buon accesso vascolare permette un trattamento efficace [A good vascular access allows an effective treatment]. G. Ital. Nefrol. 2005, 22 (Suppl. S31), S60–S69. [Google Scholar] [PubMed]
- Dember, L.M.; Beck, G.J.; Allon, M.; Delmez, J.A.; Dixon, B.S.; Greenberg, A.; Himmelfarb, J.; Vazquez, M.A.; Gassman, J.J.; Greene, T.; et al. Effect of clopidogrel on early failure of arteriovenous fistulas for hemodialysis: A randomized controlled trial. JAMA 2008, 299, 2164–2171. [Google Scholar] [CrossRef] [PubMed]
- Kahraman, N.; Demir, D. Outcomes of arteriovenous fistula reconstruction in vascular access dysfunction. Am. J. Transl. Res. 2019, 11, 1058–1065. [Google Scholar] [PubMed] [PubMed Central]
- Li, Y.-S.; Li, Y.-C.; Yu, S.-Y.; Kao, T.-C.; Ko, P.-J.; Wei, W.-C.; Su, T.-W.; Wu, Y.-J. The clinical outcome of balloon-assisted maturation procedure between autogenous radiocephalic fistula and brachiocephalic fistula in a single-center experience. J. Vasc. Surg. 2022, 76, 1060–1065. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Epidemiol. Camb. Mass. 2007, 18, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Warner, E.D.; Corsi, D.R.; Jimenez, D.; Bierowski, M.; Brailovsky, Y.; Oliveros, E.; Alvarez, R.J.; Kumar, V.; Bhardwaj, A.; Rajapreyar, I.N. Determinants of pulmonary hypertension in patients with end-stage kidney disease and arteriovenous access. Curr. Probl. Cardiol. 2024, 49, 102406. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, T.S.; Kim, K.M.; Dukkipati, R.; Nguyen, T.H.; Julka, I.; Kakazu, C.; Tokhner, V.; Chauvapun, J.P. Pre-operative regional block anesthesia enhances operative strategy for arteriovenous fistula creation. J. Vasc. Access 2011, 12, 336–340. [Google Scholar] [CrossRef] [PubMed]
- Berman, S.S.; Gentile, A.T. Impact of secondary procedures in autogenous arteriovenous fistula maturation and maintenance. J. Vasc. Surg. 2001, 34, 866–871. [Google Scholar] [CrossRef] [PubMed]
- Ascher, E.; Gade, P.; Hingorani, A.; Mazzariol, F.; Gunduz, Y.; Fodera, M.; Yorkovich, W. Changes in the practice of angioaccess surgery: Impact of dialysis outcome and quality initiative recommendations. J. Vasc. Surg. 2000, 31 Pt 1, 84–92, Erratum in J. Vasc. Surg. 2000, 31, 818. [Google Scholar] [CrossRef] [PubMed]
- Georgiadis, G.S.; Charalampidis, D.G.; Argyriou, C.; Georgakarakos, E.I.; Lazarides, M.K. The Necessity for Routine Pre-operative Ultrasound Mapping Before Arteriovenous Fistula Creation: A Meta-analysis. Eur. J. Vasc. Endovasc. Surg. 2015, 49, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Tordoir, J.H.M.; Zonnebeld, N.; van Loon, M.M.; Gallieni, M.; Hollenbeck, M. Surgical and Endovascular Intervention for Dialysis Access Maturation Failure during and after Arteriovenous Fistula Surgery: Review of the Evidence. Eur. J. Vasc. Endovasc. Surg. 2018, 55, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Babadjanov, J.; Miler, R.; Niebauer, K.; Kirksey, L. Arteriovenous Fistula Creation for End-Stage Renal Disease May Worsen Pulmonary Hypertension. Ann. Vasc. Surg. 2016, 36, 293.e1–293.e3. [Google Scholar] [CrossRef] [PubMed]
- Sathiavageesan, S.; Shanmugam, V.B.; Sundaram, V. The impact of vascular access location on pulmonary arterial pressure in chronic kidney disease patients undergoing hemodialysis. Semin. Dial. 2024, 37, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Malovrh, M. Non-invasive evaluation of vessels by duplex sonography prior to construction of arteriovenous fistulas for haemodialysis. Nephrol. Dial. Transplant. 1998, 13, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Parmar, J.; Aslam, M.; Standfield, N. Pre-operative radial arterial diameter predicts early failure of arteriovenous fistula (AVF) for haemodialysis. Eur. J. Vasc. Endovasc. Surg. 2007, 33, 113–115. [Google Scholar] [CrossRef] [PubMed]
- Davidson, I.; Chan, D.; Dolmatch, B.; Hasan, M.; Nichols, D.; Saxena, R.; Shenoy, S.; Vazquez, M.; Gallieni, M. Duplex ultrasound evaluation for dialysis access selection and maintenance: A practical guide. J. Vasc. Access. 2008, 9, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Wiese, P.; Nonnast-Daniel, B. Colour Doppler ultrasound in dialysis access. Nephrol. Dial. Transplant. 2004, 19, 1956–1963. [Google Scholar] [CrossRef] [PubMed]
- Suraj, H.S.; Anil Kumar, S.; Rachegowda, N.; Rajeswari, G.T.; Yashas Ullas, L.; Revanth, R.B. Role of Doppler Evaluation in Assessing the Maturation of the Arteriovenous Fistula for Hemodialysis: An Observational Study. Cureus 2024, 16, e55527. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Silva, M.B., Jr.; Hobson, R.W., 2nd; Pappas, P.J.; Jamil, Z.; Araki, C.T.; Goldberg, M.C.; Gwertzman, G.; Padberg, F.T., Jr. A strategy for increasing use of autogenous hemodialysis access procedures: Impact of preoperative noninvasive evaluation. J. Vasc. Surg. 1998, 27, 302–307, discussion 307–308. [Google Scholar] [CrossRef] [PubMed]
- Mendes, R.R.; Farber, M.A.; Marston, W.A.; Dinwiddie, L.C.; Keagy, B.A.; Burnham, S.J. Prediction of wrist arteriovenous fistula maturation with preoperative vein mapping with ultrasonography. J. Vasc. Surg. 2002, 36, 460–463. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.; Ward, R.; Taylor, J.; Selvakumar, S.; How, T.V.; Bakran, A. Factors associated with early failure of arteriovenous fistulae for haemodialysis access. Eur. J. Vasc. Endovasc. Surg. 1996, 12, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Beathard, G.A.; Arnold, P.; Jackson, J.; Litchfield, T.; Physician Operators Forum of RMS Lifeline. Aggressive treatment of early fistula failure. Kidney Int. 2003, 64, 1487–1494. [Google Scholar] [CrossRef] [PubMed]
- Bozzetto, M.; Poloni, S.; Caroli, A.; Curtò, D.; D’Haeninck, A.; Vanommeslaeghe, F.; Gjorgjievski, N.; Remuzzi, A. The use of AVF.SIM system for the surgical planning of arteriovenous fistulae in routine clinical practice. J. Vasc. Access 2023, 24, 1061–1068. [Google Scholar] [CrossRef] [PubMed]
- Lok, C.E.; Huber, T.S.; Lee, T.; Shenoy, S.; Yevzlin, A.S.; Abreo, K.; Allon, M.; Asif, A.; Astor, B.C.; Glickman, M.H.; et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am. J. Kidney Dis. 2020, 75 (Suppl. S2), S1–S164. [Google Scholar] [CrossRef] [PubMed]
- Purwono, G.Y.; Sultana, R.; Lee, R.E.; Yap, C.J.Q.; Soon, S.X.Y.; Tan, R.Y.; Tan, C.S.; Chong, T.T.; Tang, T.Y. Accessory Vein Obliteration and Balloon-Assisted Maturation for Immature Arteriovenous Fistulas for Haemodialysis: A Systematic Review and Meta-Analysis. Cardiovasc. Intervent Radiol. 2022, 45, 1415–1427. [Google Scholar] [CrossRef] [PubMed]
- Park, S.C.; Ko, S.Y.; Kim, J.I.; Moon, I.S.; Kim, S.D. Balloon-assisted maturation for arteriovenous fistula maturation failure: An early period experience. Ann. Surg. Treat. Res. 2016, 90, 272–278. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- DerDerian, T.; Hingorani, A.; Boniviscage, P.; Carollo, A.; Ascher, E. Acute complications after balloon-assisted maturation. Ann. Vasc. Surg. 2014, 28, 1275–1279. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-J.; Ko, P.-J.; Hsu, L.-A.; Ko, Y.-S.; Chen, C.-F.; Huang, C.-C.; Hsu, T.-S.; Lee, Y.-S.; Pang, J.-H.S. Highly increased cell proliferation activity in the restenotic hemodialysis vascular access after percutaneous transluminal angioplasty: Implication in prevention of restenosis. Am. J. Kidney Dis. 2004, 43, 74–84. [Google Scholar] [CrossRef]
- Lookstein, R.A.; Haruguchi, H.; Ouriel, K.; Weinberg, I.; Lei, L.; Cihlar, S.; Holden, A. Drug-Coated Balloons for Dysfunctional Dialysis Arteriovenous Fistulas. N. Engl. J. Med. 2020, 383, 733–742. [Google Scholar] [CrossRef] [PubMed]
- DerDerian, T.; Hingorani, A.; Ascher, E.; Marks, N.; Jimenez, R.; Aboian, E.; Jacob, T.; Boniscavage, P. To BAM or not to BAM?: A closer look at balloon-assisted maturation. Ann. Vasc. Surg. 2013, 27, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Swinnen, J.J.; Zahid, A.; Burgess, D.C. Paclitaxel drug-eluting balloons to recurrent in-stent stenoses in autogenous dialysis fistulas: A retrospective study. J. Vasc. Access 2015, 16, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Miller, G.A.; Goel, N.; Khariton, A.; Friedman, A.; Savransky, Y.; Trusov, I.; Jotwani, K.; Savransky, E.; Preddie, D.; Arnold, W.P. Aggressive approach to salvage non-maturing arteriovenous fistulae: A retrospective study with follow-up. J. Vasc. Access 2009, 10, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Samett, E.J.; Hastie, J.; Chopra, P.; Pradhan, S.; Ahmad, I.; Chiramel, T.; Joseph, R. Augmented balloon-assisted maturation (aBAM) for nonmaturing dialysis arteriovenous fistula. J. Vasc. Access 2011, 12, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Pecoraro, F.; Dinoto, E.; Pakeliani, D.; Mirabella, D.; Ferlito, F.; Bajardi, G. Efficacy and one-year outcomes of Luminor® paclitaxel-coated drug-eluting balloon in the treatment of popliteal artery atherosclerosis lesions. Ann. Vasc. Surg. 2021, 76, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Rao, A.; Pappas, K.; Silpe, J.; Garlapati, A.; Talathi, S.; Mussa, F.; Landis, G.S.; Etkin, Y. Maturation Rates of Arteriovenous Fistulas Using Small Veins in the Era of Endovascular Interventions. Ann. Vasc. Surg. 2021, 71, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Voto, C.; Panetta, T. Salvage of Suboptimal or Occluded Arteriovenous Fistulas Using a 4 French System from the Radial Artery for Initial Balloon Angioplasty Maturations. Cureus 2021, 13, e13446. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dinoto, E.; Pecoraro, F.; Mirabella, D.; Ferlito, F.; Farina, A.; Lo Biundo, N.; Conti, P.; Bajardi, G. Endovascular Treatment with Drug-Eluting Balloon for Severe Subclavian Artery Stenosis Involving the Origin of the Vertebral Artery. Transl. Med. UniSa 2020, 21, 35–37. [Google Scholar] [PubMed] [PubMed Central]
- Irani, F.G.; Teo, T.K.B.; Tay, K.H.; Yin, W.H.; Win, H.H.; Gogna, A.; Patel, A.; Too, C.W.; Chan, S.X.J.M.; Lo, R.H.G.; et al. Hemodialysis Arteriovenous Fistula and Graft Stenoses: Randomized Trial Comparing Drug-eluting Balloon Angioplasty with Conventional Angioplasty. Radiology 2018, 289, 238–247. [Google Scholar] [CrossRef]
- Roy-Chaudhury, P.; Lee, T.; Woodle, B.; Wadehra, D.; Campos-Naciff, B.; Munda, R. Balloon-assisted maturation (BAM) of the arteriovenous fistula: The good, the bad, and the ugly. Semin. Nephrol. 2012, 32, 558–563. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wakabayashi, M.; Hanada, S.; Nakano, H.; Wakabayashi, T. Ultrasound-guided endovascular treatment for vascular access malfunction: Results in 4896 cases. J. Vasc. Access 2013, 14, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Napoli, M.; Bacchini, G.; Scarpati, L.; Loizzo, G.; Zito, A. Ultrasound guided interventional procedures on arteriovenous fistulae. J. Vasc. Access 2021, 22 (Suppl. S1), 91–96. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.-C.; Hsu, C.-Y.; Kang, M.-Y. Does the balloon-assisted maturation procedure offer comparable results for AVF created with a smaller vein? J. Vasc. Access 2023, 11297298221150664. [Google Scholar] [CrossRef] [PubMed]
- Dember, L.M.; Imrey, P.B.; Beck, G.J.; Cheung, A.K.; Himmelfarb, J.; Huber, T.S.; Kusek, J.W.; Roy-Chaudhury, P.; Vazquez, M.A.; Alpers, C.E.; et al. Objectives and design of the hemodialysis fistula maturation study. Am. J. Kidney Dis. 2014, 63, 104–112. [Google Scholar] [CrossRef]
- De Marco Garcia, L.P.; Davila-Santini, L.R.; Feng, Q.; Calderin, J.; Krishnasastry, K.V.; Panetta, T.F. Primary balloon angioplasty plus balloon angioplasty maturation to upgrade small-caliber veins (<3 mm) for arteriovenous fistulas. J. Vasc. Surg. 2010, 52, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Huber, T.S.; Berceli, S.A.; Scali, S.T.; Neal, D.; Anderson, E.M.; Allon, M.; Cheung, A.K.; Dember, L.M.; Himmelfarb, J.; Roy-Chaudhury, P.; et al. Arteriovenous Fistula Maturation, Functional Patency, and Intervention Rates. JAMA Surg. 2021, 56, 1111–1118, Erratum in JAMA Surg. 2022, 157, 744. [Google Scholar] [CrossRef] [PubMed]
- La Marca, M.A.; Dinoto, E.; Rodriquenz, E.; Pecoraro, F.; Turchino, D.; Mirabella, D. Brachial artery aneurysm after hemodialysis fistula ligation: Case reports and review of literature. Int. J. Surg. Case Rep. 2024, 115, 109306. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rao, N.N.; Stokes, M.B.; Rajwani, A.; Ullah, S.; Williams, K.; King, D.; Macaulay, E.; Russell, C.H.; Olakkengil, S.; Carroll, R.P.; et al. Effects of Arteriovenous Fistula Ligation on Cardiac Structure and Function in Kidney Transplant Recipients. Circulation 2019, 139, 2809–2818. [Google Scholar] [CrossRef] [PubMed]
- Kao, T.C.; Hsieh, H.C.; Yu, S.Y.; Su, T.W.; Ko, P.J. Long-term efficacy and risk factors of balloon-assisted maturation for radial-cephalic arteriovenous fistula with small-caliber veins. Hemodial. Int. 2023, 27, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Kohiyama, M.; Hoffstaetter, T.; Silpe, J.; Garlapati, A.; Landis, G.S.; Etkin, Y. Transradial access for balloon-assisted maturation of arteriovenous fistulas. J. Vasc. Surg. Cases Innov. Tech. 2023, 9, 101133. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kanchanasuttirak, P.; Pitaksantayothin, W.; Saengprakai, W.; Kanchanabat, B. Systematic review and meta-analysis: Efficacy and safety of balloon angioplasty in salvaging non-matured arteriovenous fistulas. J. Vasc. Access 2023, 24, 1244–1252. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.K.; Han, A.; Ahn, S.; Ko, H.; Chung, C.T.Y.; Choi, K.W.; Min, S.; Ha, J.; Min, S.K. Better Efficacy of Balloon Assisted Maturation in Radial-Cephalic Arteriovenous Fistula for Hemodialysis. Vasc. Specialist Int. 2021, 37, 29–36. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Elkassaby, M.; Elsaadany, N.; Mowaphy, K.; Soliman, M. Balloon-assisted maturation of autogenous arteriovenous fistulae: A randomized controlled prospective study. Vascular 2021, 29, 776–783. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, S.A.; Usoh, F.; Hingorani, A.; Iadgarova, E.; Boniscavage, P.; Eisenberg, J.; Ascher, E.; Marks, N. The Clinical Efficacy of Balloon-Assisted Maturation of Autogenous Arteriovenous Fistulae. Ann. Vasc. Surg. 2017, 41, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, J.J.; Boniscavage, P.; Ascher, E.; Hingorani, A.; Marks, N.; Shiferson, A.; Jung, D.; Jimenez, R.; Novak, D.; Jacob, T. Clinical experience with office-based duplex-guided balloon-assisted maturation of arteriovenous fistulas for hemodialysis. Ann. Vasc. Surg. 2012, 26, 982–984. [Google Scholar] [CrossRef] [PubMed]

| N % | ||
|---|---|---|
| Diabetes | None | 5 (16.1) |
| Not requiring insulin | 9 (29) | |
| Controlled by insulin | 15 (48.4) | |
| Type 1 or uncontrolled | 2 (6.5) | |
| Tobacco Use | None (>10 years ago) | 4 (12.9) |
| Quit 1–10 years ago | 11 (35.5) | |
| Current within last year, <1 package per day | 9 (29) | |
| Current within last year, >1 package per day | 7 (22.6) | |
| Hypertension | None | 0 |
| Controlled with 1 drug | 8 (25.8) | |
| Controlled with 2 drugs | 21 (67.7) | |
| Requiring > 2 drugs or uncontrolled | 2 (6.5) | |
| Cardiac status | Asymptomatic, with normal electrocardiogram | 16 (51.6) |
| Asymptomatic, but with remote myocardial infarction by history (6 months) or occult myocardial infarction | 13 (41.9) | |
| Any one of the following: stable angina, no angina but significant reversible perfusion defect on dipyridamole thallium scan, significant silent ischemia (1% of time) on Holter monitoring, ejection fraction 25% to 45%, controlled ectopy or asymptomatic arrhythmia, or history of congestive heart failure that is now well compensated | 2 (6.5) | |
| Any one of the following: unstable angina, symptomatic or poorly compensated or recurrent congestive heart failure, ejection fraction < 25%, myocardial infarction ≤ 6 months | 0 | |
| Pulmonary status | Normal | 15 (48.4) |
| Asymptomatic or mild dyspnea | 10 (32.2) | |
| Between normal and asymptomatic or mild dyspnea | 6 (19.4) | |
| Vital capacity less than 1.85 L, FEV1 < 1.2 L or <35% of predicted, maximal voluntary ventilation < 50% of predicted, PCO2 > 45 mm Hg, supplemental oxygen use medically necessary, or pulmonary hypertension | 0 | |
| Functional status | No impairment | 23 (74.2) |
| Impaired, but able to carry out ADL without assistance | 7 (22.6) | |
| Needs some assistance to carry out ADL or ambulatory assistance | 1 (3.2) | |
| Requiring total assistance for ADL or non-ambulatory | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mirabella, D.; Dinoto, E.; Rodriquenz, E.; Bellomo, M.; Miccichè, A.; Annicchiarico, P.; Pecoraro, F. Improved Ultrasound-Guided Balloon-Assisted Maturation Angioplasty Using Drug-Eluting Balloons in the First Autogenous Arteriovenous Fistula Procedure: Early Experience. Biomedicines 2024, 12, 1005. https://doi.org/10.3390/biomedicines12051005
Mirabella D, Dinoto E, Rodriquenz E, Bellomo M, Miccichè A, Annicchiarico P, Pecoraro F. Improved Ultrasound-Guided Balloon-Assisted Maturation Angioplasty Using Drug-Eluting Balloons in the First Autogenous Arteriovenous Fistula Procedure: Early Experience. Biomedicines. 2024; 12(5):1005. https://doi.org/10.3390/biomedicines12051005
Chicago/Turabian StyleMirabella, Domenico, Ettore Dinoto, Edoardo Rodriquenz, Michele Bellomo, Andrea Miccichè, Paolo Annicchiarico, and Felice Pecoraro. 2024. "Improved Ultrasound-Guided Balloon-Assisted Maturation Angioplasty Using Drug-Eluting Balloons in the First Autogenous Arteriovenous Fistula Procedure: Early Experience" Biomedicines 12, no. 5: 1005. https://doi.org/10.3390/biomedicines12051005
APA StyleMirabella, D., Dinoto, E., Rodriquenz, E., Bellomo, M., Miccichè, A., Annicchiarico, P., & Pecoraro, F. (2024). Improved Ultrasound-Guided Balloon-Assisted Maturation Angioplasty Using Drug-Eluting Balloons in the First Autogenous Arteriovenous Fistula Procedure: Early Experience. Biomedicines, 12(5), 1005. https://doi.org/10.3390/biomedicines12051005







