Mitochondrial Dysfunction in Sporadic Amyotrophic Lateral Sclerosis Patients: Insights from High-Resolution Respirometry
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Cohort
2.2. Peripheral Blood Mononuclear Cell Isolation
2.3. High-Resolution Respirometry
2.4. Determination of Protein Concentration
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vidovic, M.; Müschen, L.H.; Brakemeier, S.; Machetanz, G.; Naumann, M.; Castro-Gomez, S. Current State and Future Directions in the Diagnosis of Amyotrophic Lateral Sclerosis. Cells 2023, 12, 736. [Google Scholar] [CrossRef] [PubMed]
- Hanhisuanto, M.; Solje, E.; Jokela, M.; Sipilä, J.O.T. Amyotrophic Lateral Sclerosis in Southwestern and Eastern Finland. Neuroepidemiology 2023, 57, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Brotman, R.G.; Moreno-Escobar, M.C.; Joseph, J.; Munakomi, S.; Pawar, G. Amyotrophic Lateral Sclerosis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Cerillo, J.L.; Parmar, M. Tofersen. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Mead, R.J.; Shan, N.; Reiser, H.J.; Marshall, F.; Shaw, P.J. Amyotrophic Lateral Sclerosis: A Neurodegenerative Disorder Poised for Successful Therapeutic Translation. Nat. Rev. Drug. Discov. 2023, 22, 185–212. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Andreucci, A.; Iwamoto, N.; Yin, Y.; Yang, H.; Liu, F.; Bulychev, A.; Hu, X.S.; Lin, X.; Lamore, S.; et al. Preclinical Evaluation of WVE-004, an Investigational Stereopure Oligonucleotide for the Treatment of C9orf72-Associated ALS or FTD. Mol. Ther. Nucleic Acids 2022, 28, 558–570. [Google Scholar] [CrossRef]
- Jiang, J.; Wang, Y.; Deng, M. New Developments and Opportunities in Drugs Being Trialed for Amyotrophic Lateral Sclerosis from 2020 to 2022. Front. Pharmacol. 2022, 13, 1054006. [Google Scholar] [CrossRef] [PubMed]
- Yerton, M.; Winter, A.; Kostov, A.; Lieberman, C.; Gelevski, D.; Weber, H.; Doyle, M.; Kane, G.; Parikh, N.; Burke, K.M.; et al. An Expanded Access Protocol of RT001 in Amyotrophic Lateral Sclerosis-Initial Experience with a Lipid Peroxidation Inhibitor. Muscle Nerve 2022, 66, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.; Shukla, S. Role of Edaravone as a Treatment Option for Patients with Amyotrophic Lateral Sclerosis. Pharmaceuticals 2020, 14, 29. [Google Scholar] [CrossRef] [PubMed]
- Paganoni, S.; Quintana, M.; Sherman, A.V.; Vestrucci, M.; Wu, Y.; Timmons, J.; Cudkowicz, M. Pooled Resource Open-Access ALS Clinical Trials Consortium Analysis of Sodium Phenylbutyrate and Taurursodiol Survival Effect in ALS Using External Controls. Ann. Clin. Transl. Neurol. 2023, 10, 2297–2304. [Google Scholar] [CrossRef] [PubMed]
- Gautam, M.; Genç, B.; Helmold, B.; Ahrens, A.; Kuka, J.; Makrecka-Kuka, M.; Günay, A.; Koçak, N.; Aguilar-Wickings, I.R.; Keefe, D.; et al. SBT-272 Improves TDP-43 Pathology in ALS Upper Motor Neurons by Modulating Mitochondrial Integrity, Motility, and Function. Neurobiol. Dis. 2023, 178, 106022. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Bracci, P.M.; Azhir, A.; Forrest, B.D.; McGrath, M.S. Macrophage-Targeted Sodium Chlorite (NP001) Slows Progression of Amyotrophic Lateral Sclerosis (ALS) through Regulation of Microbial Translocation. Biomedicines 2022, 10, 2907. [Google Scholar] [CrossRef] [PubMed]
- Mora, J.S.; Bradley, W.G.; Chaverri, D.; Hernández-Barral, M.; Mascias, J.; Gamez, J.; Gargiulo-Monachelli, G.M.; Moussy, A.; Mansfield, C.D.; Hermine, O.; et al. Long-Term Survival Analysis of Masitinib in Amyotrophic Lateral Sclerosis. Ther. Adv. Neurol. Disord. 2021, 14, 17562864211030365. [Google Scholar] [CrossRef] [PubMed]
- Camu, W.; Mickunas, M.; Veyrune, J.-L.; Payan, C.; Garlanda, C.; Locati, M.; Juntas-Morales, R.; Pageot, N.; Malaspina, A.; Andreasson, U.; et al. Repeated 5-Day Cycles of Low Dose Aldesleukin in Amyotrophic Lateral Sclerosis (IMODALS): A Phase 2a Randomised, Double-Blind, Placebo-Controlled Trial. eBioMedicine 2020, 59, 102844. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Stoklund Dittlau, K.; Van Den Bosch, L. Axonal Transport Defects and Neurodegeneration: Molecular Mechanisms and Therapeutic Implications. Semin. Cell Dev. Biol. 2020, 99, 133–150. [Google Scholar] [CrossRef] [PubMed]
- Raffaele, S.; Nguyen, N.; Milanese, M.; Mannella, F.C.; Boccazzi, M.; Frumento, G.; Bonanno, G.; Abbracchio, M.P.; Bonifacino, T.; Fumagalli, M. Montelukast Improves Disease Outcome in SOD1G93A Female Mice by Counteracting Oligodendrocyte Dysfunction and Aberrant Glial Reactivity. Br. J. Pharmacol. 2024; early view. [Google Scholar] [CrossRef]
- Raffaele, S.; Boccazzi, M.; Fumagalli, M. Oligodendrocyte Dysfunction in Amyotrophic Lateral Sclerosis: Mechanisms and Therapeutic Perspectives. Cells 2021, 10, 565. [Google Scholar] [CrossRef] [PubMed]
- Vanneste, J.; Van Den Bosch, L. The Role of Nucleocytoplasmic Transport Defects in Amyotrophic Lateral Sclerosis. Int. J. Mol. Sci. 2021, 22, 12175. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.G.; Mitchell, J.D.; Lyon, M.; Moore, D.H. Riluzole for Amyotrophic Lateral Sclerosis (ALS)/Motor Neuron Disease (MND). Amyotroph. Lateral Scler. Other Mot. Neuron Disord. 2003, 4, 191–206. [Google Scholar] [CrossRef]
- Castillo, K.; Nassif, M.; Valenzuela, V.; Rojas, F.; Matus, S.; Mercado, G.; Court, F.A.; van Zundert, B.; Hetz, C. Trehalose Delays the Progression of Amyotrophic Lateral Sclerosis by Enhancing Autophagy in Motoneurons. Autophagy 2013, 9, 1308–1320. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, L.; Martinez, A. Emerging Clinical Investigational Drugs for the Treatment of Amyotrophic Lateral Sclerosis. Expert Opin. Investig. Drugs 2023, 32, 141–160. [Google Scholar] [CrossRef] [PubMed]
- Štětkářová, I.; Ehler, E. Diagnostics of Amyotrophic Lateral Sclerosis: Up to Date. Diagnostics 2021, 11, 231. [Google Scholar] [CrossRef] [PubMed]
- Zarei, S.; Carr, K.; Reiley, L.; Diaz, K.; Guerra, O.; Altamirano, P.F.; Pagani, W.; Lodin, D.; Orozco, G.; Chinea, A. A Comprehensive Review of Amyotrophic Lateral Sclerosis. Surg. Neurol. Int. 2015, 6, 171. [Google Scholar] [CrossRef] [PubMed]
- Wijesekera, L.C.; Leigh, P.N. Amyotrophic Lateral Sclerosis. Orphanet J. Rare Dis. 2009, 4, 3. [Google Scholar] [CrossRef] [PubMed]
- Richards, D.; Morren, J.A.; Pioro, E.P. Time to Diagnosis and Factors Affecting Diagnostic Delay in Amyotrophic Lateral Sclerosis. J. Neurol. Sci. 2020, 417, 117054. [Google Scholar] [CrossRef] [PubMed]
- Shellikeri, S.; Karthikeyan, V.; Martino, R.; Black, S.E.; Zinman, L.; Keith, J.; Yunusova, Y. The Neuropathological Signature of Bulbar-Onset ALS: A Systematic Review. Neurosci. Biobehav. Rev. 2017, 75, 378–392. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, S.; Vielhaber, S.; Schreiber, F.; Cartwright, M.S. Peripheral Nerve Imaging in Amyotrophic Lateral Sclerosis. Clin. Neurophysiol. 2020, 131, 2315–2326. [Google Scholar] [CrossRef] [PubMed]
- Proudfoot, M.; Bede, P.; Turner, M.R. Imaging Cerebral Activity in Amyotrophic Lateral Sclerosis. Front. Neurol. 2019, 9, 1148. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Wang, X.; Huo, Z.; Chen, Y.; Liu, J.; Zhao, Z.; Meng, F.; Su, Q.; Bao, W.; Zhang, L.; et al. The Impact of Mitochondrial Dysfunction in Amyotrophic Lateral Sclerosis. Cells 2022, 11, 2049. [Google Scholar] [CrossRef] [PubMed]
- Genin, E.C.; Abou-Ali, M.; Paquis-Flucklinger, V. Mitochondria, a Key Target in Amyotrophic Lateral Sclerosis Pathogenesis. Genes 2023, 14, 1981. [Google Scholar] [CrossRef] [PubMed]
- Belosludtseva, N.V.; Matveeva, L.A.; Belosludtsev, K.N. Mitochondrial Dyshomeostasis as an Early Hallmark and a Therapeutic Target in Amyotrophic Lateral Sclerosis. Int. J. Mol. Sci. 2023, 24, 16833. [Google Scholar] [CrossRef] [PubMed]
- Brooks, B.R.; Miller, R.G.; Swash, M.; Munsat, T.L. World Federation of Neurology Research Group on Motor Neuron Diseases El Escorial Revisited: Revised Criteria for the Diagnosis of Amyotrophic Lateral Sclerosis. Amyotroph. Lateral Scler. Other Mot. Neuron Disord. 2000, 1, 293–299. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, M.; Dengler, R.; Eisen, A.; England, J.D.; Kaji, R.; Kimura, J.; Mills, K.; Mitsumoto, H.; Nodera, H.; Shefner, J.; et al. Electrodiagnostic Criteria for Diagnosis of ALS. Clin. Neurophysiol. 2008, 119, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Sumbalova, Z.; Kucharska, J.; Palacka, P.; Rausova, Z.; Langsjoen, P.H.; Langsjoen, A.M.; Gvozdjakova, A. Platelet Mitochondrial Function and Endogenous Coenzyme Q10 Levels Are Reduced in Patients after COVID-19. Bratisl. Lek. Listy 2022, 123, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Gnaiger, E. Mitochondrial Pathways and Respiratory Control: An Introduction to OXPHOS Analysis, 5th ed.; Bioenergetics Communications: Innsbruck, Austria, 2020. [Google Scholar]
- Javadov, S.; Kozlov, A.V.; Camara, A.K.S. Mitochondria in Health and Diseases. Cells 2020, 9, 1177. [Google Scholar] [CrossRef] [PubMed]
- Kausar, S.; Wang, F.; Cui, H. The Role of Mitochondria in Reactive Oxygen Species Generation and Its Implications for Neurodegenerative Diseases. Cells 2018, 7, 274. [Google Scholar] [CrossRef] [PubMed]
- Shi, P.; Gal, J.; Kwinter, D.M.; Liu, X.; Zhu, H. Mitochondrial Dysfunction in Amyotrophic Lateral Sclerosis. Biochim. Biophys. Acta 2010, 1802, 45–51. [Google Scholar] [CrossRef]
- Verma, M.; Lizama, B.N.; Chu, C.T. Excitotoxicity, Calcium and Mitochondria: A Triad in Synaptic Neurodegeneration. Transl. Neurodegener. 2022, 11, 3. [Google Scholar] [CrossRef] [PubMed]
- Kann, O.; Kovács, R. Mitochondria and Neuronal Activity. Am. J. Physiol. Cell Physiol. 2007, 292, C641–C657. [Google Scholar] [CrossRef] [PubMed]
- Jadiya, P.; Garbincius, J.F.; Elrod, J.W. Reappraisal of Metabolic Dysfunction in Neurodegeneration: Focus on Mitochondrial Function and Calcium Signaling. Acta Neuropathol. Commun. 2021, 9, 124. [Google Scholar] [CrossRef] [PubMed]
- Norat, P.; Soldozy, S.; Sokolowski, J.D.; Gorick, C.M.; Kumar, J.S.; Chae, Y.; Yağmurlu, K.; Prada, F.; Walker, M.; Levitt, M.R.; et al. Mitochondrial Dysfunction in Neurological Disorders: Exploring Mitochondrial Transplantation. npj Regen. Med. 2020, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.F.; Shaw, P.J.; De Vos, K.J. The Role of Mitochondria in Amyotrophic Lateral Sclerosis. Neurosci. Lett. 2019, 710, 132933. [Google Scholar] [CrossRef] [PubMed]
- Kaal, E.C.; Vlug, A.S.; Versleijen, M.W.; Kuilman, M.; Joosten, E.A.; Bär, P.R. Chronic Mitochondrial Inhibition Induces Selective Motoneuron Death in Vitro: A New Model for Amyotrophic Lateral Sclerosis. J. Neurochem. 2000, 74, 1158–1165. [Google Scholar] [CrossRef]
- Grossini, E.; Garhwal, D.; Venkatesan, S.; Ferrante, D.; Mele, A.; Saraceno, M.; Scognamiglio, A.; Mandrioli, J.; Amedei, A.; De Marchi, F.; et al. The Potential Role of Peripheral Oxidative Stress on the Neurovascular Unit in Amyotrophic Lateral Sclerosis Pathogenesis: A Preliminary Report from Human and In Vitro Evaluations. Biomedicines 2022, 10, 691. [Google Scholar] [CrossRef] [PubMed]
- Miquel, E.; Cassina, A.; Martínez-Palma, L.; Souza, J.M.; Bolatto, C.; Rodríguez-Bottero, S.; Logan, A.; Smith, R.A.J.; Murphy, M.P.; Barbeito, L.; et al. Neuroprotective Effects of the Mitochondria-Targeted Antioxidant MitoQ in a Model of Inherited Amyotrophic Lateral Sclerosis. Free Radic. Biol. Med. 2014, 70, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Jung, C.; Higgins, C.M.J.; Xu, Z. Mitochondrial Electron Transport Chain Complex Dysfunction in a Transgenic Mouse Model for Amyotrophic Lateral Sclerosis. J. Neurochem. 2002, 83, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, N.; Beal, M.F.; Matson, W.R.; Bogdanov, M.B. Increased Oxidative Damage to DNA in an Animal Model of Amyotrophic Lateral Sclerosis. Free Radic. Res. 2005, 39, 383–388. [Google Scholar] [CrossRef]
- Magrì, A.; Lipari, C.L.R.; Risiglione, P.; Zimbone, S.; Guarino, F.; Caccamo, A.; Messina, A. ERK1/2-Dependent TSPO Overactivation Associates with the Loss of Mitophagy and Mitochondrial Respiration in ALS. Cell Death Dis. 2023, 14, 122. [Google Scholar] [CrossRef] [PubMed]
- Crugnola, V.; Lamperti, C.; Lucchini, V.; Ronchi, D.; Peverelli, L.; Prelle, A.; Sciacco, M.; Bordoni, A.; Fassone, E.; Fortunato, F.; et al. Mitochondrial Respiratory Chain Dysfunction in Muscle from Patients with Amyotrophic Lateral Sclerosis. Arch. Neurol. 2010, 67, 849–854. [Google Scholar] [CrossRef] [PubMed]
- Wiedemann, F.R.; Winkler, K.; Kuznetsov, A.V.; Bartels, C.; Vielhaber, S.; Feistner, H.; Kunz, W.S. Impairment of Mitochondrial Function in Skeletal Muscle of Patients with Amyotrophic Lateral Sclerosis. J. Neurol. Sci. 1998, 156, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.J.; Suh, Y.-L. Ultrastructural Changes of Mitochondria in the Skeletal Muscle of Patients with Amyotrophic Lateral Sclerosis. Ultrastruct. Pathol. 2002, 26, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Kubat, G.B.; Picone, P. Skeletal Muscle Dysfunction in Amyotrophic Lateral Sclerosis: A Mitochondrial Perspective and Therapeutic Approaches. Neurol. Sci. 2024; ahead of printing. [Google Scholar] [CrossRef]
- Curti, D.; Malaspina, A.; Facchetti, G.; Camana, C.; Mazzini, L.; Tosca, P.; Zerbi, F.; Ceroni, M. Amyotrophic Lateral Sclerosis: Oxidative Energy Metabolism and Calcium Homeostasis in Peripheral Blood Lymphocytes. Neurology 1996, 47, 1060–1064. [Google Scholar] [CrossRef] [PubMed]
- Allen, S.P.; Duffy, L.M.; Shaw, P.J.; Grierson, A.J. Altered Age-Related Changes in Bioenergetic Properties and Mitochondrial Morphology in Fibroblasts from Sporadic Amyotrophic Lateral Sclerosis Patients. Neurobiol. Aging 2015, 36, 2893–2903. [Google Scholar] [CrossRef] [PubMed]
- Du, R.; Chen, P.; Li, M.; Zhu, Y.; He, Z.; Huang, X. Developing a Novel Immune Infiltration-Associated Mitophagy Prediction Model for Amyotrophic Lateral Sclerosis Using Bioinformatics Strategies. Front. Immunol. 2024, 15, 1360527. [Google Scholar] [CrossRef] [PubMed]
- Harvey, C.; Weinreich, M.; Lee, J.A.K.; Shaw, A.C.; Ferraiuolo, L.; Mortiboys, H.; Zhang, S.; Hop, P.J.; Zwamborn, R.A.J.; van Eijk, K.; et al. Rare and Common Genetic Determinants of Mitochondrial Function Determine Severity but Not Risk of Amyotrophic Lateral Sclerosis. Heliyon 2024, 10, e24975. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.J.; Adams, D.A.; Niedzwiecki, M.V.; Wong, M. Aberrant DNA and RNA Methylation Occur in Spinal Cord and Skeletal Muscle of Human SOD1 Mouse Models of ALS and in Human ALS: Targeting DNA Methylation Is Therapeutic. Cells 2022, 11, 3448. [Google Scholar] [CrossRef] [PubMed]
- Araujo, B.G.; Souza E Silva, L.F.; de Barros Torresi, J.L.; Siena, A.; Valerio, B.C.O.; Brito, M.D.; Rosenstock, T.R. Decreased Mitochondrial Function, Biogenesis, and Degradation in Peripheral Blood Mononuclear Cells from Amyotrophic Lateral Sclerosis Patients as a Potential Tool for Biomarker Research. Mol. Neurobiol. 2020, 57, 5084–5102. [Google Scholar] [CrossRef] [PubMed]
- Djafarzadeh, S.; Jakob, S.M. High-Resolution Respirometry to Assess Mitochondrial Function in Permeabilized and Intact Cells. J. Vis. Exp. 2017, 120, 54985. [Google Scholar] [CrossRef]
- Jang, D.H.; Greenwood, J.C.; Spyres, M.B.; Eckmann, D.M. Measurement of Mitochondrial Respiration and Motility in Acute Care: Sepsis, Trauma, and Poisoning. J. Intensive Care Med. 2017, 32, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Singh, T.; Jiao, Y.; Ferrando, L.M.; Yablonska, S.; Li, F.; Horoszko, E.C.; Lacomis, D.; Friedlander, R.M.; Carlisle, D.L. Neuronal Mitochondrial Dysfunction in Sporadic Amyotrophic Lateral Sclerosis Is Developmentally Regulated. Sci. Rep. 2021, 11, 18916. [Google Scholar] [CrossRef] [PubMed]
- Ehinger, J.K.; Morota, S.; Hansson, M.J.; Paul, G.; Elmér, E. Mitochondrial Dysfunction in Blood Cells from Amyotrophic Lateral Sclerosis Patients. J. Neurol. 2015, 262, 1493–1503. [Google Scholar] [CrossRef] [PubMed]
- Ghiasi, P.; Hosseinkhani, S.; Noori, A.; Nafissi, S.; Khajeh, K. Mitochondrial Complex I Deficiency and ATP/ADP Ratio in Lymphocytes of Amyotrophic Lateral Sclerosis Patients. Neurol. Res. 2012, 34, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Sakae, N.; Bieniek, K.F.; Zhang, Y.-J.; Ross, K.; Gendron, T.F.; Murray, M.E.; Rademakers, R.; Petrucelli, L.; Dickson, D.W. Poly-GR Dipeptide Repeat Polymers Correlate with Neurodegeneration and Clinicopathological Subtypes in C9ORF72-Related Brain Disease. Acta Neuropathol. Commun. 2018, 6, 63. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Liu, H.; Itoh, K.; Oh, S.; Zhao, L.; Murata, D.; Sesaki, H.; Hartung, T.; Na, C.H.; Wang, J. C9orf72 Regulates Energy Homeostasis by Stabilizing Mitochondrial Complex I Assembly. Cell Metab. 2021, 33, 531–546.e9. [Google Scholar] [CrossRef] [PubMed]
- Sverdlov, A.L.; Elezaby, A.; Qin, F.; Behring, J.B.; Luptak, I.; Calamaras, T.D.; Siwik, D.A.; Miller, E.J.; Liesa, M.; Shirihai, O.S.; et al. Mitochondrial Reactive Oxygen Species Mediate Cardiac Structural, Functional, and Mitochondrial Consequences of Diet-Induced Metabolic Heart Disease. J. Am. Heart Assoc. 2016, 5, e002555. [Google Scholar] [CrossRef] [PubMed]
- Mourier, A.; Larsson, N.-G. Tracing the Trail of Protons through Complex I of the Mitochondrial Respiratory Chain. PLoS Biol. 2011, 9, e1001129. [Google Scholar] [CrossRef] [PubMed]
- Browne, S.E.; Bowling, A.C.; Baik, M.J.; Gurney, M.; Brown, R.H.; Beal, M.F. Metabolic Dysfunction in Familial, but Not Sporadic, Amyotrophic Lateral Sclerosis. J. Neurochem. 1998, 71, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Duranti, E.; Villa, C. Muscle Involvement in Amyotrophic Lateral Sclerosis: Understanding the Pathogenesis and Advancing Therapeutics. Biomolecules 2023, 13, 1582. [Google Scholar] [CrossRef] [PubMed]
- Hor, J.-H.; Santosa, M.M.; Lim, V.J.W.; Ho, B.X.; Taylor, A.; Khong, Z.J.; Ravits, J.; Fan, Y.; Liou, Y.-C.; Soh, B.-S.; et al. ALS Motor Neurons Exhibit Hallmark Metabolic Defects That Are Rescued by SIRT3 Activation. Cell Death Differ. 2021, 28, 1379–1397. [Google Scholar] [CrossRef] [PubMed]
- Connolly, N.M.C.; Theurey, P.; Adam-Vizi, V.; Bazan, N.G.; Bernardi, P.; Bolaños, J.P.; Culmsee, C.; Dawson, V.L.; Deshmukh, M.; Duchen, M.R.; et al. Guidelines on Experimental Methods to Assess Mitochondrial Dysfunction in Cellular Models of Neurodegenerative Diseases. Cell Death Differ. 2018, 25, 542–572. [Google Scholar] [CrossRef] [PubMed]
- Desler, C.; Hansen, T.L.; Frederiksen, J.B.; Marcker, M.L.; Singh, K.K.; Juel Rasmussen, L. Is There a Link between Mitochondrial Reserve Respiratory Capacity and Aging? J. Aging Res. 2012, 2012, 192503. [Google Scholar] [CrossRef] [PubMed]
- Lastres-Becker, I.; Porras, G.; Arribas-Blázquez, M.; Maestro, I.; Borrego-Hernández, D.; Boya, P.; Cerdán, S.; García-Redondo, A.; Martínez, A.; Martin-Requero, Á. Molecular Alterations in Sporadic and SOD1-ALS Immortalized Lymphocytes: Towards a Personalized Therapy. Int. J. Mol. Sci. 2021, 22, 3007. [Google Scholar] [CrossRef] [PubMed]
- Goetzman, E.; Gong, Z.; Zhang, B.; Muzumdar, R. Complex II Biology in Aging, Health, and Disease. Antioxidants 2023, 12, 1477. [Google Scholar] [CrossRef] [PubMed]
- Ranganayaki, S.; Jamshidi, N.; Aiyaz, M.; Rashmi, S.-K.; Gayathri, N.; Harsha, P.K.; Padmanabhan, B.; Srinivas Bharath, M.M. Inhibition of Mitochondrial Complex II in Neuronal Cells Triggers Unique Pathways Culminating in Autophagy with Implications for Neurodegeneration. Sci. Rep. 2021, 11, 1483. [Google Scholar] [CrossRef] [PubMed]
- Guzy, R.D.; Sharma, B.; Bell, E.; Chandel, N.S.; Schumacker, P.T. Loss of the SdhB, but Not the SdhA, Subunit of Complex II Triggers Reactive Oxygen Species-Dependent Hypoxia-Inducible Factor Activation and Tumorigenesis. Mol. Cell. Biol. 2008, 28, 718–731. [Google Scholar] [CrossRef] [PubMed]
- Duan, S.; Hajek, P.; Lin, C.; Shin, S.K.; Attardi, G.; Chomyn, A. Mitochondrial Outer Membrane Permeability Change and Hypersensitivity to Digitonin Early in Staurosporine-Induced Apoptosis. J. Biol. Chem. 2003, 278, 1346–1353. [Google Scholar] [CrossRef] [PubMed]
- Schirinzi, T.; Salvatori, I.; Zenuni, H.; Grillo, P.; Valle, C.; Martella, G.; Mercuri, N.B.; Ferri, A. Pattern of Mitochondrial Respiration in Peripheral Blood Cells of Patients with Parkinson’s Disease. Int. J. Mol. Sci. 2022, 23, 10863. [Google Scholar] [CrossRef] [PubMed]
- Annesley, S.J.; Lay, S.T.; De Piazza, S.W.; Sanislav, O.; Hammersley, E.; Allan, C.Y.; Francione, L.M.; Bui, M.Q.; Chen, Z.-P.; Ngoei, K.R.W.; et al. Immortalized Parkinson’s Disease Lymphocytes Have Enhanced Mitochondrial Respiratory Activity. Dis. Model. Mech. 2016, 9, 1295–1305. [Google Scholar] [CrossRef] [PubMed]
- Arduíno, D.M.; Esteves, A.R.; Swerdlow, R.H.; Cardoso, S.M. A Cybrid Cell Model for the Assessment of the Link Between Mitochondrial Deficits and Sporadic Parkinson’s Disease. Methods Mol. Biol. 2015, 1265, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Bindoff, L.A.; Birch-Machin, M.A.; Cartlidge, N.E.F.; Parker, W.D.; Turnbull, D.M. Respiratory Chain Abnormalities in Skeletal Muscle from Patients with Parkinson’s Disease. J. Neurol. Sci. 1991, 104, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Fišar, Z.; Jirák, R.; Zvěřová, M.; Setnička, V.; Habartová, L.; Hroudová, J.; Vaníčková, Z.; Raboch, J. Plasma Amyloid Beta Levels and Platelet Mitochondrial Respiration in Patients with Alzheimer’s Disease. Clin. Biochem. 2019, 72, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Feldhaus, P.; Fraga, D.B.; Ghedim, F.V.; De Luca, R.D.; Bruna, T.D.; Heluany, M.; Matos, M.P.; Ferreira, G.K.; Jeremias, I.C.; Heluany, C.; et al. Evaluation of Respiratory Chain Activity in Lymphocytes of Patients with Alzheimer Disease. Metab. Brain Dis. 2011, 26, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Rabinovici, G.D.; Miller, B.L. Frontotemporal Lobar Degeneration. CNS Drugs 2010, 24, 375–398. [Google Scholar] [CrossRef] [PubMed]
- Perier, C.; Vila, M. Mitochondrial Biology and Parkinson’s Disease. Cold Spring Harb. Perspect. Med. 2012, 2, a009332. [Google Scholar] [CrossRef]
- Bayliak, M.M.; Gospodaryov, D.V.; Lushchak, V.I. Homeostasis of Carbohydrates and Reactive Oxygen Species Is Critically Changed in the Brain of Middle-Aged Mice: Molecular Mechanisms and Functional Reasons. BBA Adv. 2023, 3, 100077. [Google Scholar] [CrossRef] [PubMed]
- Kuzma-Kozakiewicz, M.; Kwiecinski, H. New Therapeutic Targets for Amyotrophic Lateral Sclerosis. Expert Opin. Ther. Targets 2011, 15, 127–143. [Google Scholar] [CrossRef] [PubMed]
- Matsuhashi, T.; Hishiki, T.; Zhou, H.; Ono, T.; Kaneda, R.; Iso, T.; Yamaguchi, A.; Endo, J.; Katsumata, Y.; Atsushi, A.; et al. Activation of Pyruvate Dehydrogenase by Dichloroacetate Has the Potential to Induce Epigenetic Remodeling in the Heart. J. Mol. Cell. Cardiol. 2015, 82, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Longo, N.; Frigeni, M.; Pasquali, M. Carnitine Transport and Fatty Acid Oxidation. Biochim. Biophys. Acta 2016, 1863, 2422–2435. [Google Scholar] [CrossRef] [PubMed]
- Cunha-Oliveira, T.; Montezinho, L.; Simões, R.F.; Carvalho, M.; Ferreiro, E.; Silva, F.S.G. Mitochondria: A Promising Convergent Target for the Treatment of Amyotrophic Lateral Sclerosis. Cells 2024, 13, 248. [Google Scholar] [CrossRef]


| Physiopathogenic Mechanisms | Involvement in the Pathophysiology | Method of Therapeutic Intervention | Drugs | Mechanism of Action |
|---|---|---|---|---|
| Genetic mutation | More than 120 genes linked to disease pathophysiology The most common mutations in genes: SOD1, FUS, TDP 43, C9ORF72, TARDBP | Tofersen | Antisense oligonucleotide against SOD1 [4] | |
| Antisense oligonucleotide therapy | ION-363 | Antisense oligonucleotide against FUS [5] | ||
| WVE-004 | Antisense oligonucleotide against C9orf72 [6] | |||
| Oxidative stress | An initiating factor; the accumulation of ROS leads to cell damage and subsequent cell death due to an imbalance of radical generation and antioxidant protection | Antioxidants and modified oxidative stress | Verdiperstat | Myeloperoxidase inhibitor [7] |
| RT001 | Provides resistance to membrane lipid peroxidation [8] | |||
| Mitochondrial dysfunction | An early change; a key mechanism, ALS can promote mitochondrial fission and lead to fragmentation of the mitochondrial network through an increase in fission factors and a decrease in fusion factors. Electron transport chain dysfunction leads to higher mitochondrial oxygen consumption and ROS generation levels, reduced ATP synthesis, and DNA repair. | Mitochondria-targetted antioxidant therapy | Edavarone * | Antioxidant that removes oxygen radicals and eliminates lipid peroxides in the CNS [9] |
| Sodium phenylbutyrate and Taurursodiol * | Decreases ER stress and mitochondrial dysfunction [10] | |||
| SBT-272 | Mitochondria-targeted novel peptide and peptidomimetic [11] | |||
| Microglia or macrophage | Infiltration of the gray and white matter of the spinal cord by macrophages surrounding the infiltrated nerve cells. Role of macrophages in causing neuroinflammation and subsequent degeneration of motor neurons | Anti-inflamatory therapy Autophagy targetted | NP001 | Macrophage activation regulator [12] |
| Neuroinflammation | Activated microglia can activate astrocyte neurotoxicity by secreting inflammatory factors. | Modulation of the inflammatory environment | Masitinib Aldesleukin Pegcetacoplan | CSF1R kinase inhibitor [13] Recombinant human IL-2 [14] Complement C3 regulator [7] |
| Axonal transport defects | A likely factor, it is one of the earliest impairments seen in ALS, but its underlying cause remains unclear | Targeting microtubules and motor proteins | Noscapine | Stabilizes microtubules by binding to α-tubulin [15] |
| Oligodendrocyte dysfunction | Insufficient local energy supply from oligodendrocytes to axons leads to an energy deficit of motor neurons. Oxidative stress damage and an abnormal immune microenvironment lead to impaired oligodendrocyte differentiation, causing demyelination and degeneration of motor neurons. | Restoration of lipid homeostasis (remyelination) protection against oxidative stress, promotion of proliferation and maturation | Montelucast | Promotes OPC differentiation and remyelination in vivo [16] |
| Bazedoxifene | Enhances myelin production by stimulating cholesterol biosynthesis in OL [17] | |||
| Nucleocytoplasmic defects | Impaired vesicle transport can cause protein aggregation and fragmentation of the Golgi apparatus | Down-regulation of exportin I | (SINE)-KPT-276 | Selective inhibitor of nuclear export [18] |
| Glutamate excitotoxicity | Glutamate receptor hyperstimulation, increased synaptic glutamate release, altered AMPARs, decreased clearance of glutamate by astrocytes | Glutamate inhibitors improve motor function | Riluzole * | Glutamate antagonist that inhibits glutamate release and protein kinase C [19] |
| Impaired proteostasis | Misfolded proteins and protein aggregates accumulate in affected neurons and surrounding supporting cells | Increase in proteosome activity | Trehalose | Repurposed disaccharide that may prevent mutant protein aggregation [20] |
| Trametinib | Mitogen-activated protein kinase (MEK) inhibitor that aims to activate the autophagy-lysosome pathway [21] |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Adults age 18–80 | Diagnosis of frontotemporal dementia or any other neurodegenerative diseases |
| Definitive diagnosis based on revised El Escorial criteria | Any acute or chronic condition that would limit the ability of the patient to participate in the study |
| Electromyographic findings meeting the Awaji Shima criteria | Unavailable family medical history |
| Refusal to give informed consent |
| Gender | Age | Diagnostic Delay (Months) | Duration (Month) | ALSFRS Score | Medication | Symptoms | Onset of Symptoms | |
|---|---|---|---|---|---|---|---|---|
| 1 | Male | 42 | 6 | 16 | 42 | Riluzole Coenzyme Q10 Milgamma N | Left lower limb weakness, stiffness, motor problem, spastic-paretic gait | Spinal |
| 2 | Female | 59 | 4 | 4 | 39 | Riluzole Coenzyme Q10 Magnesium | Twitching in the right upper limb, twitching, weaker lower limbs | Spinal |
| 3 | Male | 46 | 11 | 12 | 42 | No medication | Numbness of the fingers on the upper limbs, twitching of the body, fatigue | Spinal |
| 4 | Male | 44 | 8 | 21 | 30 | Riluzole Coenzyme Q10 Milgamma N | Quadriparesis with dominant involvement of the left-sided limbs, the degree of paresis is most pronounced in the left upper limb | Spinal |
| 5 | Female | 56 | 12 | 16 | 43 | Riluzole Coenzyme Q10 | Speech and swallowing problems, altered voice, progressive weakness of acral left upper limb, muscle hypotrophy, twitching of body muscles, progressively weaker left lower limb, slight shortness of breath on faster walking, exertion | Bulbar |
| 6 | Female | 52 | 18 | 46 | 43 | Riluzole Coenzyme Q10 | Head drooping, PEG, anarthria | Bulbar |
| 7 | Male | 46 | 9 | 77 | 38 | Riluzole Coenzyme Q10 Milgamma N | Lower limb weakness, right upper limb weakness, wheelchair mobility | Spinal |
| 8 | Male | 33 | 11 | 12 | 43 | Riluzole Milgamma N | Tingling, progressive weakness of the left upper limb, posture, and gait normal | Spinal |
| 9 | Male | 64 | 24 | 29 | 36 | Riluzole Milgamma N | Upper and lower limb weakness, dysarthric speech, dysphagia, hemiparetic gait | Bulbar |
| 10 | Female | 70 | 4 | 22 | 15 | Riluzole Coenzyme Q10 Milgamma N | Spastic quadriparesis, dysarthria, wheelchair movement | Spinal |
| 11 | Male | 80 | 24 | 24 | 35 | No medication | Weakness and hypotrophy of the muscles of the right upper limb, gradual weakness also in the left upper limb, weakness of the lower limbs, impairment of speech and swallowing | Spinal |
| 12 | Female | 62 | 53 | 63 | 37 | No medication | Progressive quadriparesis, dysarthric speech, wheelchair movement | Spinal |
| 13 | Female | 60 | 36 | 36 | 25 | Riluzole | Mild dysarthria, bulbar syndrome, signs of mixed quadriparesis with advanced muscle hypotrophy, walking with the help of another person | Spinal |
| 14 | Female | 56 | 16 | 17 | 41 | No medication | Weakness of the right upper and lower limbs, progressive triparesis of the limbs | Spinal |
| 15 | Male | 59 | 8 | 8 | 34 | Riluzole Coenzyme Q10 Milgamma N | Quadriparesis, dysarthria, weakening of neck and axial muscles, present generalized fasciculations, impaired swallowing | Bulbar |
| 16 | Female | 51 | 6 | 10 | 45 | Riluzole Coenzyme Q10 | Weakness of the lower limbs, instability when walking, weakness of the left upper limb | Spinal |
| 17 | Female | 56 | 5 | 11 | 43 | Riluzole Coenzyme Q10 Milgamma N | Dysarthria, difficulty swallowing, weakened neck muscles, muscle twitching | bulbar |
| 18 | Male | 69 | 6 | 6 | 41 | Riluzole Coenzyme Q10 Milgamma N | Weakness of the lower limbs, gradually also weakness of the left upper limb | Spinal |
| 19 | Male | 37 | 4 | 4 | 37 | No medication | Impaired leg mobility and buckling, upper limb insecurity and clumsiness | Spinal |
| 20 | Male | 28 | 6 | 8 | 37 | Riluzole | Weakness, clumsiness of the right upper limb, muscle twitching, impaired articulation | Spinal |
| 21 | Female | 69 | 9 | 9 | 36 | Milgama N | Lower limb weakness, gait impairment, knee buckling, upper limb weakness, walking with the aid of a cane | Spinal |
| 22 | Female | 37 | 5 | 5 | 42 | No medication | Weakness of the lower limbs, problems with walking | Spinal |
| 23 | Female | 55 | 12 | 12 | 25 | No medication | Upper limb weakness and stiffness acral left lower limb weakness | Spinal |
| 24 | Female | 66 | 3 | 3 | 45 | No medication | bulbar syndrome (dysarthria, dysphonia, dysphagia, discrete fasciculations on the tongue) | bulbar |
| 25 | Male | 55 | 14 | 14 | 46 | No medication | Progressive asymmetric weakness of the upper limbs | Spinal |
| 26 | Male | 65 | 4 | 6 | 38 | Riluzole Coenzyme Q10 Milgamma N | Weakness of the lower limbs, motor problem of the right upper limb, walking with the help of a cane | Spinal |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Adults age 18–80 | Occurrence of neurodegenerative diseases in the family history |
| Healthy with no history of chronic diseases | Any acute or chronic condition that would limit the ability of the patient to participate in the study |
| Without chronic treatment | Missing family history |
| persons without any family relation to the patients | Refusal to give informed consent |
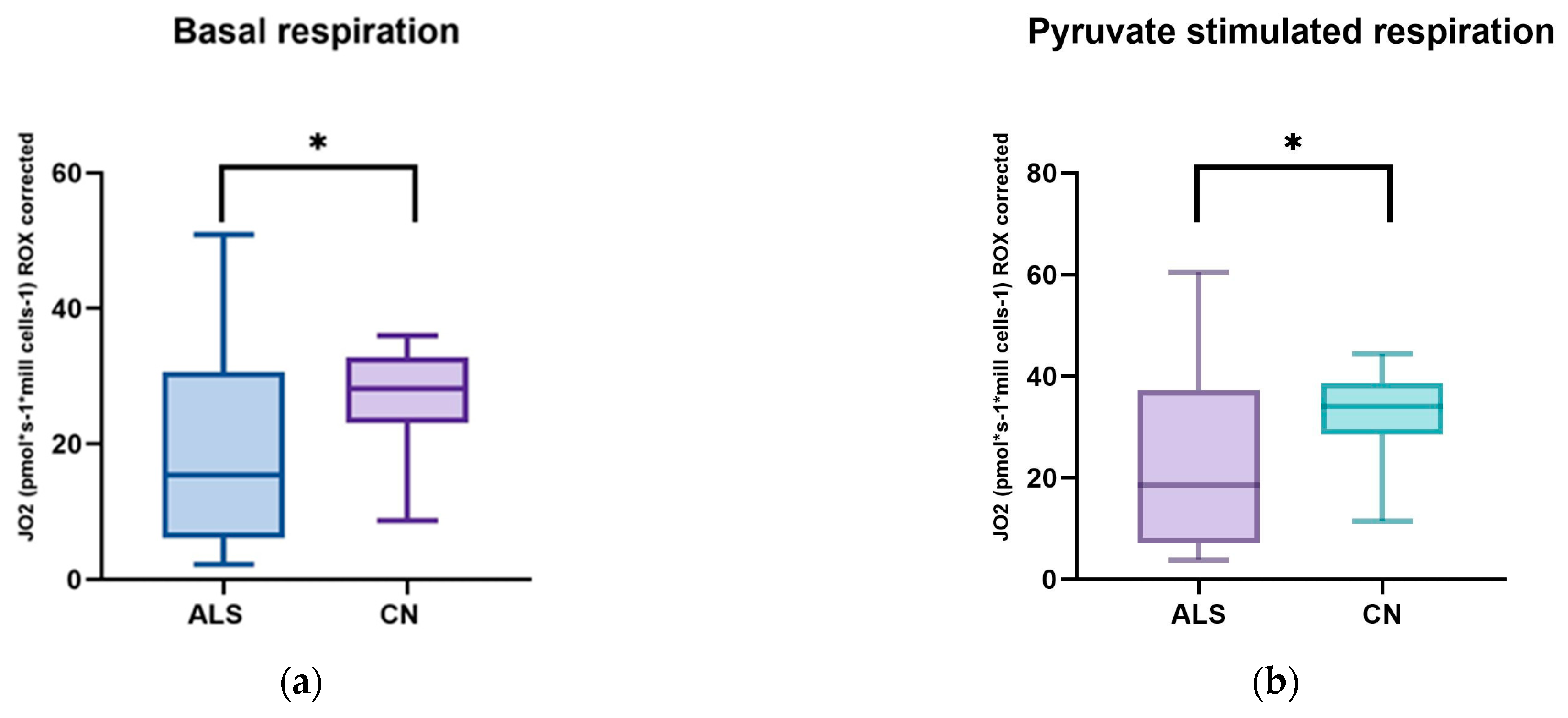
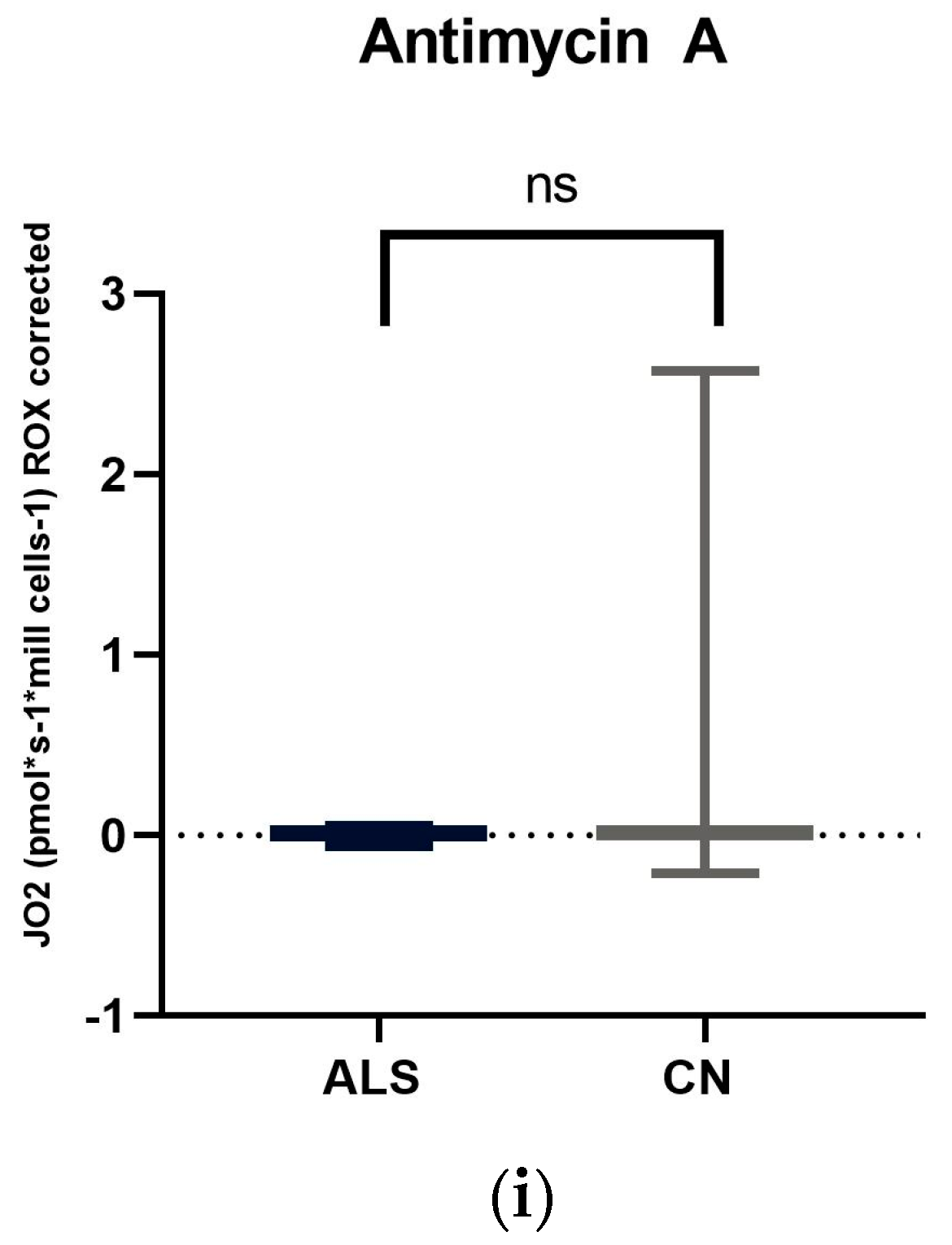
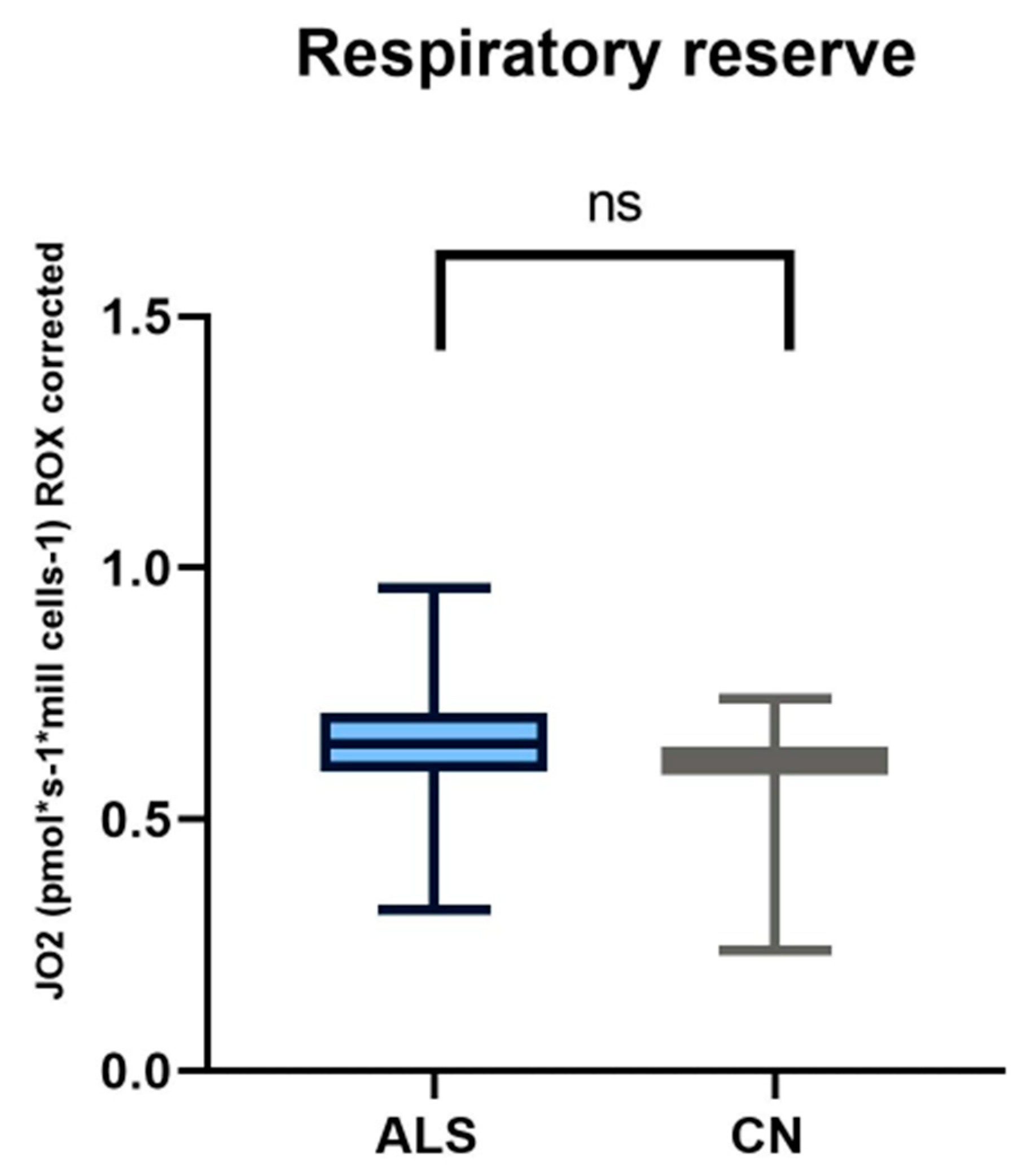
| State/Substrate | Control Subjects | ALS Patients |
|---|---|---|
| Basal respiration | 26.42 ± 1.41 | 18.63 ± 2.77 |
| Pyruvate | 32.15 ± 1.76 | 22.74 ± 3.39 |
| Oligomycin | 4.77 ± 0.60 | 2.83 ± 1.62 |
| Uncoupler | 71.01 ± 4.31 | 51.02 ± 6.66 |
| Rotenone | 0.53 ± 0.50 | 0.64 ± 0.74 |
| Succinate | 5.70 ± 0.73 | 5.37 ± 0.91 |
| Digitonin | 58.25 ± 4.45 | 42.01 ± 6.17 |
| Cytochrome C | 57.94 ± 4.35 | 42.57 ± 6.30 |
| Antimycin A | 0.27 ± 0.14 | 0.01 ± 0.14 |
| Limitations of the Study | Ideas for Future Research |
|---|---|
| Sporadic disease, limited number of patients Lack of studies addressing this disease | Studies on a larger number of patients Further work to validate the results obtained |
| Diagnostic delay | Exploring new biomarkers that could lead to earlier diagnosis of the disease |
| Heterogeneity of the disease | Monitoring interactions of pathophysiological mechanisms and risk factors |
| Elucidation of mitochondrial respiration differences between neurodegenerative diseases | |
| Individual rate of disease progression | Longitudinal follow-up of patients over time and assessment of changes according to the rate of disease progression |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parvanovova, P.; Evinova, A.; Grofik, M.; Hnilicova, P.; Tatarkova, Z.; Turcanova-Koprusakova, M. Mitochondrial Dysfunction in Sporadic Amyotrophic Lateral Sclerosis Patients: Insights from High-Resolution Respirometry. Biomedicines 2024, 12, 1294. https://doi.org/10.3390/biomedicines12061294
Parvanovova P, Evinova A, Grofik M, Hnilicova P, Tatarkova Z, Turcanova-Koprusakova M. Mitochondrial Dysfunction in Sporadic Amyotrophic Lateral Sclerosis Patients: Insights from High-Resolution Respirometry. Biomedicines. 2024; 12(6):1294. https://doi.org/10.3390/biomedicines12061294
Chicago/Turabian StyleParvanovova, Petra, Andrea Evinova, Milan Grofik, Petra Hnilicova, Zuzana Tatarkova, and Monika Turcanova-Koprusakova. 2024. "Mitochondrial Dysfunction in Sporadic Amyotrophic Lateral Sclerosis Patients: Insights from High-Resolution Respirometry" Biomedicines 12, no. 6: 1294. https://doi.org/10.3390/biomedicines12061294






