Spontaneous Reduction in the Intermetatarsal Angle in Distal First Metatarsal Osteotomies with No Lateral Head Displacement in Hallux Valgus
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Surgical Procedures
- -
- Step 1: medial longitudinal incision centered on the MTP1, exposure of the joint capsule with protection of the medial dorsal sensory branch of the hallux, longitudinal capsulotomy centered on the MTP1, and exposure of the medial aspect of the head of the M1.
- -
- Step 2: exostectomy.
- -
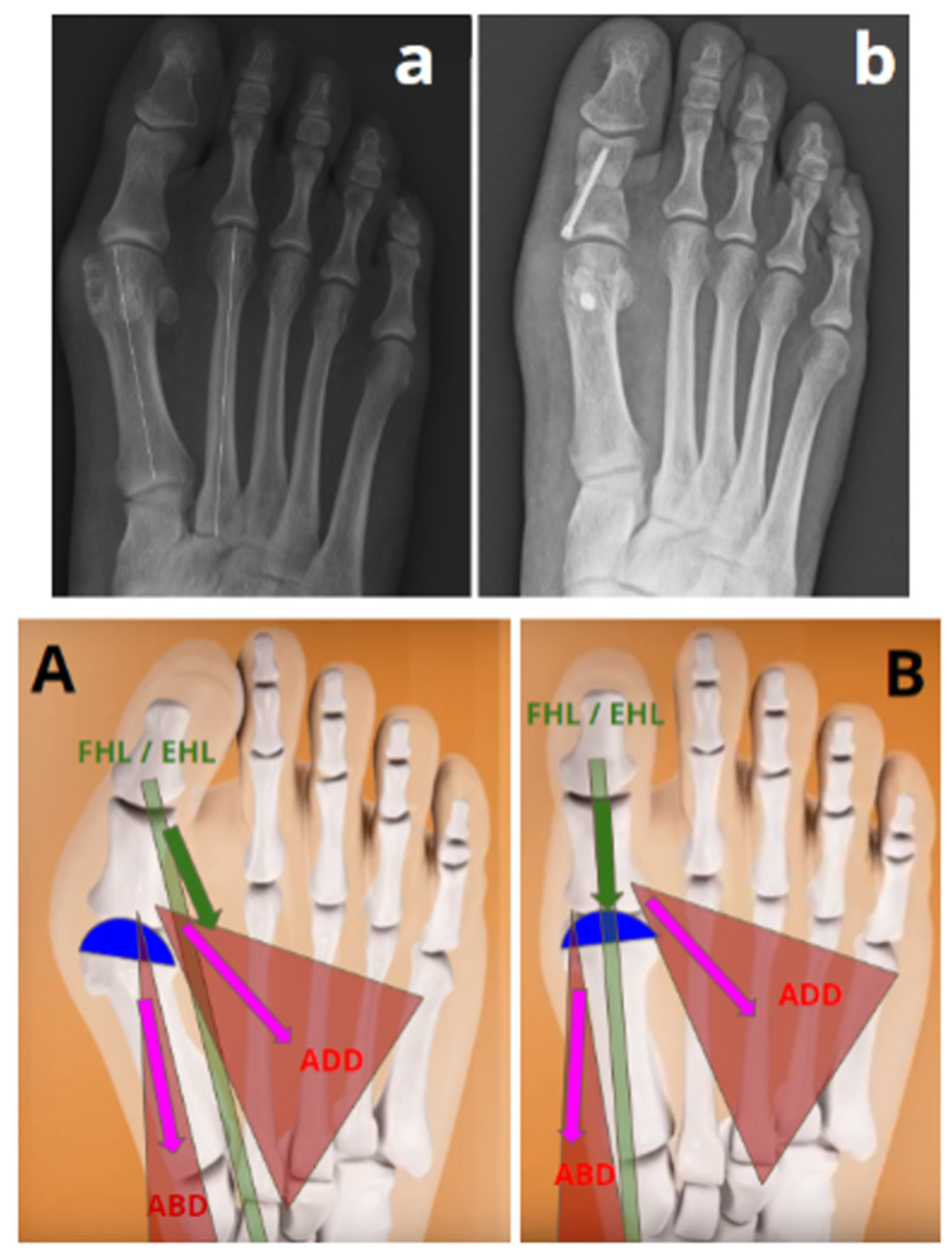
- Step 3: Chevron osteotomy (Figure 1). The dorsal cut was vertical, made 3 mm proximal to the distal articular surface of the M1, orthogonal to the axis of the 2nd metatarsal and extended over the dorsal third of the M1 head. The plantar cut began at the end of the dorsal cut and ended at the level of the neck of the M1 with an angulation of approximately 120°. The orientation of the saw in the dorsoplantar plane was aligned with the 4th metatarsal.
- -
- Step 4: Sectioning of the lateral metatarso-sesamoid ligament (i.e., suspensory ligament) through osteotomy. The phalangeal and lateral sesamoid insertions of the conjoined tendon of the adductor muscle were not severed.
- -
- Step 5: in the plantar part of the osteotomy, a medial wedge resection extending across the entire width of M1, with a Akin osteotomy thickness of 3 mm at its base, was performed, allowing for a supination movement of the head (Figure 2).
- -
- Step 6: implementation of an Akin osteotomy fixed with a screw [21].
- -
- Step 7: release of the tourniquet; hemostasis; closure without capsulorrhaphy.
2.3. Collecting Radiographic Data
2.4. Assessment Criteria
2.5. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barg, A.; Harmer, J.R.; Presson, A.P.; Zhang, C.; Lackey, M.; Saltzman, C.L. Unfavorable Outcomes Following Surgical Treatment of Hallux Valgus Deformity: A Systematic Literature Review. J. Bone Jt. Surg. 2018, 100, 1563–1573. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.; Roseiro, L.; Seiça, E.C.; Amaro, A.M. A Systematic Review of Osteotomies to Correct Hallux Valgus in the First Metatarsal. Appl. Sci. 2024, 14, 3043. [Google Scholar] [CrossRef]
- Jeuken, R.M.; Schotanus, M.G.M.; Kort, N.P.; Deenik, A.; Jong, B.; Hendrickx, R.P.M. Long-Term Follow-up of a Randomized Controlled Trial Comparing Scarf to Chevron Osteotomy in Hallux Valgus Correction. Foot Ankle Int. 2016, 37, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Lalevée, M.; Barbachan Mansur, N.S.; Dibbern, K.; Briggs, H.; Maly, C.J.; de Carvalho, K.A.M.; Lintz, F.; de Cesar Netto, C. Coronal Plane Rotation of the Medial Column in Hallux Valgus: A Retrospective Case-Control Study. Foot Ankle Int. 2022, 43, 1041–1048. [Google Scholar] [CrossRef] [PubMed]
- Lalevee, M.; de Cesar Netto, C.; ReSurg; Boublil, D.; Coillard, J.Y. Recurrence Rates with Longer-Term Follow-up After Hallux Valgus Surgical Treatment with Distal Metatarsal Osteotomies: A Systematic Review and Meta-Analysis. Foot Ankle Int. 2023, 44, 210–222. [Google Scholar] [CrossRef] [PubMed]
- Steadman, J.; Bakshi, N.; Philippi, M.; Arena, C.; Leake, R.; Barg, A.; Saltzman, C.L. Association of Normal vs Abnormal Meary Angle with Hindfoot Malalignment and First Metatarsal Rotation: A Short Report. Foot Ankle Int. 2022, 43, 706–709. [Google Scholar] [CrossRef]
- Murawski, D.E.; Beskin, J.L. Increased Displacement Maximizes the Utility of the Distal Chevron Osteotomy for Hallux Valgus Deformity Correction. Foot Ankle Int. 2008, 29, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Vernois, J.; Redfern, D.J. Percutaneous Surgery for Severe Hallux Valgus. Foot Ankle Clin. 2016, 21, 479–493. [Google Scholar] [CrossRef] [PubMed]
- Dalat, F.; Cottalorda, F.; Fessy, M.H.; Besse, J.L. Does Arthrodesis of the First Metatarsophalangeal Joint Correct the Intermetatarsal M1M2 Angle? Analysis of a Continuous Series of 208 Arthrodeses Fixed with Plates. Orthop. Traumatol. Surg. Res. 2015, 101, 709–714. [Google Scholar] [CrossRef]
- Dayton, P.; Carvalho, S.; Egdorf, R.; Dayton, M. Comparison of Radiographic Measurements Before and After Triplane Tarsometatarsal Arthrodesis for Hallux Valgus. J. Foot Ankle Surg. 2020, 59, 291–297. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, J.S.; Young, K.W.; Naraghi, R.; Cho, H.K.; Lee, S.Y. A New Measure of Tibial Sesamoid Position in Hallux Valgus in Relation to the Coronal Rotation of the First Metatarsal in CT Scans. Foot Ankle Int. 2015, 36, 944–952. [Google Scholar] [CrossRef] [PubMed]
- Mortier, J.P.; Bernard, J.L.; Maestro, M. Axial Rotation of the First Metatarsal Head in a Normal Population and Hallux Valgus Patients. Orthop. Traumatol. Surg. Res. 2012, 98, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Najefi, A.A.; Malhotra, K.; Patel, S.; Cullen, N.; Welck, M. Assessing the Rotation of the First Metatarsal on Computed Tomography Scans: A Systematic Literature Review. Foot Ankle Int. 2022, 43, 66–76. [Google Scholar] [CrossRef]
- Najefi, A.A.; Katmeh, R.; Zaveri, A.K.; Alsafi, M.K.; Garrick, F.; Malhotra, K.; Patel, S.; Cullen, N.; Welck, M. Imaging Findings and First Metatarsal Rotation in Hallux Valgus. Foot Ankle Int. 2022, 43, 665–675. [Google Scholar] [CrossRef] [PubMed]
- Steadman, J.; Barg, A.; Saltzman, C.L. First Metatarsal Rotation in Hallux Valgus Deformity. Foot Ankle Int. 2021, 42, 510–522. [Google Scholar] [CrossRef]
- Conti, M.S.; Patel, T.J.; Zhu, J.; Elliott, A.J.; Conti, S.F.; Ellis, S.J. Association of First Metatarsal Pronation Correction with Patient-Reported Outcomes and Recurrence Rates in Hallux Valgus. Foot Ankle Int. 2022, 43, 309–320. [Google Scholar] [CrossRef]
- Ono, Y.; Yamaguchi, S.; Sadamasu, A.; Kimura, S.; Watanabe, S.; Akagi, R.; Sasho, T.; Ohtori, S. The Shape of the First Metatarsal Head and Its Association with the Presence of Sesamoid-Metatarsal Joint Osteoarthritis and the Pronation Angle. J. Orthop. Sci. 2020, 25, 658–663. [Google Scholar] [CrossRef]
- Okuda, R.; Kinoshita, M.; Yasuda, T.; Jotoku, T.; Kitano, N.; Shima, H. The Shape of the Lateral Edge of the First Metatarsal Head as a Risk Factor for Recurrence of Hallux Valgus. J. Bone Jt. Surg. Am. 2007, 89, 2163–2172. [Google Scholar] [CrossRef]
- Jastifer, J.R.; Coughlin, M.J.; Schutt, S.; Hirose, C.; Kennedy, M.; Grebing, B.; Smith, B.; Cooper, T.; Golano, P.; Viladot, R.; et al. Comparison of Radiographic and Anatomic Distal Metatarsal Articular Angle in Cadaver Feet. Foot Ankle Int. 2014, 35, 389–393. [Google Scholar] [CrossRef]
- Lalevée, M.; Barbachan Mansur, N.S.; Lee, H.Y.; Maly, C.J.; Iehl, C.J.; Nery, C.; Lintz, F.; de Cesar Netto, C. Distal Metatarsal Articular Angle in Hallux Valgus Deformity. Fact or Fiction? A 3-Dimensional Weightbearing CT Assessment. Foot Ankle Int. 2022, 43, 495–503. [Google Scholar] [CrossRef]
- Lee, K.M.; Ahn, S.; Chung, C.Y.; Sung, K.H.; Park, M.S. Reliability and Relationship of Radiographic Measurements in Hallux Valgus. Clin. Orthop. Relat. Res. 2012, 470, 2613–2621. [Google Scholar] [CrossRef] [PubMed]
- Hardy, R.H.; Clapham, J.C. Observations on Hallux Valgus; Based on a Controlled Series. J. Bone Jt. Surg. Br. 1951, 33, 376–391. [Google Scholar] [CrossRef]
- Shima, H.; Okuda, R.; Yasuda, T.; Jotoku, T.; Kitano, N.; Kinoshita, M. Radiographic Measurements in Patients with Hallux Valgus before and after Proximal Crescentic Osteotomy. J. Bone Jt. Surg. Am. 2009, 91, 1369–1376. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass Correlations: Uses in Assessing Rater Reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Cronin, J.J.; Limbers, J.P.; Kutty, S.; Stephens, M.M. Intermetatarsal Angle after First Metatarsophalangeal Joint Arthrodesis for Hallux Valgus. Foot Ankle Int. 2006, 27, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Welck, M.J.; Al-Khudairi, N. Imaging of Hallux Valgus: How to Approach the Deformity. Foot Ankle Clin. 2018, 23, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Sa, I. The Reverdin-Isham Procedure for the Correction of Hallux Abducto Valgus: A Distal Metatarsal Osteotomy Procedure. Clin. Podiatr. Med. Surg. 1991, 8, 81–94. [Google Scholar]
- Bauer, T.; Biau, D.; Lortat-Jacob, A.; Hardy, P. Percutaneous Hallux Valgus Correction Using the Reverdin-Isham Osteotomy. Orthop. Traumatol. Surg. Res. 2010, 96, 407–416. [Google Scholar] [CrossRef]
- Severyns, M.; Carret, P.; Brunier-Agot, L.; Debandt, M.; Odri, G.A.; Rouvillain, J.L. Reverdin-Isham Procedure for Mild or Moderate Hallux Valgus: Clinical and Radiographic Outcomes. Musculoskelet. Surg. 2019, 103, 161–166. [Google Scholar] [CrossRef]
- Yasuda, T.; Okuda, R.; Jotoku, T.; Shima, H.; Hida, T.; Neo, M. Proximal Supination Osteotomy of the First Metatarsal for Hallux Valgus. Foot Ankle Int. 2015, 36, 696–704. [Google Scholar] [CrossRef]
- Park, C.H.; Lee, W.C. Recurrence of Hallux Valgus Can Be Predicted from Immediate Postoperative Non-Weight-Bearing Radiographs. J. Bone Jt. Surg. Am. 2017, 99, 1190–1197. [Google Scholar] [CrossRef] [PubMed]
- Mansur, N.S.B.; Lalevee, M.; Schmidt, E.; Dibbern, K.; Wagner, P.; Wagner, E.; de Souza Nery, C.A.; de Cesar Netto, C. Correlation between Indirect Radiographic Parameters of First Metatarsal Rotation in Hallux Valgus and Values on Weight-Bearing Computed Tomography. Int. Orthop. 2021, 45, 3111–3118. [Google Scholar] [CrossRef]
- Patel, T.J.; Conti, M.S.; Caolo, K.C.; Miller, M.C.; Conti, S.F.; Ellis, S.J. Pronation on Weightbearing Radiographs Does Not Correlate with Pronation from Weightbearing CT Scans. Foot Ankle Surg. 2022, 28, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Tsikopoulos, K.; Papaioannou, P.; Kitridis, D.; Mavridis, D.; Georgiannos, D. Proximal versus Distal Metatarsal Osteotomies for Moderate to Severe Hallux Valgus Deformity: A Systematic Review and Meta-Analysis of Clinical and Radiological Outcomes. Int. Orthop. 2018, 42, 1853–1863. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Song, Y.; Xu, Y.; Zhu, A.; Baker, J.S.; Liu, W.; Gu, Y. Toe Box Shape of Running Shoes Affects In-Shoe Foot Displacement and Deformation: A Randomized Crossover Study. Bioengineering 2024, 11, 457. [Google Scholar] [CrossRef]
- Perera, A.M.; Mason, L.; Stephens, M.M. The pathogenesis of hallux valgus. J. Bone Jt. Surg. Am. 2011, 93, 1650–1661. [Google Scholar] [CrossRef] [PubMed]



| IMA (Degrees) Median (IQR) | HVA (Degrees) Median (IQR) | DMAA (Degrees) Mean ± SD | Hardy and Clapham Score Median (IQR) | Okuda Classification | |
|---|---|---|---|---|---|
| Successful Group (n= 13) | 13 (IQR 2) | 25 (IQR 3) | 14.5 ± 5.5 | 6 (IQR 2) | 2 A/3 I/8 R |
| Failed Group % (n = 12) | 16 (IQR 2.25) | 35 (IQR 2.5) | 20.9 ± 6.9 | 6 (IQR 1.25) | 0 A/5 I/7 R |
| p-Value | 0.0006 | 0.001 | 0.02 | 0.31 | 0.28 |
| IMA (Degrees) Median (IQR) | HVA (Degrees) Mean ± SD | DMAA (Degrees) Mean ± SD | Hardy and Clapham Score Median (IQR) | Okuda Classification | |
|---|---|---|---|---|---|
| Preoperative (n = 13) | 13 (IQR 2) | 25.4 ± 3.1 | 14.5 ± 5.5 | 6 (IQR 2) | 2A/3I/8R |
| 1 year (n = 13) | 6 (IQR 3) | 11.5 ± 4.0 | 4.8 ± 2.9 | 3 (IQR 2) | 7A/6I/0R |
| p-Value | <0.001 | <0.001 | <0.001 | 0.002 | <0.001 |
| IMA (Degrees) Mean ± SD | HVA (Degrees) Median (IQR) | DMAA (Degrees) Mean ± SD | Hardy and Clapham Score Median (IQR) | Okuda Classification | |
|---|---|---|---|---|---|
| Preoperative (n = 12) | 16.3 ± 2.4 | 35 (IQR 2.5) | 20.9 ± 6.9 | 6 (IQR 1.25) | 0A/5I/7R |
| 1 year (n = 12) | 5.7 ± 2.1 | 12 (IQR 7.8) | 7.3 ± 3 | 2 (IQR 1.25) | 5A/6I/1R |
| p-Value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coillard, J.-Y.; Rey, R.; Civinini, A.; Billuart, F.; Schmidt, E.; de Cesar Netto, C.; Sacco, R.; Lalevée, M. Spontaneous Reduction in the Intermetatarsal Angle in Distal First Metatarsal Osteotomies with No Lateral Head Displacement in Hallux Valgus. Biomedicines 2024, 12, 1438. https://doi.org/10.3390/biomedicines12071438
Coillard J-Y, Rey R, Civinini A, Billuart F, Schmidt E, de Cesar Netto C, Sacco R, Lalevée M. Spontaneous Reduction in the Intermetatarsal Angle in Distal First Metatarsal Osteotomies with No Lateral Head Displacement in Hallux Valgus. Biomedicines. 2024; 12(7):1438. https://doi.org/10.3390/biomedicines12071438
Chicago/Turabian StyleCoillard, Jean-Yves, Romain Rey, Alessandro Civinini, Fabien Billuart, Eli Schmidt, Cesar de Cesar Netto, Riccardo Sacco, and Matthieu Lalevée. 2024. "Spontaneous Reduction in the Intermetatarsal Angle in Distal First Metatarsal Osteotomies with No Lateral Head Displacement in Hallux Valgus" Biomedicines 12, no. 7: 1438. https://doi.org/10.3390/biomedicines12071438
APA StyleCoillard, J.-Y., Rey, R., Civinini, A., Billuart, F., Schmidt, E., de Cesar Netto, C., Sacco, R., & Lalevée, M. (2024). Spontaneous Reduction in the Intermetatarsal Angle in Distal First Metatarsal Osteotomies with No Lateral Head Displacement in Hallux Valgus. Biomedicines, 12(7), 1438. https://doi.org/10.3390/biomedicines12071438






