Interactions Involving Glycine and Other Amino Acid Neurotransmitters: Focus on Transporter-Mediated Regulation of Release and Glycine–Glutamate Crosstalk
Abstract
:1. Introduction
1.1. Glycine and Its Interactions with Other Neurotransmitters
1.2. Functional Interactions Involving Gly and Other Major Amino Acid NTs: A Focus on Transporter-Mediated Mechanisms
1.3. Aims of the Study
2. Transporter-Mediated Interactions between Two (Not Only Amino Acid) NTs: Some Considerations
3. Transporter-Mediated Interactions between Gly and Glu
3.1. Gly-Evoked Glu Release from Spinal Cord Nerve Terminals
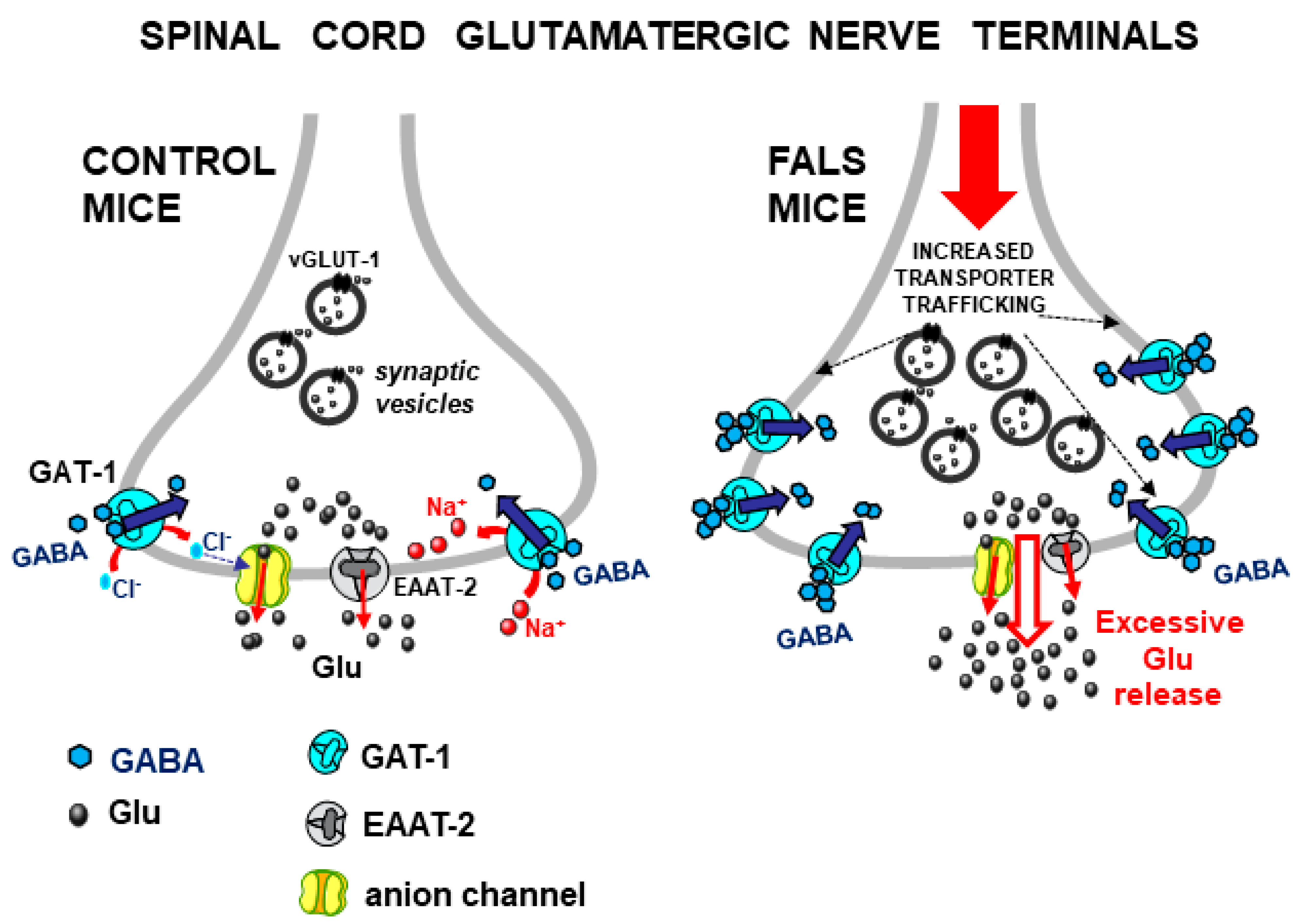
3.2. The Excessive Gly-Evoked Glu Release in an Animal Model of Amyotrophic Lateral Sclerosis
3.3. Gly–Glu Interactions in Mouse Cerebellum
3.4. Gly–Glu Interactions in Mouse Hippocampus
4. Transporter-Mediated Interactions between GABA and Glu
4.1. GABA-Induced Glu Release in the Spinal Cord
4.2. Glu–GABA Interactions in the Spinal Cord
5. Transporter-Mediated Interactions between Gly and GABA
5.1. Interactions between Gly and GABA in the Spinal Cord
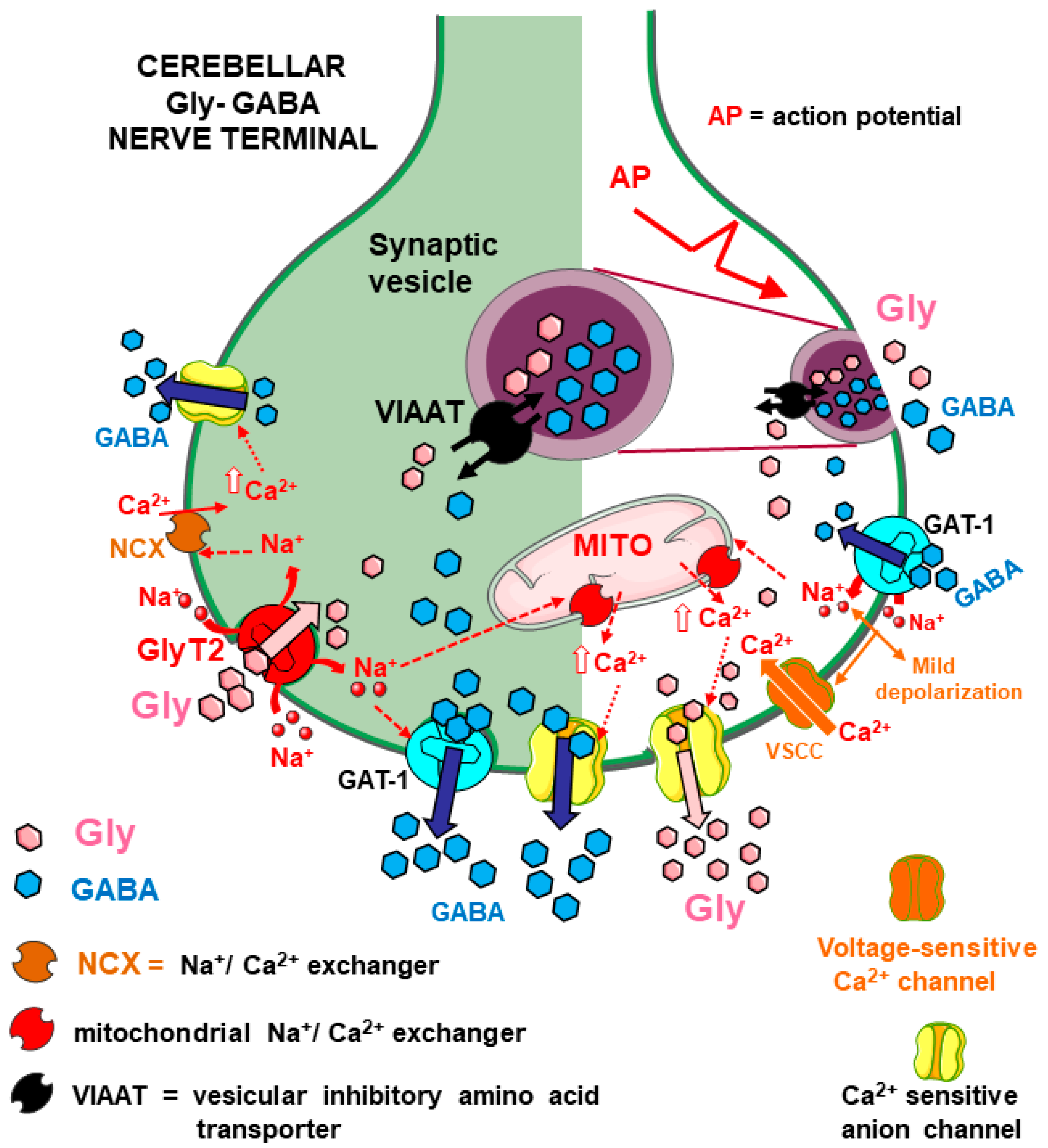
5.2. Gly and GABA Reciprocally Modulate Their Release in Mouse Cerebellum
6. Discussion
6.1. General Physiological Significance of the Transporter-Mediated Interactions among Amino Acid NTs
6.1.1. Gly, Glu, and GABA as Reciprocal Enhancers of Their Release through Transporter Activation
6.1.2. Transporters Coexistence and Transporter-Mediated Interactions as “Functional Markers” of Cotransmission
6.2. Transporter-Mediated Interactions among Amino Acid NTs Are Mediated by Multiple Mechanisms
6.3. Possible Pathophysiological Implications of Transporter-Mediated Gly–Glu (and GABA–Glu) Interactions
6.3.1. The Excessive Glu Release Evoked by Gly and GABA in the Spinal Cord in Animal Models of Amyotrophic Lateral Sclerosis
6.3.2. GlyT1, GlyT2, and GAT-1 Transporters and Pain
6.3.3. Considerations on Transporter-Mediated Interactions Involving Amino Acid NTs in the Hippocampus
7. Limitations
8. Concluding Remarks
9. Future Directions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baer, K.; Waldvogel, H.J.; Faull, R.L.M.; Rees, M.I. Localization of Glycine Receptors in the Human Forebrain, Brainstem, and Cervical Spinal Cord: An Immunohistochemical Review. Front. Mol. Neurosci. 2009, 2, 25. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.W. Native Glycine Receptor Subtypes and Their Physiological Roles. Neuropharmacology 2009, 56, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.W.; Ascher, P. Glycine Potentiates the NMDA Response in Cultured Mouse Brain Neurons. Nature 1987, 325, 529–531. [Google Scholar] [CrossRef]
- Chatterton, J.E.; Awobuluyi, M.; Premkumar, L.S.; Takahashi, H.; Talantova, M.; Shin, Y.; Cui, J.; Tu, S.; Sevarino, K.A.; Nakanishi, N.; et al. Excitatory Glycine Receptors Containing the NR3 Family of NMDA Receptor Subunits. Nature 2002, 415, 793–798. [Google Scholar] [CrossRef]
- Grand, T.; Abi Gerges, S.; David, M.; Diana, M.A.; Paoletti, P. Unmasking GluN1/GluN3A Excitatory Glycine NMDA Receptors. Nat. Commun. 2018, 9, 4769. [Google Scholar] [CrossRef] [PubMed]
- Otsu, Y.; Darcq, E.; Pietrajtis, K.; Mátyás, F.; Schwartz, E.; Bessaih, T.; Abi Gerges, S.; Rousseau, C.V.; Grand, T.; Dieudonné, S.; et al. Control of Aversion by Glycine-Gated GluN1/GluN3A NMDA Receptors in the Adult Medial Habenula. Science 2019, 366, 250–254. [Google Scholar] [CrossRef]
- Bossi, S.; Dhanasobhon, D.; Ellis-Davies, G.C.R.; Frontera, J.; De Brito Van Velze, M.; Lourenço, J.; Murillo, A.; Luján, R.; Casado, M.; Perez-Otaño, I.; et al. GluN3A Excitatory Glycine Receptors Control Adult Cortical and Amygdalar Circuits. Neuron 2022, 110, 2438–2454.e8. [Google Scholar] [CrossRef]
- Laboute, T.; Zucca, S.; Holcomb, M.; Patil, D.N.; Garza, C.; Wheatley, B.A.; Roy, R.N.; Forli, S.; Martemyanov, K.A. Orphan Receptor GPR158 Serves as a Metabotropic Glycine Receptor: mGlyR. Science 2023, 379, 1352–1358. [Google Scholar] [CrossRef]
- Raiteri, M. Presynaptic Metabotropic Glutamate and GABABReceptors. In Pharmacology of Neurotransmitter Release; Südhof, T.C., Starke, K., Eds.; Springer: Berlin/Heidelberg, Germany, 2008; pp. 373–407. ISBN 978-3-540-74805-2. [Google Scholar]
- Feuerstein, T.J. Presynaptic Receptors for Dopamine, Histamine, and Serotonin. In Pharmacology of Neurotransmitter Release; Südhof, T.C., Starke, K., Eds.; Springer: Berlin/Heidelberg, Germany, 2008; pp. 289–338. ISBN 978-3-540-74805-2. [Google Scholar]
- Lee, E.; Cho, J.; Choi, I.; Nakamura, M.; Park, H.; Lee, J.; Lee, M.; Choi, B.; Jang, I. Presynaptic Glycine Receptors Facilitate Spontaneous Glutamate Release onto Hilar Neurons in the Rat Hippocampus. J. Neurochem. 2009, 109, 275–286. [Google Scholar] [CrossRef]
- Hernandes, M.S.; De Magalhães, L.; Troncone, L.R.P. Glycine Stimulates the Release of Labeled Acetylcholine but Not Dopamine nor Glutamate from Superfused Rat Striatal Tissue. Brain Res. 2007, 1168, 32–37. [Google Scholar] [CrossRef]
- Waseem, T.V.; Fedorovich, S.V. Presynaptic Glycine Receptors Influence Plasma Membrane Potential and Glutamate Release. Neurochem. Res. 2010, 35, 1188–1195. [Google Scholar] [CrossRef]
- Pittaluga, A. Presynaptic Release-regulating NMDA Receptors in Isolated Nerve Terminals: A Narrative Review. Br. J. Pharmacol. 2021, 178, 1001–1017. [Google Scholar] [CrossRef]
- Kerchner, G.A.; Wang, G.-D.; Qiu, C.-S.; Huettner, J.E.; Zhuo, M. Direct Presynaptic Regulation of GABA/Glycine Release by Kainate Receptors in the Dorsal Horn. Neuron 2001, 32, 477–488. [Google Scholar] [CrossRef]
- Romei, C.; Raiteri, M.; Raiteri, L. Glycine Release Is Regulated by Metabotropic Glutamate Receptors Sensitive to mGluR2/3 Ligands and Activated by N-Acetylaspartylglutamate (NAAG). Neuropharmacology 2013, 66, 311–316. [Google Scholar] [CrossRef]
- Kalinina, N.I.; Zaitsev, A.V.; Vesselkin, N.P. Presynaptic Serotonin 5-HT1B/D Receptor-Mediated Inhibition of Glycinergic Transmission to the Frog Spinal Motoneurons. J. Comp. Physiol. A 2018, 204, 329–337. [Google Scholar] [CrossRef]
- Zappettini, S.; Mura, E.; Grilli, M.; Preda, S.; Salamone, A.; Olivero, G.; Govoni, S.; Marchi, M. Different Presynaptic Nicotinic Receptor Subtypes Modulate in vivo and in vitro the Release of Glycine in the Rat Hippocampus. Neurochem. Int. 2011, 59, 729–738. [Google Scholar] [CrossRef]
- Piniella, D.; Zafra, F. Functional Crosstalk of the Glycine Transporter GlyT1 and NMDA Receptors. Neuropharmacology 2023, 232, 109514. [Google Scholar] [CrossRef]
- Harvey, R.J.; Yee, B.K. Glycine Transporters as Novel Therapeutic Targets in Schizophrenia, Alcohol Dependence and Pain. Nat. Rev. Drug Discov. 2013, 12, 866–885. [Google Scholar] [CrossRef]
- Cioffi, C.L.; Guzzo, P.R. Inhibitors of Glycine Transporter-1: Potential Therapeutics for the Treatment of CNS Disorders. CTMC 2016, 16, 3404–3437. [Google Scholar] [CrossRef]
- Jonas, P.; Bischofberger, J.; Sandkühler, J. Corelease of Two Fast Neurotransmitters at a Central Synapse. Science 1998, 281, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Dumoulin, A.; Triller, A.; Dieudonné, S. IPSC Kinetics at Identified GABAergic and Mixed GABAergic and Glycinergic Synapses onto Cerebellar Golgi Cells. J. Neurosci. 2001, 21, 6045–6057. [Google Scholar] [CrossRef]
- Simat, M.; Parpan, F.; Fritschy, J. Heterogeneity of Glycinergic and Gabaergic Interneurons in the Granule Cell Layer of Mouse Cerebellum. J. Comp. Neurol. 2007, 500, 71–83. [Google Scholar] [CrossRef] [PubMed]
- Seal, R.; Edwards, R. Functional Implications of Neurotransmitter Co-Release: Glutamate and GABA Share the Load. Curr. Opin. Pharmacol. 2006, 6, 114–119. [Google Scholar] [CrossRef]
- Ishibashi, H.; Yamaguchi, J.; Nakahata, Y.; Nabekura, J. Dynamic Regulation of Glycine–GABA Co-transmission at Spinal Inhibitory Synapses by Neuronal Glutamate Transporter. J. Physiol. 2013, 591, 3821–3832. [Google Scholar] [CrossRef]
- Aubrey, K.R.; Supplisson, S. Heterogeneous Signaling at GABA and Glycine Co-Releasing Terminals. Front. Synaptic Neurosci. 2018, 10, 40. [Google Scholar] [CrossRef]
- Romei, C.; Bonifacino, T.; Milanese, M.; Usai, C.; Raiteri, L. Colocalization of Neurotransmitter Transporters on the Plasma Membrane of the Same Nerve Terminal May Reflect Cotransmission. Brain Res. Bull. 2016, 127, 100–110. [Google Scholar] [CrossRef]
- Hirrlinger, J.; Marx, G.; Besser, S.; Sicker, M.; Köhler, S.; Hirrlinger, P.G.; Wojcik, S.M.; Eulenburg, V.; Winkler, U.; Hülsmann, S. GABA-Glycine Cotransmitting Neurons in the Ventrolateral Medulla: Development and Functional Relevance for Breathing. Front. Cell. Neurosci. 2019, 13, 517. [Google Scholar] [CrossRef]
- Bonanno, G.; Raiteri, M. Release-Regulating Presynaptic Heterocarriers. Prog. Neurobiol. 1994, 44, 451–462. [Google Scholar] [CrossRef]
- Raiteri, L.; Raiteri, M.; Bonanno, G. Coexistence and Function of Different Neurotransmitter Transporters in the Plasma Membrane of CNS Neurons. Prog. Neurobiol. 2002, 68, 287–309. [Google Scholar] [CrossRef]
- Bonanno, G.; Raiteri, L.; Paluzzi, S.; Zappettini, S.; Usai, C.; Raiteri, M. Co-Existence of GABA and Glu Transporters in the Central Nervous System. CTMC 2006, 6, 979–988. [Google Scholar] [CrossRef]
- Vizi, E.; Fekete, A.; Karoly, R.; Mike, A. Non-Synaptic Receptors and Transporters Involved in Brain Functions and Targets of Drug Treatment. Br. J. Pharmacol. 2010, 160, 785–809. [Google Scholar] [CrossRef]
- Román, V.; Kedves, R.; Kelemen, K.; Némethy, Z.; Sperlágh, B.; Lendvai, B.; Vizi, E.S. Contribution of Analog Signaling to Neurotransmitter Interactions and Behavior: Role of Transporter-Mediated Nonquantal Dopamine Release. Physiol. Rep. 2021, 9, e15088. [Google Scholar] [CrossRef]
- Raiteri, L.; Raiteri, M. Synaptosomes Still Viable after 25 Years of Superfusion. Neurochem. Res. 2000, 25, 1265–1274. [Google Scholar] [CrossRef]
- Popoli, M.; Yan, Z.; McEwen, B.S.; Sanacora, G. The Stressed Synapse: The Impact of Stress and Glucocorticoids on Glutamate Transmission. Nat. Rev. Neurosci. 2012, 13, 22–37. [Google Scholar] [CrossRef]
- Kammerer, M.; Brawek, B.; Freiman, T.M.; Jackisch, R.; Feuerstein, T.J. Effects of Antiepileptic Drugs on Glutamate Release from Rat and Human Neocortical Synaptosomes. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2011, 383, 531–542. [Google Scholar] [CrossRef]
- Raiteri, L.; Stigliani, S.; Siri, A.; Passalacqua, M.; Melloni, E.; Raiteri, M.; Bonanno, G. Glycine Taken up through GLYT1 and GLYT2 Heterotransporters into Glutamatergic Axon Terminals of Mouse Spinal Cord Elicits Release of Glutamate by Homotransporter Reversal and through Anion Channels. Biochem. Pharmacol. 2005, 69, 159–168. [Google Scholar] [CrossRef]
- Raiteri, L.; Stigliani, S.; Patti, L.; Usai, C.; Bucci, G.; Diaspro, A.; Raiteri, M.; Bonanno, G. Activation of Γ-aminobutyric Acid GAT-1 Transporters on Glutamatergic Terminals of Mouse Spinal Cord Mediates Glutamate Release through Anion Channels and by Transporter Reversal. J. Neurosci. Res. 2005, 80, 424–433. [Google Scholar] [CrossRef]
- Raiteri, L.; Stigliani, S.; Usai, C.; Diaspro, A.; Paluzzi, S.; Milanese, M.; Raiteri, M.; Bonanno, G. Functional Expression of Release-Regulating Glycine Transporters GLYT1 on GABAergic Neurons and GLYT2 on Astrocytes in Mouse Spinal Cord. Neurochem. Int. 2008, 52, 103–112. [Google Scholar] [CrossRef]
- Milanese, M.; Romei, C.; Usai, C.; Oliveri, M.; Raiteri, L. A New Function for Glycine GlyT2 Transporters: Stimulation of Γ-aminobutyric Acid Release from Cerebellar Nerve Terminals through GAT1 Transporter Reversal and Ca2+-dependent Anion Channels. J. Neurosci. Res. 2014, 92, 398–408. [Google Scholar] [CrossRef] [PubMed]
- Milanese, M.; Bonifacino, T.; Fedele, E.; Rebosio, C.; Cattaneo, L.; Benfenati, F.; Usai, C.; Bonanno, G. Exocytosis Regulates Trafficking of GABA and Glycine Heterotransporters in Spinal Cord Glutamatergic Synapses: A Mechanism for the Excessive Heterotransporter-Induced Release of Glutamate in Experimental Amyotrophic Lateral Sclerosis. Neurobiol. Dis. 2015, 74, 314–324. [Google Scholar] [CrossRef] [PubMed]
- Cubelos, B.; Giménez, C.; Zafra, F. Localization of the GLYT1 Glycine Transporter at Glutamatergic Synapses in the Rat Brain. Cereb. Cortex 2005, 15, 448–459. [Google Scholar] [CrossRef] [PubMed]
- Cubelos, B.; Leite, C.; Giménez, C.; Zafra, F. Localization of the Glycine Transporter GLYT1 in Glutamatergic Synaptic Vesicles. Neurochem. Int. 2014, 73, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Musante, V.; Summa, M.; Cunha, R.A.; Raiteri, M.; Pittaluga, A. Pre-Synaptic Glycine GlyT1 Transporter—NMDA Receptor Interaction: Relevance to NMDA Autoreceptor Activation in the Presence of Mg2+ Ions: GlyT1/NMDA Autoreceptor Functional Cross-Talk. J. Neurochem. 2011, 117, 516–527. [Google Scholar] [CrossRef] [PubMed]
- Marques, B.L.; Oliveira-Lima, O.C.; Carvalho, G.A.; De Almeida Chiarelli, R.; Ribeiro, R.I.; Parreira, R.C.; Da Madeira Freitas, E.M.; Resende, R.R.; Klempin, F.; Ulrich, H.; et al. Neurobiology of Glycine Transporters: From Molecules to Behavior. Neurosci. Biobehav. Rev. 2020, 118, 97–110. [Google Scholar] [CrossRef] [PubMed]
- Danbolt, N.C.; Furness, D.N.; Zhou, Y. Neuronal vs Glial Glutamate Uptake: Resolving the Conundrum. Neurochem. Int. 2016, 98, 29–45. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Hassel, B.; Eid, T.; Danbolt, N.C. Axon-Terminals Expressing EAAT2 (GLT-1; Slc1a2) Are Common in the Forebrain and Not Limited to the Hippocampus. Neurochem. Int. 2019, 123, 101–113. [Google Scholar] [CrossRef]
- Danbolt, N.C.; López-Corcuera, B.; Zhou, Y. Reconstitution of GABA, Glycine and Glutamate Transporters. Neurochem. Res. 2022, 47, 85–110. [Google Scholar] [CrossRef]
- Burnstock, G. Cotransmission. Curr. Opin. Pharmacol. 2004, 4, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Svensson, E.; Apergis-Schoute, J.; Burnstock, G.; Nusbaum, M.P.; Parker, D.; Schiöth, H.B. General Principles of Neuronal Co-Transmission: Insights from Multiple Model Systems. Front. Neural Circuits 2019, 12, 117. [Google Scholar] [CrossRef]
- Bonanno, G.; Vallebuona, F.; Donadini, F.; Fontana, G.; Fedele, E.; Raiteri, M. Heterocarrier-Mediated Reciprocal Modulation of Glutamate and Glycine Release in Rat Cerebral Cortex and Spinal Cord Synaptosomes. Eur. J. Pharmacol. 1994, 252, 61–67. [Google Scholar] [CrossRef]
- Raiteri, L.; Paolucci, E.; Prisco, S.; Raiteri, M.; Bonanno, G. Activation of a Glycine Transporter on Spinal Cord Neurons Causes Enhanced Glutamate Release in a Mouse Model of Amyotrophic Lateral Sclerosis. Br. J. Pharmacol. 2003, 138, 1021–1025. [Google Scholar] [CrossRef]
- Gurney, M.E.; Pu, H.; Chiu, A.Y.; Dal Canto, M.C.; Polchow, C.Y.; Alexander, D.D.; Caliendo, J.; Hentati, A.; Kwon, Y.W.; Deng, H.-X.; et al. Motor Neuron Degeneration in Mice That Express a Human Cu,Zn Superoxide Dismutase Mutation. Science 1994, 264, 1772–1775. [Google Scholar] [CrossRef] [PubMed]
- Raiteri, L.; Stigliani, S.; Zappettini, S.; Mercuri, N.B.; Raiteri, M.; Bonanno, G. Excessive and Precocious Glutamate Release in a Mouse Model of Amyotrophic Lateral Sclerosis. Neuropharmacology 2004, 46, 782–792. [Google Scholar] [CrossRef] [PubMed]
- Milanese, M.; Zappettini, S.; Onofri, F.; Musazzi, L.; Tardito, D.; Bonifacino, T.; Messa, M.; Racagni, G.; Usai, C.; Benfenati, F.; et al. Abnormal Exocytotic Release of Glutamate in a Mouse Model of Amyotrophic Lateral Sclerosis. J. Neurochem. 2011, 116, 1028–1042. [Google Scholar] [CrossRef] [PubMed]
- Muller, E.; Bakkar, W.; Martina, M.; Sokolovski, A.; Wong, A.Y.C.; Legendre, P.; Bergeron, R. Vesicular Storage of Glycine in Glutamatergic Terminals in Mouse Hippocampus. Neuroscience 2013, 242, 110–127. [Google Scholar] [CrossRef] [PubMed]
- Harsing, L.G.; Matyus, P. Mechanisms of Glycine Release, Which Build up Synaptic and Extrasynaptic Glycine Levels: The Role of Synaptic and Non-Synaptic Glycine Transporters. Brain Res. Bull. 2013, 93, 110–119. [Google Scholar] [CrossRef]
- Marshak, D.W.; Chuang, A.Z.; Dolino, D.M.; Jacoby, R.A.; Liu, W.S.; Long, Y.; Sherman, M.B.; Suh, J.M.; Vila, A.; Mills, S.L. Synaptic Connections of Amacrine Cells Containing Vesicular Glutamate Transporter 3 in Baboon Retinas. Vis. Neurosci. 2015, 32, E006. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Zhang, Y.; Chen, M.; Zhou, Z.J. Segregated Glycine-Glutamate Co-Transmission from vGluT3 Amacrine Cells to Contrast-Suppressed and Contrast-Enhanced Retinal Circuits. Neuron 2016, 90, 27–34. [Google Scholar] [CrossRef]
- Cifuentes, F.; Morales, M.A. Functional Implications of Neurotransmitter Segregation. Front. Neural Circuits 2021, 15, 738516. [Google Scholar] [CrossRef]
- Cunha Xavier Pinto, M.; Lima, I.V.D.A.; Pessoa Da Costa, F.L.; Rosa, D.V.; Mendes-Goulart, V.A.; Resende, R.R.; Romano-Silva, M.A.; Pinheiro De Oliveira, A.C.; Gomez, M.V.; Gomez, R.S. Glycine Transporters Type 1 Inhibitor Promotes Brain Preconditioning against NMDA-Induced Excitotoxicity. Neuropharmacology 2015, 89, 274–281. [Google Scholar] [CrossRef]
- Shen, H.-Y.; Van Vliet, E.A.; Bright, K.-A.; Hanthorn, M.; Lytle, N.K.; Gorter, J.; Aronica, E.; Boison, D. Glycine Transporter 1 Is a Target for the Treatment of Epilepsy. Neuropharmacology 2015, 99, 554–565. [Google Scholar] [CrossRef] [PubMed]
- Cortese, K.; Gagliani, M.C.; Raiteri, L. Interactions between Glycine and Glutamate through Activation of Their Transporters in Hippocampal Nerve Terminals. Biomedicines 2023, 11, 3152. [Google Scholar] [CrossRef]
- Raiteri, L.; Zappettini, S.; Stigliani, S.; Paluzzi, S.; Raiteri, M.; Bonanno, G. Glutamate Release Induced by Activation of Glycine and GABA Transporters in Spinal Cord Is Enhanced in a Mouse Model of Amyotrophic Lateral Sclerosis. Neurotoxicology 2005, 26, 883–892. [Google Scholar] [CrossRef]
- Milanese, M.; Zappettini, S.; Jacchetti, E.; Bonifacino, T.; Cervetto, C.; Usai, C.; Bonanno, G. In Vitro Activation of GAT1 Transporters Expressed in Spinal Cord Gliosomes Stimulates Glutamate Release That Is Abnormally Elevated in the SOD1/G93A(+) Mouse Model of Amyotrophic Lateral Sclerosis. J. Neurochem. 2010, 113, 489–501. [Google Scholar] [CrossRef]
- Raiteri, L.; Raiteri, M.; Bonanno, G. Glycine Is Taken up through GLYT1 and GLYT2 Transporters into Mouse Spinal Cord Axon Terminals and Causes Vesicular and Carrier-Mediated Release of Its Proposed Co-Transmitter GABA. J. Neurochem. 2001, 76, 1823–1832. [Google Scholar] [CrossRef] [PubMed]
- Raiteri, M.; Bonanno, G.; Pende, M. γ-Aminobutyric Acid and Glycine Modulate Each Other’s Release Through Heterocarriers Sited on the Releasing Axon Terminals of Rat CNS. J. Neurochem. 1992, 59, 1481–1489. [Google Scholar] [CrossRef]
- Romei, C.; Raiteri, M.; Raiteri, L. GABA Transporters Mediate Glycine Release from Cerebellum Nerve Endings: Roles of Ca2+channels, Mitochondrial Na+/Ca2+ Exchangers, Vesicular GABA/Glycine Transporters and Anion Channels. Neurochem. Int. 2012, 61, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Raiteri, L.; Raiteri, M. Multiple Functions of Neuronal Plasma Membrane Neurotransmitter Transporters. Prog. Neurobiol. 2015, 134, 1–16. [Google Scholar] [CrossRef]
- Dumontier, D.; Mailhes-Hamon, C.; Supplisson, S.; Dieudonné, S. Neurotransmitter Content Heterogeneity within an Interneuron Class Shapes Inhibitory Transmission at a Central Synapse. Front. Cell. Neurosci. 2023, 16, 1060189. [Google Scholar] [CrossRef]
- Dugué, G.P.; Dumoulin, A.; Triller, A.; Dieudonné, S. Target-Dependent Use of Coreleased Inhibitory Transmitters at Central Synapses. J. Neurosci. 2005, 25, 6490–6498. [Google Scholar] [CrossRef]
- Crook, J.; Hendrickson, A.; Robinson, F.R. Co-Localization of Glycine and Gaba Immunoreactivity in Interneurons in Macaca Monkey Cerebellar Cortex. Neuroscience 2006, 141, 1951–1959. [Google Scholar] [CrossRef] [PubMed]
- Van Den Bosch, L.; Van Damme, P.; Bogaert, E.; Robberecht, W. The Role of Excitotoxicity in the Pathogenesis of Amyotrophic Lateral Sclerosis. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2006, 1762, 1068–1082. [Google Scholar] [CrossRef]
- Pradhan, J.; Bellingham, M.C. Neurophysiological Mechanisms Underlying Cortical Hyper-Excitability in Amyotrophic Lateral Sclerosis: A Review. Brain Sci. 2021, 11, 549. [Google Scholar] [CrossRef] [PubMed]
- Scamps, F.; Aimond, F.; Hilaire, C.; Raoul, C. Synaptic Transmission and Motoneuron Excitability Defects in Amyotrophic Lateral Sclerosis. In Amyotrophic Lateral Sclerosis; Araki, T., Ed.; Exon Publications: Brisbane, Australia, 2021; ISBN 978-0-645-00177-8. [Google Scholar]
- King, A.E.; Woodhouse, A.; Kirkcaldie, M.T.K.; Vickers, J.C. Excitotoxicity in ALS: Overstimulation, or Overreaction? Exp. Neurol. 2016, 275, 162–171. [Google Scholar] [CrossRef]
- Nijssen, J.; Comley, L.H.; Hedlund, E. Motor Neuron Vulnerability and Resistance in Amyotrophic Lateral Sclerosis. Acta Neuropathol. 2017, 133, 863–885. [Google Scholar] [CrossRef]
- Le Gall, L.; Anakor, E.; Connolly, O.; Vijayakumar, U.G.; Duddy, W.J.; Duguez, S. Molecular and Cellular Mechanisms Affected in ALS. J. Pers. Med. 2020, 10, 101. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Jarquín, U.N.; Tapia, R. Excitatory and Inhibitory Neuronal Circuits in the Spinal Cord and Their Role in the Control of Motor Neuron Function and Degeneration. ACS Chem. Neurosci. 2018, 9, 211–216. [Google Scholar] [CrossRef]
- Bonifacino, T.; Musazzi, L.; Milanese, M.; Seguini, M.; Marte, A.; Gallia, E.; Cattaneo, L.; Onofri, F.; Popoli, M.; Bonanno, G. Altered Mechanisms Underlying the Abnormal Glutamate Release in Amyotrophic Lateral Sclerosis at a Pre-Symptomatic Stage of the Disease. Neurobiol. Dis. 2016, 95, 122–133. [Google Scholar] [CrossRef]
- Armada-Moreira, A.; Gomes, J.I.; Pina, C.C.; Savchak, O.K.; Gonçalves-Ribeiro, J.; Rei, N.; Pinto, S.; Morais, T.P.; Martins, R.S.; Ribeiro, F.F.; et al. Going the Extra (Synaptic) Mile: Excitotoxicity as the Road Toward Neurodegenerative Diseases. Front. Cell. Neurosci. 2020, 14, 90. [Google Scholar] [CrossRef]
- Kazama, M.; Kato, Y.; Kakita, A.; Noguchi, N.; Urano, Y.; Masui, K.; Niida-Kawaguchi, M.; Yamamoto, T.; Watabe, K.; Kitagawa, K.; et al. Astrocytes Release Glutamate via Cystine/Glutamate Antiporter Upregulated in Response to Increased Oxidative Stress Related to Sporadic Amyotrophic Lateral Sclerosis. Neuropathology 2020, 40, 587–598. [Google Scholar] [CrossRef]
- Milanese, M.; Bonifacino, T.; Torazza, C.; Provenzano, F.; Kumar, M.; Ravera, S.; Zerbo, A.R.; Frumento, G.; Balbi, M.; Nguyen, T.P.N.; et al. Blocking Glutamate mGlu5 Receptors with the Negative Allosteric Modulator CTEP Improves Disease Course in SOD1G93A Mouse Model of Amyotrophic Lateral Sclerosis. Br. J. Pharmacol. 2021, 178, 3747–3764. [Google Scholar] [CrossRef]
- Torazza, C.; Provenzano, F.; Gallia, E.; Cerminara, M.; Balbi, M.; Bonifacino, T.; Tessitore, S.; Ravera, S.; Usai, C.; Musante, I.; et al. Genetic Downregulation of the Metabotropic Glutamate Receptor Type 5 Dampens the Reactive and Neurotoxic Phenotype of Adult ALS Astrocytes. Cells 2023, 12, 1952. [Google Scholar] [CrossRef] [PubMed]
- Bonifacino, T.; Rebosio, C.; Provenzano, F.; Torazza, C.; Balbi, M.; Milanese, M.; Raiteri, L.; Usai, C.; Fedele, E.; Bonanno, G. Enhanced Function and Overexpression of Metabotropic Glutamate Receptors 1 and 5 in the Spinal Cord of the SOD1G93A Mouse Model of Amyotrophic Lateral Sclerosis during Disease Progression. Int. J. Mol. Sci. 2019, 20, 4552. [Google Scholar] [CrossRef]
- Harsing, L.G.; Szénási, G.; Zelles, T.; Köles, L. Purinergic-Glycinergic Interaction in Neurodegenerative and Neuroinflammatory Disorders of the Retina. Int. J. Mol. Sci. 2021, 22, 6209. [Google Scholar] [CrossRef]
- Izidoro Ribeiro, R.; Almeida Carvalho, G.; Almeida Chiareli, R.; Vieira De Assis Lima, I.; Quaglio Bellozi, P.M.; Oliveira-Lima, O.C.; Oliveira Giacomelli, Á.; Birbrair, A.; Santiago Gomez, R.; Pinheiro De Oliveira, A.C.; et al. Glycine Transporter-1 Inhibition by NFPS Promotes Neuroprotection against Striatal Damage Models. Neurosci. Lett. 2024, 826, 137715. [Google Scholar] [CrossRef]
- Cioffi, C.L. Inhibition of Glycine Re-Uptake: A Potential Approach for Treating Pain by Augmenting Glycine-Mediated Spinal Neurotransmission and Blunting Central Nociceptive Signaling. Biomolecules 2021, 11, 864. [Google Scholar] [CrossRef] [PubMed]
- Werdehausen, R.; Mittnacht, S.; Bee, L.A.; Minett, M.S.; Armbruster, A.; Bauer, I.; Wood, J.N.; Hermanns, H.; Eulenburg, V. The Lidocaine Metabolite N-Ethylglycine Has Antinociceptive Effects in Experimental Inflammatory and Neuropathic Pain. PAIN 2015, 156, 1647. [Google Scholar] [CrossRef]
- Oyama, M.; Kuraoka, S.; Watanabe, S.; Iwai, T.; Tanabe, M. Electrophysiological Evidence of Increased Glycine Receptor-Mediated Phasic and Tonic Inhibition by Blockade of Glycine Transporters in Spinal Superficial Dorsal Horn Neurons of Adult Mice. J. Pharmacol. Sci. 2017, 133, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Armbruster, A.; Neumann, E.; Kötter, V.; Hermanns, H.; Werdehausen, R.; Eulenburg, V. The GlyT1 Inhibitor Bitopertin Ameliorates Allodynia and Hyperalgesia in Animal Models of Neuropathic and Inflammatory Pain. Front. Mol. Neurosci. 2018, 10, 438. [Google Scholar] [CrossRef]
- Winters, B.L.; Rawling, T.; Vandenberg, R.J.; Christie, M.J.; Bhola, R.F.; Imlach, W.L. Activity of Novel Lipid Glycine Transporter Inhibitors on Synaptic Signalling in the Dorsal Horn of the Spinal Cord. Br. J. Pharmacol. 2018, 175, 2337–2347. [Google Scholar] [CrossRef]
- Oyama, M.; Watanabe, S.; Iwai, T.; Tanabe, M. Distinct Synaptic Mechanisms Underlying the Analgesic Effects of γ-Aminobutyric Acid Transporter Subtypes 1 and 3 Inhibitors in the Spinal Dorsal Horn. PAIN 2022, 163, 334. [Google Scholar] [CrossRef] [PubMed]
- Peiser-Oliver, J.M.; Evans, S.; Adams, D.J.; Christie, M.J.; Vandenberg, R.J.; Mohammadi, S.A. Glycinergic Modulation of Pain in Behavioral Animal Models. Front. Pharmacol. 2022, 13, 860903. [Google Scholar] [CrossRef]
- Gallagher, C.I.; Frangos, Z.J.; Sheipouri, D.; Shimmon, S.; Duman, M.-N.; Jayakumar, S.; Cioffi, C.L.; Rawling, T.; Vandenberg, R.J. Novel Phenylene Lipids That Are Positive Allosteric Modulators of Glycine Receptors and Inhibitors of Glycine Transporter 2. ACS Chem. Neurosci. 2023, 14, 2634–2647. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, K.; Hara, K.; Haranishi, Y.; Terada, T.; Sata, T. The Antinociceptive Effect of SNAP5114, a Gamma-Aminobutyric Acid Transporter-3 Inhibitor, in Rat Experimental Pain Models. Anesth. Analg. 2013, 116, 1162–1169. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Li, Y.; Gu, P.; Fu, B.; Liu, F.; Li, E. Analgesic Effect of Intrathecally γ-Aminobutyric Acid Transporter-1 Inhibitor NO-711 Administrating on Neuropathic Pain in Rats. Neurosci. Lett. 2011, 494, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Zaręba, P.; Sałat, K.; Höfner, G.C.; Łątka, K.; Bajda, M.; Latacz, G.; Kotniewicz, K.; Rapacz, A.; Podkowa, A.; Maj, M.; et al. Development of Tricyclic N-Benzyl-4-Hydroxybutanamide Derivatives as Inhibitors of GABA Transporters mGAT1-4 with Anticonvulsant, Antinociceptive, and Antidepressant Activity. Eur. J. Med. Chem. 2021, 221, 113512. [Google Scholar] [CrossRef] [PubMed]
- Pradier, B.; Segelcke, D.; Reichl, S.; Zahn, P.K.; Pogatzki-Zahn, E.M. Spinal GABA Transporter 1 Contributes to Evoked-Pain Related Behavior but Not Resting Pain after Incision Injury. Front. Mol. Neurosci. 2023, 16, 1282151. [Google Scholar] [CrossRef] [PubMed]
- Al-Khrasani, M.; Mohammadzadeh, A.; Balogh, M.; Király, K.; Barsi, S.; Hajnal, B.; Köles, L.; Zádori, Z.S.; Harsing, L.G. Glycine Transporter Inhibitors: A New Avenue for Managing Neuropathic Pain. Brain Res. Bull. 2019, 152, 143–158. [Google Scholar] [CrossRef] [PubMed]
- Mohammadzadeh, A.; Lakatos, P.P.; Balogh, M.; Zádor, F.; Karádi, D.Á.; Zádori, Z.S.; Király, K.; Galambos, A.R.; Barsi, S.; Riba, P.; et al. Pharmacological Evidence on Augmented Antiallodynia Following Systemic Co-Treatment with GlyT-1 and GlyT-2 Inhibitors in Rat Neuropathic Pain Model. Int. J. Mol. Sci. 2021, 22, 2479. [Google Scholar] [CrossRef]
- Galambos, A.R.; Papp, Z.T.; Boldizsár, I.; Zádor, F.; Köles, L.; Harsing, L.G.; Al-Khrasani, M. Glycine Transporter 1 Inhibitors: Predictions on Their Possible Mechanisms in the Development of Opioid Analgesic Tolerance. Biomedicines 2024, 12, 421. [Google Scholar] [CrossRef]
- Mostyn, S.N.; Rawling, T.; Mohammadi, S.; Shimmon, S.; Frangos, Z.J.; Sarker, S.; Yousuf, A.; Vetter, I.; Ryan, R.M.; Christie, M.J.; et al. Development of an N-Acyl Amino Acid That Selectively Inhibits the Glycine Transporter 2 To Produce Analgesia in a Rat Model of Chronic Pain. J. Med. Chem. 2019, 62, 2466–2484. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.A.; Mostyn, S.N.; Frangos, Z.J.; Shimmon, S.; Rawling, T.; Vandenberg, R.J.; O’Mara, M.L. The Allosteric Inhibition of Glycine Transporter 2 by Bioactive Lipid Analgesics Is Controlled by Penetration into a Deep Lipid Cavity. J. Biol. Chem. 2021, 296, 100282. [Google Scholar] [CrossRef]
- Song, I.; Cho, S.; Nedeljkovic, S.S.; Lee, S.R.; Lee, C.; Kim, J.; Bai, S.J. Role of VVZ-149, a Novel Analgesic Molecule, in the Affective Component of Pain: Results from an Exploratory Proof-of-Concept Study of Postoperative Pain Following Laparoscopic and Robotic-Laparoscopic Gastrectomy. Pain Med. 2021, 22, 2037–2049. [Google Scholar] [CrossRef]
- Javitt, D.C. Cognitive Impairment Associated with Schizophrenia: From Pathophysiology to Treatment. Annu. Rev. Pharmacol. Toxicol. 2023, 63, 119–141. [Google Scholar] [CrossRef] [PubMed]
- Cioffi, C.L. Glycine Transporter-1 Inhibitors: A Patent Review (2011–2016). Expert Opin. Ther. Pat. 2018, 28, 197–210. [Google Scholar] [CrossRef] [PubMed]
- Bugarski-Kirola, D.; Blaettler, T.; Arango, C.; Fleischhacker, W.W.; Garibaldi, G.; Wang, A.; Dixon, M.; Bressan, R.A.; Nasrallah, H.; Lawrie, S.; et al. Bitopertin in Negative Symptoms of Schizophrenia—Results from the Phase III FlashLyte and DayLyte Studies. Biol. Psychiatry 2017, 82, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Pinard, E.; Borroni, E.; Koerner, A.; Umbricht, D.; Alberati, D. Glycine Transporter Type I (GlyT1) Inhibitor, Bitopertin: A Journey from Lab to Patient. Chimia 2018, 72, 477. [Google Scholar] [CrossRef] [PubMed]
- Moschetti, V.; Schlecker, C.; Wind, S.; Goetz, S.; Schmitt, H.; Schultz, A.; Liesenfeld, K.-H.; Wunderlich, G.; Desch, M. Multiple Rising Doses of Oral BI 425809, a GlyT1 Inhibitor, in Young and Elderly Healthy Volunteers: A Randomised, Double-Blind, Phase I Study Investigating Safety and Pharmacokinetics. Clin. Drug Investig. 2018, 38, 737–750. [Google Scholar] [CrossRef]
- Fleischhacker, W.W.; Podhorna, J.; Gröschl, M.; Hake, S.; Zhao, Y.; Huang, S.; Keefe, R.S.E.; Desch, M.; Brenner, R.; Walling, D.P.; et al. Efficacy and Safety of the Novel Glycine Transporter Inhibitor BI 425809 Once Daily in Patients with Schizophrenia: A Double-Blind, Randomised, Placebo-Controlled Phase 2 Study. Lancet Psychiatry 2021, 8, 191–201. [Google Scholar] [CrossRef]
- Lobo, M.C.; Whitehurst, T.S.; Kaar, S.J.; Howes, O.D. New and Emerging Treatments for Schizophrenia: A Narrative Review of Their Pharmacology, Efficacy and Side Effect Profile Relative to Established Antipsychotics. Neurosci. Biobehav. Rev. 2022, 132, 324–361. [Google Scholar] [CrossRef]
- Goh, K.K.; Wu, T.-H.; Chen, C.-H.; Lu, M.-L. Efficacy of N-Methyl-D-Aspartate Receptor Modulator Augmentation in Schizophrenia: A Meta-Analysis of Randomised, Placebo-Controlled Trials. J. Psychopharmacol. 2021, 35, 236–252. [Google Scholar] [CrossRef] [PubMed]
- De Bartolomeis, A.; Vellucci, L.; Austin, M.C.; De Simone, G.; Barone, A. Rational and Translational Implications of D-Amino Acids for Treatment-Resistant Schizophrenia: From Neurobiology to the Clinics. Biomolecules 2022, 12, 909. [Google Scholar] [CrossRef] [PubMed]
- De Bartolomeis, A.; Manchia, M.; Marmo, F.; Vellucci, L.; Iasevoli, F.; Barone, A. Glycine Signaling in the Framework of Dopamine-Glutamate Interaction and Postsynaptic Density. Implications for Treatment-Resistant Schizophrenia. Front. Psychiatry 2020, 11, 369. [Google Scholar] [CrossRef]
- Eulenburg, V.; Hülsmann, S. Synergistic Control of Transmitter Turnover at Glycinergic Synapses by GlyT1, GlyT2, and ASC-1. Int. J. Mol. Sci. 2022, 23, 2561. [Google Scholar] [CrossRef] [PubMed]
- Errico, F.; Rossi, S.; Napolitano, F.; Catuogno, V.; Topo, E.; Fisone, G.; D’Aniello, A.; Centonze, D.; Usiello, A. D-Aspartate Prevents Corticostriatal Long-Term Depression and Attenuates Schizophrenia-Like Symptoms Induced by Amphetamine and MK-801. J. Neurosci. 2008, 28, 10404–10414. [Google Scholar] [CrossRef] [PubMed]
- Sacchi, S.; Novellis, V.D.; Paolone, G.; Nuzzo, T.; Iannotta, M.; Belardo, C.; Squillace, M.; Bolognesi, P.; Rosini, E.; Motta, Z.; et al. Olanzapine, but Not Clozapine, Increases Glutamate Release in the Prefrontal Cortex of Freely Moving Mice by Inhibiting D-Aspartate Oxidase Activity. Sci. Rep. 2017, 7, 46288. [Google Scholar] [CrossRef] [PubMed]
- Nasyrova, R.F.; Khasanova, A.K.; Altynbekov, K.S.; Asadullin, A.R.; Markina, E.A.; Gayduk, A.J.; Shipulin, G.A.; Petrova, M.M.; Shnayder, N.A. The Role of D-Serine and D-Aspartate in the Pathogenesis and Therapy of Treatment-Resistant Schizophrenia. Nutrients 2022, 14, 5142. [Google Scholar] [CrossRef]
- Souza, I.N.D.O.; Roychaudhuri, R.; De Belleroche, J.; Mothet, J.-P. D-Amino Acids: New Clinical Pathways for Brain Diseases. Trends Mol. Med. 2023, 29, 1014–1028. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.-P.; Chang, W.-H.; Mao, Y.-W.; Cheng, M.-C.; Zhuang, X.-Y.; Kuo, C.-S.; Lai, Y.-A.; Shih, T.-M.; Chou, T.-Y.; Tsai, G.E. The Development of a Regulator of Human Serine Racemase for N-Methyl-D-Aspartate Function. Biomedicines 2024, 12, 853. [Google Scholar] [CrossRef]
- Sabatini, B.L.; Tian, L. Imaging Neurotransmitter and Neuromodulator Dynamics In Vivo with Genetically Encoded Indicators. Neuron 2020, 108, 17–32. [Google Scholar] [CrossRef]
- Da, Y.; Luo, S.; Tian, Y. Real-Time Monitoring of Neurotransmitters in the Brain of Living Animals. ACS Appl. Mater. Interfaces 2023, 15, 138–157. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, N.; Zheng, F.; van Brederode, J.; Berger, A.; Leacock, S.; Hirata, H.; Paige, C.J.; Harvey, R.J.; Alzheimer, C.; Villmann, C. Functional Consequences of the Postnatal Switch from Neonatal to Mutant Adult Glycine Receptor α1 Subunits in the Shaky Mouse Model of Startle Disease. Front. Mol. Neurosci. 2018, 11, 167. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, N.; Harvey, R.J.; Villmann, C. Startle Disease: New Molecular Insights into an Old Neurological Disorder. Neuroscientist 2023, 29, 767–781. [Google Scholar] [CrossRef] [PubMed]
- Söderpalm, B.; Lidö, H.H.; Ericson, M. The Glycine Receptor—A Functionally Important Primary Brain Target of Ethanol. Alcohol. Clin. Exp. Res. 2017, 41, 1816–1830. [Google Scholar] [CrossRef] [PubMed]
- Loftén, A.; Adermark, L.; Ericson, M.; Söderpalm, B. Regulation of ethanol-mediated dopamine elevation by glycine receptors located on cholinergic interneurons in the nucleus accumbens. Addict. Biol. 2023, 28, e13349. [Google Scholar] [CrossRef]
- Hansen, K.B.; Wollmuth, L.P.; Bowie, D.; Furukawa, H.; Menniti, F.S.; Sobolevsky, A.I.; Swanson, G.T.; Swanger, S.A.; Greger, I.H.; Nakagawa, T.; et al. Structure, Function, and Pharmacology of Glutamate Receptor Ion Channels. Pharmacol. Rev. 2021, 73, 298–487. [Google Scholar] [CrossRef]
- Mony, L.; Paoletti, P. Mechanisms of NMDA receptor regulation. Curr. Opin. Neurobiol. 2023, 83, 102815. [Google Scholar] [CrossRef]
- Thompson, S.M. Modulators of GABAA receptor-mediated inhibition in the treatment of neuropsychiatric disorders: Past, present, and future. Neuropsychopharmacology 2024, 49, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Richardson, R.J.; Petrou, S.; Bryson, A. Established and emerging GABAA receptor pharmacotherapy for epilepsy. Front. Pharmacol. 2024, 15, 1341472. [Google Scholar] [CrossRef]
- Vandenberg, R.J.; Ryan, R.M.; Carland, J.E.; Imlach, W.L.; Christie, M.J. Glycine Transport Inhibitors for the Treatment of Pain. Trends Pharmacol. Sci. 2014, 35, 423–430. [Google Scholar] [CrossRef]
- Burgos, C.F.; Yévenes, G.E.; Aguayo, L.G. Structure and Pharmacologic Modulation of Inhibitory Glycine Receptors. Mol. Pharmacol. 2016, 90, 318–325. [Google Scholar] [CrossRef]
- Zafra, F.; Ibáñez, I.; Bartolomé-Martín, D.; Piniella, D.; Arribas-Blázquez, M.; Giménez, C. Glycine Transporters and Its Coupling with NMDA Receptors. In Glial Amino Acid Transporters; Ortega, A., Schousboe, A., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 55–83. ISBN 978-3-319-55769-4. [Google Scholar]
- Zeilhofer, H.U.; Acuña, M.A.; Gingras, J.; Yévenes, G.E. Glycine Receptors and Glycine Transporters: Targets for Novel Analgesics? Cell. Mol. Life Sci. 2018, 75, 447–465. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, C.I.; Ha, D.A.; Harvey, R.J.; Vandenberg, R.J. Positive Allosteric Modulators of Glycine Receptors and Their Potential Use in Pain Therapies. Pharmacol. Rev. 2022, 74, 933–961. [Google Scholar] [CrossRef] [PubMed]
- Nedeljkovic, S.S.; Song, I.; Bao, X.; Zeballos, J.L.; Correll, D.J.; Zhang, Y.; Ledley, J.S.; Bhandari, A.; Bai, X.; Lee, S.R.; et al. Exploratory Study of VVZ-149, a Novel Analgesic Molecule, in the Affective Component of Acute Postoperative Pain after Laparoscopic Colorectal Surgery. J. Clin. Anesth. 2022, 76, 110576. [Google Scholar] [CrossRef]
- Yee, B.K.; Balic, E.; Singer, P.; Schwerdel, C.; Grampp, T.; Gabernet, L.; Knuesel, I.; Benke, D.; Feldon, J.; Mohler, H.; et al. Disruption of Glycine Transporter 1 Restricted to Forebrain Neurons Is Associated with a Procognitive and Antipsychotic Phenotypic Profile. J. Neurosci. 2006, 26, 3169–3181. [Google Scholar] [CrossRef]
- Möhler, H.; Boison, D.; Singer, P.; Feldon, J.; Pauly-Evers, M.; Yee, B.K. Glycine Transporter 1 as a Potential Therapeutic Target for Schizophrenia-Related Symptoms: Evidence from Genetically Modified Mouse Models and Pharmacological Inhibition. Biochem. Pharmacol. 2011, 81, 1065–1077. [Google Scholar] [CrossRef] [PubMed]
- Katz, P.S.; Edwards, D.H. Metamodulation: The Control and Modulation of Neuromodulation. In Beyond Neurotransmission: Neuromodulation and Its Importance for Information Processing; Katz, P., Ed.; Oxford University Press: Oxford, UK, 1999; pp. 349–382. ISBN 978-0-19-852424-3. [Google Scholar]
- Fuxe, K.; Marcellino, D.; Leo, G.; Agnati, L.F. Molecular Integration via Allosteric Interactions in Receptor Heteromers. A Working Hypothesis. Curr. Opin. Pharmacol. 2010, 10, 14–22. [Google Scholar] [CrossRef]
- Sebastião, A.M.; Ribeiro, J.A. Neuromodulation and Metamodulation by Adenosine: Impact and Subtleties upon Synaptic Plasticity Regulation. Brain Res. 2015, 1621, 102–113. [Google Scholar] [CrossRef]
- Pittaluga, A.; Marchi, M. Synaptosomes and Metamodulation of Receptors. In Synaptic Vesicles: Methods and Protocols; Dahlmanns, J., Dahlmanns, M., Eds.; Springer: New York, NY, USA, 2022; pp. 99–111. ISBN 978-1-07-161916-2. [Google Scholar]
- Olivero, G.; Grilli, M.; Marchi, M.; Pittaluga, A. Metamodulation of Presynaptic NMDA Receptors: New Perspectives for Pharmacological Interventions. Neuropharmacology 2023, 234, 109570. [Google Scholar] [CrossRef]
- Pittaluga, A.; Grilli, M.; Olivero, G. Progress in Metamodulation and Receptor-Receptor Interaction: From Physiology to Pathology and Therapy. Neuropharmacology 2023, 237, 109639. [Google Scholar] [CrossRef]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raiteri, L. Interactions Involving Glycine and Other Amino Acid Neurotransmitters: Focus on Transporter-Mediated Regulation of Release and Glycine–Glutamate Crosstalk. Biomedicines 2024, 12, 1518. https://doi.org/10.3390/biomedicines12071518
Raiteri L. Interactions Involving Glycine and Other Amino Acid Neurotransmitters: Focus on Transporter-Mediated Regulation of Release and Glycine–Glutamate Crosstalk. Biomedicines. 2024; 12(7):1518. https://doi.org/10.3390/biomedicines12071518
Chicago/Turabian StyleRaiteri, Luca. 2024. "Interactions Involving Glycine and Other Amino Acid Neurotransmitters: Focus on Transporter-Mediated Regulation of Release and Glycine–Glutamate Crosstalk" Biomedicines 12, no. 7: 1518. https://doi.org/10.3390/biomedicines12071518
APA StyleRaiteri, L. (2024). Interactions Involving Glycine and Other Amino Acid Neurotransmitters: Focus on Transporter-Mediated Regulation of Release and Glycine–Glutamate Crosstalk. Biomedicines, 12(7), 1518. https://doi.org/10.3390/biomedicines12071518






