Workflow for Maxilla/Mandible Individual [Mai®] Implant by Integra Implants—How Individual Implants Are Manufactured
Abstract
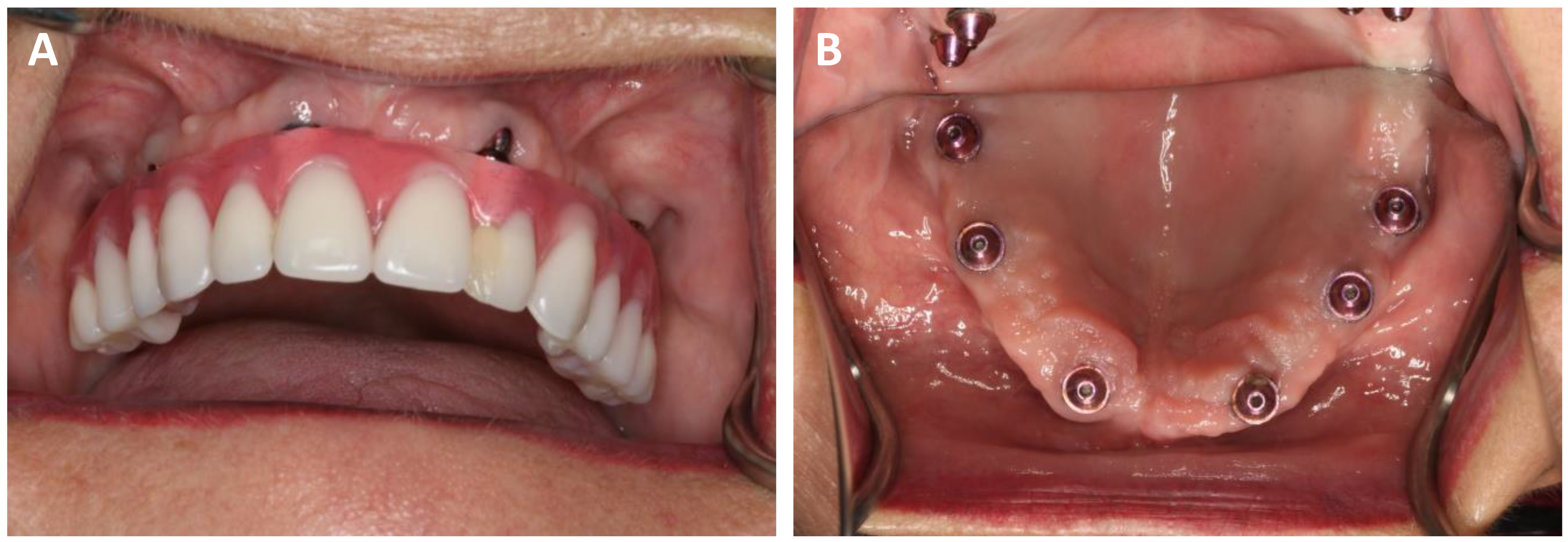
:1. Introduction
2. Materials and Methods
2.1. Patients’ Qualification for the Operation
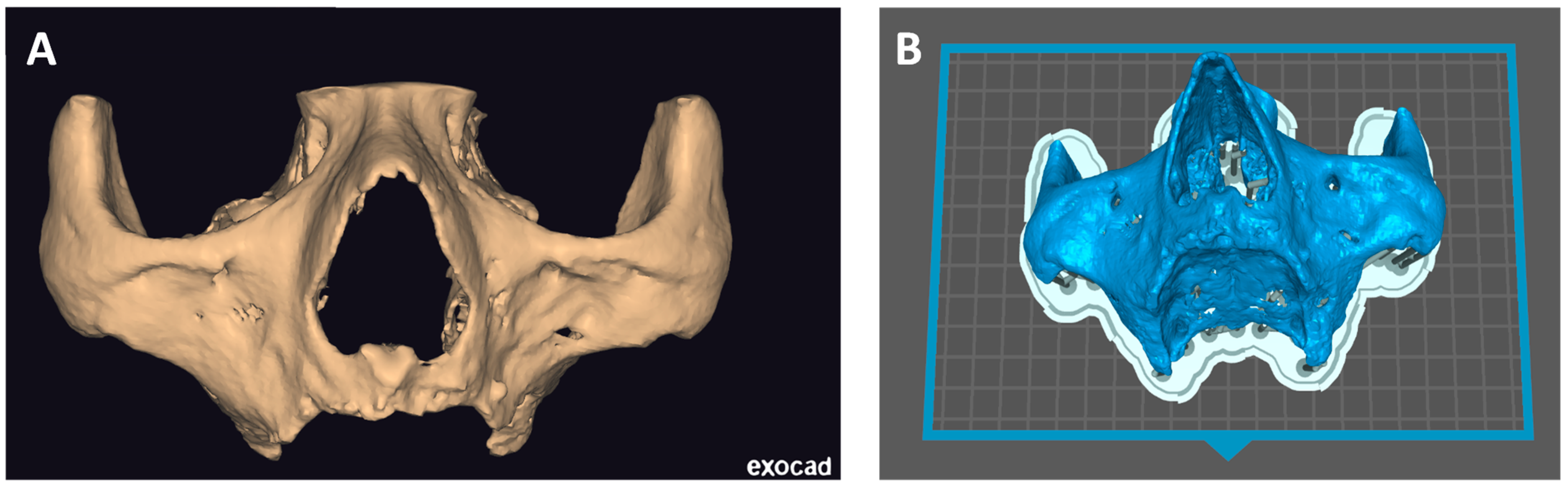
2.2. Computational Preparing and Printing of a Skull
2.3. Mai Implant® Design
2.4. Manufacturing
2.4.1. Mesh Creation
2.4.2. 3D Printing and Milling
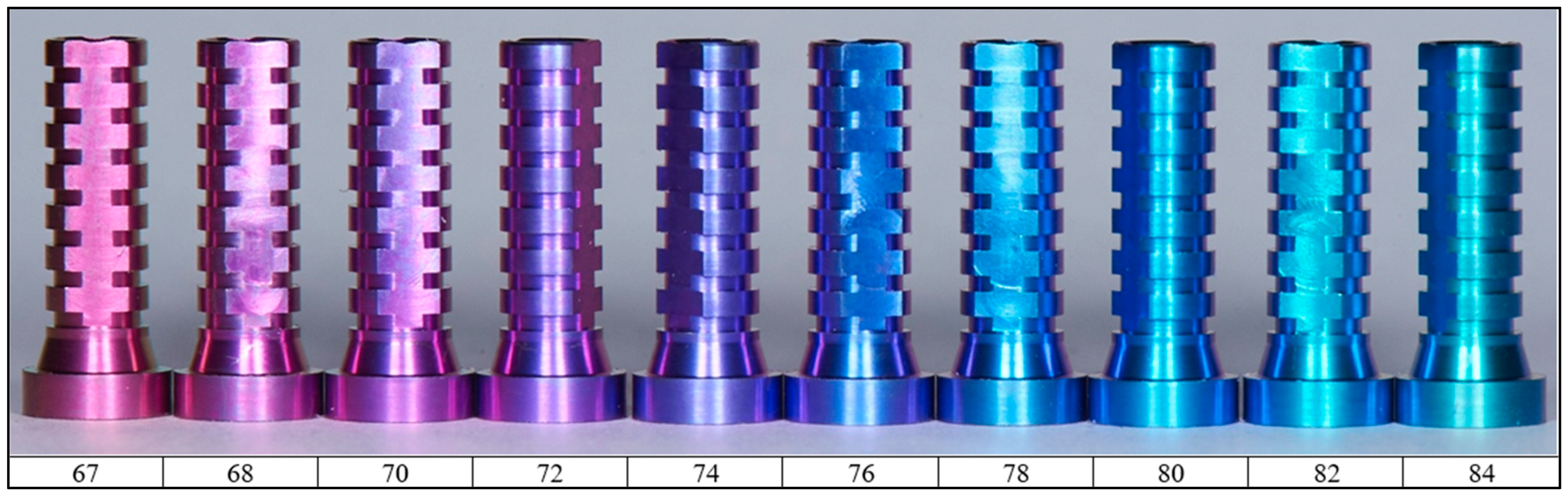
2.4.3. Cleaning, Rinsing, Anodizing and Laser Marking
2.5. Cleaning and Sterilization Process in a Hospital or Dental Clinic
3. Discussion
- (A)
- Multiunits movements—6%;
- (B)
- Implants exposure—9%;
- (C)
- Recurrent swelling—5%.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tomasi, C.; Tessarolo, F.; Caola, I.; Piccoli, F.; Wennström, J.L.; Nollo, G.; Berglundh, T. Early Healing of Peri-Implant Mucosa in Man. J. Clin. Periodontol. 2016, 43, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Branemark, P.I. Osseointegration and Its Experimental Background. J. Prosthet. Dent. 1983, 50, 399–410. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Survival and Complications of Zygomatic Implants: An Updated Systematic Review. J. Oral Maxillofac. Surg. 2016, 74, 1949–1964. [Google Scholar] [CrossRef] [PubMed]
- Carinci, F.; Farina, A.; Zanetti, U.; Vinci, R.; Negrini, S.; Calura, G.; Laino, G.; Piattelli, A. Alveolar Ridge Augmentation: A Comparative Longitudinal Study between Calvaria and Iliac Crest Bone Grafts. J. Oral Implantol. 2005, 31, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Mertens, C.; Decker, C.; Seeberger, R.; Hoffmann, J.; Sander, A.; Freier, K. Early Bone Resorption after Vertical Bone Augmentation—A Comparison of Calvarial and Iliac Grafts. Clin. Oral Implants Res. 2013, 24, 820–825. [Google Scholar] [CrossRef] [PubMed]
- García-Garzon, J.R.; Villasboas-Rosciolesi, D.; Baquero, M.; Bassa, P.; Soler, M.; Riera, E. Augmentation Procedures for the Rehabilitation of Deficient Edentulous Ridges with Oral Implants. Clin. Nucl. Med. 2016, 41, 664–665. [Google Scholar] [CrossRef] [PubMed]
- Davó, R.; David, L. Quad Zygoma: Technique and Realities. Oral Maxillofac. Surg. Clin. N. Am. 2019, 31, 285–297. [Google Scholar] [CrossRef] [PubMed]
- Zalewska, A.; Antonowicz, B.; Szulimowska, J.; Zieniewska-Siemieńczuk, I.; Leśniewska, B.; Borys, J.; Zięba, S.; Kostecka-Sochoń, P.; Żendzian-Piotrowska, M.; Lo Giudice, R.; et al. Mitochondrial Redox Balance of Fibroblasts Exposed to Ti-6Al-4V Microplates Subjected to Different Types of Anodizing. Int. J. Mol. Sci. 2023, 24, 12896. [Google Scholar] [CrossRef] [PubMed]
- Wozniak, L.; Ratajczak-Wrona, W.; Borys, J.; Antonowicz, B.; Nowak, K.; Bortnik, P.; Jablonska, E. Levels of Biological Markers of Nitric Oxide in Serum of Patients with Mandible Fractures. J. Clin. Med. 2021, 10, 2832. [Google Scholar] [CrossRef]
- Do, T.A.; Le, H.S.; Shen, Y.W.; Huang, H.L.; Fuh, L.J. Risk Factors Related to Late Failure of Dental Implant—A Systematic Review of Recent Studies. Int. J. Environ. Res. Public Health 2020, 17, 3931. [Google Scholar] [CrossRef]
- Heimes, D.; Schiegnitz, E.; Kuchen, R.; Kämmerer, P.W.; Al-nawas, B. Buccal Bone Thickness in Anterior and Posterior Teeth—A Systematic Review. Healthcare 2021, 9, 1663. [Google Scholar] [CrossRef]
- Wang, J.; Zhu, R.; Liu, Y.; Zhang, L. Understanding Melt Pool Characteristics in Laser Powder Bed Fusion: An Overview of Single- and Multi-Track Melt Pools for Process Optimization. Adv. Powder Mater. 2023, 2, 100137. [Google Scholar] [CrossRef]
- Alipal, J.; Lee, T.C.; Koshy, P.; Abdullah, H.Z.; Idris, M.I. Evolution of Anodised Titanium for Implant Applications. Heliyon 2021, 7, e07408. [Google Scholar] [CrossRef] [PubMed]
- Babilas, D.; Urbańczyk, E.; Sowa, M.; Maciej, A.; Korotin, D.M.; Zhidkov, I.S.; Basiaga, M.; Krok-Borkowicz, M.; Szyk-Warszyńska, L.; Pamuła, E.; et al. On the electropolishing and anodic oxidation of Ti-15Mo alloy. Electrochim. Acta 2016, 205, 2156–2265. [Google Scholar] [CrossRef]
- Sowa, M.; Greń, K.; Kukharenko, A.I.; Korotin, D.M.; Michalska, J.; Szyk-Warszyńska, L.; Mosiałek, M.; Zak, J.; Pamuła, E.; Kurmaev, E.Z.; et al. Influence of electropolishing and anodic oxidation on morphology, chemical composition and corrosion resistance of niobium. Mater. Sci. Eng. C 2014, 42, 529–537. [Google Scholar] [CrossRef]
- Govindaraj, S.; Muthuraman, M.S. Systematic Review on Sterilization Methods of Implants and Medical Devices. Int. J. ChemTech Res. 2015, 8, 897–911. [Google Scholar]
- PN-EN 13060+A1:2018-12; Małe Sterylizatory Parowe. Polski Komitet Normalizacyjny: Warsaw, Poland, 2018.
- PN-EN 285+A1:2022-03; Sterylizacja—Sterylizatory Parowe—Duże Sterylizatory. Polski Komitet Normalizacyjny: Warsaw, Poland, 2022.
- PN-EN 556-1:2002; Sterylizacja Wyrobów Medycznych—Wymagania Dotyczące Wyrobów Medycznych Określanych Jako STERYLNE—Część 1: Wymagania Dotyczące Finalnie Sterylizowanych Wyrobów Medycznych. Polski Komitet Normalizacyjny: Warsaw, Poland, 2002.
- ISO 17665-1:2006; Sterilization of Health Care Products Moist Heat Part 1: Requirements for the Development, Validation and Routine Control of a Sterilization Process for Medical Devices. International Organization for Standardization: Geneva, Switzerland, 2006.
- PN-EN ISO 11607-1:2020-06; Opakowania Dla Finalnie Sterylizowanych Wyrobów Medycznych—Część 1: Wymagania Dotyczące Materiałów, Systemów Bariery Sterylnej i Systemów Opakowaniowych. International Organization for Standardization: Geneva, Switzerland, 2020.
- Orłowska, A.; Kajzer, W.; Goldsztajn, K.; Gawron, A.; Godzierz, M.; Nowińska, K.; Basiaga, M.; Simka, W.; Szewczenko, J. Functionalization of 3D printed Ti6Al4V high-porous spinal implant surface with use of plasma electrolytic oxidation. Appl. Surf. Sci. 2024, 659, 159948. [Google Scholar] [CrossRef]
- Mishchenko, O.; Kopchak, A.; Chernohorskyi, D.; Deineka, V.; Waloszczyk, N.; Pogorielov, M.; Simka, W. Craniofacial reconstruction using 3D personalized implants with enhanced surface properties: Technological and clinical aspects. Appl. Surf. Sci. Adv. 2023, 16, 100437. [Google Scholar] [CrossRef]
- Vattanasup, C.; Kuntiyaratana, T.; Rungsiyakull, P.; Chaijareenont, P. Color Formation on Titanium Surface Treated by Anodization and the Surface Characteristics: A Review. Chiang Mai Dent. J. 2023, 44, 13–21. [Google Scholar] [CrossRef]
- Le Guéhennec, L.; Soueidan, A.; Layrolle, P.; Amouriq, Y. Surface Treatments of Titanium Dental Implants for Rapid Osseointegration. Dent. Mater. 2007, 23, 844–854. [Google Scholar] [CrossRef]
- Velasco-Ortega, E.; Ortiz-García, I.; Jiménez-Guerra, A.; Monsalve-Guil, L.; Muñoz-Guzón, F.; Perez, R.A.; Gil, F.J. Comparison between Sandblasted Acid-Etched and Oxidized Titanium Dental Implants: In Vivo Study. Int. J. Mol. Sci. 2019, 20, 3267. [Google Scholar] [CrossRef]
- Sul, Y.T.; Johansson, C.B.; Röser, K.; Albrektsson, T. Qualitative and Quantitative Observations of Bone Tissue Reactions to Anodised Implants. Biomaterials 2002, 23, 1809–1817. [Google Scholar] [CrossRef] [PubMed]
- Al-Nawas, B.; Groetz, K.A.; Goetz, H.; Duschner, H.; Wagner, W. Comparative Histomorphometry and Resonance Frequency Analysis of Implants with Moderately Rough Surfaces in a Loaded Animal Model. Clin. Oral Implants Res. 2008, 19, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Jayasree, A.; Ivanovski, S.; Gulati, K. Enhanced Corrosion Resistance and Local Therapy from Nano-Engineered Titanium Dental Implants. In Surface Modification of Titanium Dental Implants; Springer: Berlin/Heidelberg, Germany, 2023; pp. 153–198. [Google Scholar] [CrossRef]
- Minhas, B.; Dino, S.; Zuo, Y.; Qian, H.; Zhao, X. Improvement of Corrosion Resistance of Tio2 Layers in Strong Acidic Solutions by Anodizing and Thermal Oxidation Treatment. Materials 2021, 14, 1188. [Google Scholar] [CrossRef] [PubMed]
- Ningrum, E.O.; Khoiroh, I.; Nastiti, H.I.; Affan, R.A.; Karisma, A.D.; Agustiani, E.; Surono, A.; Suroto, H.; Suprapto, S.; Taji, L.S.; et al. Surface Coating Effect on Corrosion Resistance of Titanium Alloy Bone Implants by Anodizing Method. Int. J. Technol. 2023, 14, 749–760. [Google Scholar] [CrossRef]
- Traini, T.; Murmura, G.; Sinjari, B.; Perfetti, G.; Scarano, A.; D’Arcangelo, C.; Caputi, S. The Surface Anodization of Titanium Dental Implants Improves Blood Clot Formation Followed by Osseointegration. Coatings 2018, 8, 252. [Google Scholar] [CrossRef]
- Villaça-Carvalho, M.F.L.; de Araújo, J.C.R.; Beraldo, J.M.; Do Prado, R.F.; de Moraes, M.E.L.; Manhães Junior, L.R.C.; Codaro, E.N.; Acciari, H.A.; Machado, J.P.B.; Regone, N.N.; et al. Bioactivity of an Experimental Dental Implant with Anodized Surface. J. Funct. Biomater. 2021, 12, 39. [Google Scholar] [CrossRef] [PubMed]
- Drira, M.; Hentati, F.; Babich, O.; Sukhikh, S.; Larina, V.; Sharifian, S.; Homaei, A.; Fendri, I.; Lemos, M.F.L.; Félix, C.; et al. Bioactive Carbohydrate Polymers—Between Myth and Reality. Molecules 2021, 26, 7068. [Google Scholar] [CrossRef] [PubMed]
- Jankowski, T.; Jankowska, A.; Kazimierczak, N.; Kazimierczak, W.; Janiszewska-Olszowska, J. The Significance of Keratinized Mucosa in Implant Therapy: Narrative Literature Review and Case Report Presentation. J. Clin. Med. 2024, 13, 3501. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aparicio, C.; Polido, W.D.; Chehade, A.; Shenouda, M.; Simon, M.; Simon, P.; Al-Nawas, B. Round and flat zygomatic implants: Effectiveness after a 3-year follow-up non-interventional study. Int. J. Implant. Dent. 2024, 10, 30. [Google Scholar] [CrossRef] [PubMed]








| Description | Requirements |
|---|---|
| Time of a scan | Not older than 3 months |
| Rows × pixels | 512 × 512 |
| Tube voltage | 90–120 kVp |
| Slice thickness for CT | 0.5–0.7 mm |
| Slice thickness for CBCT | 0.15 mm |
| Feed per rotation | Max. 1.0 mm |
| Reconstructed slice increment | Max. 1.0 mm |
| Reconstruction algorithm | High-resolution bone |
| File extension | DICOM [Digital Imaging and Communication in Medicine] |
| Compression | Uncompressed |
| Optional | Overlapping axial slices |
| Patient preparation | Remove any non-permanent metal prostheses (if possible, also permanent) and other types of extracorporeal metal (jewelry). Ensure adequate head immobilization and instruct the patient not to swallow during examinations, especially during CBCT, and to remain motionless. The patient may not appear during the entire examination. |
| Temperature | 134 °C |
| Exposition time | ≥4 min |
| Drying time | >20–30 min |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zieliński, R.; Kołkowska, A.; Sowiński, J.; Konieczny, B.; Kozakiewicz, M.; Simka, W. Workflow for Maxilla/Mandible Individual [Mai®] Implant by Integra Implants—How Individual Implants Are Manufactured. Biomedicines 2024, 12, 1773. https://doi.org/10.3390/biomedicines12081773
Zieliński R, Kołkowska A, Sowiński J, Konieczny B, Kozakiewicz M, Simka W. Workflow for Maxilla/Mandible Individual [Mai®] Implant by Integra Implants—How Individual Implants Are Manufactured. Biomedicines. 2024; 12(8):1773. https://doi.org/10.3390/biomedicines12081773
Chicago/Turabian StyleZieliński, Rafał, Agata Kołkowska, Jerzy Sowiński, Bartłomiej Konieczny, Marcin Kozakiewicz, and Wojciech Simka. 2024. "Workflow for Maxilla/Mandible Individual [Mai®] Implant by Integra Implants—How Individual Implants Are Manufactured" Biomedicines 12, no. 8: 1773. https://doi.org/10.3390/biomedicines12081773






